Abstract
Purpose
To evaluate the impact of pharmacological treatment in osteoporosis patients with recent fracture and to assess the incidence of subsequent fracture and all-cause mortality.
Methods
This observational retrospective study was based on data from administrative databases of five Italian Local Health Units. Osteoporosis patients aged ≥ 50 years with hospitalization for vertebral or hip fracture occurring between 01/01/2011 and 31/12/2015 were included. Treatment adherence was calculated using the medication possession ratio. Multivariable proportional hazard Cox model was used to identify factors associated with time to re-fracture and all-cause mortality.
Results
A cohort of 3475 patients were included and 41.5% of them did not receive any specific anti-fracture treatment. Among treated patients (N = 2032), the majority (83.6%) received calcium/vitamin D supplementation. Over a mean follow-up of 3 years, the risk of subsequent fractures was 44.4% lower in treated patients compared to untreated ones (HR = 0.556, 95% CI = 0.420–0.735, p < 0.001) and 64.4% lower in those receiving calcium/vitamin D supplementation compared to osteoporosis treatment only (HR = 0.356, 95% CI = 0.237-0.533, p < 0.001). The risk of re-fracture was 77.2% lower in treated patients who were adherent to medication (HR = 0.228, 95% CI = 0.139–0.376, p < 0.001). Treated patients had 64% lower mortality risk over the follow-up compared to untreated ones (HR = 0.360, 95% CI = 0.310–0.418, p < 0.001).
Conclusions
A consistent proportion of osteoporosis patients did not receive specific treatment after a fracture, showing poor adherence to national guidelines on osteoporosis treatment. Osteoporosis drug treatment, and to a greater extent in combination with calcium/vitamin D, and adherence were correlated with lower risk of both re-fracture and all-cause mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a chronic degenerative disease characterized by a decrease in bone mineral density and an alteration in the skeletal micro-architecture, which leads to an increased risk of developing fragility fractures [1]. It is estimated that 200 million women worldwide suffer from osteoporosis [2] and this condition is mainly observed in postmenopausal women. Fragility fractures due to osteoporosis account for 9 million of the total fractures registered annually worldwide and have important consequences in terms of mortality and disability, with high health and social costs [2, 3]. The limitation in ambulation resulting from osteoporotic fractures accompanies chronic pain, loss of independence, and decreased quality of life [3]. In Italy, approximately 4 million postmenopausal women have osteoporosis [4]. These numbers are constantly growing, particularly in relation to the increase in life expectancy and an increment of 14% in the number of Italian postmenopausal osteoporotic women has been estimated between 2010 and 2020 [5].
Osteoporotic treatment has largely been shown to improve the health status of patients by reducing the risk of both vertebral and non-vertebral fractures [6, 7]. Despite this, only a small proportion of osteoporotic patients are currently treated for fracture prevention [8, 9]. In addition to the lack of treatment, poor adherence to osteoporotic treatment in clinical practice has been repeatedly reported. A number of studies have demonstrated that less than half of osteoporotic patients were adherent to the treatment prescribed [10,11,12] and a large proportion of them discontinued treatment after 30 days [12]. Poor adherence to osteoporosis therapy could be partly explained by its long-term nature and the delayed perception of its benefit by the patient [13]. Nevertheless, the risk of subsequent fracture is higher in non-adherent osteoporotic patients [8] and this is of considerable interest considering that patients with previous fragility fracture are at a higher risk of developing a subsequent fracture compared to those without [14]. A recent study evaluated medication use and the risk of subsequent fractures in postmenopausal women with osteoporosis and previous fragility fractures [8]. A large proportion of these patients were untreated: almost three out of four patients were not receiving treatment with osteoporosis medication and of those taking a drug, almost one-fourth discontinued the therapy over the 1-year follow-up period. Results from this study also identified the previous use of osteoporotic treatment as a predictor of greater use of these drugs after fracture [8].
An essential role in the treatment of osteoporosis is also played by calcium and vitamin D. Firstly, in virtually all clinical trials carried out to demonstrate the anti-fracture effects of osteoporotic medication, calcium, and vitamin D were also associated [15,16,17,18,19]. Secondly, vitamin D depletion has been found to increase the risk of osteoporosis fractures [20, 21] and reduce the protection against fractures provided by several drugs widely used for the treatment of osteoporotic patients in clinical practice [22, 23]. For these reasons, vitamin D supplementation is also recommended by the Italian Medicine Agency for patients at risk of fragility fracture or subsequent fracture initiating osteoporotic medication [24].
On this basis, we focused on a large database of osteoporotic patients aged 50 years or over with previous fracture due to osteoporosis, with the aim to analyze the pharmacoutilization profile of osteoporotic drugs with and without calcium/vitamin D supplements, and to assess the incidence of subsequent fractures and all-cause mortality.
Methods
Data source
In the present observational retrospective study, data were extracted from the administrative databases (DB) of five Italian Local Health Units (LHUs), geographically distributed in the National territory (Napoli 3 Sud, Pescara, Udine, Verona, Frosinone) with an overall health-assisted population of 3.3 million (approximately 5% of the National population). These administrative data comprise a number of DB in which information for each health-assisted subject are routinely collected; for this study, the following databases were assessed: Beneficiary DB (data on patients’ characteristics), Hospitalization DB (including primary and secondary diagnoses at hospital discharge), Pharmaceuticals DB (data on prescription of drugs reimbursed by the Italian National Health System, including the name of the drug, ATC code, dispensing date) and Payment exemption DB (including disease exemption codes). Each patient was identified in the DBs by an anonymous code, which permitted electronic linkage between them. Data were extracted by the staff of the LHUs and their DB were rendered anonymous in full compliance with the Italian code of protection of personal data (Legislative Decree 196/03, http://www.camera.it/parlam/leggi/deleghe/03196dl.htm). No identifiers related to patients were made available to the researchers involved in the present study. All results of the analyses were produced as aggregated summaries, which are not possible to assign (either directly or indirectly) to individual patients. Informed consent was not required for using encrypted retrospective information. According to Italian law (Guideline for the classification and conduction of the observational studies on medicines, Italian Medicines Agency, 2010), the local ethics committee of each LHU involved were notified of the undertaking of this study.
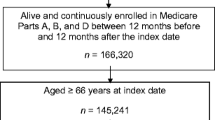
Cohort definition
All patients aged ≥ 50 years with osteoporosis and with hospitalization for vertebral or hip fracture occurring between 01/01/2011 and 31/12/2015 (inclusion period) were included. The following fractures, in primary discharge diagnosis field, were identified for inclusion: vertebral fractures, with and without spinal cord injury (ICD-9-CM codes 805 and 806) and femur fractures (ICD-9-CM code 820). In order to exclude patients with a hospital readmission for control visits after fracture, only subjects discharged for femur fractures associated with a concomitant surgical procedure (ICD-9-CM codes 79.00, 79.05, 79.10, 79.15, 79.20, 79.25, 79.30, 79.35, 79.40, 79.45, 79.50, 79.55; 81.51, 81.52) were included. All included patients had at least one hospitalization discharge diagnosis of osteoporosis (ICD-9-CM code 733.0) during the inclusion period. The following osteoporosis drugs were included in the analysis: bisphosphonates (ATC M05BA, excluding M05BA08) and their combinations with vitamin D (ATC M05BB03), other drugs affecting bone structure and mineralization (ATC M05BX), teriparatide and parathyroid hormones (H05AA), calcitonin (H05BA), selective estrogen receptor modulators (G03XC). For calcium and vitamin D we considered the following ATC codes: A12AA, A12AX, A11CC (excluding A11CC03 and A11CC04).
According to international guidelines on osteoporosis treatment, we defined patients as “treated” if they were taking anti-fracture drugs alone or in combination with calcium and vitamin D and “untreated” as those not taking anti-fracture drugs nor calcium or vitamin D. Index date was defined as the time a patient experienced a fracture. Patients who had a fracture in the year prior to the index date were excluded. Patients with renal diseases and malignancies were also excluded from the study, after their identification by the presence of the ICD-9-CM codes 584-585 or exemption code 023 (renal diseases) or ICD-9-CM codes 140-208 or exemption code 048 (malignancies) during the 2-year period preceding the index date. After inclusion, patients were followed-up for at least 1 year, from the index date to 31/12/2016.
Baseline characteristics
During the 1-year-period prior to the index date, patients were characterized by collecting their demographic data (age and gender), comorbidities and medication use. Comorbidities were identified by discharge diagnosis codes (both primary and secondary, according to ICD-9-CM) or the prescription of a specific disease-related drug (i.e., insulin for diabetes mellitus) when the diagnosis was not available. In particular, we evaluated the following comorbidities: hypertension, diabetes mellitus, dyslipidemia, ischemic heart disease, cardiac arrhythmias, heart failure, stroke, chronic obstructive pulmonary disease. Based on comorbidities, patients were also assigned the Charlson Comorbidity Index (CCI) score [25]; this index attributes a weighted score to each concomitant disease, according to the potential in influencing mortality, and is calculated by summing the resulting disease scores. CCI score was categorized as ≤ 1 and > 1. Previous medication use was only considered for those drugs with at least two reported prescriptions, in order to exclude irregular therapies. The use of the following drugs was evaluated during the 12 months before inclusion: corticosteroids for systemic use (ATC H02), platelet aggregation inhibitors (ATC B01AC), vitamin K antagonists/Xa factor inhibitors (ATC B01AA, B01AE, B01AF), analgesics (ATC N02), anticonvulsants (ATC N03), antipsychotics/anxiolytics (ATC N05A, N05B), and proton pump inhibitors (ATC A02BA).
Medication use and adherence
Both osteoporosis treatment alone or in combination with calcium/vitamin D use were analyzed.
Adherence to treatment was analyzed from the first prescription until the end of follow-up, death or hospital discharge after re-fracture (whichever came first) by medication possession ratio (MPR), calculated as the ratio between the number of days of medication supplied from filled prescriptions and the number of days the patients were followed-up. For each drug, the Defined Daily Dose was considered (Supplementary material). Patients were considered adherent for MPR ≥ 80%, whereas they were considered partially adherent for MPR = 40–79% and non-adherent for MPR < 40%.
Outcome definitions
Incident re-fracture (vertebral, femoral, radius or ulna) in primary discharge diagnosis field and all-cause mortality were assessed during the follow-up period. For re-fracture, we considered vertebral forms with and without spinal cord injury (ICD-9-CM codes 805, 806), radius and ulna (813) and femur fractures (820) with concomitant replacement procedure (79.00, 79.05, 79.10, 79.15, 79.20, 79.25, 79.30, 79.35, 79.40, 79.45, 79.50, 79.55; 81.51, 81.52).
Statistical analysis
Continuous data were summarized by mean and standard deviation (SD) whereas categorical data were summarized as percentage of patients. To identify which factors were correlated with time to all-cause mortality or to incident fractures, a multivariable proportional hazard Cox model was assessed; covariates included age, gender, comorbidities, concomitant medications, type and adherence to osteoporotic treatment. Schoenfeld residual analysis was performed to verify the proportional hazard assumption. Kaplan–Meier curves were also reported and compared using the log-rank test. p-values<0.05 were considered statistically significant. All statistical analyses were performed using STATA SE (StataCorp LP, College Station, TX, USA), version 12.0. Data management was carried out using Microsoft SQL Server 2012.
Results
Patient characteristics
Baseline clinical characteristics of the study population are presented in Table 1. A cohort of 3475 patients aged ≥ 50 years with osteoporosis and fractures was selected, with a mean follow-up duration of 2.8 ± 1.6 years. In all, 41.5% did not receive any specific anti-fracture treatment, whereas the majority of patients (58.5%) were treated with osteoporosis-related drugs. Compared to the treated cohort, untreated patients were older (83.6 ± 8.7 vs. 78.2 ± 8.7, p < 0.001) with slightly higher prevalence of comorbid diseases such as hypertension (75.1% vs. 71%, p = 0.008), diabetes (18.4% vs. 13.4%, p < 0.001) and cardiovascular diseases. Furthermore, untreated patients were less likely to have had osteoporosis treatment prior to fragility fracture (36.8% vs. 70.4%, p < 0.001).
Patient treatment and adherence
Among treated patients, 83.6% received a combination of osteoporosis drug plus calcium/vitamin D supplements, whereas 16.4% received osteoporosis drugs only (Table 2); moreover, the vast majority (83.5%) of patients receiving calcium and vitamin D supplements were receiving vitamin D. Women represented the majority of patients in both groups of treated subjects and almost 95% of those were also taking calcium/vitamin D supplements. Among the small proportion of male patients, a significant difference between the proportion receiving osteoporosis drugs compared to those receiving calcium and vitamin D supplements was observed (8.4% vs. 5.4%, p = 0.034). Patients combining anti-fracture drugs and calcium/vitamin D were more frequently on treatment with corticosteroids (18% vs. 12%, p = 0.008) and analgesics (16.4% vs. 12%, p = 0.043), whereas they were less frequently exposed to vitamin K antagonists/Xa factor inhibitors (5.9% vs. 9%, p = 0.033).
Adherence to treatment was analyzed in the treated cohort during follow-up (Fig. 1). Half of patients receiving osteoporosis drugs only were non-adherent (MPR < 40%), with this proportion being lower (31.9%) in the combination group (p < 0.001). The percentage of adherent patients (MPR ≥ 80%) was higher in those receiving calcium/vitamin D supplementation in addition to osteoporosis drug compared to osteoporosis drug only-treated subjects (48.0% vs. 29.7% respectively, p < 0.001).
Effect of calcium/vitamin D supplementation on re-fracture
During the follow-up period, 127 patients (6.1%) in the treated cohort and 108 (7.5%) in the untreated cohort were hospitalized for an incident re-fracture. The incidence rate/1000-person years was 41.2 in the untreated cohort, 48.8 in the osteoporosis drug only group and 15.1 in the group combining also calcium/vitamin D supplementation. Among the total study population with a re-fracture event, in 60.6% of cases a femur fracture was registered, with vertebral fractures and radius/ulna representing 25.2% and 14.2% of cases, respectively. During the study period, Kaplan–Meier analysis showed an increased probability of re-fracture in the untreated group compared to the treated group (Fig. 2a) and an increased probability of re-fracture in the osteoporosis drug only group compared to patients also combining calcium/vitamin D (Fig. 2b). The complete proportional hazard Cox models for time to re-fracture are presented in Table 3A, B. Patients receiving osteoporosis-related drugs after a fracture had 44.4% lower risk of developing a subsequent fracture compared to untreated patients (HR = 0.556, 95% CI = 0.420–0.735, p < 0.001); moreover, among treated patients, calcium/vitamin D supplement in addition to osteoporosis drug after a fracture was associated with a 64.4% lower risk of developing a subsequent fracture compared to the group receiving osteoporosis drug only (HR = 0.356, 95% CI = 0.237–0.533, p < 0.001). Optimal adherence to osteoporosis medication (osteoporosis drugs with or without calcium/vitamin D supplement) was associated with a 77.2% lower risk of subsequent fractures (HR = 0.228, 95% CI = 0.139–0.376, p < 0.001). Patients with cardiac arrhythmias had a threefold higher risk of developing a subsequent re-fracture during follow-up (HR = 2.657, 95% CI = 1.563–4.518, p < 0.001) and the risk in patients treated with antiplatelet drugs was two-fold higher (HR = 1.631, 95% CI = 1.080–2.463, p = 0.020). Interestingly, patients with dyslipidemia were at a significantly lower risk of new incident fractures (Table 3A).
KaplanMeier survival curves showing incidence of re-fracture events during follow-up among osteoporosis patients with a fracture. a Patients treated vs. not treated with osteoporosis drugs; b Patients treated with osteoporosis drug only vs. treated with osteoporosis drug with calcium/vitamin D supplement
Effect of calcium/vitamin D supplementation on mortality
All-cause mortality was also analyzed during the follow-up period. In all, 41.5% (N = 599) of untreated patients and 15.5% (N = 314) of treated patients died, 91 (27.3%) of the osteoporosis drug only-treated patients and 233 (13.7%) in the group of osteoporosis drug combined with calcium/vitamin D supplement. The incidence rate/1000-person years was 209.3 in the untreated group and 46.9 in the treated group (101.7 in the osteoporosis drug only group and 38.9 in the group with calcium/vitamin D supplement). Figure 3a presents the Kaplan–Meier analysis on the incidence of all-cause mortality in subjects treated with osteoporosis drug compared to untreated subjects. Patients receiving anti-fractures treatment had a 64% lower risk of death over the study period compared to untreated treated patients (HR = 0.360, 95% CI = 0.310-0.418, p < 0.001, Table 4A). The Kaplan–Meier analysis on the incidence of all-cause mortality among subjects treated with osteoporosis drug only compared with the combination group is presented in Fig. 3b. As shown, the latter was associated with a twofold lower risk of death over the study period (p < 0.001, Table 4B).
KaplanMeier survival curves showing incidence of all-cause mortality during follow-up among osteoporosis patients with a fracture. a Patients treated vs. not treated with osteoporosis drugs; b Patients treated with osteoporosis drug only vs. treated with osteoporosis drug with calcium/vitamin D supplement
Discussion
In the present investigation, a cohort of patients aged 50 years and older with osteoporosis and a fracture were retrospectively analyzed to assess their baseline characteristics, treatment prescription and adherence to treatment in relation to new incident fractures and all-cause mortality, over a mean follow-up period of 3 years. Corroborating previous reports [10, 12], the majority of our cohort was represented by elderly women. This confirms that the issue of fragility fracture incidence is widely underestimated in men, even when they are at very high fracture risk (i.e., after a previous osteoporotic fracture).
Of the 3475 fractured patients we included, two out of five were not receiving osteoporosis medication. This is in line with other retrospective studies, carried out on patients with prevalent osteoporotic fractures, then followed to assess treatment prescription attitude and effects [8, 9]. From our data, it is impossible to address the question if untreated patients had clinical characteristics that convinced their referral physicians not to treat them for the prevention of further fractures in spite of their very high risk of incident events [10, 19, 26]. However, this does not seem to be the case. Untreated patients were more likely to have comorbid conditions but they did not differ from treated according to the Charlson Comorbidity Index, a score which may be predictive of future mortality [25]. Rather, the absence of a drug prescription in these patients may reflect the well-known underestimation of the risk of fracture recurrence and its consequences in the elderly [8, 9]. In our study, this seems to be also confirmed by the lower percentage of osteoporosis drug prescription before the index date in patients who then remained untreated even after the first fracture.
The vast majority (83.6%) of patients receiving a treatment for the prevention of incident fracture were also taking the supplementation of calcium/vitamin D. This result is consistent with the Italian Medicines Agency guideline for the treatment of osteoporosis patients at risk of fragility fractures or subsequent fractures [24], in which supplementation with calcium/vitamin D is recommended when initiating treatment with drugs for osteoporosis. This recommendation is in line with the demonstration that in virtually all randomized clinical trials carried out to demonstrate the anti-fracture effects of osteoporosis medications, calcium, and vitamin D were also associated [15,16,17,18]. The importance of prescribing vitamin D supplements together with anti-fracture drugs has also been highlighted in clinical practice [20, 21]. Indeed, in postmenopausal women treated with osteoporosis drugs in association with vitamin D supplements, a larger increase in bone density and a more pronounced decrease in fracture risk compared to patients taking osteoporosis drug only was observed [22].
In the present study, adherence to osteoporosis drugs was generally poor. This is not surprising and confirms previous reports [10,11,12, 27]. Interestingly, the percentage of patients with optimal adherence (MPR ≥ 80%) was higher in subjects associating calcium/vitamin D supplements with osteoporosis medication compared to those using osteoporosis drugs only. We cannot provide a clear explanation for this. However, patients combining anti-fracture treatment with calcium/vitamin D showed a more frequent use of corticosteroids. The elevation in fracture risk associated with glucocorticoid use is well established [28,29,30]. Glucocorticoid therapy is known to decrease bone formation, due to a number of effects on both osteoblasts and osteocytes and on the modulation of GH secretion [30]. These effects lead to a consequent increased risk of hip and vertebral fractures, and this risk is even higher when glucocorticoid dose is increased [31]. Among patients undergoing glucocorticoid therapy, postmenopausal women and elderly males were identified as having the highest risk of fractures [31]. In addition to these considerations, patients treated with glucocorticoids for more than 3 months at a dose of ≥ 5 mg/day are considered at high risk of fractures by the Italian Medicines Agency and were included in the National plan for risk fracture prevention [24]. For the above-mentioned reasons, it is likely that an increased motivation towards a more proper treatment has been felt by drug users and/or prescribers. Similarly, the proportion of patients consuming analgesics was higher in the combination group. Thus, the possible presence of more significant pain may have constituted a further motivation to better adhere to the treatment assigned.
Adherence to osteoporosis treatment has already been identified as a key factor for the prevention of new fractures as well as of subsequent fractures [10] in osteoporotic patients. Our results further confirm this trend. However, our 77% lower risk of subsequent fractures in optimally adherent patients (MPR ≥ 80%) is clearly much higher than that reported in other studies, in which, in general, MPR ≥ 80% was associated with 15–40% decrease of fracture risk [10,11,12, 25]. Some possible explanations may be proposed. Firstly, we compared subjects with MPR ≥ 80% toward those with MPR < 40%, whereas in most of the studies previously published an MPR ≥ 80% was compared to an MPR < 80%. Consequently, they may also have included all patients with an MPR ranging between 79 to 40%, which still cannot be considered a very poor adherence. In line with this, our patients with an MPR of 40–79% had a lesser evident decrease in fracture risk when compared to those with an adherence of <40%. Secondly, our follow-up period was almost three-fold longer than that of most studies already published on this topic and this may have contributed to the favorable results that we observed. Finally, none of the above-mentioned studies have attempted to distinguish patients based on the presence or absence of the association with calcium/vitamin D supply and it is possible that an optimal adherence also to these supplements may positively influence fracture risk still further.
Osteoporosis drug use after a fracture among osteoporosis patients has been previously shown to reduce the risk of mortality [32, 33]. This is of considerable interest as the presence of a fracture in this population increased the risk of mortality [34]. In this study, we show that not only treatment with osteoporosis drug after a fracture reduced the risk of mortality in a cohort of osteoporosis patients, but also that mortality rates are even lower among treated patients receiving supplementation with calcium/vitamin D.
This study does have some limitations. Firstly, we analyzed the administrative databases of five Italian Local Health Units, well distributed across the Italian territory and representing a population of 3.3 million health-assisted inhabitants. However, we think that our data cannot be generalized fully to the entire National population, consisting of approximately 60 million people and further studies on a wider sample of patients are clearly needed. Secondly, medication possession ratio was calculated throughout the study period, based on data provided by an outpatient database. This means that we certainly missed drug prescription and consumption during periods in which patients were in an institutionalized care setting, such as hospital stay. However, it is unlikely that this may have affected our results. More importantly, data on the use of pharmacological treatments were retrieved from medical prescription and dispensing, so that the actual drug use was not available. Lastly, the number of vertebral fractures may have been underestimated since it was calculated only on the basis of diagnosis codes at hospital discharge [35, 36].
Conclusions
In our cohort of osteoporosis patients with a recent fracture, we observed poor adherence to national guidelines on osteoporosis treatment and a consistent proportion of patients did not receive any osteoporosis drug. However, among those treated, the vast majority only received the supplement of calcium/vitamin D. Independent of the type of treatment received, there was suboptimal adherence. However, greater adherence was observed in patients receiving both supplement and osteoporotic treatment. The group of patients receiving calcium/vitamin D supply in addition to osteoporosis drugs had a lower risk of both subsequent fracture and all-cause mortality during the 3-year follow-up; moreover, adherence to osteoporosis medication decreased the risk of subsequent fractures. The efficacy of the combination of osteoporosis drug with calcium/vitamin D supplement in the real-life setting should further stress the opportunity of increasing this treatment in patients with osteoporosis after a recent fracture.
References
Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993 Jun;94(6):646–50.
WHO Scientific Group Technical Report. Assessment of osteoporosis at the primary health care level [Internet]. 2007. Available from: https://www.sheffield.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf
O. Johnell, J.A. Kanis, An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. 17(12), 1726–1733 (2006)
Ministero della Salute-Salute della donna. Osteoporosi [Internet]. [cited 17 Jul 2018]. Available from: http://www.salute.gov.it/portale/donna/dettaglioContenutiDonna.jsp?lingua=italiano&id=4491&area=Salute%20donna&menu=patologie
P. Piscitelli, M. Brandi, H. Cawston, A. Gauthier, J.A. Kanis, J. Compston et al. Epidemiological burden of postmenopausal osteoporosis in Italy from 2010 to 2020: estimations from a disease model. Calcif. Tissue Int. 95(5), 419–427 (2014)
M.H. Murad, M.T. Drake, R.J. Mullan, K.F. Mauck, L.M. Stuart, M.A. Lane et al. Clinical review. Comparative effectiveness of drug treatments to prevent fragility fractures: a systematic review and network meta-analysis. J. Clin. Endocrinol. Metab. 97(6), 1871–1880 (2012)
N. Freemantle, C. Cooper, A. Diez-Perez, M. Gitlin, H. Radcliffe, S. Shepherd et al. Results of indirect and mixed treatment comparison of fracture efficacy for osteoporosis treatments: a meta-analysis. Osteoporos. Int. 24(1), 209–217 (2013)
A. Keshishian, N. Boytsov, R. Burge, K. Krohn, L. Lombard, X. Zhang et al. Examining the treatment gap and risk of subsequent fractures among females with a fragility fracture in the US Medicare population. Osteoporos. Int. 28(8), 2485–2494 (2017)
A.A. Yusuf, T.J. Matlon, A. Grauer, R. Barron, D. Chandler, Y. Peng, Utilization of osteoporosis medication after a fragility fracture among elderly Medicare beneficiaries. Arch. Osteoporos. 11(1), 31 (2016)
J.R. Curtis, A.O. Westfall, H. Cheng, K. Lyles, K.G. Saag, E. Delzell, Benefit of adherence with bisphosphonates depends on age and fracture type: Results from an analysis of 101,038 new bisphosphonate users. J. Bone Miner. Res. 23(9), 1435–1441 (2008)
M. Hiligsmann, V. Rabenda, H.-J. Gathon, O. Ethgen, J.-Y. Reginster, Potential clinical and economic impact of nonadherence with osteoporosis medications. Calcif. Tissue Int. 86(3), 202–210 (2010)
L. Tafaro, G. Nati, E. Leoni, R. Baldini, M.S. Cattaruzza, M. Mei et al. Adherence to anti-osteoporotic therapies: role and determinants of ‘spot therapy’. Osteoporos. Int. 24(8), 2319–2323 (2013)
M. Rossini, G. Bianchi, O. Di Munno, S. Giannini, S. Minisola, L. Sinigaglia et al. Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos. Int. 17(6), 914–921 (2006)
J.A. Kanis, C. Cooper, R. Rizzoli, B. Abrahamsen, N.M. Al-Daghri, M.L. Brandi et al. Identification and management of patients at increased risk of osteoporotic fracture: outcomes of an ESCEO expert consensus meeting. Osteoporos. Int. 28(7), 2023–2034 (2017)
D.M. Black, D.E. Thompson, D.C. Bauer, K. Ensrud, T. Musliner, M.C. Hochberg et al. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J. Clin. Endocrinol. Metab. 85(11), 4118–4124 (2000)
H.K. Genant, E. Siris, G.G. Crans, D. Desaiah, J.H. Krege, Reduction in vertebral fracture risk in teriparatide-treated postmenopausal women as assessed by spinal deformity index. Bone 37(2), 170–174 (2005)
J. Reginster, H.W. Minne, O.H. Sorensen, M. Hooper, C. Roux, M.L. Brandi et al Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos. Int. 11(1), 83–91 (2000)
S.R. Cummings, J. San Martin, M.R. McClung, E.S. Siris, R. Eastell, I.R. Reid et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N. Engl. J. Med. 361(8), 756–765 (2009)
P. Ebeling, R. Adler, G. Jones, Management of endocrine disease: Therapeutics of Vitamin D. Eur. J. Endocrinol. 5(179), R239–59 (2018)
R. Bouillon, C. Marcocci, G. Carmeliet. Skeletal and extra-skeletal actions of vitamin D: Current evidence and outstanding questions. Endocr. Rev. [Internet]. 12, 2018;12. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30321335
A. Giustina, R. Adler, N. Binkley. Controversies in vitamin D: Summary statement from an international conference. J Clin Endocrinol Metab [Internet]. 31, 2018. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30383226
S. Adami, S. Giannini, G. Bianchi, L. Sinigaglia, O. Di Munno, C.E. Fiore et al. Vitamin D status and response to treatment in post-menopausal osteoporosis. Osteoporos. Int. 20(2), 239–244 (2009)
S. Adami, E. Romagnoli, V. Carnevale, A. Scillitani, A. Giusti, M. Rossini et al. [Guidelines on prevention and treatment of vitamin D deficiency. Italian Society for Osteoporosis, Mineral Metabolism and Bone Diseases (SIOMMMS)]. Reumatismo 63(3), 129–147 (2011)
Agenzia Italiana del Farmaco (AIFA). Nota 79-Prescription of osteoporosis medications at risk of fragility fracture or subsequent fracture [Internet]. Available from: http://www.gazzettaufficiale.it/eli/id/2015/05/20/15A03762/sg
M.E. Charlson, P. Pompei, K.L. Ales, C.R. MacKenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40(5), 373–383 (1987)
C. Cipriani, J. Pepe, F. Bertoldo, G. Bianchi, F.P. Cantatore, A. Corrado et al. The epidemiology of osteoporosis in Italian postmenopausal women according to the National Bone Health Alliance (NBHA) diagnostic criteria: a multicenter cohort study. J. Endocrinol. Invest. 41(4), 431–438 (2018)
R. Halpern, L. Becker, S.U. Iqbal, L.E. Kazis, D. Macarios, E. Badamgarav, The association of adherence to osteoporosis therapies with fracture, all-cause medical costs, and all-cause hospitalizations: a retrospective claims analysis of female health plan enrollees with osteoporosis. J. Manag. Care Pharm. 17(1), 25–39 (2011)
J. Compston, Glucocorticoid-induced osteoporosis: an update. Endocrine 61(1), 7–16 (2018)
G. Mazziotti, E. Canalis, A. Giustina, Drug-induced osteoporosis: mechanisms and clinical implications. Am. J. Med. 10(123), 877–884 (2010)
G. Mazziotti, A. Formenti, R. Adler, Glucocorticoid-induced osteoporosis: pathophysiological role of GH/IGF-I and PTH/VITAMIN D axes, treatment options and guidelines. Endocrine 3(54), 603–611 (2016)
P. Vestergaard, L. Rejnmark, L. Mosekilde, Fracture risk associated with different types of oral corticosteroids and effect of termination of corticosteroids on the risk of fractures. PubMed-Ncbi. 4(82), 249–257 (2008)
F.-M. Su, Y.-C. Chen, T.-T. Cheng, W.-C. Lin, C.-C. Lui, Is raloxifene associated with lower risk of mortality in postmenopausal women with vertebral fractures after vertebroplasty?: a hospital-based analysis. BMC Musculoskelet. Disord. 16, 209 (2015)
M.J. Bolland, A.B. Grey, G.D. Gamble, I.R. Reid, Effect of osteoporosis treatment on mortality: a meta-analysis. J. Clin. Endocrinol. Metab. 95(3), 1174–1181 (2010)
J.R. Center, T.V. Nguyen, D. Schneider, P.N. Sambrook, J.A. Eisman, Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353(9156), 878–882 (1999)
S. Frara, M. Losa, M. Doga, A.M. Formenti, P. Mortini, G. Mazziotti et al. High prevalence of radiological vertebral fractures in patients with TSH-secreting pituitary adenoma. J. Endocr. Soc. 2(9), 1089–1099 (2018)
G. Mazziotti, A.M. Formenti, S. Frara, R. Olivetti, G. Banfi, M. Memo et al. High prevalence of radiological vertebral fractures in women on thyroid-stimulating hormone-suppressive therapy for thyroid carcinoma. J. Clin. Endocrinol. Metab. 103(3), 956–964 (2018)
Acknowledgements
We would like to thank all participants who took part in this study.
on the behalf of the Study group:
A. Vercellone5 and E. Nava5, F. Ferrante6, C. Bianchi6, S. Crescenzi6, P. F. Venditti6, M. Folcatrelli6, A. Constantini7, C. Cattaruzzi8
Funding
This study was sponsored unconditionally by Abiogen Pharma S.p.A, Pisa, Italy.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Supplementary Information
Rights and permissions
About this article
Cite this article
Degli Esposti, L., Girardi, A., Saragoni, S. et al. Use of antiosteoporotic drugs and calcium/vitamin D in patients with fragility fractures: impact on re-fracture and mortality risk. Endocrine 64, 367–377 (2019). https://doi.org/10.1007/s12020-018-1824-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1824-9