Abstract
Purpose
Little is known about the underlying physiology that contributes to Haemoglobin A1c (HbA1c) in the normal and pre-diabetic range. We determined the contribution of fasting plasma glucose (FPG), 2-h plasma glucose (2hPG), insulin secretion, insulin sensitivity and endogenous glucose production to HbA1c levels in the normal and pre-diabetic range.
Methods
A total of 62 Danish men and women with normal or impaired glucose regulation were studied. HbA1c levels were measured and participants underwent an oral glucose tolerance test with measurements of FPG and 2hPG, an intravenous glucose tolerance test for determination of first-phase insulin release, and a hyperinsulinaemic euglycaemic clamp for estimation of peripheral and hepatic insulin sensitivity. Associations of HbA1c with the different measures of glucose metabolism were analysed by linear regression analysis.
Results
HbA1c levels ranged from 28 to 45 mmol/mol (4.7–6.3%) in the study population. 1 SD higher (log) FPG concentration (~1 mmol/L) was associated with 2 mmol/mol higher HbA1c concentration (P < 0.001). In comparison, 1 SD higher levels of (log) first-phase insulin secretion or (log) disposition index were associated with 1.5 mmol/mol lower HbA1c levels (P < 0.05). HbA1c was not associated with peripheral or hepatic insulin sensitivity, endogenous glucose production or 2hPG levels.
Conclusion
HbA1c levels within the normal and pre-diabetic range seem to reflect decreased insulin secretion to a higher extent than insulin resistance. Therefore, early prevention strategies for high-risk individuals identified by HbA1c are not straightforward. More research on how to improve the health of beta cells either directly or indirectly in high-risk individuals is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term ‘pre-diabetes’ represents collective dysglycaemic states intermediate between normal glucose regulation and diabetes. Up to 70% of individuals with pre-diabetes will develop diabetes over their lifetime, and therefore early diagnosis and preventive interventions in individuals with pre-diabetes are essential [1]. Furthermore, diabetes-related complications may be seen in individuals with pre-diabetes, prior to or independent of their conversion to overt diabetes [2].
Individuals with pre-diabetes have marked differences in their underlying pathophysiology depending on the specific type of pre-diabetes. Historically, ‘pre-diabetes’ referred to people with impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT)—as they can occur in isolation or in combination (IFG + IGT). It is important to note that the definition of IGT derives from the 2-h oral glucose tolerance test (OGTT)—a test rarely performed in non-pregnant adults in clinical practice. The OGTT is inconvenient for both patient and health care provider, and additionally misclassification is common due to high day-to-day variability in 2-h plasma glucose (2hPG) concentrations (46%) [3]. Nevertheless, abandonment of the OGTT leaves much unknown about relevant physiologic differences in pre-diabetes subtypes, e.g., differences in insulin sensitivity and insulin secretion, which seems relevant for targeted preventive interventions [4].
With the standardisation of the haemoglobin A1c (HbA1c) assay, in 2010, the American Diabetes Association advocated its use in the diagnosis of both diabetes and pre-diabetes with a cut-point of 39-47 mmol/mol (5.7–6.4%) for the latter [5]. The International Expert Committee suggested a cut-point of 42–47 mmol/mol (6.0–6.4%) for identifying high-risk individuals [6]. In addition, HbA1c is the clinical benchmark for the prevention of diabetes-related complications, which is relevant not only in diabetes but also in pre-diabetes. This is best exemplified in the long-term follow-up of the UK Prospective Diabetes Study, clearly demonstrating a reduction in the classic complications of diabetes in participants achieving reductions in HbA1c into the normal versus the pre-diabetic HbA1c range [7]. With the advent of personalised medicine, however, further delineation of preventive strategies may rely on knowing more about the defects that contribute to HbA1c levels in the pre-diabetic range. Thus, the aim of the present analysis was to describe the underlying physiology of different HbA1c levels and to quantify the contributions of fasting plasma glucose (FPG), 2hPG, insulin secretion and insulin sensitivity to HbA1c levels in the normal and pre-diabetic range.
Materials and methods
Study population
In 2004–2006, 66 study participants were recruited from the Danish population-based Inter99 study [8] to participate in a study examining the pathophysiology of isolated IFG (i-IFG) versus isolated IGT (i-IGT) [9]. Four persons had a missing HbA1c value, so the analyses are based on 62 study participants of whom 20 had normal glucose tolerance (NGT), 16 had i-IFG and 26 had i-IGT based on the WHO 1999 definition. The recruitment of participants and the study procedures have been described in detail elsewhere [9].
Study procedures
Participants underwent examination of first-phase insulin release and whole-body insulin sensitivity after an overnight fast. Basal samples for determination of plasma glucose, serum insulin and HbA1c were obtained. Thereafter, the study started out with a basal period of 2 h for estimation of endogenous glucose production (EGP). The basal period was initiated by an adjusted priming tracer dose of [3-3H]-glucose followed by a constant intravenous tracer infusion (0.22 MBq/h), which was continued for the entire study period of 4.5 h. After the 2-h basal period, a 30-min intravenous glucose tolerance test (IVGTT) was performed to characterise first-phase insulin release. The IVGTT was initiated by a 1-min intravenous glucose bolus (20% [wt/vol.], 0.3 g/kg body weight) infused at time 0 min. Blood samples were drawn for determination of whole blood glucose and serum insulin concentrations at −2, 0, 2, 4, 6, 8, 10 and 30 min. Thereafter, a 2-h euglycaemic–hyperinsulinaemic clamp (40 mU/m2/min) was initiated for estimation of peripheral insulin sensitivity [10]. During the clamp, a 20% glucose solution was infused at a variable rate, adjusted every 5 min in order to maintain a predetermined blood glucose concentration of 5 mmol/l. 3H-labelled glucose (3,670 Bq/ml [3-3H]-glucose) was added to the infused glucose solution to obtain constant specific activity during insulin infusion.
Body weight was measured to the nearest 0.1 kg using a standard electronic weighing machine (BWB-620A; Tanita, Chicago, IL, USA) with the participant wearing light clothes. Height was measured to the nearest 0.5 cm with the participant not wearing shoes. Body fat content and fat-free mass were estimated using a bioimpedance analyser (Biodynamics, Seattle, WA, USA). Information on smoking was captured from a questionnaire.
Calculations
First-phase insulin release was calculated as the incremental area under the curve for insulin during the first 10 min of the IVGTT using the trapezoidal rule. Peripheral insulin sensitivity was calculated from the clamp as the glucose rate of disappearance divided by the mean serum insulin concentration during the last 30 min steady-state period of the clamp. Relative beta-cell function (expressed as the disposition index [11]) was calculated as peripheral insulin sensitivity multiplied by first-phase insulin secretion. We estimated basal EGP in the basal steady-state period using the Steeleʼs non-steady-state equation [12]. This method takes minor fluctuations in blood glucose concentration into account. EGP was calculated as the ratio between the tracer infusion rate (Bq/mg) and the specific activity (Bq/mg). Hepatic insulin sensitivity was calculated as 1/(EGP × fasting serum insulin concentration) [13]. Insulin-stimulated non-oxidative glucose metabolism was calculated from tritiated glucose as total glucose metabolism minus the glucose oxidation rate [14].
Biochemical analysis
Plasma glucose concentration was determined using the Hitachi 912 system (Roche Diagnostics, Mannheim, Germany) and [3-3H]glucose activity was determined from evaporated plasma samples [15]. Serum insulin concentration was measured by immunoassay (AutoDELFIA, Perkin Elmer, Waltham, MA, USA) and HbA1c by high performance lipid chromatography.
Statistical analyses
For presentation of data, study participants were divided into quartiles of HbA1c. The different measures of glucose metabolism and the distribution of glucose tolerance status were analysed across these quartiles. Furthermore, associations of HbA1c with FPG, 2hPG, first-phase insulin release, peripheral insulin sensitivity, hepatic insulin sensitivity and disposition index were analysed by linear regression analysis using HbA1c as a continuous variable. Measures of glucose metabolism were log-transformed and standardised prior to analysis to facilitate direct comparisons of the regression coefficients. Associations were calculated both with and without adjustment for age, sex, BMI and smoking status. All analyses were performed in R version 3.3.3 (The R Foundation for Statistical Computing) and SAS version 9.4 (SAS Institute, Cary, NC). Statistical significance was inferred at a two-tailed P value < 0.05.
Results
Characteristics of the study participants are presented in Table 1. Table 2 shows the measures of glucose metabolism derived from the OGTT, IVGTT and the euglycaemic–hyperinsulinaemic clamp by quartiles of HbA1c. The prevalence of current smokers was highest in the highest quartile of HbA1c. There were no differences in the proportion of individuals with NGT, i-IGT or i-IFG across the quartiles; however, the proportion of individuals with i-IFG tended to increase from the lowest to the highest HbA1c quartile. In support of this, FPG concentrations increased progressively from the lowest to the highest HbA1c quartile, whereas no trend was seen for 2hPG concentrations.
First-phase insulin release and the disposition index decreased from Q1 to Q4, whereas the levels of peripheral and hepatic insulin sensitivity as well as EGP and non-oxidative glucose disposal did not differ across HbA1c quartiles (Table 2). Adjusting the analysis for age, sex, BMI and smoking did not change any of the results.
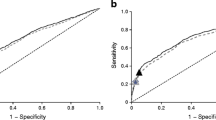
The mean differences in HbA1c by a SD difference in log of the different measures of glucose metabolism are shown in Fig. 1. 1 SD higher (log) FPG concentration (~1 mmol/L) was associated with 2 mmol/mol higher HbA1c concentration. In comparison, 1 SD higher levels of (log) first-phase insulin secretion or (log) disposition index were associated with 1.5 mmol/mol lower HbA1c levels. HbA1c levels were not associated with peripheral or hepatic insulin sensitivity. Adjustment for age, sex, BMI and smoking did not change the results (Fig. 1).
Discussion
Impaired insulin secretion and insulin resistance are the major pathophysiological mechanisms leading to type 2 diabetes [16]. It has previously been demonstrated that individuals with i-IFG have a profound defect in first-phase insulin release and abnormal EGP, whereas individuals with i-IGT are mainly characterised by insulin resistance in peripheral tissues and impaired 2nd phase insulin release [4]. Until now, it has remained largely unknown which pathophysiological disturbances in glucose metabolism non-diabetic individuals identified by HbA1c exhibit. By use of gold-standard measures for assessing insulin sensitivity and insulin release, we found that HbA1c in the normal and pre-diabetic range was associated with elevated FPG levels and lower first-phase insulin release (even after taking insulin sensitivity into account), but not with 2hPG and insulin sensitivity.
In general, the overlap between HbA1c, FPG and 2hPG as diagnostic tests is poor [17]. In 2003, Monnier et al. suggested that postprandial glucose concentrations contribute more than FPG to HbA1c in the lower HbA1c range in individuals with type 2 diabetes [18]. This hypothesis has since been debunked with evidence to the converse [19, 20]. Evidence regarding the relative contributions of FPG versus postprandial glucose to HbA1c in individuals without diabetes is scarce [20]. The present study suggests that FPG, not 2hPG (reflecting postprandial glucose), is more accurately reflected in HbA1c in the lower range, and, accordingly is associated with some of the physiological features that drive FPG. This is supported by our findings that insulin secretion, rather than insulin sensitivity, is more closely related to HbA1c in the normal and pre-diabetic range.
Most genetic variants related to type 2 diabetes and pre-diabetes are associated with reduced beta-cell function and increased FPG levels and not with insulin resistance and elevated 2hPG levels [4]. This could suggest that early beta-cell failure, and concomitant rise in HbA1c, is more related to genetic influence than to sedentary behaviour, overeating and weight gain. However, in addition to genetics, smoking has shown to be partly responsible for early beta-cell dysfunction and concomitant increased FPG and HbA1c levels as suggested by both animal and human studies [21,22,23]. Our finding of a relationship of HbA1c with smoking supports this notion.
Current evidence does not support a strong relationship between HbA1c and insulin sensitivity, but variation exists depending on the severity of glycaemic disturbances, the ethnicity of the study population, as well as the methods used to assess insulin sensitivity and insulin secretion [24,25,26,27]. The lack of association between HbA1c and insulin sensitivity in this and other studies is to some extent in alignment with a recent analysis of the A1c-Derived Average Glucose study, suggesting that non-glycaemic factors, such as age, sex, BMI and ethnicity, account for more than half of the explained variance in HbA1c among healthy, non-diabetic individuals [20]. In support of this, a large study in Finnish men without type 2 diabetes showed that insulin sensitivity and disposition index estimated from OGTTs explained only <2% of the variance in HbA1c in non-diabetic individuals [28]. Taken together, non-glycaemic factors seem to play a predominant role for HbA1c levels in the normal and lower pre-diabetic HbA1c range, potentially indicating that strategies for early diabetes prevention may need to account for e.g., ethnicity and/or genetics.
A major strength of this study was the detailed assessment of insulin sensitivity and insulin release using gold-standard measures. Other studies have used surrogate markers calculated from fasting samples or during an OGTT, which may explain some of the differences between our findings and findings from other studies. Because of the detailed measures, the study population was relatively small, which may limit the generalisability of our findings to other populations. The relatively small sample size also challenges nonsignificant findings, which should therefore be interpreted with caution. Another limitation was that participants for this study were recruited on the basis of their OGTT values (NGT, i-IFG or i-IGT) and not HbA1c. This resulted in a relatively narrow range of HbA1c levels, so extrapolation of our findings to populations with HbA1c levels above 45 mmol/mol is not possible.
In conclusion, findings from the current study highlight insulin secretion, rather than insulin resistance, as the major glycaemic feature contributing to HbA1c levels in the normal and pre-diabetic range. The underlying pathophysiology is likely relevant to strategies for diabetes prevention [29]. For instance, there is strong evidence that diabetes can be prevented in insulin-resistant individuals with IGT [30], whereas the evidence is less clear in individuals with IFG [31] and HbA1c-defined pre-diabetes who mainly seem to suffer from a defective first-phase insulin release. Defective beta-cell function is not easily restored by drug therapy aimed at providing beta-cell rest [32, 33]. Therefore, in contrast to prevention strategies in people with IGT who have severe insulin resistance [9], prevention strategies for high-risk individuals identified by HbA1c are not straightforward. More research in how to improve the health of beta cells either directly or indirectly is needed to optimise early prevention of diabetes in people identified with high risk by HbA1c.
References
S. Ligthart, T.T. van Herpt, M.J. Leening, M. Kavousi, A. Hofman, B.H. Stricker, M. van Hoek, E.J. Sijbrands, O.H. Franco, A. Dehghan, Lifetime risk of developing impaired glucose metabolism and eventual progression from prediabetes to type 2 diabetes: a prospective cohort study. Lancet Diabetes Endocrinol. 4(1), 44–51 (2016)
E.S. Ford, G. Zhao, C. Li, Pre-diabetes and the risk for cardiovascular disease: a systematic review of the evidence. J. Am. Coll. Cardiol. 55(13), 1310–1317 (2010)
J.M. Mooy, P.A. Grootenhuis, H. de Vries, P.J. Kostense, C. Popp-Snijders, L.M. Bouter, R.J. Heine, Intra-individual variation of glucose, specific insulin and proinsulin concentrations measured by two oral glucose tolerance tests in a general Caucasian population: the Hoorn Study. Diabetologia 39(3), 298–305 (1996)
K. Færch, K. Borch-Johnsen, J.J. Holst, A. Vaag, Pathophysiology and aetiology of impaired fasting glycaemia and impaired glucose tolerance: does it matter for prevention and treatment of type 2 diabetes? Diabetologia 52(9), 1714–1723 (2009)
American Diabetes Association, Standards of medical care in diabetes—2010. Diabetes Care 33(Suppl 1), S11–S61 (2010)
The International Expert Committee, International Expert Committee Report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 32(7), 1327–1334 (2009)
I.M. Stratton, A.I. Adler, H.A. Neil, D.R. Matthews, S.E. Manley, C.A. Cull, D. Hadden, R.C. Turner, R.R. Holman, Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321, 405–412 (2000)
T. Jørgensen, K. Borch-Johnsen, T.F. Thomsen, H. Ibsen, C. Glümer, P. Charlotta, A randomized non-pharmacological intervention study for prevention of ischaemic heart disease: baseline results Inter99 (1). Eur. J. Cardiovasc. Prev. Rehab. 10(5), 377–386 (2003)
K. Færch, A. Vaag, J. Holst, C. Glümer, O. Pedersen, K. Borch-Johnsen, Impaired fasting glycaemia vs impaired glucose tolerance: similar impairment of pancreatic alpha and beta cell function but differential roles of incretin hormones and insulin action. Diabetologia 51(5), 853–861 (2008)
R.A. DeFronzo, J.D. Tobin, R. Andres, Glucose clamp tecnique: a method for quantifying insulin secretion and resistance, Am. J. Physiol. 237(3), E214–E223 (1979)
K. Færch, C. Brøns, A.C. Alibegovic, A. Vaag, The disposition index: adjustment for peripheral vs. hepatic insulin sensitivity? J. Physiol. 588(5), 759–764 (2010)
R. Steele, Influences of glucose loading and of injected insulin on hepatic glucose output. Ann. N. Y. Acad. Sci. 82, 420–430 (1959)
M.A. Abdul-Ghani, M. Matsuda, B. Balas, R.A. DeFronzo, Muscle and liver insulin resistance indexes derived from the oral glucose tolerance test. Diabetes Care 30(1), 89–94 (2007)
M.J. Christopher, C. Rantzau, G.M. Ward, F.P. Alford, Insulinopenia and hyperglycemia influence the in vivo partitioning of GE and SI. Am. J. Physiol. 268(3 Pt 1), E410–E421 (1995)
O. Hother-Nielsen, H. Beck-Nielsen, On the determination of basal glucose production rate in patients with type 2 (non-insulin-dependent) diabetes mellitus using primed-continuous 3-3H-glucose infusion. Diabetologia 33(10), 603–610 (1990)
R.A. DeFronzo, Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 58(4), 773–795 (2009)
E. Barry, S. Roberts, J. Oke, S. Vijayaraghavan, R. Normansell, T. Greenhalgh, Efficacy and effectiveness of screen and treat policies in prevention of type 2 diabetes: systematic review and meta-analysis of screening tests and interventions, BMJ 356, i6538 (2017)
L. Monnier, H. Lapinski, C. Colette, Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA1c. Diabetes Care 26(3), 881–885 (2003)
M. Riddle, G. Umpierrez, A. DiGenio, R. Zhou, J. Rosenstock, Contributions of basal and postprandial hyperglycemia over a wide range of A1C levels before and after treatment intensification in type 2 diabetes. Diabetes Care 34(12), 2508–2514 (2011)
K. Færch, M. Alssema, D.J. Mela, R. Borg, D. Vistisen, Relative contributions of preprandial and postprandial glucose exposures, glycemic variability, and non-glycemic factors to HbA1c in individuals with and without diabetes. Nutr. Diabetes 8(1), 38 (2018)
C. Chen, Y.Q. Tu, P. Yang, Q.L. Yu, S. Zhang, F. Xiong, C.Y. Wang, Assessing the impact of cigarette smoking on beta-cell function and risk for type 2 diabetes in a non-diabetic Chinese cohort. Am. J. Transl. Res. 10(7), 2164–2174 (2018)
T. Li, L. Ni, Z. Zhao, X. Liu, Z. Lai, X. Di, Z. Xie, X. Song, X. Wang, R. Zhang, C. Liu, Melatonin attenuates smoking-induced hyperglycemia via preserving insulin secretion and hepatic glycogen synthesis in rats. J. Pineal Res. 64(4), e12475 (2018)
K. Færch, A. Vaag, D.R. Witte, T. Jørgensen, O. Pedersen, K. Borch-Johnsen, Predictors of future fasting and 2-hour post-OGTT plasma glucose levels in middle-aged men and women—the Inter99 study. Diabet. Med. 26(4), 377–383 (2009)
A. Borai, C. Livingstone, F. Abdelaal, A. Bawazeer, V. Keti, G. Ferns, The relationship between glycosylated haemoglobin (HbA1c) and measures of insulin resistance across a range of glucose tolerance. Scand. J. Clin. Lab. Investig. 71(2), 168–172 (2011)
Y. Heianza, Y. Arase, K. Fujihara, H. Tsuji, K. Saito, S.D. Hsieh, S. Kodama, H. Shimano, N. Yamada, S. Hara, H. Sone, High normal HbA(1c) levels were associated with impaired insulin secretion without escalating insulin resistance in Japanese individuals: the Toranomon Hospital Health Management Center Study 8 (TOPICS 8). Diabet. Med. J. Br. Diabet. Assoc. 29(10), 1285–1290 (2012)
M. Kanat, D. Winnier, L. Norton, N. Arar, C. Jenkinson, R.A. DeFronzo, M.A. Abdul-Ghani, The relationship between beta-cell function and glycated hemoglobin: results from the Veterans Administration Genetic Epidemiology Study. Diabetes Care 34(4), 1006–1010 (2011)
K. Færch, N. Borup-Johansen, D.R. Witte, T. Lauritzen, M.E. Jørgensen, D. Vistisen, Relationship between insulin resistance and beta cell dysfunction in subphenotypes of pre-diabetes and type 2 diabetes. J. Clin. Endocrinol. Metab. 100(2), 707–716 (2015)
M. Fizelova, A. Stancáková, C. Lorenzo, S.M. Haffner, H. Cederberg, J. Kuusisto, M. Laakso, Glycated hemoglobin levels are mostly dependent on nonglycemic parameters in 9398 Finnish men without diabetes. J. Clin. Endocrinol. Metab. 100(5), 1989–1996 (2015)
K. Færch, A. Hulman, T.P. Solomon, Heterogeneity of pre-diabetes and type 2 diabetes: implications for prediction, prevention and treatment responsiveness. Curr. Diab Rev. 12(1), 30–41 (2015)
W.C. Knowler, E. Barrett-Connor, S.E. Fowler, R.F. Hamman, J.M. Lachin, E.A. Walker, D.M. Nathan, P.P.R.G. Diabetes, Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med 346(6), 393–403 (2002)
T. Saito, M. Watanabe, J. Nishida, T. Izumi, M. Omura, T. Takagi, R. Fukunaga, Y. Bandai, N. Tajima, Y. Nakamura, M. Ito, Lifestyle modification and prevention of type 2 diabetes in overweight Japanese with impaired fasting glucose levels: a randomized controlled trial. Arch. Intern. Med. 171(15), 1352–1360 (2011)
RISE Consortium, Impact of insulin and metformin versus metformin alone on beta-cell function in youth with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care 41(8), 1717–1725 (2018)
RISE Consortium, Lack of durable improvements in beta-cell function following withdrawal of pharmacological interventions in adults with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care 42(9), 1742–1751 (2019)
Acknowledgements
The authors thank the laboratory technicians and all the participants. The experimental study was supported by the Danish Ministry of Science, Technology and Innovation, the Danish Diabetes Association, the Novo Nordisk Foundation and the Foundation of Gerda and Aage Haensch.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
L.B. has received scholarship funding from Innovation Fund Denmark, the Novo Nordisk Foundation and the University of Copenhagen. K.F. is supported by the Novo Nordisk Foundation (NNF14OC0009875). The funders had no influence on the manuscript preparation or the decision to publish. The other authors declare no conflict of interest.
Ethical approval
The protocol was in accordance with the Helsinki declaration and approved by the local ethical committee.
Informed consent
All participants provided written informed consent before taking part in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bruhn, L., Vistisen, D., Vainø, C.T.R. et al. Physiological factors contributing to HbA1c in the normal and pre-diabetic range: a cross-sectional analysis. Endocrine 68, 306–311 (2020). https://doi.org/10.1007/s12020-020-02234-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02234-3