Abstract
Bone metastases are a frequent and debilitating consequence for many tumors, of which breast, lung, prostate, and kidney cancer are the most common. The dialog among cancer cells, bone microenvironment, and immune system regulates bone metastasis formation. Indeed, bone and immune system are strictly linked to each other because bone regulates the hematopoietic stem cells from which all cells of the immune system derive. Many immunoregulatory cytokines influence the fate of bone cells and promote the growth of tumor cells in bone, contributing to sustain the vicious cycle of bone metastasis. Bone is an attractive soil for cancer cells, which can remain dormant for years or directly form bone lesions. The fate of cancer cells after their arrival to bone marrow depends on a complex cross-talk among cancer, bone, and immune cells in the microenvironment. This review provides an overview of the different steps occurring during bone metastatic process, with particular attention to the osteoimmunology field. Furthermore, we will revise the current available clinical approaches for the therapy of bone metastatic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The metastatic process at all is inefficient; indeed, despite disseminated tumor cells (DTCs) that are found in the bone marrow (BM) of cancer patients, many of them do not develop overt metastatic disease [1]. Even though bone is conducive for tumor dissemination and survival of cancer cells, other processes need to sustain tumor progression. Indeed, the diffusion of cancer cells from the primary site to other organs is a complex process depending both on the invasive abilities of cancer cells and on the microenvironment of the target organ. Tissues are not prone to welcome metastatic cells since in a healthy organ there are active innate immune system and stroma that commonly do not support the growth of “foreign cells” [2]. Nonetheless, certain organs have a less hostile microenvironment than others, such as the bone, which seems to be the most attractive “soil” for many cancers. Bone metastases are particularly common complications for solid tumors, such as breast, prostate cancer, and to a lesser extent melanoma, lung, and kidney cancer [3]. Bone lesions cause morbidity due to the frequent occurrence of skeletal related events (SREs), such as pathological fracture, spinal cord compression, bone pain, and hypercalcemia [4]. Several reasons account for the “peculiar attraction” of cancer cells to bone, for instance the genetic component demonstrated in breast cancer, where cancer cells in the primary tumor acquire a bone tropism signature [5, 6]; the hematopoietic stem cell (HSC) niche is an appealing site for cancer cells because it induces HSC mobilization to occupy the niche [7] and activates myeloid subsets, which perform an immunosuppressive action in the bone microenvironment [8]. Nowadays, the role of the immune system in promoting bone metastases has become more and more evident. This review will focus on different aspects affecting the bone metastatic process and will revise the current available therapeutic options.
Bone is an Attractive Soil for Cancer Cells to Thrive on
BM is constituted by red and yellow marrow. The red marrow is highly vascularized and provides a fertile soil for homing, survival, and proliferation of disseminated tumor cells (DTCs), which often acquired characteristics of stem cells. The yellow marrow contains BM adipocytes, which promote the growth of metastatic tumor cells in the bone [9]. Moreover, BM provides both endosteal and vascular niches, which support HSCs and non-hematopoietic stem cells such as mesenchymal stem cells (MSCs) [10, 11]. Cancer cells recognize chemokine gradients toward BM, similar to the gradient followed by HSCs and leukocytes to migrate to the bone [12]. HSCs migrate to the BM after the activation of CXCL12/CXCR4 axis and osteoblasts (OBs) in BM constitutively express CXCL12, the ligand of CXCR4 [13]. The overexpression of CXCR4 and CXCR7 by breast and prostate cancer cells increases their ability to exit the vascular niche then to colonize bone in mice models [5, 14]. Other than tumor cells, cancer-associated fibroblasts in the tumor microenvironment can also produce CXCL12, which stimulates the release of pro-angiogenic hematopoietic progenitor cells into the circulation [15]. In both breast and non-small cell lung cancer, the CXCR4 inhibition by neutralizing antibodies or pharmacological agents decreases metastatization to bone and lung [16, 17]. Moreover, CXCR4 stimulates the CCL20 production by different tumor cells, further promoting tumor growth and invasion [18, 19]. In particular, CCL20 serum levels were higher in renal cancer patients with bone metastases compared to the non-bone metastatic ones [20], and in multiple myeloma patients, CCL20 overexpression contributes to the increased OC formation and osteolysis [21]. Osteocytes express CXCL16 [22], the ligand of CXCR6, promoting the migration of cancer cells, such as prostate cancer cells, which express this chemokine receptor [23]. Differentiating osteoclasts (OCs) release CCL22 that links CCR4 expressed on breast cancer cells [24], and again OBs express CCL12, which stimulates the tropism of cells expressing CCR7, such as breast cancer cells [12].
Living in the Bone Marrow
Once in the BM, DTCs can die, remain dormant, or proliferate according to the signals received by the local microenvironment [25]. Dormancy signals derive from both endosteal and vascular niches. In endosteal niches, OBs secrete factors such as growth arrest specific 6, a receptor for annexin II [26] and osteopontin, whereas vascular niches release thrombospondin-1 and Notch1 [27], which maintain tumor cells in quiescence. Recently, also the expression of interleukin-6 (IL-6) cytokine leukemia inhibitory factor has been associated to the dormancy phenotype in breast DTCs disseminated to the BM [28]. Conversely, the release in the bone microenvironment of fibronectin, type I collagen, and periostin repress dormancy [29]. After their arrival in BM, HSCs and DTCs compete to endosteal niche since they express cadherins, which allow bonds with OBs residing in these niches [30] and with bone matrix [31, 32]. Indeed, tumor cells express adhesion molecules, able to bind BM stromal cells, releasing angiogenic and bone-resorbing factors that disrupt the normal homeostasis of BM microenvironment leading to bone metastasis [33, 34]. αvβ3 is an integrin expressed by breast and prostate cancer cells, which is particularly important for OC adhesion to bone. Indeed, treatment with non-peptide antagonists of αvβ3 blocked bone colonization [35, 36]. In breast cancer, the vascular-endothelial molecule-1 (VCAM-1) binds α4β7 and α4β1 (VLA-4) integrins on OC precursors with high affinity, causing osteoclastogenesis. α4 or VCAM-1 blocking antibodies effectively inhibit bone metastasis [37]. Further, CD44 is a molecule highly expressed by breast cancer cells, which promotes invasion and adhesion to BM [38]. Breast CSCs express CD44; they can lie in a dormant state in the BM [39] and then directly induce bone metastases [6]. Annexin II is expressed by prostate cancer cells and can link its receptor on OBs promoting the homing in bone [40]. Thus, OBs and OCs both affect the HSC maintenance and mobilization [32].
Dynamic interactions between DTCs and stromal cells in bone cause the release of different molecules which provide a fertile soil for tumor cells, such as transforming growth factor-β (TGF-β), insulin-like growth factors I and II, platelet-derived growth factor, fibroblast growth factor, and bone morphogenetic proteins [41, 42]. Also, the physiological bone remodeling, which is a tightly regulated activity of bone-resorbing OCs and bone-forming OBs, determines the release from the bone matrix of different factors, promoting the growth of cancer cells and/or the outgrowth from dormancy of DTCs [37]. Moreover, physical factors such as acid pH, hypoxia, and high extracellular calcium concentration contribute to tumor cell growth [43]. For instance, the high extracellular Ca2+ concentration present in bone (due to the physiological bone remodeling) can bind to calcium-sensing receptor and stimulate PTH-related peptide in cancer cells, promoting tumor cell proliferation and survival [44, 45]. In breast cancer, it has been shown that tumor cells activate OC precursors, which in turn stimulate dormant DTCs [37]. Tumor cells can secrete prostaglandins, PTH, activated vitamin D, interleukin-6 (IL-6), and tumor necrosis factor (TNF), leading to an increase in receptor activator of nuclear factor NF-kB ligand (RANKL) expression on OBs and BM stromal cells [42], which stimulates the OC number, survival, and activity. Jagged1, a ligand of Notch, is a downstream mediator of the pro-metastatic TGF-β that directly activates OC differentiation and promotes tumor growth stimulating IL-6 production by OBs [46]. Moreover, tumor-derived microvesicles such as exosomes are involved in metastasis formation because they can transfer oncogenic proteins and nucleic acids that modulate the fate of tumor cells and target organs [47,48,49,50].
Interaction Between Immune System and Bone Cells
A basic link between immune system and bone is represented by the axis including the receptor activator of nuclear factor NF-kB ligand (RANKL), its receptor RANK, and the natural decoy receptor osteoprotegerin (OPG). The membrane RANKL is expressed by OBs/stromal cells, whereas the soluble RANKL is secreted by activated T cells [51, 52], whereas the receptor RANK is expressed on OC precursors on tumor cells as well [53]. The serum RANKL to OPG ratio is a critical factor in determining OC activation at bone level, with a high serum RANKL to OPG ratio reflecting up-regulation of osteoclastogenesis [54]. OC precursors, circulating in peripheral blood, derive from the monocyte-macrophage lineage, and they can be recruited in response to pathological or healthy conditions. In patients affected by breast, prostate, and lung cancer with bone metastases, we demonstrated an increase in circulating OC precursors compared to patients without bone metastases and healthy controls [55, 56]. Moreover, in bone metastatic patients, OC precursors differentiate into mature OCs in vitro in the presence of T cells without the addition of M-CSF and RANKL, whereas T-cell depletion results in the absence of OC formation without exogenous stimulation [55]. Literature data from our group and others showed that T cells can directly carry on a modulatory action on OCs, thus regulating bone resorption in bone metastasis [55, 57].
IL-7, a cytokine produced by stromal and T cells at inflammatory sites, is an important mediator of the interactions between T lymphocytes and bone cells [58] other than being the main regulator of B and T lymphopoiesis [59]. IL-7 displays either a positive or negative effect on OCs [60, 61], thus it contributes to the maintenance of a correct bone homeostasis [61, 62]. T cells release IL-7 that in turn promotes osteoclastogenesis by up-regulating T-cell release of RANKL and TNFα [63,64,65]. We demonstrated that in bone metastatic patients, IL-7 serum levels were significantly higher than in non-bone metastatic ones and healthy controls [56, 65, 66]. We also showed in a human-in-mice model of bone metastasis by lung cancer that tumor cells release IL-7, thus they are responsible at least in part for the increased IL-7 serum levels [67]. T cells can also mediate a negative regulation of osteoclastogenesis by inducing CD137, a co-stimulatory member of the TNF receptor [68]. CD137 ligand is expressed on OC precursors and its link to CD137 causes an osteoclastogenesis suppression through the inhibition of OC precursor fusion [68].
Bone Shows a Dampened Immune System Response that Favor Tumor Cells
A relevant factor influencing tumor cell dormancy or growth in bone is represented by the reduced immunoreactivity of bone, likely depending on its function as protector of HSC niches [69, 70]. MSCs support HSCs and interact with bone microenvironment maintaining a correct bone remodeling. MSCs can help the entrance of tumor cells in the bone microenvironment through the production of chemoattractant factors, such as stromal derived factor 1α (SDF-1α/CXCL12) [71, 72]. Thus, tumor cells refuge in bone with mechanisms of quiescence similar to HSCs [25], and they often show a more immunoevasive phenotype than cells in the primary tumor [73], easily escaping immunosurveillance. Bone is characterized by a dampened immune system response, with the failure of both innate and adaptive immune system leading to bone metastasis formation [74, 75].
Commonly, the percentage of activated CD4 and CD8 T cells is low in BM, but these populations have been reported in BM of untreated breast cancer patients, suggesting their protective role against tumor growth in bone [76]. At least in an early phase, T cells try to counteract tumor cell diffusion, for instance by releasing IFNγ after their activation. Indeed, the lack of IFNγ has been related to the increase of bone metastases [77]. Furthermore, the importance of T cells in controlling bone metastases has been shown in a mouse model, where T-cell deficiency reduced the anti-tumor effect of zoledronic acid, which is commonly utilized to treat bone lesions. Indeed the anti-resorptive therapy blocked the bone loss due to tumor, but was ineffective to reduce tumor burden, suggesting that impairment or reduction of T cells affects the efficacy of zoledronic acid [78]. In the era of the immune checkpoint inhibitors, it has been shown in a melanoma mice model that ipilimumab (an antibody blocking the inhibitor signal CTLA4 on T cells) suppressed bone metastases [78], and it has been introduced in clinical practice for the treatment of metastatic melanoma.
Moreover, bone has a large number of immature and suppressor immune cell types, such as T regulatory cells, which have to maintain a balanced immunoreactivity [79], and the immunosuppressive myeloid derived suppressor cells (MDSCs) that stimulate osteoclastogenesis [80]. In breast cancer, infiltrating T reg produce RANKL, promoting OC differentiation, activity, and subsequent bone lesions [81]. On the other side, OCs affect T-cell activity, inducing the activation of CD8 T regulatory cells, which regulate an inappropriate activation of the immune response [82].
Another subset of CD4 T cells promoting bone damage is represented by T helper type 17 (Th17) cells, which are linked to an increased osteoclastogenesis and bone lesions in inflammatory arthritis [83]. Th17 cells release IL-17 and RANKL production [84], which stimulate OC activity. IL-17 is also produced by BM-derived stem cells, promoting tumor growth in the bone [85].
Cancer patients show an increased level of circulating myeloid populations, which help tumor growth and metastatization suppressing innate and adaptive immune response. MDSC expansion is due to the production of different factors, such as granulocyte colony-stimulating factor (G-CSF), TGF-β, and interleukin-1β (IL-1β) by tumor cells. After mobilization, MDSCs move from the BM into the circulation, where they show a strong suppressive function on T-cell-mediated immune response, particularly on CD8+ T cells [86, 87] but also CD4 T and NK cells [78]. In turn, MDSCs stimulate T regs [88] and release many cytokines and angiogenic factors which promote tumor growth in bone, inhibiting T-cell response [78, 89]. In cancer patients and mostly in advanced cancer ones, MDSCs are largely increased, particularly in the circulation of bone metastatic patients. Indeed, MDSCs can rise from 2% up to 25% [80, 90]. Moreover, it has been demonstrated that MDSCs derived from bone metastatic microenvironment can differentiate into mature and functional OCs in vitro [91], and in multiple myeloma they act as OC precursors [92].
Clinical Approach for Treatment of Bone Metastases
Treatment of patients with bone metastases showed a progressive improvement in the last 15 years. Indeed, the survival rate of the patients with bone localizations of solid tumors increased dramatically. Second therapeutic lines on gastrointestinal, prostate, kidney, and lately lung tumors raised the problem to preserve the quality of life of these patients for longer periods of time.
The paramount clinical condition of bone metastasis is pain, and reversibly, bone cancer pain is the most common form of distress for a patient with cancer. Thus, pain reduction and functional preservation remain the mail goal of therapy which, due to the increase life expectancy, must be modified accordingly. The issue of pain control was addressed showing that 45% of patients with cancer accompanied by pain could not be effectively controlled [93]. These observations led to the development of a rat mouse model of femoral cancer pain, and a good animal foundation has been developed for the investigation of the mechanisms of cancer pain in animal models [94]. On clinical grounds, pain from bone metastasis can be controlled by radiotherapy or radioisotopes, pharmacologic therapy (mainly opioids), surgery, bone cement, and novel approaches.
The use of external beam radiotherapy in a single fraction of 8 Gy to treat patients with bone metastases and pain is strongly recommended and still represents the gold standard for local control of bone lesions. Further techniques include an increased radiation dose in order to achieve a radical radiation treatment on oligometastatic patients and the more sophisticated imaging-mediated stereotactic body radiation therapy [95]. It offers the patient a short course of outpatient, non-invasive ablative therapy [96].
The efficacy of radioisotopes for relieving pain has been proven, looking at the reduction of patients’ needs for conventional painkillers, improvements in quality of life, and increased survival. Indeed, there is some evidence that radioisotopes may give pain relief over 1 to 6 months, although the treatment also seems to be associated with adverse effects, notably reduction of leukocytes [97].
Currently, opioids are one of the most effective drugs for cancer pain. More than 80% of patients with bone metastasis need to use opioids to improve or control pain. However, the associated side effects of opioid drugs (tolerance, addiction, excitement, drowsiness, constipation, nausea, vomiting, and respiratory depression) limit further application [98].
High dose of bisphosphonates, such as zoledronic acid, was introduced as a treatment for bone metastasis and prevention of its complications. Decreased progression of the disease in the bone was proven, and eventually, according to various studies, nesting of tumor cells in the bone was prevented [99].
Bone-targeting therapy reduces skeletal-related events associated to bone metastases in patients with solid tumors and multiple myeloma [100,101,102]. In particular, the introduction of denosumab, a fully human antibody that specifically binds to RANKL in a reversible way, without interfering with other TNF ligands, resulted effective in preventing the homing of RANK-expressing tumor cells to bone and inhibiting the formation of bone lesions [103, 104]. Denosumab inhibited bone resorption in patients refractory to bisphosphonate therapy [105] and was superior to zoledronic acid in preventing SREs in patients with bone metastases from advanced cancer [103, 106].
The orthopedic surgeon has a leading role in pain control and in the prevention of SREs, consisting primarily in fracture of the affected bone, spinal cord compression, and hypercalcemia, all of which may profoundly impair the quality of life of patients [107]. All patients at risk of a long bone fracture should therefore be assessed to consider prophylactic surgery. Orthopedic surgeons had learned that solitary bone metastases, when surgically removable, had to be treated with oncologic rigor, preserving margins, considering that the surgical treatment needed a longer half life and had to provide function and durability for patients that could heal from cancer. Next, they further learned how to treat multiple metastatic patients keeping in mind that pathologic fractures never heal and therefore the surgical treatment had to provide stability for as long as the life expectancy of the patients. The surgical orthopedic solutions had to be modified according to the increased survival rate of metastatic patients. For instance, wide resection prostheses started to be used in upper and lower limbs, nail quality increased for intramedullary nailing of long bone metastases, and carbon fiber composite nails were recently introduced allowing better imaging after nailing and lack of electron scattering during post-surgical radiotherapy [108]. Particularly new light polymerized nails were recently introduced for upper limbs and are on trials on lower limb metastases [109]. Their peculiar characteristics allow mini-invasive surgery and immediate control of the stability of the bone especially in rotational motion due to the on-site polymerization of the nail itself. They also offer a perfect visibility of the bone after nailing, being RX translucent and MRI compatible. They also represent a perfect fixation system for further radiotherapy. The increased life expectancy of bone metastatic patients represented a new challenge for spine surgeons as well. Indeed, the indications for surgical stabilization of vertebral lesions increased and, in selected cases, partial or complete vertebrectomy of the affected vertebral body was performed [110]. In bone metastasis of the spine, the radiotherapy continues to be the most reliable treatment, but vertebroplasty became a new and rapidly growing method for stabilization of lytic lesions that could be performed on outpatients and on multiple sites, avoiding corsets, allowing pain control, preservation of function, and therefore quality of life [111]. Another option of imaging guided non-invasive treatment for bone localization of tumor cells is thermal ablation, which has been used for oncologic patients for over 20 years with limited but effective results, especially in non-weight-bearing segments [112]. Electrochemotherapy is under evaluation in many multicenter studies. It consists of electroporation of the affected bone segment using electrodes driven into bone under imaging control. The electroporated bone segment, together with the tumor tissue, then becomes susceptible to bleomycin i.v. infusion. Preliminary results are promising for palliation treatment [113].
Conclusions
A relentless research effort to explain the biological insights of the interaction between DTCs and bone has led to a clearer view of the bone metastatic process. We believe we are active spectators of a turning point in metastatic patients’ treatment from basic knowledge to patients’ bed. Examples of this transition are represented by many novel agents able to prevent or block bone metastases. One is denosumab, which is currently in clinical practice for bone metastases in solid tumors, and another is anti-DKK1 antibody, which is in clinical trials. On clinical grounds, the awareness of novel concepts and the availability of new treatments lead to a new philosophy of care for bone metastases which is more effective, decreases SREs, and improves the life quality of these patients.
References
Kang Y, Pantel K. Tumor cell dissemination: emerging biological insights from animal models and cancer patients. Cancer Cell. 2013;23(5):573–81.
Valastyan S, Weinberg RA. Tumor metastasis: molecular insights and evolving paradigms. Cell. 2011;147(2):275–92.
Coleman RE. Management of bone metastases. Oncologist. 2000;5(6):463–70.
Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001;27(3):165–76.
Kang Y, Siegel PM, Shu W, Drobnjak M, Kakonen SM, Cordon-Cardo C, et al. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell. 2003;3(6):537–49.
D'Amico L, Patane S, Grange C, Bussolati B, Isella C, Fontani L, et al. Primary breast cancer stem-like cells metastasise to bone, switch phenotype and acquire a bone tropism signature. Br J Cancer. 2013;108(12):2525–36.
Shiozawa Y, Pedersen EA, Havens AM, Jung Y, Mishra A, Joseph J, et al. Human prostate cancer metastases target the hematopoietic stem cell niche to establish footholds in mouse bone marrow. J Clin Invest. 2011;121(4):1298–312.
Giles AJ, Reid CM, Evans JD, Murgai M, Vicioso Y, Highfill SL, et al. Activation of hematopoietic stem/progenitor cells promotes immunosuppression within the pre-metastatic niche. Cancer Res. 2016;76(6):1335–47.
Herroon MK, Rajagurubandara E, Hardaway AL, Powell K, Turchick A, Feldmann D, et al. Bone marrow adipocytes promote tumor growth in bone via FABP4-dependent mechanisms. Oncotarget. 2013;4(11):2108–23.
Shiozawa Y, Eber MR, Berry JE, Taichman RS. Bone marrow as a metastatic niche for disseminated tumor cells from solid tumors. Bonekey Rep. 2015;4:689.
Azizidoost S, Babashah S, Rahim F, Shahjahani M, Saki N. Bone marrow neoplastic niche in leukemia. Hematology. 2014 Jun;19(4):232–8.
Muller A, Homey B, Soto H, Ge N, Catron D, Buchanan ME, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410(6824):50–6.
Broxmeyer HE, Orschell CM, Clapp DW, Hangoc G, Cooper S, Plett PA, et al. Rapid mobilization of murine and human hematopoietic stem and progenitor cells with AMD 3100, a CXCR4 antagonist. J Exp Med. 2005;201(8):1307–18.
Wang J, Shiozawa Y, Wang Y, Jung Y, Pienta KJ, Mehra R, et al. The role of CXCR7/RDC1 as a chemokine receptor for CXCL12/SDF-1 in prostate cancer. J Biol Chem. 2008;283(7):4283–94.
Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R, et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121(3):335–48.
Richert MM, Vaidya KS, Mills CN, Wong D, Korz W, Hurst DR, et al. Inhibition of CXCR4 by CTCE-9908 inhibits breast cancer metastasis to lung and bone. Oncol Rep. 2009;21(3):761–7.
Bertolini G, D'Amico L, Moro M, Landoni E, Perego P, Miceli R, et al. Microenvironment-modulated metastatic CD133+/CXCR4+/EpCAM-lung cancer-initiating cells sustain tumor dissemination and correlate with poor prognosis. Cancer Res. 2015;75(17):3636–49.
Beider K, Abraham M, Begin M, Wald H, Weiss ID, Wald O, et al. Interaction between CXCR4 and CCL20 pathways regulates tumor growth. PLoS One. 2009;4(4):e5125.
Schutyser E, Struyf S, Van Damme J. The CC chemokine CCL20 and its receptor CCR6. Cytokine Growth Factor Rev. 2003;14(5):409–26.
D'Amico L, Belisario D, Migliardi G, Grange C, Bussolati B, D'Amelio P, et al. C-met inhibition blocks bone metastasis development induced by renal cancer stem cells. Oncotarget. 2016;7(29):45525–37.
Giuliani N, Lisignoli G, Colla S, Lazzaretti M, Storti P, Mancini C, et al. CC-chemokine ligand 20/macrophage inflammatory protein-3alpha and CC-chemokine receptor 6 are overexpressed in myeloma microenvironment related to osteolytic bone lesions. Cancer Res. 2008;68(16):6840–50.
Hu W, Zhen X, Xiong B, Wang B, Zhang W, Zhou W. CXCR6 is expressed in human prostate cancer in vivo and is involved in the in vitro invasion of PC3 and LNCap cells. Cancer Sci. 2008;99(7):1362–9.
Ha HK, Lee W, Park HJ, Lee SD, Lee JZ, Chung MK. Clinical significance of CXCL16/CXCR6 expression in patients with prostate cancer. Mol Med Rep. 2011;4(3):419–24.
Nakamura ES, Koizumi K, Kobayashi M, Saitoh Y, Arita Y, Nakayama T, et al. RANKL-induced CCL22/macrophage-derived chemokine produced from osteoclasts potentially promotes the bone metastasis of lung cancer expressing its receptor CCR4. Clin Exp Metastasis. 2006;23(1):9–18.
Li L, Bhatia R. Stem cell quiescence. Clin Cancer Res. 2011;17(15):4936–41.
Shiozawa Y, Pedersen EA, Patel LR, Ziegler AM, Havens AM, Jung Y, et al. GAS6/AXL axis regulates prostate cancer invasion, proliferation, and survival in the bone marrow niche. Neoplasia. 2010;12(2):116–27.
Ghajar CM, Peinado H, Mori H, Matei IR, Evason KJ, Brazier H, et al. The perivascular niche regulates breast tumour dormancy. Nat Cell Biol. 2013;15(7):807–17.
Johnson RW, Finger EC, Olcina MM, Vilalta M, Aguilera T, Miao Y, et al. Induction of LIFR confers a dormancy phenotype in breast cancer cells disseminated to the bone marrow. Nat Cell Biol. 2016;18(10):1078–89.
Malanchi I, Santamaria-Martinez A, Susanto E, Peng H, Lehr HA, Delaloye JF, et al. Interactions between cancer stem cells and their niche govern metastatic colonization. Nature. 2011;481(7379):85–9.
Wang H, Yu C, Gao X, Welte T, Muscarella AM, Tian L, et al. The osteogenic niche promotes early-stage bone colonization of disseminated breast cancer cells. Cancer Cell. 2015;27(2):193–210.
Calvi LM, Adams GB, Weibrecht KW, Weber JM, Olson DP, Knight MC, et al. Osteoblastic cells regulate the haematopoietic stem cell niche. Nature. 2003;425(6960):841–6.
Zhang J, Niu C, Ye L, Huang H, He X, Tong WG, et al. Identification of the haematopoietic stem cell niche and control of the niche size. Nature. 2003;425(6960):836–41.
Suva LJ, Washam C, Nicholas RW, Griffin RJ. Bone metastasis: mechanisms and therapeutic opportunities. Nat Rev Endocrinol. 2011;7(4):208–18.
Chiang AC, Massague J. Molecular basis of metastasis. N Engl J Med. 2008;359(26):2814–23.
Pecheur I, Peyruchaud O, Serre CM, Guglielmi J, Voland C, Bourre F, et al. Integrin alpha (v)beta3 expression confers on tumor cells a greater propensity to metastasize to bone. FASEB J. 2002;16(10):1266–8.
Sung V, Stubbs JT 3rd, Fisher L, Aaron AD, Thompson EW. Bone sialoprotein supports breast cancer cell adhesion proliferation and migration through differential usage of the alpha (v)beta3 and alpha (v)beta5 integrins. J Cell Physiol. 1998;176(3):482–94.
Lu X, Mu E, Wei Y, Riethdorf S, Yang Q, Yuan M, et al. VCAM-1 promotes osteolytic expansion of indolent bone micrometastasis of breast cancer by engaging alpha4beta1-positive osteoclast progenitors. Cancer Cell. 2011;20(6):701–14.
Reuben JM, Lee BN, Gao H, Cohen EN, Mego M, Giordano A, et al. Primary breast cancer patients with high risk clinicopathologic features have high percentages of bone marrow epithelial cells with ALDH activity and CD44(+)CD24lo cancer stem cell phenotype. Eur J Cancer. 2011;47(10):1527–36.
Patel SA, Ramkissoon SH, Bryan M, Pliner LF, Dontu G, Patel PS, et al. Delineation of breast cancer cell hierarchy identifies the subset responsible for dormancy. Sci Rep. 2012;2:906.
Shiozawa Y, Havens AM, Jung Y, Ziegler AM, Pedersen EA, Wang J, et al. Annexin II/annexin II receptor axis regulates adhesion, migration, homing, and growth of prostate cancer. J Cell Biochem. 2008;105(2):370–80.
Bussard KM, Gay CV, Mastro AM. The bone microenvironment in metastasis; what is special about bone? Cancer Metastasis Rev. 2008;27(1):41–55.
Roodman GD. Mechanisms of bone metastasis. N Engl J Med. 2004;350(16):1655–64.
Yoneda T, Hiraga T. Crosstalk between cancer cells and bone microenvironment in bone metastasis. Biochem Biophys Res Commun. 2005;328(3):679–87.
Sanders JL, Chattopadhyay N, Kifor O, Yamaguchi T, Butters RR, Brown EM. Extracellular calcium-sensing receptor expression and its potential role in regulating parathyroid hormone-related peptide secretion in human breast cancer cell lines. Endocrinology. 2000;141(12):4357–64.
Kim W, Takyar FM, Swan K, Jeong J, Van Houten J, Sullivan C, et al. Calcium-sensing receptor promotes breast cancer by stimulating intracrine actions of parathyroid hormone-related protein. Cancer Res. 2016;76(18):5348–60.
Sethi N, Dai X, Winter CG, Kang Y. Tumor-derived JAGGED1 promotes osteolytic bone metastasis of breast cancer by engaging notch signaling in bone cells. Cancer Cell. 2011;19(2):192–205.
Dos Anjos PB, Andres Cordero da Luz F, Socorro Faria S, Peixoto Ferreira de Souza L, Cristina Brigido Tavares P, Alonso Goulart V, et al. The multifaceted role of extracellular vesicles in metastasis: priming the soil for seeding. Int J Cancer. 2017.
Bigagli E, Luceri C, Guasti D, Cinci L. Exosomes secreted from human colon cancer cells influence the adhesion of neighboring metastatic cells: role of micro RNA-210. Cancer Biol Ther. 2016;11:1–8.
Wang Z, von Au A, Schnolzer M, Hackert T, Zoller M. CD44v6-competent tumor exosomes promote motility, invasion and cancer-initiating cell marker expression in pancreatic and colorectal cancer cells. Oncotarget. 2016;7(34):55409–36.
McAllister SS, Weinberg RA. The tumour-induced systemic environment as a critical regulator of cancer progression and metastasis. Nat Cell Biol. 2014;16(8):717–27.
Kostenuik PJ, Shalhoub V. Osteoprotegerin: a physiological and pharmacological inhibitor of bone resorption. Curr Pharm Des. 2001;7(8):613–35.
Hofbauer LC, Kuhne CA, Viereck V. The OPG/RANKL/RANK system in metabolic bone diseases. J Musculoskelet Neuronal Interact. 2004;4(3):268–75.
Santini D, Perrone G, Roato I, Godio L, Pantano F, Grasso D, et al. Expression pattern of receptor activator of NFkappaB (RANK) in a series of primary solid tumors and related bone metastases. J Cell Physiol. 2011;226(3):780–4.
Hofbauer LC, Khosla S, Dunstan CR, Lacey DL, Boyle WJ, Riggs BL. The roles of osteoprotegerin and osteoprotegerin ligand in the paracrine regulation of bone resorption. J Bone Miner Res. 2000;15(1):2–12.
Roato I, Grano M, Brunetti G, Colucci S, Mussa A, Bertetto O, et al. Mechanisms of spontaneous osteoclastogenesis in cancer with bone involvement. FASEB J. 2005;19(2):228–30.
Roato I, Gorassini E, Buffoni L, Lyberis P, Ruffini E, Bonello L, et al. Spontaneous osteoclastogenesis is a predictive factor for bone metastases from non-small cell lung cancer. Lung Cancer. 2008;61(1):109–16.
Colucci S, Brunetti G, Rizzi R, Zonno A, Mori G, Colaianni G, et al. T cells support osteoclastogenesis in an in vitro model derived from human multiple myeloma bone disease: the role of the OPG/TRAIL interaction. Blood. 2004;104(12):3722–30.
Appasamy PM. Biological and clinical implications of interleukin-7 and lymphopoiesis. Cytokines Cell Mol Ther. 1999;5(1):25–39.
Namen AE, Lupton S, Hjerrild K, Wignall J, Mochizuki DY, Schmierer A, et al. Stimulation of B-cell progenitors by cloned murine interleukin-7. Nature. 1988;333(6173):571–3.
Lee SK, Kalinowski JF, Jastrzebski SL, Puddington L, Lorenzo JA. Interleukin-7 is a direct inhibitor of in vitro osteoclastogenesis. Endocrinology. 2003;144(8):3524–31.
Miyaura C, Onoe Y, Inada M, Maki K, Ikuta K, Ito M, et al. Increased B-lymphopoiesis by interleukin 7 induces bone loss in mice with intact ovarian function: similarity to estrogen deficiency. Proc Natl Acad Sci U S A. 1997;94(17):9360–5.
Weitzmann MN, Roggia C, Toraldo G, Weitzmann L, Pacifici R. Increased production of IL-7 uncouples bone formation from bone resorption during estrogen deficiency. J Clin Invest. 2002;110(11):1643–50.
Toraldo G, Roggia C, Qian WP, Pacifici R, Weitzmann MN. IL-7 induces bone loss in vivo by induction of receptor activator of nuclear factor kappa B ligand and tumor necrosis factor alpha from T cells. Proc Natl Acad Sci U S A. 2003;100(1):125–30.
Giuliani N, Colla S, Sala R, Moroni M, Lazzaretti M, La Monica S, et al. Human myeloma cells stimulate the receptor activator of nuclear factor-kappa B ligand (RANKL) in T lymphocytes: a potential role in multiple myeloma bone disease. Blood. 2002;100(13):4615–21.
Roato I, Brunetti G, Gorassini E, Grano M, Colucci S, Bonello L, et al. IL-7 up-regulates TNF-alpha-dependent osteoclastogenesis in patients affected by solid tumor. PLoS One. 2006;1:e124.
Roato I, Gorassini E, Brunetti G, Grano M, Ciuffreda L, Mussa A, et al. IL-7 modulates osteoclastogenesis in patients affected by solid tumors. Ann N Y Acad Sci. 2007;1117:377–84.
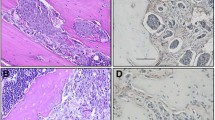
Roato I, Caldo D, Godio L, D'Amico L, Giannoni P, Morello E, et al. Bone invading NSCLC cells produce IL-7: mice model and human histologic data. BMC Cancer. 2010;10:12.
Senthilkumar R, Lee HW. CD137L- and RANKL-mediated reverse signals inhibit osteoclastogenesis and T lymphocyte proliferation. Immunobiology. 2009;214(2):153–61.
Glennie S, Soeiro I, Dyson PJ, Lam EW, Dazzi F. Bone marrow mesenchymal stem cells induce division arrest anergy of activated T cells. Blood. 2005;105(7):2821–7.
Baschuk N, Rautela J, Parker BS. Bone specific immunity and its impact on metastasis. Bonekey Rep. 2015;4:665.
Corcoran KE, Trzaska KA, Fernandes H, Bryan M, Taborga M, Srinivas V, et al. Mesenchymal stem cells in early entry of breast cancer into bone marrow. PLoS One. 2008;3(6):e2563.
Zhang XH, Jin X, Malladi S, Zou Y, Wen YH, Brogi E, et al. Selection of bone metastasis seeds by mesenchymal signals in the primary tumor stroma. Cell. 2013;154(5):1060–73.
Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21(2):137–48.
Bidwell BN, Slaney CY, Withana NP, Forster S, Cao Y, Loi S, et al. Silencing of Irf 7 pathways in breast cancer cells promotes bone metastasis through immune escape. Nat Med. 2012;18(8):1224–31.
Kudo-Saito C, Fuwa T, Murakami K, Kawakami Y. Targeting FSTL1 prevents tumor bone metastasis and consequent immune dysfunction. Cancer Res. 2013;73(20):6185–93.
Feuerer M, Rocha M, Bai L, Umansky V, Solomayer EF, Bastert G, et al. Enrichment of memory T cells and other profound immunological changes in the bone marrow from untreated breast cancer patients. Int J Cancer. 2001;92(1):96–105.
Xu Z, Hurchla MA, Deng H, Uluckan O, Bu F, Berdy A, et al. Interferon-gamma targets cancer cells and osteoclasts to prevent tumor-associated bone loss and bone metastases. J Biol Chem. 2009;284(7):4658–66.
Zhang K, Kim S, Cremasco V, Hirbe AC, Collins L, Piwnica-Worms D, et al. CD8+ T cells regulate bone tumor burden independent of osteoclast resorption. Cancer Res. 2011;71(14):4799–808.
Zou L, Barnett B, Safah H, Larussa VF, Evdemon-Hogan M, Mottram P, et al. Bone marrow is a reservoir for CD4+CD25+ regulatory T cells that traffic through CXCL12/CXCR4 signals. Cancer Res. 2004;64(22):8451–5.
Almand B, Clark JI, Nikitina E, van Beynen J, English NR, Knight SC, et al. Increased production of immature myeloid cells in cancer patients: a mechanism of immunosuppression in cancer. J Immunol. 2001;166(1):678–89.
Tan W, Zhang W, Strasner A, Grivennikov S, Cheng JQ, Hoffman RM, et al. Tumour-infiltrating regulatory T cells stimulate mammary cancer metastasis through RANKL-RANK signalling. Nature. 2011;470(7335):548–53.
Kiesel JR, Buchwald ZS, Aurora R. Cross-presentation by osteoclasts induces FoxP3 in CD8+ T cells. J Immunol. 2009;182(9):5477–87.
Roy LD, Ghosh S, Pathangey LB, Tinder TL, Gruber HE, Mukherjee P. Collagen induced arthritis increases secondary metastasis in MMTV-PyV MT mouse model of mammary cancer. BMC Cancer. 2011;11:365.
Okamoto K, Takayanagi H. Regulation of bone by the adaptive immune system in arthritis. Arthritis Res Ther. 2011;13(3):219.
Goldstein RH, Reagan MR, Anderson K, Kaplan DL, Rosenblatt M. Human bone marrow-derived MSCs can home to orthotopic breast cancer tumors and promote bone metastasis. Cancer Res. 2010;70(24):10044–50.
Bronte V, Apolloni E, Cabrelle A, Ronca R, Serafini P, Zamboni P, et al. Identification of a CD11b(+)/gr-1(+)/CD31(+) myeloid progenitor capable of activating or suppressing CD8(+) T cells. Blood. 2000;96(12):3838–46.
Kusmartsev S, Nagaraj S, Gabrilovich DI. Tumor-associated CD8+ T cell tolerance induced by bone marrow-derived immature myeloid cells. J Immunol. 2005;175(7):4583–92.
Kusmartsev S, Gabrilovich DI. Inhibition of myeloid cell differentiation in cancer: the role of reactive oxygen species. J Leukoc Biol. 2003;74(2):186–96.
Kusmartsev S, Gabrilovich DI. Role of immature myeloid cells in mechanisms of immune evasion in cancer. Cancer Immunol Immunother. 2006;55(3):237–45.
Zea AH, Rodriguez PC, Atkins MB, Hernandez C, Signoretti S, Zabaleta J, et al. Arginase-producing myeloid suppressor cells in renal cell carcinoma patients: a mechanism of tumor evasion. Cancer Res. 2005;65(8):3044–8.
Sawant A, Deshane J, Jules J, Lee CM, Harris BA, Feng X, et al. Myeloid-derived suppressor cells function as novel osteoclast progenitors enhancing bone loss in breast cancer. Cancer Res. 2013;73(2):672–82.
Zhuang J, Zhang J, Lwin ST, Edwards JR, Edwards CM, Mundy GR, et al. Osteoclasts in multiple myeloma are derived from gr-1+CD11b+myeloid-derived suppressor cells. PLoS One. 2012;7(11):e48871.
Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S. Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology. Pain. 2001;93(3):247–57.
Portenoy RK, Lesage P. Management of cancer pain. Lancet. 1999;353(9165):1695–700.
Alongi F, Arcangeli S, Filippi AR, Ricardi U, Scorsetti M. Review and uses of stereotactic body radiation therapy for oligometastases. Oncologist. 2012;17(8):1100–7.
Yu HH, Hoffe SE. Beyond the conventional role of external-beam radiation therapy for skeletal metastases: new technologies and stereotactic directions. Cancer Control. 2012;19(2):129–36.
Das T, Banerjee S. Radiopharmaceuticals for metastatic bone pain palliation: available options in the clinical domain and their comparisons. Clin Exp Metastasis. 2017;34(1):1–10.
Buga S, Sarria JE. The management of pain in metastatic bone disease. Cancer Control. 2012;19(2):154–66.
Beuzeboc P, Scholl S. Prevention of bone metastases in breast cancer patients. Therapeutic perspectives. J Clin Med. 2014;3(2):521–36.
Alibhai SM, Zukotynski K, Walker-Dilks C, Emmenegger U, Finelli A, Morgan SC, et al. Bone Health and Bone-targeted Therapies for Prostate Cancer: a Programme in Evidence-based Care—Cancer Care Ontario Clinical Practice Guideline. Clin Oncol (R Coll Radiol). 2017.
Henry DH, Costa L, Goldwasser F, Hirsh V, Hungria V, Prausova J, et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol. 2011;29(9):1125–32.
Fizazi K, Carducci M, Smith M, Damiao R, Brown J, Karsh L, et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet. 2011;377(9768):813–22.
Lipton A, Fizazi K, Stopeck AT, Henry DH, Smith MR, Shore N, et al. Effect of denosumab versus zoledronic acid in preventing skeletal-related events in patients with bone metastases by baseline characteristics. Eur J Cancer. 2016;53:75–83.
Lipton A, Steger GG, Figueroa J, Alvarado C, Solal-Celigny P, Body JJ, et al. Randomized active-controlled phase II study of denosumab efficacy and safety in patients with breast cancer-related bone metastases. J Clin Oncol. 2007;25(28):4431–7.
Body JJ, Facon T, Coleman RE, Lipton A, Geurs F, Fan M, et al. A study of the biological receptor activator of nuclear factor-kappa B ligand inhibitor, denosumab, in patients with multiple myeloma or bone metastases from breast cancer. Clin Cancer Res. 2006;12(4):1221–8.
Lipton A, Fizazi K, Stopeck AT, Henry DH, Brown JE, Yardley DA, et al. Superiority of denosumab to zoledronic acid for prevention of skeletal-related events: a combined analysis of 3 pivotal, randomised, phase 3 trials. Eur J Cancer. 2012;48(16):3082–92.
Molloy AP, O'Toole GC. Orthopaedic perspective on bone metastasis. World J Orthop. 2013;4(3):114–9.
Zimel MN, Hwang S, Riedel ER, Healey JH. Carbon fiber intramedullary nails reduce artifact in postoperative advanced imaging. Skelet Radiol. 2015;44(9):1317–25.
Hagenaars T, Van Oijen GW, Roerdink WH, Vegt PA, Vroemen JP, Verhofstad MH, et al. Functional recovery after treatment of extra-articular distal radius fractures in the elderly using the Illumin Oss (R) system (IO-wrist); a multicenter prospective observational study. BMC Musculoskelet Disord. 2016;17:235.
Li H, Gasbarrini A, Cappuccio M, Terzi S, Paderni S, Mirabile L, et al. Outcome of excisional surgeries for the patients with spinal metastases. Eur Spine J. 2009;18(10):1423–30.
Vertebral Augmentation Involving Vertebroplasty or Kyphoplasty for Cancer-Related Vertebral Compression Fractures. A systematic review. Ont Health Technol Assess Ser. 2016;16(11):1–202.
Huisman M, ter Haar G, Napoli A, Hananel A, Ghanouni P, Lovey G, et al. International consensus on use of focused ultrasound for painful bone metastases: current status and future directions. Int J Hyperth. 2015;31(3):251–9.
Bianchi G, Campanacci L, Ronchetti M, Donati D. Electrochemotherapy in the treatment of bone metastases: a phase II trial. World J Surg. 2016;40(12):3088–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by Cassa di Risparmio di Torino (CRT) and Compagnia di San Paolo Foundations and by Fondazione Ricerca Molinette ONLUS.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Roato, I., Massè, A., Piana, R. et al. Bone Metastasis from Solid Tumors: Biologic and Clinical State of the Art. Clinic Rev Bone Miner Metab 15, 115–122 (2017). https://doi.org/10.1007/s12018-017-9233-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12018-017-9233-9