Abstract
Thyroid hormone (TH) abnormalities are common in patients with diabetes mellitus (DM). These thyroid hormone abnormalities have been associated with inflammatory activity in several conditions but this link remains unclear in DM. We assessed the influence of subclinical inflammation in TH metabolism in euthyroid diabetic patients. Cross-sectional study involving 258 subjects divided in 4 groups: 70 patients with T2DM and 55 patients with T1DM and two control groups of 70 and 63 non-diabetic individuals, respectively. Groups were paired by age, sex, and body mass index (BMI). We evaluated the association between clinical and hormonal variables [thyrotropin, reverse T3 (rT3), total and free thyroxine (T4), and triiodothyronine (T3)] with the inflammation markers C-reactive protein (hs-CRP), serum amyloid A (SAA), and interleukin-6 (IL-6). Serum T3 and free T3 were lower in patients with diabetes (all P < 0.001) compared to the control groups. Interleukin-6 showed positive correlations with rT3 in both groups (P < 0.05). IL-6 was independently associated to FT3/rT3 (B = −0.193; 95 % CI −0.31; −0.076; P = 0.002) and FT4/rT3 (B = −0.107; 95 % CI −0.207; −0.006; P = 0.039) in the T1DM group. In the T2DM group, SAA (B = 0.18; 95 % CI 0.089; 0.271; P < 0.001) and hs-CRP (B = −0.069; 95 % CI −0.132; –0.007; P = 0.03) predicted FT3 levels. SAA (B = −0.16; 95 % CI −0.26; −0.061; P = 0.002) and IL6 (B = 0.123; 95 % CI 0.005; 0.241; P = 0.041) were related to FT4/FT3. In DM, differences in TH levels compared to non-diabetic individuals were related to increased subclinical inflammatory activity and BMI. Altered deiodinase activity was probably involved. These findings were independent of sex, age, BMI, and HbA1c levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The non-thyroidal illness syndrome (NTIS), also known as the euthyroid sick syndrome or the low T3 syndrome, was initially described in the 1970s. It represents a state of alterations in thyroid hormone (TH) economy that, by definition, are not related to intrinsic diseases of the hypothalamus-pituitary-thyroid axis but rather represent imbalances in thyroid hormone production, metabolism, and action [1].
Serum thyroid hormone (TH) abnormalities are common in patients with Diabetes Mellitus (DM), especially in those with type 1 DM (T1DM) because of the possible coexistence of thyroid and pancreatic autoimmunity [2, 3]. In T1DM, thyrotropin levels were related to differences in lipid profile, even in the euthyroid range, but this association was dependent on insulin resistance [4]. Subclinical thyroid dysfunction is common among patients with type 2 diabetes and although hypothyroidism is seen more often, there have been reports of increased prevalence of subclinical hyperthyroidism in this setting, especially in older patients with goiter [5]. In addition, patients with obesity, metabolic syndrome, and type 2 diabetes (T2DM) also show differences in serum TH when compared to lean and healthy individuals [6–8]. Therefore, recognizing NTIS is important to avoid misdiagnosis with primary thyroid dysfunctions that would otherwise indicate treatments that have not been proven beneficial in patients with low T3 secondary to systemic illnesses [9] and also to be aware of the possibility that interplay between diabetes mellitus and thyroid axis could explain the abnormalities found in these patients.
In cases with poor metabolic control, a state of low serum triiodothyronine (T3) concentration has been described for more than three decades in patients with both types of diabetes [10, 11]. These patients are often evaluated in the setting of acute metabolic decompensation or in the presence of diabetic ketoacidosis [11]. Similar changes in TH have been shown in other chronic conditions such as heart failure [12], chronic obstructive pulmonary disease [13], liver and kidney failure [14, 15], among others. In these situations, the low T3 syndrome is associated to an increased inflammatory activity and becomes more evident during acute exacerbations, returning to baseline values upon recovery [10, 13]. Moreover, they are intimately connected to prognosis [12, 16]. In intensive care units, clearly identifiable alterations can be found in serum TH levels, which have been linked to the amplified inflammatory activity characteristic of acutely infirm patients [17, 18]. Our group has previously found an association of C-reactive protein (CRP) and reverse T3 in patients with T2DM [19], while differences in rT3 levels were apparent only in those with previous cardiovascular events, who also showed a more pronounced subclinical inflammatory pattern [20].
Despite DM being increasingly characterized as an inflammatory disease in recent years, TH abnormalities remain related only to poor glycemic control [8, 10, 11]. Moreover, the pathophysiology of these abnormalities remains not well understood and it is not known whether patients with T1DM and T2DM share the same pathophysiological processes. Also, cytokines other than CRP that are closely related to NTIS and DM, such as interleukin-6 (IL-6), have not been extensively studied in patients with DM, especially T1DM. Thus, our aims were to (a) show the presence of a low T3 state in patients with both T1DM and T2DM under outpatient care and no clinical or laboratorial evidence of thyroid autoimmunity; and (b) verify the association of TH abnormalities seen in this state to the subclinical, low-grade systemic inflammation of DM (Fig. 1).
Subjects and methods
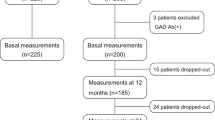
This was a cross-sectional study involving 258 individuals, divided into 4 groups: 70 patients with T2DM, 55 patients with T1DM, and two groups of 70 and 63 non-diabetic individuals as control groups for patients with T2DM and T1DM (T2DMc and T1DMc groups), respectively. Control groups were paired by age, sex, and body mass index (BMI). All individuals were aged between 18 and 70 years. Exclusion criteria were any conditions associated to low T3 states such as acute illnesses, recent caloric restriction (loss equal or more than 5 % body weight in the previous 3 months), renal (creatinine clearance <60 ml/min/m2 calculated by the Cockroft-Gault formula) or hepatic (Child-Pugh classification B or C) impairment, heart failure (class III or IV NYHA), active neoplastic or inflammatory illnesses and myocardial infarction or stroke occurring less than 6 months previously to study recruitment. Additionally, patients with any history of thyroid disease, thyroid nodules, detectable serum anti-thyroid antibodies (anti-thyroperoxidase or anti-thyroglobulin antibodies) and prescription for medications that could affect thyroid hormone levels (levothyroxine, anti-thyroid medication, corticosteroids, amiodarone, initiation of beta-blockers less than 6 months previous to study recruitment and exposure to iodine containing contrast agents less than 1 year previous to study evaluation) were also excluded. All individuals selected for this study were required to have serum thyrotropin (TSH) levels within the normal range. All lived in an iodine-sufficient area.
Patients were recruited from the Type 1 and Type 2 Diabetes Outpatient Clinics of our Tertiary University Hospital. Patients were enrolled continuously, respecting exclusion criteria (Fig. 2). Control subjects were recruited from the patients’ family members or accompanying personnel and were from the same socio-economical population. Data were collected between July 2012 and April 2014. Blood was drawn during routine appointments at each clinic, immediately centrifuged and stored at −80 °C for subsequent analysis.
Diagnosis of diabetes followed ADA criteria [21]. Patients were considered to have type 1 diabetes if 3 or more of the following characteristics were present at diagnosis: age <30 years, peptide C at first evaluation <0.1 ng/ml, detectable serum anti-GAD65 antibodies, presence of weight loss >5 % of usual body weight, BMI <27, no family history of diabetes in first degree relatives, or presence of diabetic ketoacidosis [22].
Clinical data studied consisted of age, sex, time since diabetes diagnosis (disease duration), current therapy (oral drugs, insulin alone, or combination therapy), waist (measured at the midline between the inferior border of ribcage and the superior iliac crest) to hip ratio (WHR), BMI, presence of hypertension (blood pressure >130/80 mmHg or treatment for this condition), smoking and presence of microvascular (diabetic nephropathy, retinopathy, or neuropathy) and macrovascular (angina, previous myocardial infarction, or stroke) complications. Diabetic nephropathy was diagnosed on the basis of at least 2 abnormal albumin/creatinine ratio in urine (>30 mg/g); retinopathy was considered positive on the basis of characteristic findings on fundoscopy, as reported by the ophthalmology service of the same University Hospital; neuropathy was considered present if the patient was incapable of feeling the 10g Semmes–Weinstein monofilament test on 2 or more sites.
Laboratory measurements consisted of TSH, total (T) and free (F) thyroxine (T4), T3 and reverse T3 (rT3). Sample size calculations (described below) were done with results in original mass units. Conversion formulas from SI to mass units are provided at the bottom of Table 2. Inflammatory activity was measured by high-sensitivity C-reactive protein (hs-CRP), IL-6 and serum amyloid A (SAA). As surrogate measures of deiodinase activity we calculated the FT3/rT3, FT4/FT3, and FT4/rT3 relations by simple division of values.
TSH and FT4 were measured by electro-chemiluminescence (Roche Hitachi-Elecsys Cobas, USA –reference values—RV: TSH 0.45-4.5iu/l; FT4: 11.6–23.2 pmol/l). Total T4 (RV: 57.9–160.9 nmol/l), TT3 (RV: 1.32–2.87 nmol/l), FT3 (RV: 2.15–6.76 pmol/l) and rT3 (RV: 0.14–0.54 nmol/l) were measured by radioimmunoassay (Siemens Medical Solution Diagnostics, Los Angeles, USA). All intra and inter-assay coefficient of variation were <10 %. Anti-thyroperoxidase and anti-thyroglobulin antibodies were measured by electro-chemiluminescence (Roche Hitachi-Elecsys Cobas, USA—RV <34 IU/ml and <115 IU/ml, respectively). High-sensitivity CRP (Cusabio Biotech Co, Wuhan, China; sensitivity: the least amount that can be differentiated from zero), IL-6 (R&D Systems Inc Minneapolis, USA; sensitivity 0.016–0.11 pg/ml) and SAA (Uscn Life Science Inc., Wuhan, China; sensitivity: the least amount that can be differentiated from zero) were measured by ELISA. HbA1c was measured by high performance liquid chromatography (RV: 4–5.7 %).
The study was approved by the University Ethics in Research Committee and functioned according to the 3rd edition of the Guidelines on the Practice of Ethical Committees in Medical Research issued by the Royal College of Physicians of London.
Statistical methods
We conducted a pilot study to estimate the minimum sample size required to have an 80 % probability of detecting a difference of 10 ng/ml (0.15 nmol/l) in TT3 levels and 0.2 pg/ml (0.3 pmol/l) in FT3 levels. This pilot study included 10 subjects in each group. The standard deviations found for TT3 were 5.1, 5.2, 6.2, and 4.6 ng/dl and for FT3 0.93, 0.88, 0.85, and 0.62 pg/ml in groups T2DM, T1DM, T2DMc, and T1DMc, respectively. Thus, we estimated that at least 63 patients with T2DM and 46 patients with T1DM would be required. The control group numbers were set to match the number of patients with DM in each group.
Descriptive analysis was made by providing measures of position and dispersion; median and interquartile range (IQR) for continuous data and frequencies and percentages for categorical variables. Normality was assessed by the Kolmogorov–Smirnov test. Data on TH, their relations and inflammatory markers as well as HbA1c were not normally distributed (P < 0.001 for all), except for FT3 and FT4 (P = 0.2 for both). Non-parametric tests were preferred for all variables as even FT3 and FT4 had relatively skewed distributions (P < 0.3). Comparisons of serum TH levels and inflammatory markers between groups were done by Kruskal–Wallis one-way ANOVA with post hoc Bonferroni corrections for multiple comparisons (P for differences between groups considered significant only if <0.008). Comparison of gender frequency between groups was done by the Chi Square test. Associations between TH, inflammatory markers and clinical variables were assessed by the Spearman correlation coefficient.
To evaluate the influence of inflammatory markers on TH levels, multivariate linear regression analyses were conducted with all non-normally distributed variables log-transformed. The model was adjusted for age, sex, BMI, WHR and HbA1c. All analyses were checked for colinearity by tolerance analysis and values were considered significant if <0.2.
Results were considered significant if P value was <0.05. All tests were two-tailed. Calculations were done with SPSS (IBM Inc) version 20.0.
Results
Characteristics of patients with diabetes
Characteristics of patients with DM are shown in Table 1. Noteworthy, when comparing patients with DM below and above median HbA1c of the respective group, we found no differences in thyroid hormone levels. In the T2DM group, patients with HbA1c above the median had higher hs-CRP (1.17 vs 0.45 mg/l; P = 0.04). No other differences for inflammatory variables were found in both groups.
Of interest, there were no differences in total and free T3 levels or between FT3/rT3, FT4/FT3, and FT4/r in patients with T1DM compared to the T2DM group. Also, we observed no differences in TH levels between patients with and without microvascular complications.
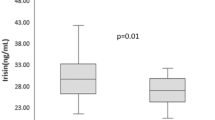
Patients with type 2 diabetes and control group
Compared to the T2DMc group, patients with T2DM had higher WHR (0.99 vs 0.89; P < 0.001). The T2DM group showed lower T3 (1.19 vs 1.38 nmol/l; P < 0.001) and FT3 (2.99 vs 3.71 pmol/l; P < 0.001) than the T2DMc group. Free T4 (16.22 vs 13.91 pmol/l; P < 0.001) and IL-6 (1.40 vs 0.88 pg/ml; P = 0.007) levels were higher in the T2DM group. FT3/rT3 was lower (8.51 vs 10.7; P = 0.001) and FT4/FT3 was higher (5.27 vs 4.08; P < 0.001) in the T2DM group. No differences were observed in TSH or rT3 levels (Table 2).
We found inverse associations between TSH and WHR (r = −0.35; P = 0.003) and between BMI and TT3 (r = −0.28; P = 0.02). The WHR was positively associated with IL-6 (r = 0.24; P = 0.04) and SAA (r = 0.24; P = 0.04). Similarly, BMI also showed a direct association to IL-6 (r = 0.23; P = 0.048) and hs-CRP (r = 0.27; P = 0.02). Table 3 summarizes correlation coefficients between serum TH levels and inflammatory markers. In the T2DMc group, WHR was correlated to hs-CRP (r = 0.26; P = 0.03). BMI was related to SAA (r = 0.35; P = 0.003) and hs-CRP (r = 0.47; P < 0.001). Age was correlated to FT4/FT3 (r = 0.27; P = 0.02). No associations between hormonal and inflammatory variables were found.
Multivariate linear regression analyses revealed that SAA (B = 0.18; 95 % CI 0.089; 0.271; P < 0.001) and hs-CRP (B = −0.069; 95 % CI −0.132; −0.007; P = 0.03) were independent predictors of FT3 levels. SAA (B = −0.16; 95 % CI −0.26; −0.061; P = 0.002) and IL-6 (B = 0.123; 95 % CI 0.005; 0.241; P = 0.041) were independent predictors of FT4/FT3. BMI was independently associated to TT3 levels (B = −0.006; 95 % CI −0.01; −0.002; P = 0.003).
No significant results were found in the T2DMc in this model.
Patients with type 1 diabetes and control group
Patients with T1DM had lower serum T4 (71.18 vs 93.63 nmol/l), T3 (1.14 vs 1.41 nmol/l) and FT3 (3.28 vs 3.91 pmol/l); all P < 0.001 compared to the T1DMc group. TSH levels were also lower (1.46 vs 2.06 iu/l; P = 0.002). High-sensitivity CRP was higher in the T1DM group (0.87 vs 0.36 mg/l; P < 0.001). FT3/rT3 was lower (8.51 vs 11.4) and FT4/FT3 higher (4.97 vs 4.0) in patients with T1DM (P < 0.001 for both). No differences were found in FT4 or rT3 levels (Table 2).
In the T1DM group, we found a positive association between WHR and hs-CRP (r = 0.36; P = 0.007). The relation of HbA1c with FT3/rT3 (r = −0.24; P = 0.07) and FT4/FT3 (r = 0.24; P = 0.08) approached but did not reach statistical significance. Correlations between TH levels and inflammatory markers are shown in Table 3. In the T1DMc group, BMI was directly associated to SAA (r = 0.29; P = 0.02) and hs = CRP (r = 0.31; P = 0.01). There were inverse correlations of age with TT4 (r = −0.5; P < 0.001) and TT3 (r = −0.3; P = 0.01), and between WHR and TT4 (r = −0.28; P = 0.02). TSH was associated to weight (r = 0.27; P = 0.03) and waist circumference (r = 0.3; P = 0.01). We observed no associations between inflammatory and hormonal variables in this group.
In multivariate linear regression, IL-6 was an independent predictor of FT3/rT3 (B = −0.193; 95 % CI −0.31; −0.076; P = 0.002) and FT4/rT3 (B = −0.107; 95 % CI −0.207; −0.006; P = 0.039). HbA1c was independently associated to FT4/FT3 (B = 0.018; 95 % CI 0.004; 0.033; P = 0.014).
No predictors of TH levels were found with this model in the T1DMc group.
Discussion
In this study, the main novel findings were that patients with T1DM and T2DM share similar hormone abnormalities and also that the latter arise from imbalances in deiodinase activity, which were associated to subclinical inflammatory activity. Of note, a more thorough evaluation of inflammatory activity revealed that IL-6 and SAA, which are pro-inflammatory cytokines characteristically increased in patients with DM, played a major role in these results. All patients had lower serum concentrations of TT3 and FT3 than non-diabetic individuals paired by age, sex, and BMI. In previous works, the low T3 state in patients with T1DM and T2DM has been mainly associated to poor glycemic control [10, 23, 24]. However, in critically ill patients [25–27] as well as in other chronic conditions [10, 12, 13], this syndrome has been related to inflammatory activity. Diabetes itself is a condition that has been increasingly linked to pro-inflammatory activity, especially T2DM [28–30]. In our study, the relationship between inflammatory response and TH levels was not replicated in the control groups, despite similar BMI values.
The T2DM group had higher serum levels of IL-6 alongside more evident central adiposity, represented by the larger WHR. In the T2DM group, rT3 levels and a lower FT3/rT3 ratio were associated to an increased inflammatory response, implying decreased peripheral T3 generation and/or increased T4 inactivation to rT3. The increased FT4 concentration when compared to the T2DMc group favors the hypothesis of inhibited type 1 deiodinase activity, as conversion to T3 is the main pathway of T4 metabolism [31]. In multivariate adjusted regression, SAA and hs-CRP were the main determinants of FT3 and independently predicted FT4/FT3 levels. Serum amyloid A is an acute-phase pro-inflammatory cytokine produced in the liver in response to IL-6 and is related to hs-CRP, with higher levels encountered in patients of higher cardiovascular risk [32, 33]. A surprising finding was the direct association of SAA with FT3 and inverse with the FT4/FT3 ratio, which suggests increased peripheral formation of T3. This may help explain the intra-pituitary induction of type 2 deiodinase, which is held as one possible explanation for the normal serum TSH levels often found in patients with NTIS. The increased intra-pituitary concentration of T3 could render the gland tissue euthyroid, preventing the otherwise expected rise in TSH [34]. Therefore, it is possible that some cytokines could be responsible for enhancing T3 formation [35], which could help explain why our patients had TSH levels comparable to the control groups despite lower serum FT3 concentrations. Genetic abnormalities undermining the expression and activity of type 2 deiodinase have been associated to increased insulin resistance [36, 37]. In fact, a case–control study of Brazilian patients with type 2 diabetes demonstrated a higher prevalence the Thr92Ala polymorphism in patients with type 2 diabetes compared to nondiabetic subjects [38]. The following metanalysis pooling other 3 studies from other countries confirmed the association between this polymorphism and T2DM [38]. On the other hand, type 2 deiodinase is believed to have a rather low contribution to circulating T3 in humans [39]. Whether some cytokines may have different effects on deiodinase activity from others is not clear to us at this point, but deserves confirmation and further investigation in future basic as well as clinical studies. We found no other works assessing the relation of SAA and TH in NTIS or DM. Another point worthy of note is that these associations were found exclusively in patients with DM. Higher hs-CRP levels, however, showed opposite results and were associated to lower serum FT3 concentrations.
Comparable findings regarding increased inflammatory markers were encountered in patients with T1DM, represented by higher hs-CRP levels than the T1DMc group, even with comparable WHR measures. In this group, interleukin-6 correlated positively with rT3 and was an independent predictor of the relations FT3/rT3 and FT4/rT3, suggesting decreased peripheral conversion of T4 to T3, a common finding in non-thyroidal illness (NTIS) [40, 41]. Interleukin-6 is a cytokine closely associated to NTIS, showing a tight correlation with the falling T3 in several studies [17, 26, 42]. As for glycemic control, it was the major predictor of FT4/FT3 in the T1DM group. Higher blood glucose or even the insulin deficiency characteristic of T1DM could decrease type 1 deiodinase activity in the liver, further reducing peripheral activation of T4 to T3. Alternatively, poorer glycemic control could act through the action of increased pro-inflammatory mediators. This already established role of glycemic control in TH metabolism was confirmed only in this group of patients. We believe this could be due to the more heterogeneous HbA1c levels in the T1DM group and the more manifest glycemic variability that is usually found in patients with T1DM. In addition, the inflammatory response was more evident in patients with T2DM, an effect that could have predominated over glycemic levels in that group.
The lower serum TT3 and FT3 levels are in line with previous works showing decreased levels of T3 in patients with diabetes [8, 10, 11]. Notwithstanding comparable age and BMI, the subclinical inflammation process was more prominent in the groups of patients with T1DM and T2DM, a fact that could explain differences regarding the correlations found when compared to the control groups and also in comparison to studies involving individuals with metabolic syndrome but no DM [43, 44]. In such, patients with metabolic syndrome presented higher FT4 levels, as well as an inverse association between FT4 and BMI [45], findings that are similar to those in our patients with T2DM. However, in our T2DM group, BMI was independently and negatively associated to TT3. We believe that this could be due to the hyperinsulinemia characteristic of these patients, which could decrease thyroid hormone binding globulin synthesis by the liver, similarly to what is often observed for SHBG [46].
The strengths of the current study include the presence of control groups paired by BMI, which is an established confounding factor when analyzing thyroid hormone levels in patients with diabetes, and the fact that individuals under acute metabolic stress were not included. In addition, both type 1 and type 2 diabetes were analyzed and all patients were euthyroid, with undetectable serum anti-thyroid antibodies. Nevertheless, the study has some limitations. Firstly, the cross-sectional design may limit conclusions on causality. Moreover, the relatively small sample size in each group may have precluded additional findings, despite the fact that we based our numbers in a minimal sample size calculation, which was estimated in a pilot study. Finally, the inference of abnormal deiodinase activity was indirect, as we did not measure the enzymes’ activity in liver or muscle, because biopsies were deemed unethical in our present clinical situation. For similar reasons, we were not able to confirm that lower serum levels of TH translate into actual tissue hypothyroidism. These indirect estimations have, nonetheless, shown a good correlation with the enzymes’ activities [47].
In conclusion, we have shown that the TH abnormalities described in patients with type 1 and type 2 diabetes were related not only to glycemic control as previously described, but also to the increased inflammatory activity seen in both groups of patients with DM, which in turn were associated to imbalances in deiodinase activity. These findings were independent of sex, age, BMI, and HbA1c levels. One recent study showed that anti-inflammatory medications could prevent the occurrence of NTIS in the setting of acute myocardial infarction [48]. Further research is warranted to clarify if ameliorating inflammation can reverse TH abnormalities in either type of diabetes and if T3 replacement shows any beneficial impact on the course of the disease.
References
B. McIver, C.A. Gorman, Euthyroid sick syndrome: an overview. Thyroid 7, 125–132 (2007)
L.H. Duntas, J. Orgiazzi, G. Brabant, The interface between thyroid and diabetes mellitus. Clin. Endocrinol. (Oxf.) 75, 1–9 (2011)
G.E. Umpierrez, K.A. Latif, M.B. Murphy, H.C. Lambeth, F. Stentz, A. Bush, A.E. Kitabch, Thyroid dysfunction in patients with type 1 diabetes: a longitudinal study. Diabetes Care 26, 1181–1185 (2003)
T. Bulum, B. Kolaric, L. Duvnjak, Insulin sensitivity modifies the relationship between thyroid function and lipid profile in euthyroid type 1 diabetic patients. Endocrine 42, 139–145 (2012)
J.J. Díez, P. Iglesias, Subclinical hyperthyroidism in patients with type 2 diabetes. Endocrine 42, 157–163 (2012)
A. Roos, S.J.L. Bakker, T.P. Links, R.O.B. Gans, B.H.R. Wolffenbuttel, Thyroid function is associated with components of the metabolic syndrome in euthyroid subjects. J. Clin. Endocrinol. Metab. 92, 491–496 (2007)
N. Knudsen, P. Laurberg, L.B. Rasmussen, I. Bülow, H. Perrild, L. Ovesen, T. Jørgensen, Small differences in thyroid function may be important for body mass index and the occurrence of obesity in the population. J. Clin. Endocrinol. Metab. 90, 4019–4024 (2006)
J.L. Schlienger, A. Anceau, G. Charbrier, M.L. North, F. Stephan, Effect of diabetic control on the level of circulating thyroid hormones. Diabetologia 22, 486–488 (1982)
N. Stathatos, L. Wartofsky, The euthyroid sick syndrome: is there a physiologic rationale for thyroid hormone treatment? J. Endocrinol. Invest. 26, 1174–1179 (2003)
U.M. Kabadi, Impaired pituitary thyrotroph function in uncontrolled type II diabetes mellitus: normalization on recovery. J. Clin. Endocrinol. Metab. 59, 521–525 (1984)
R. Naeije, J. Golstein, N. Clumeck, H. Meinhold, K.W. Wenzel, L. Vanhaelst, A low T3 syndrome in diabetic ketoacidosis. Clin. Endocrinol. (Oxf.) 8, 467–472 (1978)
G. Iervasi, A. Pingitori, P. Landi, M. Raciti, A. Ripoli, M. Scarlattini, A. L’Abbate, L. Donato, Low-T3 syndrome: a strong prognostic predictor of death in patients with heart disease. Circulation 107, 708–713 (2003)
F. Karadag, H. Ozcan, A.B. Karul, M. Yilmaz, O. Cildag, Correlates of non-thyroidal illness in chronic obstructive pulmonary disease. Respir. Med. 101, 1439–1446 (2007)
M. Borzio, R. Caldara, F. Borzio, V. Piepoli, P. Rampini, C. Ferrari, Thyroid function tests in chronic liver disease: evidence for multiple abnormalities despite clinical euthyroidism. Gut 24, 631–636 (1983)
C. Zocalli, F. Mallamaci, G. Tripepi, S. Cutrupi, P. Pizzini, Low triiodothyronine and survival in end-stage renal disease. Kidney Int. 70, 523–528 (2006)
E. Scoscia, S. Baglioni, A. Eslami, G. Iervasi, S. Monti, T. Todisco, Low triiodothyronine (T3) state: a predictor of outcome in respiratory failure? Results of a clinical pilot study. Eur. J. Endocrinol. 151, 557–560 (2004)
A. Boelen, M.C. Platvoet Schiphorst, W.M. Wiersinga, Association between serum interluekin-6 and serum 3,5,3’-triiodothyronine in non-thyroidal illness. J. Clin. Endocrinol. Metab. 77, 1695–1699 (1993)
M. Michalaki, A.G. Vagenakis, M. Makri, F. Kalfarentzos, V. Kyriazopoulou, Dissociation of the early decline in serum T3 concentration and serum IL-6 rise and TNF-a in non-thyroidal illness syndrome induced by abdominal surgery. J. Clin. Endocrinol. Metab. 86, 4198–4205 (2001)
A. Moura Neto, M.C. Parisi, M.A. Tambascia, S.M. Alegre, E.J. Pavin, D.E. Zantut-Wittmann, The influence of body mass index and low-grade systemic inflammation on thyroid hormone abnormalities in patients with type 2 diabetes. Endocr. J. 60, 877–884 (2013)
A. Moura Neto, M.C. Parisi, M.A. Tambascia, S.M. Alegre, E.J. Pavin, D.E. Zantut-Wittmann, Relationship of thyroid hormone levels and cardiovascular events in patients with type 2 diabetes. Endocrine 45, 84–91 (2014)
American Diabetes Association, Standards of medical care in diabetes—2012. Diabetes Care 35, S11–S63 (2012)
American Diabetes Association, Diagnosis and classification of diabetes mellitus. Diabetes Care 35, S65–S71 (2012)
N. Custro, V. Scafidi, T. Borsellino, Changes in the thyroid hormone picture that may be found in severely decompensated type II diabetes. Minerva Med. 82, 9–14 (1991)
U.M. Kabadi, B.N. Premachandra, Low triiodothyronine and raised reverse triiodothyronine levels in patients over fifty years of age who have type II diabetes mellitus: influence of metabolic control, not age. J. Am. Geriatr. Soc. 32, 375–379 (1984)
A. Rodriguez-Perez, F. Palos-Paz, E. Kaptein, T.J. Visser, L. Dominguez-Gerpe, J. Alvarez-Escudero, J. Lado-Abeal, Identification of molecular mechanisms related to nonthyroidal illness syndrome in skeletal and adipose tissue from patients with septic shock. Clin. Endocrinol. (Oxf.) 68, 821–827 (2008)
P.H. Davies, E.G. Black, M.C. Sheppard, J.A. Franklyn, Relation between serum interleukin-6 and thyroid hormone concentrations in 270 hospital in-patients with non-thyroidal illness. Clin. Endocrinol. (Oxf.) 44, 199–205 (1996)
A. Boelen, J. Kwakkel, E. Fliers, Beyond low plasma T3: local thyroid hormone metabolism during inflammation and infection. Endocr. Rev. 32, 670–693 (2011)
N. Rasouli, P. Kern, Adipocytokines and the metabolic complications of obesity. J. Clin. Endocrinol. Metab. 93, S64–S73 (2008)
B. Antuna-Puente, B. Feve, S. Fellahi, J.P. Bastard, Adipokines: the missing link between insulin resistance and obesity. Diabetes Metab. 34, 2–11 (2008)
M.C. Calle, M.L. Fernandez, Inflammation and type 2 diabetes. Diabetes Metab. 38, 183–191 (2012)
A.C. Bianco, D. Salvatore, B. Gereben, M.J. Berry, P.R. Larsen, Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr. Rev. 23, 38–89 (2002)
T.L. Wu, I. Chen Tsai, P.Y. Chang, K.C. Tsao, C.F. Sun, L.L. Wu, J.T. Wu, Establishment of an in-house ELISA and the reference range for serum amyloid A (SAA): complimentary between SAA and C-reactive protein as markers of inflammation. Clin. Chim. Acta 376, 72–76 (2007)
J.T. Wu, L.L. Wu, Linking inflammation and atherogenesis: soluble markers identified for the detection of risk factors and for early risk assessment. Clin. Chim. Acta 366, 74–80 (2006)
E. Sánchez, P.S. Singru, C. Fekete, R.M. Lechan, Induction of type 2 iodothyronine deiodinasein the mediobasal hypothalamus by bacterial lipopolysaccharide: role of corticosterone. Endocrinology 149, 2484–2493 (2008)
L. Mebis, L. Langouche, T.J. Visser, G. Van den Berghe, The type II iodothyronine deiodinase is up-regulated in skeletal muscle during prolonged critical illness. J. Clin. Endocrinol. Metab. 92, 3330–3333 (2007)
A. Marsili, C. Aguayo-Mazzucato, T. Chen, M. Kumar, E.P. Chung, J.W. Lunsford, T. Harney, E. Van-Tran, W. Gianetti, C. Ramadan, S. Chou, P.R. Bonner Weir, J.E. Larsen, A.M. Silva, M. Zavacki, Mice with a targeted deletion of the type 2 deiodinase are insulin resistant and susceptible to diet induced obesity. PLoS One 6, e20832 (2006)
L.B. Leiria, J.M. Dora, S.M. Wajner, A.A. Estivalet, D. Crispim, A.L. Maia, The rs225017 polymorphism in the 3′UTR of the human DIO2 gene is associated with increased insulin resistance. PLoS One 9, e103960 (2014)
J.M. Dora, W.E. Machado, J. Rheinheimer, D. Crispim, A.L. Maia, Association of the type 2 deiodinase Thr92Ala polymorphism with type 2 diabetes: case-control study and meta-analysis. Eur. J. Endocrinol. 163, 427–434 (2010)
K.A. Heemstra, M.R. Soeters, E. Fliers, M.J. Serlie, J. Burggraaf, M.B. van Doorn, A.A. van der Klaauw, J.A. Romijn, J.W. Smit, E.P. Corssmit, T.J. Visser, Type 2 iodothyronine deiodinase in skeletal muscle: effects of hypothyroidism and fasting. J. Clin. Endocrinol. Metab. 94, 2144–2150 (2009)
E.L. Olivares, M.P. Marasi, R.S. Fortunato, A.C. da Silva, R.H. Costa-e-Souza, I.G. Araújo, E.C. Mattos, M.O. Masuda, M.A. Mulcahey, S.A. Huang, A.C. Bianco, D.P. Carvalho, Thyroid function disturbance and type 3 iodothyronine deiodinase induction after myocardial infarction in rats a time course study. Endocrinology 148, 4786–4792 (2007)
S.M. Wajner, I.M. Goemann, A.L. Bueno, P.R. Larsen, A.L. Maia, IL-6 promotes nonthyroidal illness syndrome by blocking thyroxine activation while promoting thyroid hormone inactivation in human cells. J. Clin. Invest. 121, 1834–1845 (2011)
A. Boelen, M.A. Maas, C.W. Lowik, M.C. Platvoet, W.M. Wiersinga, Induced illness in interleukin-6 (IL-6) knock-out mice: a causal role of IL-6 in the development of the low 3,5,3′-triiodothyronine syndrome. Endocrinology 137, 5250–5254 (1996)
L. Mehran, A. Amouzegar, M. Tohidi, M. Moayedi, F. Azizi, Serum free thyroxine concentration is associated with metabolic syndrome in euthyroid subjects. Thyroid 2014(24), 1566–1574 (2014)
O. Tarcin, G.B. Abanonu, D. Yazici, O. Tarcin, Association of metabolic syndrome parameters with TT3 and FT3/FT4 ratio in obese Turkish population. Metab. Syndr. Relat. Disord. 10, 137–142 (2012)
G. Roef, B. Lapauw, S. Goemaere, H.G. Zmierczak, K. Toye, J.M. Kaufman, Y. Taes, Body composition and metabolic parameters are associated with variation in thyroid hormone levels among euthyroid young men. Eur. J. Endocrinol. 167, 718–726 (2012)
L.J. Moran, H.J. Teede, M. Moakes, P.M. Clifton, R.J. Norman, G.A. Wittert, Sex hormone binding globulin, but not testosterone, is associated with the metabolic syndrome in overweight and obese women with polycystic ovary syndrome. J. Endocrinol. Invest. 36, 1004–1010 (2013)
Y. Debaveye, B. Ellger, L. Mebis, V.M. Darras, G. Van den Berghe, Regulation of tissue iodothyronine deiodinase activity in a model of prolonged critical illness. Thyroid 18, 551–560 (2008)
J. Vidart, S.M. Wajner, R.S. Leite, A. Manica, B.D. Schaan, P.R. Larsen, A.L. Maia, N-acetylcysteine administration prevents nonthyroidal illness syndrome in patients with acute myocardial infarction: a randomized clinical trial. J. Clin. Endocrinol. Metab. 99, 4537–4545 (2014)
Acknowledgments
The authors wish to thank the biologist Conceição Aparecida da Silva for her inestimable help in collecting blood samples and laboratory analysis. This study was received financial support of FAPESP (Sao Paulo Research Support Foundation—Grants 2010/08854-0 and 2013/03295-1).
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moura Neto, A., Parisi, M.C.R., Alegre, S.M. et al. Relation of thyroid hormone abnormalities with subclinical inflammatory activity in patients with type 1 and type 2 diabetes mellitus. Endocrine 51, 63–71 (2016). https://doi.org/10.1007/s12020-015-0651-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0651-5