Abstract
Purpose
To evaluate the reliability of intermittent intraoperative neuromonitoring (I-IONM) through recurrent laryngeal nerve (RLN) stimulation and laryngeal palpation in predicting postoperative vocal cord palsy and to examine the reliability of this technique in providing useful information in the decision to perform a staged surgery in initially planned total thyroidectomy.
Methods
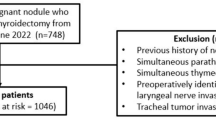
This was a retrospective cohort study of patients who underwent thyroid surgery at the ENT Department of the University of Bologna from January 2014 to June 2017. In all cases, preoperative and postoperative laryngoscopy was performed. All surgeries were conducted with I-IONM and RLN simultaneous laryngeal palpation (NSLP) to detect contraction (laryngeal twitch) of the posterior crico-arytenoid muscle. The incidence of vocal cord palsy was calculated for nerves at risk. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV), positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio were calculated with a confidence interval determined at 95% level.
Results
Seven hundred and sixteen patients were enrolled in the study. The incidence of vocal cord palsy was 3.16%. Specificity of I-IONM in predicting vocal cord paralysis was 99.1% and sensitivity was 90%. The NPV was 99.7% and PPV 78.3%. Two-stage thyroidectomy (ST) was performed in 22 cases (22/570: 3.85%). Six patients (27.3%) were false positive and 16 true positive (72.7%) at I-IONM.
Conclusion
High sensitivity and specificity values confirm the validity of I-IONM with NSLP in predicting postoperative normal vocal cord function. Our results confirm that I-IONM may safely guide an ST overall in benign thyroid diseases and in low-grade malignancies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recurrent laryngeal nerve (RLN) injury is one of the most serious complications during thyroid surgery and represents one of the leading reasons for surgical malpractice claims.
Even in experienced hands, transient RLN palsy occurs in approximately 0.4–12% of cases and permanent palsy in 5–6% of cases.
A more fearful and sometimes life-threatening situation is bilateral RLN palsy even if transient. Not only vocal cord dysfunction and physical limitation but also airway obstruction threat makes this complication, even if extremely rare (0.2–0.5%), potentially lethal for the patient.
Over the years, surgical strategy has advanced from non-visualization and avoidance of the RLN to the adoption of routine identification of the RLN, which has been shown to be associated with a lower incidence of RLN injury [1,2,3,4,5]. There is now strong evidence that routine intraoperative identification and capsular dissection are crucial in the preservation of the RLN.
However, an anatomically intact nerve identified by gross visualization does not confirm a functional nerve.
In the past few years the introduction of intraoperative neuromonitoring (IONM) has gained increasing acceptance as an adjunct for functional RLN assessment [6].
Guidelines of American Academy of Otolaryngology Head and Neck Surgery suggest IONM adoption in revision surgery, in the setting of pre-existing RLN paralysis, and in bilateral thyroid procedures to prevent two-sided vocal cord palsy [7]. Nevertheless, the debate of whether the use of IONM can lead to modify the surgical strategy during a planned total thyroidectomy still exists [8,9,10].
Some authors have suggested that the electromyographic (EMG) signal may guide reliably the decision to stage surgery when a loss of RLN signal on initial side is detected [11,12,13,14], while other authors argue on IONM low accuracy in predicting RLN palsy [15, 16].
Other studies have shown that intermittent RLN stimulation with simultaneous posterior crico-arytenoid (PCA) palpation is a safe and reliable intraoperative method of RLN monitoring, having a high correlation with evoked laryngeal EMG activity [17, 18].
The aim of this study was firstly to report our experience about reliability of I-IONM, through RLN stimulation and laryngeal palpation (NSLP), in predicting postoperative vocal cord palsy. Secondly to examine the reliability of this technique in providing useful information in the decision to perform a staged surgery in initially planned total thyroidectomy.
Materials and methods
A retrospective review of prospectively collected data from patients undergoing thyroid surgery with or without neck dissection from January 2014 to June 2017 was conducted with institutional review board approval.
In all cases preoperative and postoperative laryngoscopy was performed. Patients with pre-existing vocal cord dysfunction were excluded.
NSLP was performed by a disposable nerve stimulator (Xomed, Jacksonville, FL, USA) with the current intensity set between 0.5 and 2.0 mA, depending on the threshold of the nerve stimulation. Palpation for contraction of the PCA muscle was performed after identification of the thyroid cartilage. A finger was inserted deep to the posterior lamina and fascia overlying the vertebral column. In this way, the posterior lamina of the PCA was palpated through the wall of the hypopharynx to detect contraction (laryngeal twitch (LT)).
IONM was done according to the International Neural Monitoring Study group Guidelines [6].
Surgical interventions were performed by an experienced surgical team (>100 monitored procedures per year). In case of planned total thyroidectomy, the surgical procedure started with the dominant thyroid lobe according to malignancy and or size criteria.
The RLNs were stimulated upon initial identification before extensive dissection of the ipsilateral thyroid lobe. At the end of the resection of the thyroid lobe, the RLN was stimulated at various sites along its course, including at the thoracic inlet and more distally. The ipsilateral vagus nerve was also stimulated. In case of loss of LT and planned total thyroidectomy, the surgical procedure was always aborted. Contralateral lobectomy was planned depending on histopathologic definitive diagnosis and recovery of vocal cord function during postoperative follow-up.
Definitions
The results of IONM were retrospectively assessed. Patients outcome were categorized based on the results of IONM and postoperative laryngoscopy as follows:
-
1.
True positive (TP): Absence of LT found during IONM a postoperative nerve paralysis.
-
2.
True negative (TN): Normal LT during IONM with no postoperative nerve paralysis.
-
3.
False positive (FP): Absence of LT found during IONM with no postoperative nerve paralysis.
-
4.
False negative (FN): Normal LT signal during IONM and postoperative nerve paralysis.
We classified nerve injury into two categories according to the International Neural Monitoring Study Group: segmental injury (LOS1), which involves a clear-cut RLN segment that is lesioned and global injury (LOS2), where the entire RLN and vagus nerve were non-conductive.
RLN dysfunction lasting more than 12 months was considered permanent.
Outcomes measured
The primary outcome was to determine the incidence of LOS. The secondary outcome was to evaluate the rate of unilateral and bilateral RLN injuries, both transient and permanent.
Finally, to describe the surgical strategy in patients in which an LOS occurred on the first side of a planned total thyroidectomy and methods and timing for completion thyroidectomy.
Statistical analysis
The incidence of palsy was calculated based on the number of nerves at risk. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV), positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio were calculated with a confidence interval (CI) determined at 95% level. CIs for sensitivity and specificity were determined by the Wilson score method [19]. CIs for positive and negative likelihood ratios were calculated with the method described by Simel and colleagues [20]. The CI for the diagnostic odds ratio was calculated as described by Armitage and Berry [21].
Results
Seven hundred and sixteen patients were enrolled in the study. Five hundred and fifty-two were females (77.1%), while 164 were males (22.9%). Unilateral lobectomy was planned and performed in 146 patients (20.4%). In 570 cases (79.6%), the planned surgical procedure was a total thyroidectomy with central neck dissection in 52 (7.2%) patients and lateral neck dissection in 25 (3.5%) cases. Histopathological findings are listed in Table 1.
IONM outcomes
There were 1.264 nerves at risk (NAR). The RLN was identified in all cases. The incidence of vocal cord palsy, calculated for NAR, was 3.16% (40/1.264). No bilateral vocal cord palsy was observed.
Sensitivity and specificity of IONM with NSLP to predict postoperative RLN function are summarized in Table 2. Statistical results are listed in Table 3.
Of the 36 true-positive patients, 30 cases were defined as LOS2 and 6 cases as LOS1. Recovery of vocal cord function was detected in 25 cases of LOS2 within a mean follow-up of 12 week, while the remaining 5 cases are still under annual follow-up.
None of the LOS1 patients experienced recovery of vocal cord function after 1 year follow-up.
Surgical strategy
The clinical and I-IONM data of the staged cases are resumed in Table 4. Twenty two patients, initially planned for total thyroidectomy, were staged according to I-IONM results (22/570: 3.85%). Six of these patients (27.3%) were FP, while 16 were TP (72.7%). Thirteen (81.25%) of the TP patients experienced vocal cord function recovery within a mean of 6.1 weeks. The remaining 3 (18.75%) patients were found to have unilateral permanent vocal cord paralysis.
ST was performed in three patients with preoperative fine needle aspiration (FNA) diagnosis of PTC (T1a in two cases, T1bN0M0 in one case) [22]. ST was also performed in one patient with preoperative FNA diagnosis of atypia of undetermined significance (Bethesda System [23]).
All the four cases were found to be unifocal PTC with minimal extrathyroidal invasion in the final histopathology. (pT3N0MX)[22]. The ATA stratification risk for recurrence showed that all cases were at intermediate risk [24]. For the above reasons, the patients underwent completion thyroidectomy and radioactive iodine ablation therapy, when recovery of vocal cord function was observed.
Twelve patients affected by multinodular goiter and initially planned for total thyroidectomy were staged. In none of these cases completion thyroidectomy was performed, although final diagnosis resulted in microcarcinoma in three patients. Surgery was stopped also in three patients affected by Graves’ disease. In two cases, we decided against the completion of the operation because the patients were euthyroid and remain under endocrinological supervision. The third patient, affected by serious exophthalmos and persistent hyperthyroidism, underwent completion thyroidectomy. ST was adopted in three3 patients affected from undeterminate lesions (two atypia of undetermined significance and one follicular lesion of undetermined significance [23]). The histopathological postoperative examination showed a benign diagnosis.
Discussion
RLN IONM is gaining acceptance as an adjunct in thyroid surgery because it is the only method that provides the surgeon intraoperative information regarding nerves identification and functional integrity. Therefore, it supplements the gold standard method of visual identification with valuable information about nerves anatomical integrity and functional ability [8, 25].
A recent metanalysis reported a slightly lower rate of postoperative bilateral RLN paralysis with IONM (0.27% vs. 0.5%), but this difference was not statistically significant [26].
Because of the rarity of RLN paralysis, it is calculated that to achieve significant study power, recruitment of over 40,000 patients to each arm of randomized study focusing on thyroid cancer would be required to unveil a true effect, and over nine million patients if examining benign disease [14].
Nevertheless, many authors suggested that IONM can prevent bilateral RLN paralysis after signal loss on the initial side of resection, by guiding the decision to stage planned total thyroidectomy [11,12,13,14, 27, 28].
The results of the present study seem to confirm this notion. As demonstrated by other authors, the validity of IONM is mainly due to its high specificity and NPV [6, 8, 14, 18, 25, 29,30,31,32,33,34,35,36]. This means that when LT is detected after first lobe resection, in initially planned total thyroidectomy, the surgeon can safely approach the contralateral lobe.
The relatively low PPV of a lost IONM signal and the possibility to have FP results are widely documented in the literature [14, 16, 25, 32, 33] and the reasons are not yet completely understood. In our study, both PPV and sensitivity of IONM were higher than those reported in previous studies [14, 18, 32], while FP results were obtained in <1% of the patients. These results confirm that NSLP may be an effective tool to modify surgical strategy during thyroid surgery. Consequently, when a loss of signal occurs after resection of the first lobe in planned total thyroidectomy, we strongly advise to postpone the excision of the contralateral side. Certainly, benign disease cannot dictate completion thyroid surgery on the uninjured contralateral side in case of LOS on the first side of resection. The risk of bilateral vocal fold paralysis would be an unjustified complication related to the non-neoplastic disease [28]. In our experience, we have modified the surgical plan in 12 cases of multinodular goiter. As recommend by other authors and guidelines, it is mandatory to start surgery from the affected/prevalent side [6, 13]. At present, none of these patients experienced any clinical reasons to perform completion thyroidectomy. Moreover, in our study, we have adopted two-stage thyroidectomy also in Graves' disease (GD). One patient, TP at I-IONM, needed a completion thyroidectomy after recovery of vocal fold function for persisting uncontrollable hyperthyroidism and exophthalmos. The remaining two cases, FP at I-IONM, did not need re-operation because they were biochemically and clinically euthyroid. These results suggest that ST may be safely applied also in GD. In case of persistence or relapse of hyperthyroidism and permanent paralysis that contraindicates completion thyroidectomy, the remnant contralateral lobe, if relatively small, may be ablate by radioiodine therapy [13].
To date, there is no consensus on ST for malignant diseases. The main types of thyroid cancer not only differ regarding morphology, pathogenesis, genetics, and pathophysiology, but also concerning tumor biology, metastatic behavior, and prognosis. Knowledge of these features is the basis of the surgical concept of stage thyroidectomy even in thyroid cancer management.
In our experience, we performed two-stage thyroidectomy in three patients with preoperative FNA diagnosis of differentiated thyroid carcinoma and in one patient affected by undetermined cytological lesion that was diagnosed as papillary carcinoma at final examination. Considering that differentiated thyroid carcinomas have an acceptable prognosis despite local invasion and distant metastases and considering the high chance of an early recovery of the RLN function, staged thyroidectomy can be carried out even in case of low-grade malignant diseases [27, 28]. Moreover, in case of unifocal PTC without extrathyroidal extension, lymph node metastases and vascular invasion, patients can receive only a strict follow-up.
On the other hand, in patients with plurifocality or extracapsular invasion, re-operation and postoperative RAI are recommended. Undoubtedly the decision to perform completion thyroidectomy may be very difficult in case of permanent paralysis [34]. In these cases, radioactive iodine remnant lobe ablation can be an alternative to completion thyroidectomy [13, 37].
However, it is clear that patients must be informed preoperatively about the limitations of IONM and any potential strategy changes that may occur during the planned bilateral surgery. The possibility to stage the procedure in case of an LOS on the initially operated side must be specified in the preoperative informed consent. Patients must be informed about the possibility of staging the intervention in case of an LOS, in order to maintain patient autonomy and with emphasis on shared decision making [13, 38]. Most of our patients perfectly agree with this concept and understand the clear benefit in deciding on a two-step approach in case of an LOS on the initially operated side.
Conclusion
High sensitivity and specificity values confirm the validity of I-IONM with NSLP in predicting postoperative normal vocal cord function. Our results confirm that I-IONM can safely guide a staged thyroidectomy overall in benign diseases and in low-grade malignancies. The option of a two-stage surgery must be shared with the patients who shall be preoperatively informed about the advantages and disadvantages of IONM and on the potential surgical complications when IONM data are not considered.
References
J.P. Jeannon, A.A. Orabi, G.A. Bruch, H.A. Abdalsalm, R. Simo, Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int. Clin. Pract. 63, 624–629 (2009)
K. Dralle Hm Lorenz, A. Machens, Verdicts on malpractice claims after thyroid surgery: emerging trends and future directions. Head Neck 34, 1591–1596 (2012)
L. Rosato, N. Avenia, P. Bernante, M. De Palma, G. Gulino, P.G. Nasi et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J. Surg. 28, 271–276 (2004)
A. Bergenfelz, S. Jansson, A. Kristoffersson, Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3660 patients. Langebeck's Arch. Surg. 393, 667–673 (2008)
S.K. Snyder, T.C. Lairmore, J.C. Hendricks, J.W. Roberts, Elucidating mechanisms or recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J. Am. Coll. Surg. 206, 123–30 (2008)
G.W. Randolph, H. Dralle, International Intraoperative Monitoring Study Group, Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guidelines statement. Laryngoscope 121, S1–S16 (2011)
S.S. Chandrasekhar, G.W. Randolph, M.D. Seidman et al. American Academy of Otolaryngology Head and Neck Surgery Clinical Practice Guidelines: improving voice outcomes after thyroid surgery. Otolaryngol. Head Neck Surg. 148, S1–S37 (2013)
W.F. Chan, B.H. Lang, C.Y. Lo, The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery 140, 866–872 (2006)
T.S. Higgins, R. Gupta, A.S. Ketcham et al. Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope 121, 1009–1017 (2011)
M. Barczynski, A. Konturek, S. Chichon, Randomized clinical trial of visulalization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br. J. Surg. 96, 240–246 (2009)
T.E. Fontenot, G.W. Randolph, T.E. Setton, N. Alsaleh, E. Kandil, Does intraoperative nerve monitoring reliably aid in staging of total thyroidectomy? Laryngoscope 125, 2232–2235 (2015)
P.E. Goretzki, K. Schwartz, J. Brinkmann, D. Wirowski, B.J. Lammers, The impact of intraoperative neuromonitoring (IONM) on surgical strategy in bilateral thyroid disease: Is it worth the effort? World J. Surg. 34, 1274–1284 (2010)
G.L. Dionigi, F. Frattini, Staged thyroidectomy: time to consider intraoperative neuromonitoring as standard of care. Thyroid 23, 906–908 (2013)
H. Dralle, C. Sekulla, K. Lorenz, P. Nguyen Thanh, A. Machens, Loss of the nerve monitoring signal during bilateral thyroid surgery. Br. J. Surg. 99, 1089–1095 (2012)
M. Herman, C. Hellebart, M. Freissmuth, Neuromoniotring in thyroid surgery: prospective evaluation of intraoperative electrophysiological responsens for the prediction of the recurrent laryngeal nerve injury. Ann. Surg. 240(1), 9–17 (2004)
A. Sitges-Serra, J. Fontanè, I.P. Duenas, C.S. Duque, L. Lorente, L. Trillo, Prospective study on loss of signal on the first side during neuromonitoring of the recurrent laryngeal nerve in total thyroidectomy. Br. J. Surg. 100(5), 662–666 (2013)
O. Cavicchi, U. Caliceti, I.J. Fernandez, G. Macri’, C. Di Lieto, A. Marcantoni, A. Rinaldi Ceroni, O. Piccin, The value of neurostimulation and intraoperative nerve monitoring of inferior laryngeal nerve in thyroid surgery. Otolaryngol. Head Neck Surg. 140, 866–870 (2009)
G.W. Randolph, J.B. Kobler, J. Wilkins, Recurrent laryngeal nerve identification and assesment during thyroid surgery: laryngeal palpation. World J. Surg. 28, 755–760 (2004)
R.G. Newcombe, Interval estimation for the difference between independent proportions: comparison of eleven methods. Stat. Med. 17, 873–890 (1998). Erratum in: Stat. Med. 18(10), 1293 (1999)
D.L. Simel, G.P. Samsa, D.B. Matchar, Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J. Clin. Epidemiol. 44, 763–770 (1991)
P. Armitage, G. Berry, Statistical Methods in Medical Research, 3rd edn. (Blackwell, London, 1994), p. 131
S.B. Edge, C.C. Compton, The American Joint Committee on Cancer: the 7th edition of the AJCC Cancer Staging Manual and the future of TNM. Ann. Surg. Oncol. 17(6), 1471–1474 (2010)
E.S. Cibas, S.Z. Ali, The Bethesda System for reporting thyroid cytopathology. Am. J. Clin. Pathol. 132, 658–665 (2009)
B.R. Haugher, E.K. Alexander, K. Bible, G.M. Doherty, S.J. Mandel, Y.F. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26(1), 1–133 (2015)
F.Y. Chiang, I.C. Lu, W.R. Kuo, K.W. Lee, N.C. Chang, C.W. Wu, The mechanism of recurrent laryngeal nerve injury during thyroid surgery—the application of intraoperative neuromonitoring. Surgery 143, 743–749 (2008)
J. Pardal-Refoyo, C. Ochoa-Sangrador, Bilateral recurrent laryngeal nerve injury in total thyroidectomy with or without intraoperative neuromonitoring. Systematic review and meta-analysis. Acta Otorrinolaringol. 67, 66–74 (2015)
S.M. Sadowski, P. Soardo, I. Leuchter, J.H. Robert, F. Triponez, Systematic use of recurrent laryngeal nerve neuromonitoring changes the operative strategy in planned bilateral thyroidectomy. Thyroid 3, 329–333 (2013)
M. Melin, K. Schwarz, B.J. Lammers, P.E. Goretzki, IONM-guided goiter surgery leading to two-stage thyroidectomy—indications and results. Langebeck's Arch. Surg. 398, 411–418 (2013)
H. Dralle, C. Sekulla, J. Haerting, W. Timmermann, H.J. Neumann, E. Kruse, S. Grond, H.P. Mĩhlig, C. Richter, J. Voss, O. Thomusch, H. Lippert, I. Gastinger, M. Brauckhoff, O. Gimm, Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 136(6), 1310–1322 (2004)
B. Wojtczak, K. Kaliszewski, K. Sutkowski, M. Bolanowski, M. Barczyński, A functional assessment of anatomical variants of the recurrent laryngeal nerve during thyroidectomies using neuromonitoring. Endocrine 59(1), 82–89 (2018)
C.R. Cernea, G.L. Brandao, J. Brandao, Neuromonitoring in thyroid surgery. Curr. Opin. Otolaryngol. Head Neck Surg. 20, 125–129 (2012)
G.W. Randolph, D. Kamani, Intraoperative electrophysiologic monitoring of the recurrent laryngeal nerve during thyroid and parathyroid surgery: experience with 1,381 nerves at risk. Laryngoscope 127(1), 280–286 (2017)
P.G. Calò, F. Medas, G. Conzo, F. Podda, G.L. Canu, C. Gambardella, G. Pisano, E. Erdas, A. Nicolosi, Intraoperative neuromonitoring in thyroid surgery: Is the two-staged thyroidectomy justified?. Int. J. Surg. 1, S13–S20 (2017)
H. Dralle, C. Sekulla, K. Lorenz et al. German IONM Study Group. Intraoperative monitoring of the recurrent laringeal nerve in thyroid surgery. World J. Surg. 32, 1098–1102 (2004)
C. Tomoda, Y. Hirokawa, T. Uruno, Sensitivity and specificity of intraoperative recurrent laryngeal nerve stimulation test for predicting vocal cord palsy after thyroid surgery. World J. Surg. 30, 1230–1233 (2006)
I. Vasileiadis, T. Karatzas, G. Charitoudis, E. Karakostas, S. Tseleni-Balafouta, G. Kouraklis, Association of intraoperative neuromonitoring with reduced recurrent laryngeal nerve injury in patients undergoing total thyroidectomy. JAMA Otolaryngol. Head Neck Surg. 142(10), 994–1001 (2016)
G.W. Randolph, G.H. Daniels, Radioactive iodine lobe ablation as an alternative to completion thyroidectomy for follicular carcinoma of the thyroid. Thyroid 12, 989–996 (2002)
P. Angelos, Ethical and medicolegal issues in neuromonitoring during thyroid and parathyroid surgery: a review of the recent literature. Curr. Opin. 24, 1621 (2012)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Cavicchi, O., Burgio, L., Cioccoloni, E. et al. Intraoperative intermittent neuromonitoring of inferior laryngeal nerve and staged thyroidectomy: our experience. Endocrine 62, 560–565 (2018). https://doi.org/10.1007/s12020-018-1739-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1739-5