Abstract
Purpose
To evaluate the safety and effectiveness of microwave ablation (MWA) versus lobectomy for the treatment of benign thyroid nodules > 4 cm.
Methods
We retrospectively analyzed the data of 48 patients who underwent MWA and 53 patients who underwent lobectomy to treat benign thyroid nodules > 4 cm. The patients were followed up for 12 months. The volume reduction ratio (VRR) was calculated. The operation time, incision length, hospitalization time, complications, thyroid function, symptoms, and cosmetic improvement were analyzed and compared between the two groups.
Results
During the 12-month follow-up, the mean nodule volume in the MWA group was reduced from 36.1 ± 23.1 to 4.0 ± 4.1 ml, and the mean VRR of the nodules was 90 ± 5% in the MWA group, which was comparable with that in the surgery group. No significant postoperative change in thyroid function was observed in the MWA group. Compared with the surgery group, the incidence of complications and postoperative pain in the MWA group were lower, the operation time, incision length, and hospitalization time in the MWA group were shorter, and satisfaction with the esthetic results in the MWA group was greater.
Conclusion
MWA is safe and effective for the treatment of benign thyroid nodules > 4 cm. Moreover, MWA is associated with a faster recovery, fewer complications, better protection of thyroid function, and superior esthetic results relative to thyroid lobectomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, the prevalence of thyroid nodules has increased annually. The detection rate of thyroid nodules has increased to 65% in the general population, and 90–95% of the nodules are benign [1]. In most cases, benign thyroid nodules are simply followed up and monitored [2]. However, according to the 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer, surgery may be considered for growing nodules that are benign if they are large (>4 cm), causing compressive or structural symptoms, or based on clinical concern [3]. Although surgery is widely used and effective, it may be associated with significant incidence of postoperative complications and unsatisfactory esthetic effects. Some patients must take medications for life after surgery, which affects their mental health and quality of life [4, 5]. Therefore, increasing numbers of patients are seeking a minimally invasive treatment alternative to surgery.
Thermal ablation methods, such as laser, radiofrequency, and microwave ablation (MWA), are being used more extensively in clinical practice due to their advantages, such as reduced trauma and no scarring [6]. MWA is characterized by rapid heating, good coagulation, a large ablation area, and relative ease of use and is currently used to treat liver, kidney, lung, and breast lesions [7,8,9,10]. In recent years, researchers have gradually adopted the use of MWA to treat thyroid nodules [11]. Studies have shown that ultrasound-guided MWA is safe and effective for the treatment of benign thyroid nodules [5]. Moreover, researchers have investigated MWA versus surgery for the treatment of benign thyroid nodules with maximum diameters > 2 cm. Their studies have suggested that MWA can significantly reduce nodule volume and nodule-related symptoms and provide a faster recovery and more satisfactory esthetic outcomes with less physiologic disruption and a lower cost compared with surgery [12]. However, no studies have been conducted in China or elsewhere to investigate the efficacy of MWA versus thyroid lobectomy for the treatment of benign thyroid nodules > 4 cm. In this study, we retrospectively analyzed the data of 48 patients who underwent ultrasound-guided MWA and 53 patients who underwent lobectomy to treat benign thyroid nodules > 4 cm. The patients were followed up for 12 months to evaluate the safety and effectiveness of MWA and to compare the treatment outcomes of the two methods.
Materials and methods
This study was approved by the Ethics Committee of the China-Japan Union Hospital of Jilin University and was registered in the Chinese Clinical Trial Registry (registration number: ChiCTR1900025643). All patients signed an informed consent form before treatment.
Patients
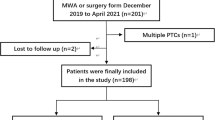
The data of 101 patients with benign thyroid nodules > 4 cm who underwent either MWA (n = 48) or unilateral lobectomy (n = 53) at our hospital between December 2017 and August 2018 were collected. The inclusion criteria were nodules > 4 cm that were unilateral or fused to one side and a sonograph pattern consistent with low or very low suspicion of malignancy. For all patients in the MWA group, benign nodules were diagnosed based on pathologic findings by core needle biopsy (CNB) rather than fine needle aspiration (FNA). Studies have shown that for nodules with a diameter ≥4 cm, FNA has a higher probability of producing a false-negative result [13]. The histologic information obtained by analysis of CNB specimens may enable a more confident diagnosis of benign nodules and reduce the need for repeat FNA [14]. For the patients in the lobectomy group, benign nodules were diagnosed by surgical pathology. One or more of the following inclusion criteria needed to be satisfied: (1) the nodules were associated with pressure symptoms or clinical concern; (2) treatment was sought because the nodules affected the patients’ appearance; (3) clinical observation as a treatment approach was rejected due to the patients’ concerns about the effect of the nodules on normal daily activities; and (4) the nodule volume increased rapidly (more than double in 6 months) [12]. The exclusion criteria (any) were (1) equivocal pathological results or malignant nodules; (2) a history of head or neck irradiation; (3) other endocrine disease; (4) previous contralateral lobectomy; (5) head or neck surgery; (6) a history of severe bleeding and coagulopathy; (7) a history of important organ damage; (8) pregnancy or nursing; and (9) incomplete clinical data.
Preoperative evaluation
All patients underwent routine ultrasonography before treatment to evaluate nodule size, location, composition, and vascularity. The nodule volume (V) was calculated according to the following formula: V = π abc/6 (a: the maximum diameter of the nodule; b and c: two diameters perpendicular to a). Vascularity was evaluated according to a 4-point scale (0: no visible flow, 1: only peripheral flow, 2: peripheral flow with a small amount of central flow, 3: peripheral flow plus extensive intranodular flow, and 4: only central flow) [15]. Ultrasonography and guidance were performed with a Mindray Resona 7 (Mindray, Shenzhen, China) color Doppler ultrasound diagnostic device equipped with a line array probe (L14–5WU).
All patients underwent laboratory tests before treatment, including thyroid function (triiodothyronine (T3), thyroxine (T4), free triiodothyronine (FT3), free thyroxine (FT4), thyroid-stimulating hormone (TSH), thyroglobulin II (Tg II), and thyroglobulin antibody (TgAb)) and coagulation. Patients taking anticoagulants were required to discontinue these medications 1 week before treatment.
To quantify the improvement of nodule-related symptoms, we used a visual analog scale (VAS; 0–10) to evaluate neck compression-related symptoms and difficulty swallowing. Moreover, the physician recorded a cosmetic score (1: no palpable mass; 2: invisible but palpable mass; 3: visible mass when swallowing; and 4: obvious mass) to evaluate cosmetic conditions [16, 17].
Patients in the MWA group underwent contrast-enhanced ultrasonography (CEUS) before MWA to determine the location of nodule-feeding arteries and develop an optimal ablation path. SonoVue (Bracco) was used as the ultrasound contrast agent, which was diluted in 5 ml of 0.9% physiological saline (Jilin Cornell Pharmaceutical Co., Ltd.) and mixed well by shaking before use. A 4.0-ml bolus was injected into the median cubital vein.
Methods
MWA
All MWA procedures were performed by a physician with more than 5 years of ultrasound-guided ablation experience. The patient was maintained in the supine position with the shoulders slightly elevated to place the neck in hyperextension. The patient was instructed not to cough or swallow during the procedure. An Ego ECO-100A1 machine (YIGAO Microwave System Engineering Co., Ltd., Nanjing, Jiangsu Province, China) and ECO-100AI3 superficial organ ablation needle (16G, total length: 10 cm, microwave transmitter length: 3 mm) were used. After routine disinfection and draping, 1% lidocaine was used for local anesthesia, and an appropriate amount was injected around the capsule of the thyroid. The entire process was dynamically monitored with ultrasound. Before MWA, we developed the treatment protocol according to the volume of nodules and predicted the required number of ablation layers and needle insertions. The following standard was used: if the ablation power is set to 30 W, 1 min of ablation can form a 5-mm × 5-mm × 7-mm ablation area. According to the estimated results, the multiple overlapping shot technique (MOST) was used to perform ablation layer by layer [18]. For each lesion layer, ablation was performed from deep to shallow surfaces and in a distal to proximal direction. When the ablation position was confirmed, MWA was started after the whole active tip was placed within the nodule, and the initial power was set to 25 W. If a hyperecho did not appear in the ablating area after 10–20 s of ablation with this power, we increased the power gradually (to a maximum of 35 W). The electrode was not moved at the beginning of MWA until the nodule showed an obvious hyperechogenic vaporization area. Once a part of the nodule had been treated, the antenna was repositioned next to the previous ablation area, and ablation was started again to create overlapping ablation zones. This process was repeated until the hyperechoic zone of vaporization covered the whole thyroid nodule completely. The ablation times were different for different parts of the nodules. For areas with nodule-feeding arteries, after formation of the hyperechoic vaporization area, we continued with MWA for 3–5 s to ensure complete inactivation of the tissues in this area. During the procedure, the physician communicated with the patient regularly to monitor any intraoperative complications, such as hoarseness and pain, to prevent damage to the recurrent laryngeal nerve. If the nodule was next to the ipsilateral recurrent laryngeal nerve or large vessels in the neck, we used the hydrodissection technique (0.9% physiological saline) under ultrasound guidance to separate the nodule from the trachea, esophagus, common carotid artery, internal jugular vein, and recurrent laryngeal nerve before ablation [19]. If the ablation time was too long, supplemental hydrodissection was provided in a timely manner during MWA. In addition, for nodules that were difficult to separate by hydrodissection and were close to critical sites, a safety margin of 2–3 mm was preserved. CEUS was performed immediately after ablation to evaluate the ablation area. Ablation was completed once the lesions had been completely inactivated and no residual lesions were observed; otherwise, ablation was repeated.
Surgery
All patients included in the surgery group underwent unilateral lobectomy performed by the same thyroid surgical team. The patient was placed in the supine position and received general anesthesia, and the shoulder was elevated to straighten the neck. After routine disinfection, a low arc incision was made; the skin, subcutaneous tissue, and platysma were cut open, and a flap was separated up to the level of the laryngeal protuberance. The white line was longitudinally cut to the level of the thyroid. The isthmus was cut, separated, and clamped, the vessels were double ligated, the recurrent laryngeal nerve and parathyroid glands were protected, nerve signals were monitored, and the nodules and thyroid lobe tissue were removed and sent for frozen sectioning. Vital signs were monitored throughout the procedure. After surgery, nerve function and bleeding were assessed. After hemostasis, a drainage tube was placed, and the incision was sutured.
Postoperative evaluation
To compare the effects of the two treatments, postoperative complications, operation time, hospitalization time, and incision length were recorded. The serum calcium levels of the two groups were measured 24 h after the operation, and thyroid function was evaluated 1 month after treatment. We considered the presence of early hypocalcemia when serum calcium levels lower than 8.0 mg/dl were measured 24 h after surgery [20]. Subclinical hypothyroidism was defined as elevated serum TSH and normal FT4, and hypothyroidism was defined as elevated serum TSH and decreased FT4 [21]. In addition, we required patients to undergo an ultrasound examination on the second day after treatment. If an area of bleeding was still visible on the ultrasound image, we defined it as a hematoma. At 12 months after treatment, both groups were reevaluated for symptom and cosmetic scores, and the patients evaluated the esthetic results (poor, acceptable, good, and excellent). Clinical data were retrospectively analyzed.
To evaluate the safety and effectiveness of MWA, the following information was collected from the MWA group: (1) the three diameters (a, b, and c; a: the maximum diameter of the nodule; b and c: two diameters perpendicular to a) of the nodules were measured before MWA and at 1, 3, 6, and 12 months after ablation to calculate the volume of ablation and the volume reduction ratio (VRR). Effective treatment was defined as a VRR > 50% [22]; VRR = [(preoperative volume − volume at the follow-up point)/preoperative volume] × 100%. (2) Thyroid function was also assessed 12 months after MWA. In addition, we evaluated regrowth during the 12-month follow-up period. Regrowth was defined by new blood flow in the nodules in the total ablation area or/and an increase in nodule volume compared with the previous ultrasound examination result [23].
Statistical analysis
SPSS 22.0 was used for statistical analysis. Measurement data, such as the size and vascularity of the nodules, patient age, thyroid function, operation time, hospitalization time, incision length, and symptom and cosmetic scores, are described as the mean ± standard deviation. Intergroup comparisons of measurement data were performed using the independent-sample t-test. Enumeration data, such as the location and composition of the nodules, patient sex, and postoperative complications, were analyzed with the chi-square test. Changes in the maximum diameter and volume of the thyroid nodules before and after ablation were analyzed with the paired t-test. Esthetic results were analyzed with the Wilcoxon rank sum test. P < 0.05 was considered statistically significant.
Results
Clinical characteristics
A total of 101 patients (nodules) underwent MWA (n = 48) or surgery (n = 53). The baseline data are provided in Table 1. The MWA group included 15 (31.3%) males and 33 (68.7%) females aged 18–66 years (mean: 45.2 ± 12.2 years). The surgery group included 14 (26.4%) males and 39 (73.6%) females aged 17–81 years (mean: 48.9 ± 12.5 years). No significant intergroup differences were observed in age, sex, thyroid function, or the maximum diameter, volume, location, composition, or vascularity of the nodules (P > 0.05).
MWA
Procedure
All 48 patients tolerated ablation well. Strong echo images of the ablation needle were detected during the entire procedure. Color Doppler flow imaging showed color blood flow signals inside and around the nodules before ablation and the absence of blood flow signals in all nodules after ablation. CEUS showed no contrast filling and a “black hole” sign. After ablation, ultrasound showed a heterogeneous ablation zone. Based on the initial volume, the mean transmitted energy per ml was 0.9 ± 0.7 KJ/ml. For 24 nodules at critical sites, we used the hydrodissection technique during ablation.
Follow-up
After MWA, the patients were followed up for 12 months. The maximum diameters of the nodules, nodule volumes, and the VRR at each follow-up point are provided in Table 2. The mean maximum diameter was reduced from 5.2 ± 1.1 cm (4.0–8.4 cm) before ablation to 2.5 ± 0.7 cm (1.0–4.3 cm) at 12 months after ablation, and the mean nodule volume was reduced from 36.1 ± 23.1 ml (9.6–128.6 ml) to 4.0 ± 4.1 ml (0.3–19.9 ml), indicating significant reductions in nodule diameter and volume (P < 0.001, Fig. 1). The mean VRR was 51 ± 14% at 1 month, 71 ± 11% at 3 months, 82 ± 9% at 6 months, and 90 ± 5% at 12 months after MWA. No nodules regrew during our 12-month follow-up. The mean nodule volume and VRR at each follow-up point after MWA are shown in Fig. 2.
A 53-year-old woman had a nodule diagnosed as a benign thyroid nodule in the left thyroid lobe. The images of the nodule in preoperative, intraoperative, and postoperative follow-up are given; a Before MWA, a nodule with 3.7 cm × 2.6 cm × 4.0 cm in size and 20.0 ml in volume; b the nodule was rich in blood flow signals before MWA; c CEUS showed that the nodule was highly enhanced before MWA; d the ablation electrode was implanted into the nodule, and the ablation mode was started at a output power of 25 W; e CEUS showed that there was no contrast agent filling in nodule after MWA, indicating that the blood perfusion in nodule disappeared and ablation was completed; f 1 month after MWA, the ablation area was 2.6 cm × 2.1 cm × 2.9 cm in size and 8.7 ml in volume; g 3 month after MWA, the ablation area was 1.9 cm × 1.8 cm × 2.6 cm and 4.8 ml in volume; h 6 months after MWA, the ablation area was 1.5 cm × 1.4 cm × 2.1 cm and 2.3 ml in volume; i 12 months after MWA, the ablation area was 1.2 cm × 1.2 cm × 1.9 cm and 1.4 ml in volume, the VRR after 1 year was 93%
Thyroid function at 1 and 12 months after MWA is shown in Fig. 3. TSH, FT3, FT4, T3, T4, and TgAb showed no significant changes at 1 and 12 months after MWA relative to the values before MWA (P > 0.05). Tg II levels at 1 and 12 months after MWA were significantly reduced compared with those before MWA (P < 0.001).
Surgery
All patients successfully underwent unilateral lobectomy under general anesthesia and were confirmed to have benign nodules via intraoperative frozen sections.
Complications, operation time, incision length, and hospitalization time in the two groups
Postoperative complications, operation time, incision length, and hospitalization time are provided in Table 3. All 48 patients in the MWA group tolerated local anesthesia during the procedure. One patient had hoarseness after MWA, which resolved spontaneously in 2 months. One patient had a hematoma after MWA, which underwent spontaneous reabsorption within 2 months. Four patients experienced slight pain during the MWA procedure that disappeared shortly after the electrode was turned off. None of the patients required pain medications after MWA. No infection occurred after MWA.
Of the 53 patients in the surgery group, two patients had hoarseness after surgery, which resolved spontaneously in 2 months, with no significant difference compared with the MWA group (P = 0.617). Three patients had a hematoma after the operation, which was reabsorbed spontaneously in 2 months, with no significant difference compared with the MWA group (P = 0.357). A total of 45 patients had varying degrees of incision pain after surgery, which was alleviated in 27 patients after receiving pain medications; these results differed significantly from the results for the MWA group (P < 0.001). Two patients had incision infections after the operation, which resolved after symptomatic treatment, with no significant difference compared with the MWA group (P = 0.174).
Thyroid function was assessed 1 month after treatment. No hypothyroidism was observed in the MWA group, whereas 10 patients among the 53 patients in the surgery group had subclinical hypothyroidism, and 6 were diagnosed with hypothyroidism and received prescriptions for levothyroxine sodium. The TSH results differed significantly between the two groups (P < 0.001). Moreover, seven patients in the surgery group had transient hypocalcemia, including one patient with mild facial paresthesia; the other six patients were asymptomatic. After calcium supplement treatment, the serum calcium level was restored within 2 months, whereas none of the patients in the MWA group had obvious changes in serum calcium levels. Therefore, a significant intergroup difference was noted (P = 0.009).
Significant intergroup differences were also observed in hospitalization time, incision length, and operation time (P < 0.001).
Symptom and cosmetic scores and esthetic results in the two groups
The symptom scores, cosmetic scores, and esthetic results before and after treatment for the two groups are provided in Table 4. The symptom scores were significantly different at 12 months after treatment compared with those before the operation in both groups (both P < 0.001), with no significant intergroup differences (P > 0.05).
The cosmetic scores were significantly different at 12 months after treatment compared with those before the intervention in both groups (both P < 0.001), with no significant intergroup differences (P > 0.05). Regarding the esthetic results, 32 patients in the MWA group rated the results as “excellent,” 13 rated the results as “good,” and only three patients rated the results as “acceptable”; 6 of the 53 patients in the surgery group rated the results as “excellent,” 25 rated the results as “good,” 20 rated the results “acceptable,” and 2 patients rated the results as “poor.” The results were significantly different between the two groups (P < 0.001).
Discussion
In this study, we retrospectively analyzed the data of 48 patients who underwent MWA and 53 patients who underwent lobectomy to treat benign thyroid nodules > 4 cm. The patients were followed up for 12 months; our research showed comparable efficacy between MWA and lobectomy, and MWA is safer than lobectomy.
As for efficacy, MWA was comparable with that in the lobectomy group. First, in the MWA group, the VRR was 90 ± 5% at 12 months, which is consistent with the findings of Liu et al. [24]. Some studies have reported slightly smaller VRRs than ours [11, 16]. The reasons may be as follows: our study included mainly solid nodules and mainly cystic nodules; we used an ablation power of 25–35 W during MWA to avoid over-ablating the nodules, resulting in relatively faster absorption. Second, all nodules were successfully removed, and no nodules regrew during our 12-month follow-up in both groups. Treating nodule-feeding arteries before treating the nodules and the use of CEUS before and after MWA can improve ablation efficiency and reduce relapse.
In terms of safety, our research shows that MWA was better than lobectomy. First, MWA was better tolerated than lobectomy. Second, MWA offers better protection of thyroid function because MWA accurately ablates the tumor itself, whereas lobectomy involves removing part of the thyroid gland in addition to removing lesions, thus causing hypothyroidism in some patients who then require replacement therapy, which in the long term may place postmenopausal women at increased risk of osteoporosis and cardiovascular disease and can have a psychological impact [25]. In addition, with MWA, protection of nerves and other tissues around the thyroid can effectively reduce the occurrence of complications. Seven patients in the surgery group had transient hypocalcemia, which was restored within 2 months after calcium supplement treatment. The use of the MOST and hydrodissection can minimize potential damage to other important tissues during MWA. When nodules are too close to critical structures to be separated by hydrodissection during MWA, a safety margin of 2–3 mm is preserved to protect the important structures. Moreover, two patients in the surgery group and one patient in the MWA group experienced voice changes, all of which improved in 2 months. For the patients in the surgery group, the voice changes may have been caused by inadvertent pulling on the recurrent laryngeal nerve during the operation. For the patient in the MWA group, the possible reason for the voice change was the relatively long ablation time, and hydrodissection may have gradually increased the temperature, causing the fluid to be absorbed and thus resulting in thermal damage. Furthermore, several patients developed postoperative hematomas in both groups, which were reabsorbed within 2 months. In lobectomy surgery, successful ligation of blood vessels and timely hemostasis during the operation are the keys to avoiding hematoma development. In MWA, the use of small-bore needles and intraoperative color Doppler monitoring can reduce the risk of this complication compared with surgery [26].
Moreover, the operation time and hospitalization time were shorter in the MWA group than in the surgery group, which is consistent with reports in the literature [27]. Notably, similar to previous studies, MWA and surgery effectively alleviated patients’ symptoms and cosmetic issues [28], and MWA yielded better esthetic results due to its needle-sized incisions and a faster recovery.
This study still has certain limitations. First, this is a small, retrospective, single-center study. Second, although no regrowth of the nodules was noted within 12 months, benign nodules grow slowly, and the 12-month follow-up was not sufficient to assess recurrence. In the future, a long-term, prospective, multicenter study should be conducted to further validate the results.
Conclusion
In summary, this study showed that MWA is a safe and effective treatment for benign thyroid nodules > 4 cm. MWA is characterized by a faster recovery, fewer complications, better protection of thyroid function, and superior esthetic results relative to those for lobectomy and may become an alternative to surgery in clinical practice.
References
C. Durante, G. Grani, L. Lamartina, S. Filetti, S.J. Mandel, D.S. Cooper, The diagnosis and management of thyroid nodules: a review. JAMA 319(9), 914–924 (2018). https://doi.org/10.1001/jama.2018.0898
J. Yan, T. Qiu, J. Lu, Y. Wu, Y. Yang, Microwave ablation induces a lower systemic stress response in patients than open surgery for treatment of benign thyroid nodules. Int. J. Hyperth. 34(5), 606–610 (2018). https://doi.org/10.1080/02656736.2018.1427286
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26(1), 1–133 (2016). https://doi.org/10.1089/thy.2015.0020
Y. Korkusuz, O.M. Mader, W. Kromen, C. Happel, S. Ahmad, D. Groner, M. Koca, A. Mader, F. Grunwald, H. Korkusuz, Cooled microwave ablation of thyroid nodules: initial experience. Eur. J. Radiol. 85(11), 2127–2132 (2016). https://doi.org/10.1016/j.ejrad.2016.09.019
W.W. Yue, S.R. Wang, F. Lu, L.P. Sun, L.H. Guo, Y.L. Zhang, X.L. Li, H.X. Xu, Radiofrequency ablation vs. microwave ablation for patients with benign thyroid nodules: a propensity score matching study. Endocrine 55(2), 485–495 (2017). https://doi.org/10.1007/s12020-016-1173-5
I.J. Nixon, P. Angelos, A.R. Shaha, A. Rinaldo, M.D. Williams, A. Ferlito, Image-guided chemical and thermal ablations for thyroid disease: review of efficacy and complications. Head. Neck 40(9), 2103–2115 (2018). https://doi.org/10.1002/hed.25181
P. Liang, Y. Wang, X. Yu, B. Dong, Malignant liver tumors: treatment with percutaneous microwave ablation–complications among cohort of 1136 patients. Radiology 251(3), 933–940 (2009). https://doi.org/10.1148/radiol.2513081740
J. Yu, P. Liang, X.L. Yu, Z.G. Cheng, Z.Y. Han, X. Zhang, J. Dong, M.J. Mu, X. Li, X.H. Wang, US-guided percutaneous microwave ablation versus open radical nephrectomy for small renal cell carcinoma: intermediate-term results. Radiology 270(3), 880–887 (2014). https://doi.org/10.1148/radiol.13130275
L. Sidoff, D.E. Dupuy, Clinical experiences with microwave thermal ablation of lung malignancies. Int. J. Hyperth. 33(1), 25–33 (2017). https://doi.org/10.1080/02656736.2016.1204630
J. Xu, H. Wu, Z. Han, J. Zhang, Q. Li, J. Dou, C. An, E. Qi, J. Yu, P. Liang, Microwave ablation of benign breast tumors: a prospective study with minimum 12 months follow-up. Int. J. Hyperth. 35(1), 253–261 (2018). https://doi.org/10.1080/02656736.2018.1494340
W.J. Wu, X.H. Gong, Q. Zhou, X. Chen, X.J. Chen, B.M. Shi, US-guided percutaneous microwave ablation for the treatment of benign thyroid nodules. Endocr. J. 64(11), 1079–1085 (2017). https://doi.org/10.1507/endocrj.EJ17-0152
X. Zhi, N. Zhao, Y. Liu, J.B. Liu, C. Teng, L. Qian, Microwave ablation compared to thyroidectomy to treat benign thyroid nodules. Int. J. Hyperth. 34(5), 644–652 (2018). https://doi.org/10.1080/02656736.2018.1456677
K.L. McCoy, N. Jabbour, J.B. Ogilvie, N.P. Ohori, S.E. Carty, J.H. Yim, The incidence of cancer and rate of false-negative cytology in thyroid nodules greater than or equal to 4 cm in size. Surgery 142(6), 837–844.e833 (2007). https://doi.org/10.1016/j.surg.2007.08.012
E.J. Ha, J.H. Baek, J.H. Lee et al. Sonographically suspicious thyroid nodules with initially benign cytologic results: the role of a core needle biopsy. Thyroid 23(6), 703–708 (2013). https://doi.org/10.1089/thy.2012.0426
S. Bernardi, C. Dobrinja, B. Fabris, G. Bazzocchi, N. Sabato, V. Ulcigrai, M. Giacca, E. Barro, N. De Manzini, F. Stacul, Radiofrequency ablation compared to surgery for the treatment of benign thyroid nodules. Int. J. Endocrinol. 2014, 934595 (2014). https://doi.org/10.1155/2014/934595
Z. Cheng, Y. Che, S. Yu, S. Wang, D. Teng, H. Xu, J. Li, D. Sun, Z. Han, P. Liang, US-guided percutaneous radiofrequency versus microwave ablation for benign thyroid nodules: a prospective multicenter study. Sci. Rep. 7(1), 9554 (2017). https://doi.org/10.1038/s41598-017-09930-7
H. Dobnig, K. Amrein, Monopolar radiofrequency ablation of thyroid nodules: a prospective austrian single-center study. Thyroid. 28(4), 472–480 (2018). https://doi.org/10.1089/thy.2017.0547
C. Vorlander, K. David Kohlhase, Y. Korkusuz, C. Erbelding, W. Luboldt, I. Baser, H. Korkusuz, Comparison between microwave ablation and bipolar radiofrequency ablation in benign thyroid nodules: differences in energy transmission, duration of application and applied shots. Int. J. Hyperth. 35(1), 216–225 (2018). https://doi.org/10.1080/02656736.2018.1489984
J. Li, Y. Liu, J. Liu, P. Yang, X. Hu, L. Qian, A comparative study of short-term efficacy and safety for thyroid micropapillary carcinoma patients after microwave ablation or surgery. Int. J. Hyperth. 36(1), 640–646 (2019). https://doi.org/10.1080/02656736.2019.1626492
P. Del Rio, M. Rossini, C.M. Montana, L. Viani, G. Pedrazzi, T. Loderer, F. Cozzani, Postoperative hypocalcemia: analysis of factors influencing early hypocalcemia development following thyroid surgery. BMC Surg. 18(Suppl 1), 25 (2019). https://doi.org/10.1186/s12893-019-0483-y
D. Ahn, G.J. Lee, J.H. Sohn, Levothyroxine supplementation following hemithyroidectomy: incidence, risk factors, and characteristics. Ann. Surg. Oncol. 26(13), 4405–4413 (2019). https://doi.org/10.1245/s10434-019-07786-x
Y.H. Jung, H.B. Jung, C. Hoon, K.K. Jae, H.L. Jeong, Symptomatic benign thyroid nodules: efficacy of additional radiofrequency ablation treatment session—prospective randomized study. Radiology 263, 909–916 (2012). https://doi.org/10.1148/radiol.12111300
B. Wang, Z.Y. Han, J. Yu, Z. Cheng, F. Liu, X.L. Yu, C. Chen, J. Liu, P. Liang, Factors related to recurrence of the benign non-functioning thyroid nodules after percutaneous microwave ablation. Int. J. Hyperth. 33(4), 459–464 (2017). https://doi.org/10.1080/02656736.2016.1274058
Y.J. Liu, L.X. Qian, D. Liu, J.F. Zhao, Ultrasound-guided microwave ablation in the treatment of benign thyroid nodules in 435 patients. Exp. Biol. Med. 242(15), 1515–1523 (2017). https://doi.org/10.1177/1535370217727477
E. Bandeira-Echtler, K. Bergerhoff, B. Richter, Levothyroxine or minimally invasive therapies for benign thyroid nodules. Cochrane Database Syst. Rev. (6), CD004098 (2014). https://doi.org/10.1002/14651858.CD004098.pub2
H. Gharib, L. Hegedus, C.M. Pacella, J.H. Baek, E. Papini, Clinical review: nonsurgical, image-guided, minimally invasive therapy for thyroid nodules. J. Clin. Endocrinol. Metab. 98(10), 3949–3957 (2013). https://doi.org/10.1210/jc.2013-1806
S.Y. Liu, W.H. Guo, B. Yang, Y.F. Li, X.Y. Huang, X.Q. Wang, J. Chen, D. Xue, X.H. Zhou, Comparison of stress response following microwave ablation and surgical resection of benign thyroid nodules. Endocrine 65(1), 138–143 (2019). https://doi.org/10.1007/s12020-019-01900-5
B. Feng, P. Liang, Z. Cheng, X. Yu, J. Yu, Z. Han, F. Liu, Ultrasound-guided percutaneous microwave ablation of benign thyroid nodules: experimental and clinical studies. Eur. J. Endocrinol. 166(6), 1031–1037 (2012). https://doi.org/10.1530/eje-11-0966
Acknowledgements
This study was funded by the Finance Department of Jilin Province (No. SCZSY201701) and the Jilin Province Science and Technology Department (No. 20190303140SF).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dong, P., Wu, XL., Sui, GQ. et al. The efficacy and safety of microwave ablation versus lobectomy for the treatment of benign thyroid nodules greater than 4 cm. Endocrine 71, 113–121 (2021). https://doi.org/10.1007/s12020-020-02338-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02338-w