Abstract
Purpose
The objectives were to study the effect of a single dose of intravenous (IV) zoledronic acid (ZA) on changes in bone mineral density (BMD) (lumbar spine (LS), hip, & distal forearm), trabecular bone score (TBS) and bone turnover markers (BTMs) in postmenopausal osteoporotic women with and without diabetes over 12 months.
Methods
Patients were divided into two groups: type 2 diabetes mellitus (T2DM) (n = 40) and non-DM (n = 40). Both groups received a single dose of 4 mg IV ZA at baseline. The BMD with TBS and BTMs (β-CTX, sclerostin, P1NP) were measured at baseline, six months, and 12 months.
Results
At baseline, BMD in all three sites was similar in both groups. T2DM patients were older and had lower BTMs than non-DM patients. The mean increase in LS-BMD (gram/cm2) at 12 months in T2DM and the non-DM group was 3.6 ± 4.7% and 6.2 ± 4.7 %, respectively (P = 0.01). However, the age adjusted mean difference in LS BMD increment between two groups at one year was − 2.86 % (−5.02% to −0.69%), P = 0.01. There was a comparable change in BMD at other two sites, BTMs, and TBS in both the groups over one year follow-up.
Conclusion
The gain in the LS-BMD was significantly lower in T2DM group compared to non-DM subjects over 12 months after a single IV infusion of 4 mg ZA. The explanation for this could be low bone turnover in diabetes subjects at baseline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a silent disease that causes disruption of bone architecture and increases the risk of fragility fractures [1]. The prevalence of type 2 diabetes mellitus (T2DM) increases with age. So, a significant number of postmenopausal women have both diabetes and osteoporosis in the world [2]. Bisphosphonates (BP) are commonly used drugs for managing postmenopausal osteoporosis (PMO) [3]. These drugs help in decreasing bone loss by suppressing osteoclastic activity. Zoledronic acid (ZA) is the most potent BP used for the treatment of osteoporosis [4]. It is particularly useful when the bone turnover markers (BTMs) are high (e.g., postmenopausal state).
Studies have shown normal or high bone mineral density (BMD) in patients with T2DM [5, 6]. The risk of fractures increases in patients with diabetes irrespective of their BMD because of the poor bone quality [7]. The alteration in the quality of bone is due to accumulation of advanced glycation end products and associated microvascular complications [8]. Trabecular bone score (TBS) is a marker of bone microarchitectural texture calculated from lumbar spine scans obtained during dual-energy X-ray absorptiometry (DXA) and predicts fracture risk independent of BMD [9]. Once-yearly intravenous (IV) ZA therapy significantly increased TBS along with BMD compared to placebo over two years in subjects of PMO [10]. However, the effect of ZA on TBS has not been compared between diabetes and non-diabetes PMO women. Hyperglycemia leads to low bone turnover in T2DM subjects because of its inhibitory effects on osteoblasts and osteoclasts [11, 12]. As both bone formation and resorption markers are low in T2DM subjects, and the information about BMD in them varies widely, the effect of ZA is expected to be different in PMO with and without T2DM.
Few studies have compared the effects of BPs on BMD, BTMs, and fractures in PMO with and without T2DM [13,14,15,16,17,18,19,20,21]. Studies on BPs like alendronate, risedronate, and ibandronate suggest that the improvement in BMD and fracture prevention in T2DM patients was not different from non-DM subjects [14,15,16,17]. However, the studies by both Yilmaz et al. and Dagdalen et al. showed lesser response to BPs in T2DM group [18, 19]. To the best of our knowledge, only one study compared the effect of ZA in PMO with and without T2DM, namely, the post hoc analysis of The Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly- Pivotal Fracture trial (HORIZON-PFT) [20, 21]. This study did not include any patients of Indian origin and Indians differ from Caucasians in skeletal size, BMD, and bone geometry [22]. Hence, we decided to compare the effects of ZA on BMD, TBS, BTMs, and incident fractures over one year in Indian PMO women with and without T2DM.
Subjects, Material and Methods
Study setting and participants
This prospective cohort pilot study was conducted in the department of Endocrinology of an academic research institute in India from October 2018 to January 2021. The primary objective was to compare the effect of a single 4 mg dose of intravenous ZA on changes in BMD at the lumbar spine (LS), femoral neck (FN), and total hip (TH) in PMO women with and without T2DM after 12 months of treatment. The secondary objectives were to study the effect of intravenous ZA on BMD at distal forearm (FA), TBS, BTMs, and incident fractures in them. This study was performed in line with the principles of the Declaration of Helsinki after obtaining the Institute Ethics Committee’s approval.
The patients attending endocrinology outpatient department and diagnosed to have osteoporosis fulfilling the inclusion and exclusion criteria were enrolled to the study after getting informed consent. Osteoporosis was defined as a BMD T-score of − 2.5 or less at the LS (L1–L4), FN, or TH. Women aged 50–80 years and postmenopausal for more than 5 years with BMD T-score of −2.5 or less were included in the study. They were screened for presence of both secondary causes of osteoporosis and T2DM. Patients with evidence of secondary osteoporosis, chronic kidney disease, chronic liver disease, rheumatological disorders, chronic infection, cancer, serum 25 hydroxyvitamin D[25(OH)D] < 12 ng/ml [23], and usage of medications known to affect the skeleton, for example, corticosteroids, anti-convulsants, thiazolidinediones, sodium-glucose cotransporter 2 inhibitors, bisphosphonates, teriparatide, calcitonin, hormone replacement therapy were excluded from this study. Patients were divided into T2DM and non-DM groups based on the American Diabetes Association criteria [24]. Those already on treatment for T2DM diagnosed prior were included in T2DM group, and the rest underwent an oral glucose tolerance test (OGTT) with 75-gram anhydrous glucose. Those diagnosed as having diabetes during OGTT were included in T2DM group, and the patients with normal glucose tolerance were included in non-DM group.
At baseline, detailed history, including age, years since menopause, past history, and family history of fracture(s), was taken. The history of any chronic disease or drug intake was asked to rule out secondary osteoporosis. Physical examination, including anthropometric evaluation, was done for all subjects. Body weight was measured using an electronic scale (1–300 kg accurate to the nearest 50 g). Height was measured to the nearest 0.1 cm by using a stadiometer. The subjects’ height was taken in the standing position, without footwear, keeping heads in the Frankfurt plane. Body mass index (BMI) was calculated by dividing the body weight in kg by the square of height in meters. Blood pressure was measured with an appropriately sized cuff using a digital sphygmomanometer, and the average of two readings was recorded.
Biochemical assay methods
Baseline laboratory investigations included fasting plasma beta-CrossLaps (β-CTX), amino-terminal propeptide of type 1 procollagen (P1NP), sclerostin, serum 25(OH)D, creatinine, calcium, albumin, phosphorus, thyroid function tests, liver function test (LFT), complete blood count and erythrocyte sedimentation rate. Fasting plasma β-CTX, P1NP, and serum 25(OH)D, along with calcium, albumin, phosphorus, and alkaline phosphatase (ALP), were repeated at six months and 12 months. However, plasma sclerostin was repeated only at 12 months. Venous blood samples were collected in the early morning after an overnight fast. Blood was collected in clot activator and dipotassium EDTA (K2-EDTA) tubes. Collected blood samples in clot activator tubes were kept for 15–30 min for clot formation and then centrifuged at 2500 rpm for 10 minutes at 4 °C. All parameters except BTMs were processed on the same day [25]. For BTMs, samples were centrifuged, and plasma was separated and stored at −80 ˚C. Stored plasma samples were batch analyzed at the end of the study.
Biochemical parameters, including calcium, phosphorus, albumin, LFT, and creatinine, were measured using a Beckman Coulter analyzer. The normal range of albumin-adjusted serum calcium, phosphorous, and ALP in our lab was 8.8–10.2 mg/dl, 2.5–4.5 mg/dl, and 30–120 IU/l, respectively. Serum 25(OH)D was measured by chemiluminometric technology (ADVIA Centaur XP Immunoassay System, Siemens Healthcare Global, USA). The range of detection of serum 25(OH) D was 4.2–150 ng/ml (10.5–375 nmol/L). The within run and total coefficient of variation (CV) of 25(OH)D assay were 7.0% and 11.1%, respectively. Both plasma β-CTX and P1NP were measured by electrochemiluminescence immunoassay (Cobas e411 immunoanalyzer, Roche diagnostics GmbH, Mannheim, Germany). The range of detection of β-CTX was 0.010–6.00 ng/ml. The intra-assay and inter-assay CVs for values between 0.03 and 0.5 ng/ml were < 10%, and those between 0.5 and 5 ng/ml were < 3% and < 6%, respectively. The range of detection of P1NP was 5–1200 ng/ml. The intra-assay and inter-assay CVs for values < 50 ng/ml were < 5% and < 7%, respectively, and for values between 50 and 500 ng/ml were < 4% and < 5%, respectively. The plasma sclerostin level was measured using the enzyme immunoassay kit (TECOmedical AG, Sissach, Switzerland). The lower limit of quantitation of plasma sclerostin was 0.025 ng/ml with both intra-assay and inter-assay CV < 5%.
Imaging
The patients underwent lateral and anteroposterior radiographs of the thoracic and lumbar spine (T4-L4) using the same x-ray machine at baseline, six months, and 12 months, or if the patient complained of back pain suggestive of vertebral fracture (VF). Radiographs were assessed using the Genant grading scale [26] by the same radiologist at all time points. The radiologist was blinded to the diabetes status of the subjects. Patients were considered to have a new VF if there was at least a grade increase in previously normal vertebrae. Determination of worsening of preexisting fractures also required an increase of at least one grade. Other findings were also noted, such as aortic calcification, soft tissue calcification, or any spinal abnormality, such as scoliosis or spondylolisthesis.
The BMD (in g/cm2) was measured at LS (L1-L4), FN, TH, FA and TBS at lumbar spine using a Hologic dual-energy x-ray absorptiometer (Hologic Discovery Wi) at baseline, six months and 12 months. The same technician carried out measurements for the entire study period and the quality control for the machine was performed with daily phantom scans for LS. The data from calibration and phantom scans were plotted and the least significant change (LSC) was calculated for the technologist. In vivo precision assessment of our technologist was done by measuring 15 patients three times following International Society for Clinical Densitometry guidelines [27]. These values were entered in the online LSC calculator, and precision error (CV) was obtained at a 95% confidence level (CI) for serial BMD testing [28]. The precision error was multiplied by 2.77 to yield the LSC. The precision errors for LS, FN, and TH were 1.24%, 1.72%, and 1.49%, respectively. The TBS was derived from the LS DXA image (L1 to L4) using TBS Osteo powered by TBS iNsight software v 3.1.1 (Medimaps, Geneva, Switzerland) [29]. A TBS value > 1.35 was labelled as normal microarchitecture, a value 1.2–1.35 was labelled as partially degraded microarchitecture, and a value < 1.2 was labelled as degraded bone microarchitecture. The patients with partially degraded microarchitecture and degraded bone microarchitecture were added together to calculate the proportion of low TBS in the study.
Treatment
All the patients received an IV infusion of 4 mg ZA in 100 ml normal saline over 30 minutes after documenting a normal ECG done at baseline. We have used 4 mg instead of 5 mg ZA based on the availability in our hospital. The patients were monitored for post-infusion adverse effects. Those subjects who developed flu-like illnesses were treated with paracetamol tablets. Patients were also advised to report immediately if they developed palpitations, carpopedal spasms, oliguria, or any allergic reaction after infusion. In addition to ZA, all patients in both groups received oral daily calcium (1000 mg) and cholecalciferol (500 IU/day) supplementation.
Statistical analysis
Analysis was carried out using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 21.0 for Windows). The distribution of the data of all continuous variables was assessed using the Shapiro-Wilk test for normality. Continuous and categorical variables were summarized using mean with standard deviation (SD) /median with inter-quartile range (IQR) and proportions, respectively. Test of significance of continuous variables between diabetes and non-diabetes group were assessed using an independent t-test or Mann-Whitney U test, depending on the normality. A significant difference between the categorical variables was evaluated using the chi-square test or Fisher’s exact test, whichever was applicable. The percentage change of BMD from baseline to 6 months [(BMD at 6 months - BMD at baseline)/BMD at baseline] was calculated for the DM group. Linear regression with BMD% change as the dependent variable and the presence of DM as the independent variable was done. The beta-coefficient (which is the mean difference between the BMD% change between the DM and non-DM groups) was reported. Adjusted beta-coefficient was estimated after adding age as a covariate. The same analysis was repeated for BMD% change from baseline to 12 months. Similar analysis was also done for BTM% change at both at 6 and 12 months. TBS was compared between DM and non-diabetes groups both at baseline and 12 months using independent t-test. Similarly, the proportion “low TBS” was compared between the two groups both at baseline and 12 months using chi-square test. As the sample size is greater than 30, linear regression was done assuming that the distribution of the parameter is normal, although the distribution of BMD% change seems non-normal. In all statistical tests, a p-value ≤ 0.05 was considered statistically significant.
Results
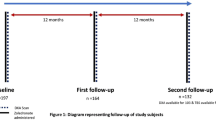
A total of 146 subjects were screened and eighty subjects (40 in each group) were finally included after eliminating 66 subjects, as shown in Fig. 1. Only two out of 40 T2DM patients were newly diagnosed with OGTT. The comparison between the baseline characteristics of two groups is presented in Table 1. The patients in diabetes group were older compared to those in non-diabetes group (60.5 (57.2–65) vs. 57.5 (53–64.7) years, p = 0.03) with a higher proportion of hypertensives (15 (37.5%) vs. 7 (17.5%), p = 0.04). However, there was no difference in the years since menopause between two groups. The mean duration of diabetes was 9 ± 6.1 years with 10 (25%) patients on insulin treatment. Metformin was prescribed for all of them. Other oral antidiabetes drugs taken by the patients were sulphonylureas (62.5%) and gliptins (15%). The blood glucose control was optimal, with median glycosylated hemoglobin (HbA1c) of 7.5% (58 mmol/mol) (IQR: 6.4–8.7%) (IQR: 46 mmol/mol–72 mmol/mol) and 42% of subjects had HbA1c ≤ 7% (53 mmol/mol). Hypertension was present in 22(27.5%) patients and was treated with anti-hypertensive medications (angiotensin-converting enzyme inhibitors-80%, angiotensin II receptor blockers-18%, calcium channel blockers- 31%). Hypothyroidism was present in 36 (45%) patients and was treated with levothyroxine to maintain a euthyroid state throughout the study period.
Nine (11%) patients had a history of clinical fractures (distal radius-2, vertebral-2, neck of femur-2, shaft of tibia-3), as shown in Table 1. VFs based on x-ray done at baseline in two groups are shown in Supplementary Table 1. Two patients in diabetes group and ten patients in non-diabetes group had a total of seventeen VFs at baseline (2(5%) vs. 10 (25%), p = 0.02). Diabetes subjects had lower plasma BTMs with higher serum calcium levels compared to non-diabetes subjects at the baseline. But all of them had serum calcium levels in the normal range. However, BMD measured at all four sites and TBS were similar in both groups.
Changes in bone mineral density, trabecular bone score, and incident fracture
The mean increase in LS-BMD in diabetes group was 3.6 ± 4.7%, and that in non-diabetes group was 6.2 ± 4.7 % at 12 months compared to the baseline (p = 0.01) (Table 2). The age adjusted mean difference in LS BMD increment between two groups at one year was − 2.86% (−5.02% to −0.69%), p = 0.01. The improvement in LS-BMD was more in first six months after the treatment in non-diabetes group, and the gains accumulated were maintained in later-half of the year (Fig. 2). In diabetes group, the improvement was uniform throughout the study period. There was no difference in BMD increment at other three sites between two groups during the study period. TBS was also similar in both groups at 12 months, as shown in Supplementary Table 2. One patient in non-diabetes group developed two new grade 1 VFs during a 12-month follow-up. There was no deterioration (i.e., increase in grading) of any prevalent fracture in either group during the study duration.
Change in biochemical parameters
Both β-CTX and P1NP were significantly lower at baseline in diabetes group. However, a similar reduction at 6 and 12 months from the baseline was noted in both groups (Table 3). The nadir level of both the markers was recorded at 6 months, following which there was a mild rise in the levels. At 12 months, both markers were below their baseline values, demonstrating the durability of response in both groups. Similarly, no difference in change in plasma sclerostin over one year was noted between two groups (Table 3). However, there was a significant increase in plasma sclerostin level in each group at 12 months following ZA administration compared to baseline (diabetes: 0.57 (0.43–0.74) vs. 0.64 (0.56–0.74), p = 0.008 & non-diabetes: 0.63 (0.55–0.75) vs. 0.70(0.55–0.88), p = 0.03). There was no difference in median HbA1c value between baseline and end of the study in the diabetes group (7.5% (58 mmol/mol) (6.4–8.7%) (46 mmol/mol–72 mmol/mol) vs. 8.15% (66 mmol/mol) (6.7–9.9%) (50 mmol/mol–85 mmol/mol), p = 0.26).
Adverse effects
Acute phase reactions (APR) were the most common adverse effects in this study, occurring within three days of the drug administration. 60 patients developed APR, with pyrexia being more common in non-diabetes group, as shown in Supplementary Table 3. Patients developing APR were treated symptomatically with paracetamol tablets. One patient in non-diabetes group developed arthritis in both knee joints following ZA injection. None of our patients developed osteonecrosis of jaw or symptomatic hypocalcemia, or atrial fibrillation.
Discussion
Eighty patients with PMO, 40 each in diabetes and non-diabetes groups were included in this prospective cohort study and given a single IV dose of 4 mg ZA. The duration of the study was 12 months, and the baseline BMD was similar in both groups. In our study, although there was an improvement in LS-BMD from the baseline in diabetes group, it was lower compared to non-diabetes patients. The mean increase in LS-BMD was 3.6% in diabetes group as compared to 6.2% in non-diabetes group at the end of 12-month period (p = 0.01). However, there was no difference in change in TBS between the two groups.
The higher bone turnover at baseline in non-diabetes group might have led to a better increase in LS BMD in our study. A similar result was found in a study involving 35 subjects with PMO in each group (diabetes & non-diabetes) receiving alendronate therapy over five years by Yilmaz et al. [18]. After one year of treatment, there were no significant differences between the T scores of LS and FN BMD of both groups. But LS and FN T scores became significantly lower in diabetes subjects compared to non-diabetes group after the end of 5th year. The diabetes subjects also had lower BTMs at baseline, similar to our findings. A retrospective case-control study involving 26 patients each in diabetes and non-diabetes group, noted a mean percent increase of 5.5% in diabetes subjects and 4.8% in non-diabetes patients in the LS-BMD (p = 0.85) [19]. But a decrease in the BMD at TH (−5.6% vs. +1.4%, p = 0.096), FN (−8.1% vs. +1.1%, p = 0.015), and FA (−3.6% vs. 12.7%, p = 0.013) was observed in diabetes patients compared to a non-diabetes group over five years of alendronate therapy.
The studies by Black et al., Keegan et al., Chesnut et al., McClung et al., and Kim et al. showed similar changes in BMD between diabetes and non-diabetes groups following BP therapy [14,15,16,17, 21]. In the post hoc analysis of the HORIZON PFT trial, LS BMD improved by 7.6% in diabetes group (n = 502) and 5.8% in non-diabetes (n = 7234) subjects over 24 months following yearly IV ZA therapy (p = 0.42) [21]. Similarly, there was no difference in the change in BMD at TH (4.4 % vs. 4.7%, p = 0.57) and FN (3.6% vs. 3.9%, p = 0.66) between two groups. A post hoc analysis of risedronate use in diabetes (n = 515) and non-diabetes patients (n = 8816) showed an increase in LS BMD over 24 months from baseline in both groups without any difference between them (4.3% vs. 3.9%, p = 0.82) [17]. The change in LS BMD was similar (6.6% in diabetes vs. 7.5% in the non-diabetes group, p = 0.4) following three years of alendronate therapy in the Fracture Intervention Trial (FIT) [14]. However, the increment in LS BMD was 3.71% in diabetes and 3.41% in non-diabetes subjects following one year of ibandronate therapy without any difference between them in a study by Kim et al. [16]. The comparable change in BMD in both groups can be explained by the similar plasma BTM levels found at the baseline in both of these studies [14, 16].
The effect of BPs on changes in BTMs in patients with PMO with and without T2DM was evaluated in a few studies [14,15,16,17, 20, 21]. There was no difference in reduction of both β-CTX (52.7% vs. 68.9%, p = 0.09) and P1NP (53% vs. 57%, p = 0.58) over 12 months after ZA administration between diabetes and non-diabetes patients in HORIZON PFT trial [20, 21]. Similar results were found in different studies on other BPs like alendronate, risedronate, and ibandronate [14,15,16,17, 21]. The range of percentage reductions in both β-CTX (40.1% to 54.1% vs. 48.1% to 59.6%) and PINP (29.6% to 52.3% vs. 33.2% to 54.9%) were not different between diabetes and non-diabetes groups during the study period (6 months to 3 years) in different trials [14, 16, 17, 21].
The increase in LS BMD was lesser in diabetes group compared to non-diabetes group in our study. The higher baseline BTM levels are associated with better response in BMD increment and fracture prevention following treatment with osteoporosis medications like BP [30, 31]. So, BMD increment following anti-resorptive therapy will be decreased in low bone turnover state like diabetes. Trabecular bone is the more metabolically active compartment of the bone, and cortical bone undergoes slower remodeling than trabecular bone. The spine is rich in trabecular bone compared to other areas like the hip [32]. So, the difference between BMD increment in diabetes and non-diabetes groups at LS will be more prominent following treatment with an antiresorptive drug like ZA. This may be the reason why there was a significant difference in only LS BMD response to ZA between diabetes and non-diabetes subjects in our study. Therefore, an anabolic agent like intermittent recombinant human PTH therapy (1–34) can be considered a better treatment option for PMO patients with T2DM. During teriparatide treatment, increases in both LS and TH BMD and fracture prevention did not differ between diabetes and non-diabetes groups in a study by Schwartz et al. [33]. However, the increase in FN BMD was greater in T2DM patients than in patients without diabetes (0.34 vs. 0.004 g/cm2, respectively; p = 0.014). Similarly, the reduction in clinical fracture rate was greater for diabetes subjects compared to non-diabetes group (77% vs.48%, p = 0.046) in an analysis of the data from 4 real-world observational studies on the effectiveness of teriparatide [34].
In our study, 75% of patients experienced adverse effects in the form of APR. Pyrexia was seen in 25%, whereas flu-like illness was seen in 30% of the patients. APRs occurred within three days of drug administration and pyrexia was more common in the non-diabetes group. The prevalence of AE varies from 42.4% to 87% in different studies [35,36,37,38]. APR in the HORIZON-PFT trial was also less common in diabetes subjects (odds ratio-0.73; 95% CI, 0.58 to 0.92) [35]. This can be explained by the lesser immune response found in diabetes subjects [39].
This is the first prospective study to compare the effect of IV ZA on change in BMD in PMO women with and without diabetes. Additionally, OGTT was done to rule out diabetes in our study. However, it also has a few limitations. First, the short duration of follow-up (e.g., one year) is not enough to comment on the long-term trend of changes in BMD and the fracture preventive potential of ZA. Second, the sample size was not calculated as this was a pilot study. Third, the study was done exclusively in Asian Indians and may not apply to other ethnic groups.
Conclusion
The gain in the LS-BMD was significantly lower in diabetes group compared to non-diabetes group at 12 months following a single IV infusion of 4 mg ZA. The explanation for this could be low bone turnover in diabetes subjects at baseline. These findings need confirmation in further large multicentric clinical trials.
References
O. Johnell, J.A. Kanis, An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 17(12), 1726–1733 (2006). https://doi.org/10.1007/s00198-006-0172-4
A.P. Hills, R. Arena, K. Khunti, C.S. Yajnik, R. Jayawardena, C.J. Henry, S.J. Street, M.J. Soares, A. Misra, Epidemiology and determinants of type 2 diabetes in south Asia. Lancet Diabetes Endocrinol. 6, 966–978 (2018). https://doi.org/10.1016/S2213-8587(18)30204-3
R. Eastell, C.J. Rosen, D.M. Black, A.M. Cheung, M.H. Murad, D. Shoback, Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 104(5), 1595–1622 (2019). https://doi.org/10.1210/jc.2019-00221
P. Barrionuevo, E. Kapoor, N. Asi, F. Alahdab, K. Mohammed, K. Benkhadra, J. Almasri, W. Farah, M. Sarigianni, K. Muthusamy, A. Al Nofal, Q. Haydour, Z. Wang, M.H. Murad, Efficacy of pharmacological therapies for the prevention of fractures in postmenopausal women: A network meta-analysis. J. Clin. Endocrinol. Metab. 104(5), 1623–1630 (2019). https://doi.org/10.1210/jc.2019-00192
P. Vestergaard, Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes–a meta-analysis. Osteoporos Int. 18(4), 427–444 (2007). https://doi.org/10.1007/s00198-006-0253-4
S. Kamalanathan, V. Nambiar, V. Shivane, T. Bandgar, P. Menon, N. Shah, Bone mineral density and factors influencing it in Asian Indian population with type 2 diabetes mellitus. Indian J. Endocrinol. Metab. 18(6), 831–837 (2014). https://doi.org/10.4103/2230-8210.140268
M. Saito, K. Marumo, Bone quality in diabetes. Front. Endocrinol. (Lausanne) 4, 72 (2013). https://doi.org/10.3389/fendo.2013.00072
S. Khosla, P. Samakkarnthai, D.G. Monroe, J.N. Farr, Update on the pathogenesis and treatment of skeletal fragility in type 2 diabetes mellitus. Nat. Rev. Endocrinol. 17(11), 685–697 (2021). https://doi.org/10.1038/s41574-021-00555-5
L.T. Ho-Pham, T.V. Nguyen, Association between trabecular bone score and type 2 diabetes: a quantitative update of the evidence. Osteoporos Int. 30(10), 2079–2085 (2019). https://doi.org/10.1007/s00198-019-05053-z
A.W. Popp, S. Guler, O. Lamy, C. Senn, H. Buffat, R. Perrelet, D. Hans, K. Lippuner, Effects of zoledronate versus placebo on spine bone mineral density and microarchitecture assessed by the trabecular bone score in postmenopausal women with osteoporosis: a three-year study. J. Bone Miner. Res. 28(3), 449–454 (2013). https://doi.org/10.1002/jbmr.1775
K. Hygum, J. Starup-Linde, T. Harsløf, P. Vestergaard, B.L. Langdahl, MECHANISMS IN ENDOCRINOLOGY: Diabetes mellitus, a state of low bone turnover - a systematic review and meta-analysis. Eur. J. Endocrinol. 176(3), R137–R157 (2017). https://doi.org/10.1530/EJE-16-0652
W. Dong, M. Qi, Y. Wang, X. Feng, H. Liu, Zoledronate and high glucose levels influence osteoclast differentiation and bone absorption via the AMPK pathway. Biochem. Biophys. Res. Commun. 505(4), 1195–1202 (2018). https://doi.org/10.1016/j.bbrc.2018.10.059
P. Anagnostis, S.A. Paschou, N.N. Gkekas, A.-M. Artzouchaltzi, K. Christou, D. Stogiannou, A. Vryonidou, M. Potoupnis, D.G. Goulis, Efficacy of anti-osteoporotic medications in patients with type 1 and 2 diabetes mellitus: a systematic review. Endocrine. 60, 373–383 (2018). https://doi.org/10.1007/s12020-018-1548-x
T.H.M. Keegan, A.V. Schwartz, D.C. Bauer, D.E. Sellmeyer, J.L. Kelsey; fracture intervention trial, Effect of alendronate on bone mineral density and biochemical markers of bone turnover in type 2 diabetic women: The fracture intervention trial. Diabetes Care 27, 1547–1553 (2004). https://doi.org/10.2337/diacare.27.7.1547
C.H. Chesnut 3rd, A. Skag, C. Christiansen, R. Recker, J.A. Stakkestad, A. Hoiseth, D. Felsenberg, H. Huss, J. Gilbride, R.C. Schimmer, P.D. Delmas; Oral Ibandronate Osteoporosis Vertebral Fracture Trial in North America and Europe (BONE), Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J. Bone Miner. Res. 19(8), 1241–1249 (2004). https://doi.org/10.1359/JBMR.040325
J. Kim, K.M. Kim, S. Lim, M.I. Kang, K.H. Baek, Y.K. Min, Efficacy of bisphosphonate therapy on postmenopausal osteoporotic women with and without diabetes: a prospective trial. BMC Endocr. Disord. 22(1), 99 (2022). https://doi.org/10.1186/s12902-022-01010-w
M.R. McClung, P. Geusens, P.D. Miller, H. Zippel, W.G. Bensen, C. Roux, S. Adami, I. Fogelman, T. Diamond, R. Eastell, P.J. Meunier, J.Y. Reginster; Hip Intervention Program Study Group, Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N. Engl. J. Med. 344(5), 333–340 (2001). https://doi.org/10.1056/NEJM200102013440503
V. Yilmaz, E. Umay, I. Gundogdu, N. Tezel, Effect of type 2 diabetes mellitus on treatment outcomes of patients with postmenopausal osteoporosis: a retrospective study. J Diabetes Metab. Disord. 17(2), 181–187 (2018). https://doi.org/10.1007/s40200-018-0359-1
S. Dagdelen, D. Sener, M. Bayraktar, Influence of type 2 diabetes mellitus on bone mineral density response to bisphosphonates in late postmenopausal osteoporosis. Adv. Ther. 24, 1314–1320 (2007). https://doi.org/10.1007/BF02877778
D.M. Black, P.D. Delmas, R. Eastell, I.R. Reid, S. Boonen, J.A. Cauley, F. Cosman, P. Lakatos, P.C. Leung, Z. Man, C. Mautalen, P. Mesenbrink, H. Hu, J. Caminis, K. Tong, T. Rosario-Jansen, J. Krasnow, T.F. Hue, D. Sellmeyer, E.F. Eriksen, S.R. Cummings; HORIZON Pivotal Fracture Trial, Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N. Engl. J. Med. 356(18), 1809–1822 (2007). https://doi.org/10.1056/NEJMoa067312
R. Eastell, E. Vittinghoff, L.Y. Lui, S.K. Ewing, A.V. Schwartz, D.C. Bauer, D.M. Black, M.L. Bouxsein, Diabetes Mellitus and the Benefit of Antiresorptive Therapy on Fracture Risk. J. Bone Miner. Res. 37(11), 2121–2131 (2022). https://doi.org/10.1002/jbmr.4697
S. Shetty, N. Kapoor, D. Naik, H.S. Asha, N. Thomas, T.V. Paul, The impact of the Hologic vs the ICMR database in diagnosis of osteoporosis among South Indian subjects. Clin. Endocrinol. (Oxf) 81, 519–522 (2014). https://doi.org/10.1111/cen.12495
J.E. Manson, P.M. Brannon, C.J. Rosen, C.L. Taylor, Vitamin D Deficiency - Is There Really a Pandemic? N. Engl. J. Med. 375(19), 1817–1820 (2016). https://doi.org/10.1056/NEJMp1608005
American Diabetes Association, 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care 44, S15–S33 (2021). https://doi.org/10.2337/dc21-S002
P. Szulc, K. Naylor, N.R. Hoyle, R. Eastell, E.T. Leary; National Bone Health Alliance Bone Turnover Marker Project, Use of CTX-I and PINP as bone turnover markers: National Bone Health Alliance recommendations to standardize sample handling and patient preparation to reduce pre-analytical variability. Osteoporos. Int. 28(9), 2541–2556 (2017). https://doi.org/10.1007/s00198-017-4082-4
H.K. Genant, C.Y. Wu, C. van Kuijk, M.C. Nevitt, Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 8, 1137–1148 (1993). https://doi.org/10.1002/jbmr.5650080915
J.A. Shepherd, J.T. Schousboe, S.B. Broy, K. Engelke, W.D. Leslie, Executive Summary of the 2015 ISCD Position Development Conference on Advanced Measures from DXA and QCT: Fracture Prediction Beyond BMD. J. Clin. Densitometry 18, 274–286 (2015). https://doi.org/10.1016/j.jocd.2015.06.013
www.iscd.org / resources / calculators / precision-calculator Accessed 26 Feb 2023
Medimaps. T.B.S. iNsight to boost your DXA The bone quality assessment. 1–12. Available from: https://www.medimapsgroup.com/doc/white-paper/ Accessed 26 Feb 2023
D.C. Bauer, P. Garnero, M.C. Hochberg, A. Santora, P. Delmas, S.K. Ewing, D.M. Black; Fracture Intervention Research Group, Pretreatment levels of bone turnover and the antifracture efficacy of alendronate: the fracture intervention trial. J. Bone Miner. Res. 21(2), 292–299 (2006). https://doi.org/10.1359/JBMR.051018
R. Eastell, S. Boonen, F. Cosman, I.R. Reid, L. Palermo, S.R. Cummings, D.M. Black, Relationship between pretreatment rate of bone loss and bone density response to once-yearly ZOL: HORIZON-PFT extension study. J. Bone Miner. Res. 30(3), 570–574 (2015). https://doi.org/10.1002/jbmr.2361
M. Pazianas, S. van der Geest, P. Miller, Bisphosphonates and bone quality. Bonekey Rep. 3, 529 (2014). https://doi.org/10.1038/bonekey.2014.24
A.V. Schwartz, I. Pavo, J. Alam, D.P. Disch, D. Schuster, J.M. Harris, J.H. Krege, Teriparatide in patients with osteoporosis and type 2 diabetes. Bone. 91, 152–158 (2016). https://doi.org/10.1016/j.bone.2016.06.017
B.L. Langdahl, S. Silverman, S. Fujiwara, K. Saag, N. Napoli, S. Soen, H. Enomoto, T.E. Melby, D.P. Disch, F. Marin, J.H. Krege, Real-world effectiveness of teriparatide on fracture reduction in patients with osteoporosis and comorbidities or risk factors for fractures: Integrated analysis of 4 prospective observational studies. Bone. 116, 58–66 (2018). https://doi.org/10.1016/j.bone.2018.07.013
I.R. Reid, G.D. Gamble, P. Mesenbrink, P. Lakatos, D.M. Black, Characterization of and risk factors for the acute-phase response after zoledronic acid. J. Clin. Endocrinol. Metab. 95, 4380–4387 (2010). https://doi.org/10.1210/jc.2010-0597
A.D. Anastasilakis, S.A. Polyzos, P. Makras, G.T. Sakellariou, I. Bisbinas, A. Gkiomisi, S. Delaroudis, S. Gerou, I. Ballaouri, D. Oikonomou, S.E. Papapoulos, Acute phase response following intravenous zoledronate in postmenopausal women with low bone mass. Bone. 50(5), 1130–1134 (2012)
H. Karga, I. Giagourta, G. Papaioannou, P. Katsichti, A. Pardalakis, G. Kassi, A. Zagoreou, M. Triantaphyllopoulou, C. Zerva, Transient changes in thyroid functions tests after zoledronic acid infusion. Endocr J 58(11), 969–977 (2011)
P. Kotian, A. Boloor, S. Sreenivasan, Study of adverse effect profile of parenteral Zoledronic acid in female patients with osteoporosis. J. Clin. Diagn. Res. 10(1), OC04-6 (2016). https://doi.org/10.7860/JCDR/2016/17061
A. Berbudi, N. Rahmadika, A.I. Tjahjadi, R. Ruslami, Type 2 Diabetes and its Impact on the Immune System. Curr. Diabetes Rev. 16(5), 442–449 (2020). https://doi.org/10.2174/1573399815666191024085838
Acknowledgements
The manuscript was presented as an e-poster both at the Indian Society for Bone and Mineral Research (ISBMR) Annual Meeting, October 30–31, 2021, at Hyderabad, India, and at the American Society for Bone and Mineral Research (ASBMR) Annual Meeting, October 1–4, 2021 at the San Diego Convention Center in California, USA.
Author contributions
All authors contributed to the study’s conception and design. The data collection, analysis, and interpretation were performed by C.M., G.R., J.S., and S.S.K. All authors revised it critically for important intellectual content and approved the final manuscript.
Funding
This study was funded by both an extramural grant from the endocrine society of India (TG2019015/18-10-2019) and an intramural grant from Jawaharlal Institute of Postgraduate Medical Education and Research (JIP/Res/Intramural/Phs 2 /2018–2019).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki after obtaining the Institute Ethics Committee’s approval (JIP/IEC/2018/379 date-28.12.2018).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merugu, C., Sahoo, J., Kamalanathan, S. et al. Effect of a single dose of zoledronic acid on bone mineral density and trabecular bone score in Indian postmenopausal osteoporotic women with and without type 2 diabetes mellitus – A prospective cohort pilot study. Endocrine 82, 171–180 (2023). https://doi.org/10.1007/s12020-023-03432-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03432-5