Abstract
Objectives
Minimal extrathyroid extension (mETE) was removed from the TNM staging system. This study was designed prospectively to compare the safety and efficacy of microwave ablation (MWA) versus surgery for treating T1N0M0 papillary thyroid carcinomas (PTC) with sonographically detected mETE.
Methods
From December 2019 to April 2021, 198 patients with T1N0M0 mETE-PTCs evaluated by preoperative ultrasound from 10 hospitals were included. Ninety-two patients elected MWA, and 106 patients elected surgery for treatment. MWA was performed using extensive ablation with hydrodissection. Surgery consisted of lobectomy with ipsilateral central lymph node dissection (CLD), lobe and isthmus excision with ipsilateral CLD and total thyroidectomy with ipsilateral CLD. The rates of technical success, cost, oncologic outcomes, complications and quality of life of the two groups were assessed.
Results
The follow-up times for the MWA and surgery groups were 12.7 ± 4.1 and 12.6 ± 5.0 months, respectively. The technical success rate was 100% for both groups. Oncological outcomes of the two groups were similar during the follow-up (all p > 0.05). The MWA group had a shorter operation time, less blood loss and lower costs (all p < 0.001). Three complications (3.3%) were reported in the MWA group and 4 (3.8%) in the surgery group (p = 0.846). The surgery group had higher scores for scar problems and anxiety (p < 0.001 and p = 0.003, respectively).
Conclusions
Microwave ablation was comparable in the short term to surgery in terms of treatment safety and efficacy in selected patients with T1N0M0 mETE-PTC detected by ultrasound.
Key Points
• Microwave ablation is comparable to surgery in the safety and short-term efficacy for PTCs with sonographically detected mETE.
• Thermal ablation is technically feasible for mETE-PTC treatment.
• Patients with mETE-PTC have similar quality of life in the two groups, except for worse scar problems and anxiety in the surgery group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The incidence of papillary thyroid carcinoma (PTC) is increasing rapidly worldwide [1]. In general, PTCs show indolent characteristics, especially those in stage T1 [2], but some clinically aggressive features still result in controversy regarding clinical significance and disease management [3].
Extrathyroid extension (ETE) of the primary tumour was reported as a risk factor for poor prognosis and has been accepted as an important factor for determining surgical extent in patients with PTC [4, 5]. On histology, ETE has been divided into two grades based on the extent of invasion. One grade is ‘minimal ETE (mETE)’, which was defined as an invasion of the tumour to the capsule, sternothyroid muscle, or perithyroidal soft tissue, and the other is ‘gross ETE (gETE)’, including extension to subcutaneous soft tissues, the larynx, the trachea, oesophagus, or the recurrent laryngeal nerve, and extension to the prevertebral fascia, mediastinal vessels, or the carotid artery [6]. In the recently released 8th American Joint Committee on Cancer (AJCC) TNM staging system, mETE was removed from the T3 stage classification, which means that a PTC diameter no more than 2 cm with mETE (mETE-PTC) was reclassified as T1 [7].
Lobectomy is recommended by most professional society guidelines as the definitive treatment for those reclassified T1 stage PTCs [8, 9]. Although most patients who undergo surgery have excellent outcomes, surgery may lead to temporary or permanent recurrent laryngeal nerve paralysis, hypothyroidism, hypoparathyroidism [10, 11], and an unsightly scar [12]. In addition, many surgeons are also seeking a less aggressive method for tumours with such an indolent nature, such as partial thyroidectomy [13, 14].
Thermal ablation (TA) has been reported as an optional curative treatment method for T1N0M0 PTC treatment with the advantage of minimal invasiveness [15,16,17,18,19]. However, PTCs with ultrasound (US)–detected mETE are always excluded from TA due to the possibility of aggressive features and the high risk of thermal injury [20]. No research has yet been performed to prove its feasibility.
This study aimed to compare the safety and efficacy of microwave ablation (MWA) versus open surgery for treating T1N0M0 PTC with sonographically detected mETE.
Materials and methods
Patients
This prospective multicentre study was approved by the Institutional Ethics Committees of PLA General Hospital. Informed consent was obtained from all patients or their responsible caregivers before enrolment.
The inclusion criteria were as follows: (1) single solitary suspicious thyroid nodule diameter of 2 cm or less detected by US; (2) preoperative sonographically detected invasion of the capsule, sternothyroid muscle, or perithyroidal soft tissue; (3) no sonographic evidence of lymph node metastasis or distant metastasis; (4) fine needle aspiration (FNA) or core needle biopsy (CNB)–confirmed PTC before ablation or surgery; and (5) no prior therapy for thyroid issues. Patients with severe conditions, vocal cord palsy, clinically apparent multicentricity or coexisting thyroid malignancies such as medullary carcinoma were excluded.
We identified sonographically detected capsule invasion or mETE with features of capsular abutment by the nodule, subtle capsular distortion or bulging of the normal thyroid contour, but without replacement of the strap muscle or obtuse margins between the tumour and trachea, oesophagus, mediastinal vessels, or carotid artery [21].
The eligibility of patients was evaluated by interventional radiologists and surgeons. Surgery and MWA were recommended for the eligible patients if they refused AS, with the notification of the advantages and disadvantages of both methods and that surgery was the current standard therapy while thermal ablation was just a new technique. Patients chose MWA or surgery according to their will.
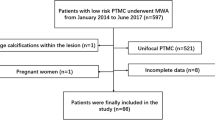
From December 2019 to April 2021, 201 patients were admitted according to the inclusion criteria. After exclusion of 3 patients, 198 patients were enrolled in the present study, and 92 were treated with MWA 106 with surgery (Fig. 1). Patients were divided into an MWA group and a surgery group according to their operation method.
Pre-ablation evaluations
Laboratory tests, including complete blood count and thyroid function tests, and imaging studies, including chest radiography, US of the thyroid and cervical lymph nodes, and examinations of the bilateral vocal cords with fiberoptic laryngoscopy, were performed in all patients before treatment.
US examination played a key role in characterising the target tumour and distinguishing the relationship between the tumour and the thyroid capsule by experienced ultrasonography physicians with more than 12 years of experience. The instruments applied included Philips iU22 Ultrasound System (Philips Healthcare), Siemens Acuson Sequoia 512 Ultrasound System (Siemens) or a Mindray M9 Ultrasound System (Mindray). For each tumour, the maximal diameter (a) and two orthogonal diameters (b and c), echogenic features and the internal vascularity on US and the location of capsule extension were assessed. The volume of tumours observed by US was estimated by the ellipsoid formulation V = πabc/6. According to the US presentation of the internal nodule on colour Doppler flow imaging (CDFI), the nodular vascular scores were classified into four grades (18). The anterior capsule refers to the capsule close to the anterior cervical muscle, the medial capsule close to the trachea, the lateral capsule close to the carotid sheath, and the posterior capsule close to the retropharyngeal space.
Operation procedures
MWA
High-resolution linear probes (6–12 MHz) were employed in the guidance of biopsies, preablation evaluation, ablation procedures and follow-up. The MWA system applied in this study was the KY-2000 2450 MHz microwave system (KY2000, Canyon Medical Instruments) with a 16-gauge, Teflon-coated, internal-cooled microwave antenna.
All MWA procedures were performed by experienced ultrasonography physicians with more than 7 years of experience on interventional sonography. The operation procedure of MWA for mETE-PTC was the same as that described in earlier papers for lesions located centrally on the gland [17]. Hydrodissection was performed more carefully in mETE-PTC ablation to prevent unexpected thermal injury. A safe distance between the tumour and the critical structure was maintained throughout the operation to protect the critical structures from thermal injury [22]. Contrast-enhanced ultrasound (CEUS) (SonoVueR used as contrast agent) was performed to evaluate the completeness of the ablation 1 h later, which required the ablation area to be extended no less than 3 mm beyond the tumour edge (Fig. 2).
Images in a 47-year-old man with papillary thyroid carcinoma with minimal capsule invasion in the right lobe of the thyroid treated with microwave ablation. a Pre-ablation US image of the tumour (arrowheads). b Hydrodissection technique (arrows) was used to protect the carotid artery and vagus nerve. c Hyperechoic pattern in tumour during the ablation procedure (arrowheads). d Postablation contrast-enhanced US image shows no enhancement in the tumour area (arrowheads)
Surgery
Thyroidectomy was performed by surgeons with more than 6 years of experience in thyroid surgery. The range of thyroid excision was determined according to the ATA guidelines. Of all the patients, 6 (5.7%) underwent lobectomy with ipsilateral central lymph node dissection (CLD), 45 (42.5%) underwent lobe and isthmus excision with ipsilateral CLD, and 55 (51.9%) underwent total thyroidectomy with ipsilateral CLD because of the presence of sonographic benign nodules in the other lobe. The glands and lymph nodes excised were sent for pathologic examination to identify the pathological type.
For both groups, the operation time was defined as from the beginning of skin disinfection until the patient left the operating room. Immediate postoperative pain score scaled from 0 to 10 according to the patient feeling. The costs of MWA included the preoperative examination, operation (MWA needle and other consumable fees), local anaesthesia fees and hospital bed, nursing and postoperative medication fees if needed. The costs of surgery included the preoperative examination, operation (including the use of nerve monitoring, haemostatic materials and other consumables), general anaesthesia, hospital bed, nursing and postoperative medication fees. Complications were defined according to the reporting standards of thyroid ablation [15].
Follow-up
All patients in both groups had their TSH suppressed in a range of 0.5–1 mU/L to reduce tumour recurrence risk. The US presentations and thyroid functions of patients were evaluated and recorded at the 3rd, 6th, and 12th months in the first year after treatment and every 6–12 months thereafter. CEUS was performed 6 months and 12 months after MWA to verify the effectiveness of the treatment. The effectiveness of MWA was defined as the absence of enhancement of any areas of the mass. Ultrasonographically suspected local tumour progression (LTP), lymph node metastasis (LNMs) or new lesions of both groups were confirmed by biopsy.
The LTP was defined as the appearance of a new nodule with typical features of thyroid cancer in the edge of the ablation zone and confirmed by FNA or CNB. LNMs were the new detected abnormal lymph nodes with pathologic results of PTC metastasis. New lesion was defined as new recurrent malignant thyroid tumour in thyroid gland. Distant metastasis was PTC cells metastasised to other organs beyond cervical lymph nodes. Additional ablation or surgical resection might be applied for unsuccessfully treated or recurrent tumours based on patients’ intentions.
We used two Chinese version questionnaires to evaluate the quality of life of patients in both groups during the follow-up, including the Thyroid Cancer-specific Quality of Life (THYCA-QoL) and the Hospital Anxiety and Depression Scale (HADS). The THYCA-QoL is a specific scale for patients with thyroid cancer, consisting of seven symptom areas and six single items [23]. HADS is commonly used in diagnosing anxiety and major depressive disorders in patients with cancer [24].
Statistical analysis
Quantitative data measurements are described as the means ± standard deviations (SDs). We compared data for the two groups using Student’s unpaired t test. Categorical data comparisons were performed using the chi-squared test or Fisher’s exact test. Patients’ progression-free survival curves were generated by Kaplan-Meier method, and between-group differences were assessed by log-rank test. All analyses were performed with SPSS26. Difference was considered significant when p < 0.05.
Results
The number of enrolled patients and operators’ experience in the 10 participating institutions are listed in Supplementary Table 1. The mean follow-up times for the MWA and surgery groups were 12.7 ± 4.1 and 12.6 ± 5.0 months, respectively.
Patients and tumours
The general information of the two groups is shown in Table 1, and tumour characteristics are shown in Table 2.
The diameter and volume of tumours in the MWA group vs. surgery group were 0.81 ± 0.30 cm vs. 0.89 ± 0.33 cm and 0.23 ± 0.33 mL vs. 0.32 ± 0.37 mL, respectively (p = 0.067 and p = 0.067). No difference was found in US characteristics, including tumour echogenicity, vascularity, calcification and location (all p > 0.05). The numbers of tumours with T1a stage and T1b stage in the MWA group vs. surgery group were 77 (83.7%) vs. 82 (77.4%) and 15 (16.3%) vs. 24 (22.6%), respectively (p = 0.263). The numbers of tumours extending anterior, posterior, medial and lateral thyroid capsules in the MWA group vs. surgery group were 49 (53.3%) vs. 52 (49.1%), 17 (18.5%) vs. 30 (28.3%), 11 (12.0%) vs. 12 (11.3%) and 15 (16.3%) vs. 12 (11.3%), respectively (p = 0.378).
Pathology result of the surgery group
The pathological results of excised thyroid gland in the surgery group are shown in Supplementary Table 2. Presence of preoperative US-undetectable additional microcarcinomas was confirmed in 6 (5.7%) patients, and central LNMs in 26 (24.5%) patients, with ≤ 5 nodes in 20 patients, 6–10 in 4 patients and 11–20 in 2 patients. Pathology results also showed 12 (11.3%) tumours confined in the gland without capsule invasion, 93 (87.7%) with invasion into the capsule or through the capsule into fibrous or adipose tissue around glands (mETE), and 1 (0.9%) adjacent to a few skeletal muscles outside the capsule (gETE).
Treatment variables and safety
The treatment variables and complications of the two groups are presented in Tables 3 and 4. The MWA group had shorter operation time, less blood loss, lower postoperative pain score and lower treatment costs in general than the surgery group (all p < 0.05).
Complete absence of enhancement at CEUS was observed in all target tumours at the end of ablation. The technical success rate was 100%. In the MWA group, 3 (3.3%) complications were reported, which were all hoarseness, while in the surgery group, 4 (3.8%) complications, including 2 (1.9%) hoarseness (one ipsilateral and one contralateral to the primary tumour) and 2 (1.9%) infections, were reported (p = 0.846). In the subgroup analysis of stage, the incidences of complications of MWA vs. surgery were 2 (2.6%) vs. 4 (4.9%) in T1a and 1 (6.7%) vs. 0 (0%) in T1b (all p > 0.05). In subgroup analyses of anterior, posterior, medial and lateral thyroid capsule extension, the incidences of complications of MWA vs. surgery were 0 (0%) vs. 3 (5.8%), 3 (17.6%) vs. 0 (0%), 0 (0%) vs.0 (0%) and 0 (0%) vs. 1 (8.3%), respectively. The complication incidence rate of MWA for tumours with posterior capsule extension was significantly higher than surgery (p = 0.019). Of all the complications that occurred, 1 (0.9%) patient in the surgery group had permanent recurrent laryngeal nerve injury (ipsilateral to the primary tumour), which demonstrated persistent dysphonia and documented palsy by fiberoptic laryngoscopy more than 6 months after surgery. All voice hoarseness reported in the MWA group recovered within 3 months after ablation.
Treatment efficacy
The oncological outcomes of the two treatment methods are shown in Supplementary tables 3.1–3.2. Patients in the MWA group had no new lesions in the remaining parenchyma of the gland, while 1 (0.9%) patient in the surgery group had a new lesion in the contralateral lobe (p = 0.352). The MWA group included 2 (2.2%) cases with cervical LNMs, and the surgery group included 2 (1.9%) cases with cervical LNMs in the untreated central neck during follow-up (p = 0.866). No LTP or distant metastasis was identified in either group. No significant differences between the two groups were found in either stage or capsule extension location subgroup analysis (all p ≥ 0.05).
Quality of life
The results of the THYCA-QoL and HADS questionnaire scores are shown in Supplementary Table 4. The THYCA-QoL showed similar results regarding the specific domains affected, including voice, sympathetic symptoms, throat/mouth problems, psychological problems, sensory problems cold sensitivity, and weight gain, and had similar scores for the two groups (all p > 0.05), but for problems with scarring, the score of the surgery group was significantly higher (p < 0.001). The HADS questionnaire showed a higher anxiety score in the surgery group (p = 0.010) and similar depression scores between the two groups (p = 0.985). These results indicate a similar quality of life in the two groups, except for worse results for scar problems and anxiety in the surgery group.
Discussion
Current guidelines advise a reduction of diagnostic and therapeutic burden for low-risk thyroid cancers [25]. The available management approaches for T1N0M0 PTCs include surgery, thermal ablation, and active surveillance.
Active surveillance may be a good option for tumours located in the centre of the thyroid gland, but for mETE-PTCs, there are higher risk of developing into gETE and then upstaging to T3 in long-term surveillance. The psychological pressure of some patients about the progression of the disease also makes treatment necessary. Surgical resection is so aggressive that may do more harm than benefits for tumour with such indolent nature. US-guided thermal ablation represents an intermediate approach between active surveillance and surgery for mETE-PTC treatment with a principle of as little therapy as possible. In so far, MWA might be a better choice than surgery. In this multicentre prospective study, we compared the efficacy and safety of MWA and surgery in patients with US-detected T1N0M0 mETE-PTC, and our results demonstrated that MWA was technically feasible and we observed no significant different with surgery in terms of oncologic efficacy in short-time follow-up.
The first challenge faced by MWA treatment for PTC with mETE was its safety. The overall complication rates of MWA vs. surgery in our study were 3.3% vs. 3.8%. Similar results of 3.0–3.3% after TA and 1.2–4.5% after surgery were reported in previous studies [26,27,28,29]. However, it should be noted that MWA of tumours with posterior capsular extension has a significantly higher risk of hoarseness than surgery, with rates of 17.6% vs. 0%. This may be attributable to the proximity of the recurrent laryngeal nerve of tumours located near the posterior capsule. Thermal ablation necessitates a larger ablation zone, thereby increasing the risk of thermal injury to surrounding structures. This may indicate that, for tumours near the posterior capsule, MWA has a higher risk of temporary recurrent laryngeal nerve injury. However, all 3 cases of hoarseness due to mild thermal injuries quickly recovered within 3 months after treatment and no abnormality was found in vocal cord by laryngoscopy. In addition, 1 (0.9%) case of hoarseness in the surgical group was permanent. This may indicate that the damage to nerves caused by heat tends to be temporary, but inadvertent transection is hard to recover, and further research is valuable. Therefore, TA is safe in selected patients with T1N0M0 mETE-PTC.
LNM, especially central LNM, was another challenge for MWA. Some studies have shown favourable outcomes of TA in PTC without extrathyroidal invasion in a long-term follow-up [15, 30, 31]. Yan et al reported that 2.42% developed recurrent lesions, and 0.97% developed LNMs at a mean follow-up time of about 4 years and Zhang et al reported new lesions development and LNMs of TA vs. surgery for PTMC over 5 years follow-up, with incidences of 1.1% vs. 1.3% and 0 vs. 1.3%, respectively. Consistent with these results, 0 vs. 0.9% of new lesions and 2.2% vs. 1.9% of lymph metastases were found after MWA and surgery in our study. This may be part of the fact that mETE has no significant influence on the prognosis in solitary PTC [32,33,34]. In addition, our results showed that regardless of the tumours in T1a or T1b stage and the locations of capsule extension, the prognosis of the MWA group was similar to that of the surgical group. However, it should be noted that these results may be part of the short follow-up time and indolent nature of the tumour regardless of treatment strategy. Pathological results after dissection in surgery group showed that 24.5% patients had ultrasound-undetectable LNM and 5.7% had additional microcarcinoma foci, which could be similar in the MWA group for the same inclusion criteria. MWA could not eliminate ultrasound-undetectable LNM and microcarcinomas foci. Therefore, there were occasions that, for patients in the MWA group, only the primary lesion can be treated, but metastatic lymph nodes and additional foci remain. This might affect the incidence rate of LNM and NTC during the follow-up. Therefore, longer follow-up time was required to verify the LNM and NTC rate in this study. MWA may be as effective in the short term as surgery in treating primary thyroid cancer lesions.
Quality of life is an important measure for tumours with such good prognosis. The THYCA-QoL and HADS questionnaire results in our study showed similar scores in both groups, except for worse results for scar problems and anxiety in the surgery group. The higher anxiety scores of the surgery group may be related to the long-term thyroid hormone replacement therapy or that patients seriously anxious about their disease tend more to adopt surgical resection. MWA damages thyroid function less and does not require life-long hormone replacement, which may improve the patient’s survival experience. However, further preoperative psychological evaluation is needed.
The cost and convenience of treatment for patients cannot be ignored for tumours with such a high prevalence. In our centre, patients with TA can choose outpatient or inpatient treatment. Outpatients can be discharged after 1 h of postoperative observation without obvious discomfort. Hospitalised patients can be discharged the next day after 1 day of postoperative observation. But for patients who underwent surgery, they were generally discharged 2–3 days after the operation for postoperative observation in our country. At the same time, ablation treatment does not require general anaesthesia, which reduces the risk of anaesthesia accidents. However, this may be affected by national factors, and further multi-country studies are needed.
Evaluation of tumour relies on preoperative ultrasonographic images. Previous studies reported a sensitivity of 87.5% in the diagnosis of mETE with sonography [35, 36], and our surgery group result showed an accuracy of 87.7%. Of the remaining, 11.3% were capsule-invasion-free and 0.9% were gETE. In addition, consistent with previous study [29], 6 (5.7%) patients in the surgery group had US-undetectable microscopic cancer foci, and 26 (24.5%) patients had clinically negative LNMs. These suggest that this may be same in the MWA group. Studies reported no clear benefit of prophylactic CLD in patients with clinically node-negative PTC [29, 37, 38]. Long-term observational studies are needed to determine whether these US-undetectable subtle lesions, LNMs and gETE will affect the survival prognosis of patients after ablation.
This study has several limitations. First, the number of cases is small and the follow-up time is short. Papillary thyroid carcinoma is a tumour with indolent nature, positive events after operation may take a considerable time to be observed and the results may vary as subsequent studies are carried out. Second, the assessment of tumour depends largely on the experience of the sonographer and occult PTCs and LNMs may be missed due to the sensitivity limitation of US. It remains unclear whether these are clinically relevant. Third, the diagnosis of PTC is based mostly on cytological samples, some aggressive histological types may not be excluded [39] and the effect of different subtypes on prognosis cannot be analysed. However, the above two points are unavoidable problems that MWA needs to face in the real world. In this study, patients in both groups were enrolled with results of preoperative ultrasound assessment and FNA or CNB. The comparison results of the two treatment methods should be more persuasive in a long follow-up for the same inclusion criteria. Further comparison with active surveillance would be especially valuable to clarify the clinical significance of ablation therapy.
In conclusion, MWA was comparable in the short term to surgery in terms of treatment safety and efficacy in selected patients with T1N0M0 mETE-PTC detected by ultrasound. More patients with longer follow-up will be necessary to validate whether these findings are durable.
Abbreviations
- CLD :
-
Central lymph node dissection
- gETE :
-
Gross extrathyroid extension
- HADS:
-
Hospital Anxiety and Depression Scale
- LNMs:
-
Lymph node metastasis
- LTP :
-
Local tumour progression
- mETE :
-
Minimal extrathyroid extension
- MWA :
-
Microwave ablation
- PTC :
-
Papillary thyroid carcinoma
- TA :
-
Thermal ablation
- THYCA-QoL:
-
Thyroid Cancer-specific Quality of Life
- US :
-
Ultrasound
References
Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM (2017) Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA 317(13):1338–1348
Lubitz CC, Sosa JA (2016) The changing landscape of papillary thyroid cancer: epidemiology, management, and the implications for patients. Cancer 122(24):3754–3759
Povoa AA, Teixeira E, Bella-Cueto MR et al (2020) Clinicopathological features as prognostic predictors of poor outcome in papillary thyroid carcinoma. Cancers (Basel) 12(11)
Ito Y, Hirokawa M, Jikuzono T et al (2007) Extranodal tumor extension to adjacent organs predicts a worse cause-specific survival in patients with papillary thyroid carcinoma. World J Surg 31(6):1194–1201
Sia MA, Tsang RW, Panzarella T, Brierley JD (2010) Differentiated thyroid cancer with extrathyroidal extension: prognosis and the role of external beam radiotherapy. J Thyroid Res 2010:183461
Sobin LH, Compton CC (2010) TNM seventh edition: what's new, what's changed: communication from the International Union Against Cancer and the American Joint Committee on Cancer. Cancer 116(22):5336–5339
Tran B, Roshan D, Abraham E et al (2018) An analysis of The American Joint Committee on Cancer 8th Edition T Staging System for Papillary Thyroid Carcinoma. J Clin Endocrinol Metab 103(6):2199–2206
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26(1):1–133
Kim JH, Baek JH, Lim HK et al (2018) 2017 Thyroid Radiofrequency Ablation Guideline: Korean Society of Thyroid Radiology. Korean J Radiol 19(4):632–655
Lang BH-H, Wong CKH (2016) Lobectomy is a more cost-effective option than total thyroidectomy for 1 to 4 cm papillary thyroid carcinoma that do not possess clinically recognizable high-risk features. Ann Surg Oncol 23(11):3641–3652
Kazaure HS, Zambeli-Ljepovic A, Oyekunle T et al (2021) Severe hypocalcemia after thyroidectomy: an analysis of 7366 patients. Ann Surg 274(6):e1014–e1021
Sethukumar P, Ly D, Awad Z, Tolley NS (2018) Scar satisfaction and body image in thyroidectomy patients: prospective study in a tertiary referral centre. J Laryngol Otol 132(1):60–67
Dobrinja C, Pastoricchio M, Troian M et al (2017) Partial thyroidectomy for papillary thyroid microcarcinoma: is completion total thyroidectomy indicated? Int J Surg 41(Suppl 1):S34–S39
Nahm HJ, Choi SJ, Lim YC (2019) Conservative thyroidectomy for papillary thyroid microcarcinoma. Am J Otolaryngol 40(3):427–430
Zhang M, Tufano RP, Russell JO et al (2020) Ultrasound-guided radiofrequency ablation versus surgery for low-risk papillary thyroid microcarcinoma: results of over 5 years’ follow-up. Thyroid 30(3):408–417
Cao XJ, Liu J, Zhu YL et al (2020) Efficacy and safety of thermal ablation for solitary T1bN0M0 papillary thyroid carcinoma: a multicenter study. J Clin Endocrinol Metab 106(2):e573–e581
Cao XJ, Wang SR, Che Y et al (2021) Efficacy and safety of thermal ablation for treatment of solitary T1N0M0 papillary thyroid carcinoma: a multicenter retrospective study. Radiology 300(1):209–216
Zhang M, Luo Y, Zhang Y, Tang J (2016) Efficacy and safety of ultrasound-guided radiofrequency ablation for treating low-risk papillary thyroid microcarcinoma: a prospective study. Thyroid 26(11):1581–1587
Kim JH, Baek JH, Sung JY et al (2017) Radiofrequency ablation of low-risk small papillary thyroidcarcinoma: preliminary results for patients ineligible for surgery. Int J Hyperthermia 33(2):212–219
Association CUD (2019) Expert consensus of thermal ablation treatment for papillary thyroid microcarcinoma. Chin J Med Ultrasound 16(8):571–574
Moon SJ, Kim DW, Kim SJ, Ha TK, Park HK, Jung SJ (2014) Ultrasound assessment of degrees of extrathyroidal extension in papillary thyroid microcarcinoma. Endocr Pract 20(10):1037–1043
Wu J, Zhao ZL, Cao XJ et al (2021) A feasibility study of microwave ablation for papillary thyroid cancer close to the thyroid capsule. Int J Hyperthermia 38(1):1217–1224
Husson O, Haak HR, Mols F et al (2013) Development of a disease-specific health-related quality of life questionnaire (THYCA-QoL) for thyroid cancer survivors. Acta Oncol 52(2):447–454
Annunziata MA, Muzzatti B, Bidoli E et al (2020) Hospital Anxiety and Depression Scale (HADS) accuracy in cancer patients. Support Care Cancer 28(8):3921–3926
Zhu CY, Sha S, Tseng CH et al (2020) Trends in the surgical management of known or suspected differentiated thyroid cancer at a single institution, 2010–2018. Thyroid 30(11):1639–1645
Lim HK, Cho SJ, Baek JH et al (2019) US-guided radiofrequency ablation for low-risk papillary thyroid microcarcinoma: efficacy and safety in a large population. Korean J Radiol 20(12):1653–1661
Teng DK, Li HQ, Sui GQ et al (2019) Preliminary report of microwave ablation for the primary papillary thyroid microcarcinoma: a large-cohort of 185 patients feasibility study. Endocrine 64(1):109–117
Bergenfelz A, Salem AF, Jacobsson H et al (2016) Risk of recurrent laryngeal nerve palsy in patients undergoing thyroidectomy with and without intraoperative nerve monitoring. Br J Surg 103(13):1828–1838
Sippel RS, Robbins SE, Poehls JL et al (2020) A randomized controlled clinical trial: no clear benefit to prophylactic central neck dissection in patients with clinically node negative papillary thyroid cancer. Ann Surg 272(3):496–503
Xiao J, Zhang M, Zhang Y et al (2020) Efficacy and safety of ultrasonography-guided radiofrequency ablation for the treatment of T1bN0M0 papillary thyroid carcinoma: a retrospective study. Int J Hyperthermia 37(1):392–398
Yan L, Lan Y, Xiao J, Lin L, Jiang B, Luo Y (2021) Long-term outcomes of radiofrequency ablation for unifocal low-risk papillary thyroid microcarcinoma: a large cohort study of 414 patients. Eur Radiol 31(2):685–694
Bortz MD, Kuchta K, Winchester DJ, Prinz RA, Moo-Young TA (2020) Extrathyroidal extension predicts negative clinical outcomes in papillary thyroid cancer. Surgery:1–5
Hay ID, Johnson TR, Thompson GB, Sebo TJ, Reinalda MS (2016) Minimal extrathyroid extension in papillary thyroid carcinoma does not result in increased rates of either cause-specific mortality or postoperative tumor recurrence. Surgery 159(1):11–19
Woo CG, Sung CO, Choi YM et al (2015) Clinicopathological significance of minimal extrathyroid extension in solitary papillary thyroid carcinomas. Ann Surg Oncol 22(Suppl 3):S728–S733
Hu S, Zhang H, Sun Z et al (2020) Preoperative assessment of extrathyroidal extension of papillary thyroid carcinomas by ultrasound and magnetic resonance imaging: a comparative study. Radiol Med 125(9):870–876
Chung SR, Baek JH, Choi YJ et al (2020) Sonographic assessment of the extent of extrathyroidal extension in thyroid cancer. Korean J Radiol 21(10):1187–1195
Dobrinja C, Troian M, Cipolat Mis T et al (2017) Rationality in prophylactic central neck dissection in clinically node-negative (cN0) papillary thyroid carcinoma: is there anything more to say? A decade experience in a single-center. Int J Surg 41(Suppl 1):S40–S47
Moreno MA, Edeiken-Monroe BS, Siegel ER, Sherman SI, Clayman GL (2012) In papillary thyroid cancer, preoperative central neck ultrasound detects only macroscopic surgical disease, but negative findings predict excellent long-term regional control and survival. Thyroid 22(4):347–355
Bayona A, Benavent P, Muriel A et al (2021) Outcomes of repeat fine needle aspiration biopsy for AUS/FLUS thyroid nodules. A systematic review and meta-analysis. Eur J Endocrinol 185(4):497–506
Acknowledgements
All authors contributed to the idea, gathered the information, interpreted the data, and wrote and approved the final version of the manuscript.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ping Liang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethics approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• multicentre study performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 35 kb)
Rights and permissions
About this article
Cite this article
Zheng, L., Dou, Jp., Liu, Fy. et al. Microwave ablation vs. surgery for papillary thyroid carcinoma with minimal sonographic extrathyroid extension: a multicentre prospective study. Eur Radiol 33, 233–243 (2023). https://doi.org/10.1007/s00330-022-08962-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08962-6