Abstract
The purpose of this study was to systematically review the literature for studies that have investigated possible differences in the prevalence of subclinical Cushing’s syndrome (SCS) and related clinical implications between patients with unilateral (UAI) and bilateral adrenal incidentalomas (BAI) and to meta-analyze the best evidence available. Electronic databases PubMed and EMBASE were systematically searched. Main study outcome was the prevalence of SCS in patients with UAI and BAI. Secondary outcomes were the prevalence of obesity, diabetes, glucose intolerance, hypertension, dyslipidemia, and osteoporosis in patients with UAI and BAI. Risk differences (RD) or mean differences (MD) and 95 % confidence intervals (CIs) were calculated. Meta-analysis was conducted using Review Manager (RevMan 5.3). Six studies were included in the meta-analysis involving in total 1239 patients, 968 with UAI, and 271 with BAI. Patients with UAI had lower prevalence of SCS compared with those with BAI [RD (95 % CI) −0.13 (−0.22 to −0.05), I 2 = 42 %]. The mass diameter of UAI did not differ from BAI (the size of the largest lesion) [MD (95 % CI) −0.45 (−1.09 to 0.19), I 2 = 91 %]. The prevalence of obesity [MD (95 % CI) 0.42 (−0.53 to 1.37), I 2 = 4 %], diabetes [RD (95 % CI) −0.04 (−0.11 to 0.04), I 2 = 0 %], hypertension [RD (95 % CI) 0.00 (−0.18 to 0.18), I 2 = 75 %], and dyslipidemia [RD (95 % CI) −0.02 (−0.16 to 0.13), I 2 = 50 %] did not differ between UAI and BAI. The present meta-analysis provided evidence that patients with BAI present a higher prevalence of SCS compared to patients with UAI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The term “adrenal incidentalomas” (AI) refers to clinically silent adrenal masses, which are detected incidentally during imaging procedures performed for unrelated diseases [1]. The prevalence of AI varies between 0.4 and 5.0 % in clinical series [2–5], depending on patient inclusion criteria, and is steadily increasing because of better availability and accessibility to imaging evaluation [1, 2].
The majority of AI are benign and non-functional. However, there is a percentage of hormonally active AI. The most frequent endocrine dysfunction detected in such subjects is autonomous cortisol subtle hypersecretion, not associated with typical signs and symptoms of hypercortisolism. This disorder is also known as subclinical Cushing’s syndrome (SCS) [6]. The reported prevalence for SCS in patients with AI varies between 5 and 24 % in most studies and depends on the applied diagnostic biochemical criteria [7–10].
In patients with AI, an increased prevalence of several metabolic problems has been described including glucose intolerance, diabetes, hypertension, dyslipidemia, and osteoporosis. These clinical implications have been described in patients both with non-secreting AI and SCS [1, 5–11]. However, a higher percentage has been reported for patients with SCS, and this could be potentially associated with chronic exposure to slight cortisol excess [6–8, 11, 12].
AI are most commonly unilateral (UAI). Nevertheless, bilateral AI (BAI) are reported in a substantial proportion of such patients, between 7.8 and 15 % [4–9, 11, 12]. BAI commonly appear in the form of single discrete bilateral lesions, while a minority presents as bilateral macronodular or micronodular enlargement or diffuse adrenal hyperplasia. BAI are most frequently benign and non-functional as well. There are few data, which suggest possible pathophysiologic differences between UAI and BAI [13, 14]. Recently, a small number of studies have attempted to assess the possibility of a different prevalence in SCS and adverse metabolic implications between patients with UAI and BAI. The existing data are limited and the results controversial, as three of them have detected differences, while the rest have not [15–19].
The aim of the present study was to systematically review the literature for studies that have investigated possible differences in prevalence of SCS and related clinical implications between patients with UAI and BAI and to meta-analyze the best evidence available.
Materials and methods
Search strategy
In order to identify eligible studies, the main search was conducted in two electronic databases, namely PubMed and EMBASE. We used combinations of the key-terms: “adrenal incidentalomas” OR “unilateral adrenal incidentalomas” OR “bilateral adrenal incidentalomas” AND “subclinical hypercortisolism” OR “subclinical hypercortisolemia” OR “subclinical Cushing’s syndrome” AND “diabetes” OR “glucose intolerance” OR “hypertension” OR “dyslipidemia” OR “osteoporosis.” The procedure was concluded by (i) the perusal of the reference sections of all relevant studies and (ii) a manual search of key journals and abstracts from the major annual meetings in the field of endocrinology. The main search was completed independently by three investigators (SAP, EK, FD). Any discrepancy was solved by consultation of an investigator, not involved in the initial procedure (DGG).
Selection of studies
Criteria for inclusion/exclusion of studies were established prior to the literature search. Eligible for the systematic review and meta-analysis were only studies that have assessed the possibility of a different prevalence in SCS and/or in clinical disorders between patients with UAI and BAI. Reviews, letters to the editor, and studies published in language other than English were excluded from the systematic review and meta-analysis.
Data extraction
Information from each study was extracted independently by two reviewers using a standardized data extraction form. Main study outcome was the prevalence of SCS in patients with UAI and BAI. Secondary outcomes were the prevalence of obesity, diabetes, glucose intolerance, hypertension, dyslipidemia, and osteoporosis in patients with UAI and BAI. Study general characteristics (author, year of publication, journal, country, design, type of hospital, number of patients), clinical characteristics of the patients [gender, age, body mass index (BMI), mass size of the adrenal incidentalomas], biochemical characteristics of the patients [post-dexamethasone suppression test (DST) cortisol, midnight cortisol, dehydroepiandrosterone sulfate (DHEA-S), urinary free cortisol (UFC), adrenocorticotropic hormone (ACTH) etc.], and main and secondary study outcomes were recorded (where available) and double-checked. Where appropriate, the dataset was completed through communication with the authors. Specifically, an e-mail was sent, and when no answer was received, a second one followed after a 2-week interval. Disagreement was resolved by consensus.
Risk of bias and study quality
In order to assess the quality of the included studies, the RTI Item Bank Tool for observational studies was used [20]. The assessment was performed independently by two investigators (SAP, DGG). All studies were examined with the appropriate tool questions in order to detect different types of bias, namely selection, performance, detection, attrition, and reporting bias.
Statistical analysis
Risk differences (RD) or mean differences (MD) and 95 % confidence intervals (CIs) were calculated for main outcome and secondary study outcomes for all eligible studies for the meta-analyses [21]. Qualitative descriptors of the effect sizes obtained were less than 0.3, small; 0.4–0.8, moderate; and greater than 0.8, large. Heterogeneity between the results of different studies was examined by I 2 test [22]. Meta-analysis was conducted using Review Manager (RevMan) for Mac (version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). Meta-regression was conducted using STATA/IC 13.0 for Mac (StataCorp LP, Texas, USA). The report of the study was complemented in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) group standards for reporting meta-analysis of observational studies [23].
Results
Systematic review
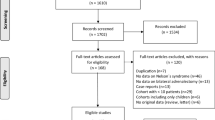
The literature search yielded 54 publications in total. After application of the inclusion/exclusion criteria, six studies were included in the systematic review. Forty of the studies were excluded already as abstracts due to irrelevant content, while other eight were assessed as full-text articles, but they did not finally provide any information about the prevalence of SCS and/or clinical implications between patients with UAI and BAI. A flow chart of this process is presented in Fig. 1. The main characteristics of the studies are presented in Table 1. The clinical characteristics of patients with UAI and BAI are presented in Table 2. The biochemical characteristics of these patients are presented in Table 3. The criteria used for the diagnosis of SCS and the prevalence of SCS in patients with UAI and BAI are presented in Table 4. The clinical implications in these patients are presented in Table 5.
The six eligible studies included in the systematic review were published between 2011 and 2014. They involved in total 1239 patients. Of these patients, 968 (78.1 %) presented with UAI, while the rest 271 (21.9 %) presented with BAI. Three of the studies originated from Greece [15, 16, 19], one from Sweden [17], one from Italy [18], and one from Turkey [24] (Table 1).
The criteria used for the diagnosis of SCS varied in the studies included. They were mostly based on post-DST high morning cortisol concentrations combined with at least one abnormal result of other hormonal measurements, such as high midnight cortisol, low morning ACTH, low-for-age DHEA-S, and high 24-h urinary free cortisol (UFC). In the study by Androulakis et al., only the post-LDDST high morning cortisol concentrations was used as criterion, but the cut-off was based on the values calculated from a control population [16]. In three of the studies, 1 mg DST was performed [17, 18, 24], while in the rest three studies LDDST was used as diagnostic tool [15, 16, 19] (Table 4).
Regarding the prevalence of SCS, the results are controversial. Three studies detected significantly higher prevalence of SCS in patients with BAI [15, 17, 19], while there was no significant difference between patients with BAI and UAI in the rest three studies [16, 18, 24] (Table 4). The mass size between UAI and BAI (the size of the largest lesion) did not differ in three studies [16, 17, 19], while it was significantly larger for BAI in the study by Vassiliadi et al. [15]. Statistically significant larger mass size in BAI was reported in the study by Morelli et al., but here the sum of the largest diameters of adrenal lesions was calculated [18] (Table 2).
The frequency of obesity did not differ between patients with BAI and UAI in the studies reported information for BMI (Table 5). Regarding other morbidities that could be considered as adverse effects of subtle cortisol hypersecretion, type 2 diabetes, IGT, and dyslipidemia did not differ between patients with BAI and UAI in any of the studies reported such information (Table 5). As far as hypertension is concerned, the study by Vassiliadi et al. reported an increased frequency of hypertension in patients with UAI [15], while the study by Vassilatou et al. reported a trend for increased frequency of hypertension in patients with BAI [19] (Table 5). Information on BMD and vertebral fractures is reported only in the study by Morelli et al., where the femoral neck BMD was lower and the prevalence of fractures was higher in patients with BAI compared to patients with UAI [18] (Table 5).
Risk of bias and study quality
According to authors’ judgment, all studies [15–19, 24] had low risk of selection and performance bias. Three of them [17, 18, 24] had unclear risk and three [15, 16, 19] low risk for detection bias. One study [24] had unclear risk, and the rest [15–19] had low risk for attrition bias. Finally, two studies [18, 24] had unclear risk and the rest [15–17, 19] low risk for reporting bias.
Meta-analysis of main and secondary outcomes
All six studies included in the meta-analysis [15–19, 24], involving in total 1239 patients, 968 with unilateral and 271 with bilateral adrenal incidentalomas. The result of the meta-analysis of the main study outcome, the prevalence of SCS in patients with UAI and BAI, is shown in Fig. 2. Patients with UAI demonstrated reduced odds ratio for SCS when compared with patients with BAI, yet with significant between-study heterogeneity [RD (95 % CI) −0.13 (−0.22 to −0.05), I 2 = 42 %].
The mass size of UAI did not differ from BAI (the size of the largest lesion), but with significant between-study heterogeneity [MD (95 % CI) −0.45 (−1.09 to 0.19), I 2 = 91 %]. The study by Morelli et al. was excluded from the meta-analysis, as they reported the sum of the largest diameters of adrenal lesions and not the size of the largest lesion (Fig. 3).
The meta-analysis of secondary outcomes, which were the prevalence of clinical implications possibly related to subtle cortisol hypersecretion, is shown in Figs. 4, 5, 6, and 7 and did not result in any differences between UAI and BAI, without heterogeneity in obesity and diabetes. Four studies reported information regarding BMI [MD (95 % CI) 0.42 (−0.53 to 1.37), I 2 = 4 %] (Fig. 4). Three studies reported information regarding the prevalence of diabetes [RD (95 % CI) −0.04 (−0.11 to 0.04), I 2 = 0 %] (Fig. 5). Two studies reported information regarding the prevalence of dyslipidemia [RD (95 % CI) −0.02 (−0.16 to 0.13), I 2 = 50 %] (Fig. 6). Three studies reported information regarding the prevalence of hypertension [RD (95 % CI) 0.00 (−0.18 to 0.18), I 2 = 75 %] (Fig. 7). Only one study reported information on BMD and prevalence of vertebral fractures, so a meta-analysis was not possible to be performed.
The meta-analysis of the biochemical characteristics of the patients with UAI and BAI are presented in Figs. 8, 9, 10, 11, and 12. Five studies reported information regarding morning cortisol concentrations post-DST, two studies after 1 mg DST [17, 18] and three studies after LDDST [15, 16, 19]. Patients with UAI demonstrated reduced SMD for morning cortisol concentrations post-DST when compared with patients with BAI, yet with significant between-study heterogeneity [MD (95 % CI) −0.73 (−1.27 to 0.19), I 2 = 55 %] (Fig. 8). Two studies reported information regarding midnight cortisol concentrations, without difference between patients with UAI and patients with BAI [MD (95 % CI) −0.52 (−1.13 to 0.10), I 2 = 0 %] (Fig. 9). Five studies reported information regarding morning ACTH concentrations. Patients with UAI demonstrated elevated SMD for morning ACTH concentrations when compared with patients with BAI, with low between-study heterogeneity [MD (95 % CI) 3.10 (1.49 to 4.71), I 2 = 24 %] (Fig. 10). Three studies reported information regarding DHEA-S, without difference between patients with UAI and patients with BAI [MD (95 % CI) 26.42 (−1.36 to 54.20), I 2 = 82 %] (Fig. 11). Four studies reported information regarding 24-h urinary free cortisol (UFC) concentrations, without difference between patients with UAI and patients with BAI [MD (95 % CI) −5.34 (−18.31 to 7.63), I 2 = 65 %] (Fig. 12).
Subgroup meta-analysis
Subgroup meta-analysis was performed regarding morning cortisol concentrations post-DST. Subgroups consisted of two studies that used 1 mg DST [17, 18] and three studies that used LDDST [15, 16, 19]. Patients with UAI did not demonstrate any differences in MD for morning cortisol concentrations post 1 mg DST when compared with patients with BAI [MD (95 % CI) −0.47 (−1.14 to 0.20), I 2 = 40 %]. Patients with UAI demonstrated marginally reduced MD for morning cortisol concentrations post-LDDST when compared with patients with BAI, yet with significant between-study heterogeneity [MD (95 % CI) −1.02 (−2.07 to 0.03), I 2 = 69 %].
Publication bias
As six studies were included in the meta-analysis, tests for funnel plot asymmetry, such as Egger’s test, were not used. Such a test can be performed only when at least ten studies are included in the meta-analysis, otherwise the power is too low to distinguish chance from real asymmetry.
Explanation of heterogeneity: sensitivity analysis
Significant between-study heterogeneity was present in the comparison of patients with UAI and BAI regarding prevalence of SCS, mass size, prevalence of dyslipidemia and hypertension, cortisol concentrations post-DST, DHEA-S concentrations, and UFC. When the study by Vassiliadi et al. [15] was excluded, I2 was reduced from 42 to 7 % for prevalence of SCS, from 91 to 0 % for mass size, from 75 to 25 % for prevalence of hypertension, and from 55 to 0 % for cortisol concentrations post-DST.
Explanation of heterogeneity: meta-regression
Meta-regression for possible predictors of primary and secondary outcomes was not performed due to the small number of studies. Furthermore, there were not enough data to perform a meta-regression for the association between prevalence of SCS and mass size.
Discussion
The aim of the present study was to systematically review the literature for studies that have investigated possible differences in the prevalence of SCS and related clinical implications between patients with UAI and BAI and to meta-analyze the best evidence available. We found that patients with BAI present a higher prevalence of SCS compared to patients with UAI, without any differences in the prevalence of obesity, diabetes, hypertension, and dyslipidemia.
Significant between-study heterogeneity was present in the comparison of patients with UAI and BAI regarding many of primary and secondary outcomes. When the study by Vassiliadi et al. [15] was excluded, the heterogeneity was significantly reduced for all parameters. Yet, the risk of bias and study quality assessment did not result in any selection, performance, detection, attrition, or reporting bias for this study [15]. Regarding dyslipidemia, only two studies reported information, and this small number could explain heterogeneity.
The possibility of a different prevalence in subtle cortisol hypersecretion between patients with BAI and UAI has been previously investigated in six studies, with controversial results. Three studies detected significantly higher prevalence of SCS in patients with BAI [15, 17, 19], while there was no significant difference between patients with BAI and UAI in the rest of the studies [16, 18, 24]. The present meta-analysis provided evidence that patients with BAI present a higher prevalence of SCS compared to patients with UAI. This result is important for the clinical approach and management of patients with BAI, and it is consistent with the hypothesis that different pathogenetic mechanisms exist between BAI and UAI. In agreement, recent studies have indicated that BAI are more commonly associated with genetic alterations than UAI and especially with genes favoring tumor growth rather than cortisol overproduction [13].
In the present meta-analysis, the mass size of UAI did not differ from the size of the largest lesion for BAI. This is clinically relevant, as previous studies have shown that the size of the adrenal mass is positively correlated with hormonal abnormalities compatible with subtle cortisol hypersecretion [10, 17]. Moreover, a catheterization study showed that in most cases of BAI the larger incidentaloma of the two is the hypersecreting one [25]. Therefore, the present meta-analysis provided evidence that it is rather the bilaterality itself than the mass size, which is responsible for the higher frequency of SCS.
A limitation of this meta-analysis is the fact that different criteria were used across the included studies for the diagnosis of subclinical Cushing’s syndrome [15–19, 24]. The most commonly used were post-DST high morning cortisol concentrations combined with at least one abnormal result of other hormonal measurements, such as high midnight cortisol, low morning ACTH, low-for-age DHEA-S and high 24-h UFC. This variation in criteria [15–19, 24] reflects the clinical reality, as there is still no consensus on diagnostic criteria for SCS diagnosis. The meta-analysis of the biochemical characteristics of the patients demonstrated lower post-DST cortisol concentrations and higher morning ACTH concentrations for patients with UAI when compared to patients with BAI, without any differences regarding other laboratory measurements.
Regarding the prevalence of clinical implications possibly related to cortisol hypersecretion such as obesity, diabetes, dyslipidemia and hypertension, the present meta-analysis did not result in any differences between UAI and BAI. This finding indicates that the higher prevalence of SCS in patients with BAI does not lead to a higher frequency of such clinical morbidities. This may be due to subtle or even intermittent autonomous cortisol hypersecretion in patients with AI [10, 26, 27]. Furthermore, clinical manifestations of cortisol hypersecretion can vary and depend not only on the degree but also on the duration of hypersecretion, as well as the sensitivity of each individual to cortisol excess [26].
In conclusion, the present meta-analysis provided evidence that patients with BAI present a higher prevalence of SCS compared to patients with UAI.
References
R.T. Kloos, M.D. Gross, I.R. Francis, M. Korobkin, B. Shapiro, Incidentally discovered adrenal masses. Endocr. Rev. 16, 460–484 (1995)
C. Davenport, A. Liew, B. Doherty, H.H. Win, H. Misran, S. Hanna, D. Kealy, F. Al-Nooh, A. Agha, C.J. Thompson, M. Lee, D. Smith, The prevalence of adrenal incidentaloma in routine clinical practice. Endocrine 40, 80–83 (2011)
S. Bovio, A. Cataldi, G. Reimondo, P. Sperone, S. Novello, A. Berruti, P. Borasio, C. Fava, L. Dogliotti, G.V. Scagliotti, A. Angeli, M. Terzolo, Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J. Endocrinol. Invest. 29, 298–302 (2006)
J.H. Song, F.S. Chaudhry, W.W. Mayo-Smith, The incidental adrenal mass on CT: prevalence of adrenal disease in 1,029 consecutive adrenal masses in patients with no known malignancy. AJR Am. J. Roentgenol. 190, 1163–1168 (2008)
L. Barzon, N. Sonino, F. Fallo, G. Palu, M. Boscaro, Prevalence and natural history of adrenal incidentalomas. Eur. J. Endocrinol. 146, 61–66 (2002)
M. Terzolo, S. Bovio, G. Reimondo, A. Pia, G. Osella, G. Borretta, A. Angeli, Subclinical Cushing’s syndrome in adrenal incidentalomas. Endocrinol. Metab. Clin. N. Am. 34, 423–439 (2005)
M. Reincke, J. Nieke, G.P. Krestin, W. Saeger, B. Allolio, W. Winkelmann, Preclinical Cushing’s syndrome in “adrenal incidentalomas”: comparison with adrenal Cushing’s syndrome. J. Clin. Endocrinol. Metab. 75, 826–832 (1992)
R. Rossi, L. Tauchmanova, A. Luciano, M. Di Martino, C. Battista, L. Del Viscovo, V. Nuzzo, G. Lombardi, Subclinical Cushing’s syndrome in patients with adrenal incidentaloma: clinical and biochemical features. J. Clin. Endocrinol. Metab. 85, 1440–1448 (2000)
F. Mantero, M. Terzolo, G. Arnaldi, G. Osella, A.M. Masini, A. Ali, M. Giovagnetti, G. Opocher, A.A. Angeli, Survey on adrenal incidentaloma in Italy. Study group on adrenal tumors of the Italian Society of Endocrinology. J. Clin. Endocrinol. Metab. 85, 637–644 (2000)
E. Vassilatou, A. Vryonidou, S. Michalopoulou, J. Manolis, J. Caratzas, C. Phenekos, I. Tzavara, Hormonal activity of adrenal incidentalomas—results from a long term follow-up study. Clin. Endocrinol. (Oxf.) 70, 674–679 (2009)
D. Aron, M. Terzolo, T.J. Cawood, Adrenal incidentalomas. Best Pract. Res. Clin. Endocrinol. Metab. 26, 69–82 (2012)
R. Giordano, F. Guaraldi, R. Berardelli, I. Karamouzis, V. D’Angelo, E. Marinazzo, A. Picu, E. Ghigo, E. Arvat, Glucose metabolism in patients with subclinical Cushing’s syndrome. Endocrine 41, 415–423 (2012)
K. Duan, H.K. Gomez, O. Mete, Clinicopathological correlates of adrenal Cushing’s syndrome. J. Clin. Pathol. 68, 175–186 (2015)
A. Patocs, M. Toth, C. Barta, M. Sasvari-Szekely, I. Varga, N. Szucs, C. Jakab, E. Glaz, K. Racz, Hormonal evaluation and mutation screening for steroid 21-hydroxylase deficiency in patients with unilateral and bilateral adrenal incidentalomas. Eur. J. Endocrinol. 147, 349–355 (2002)
D.A. Vassiliadi, G. Ntali, E. Vicha, S. Tsagarakis, High prevalence of subclinical hypercortisolism in patients with bilateral adrenal incidentalomas: a challenge to management. Clin. Endocrinol. (Oxf.) 74, 438–444 (2011)
I. Androulakis, G. Kaltsas, A. Markou, E. Tseniklidi, P. Kafritsa, T. Pappa, L. Papanastasiou, G. Piaditis, The functional status of incidentally discovered bilateral adrenal lesions. Clin. Endocrinol. (Oxf.) 75, 44–49 (2011)
H. Olsen, E. Nordensrom, A. Bergenfelz, U. Nyman, S. Valdemarsson, E. Palmqvist, Subclinical hypercortisolism and CT appearance in adrenal incidentalomas: a multicenter study from Southern Sweden. Endocrine 42, 164–173 (2012)
V. Morelli, S. Palmieri, A.S. Salcuni, C. Eller-Vainicher, E. Cairoli, V. Zhukouskaya, A. Scillitani, P. Beck-Peccoz, I. Chiodini, Bilateral and unilateral adrenal incidentalomas: biochemical and clinical characteristics. Eur. J. Endocrinol. 168, 235–241 (2013)
E. Vassilatou, A. Vryonidou, D. Ioannidis, S.A. Paschou, M. Panagou, I. Tzavara, Bilateral adrenal incidentalomas differ from unilateral adrenal incidentalomas in subclinical cortisol hypersecretion but not in potential clinical implications. Eur. J. Endocrinol. 171, 37–45 (2014)
M. Viswanathan, N.D. Berkman, D.M. Dryden, L. Hartling, Assessing Risk of Bias and Confounding in Observational Studies of Interventions or Exposures: Further Development of the RTI Item Bank. Methods Research Report (Prepared by RTI–UNC Evidence-based Practice Center under Contract No. 290-2007-10056-I). AHRQ Publication No. 13-EHC106-EF (Agency for Healthcare Research and Quality, Rockville, 2013)
R. DerSimonian, N. Laird, Meta-analysis in clinical trials. Control Clin. Trials 7, 177–188 (1986)
M. Egger, G. Davey Smith, D. Altman, Systematic Reviews in Health Care: Meta-analysis in Context (BMJ Publishing Group, London, 2001)
D. Moher, A. Liberati, J. Tetzlaff, D.G. Altman, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6, e1000097 (2009)
S. Yener, H. Yilmaz, T. Demir, M. Secil, A. Comlekci, DHEAS for the prediction of subclinical Cushing’s syndrome: perplexing or advantageous? Endocrine 48, 669–676 (2015)
W.F. Young Jr, H. du Plessis, G.B. Thompson, C.S. Grant, D.R. Farley, M.L. Richards, D. Erickson, A. Vella, A.W. Stanson, J.A. Carney, C.F. Abboud, P.C. Carpenter, The clinical conundrum of corticotropin-independent autonomous cortisol secretion in patients with bilateral adrenal masses. World J. Surg. 32, 856–862 (2008)
M. Terzolo, G. Osella, A. Ali, G. Borretta, F. Cesario, P. Paccotti, A. Angeli, Subclinical Cushing’s syndrome in adrenal incidentaloma. Clin. Endocrinol. (Oxf.) 48, 89–97 (1998)
G.P. Bernini, A. Moretti, C. Oriandini, M. Bardini, C. Taurino, A. Salvetti, Long-term morphological and hormonal follow-up in a single unit on 115 patients with adrenal incidentalomas. Br. J. Cancer 92, 1104–1109 (2005)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Paschou, S.A., Kandaraki, E., Dimitropoulou, F. et al. Subclinical Cushing’s syndrome in patients with bilateral compared to unilateral adrenal incidentalomas: a systematic review and meta-analysis. Endocrine 51, 225–235 (2016). https://doi.org/10.1007/s12020-015-0776-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0776-6