Abstract
Osteoclasts require coordinated co-stimulation by several signaling pathways to initiate and regulate their cellular differentiation. Receptor activator for NF-κB ligand (RANKL or TNFSF11), a tumor necrosis factor (TNF) superfamily member, is the master cytokine required for osteoclastogenesis with essential co-stimulatory signals mediated by immunoreceptor tyrosine-based activation motif (ITAM)-signaling adaptors, DNAX-associated protein 12 kDa size (DAP12) and FcεRI gamma chain (FcRγ). The ITAM-signaling adaptors do not have an extracellular ligand-binding domain and, therefore, must pair with ligand-binding immunoreceptors to interact with their extracellular environment. DAP12 pairs with a number of different immunoreceptors including triggering receptor expressed on myeloid cells 2 (TREM2), myeloid DAP12-associated lectin (MDL-1), and sialic acid-binding immunoglobulin-type lectin 15 (Siglec-15); while FcRγ pairs with a different set of receptors including osteoclast-specific activating receptor (OSCAR), paired immunoglobulin receptor A (PIR-A), and Fc receptors. The ligands for many of these receptors in the bone microenvironment remain unknown. Here, we will review immunoreceptors known to pair with either DAP12 or FcRγ that have been shown to regulate osteoclastogenesis. Co-stimulation and the effects of ITAM-signaling have turned out to be complex, and now include paradoxical findings that ITAM-signaling adaptor-associated receptors can inhibit osteoclastogenesis and immunoreceptor tyrosine-based inhibitory motif (ITIM) receptors can promote osteoclastogenesis. Thus, co-stimulation of osteoclastogenesis continues to reveal additional complexities that are important in the regulatory mechanisms that seek to maintain bone homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Immunoreceptor Regulation of Osteoclasts
Osteoclast differentiation is a highly regulated process, meant to ensure that osteoclasts are formed on bone surfaces and specifically respond to bone remodeling stimuli [1, 2]. Osteoclast differentiation and activity must be closely coupled to processes of bone formation and require cell-cell communication through both intercellular interactions and soluble cytokines [3]. Like many immune cells, osteoclasts require coordinated co-stimulation by several signaling pathways to initiate cellular differentiation at defined places and times. Receptor activator for NF-κB ligand (RANKL or TNFSF11), a tumor necrosis factor (TNF) superfamily member, is the essential cytokine required for osteoclastogenesis [4]. The critical co-stimulatory signals are directed by immunoreceptors that signal through immunoreceptor tyrosine-based activation motif (ITAM)-signaling adaptors, DNAX-associated protein 12 kDa size (DAP12) and FcεRI gamma chain (FcRγ) [5, 6]. ITAM-signaling adaptors initiate a calcium flux that is necessary for nuclear factor of activated T cells, cytoplasmic, calcineurin-dependent 1 (NFATc1) activation to drive the differentiation process [7]. NFATc1 is known as the master transcriptional regulator required for osteoclastogenesis [7]. While a number of ITAM-signaling adaptor-associated receptors have been identified as regulators of osteoclastogenesis, the exact roles of each of these receptors in basal or pathological bone remodeling remain incompletely understood [8]. In addition, at specific sites and/or conditions, osteoclastogenesis can be initiated in the absence of the ITAM-signaling adaptors suggesting that alternative co-stimulatory pathways can be utilized [9].
The role of these immunoreceptors in innate immune cells is primarily to enable or limit the response of cells to microenvironmental change [10]. However, in the bone environment, we have limited understanding of the receptors utilized by osteoclasts to respond and the ligands that are sensed. Here we review immunoreceptors that have been identified to activate or inhibit osteoclastogenesis and discuss their effects on bone homeostasis. While the list of potential co-stimulatory receptors is likely not complete, we have learned that for osteoclasts, like other innate cells, it is the combined input of arrays of receptors that fine-tune the differentiation and function of these unique cells to carry out bone resorption.
Co-stimulation by ITAM-Signaling Adaptor-Associated Immunoreceptors
The evidence that receptor activator for NF-κB (RANK) requires a co-stimulatory signal to initiate osteoclastogenesis was first demonstrated by examining mice deficient in DAP12 and the FcRγ chains [5, 6]. These ITAM-signaling adaptors present in myeloid cells are known to contain immunoreceptor tyrosine-based activation motifs (ITAMs) that initiate a tyrosine kinase-based signaling cascade. The finding that mice deficient in both ITAM-signaling adaptors are severely osteopetrotic, despite the presence of intact RANK and macrophage colony-stimulating factor (M-CSF) signaling pathways, serves as the critical evidence for the requirement for ITAM co-stimulation during osteoclastogenesis. Mice deficient in both the DAP12 and the FcRγ ITAM-signaling adaptors are unable to form osteoclasts in vitro or in vivo [5, 6]. Koga et al. proposed the model of co-stimulation in osteoclastogenesis in which ITAM signals are required to cooperate with RANK signals to induce the master transcription factor for osteoclastogenesis, NFATc1 [5, 7].
The ITAM-signaling adaptors do not have an extracellular ligand-binding domain and are known to pair with a number of different receptors through paired charged residues in their transmembrane domains [11] (Fig. 1). Several immunoreceptors that pair with either DAP12 or FcRγ have been identified as co-stimulatory molecules for RANKL and while they share the ability to stimulate osteoclastogenesis, their expression is differentially regulated and responsive to distinct stimuli [2, 12]. Ligands identified for some of these receptors are also differentially regulated, although most stimulatory ligands in the bone microenvironment are not well understood. In combination, these regulatory mechanisms serve to locally modulate osteoclastogenesis and maintain bone homeostasis. ITAM-signaling adaptor-associated receptors in immune cells often activate cellular differentiation or function which can be inhibited by related receptors with immunoreceptors tyrosine-based inhibitory motif (ITIM)-signaling domains. It was initially thought that the balance between ITAM and ITIM receptor expression might be the primary means to regulate co-stimulation during osteoclastogenesis, However, co-stimulation and the effects of ITAM and ITIM signaling have turned out to be much more complex.
ITAM-signaling adaptor-associated immunoreceptors. a DAP12-associated receptors TREM2 and MDL-1. TREM2 has been shown to interact with bacteria, dextran sulfate, and HSP60 as ligands. Dengue virus is a ligand for MDL-1. b FcRγ-associated receptor PIR-A interacts with MHC class I ligands on cell surfaces. OSCAR is also an FcRγ-associated receptor, and collagen fragments are functional ligands for OSCAR
DAP12-Associated Receptors
DAP12 was originally identified in natural killer (NK) cells and some lymphocytes, was found to be expressed in myeloid cells, including osteoclast precursors, and became of significant interest in osteoclasts due to the consequences of DAP12 loss-of-function mutations in humans [13]. The rare disorder of Nasu-Hakola disease or polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy (PLOSL) is a recessive genetic disorder characterized by rapidly progressive dementia with large bony cysts, osteopenia, and early degenerative arthritis in the wrists and ankles. Patients with PLOSL have either functional deficiency of DAP12 or a DAP12-associated receptor, triggering receptor expressed on myeloid cells-2 (TREM2) [13]. Peripheral blood mononuclear cells isolated from PLOSL patients (DAP12- or TREM2-deficient humans) fail to differentiate normally into osteoclasts when stimulated with RANKL and M-CSF [14, 15]. Instead, cells from PLOSL patients show inefficient and delayed differentiation of osteoclasts with a remarkably reduced bone resorption capability in vitro [14, 15]. DAP12−/− mice show a mild increase in bone mass in vivo while DAP12−/− osteoclasts (OC) have defects in cytoskeletal organization with impaired formation of multinucleated OC and impaired resorption [16–20]. Interestingly, DAP12−/− mice have recently been shown to have impaired fracture healing, suggesting a role for DAP12 in the inflammatory and bone regeneration response of fracture repair [21]. DAP12 pairs with a number of different immunoreceptors in myeloid cells, and a few of these individual receptors have been examined in osteoclastogenesis. While TREM2 is the DAP12-associated receptor of importance in the PLOSL phenotype, it is not the only DAP12-associated receptor that regulates osteoclastogenesis.
TREM2
Due to its known role in PLOSL, TREM2 was the first DAP12-associated receptor examined in osteoclasts. TREM2 has also been studied in other immune cells and interestingly plays dual roles in immune responses. While TREM2 stimulates dendritic cell differentiation [22], it also inhibits inflammatory cytokine production by macrophages and dendritic cells in response to TLR (toll-like receptor) stimulation by lipopolysaccharide (LPS) or CpG DNA [23, 24]. TREM2 cross-linking on mouse osteoclasts inhibits resorption while promoting multinucleation, migration, and osteoclast differentiation [25]. While TREM2 cross-linking on mouse osteoclasts leads to Syk phosphorylation and osteoclast differentiation [25], TREM2 cross-linking also to lead to association of the SH2-domain inositol phosphatase (SHIP-1) with DAP12, which leads to inhibitory signals [26]. TREM2 also associates with DNAX-associated protein 10 kDa (DAP10) leading to strong activation of PI3K [26]. Thus, the TREM2 receptor can activate and inhibit osteoclastogenesis [25, 27]. The dual action of the TREM2–DAP12 complex may be regulated by differing TREM2 ligands, differing strength of ligand signals, or combinations of different co-stimulatory signals; but this is not yet delineated [27].
The ligand specificity of TREM2 has been a topic of considerable interest, and a number of studies suggest that TREM2 functions as a pattern recognition receptor, able to bind to a variety of anionic ligands including Gram-negative and Gram-positive bacteria, heparin and dextran sulfate, HSP60, and apoptotic cells [28–31]. TREM2 has also been shown to associate with neighboring plexin-A1 receptors, and interaction of plexin-A1 with its ligand, semaphorin 6D, leads to phosphorylation of the associated DAP12 ITAM [32]. TREM2 expression is upregulated by RANKL stimulation but downregulated by LPS and IL-10 [25, 28, 33]. TREM2 is highly upregulated in active rheumatoid arthritis (RA) synovium and subsequently downregulated in inactive RA, suggesting a role in RA-induced inflammation [34]. Human TREM2-deficient osteoclasts fail to multinucleate in vitro [15]; however, TREM2-deficient mouse osteoclasts show accelerated osteoclastogenesis in vitro due to excess M-CSF-induced activation of β-catenin that limits pre-osteoclast proliferation and diverts development towards osteoclasts [35]. Despite intensive investigation around TREM2, a number of questions remain unanswered, particularly with regards to the roles for TREM2 in bone. Differences between the mouse and human phenotype in TREM2 deficiency are incompletely explained, and the relevant ligands in the bone microenvironment are not clearly identified. In other immune cells, TREM2 plays a role in resolving inflammatory responses and recognition of apoptotic cells, processes that could also be of importance in maintaining bone homeostasis.
MDL-1
Myeloid DAP12-associated lectin (MDL-1 or CLEC5A) is a C-type lectin DAP12-associated receptor but, in contrast to TREM2, stimulates myeloid cell-associated inflammatory responses [36]. MDL-1 associates with signaling adaptors DAP12 and DAP10 and is most highly expressed in activated myeloid cells [37]. MDL-1 is potently induced by TNF-α and IL-23 [38, 39]. MDL-1 stimulates osteoclastogenesis in vitro, and MDL knockdown in osteoclast precursor cells inhibits osteoclastogenesis. Studies in MDL-1−/− mice demonstrate that MDL-1 plays a significant role in inflammatory arthritis, suggesting that MDL-1 promotes inflammatory bone loss [38]. Treatment with an agonist anti-MDL-1 antibody increased both disease incidence and severity in a murine collagen antibody-induced arthritis model (CAIA) and in a collagen-induced arthritis (CIA) model. CAIA is diminished in severity and incidence in both DAP12−/− and MDL-1−/− animals, indicating that the receptor and signaling adaptor are required to promote bone loss. Blockade of MDL-1 function with a soluble receptor fusion protein (MDL-1-Ig) induces resistance to CAIA or CIA-induced arthritis [38]. Importantly, MDL-1-Ig treatment downregulates TRAP, cathepsin K, and MMP9 expressions, reducing both clinical signs of autoimmune joint inflammation and bone destruction [38]. These studies suggest that MDL-1 is an important regulator of osteoclastogenesis during inflammation.
Ligands important for activating MDL-1 in inflammatory arthritis are not known. The only identified MDL-1 ligand is a dengue virus capsid protein [40]. Interestingly, dengue hemorrhagic fever is also known as “break bone” fever; thus, dengue might regulate osteoclastogenesis through MDL-1, which may contribute to osseous symptoms. MDL-1 does regulate the intense inflammatory response to dengue fever because blockade of MDL-1 inhibits the cytokine storm and vascular leakage in a mouse model of dengue fever [40]. In RA patients, the frequencies of MDL-1-expressing monocytes and levels of MDL-1 and DAP12 gene expression were significantly increased in active RA patients compared to inactive RA patients or healthy controls [41]. Interestingly, the frequency of MDL-1 expression also significantly decreased after effective RA therapy. Concordant overexpression of MDL-1 and DAP12 correlated with increased production of proinflammatory cytokines in RA patients, suggesting that MDL-1 plays a role in regulating articular inflammation as well as osteoclastogenesis in inflammatory conditions [41, 42].
Siglec-15
Sialic acid-binding immunoglobulin-like lectin 15 (Siglec-15) is one of a family of receptors that binds to sialylated O-linked sugars. Siglec-15 binds to cells expressing the sialic acid motif Neu5Acalpha2-6GalNAcalpha structure [43]. Siglec-15, initially identified as a markedly overexpressed gene in giant cell tumor of the bone, was subsequently investigated for its role in osteoclastogenesis. Other Siglecs associate with DAP12 and their expression or function have not yet been examined in osteoclasts. Siglec-15 is the only Siglec highly conserved throughout vertebrate evolution [44]. Siglec-15 is upregulated in differentiated osteoclasts, and anti-Siglec-15 polyclonal antibody inhibits human and mouse osteoclast differentiation in vitro [45]. Siglec-15−/− mice have mild osteopetrosis with increased trabecular bone mass in the lumbar vertebrae and metaphyseal regions of the femur and tibia. Interestingly, osteoclast numbers are unchanged but a systemic bone resorption marker, urinary deoxypyridinoline, is decreased in Siglec-15−/− mice, suggesting that the increased bone mass in the mutant mice is due to a functional osteoclast defect [46]. Indeed, Siglec15−/− osteoclasts have impaired functional resorption in vitro [46]. The osteoclast defect is more prominent in the secondary spongiosa, consistent with a localized effect, which is also seen in an antigen-induced arthritis model in Siglec 15−/− mice [47]. In murine antigen-induced arthritis, the degree of periarticular bone loss in the proximal tibia is significantly lower in Siglec-15−/− mice compared to wild-type (WT) mice; however, the degree of joint inflammation and cartilage and subchondral bone destruction is comparable [48]. Interestingly, TNF-α-mediated induction of TRAP-positive multinucleated cells is also impaired in Siglec-15−/− cells, and Siglec-15−/− mice are resistant to estrogen deficiency-induced bone loss compared to WT mice suggesting that Siglec-15 blockade may be useful as a therapeutic strategy [49].
Other DAP12-Associated Receptors
DAP12-associated receptors such as TREM1, TREM3, SIRPβ1, PILRB, CD200R3, CD200R4, CD300B, CD300LE, and MAIRII are known to be present on myeloid cells but their roles have not been examined or demonstrated in osteoclasts [50]. However, DAP12 is known to cooperate with non-immunoreceptors in osteoclasts particularly αvβ3 integrin and c-Fms receptor to regulate the osteoclast cytoskeleton, adhesion, and proliferation. Integrin β3 stimulation on osteoclasts leads to activation of Syk and Src associated with DAP12 during cytoskeletal changes in bone resorption and actin ring formation [51]. Similarly, M-CSF stimulation of c-Fms leads to c-Src-induced phosphorylation of DAP12 with recruitment of Syk to the DAP12 ITAM domain and activation of Vav leading to osteoclast spreading [17, 52]. DAP12−/− osteoclastogenesis is partially rescued by high-dose M-CSF in vitro but fails to correct the abnormal cytoskeleton formation [52]. Thus, DAP12 can participate in intracellular signaling initiated by several different types of ligand/receptor interactions in addition to the immunoreceptors that pair specifically with DAP12.
Fcgamma-Associated Receptors
The FcRγ is similar to DAP12 in that it contains an ITAM domain and no extracellular domain. FcRγ also pairs with ligand-binding receptors through interactions in the transmembrane domains of the ITAM-signaling adaptor and the immunoreceptor. FcRγ-associated receptors are a distinct group from receptors that pair with DAP12 [8]. The FcRγ−/− mouse does not have a bone phenotype at baseline and forms normal osteoclasts in vivo and in vitro [6]. However, when combined with DAP12 deficiency, the resulting severe osteoclast deficiency and osteopetrosis suggest that FcRγ chain-associated receptors are essential in the absence of DAP12 [5, 6]. A recent study of mice with combined deficiency of DAP12 and the beta3 integrin showed osteopetrosis and osteoclast deficiency similar to the combined DAP12/FcRγ chain deficiency. Further studies demonstrated that beta 3 integrin requires FcRγ association to function in the absence of DAP12 [51]. FcRγ, named for its association with receptors binding to the Fc portion of immunoglobulin molecules, also pairs with a number of additional immunoreceptors. Some FcRγ chain-associated receptors identified in other myeloid cells such as dendritic cell-activating receptor (DCAR) and immunoglobulin-like transcript/leukocyte immunoglobulin-like receptor (ILT/LILR) have yet to be examined in osteoclasts.
OSCAR
Osteoclast activating receptor (OSCAR) is an FcRγ-associated receptor that is a member of the leukocyte receptor complex protein family [53]. OSCAR was named for the original finding that it is upregulated during osteoclast differentiation; however, subsequent studies have revealed that OSCAR expression is not specific to osteoclasts [54]. OSCAR is one of the few ITAM-signaling adaptor-associated receptors shown to have a functional ligand in the bone microenvironment. OSCAR binding sites are found in collagens I, II and III; and recognition of exposed extracellular matrix (ECM) ligands has been shown to mediate co-stimulation of osteoclastogenesis dependent on FcRγ [55]. Thus, OSCAR is a collagen receptor and it can provide co-stimulatory signals for osteoclast differentiation in DAP12−/− cells [55]. In vivo, OSCAR deficiency alone fails to alter bone mass, which is not surprising given that the absence of its associated signaling chain, FcRγ, in mice also fails to induce a change in bone phenotype [5, 6, 55]. OSCAR gene expression is coordinately regulated by the osteoclastogenic transcription factors PU.1/MITF and is further enhanced by RANK-induced MKK6/p38 signals. Thus, while OSCAR can stimulate osteoclast differentiation, it is also upregulated during osteoclast differentiation [56].
OSCAR expression has been associated with both bone loss and inflammation in human disease. A single-nucleotide polymorphism within the promoter of the OSCAR gene has been linked to increased risk of postmenopausal osteoporosis [57]. In RA, OSCAR expression in monocytes is correlated with disease activity, and monocytes with high OSCAR expression exhibited an enhanced potential to differentiate into osteoclasts [58]. TNF-α is the main inducer of OSCAR expression in monocytes [58]. Serum levels of OSCAR are reduced in RA patients compared with healthy controls, suggesting that the expression and secretion or cleavage of OSCAR to a soluble form is immune modulated [59]. Supporting this idea, OSCAR transcript expression and soluble OSCAR release are stimulated by TNF-α and IL-1β in cultured endothelial cells. OSCAR is strongly expressed in the microvasculature of active synovial tissue in RA [42]. OSCAR has also been demonstrated to be a receptor for surfactant protein D, and the interaction can activate TNF-α release from human CCR2+ inflammatory monocytes [60]. OSCAR expression is also regulated by oxidized low-density lipoprotein; thus, OSCAR has been suggested to play a role in oxidative stress-mediated atherogenesis as well as monocyte adhesion [61].
PIR-A
Paired immunoglobulin-like receptor A (PIR-A) is an FcRγ-associated receptor of the immunoglobulin superfamily present in mice, whose ligands are known to be major histocompatibility complex class I (MHC class I) molecules. TNF-α induces the expression of PIR-A on osteoclasts and PIR-A ligands on osteoblasts, and these interactions contribute to TNF-α-induced osteoclastogenesis and TNF-α-induced bone loss in vivo [62]. Transgenic expression of TNF-α in mice deficient in FcRγ leads to inflammation but not bone erosion or osteoporosis, suggesting that one or more FcRγ-associated receptors is required for TNF-α-induced bone loss. TNF-α induces PIR-A upregulation but not other co-stimulatory receptors such as OSCAR, TREM2, and SIRPβ in osteoclasts [62]. Mice deficient in expression of PIR-A ligands (β2-microglobulin-deficient mice lacking MHC class I expression) also showed abrogation of bone loss with transgenic TNF-α exposure. PIR-A-Fc blocks enhanced TNF-α-induced osteoclastogenesis in vitro, suggesting that PIR-A is required for enhanced TNF-α-induced osteoclastogenesis [62]. PIR-A receptors are only present in mice; however, there are human orthologues in the immunoglobulin-like transcript, ILT/LILR families that respond to MHC class I ligands as well [63]. Additional studies are needed to determine whether the FcRγ-associated receptors in these receptor families regulate human osteoclasts.
Fc Receptors
Fc receptors (FcR) are capable of binding to and responding to the Fc domain of serum immunoglobulin and immune complexes. FcγRI, FcγRIII, and FcγRIV are all Fc receptors that utilize the FcRγ chain, and their interactions with immune complexes have been speculated to promote osteoclastogenesis. Fc receptors could have a direct effect on osteoclast precursors or an indirect effect due to the release of proinflammatory cytokines and chemokines upon stimulation of Fc receptor-bearing immune cells. The role of autoantibodies and immune complexes in regulating osteoclastogenesis has been difficult to sort out and is further complicated because both activating and inhibitory Fc receptors are expressed on osteoclast precursors. FcγRIIB is an ITIM-signaling receptor and generally inhibits signaling by FcγRI, FcγRIII, or FcγRIV (Fig. 2a). It was suspected that the relative expression of different activating FcRs (FcγRI/III/IV) and inhibitory FcR (FcγRIIB) on osteoclast precursors would determine osteoclastogenesis in response to immune complex stimulation.
Fc receptors in osteoclasts activate and inhibit osteoclastogenesis. a Multiple Fc receptors are expressed in osteoclasts. FcγRIIB is an ITIM-signaling receptor. FcγRI, FcγRIII, and FcγRIV are all ITAM-signaling adaptor-associated immunoreceptors that associate with the FcRγ adaptor chain. b Under basal conditions, osteoclast precursors express only FcγRIIB and FcγRIII. Osteoclastogenesis is inhibited. FcγRIII is thought to inhibit osteoclastogenesis by sequestering the FcRγ adaptor chain from PIR-A and OSCAR, which remain intracellular but are not expressed on the cell surface due to the lack of availability of FcRγ adaptor chains. c RANKL stimulation in the presence of inflammation and immune complex formation leads to downregulation of FcγRIIB and FcγRIII and upregulation of PIR-A and OSCAR. Osteoclastogenesis is enhanced (based on [64])
Recent studies have dissected the roles of individual Fc receptors more carefully and demonstrated several interesting findings. Under basal conditions, osteoclast precursors express FcγRIIB and FcγRIII [64]. FcγRIII is well known to respond to immune complexes during infections. As an activating receptor that pairs with the FcRγ chain, it might be expected that FcγRIII would lead to activation of osteoclastogenesis. Interestingly, FcγRIII is downregulated with RANKL stimulation during osteoclastogenesis, and overexpression of FcγRIII actually inhibits osteoclastogenesis [64]. FcγRIII−/− mice are osteopenic with increased osteoclasts in vivo, indicating that FcγRIII is actually a negative regulator of osteoclastogenesis. Consistent with this finding, inhibition of osteoclastogenesis by immune complexes was observed in FcγRIIB−/− precursors but not FcRγ−/− precursors, suggesting that the inhibition was mediated by an activating ITAM-signaling adaptor-associated receptor [65]. The mechanism behind the inhibition is thought to be that the presence of FcγRIII sequesters the FcRγ chain away from other osteoclastogenic Ig-like receptors (such as PIR-A and OSCAR) preventing them from associating with FcRγ to promote osteoclastogenesis [64] (Fig. 2b).
Other ITAM-signaling adaptor-associated Fc receptors, FcγRI and FcγRIV, are induced under inflammatory conditions, and IgG2 immune complexes binding to these receptors can activate osteoclastogenesis. FcγRIV is also upregulated with RANKL stimulation, and cross-linking of FcγRIV enhances osteoclast differentiation [64] (Fig. 2c). FcγRIV−/− mice and mice with a targeted deletion of FcγRIV limited to osteoclasts (cathepsin K-Cre) are protected from autoantibody-dependent bone destruction in a serum transfer arthritis model and have lower numbers of osteoclasts in the inflamed joints [64]. Mice with an osteoclast-specific deletion of FcγRIV showed decreased bone destruction despite persistence of inflammation, suggesting that FcγRIV on osteoclasts is critical for bone destruction during antibody-dependent inflammatory arthritis in mice [64]. Another group attempted to modify these interactions therapeutically using a staphylococcal protein A complex (SPA) which binds to circulating IgG and generates small immunoglobulin complexes that interact with monocytes, macrophages, and preosteoclasts. Formation of these complexes resulted in polarization of macrophages to a regulatory phenotype and directly inhibited differentiation of preosteoclasts into osteoclasts [66]. Administration of SPA in the early stages of disease substantially alleviated the clinical and histologic erosive features of CIA in mice and though it was not determined which FcR was responsible for the effects, the study demonstrates that specific types of immune complexes can be utilized to downregulate inflammation and osteoclastogenesis [66]. It should be noted that FcγRIV is not present in humans and human cells have a unique Fc receptor, FcRIIA, which is a single chain receptor with a cytoplasmic ITAM domain. Thus, ITAM-signaling receptors that interact with the Fc domains of immunoglobulin differ between mice and humans.
The presence of autoantibodies against citrullinated peptides (ACPA) highly correlates with development of bone loss and erosive disease in patients with rheumatoid arthritis. In vitro, affinity-purified human autoantibodies against mutated citrullinated vimentin (MCV) bind to osteoclasts and stimulate osteoclastogenesis and bone resorption [67]. Adoptive transfer of these purified human MCV autoantibodies into mice induces increased osteoclastogenesis and osteopenia [67]. Interestingly, desialylated, but not sialylated, immune complexes enhance osteoclastogenesis in vitro and in vivo [68]. IgG sialylation is of importance in determining the engagement of Fc receptors and the type of resulting immune response [69]. Recently in RA patients, it was shown that the sialylation state of random IgG and specific anti-IgG autoantibodies correlates with bone volume and trabecular number [68]. A direct demonstration of desialylated antibodies in vivo is seen when desialylated or sialylated immune complexes are directly injected into a knee joint of mice. Injection with desialylated immune complexes increases osteoclast number and surface area compared with injection of sialylated immune complexes. However, addition of TNF-α to the antibody injection eliminates the differential effect due to immune complex sialylation [68]. Treatment of mice with the sialic acid precursor N-acetylmannosamine (ManNAc), which results in increased IgG sialylation in vivo, renders mice less susceptible to development of CIA [68], suggesting that modification of sialylation may be therapeutically useful. ACPA are reported to show less sialylation than random IgG, consistent with their pro-osteoclastogenic capacity [70].
ITIM-Signaling Receptors that Positively Regulate Osteoclastogenesis
ITAM domains are defined by a specific amino acid sequence that includes a tyrosine that when phosphorylated leads to recruitment of tyrosine kinases that initiate an activating signaling cascade. Opposing the ITAM signals are signals mediated through receptors with ITIM domains. ITIM domains are defined by a related amino acid sequence that includes a tyrosine that when phosphorylated leads to recruitment of specific phosphatases that can inhibit cellular activation [71]. While some ITIM-signaling receptors have been demonstrated to inhibit osteoclastogenesis as expected, the following ITIM-signaling receptors have been demonstrated to paradoxically promote osteoclastogenesis.
Ly49Q
The Ly49 is a family of C-type lectin receptors that includes ITIM receptors and DAP12-associated receptors that are primarily expressed on NK cells and interact with class I MHC ligands [72]. Ly49Q is an ITIM receptor present on mouse myeloid cells. Surprisingly, knockdown or deletion of Ly49Q resulted in decreased in vitro osteoclastogenesis [72]. Ly49Q is upregulated with RANKL stimulation and mechanistically, Ly49Q has been shown to sequester SH2 domain hematopoietic phosphatase-1 (SHP-1) away from paired immunoglobulin-like receptor B (PIR-B), a different ITIM-containing receptor, to enable osteoclastogenesis to proceed. Ly49Q-deficient mice do not demonstrate a significant bone phenotype in vivo [72].
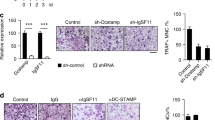
DC-STAMP
Dendritic cell-specific transmembrane protein (DC-STAMP), despite its name, is expressed in osteoclasts and has been shown to be an important regulator of cell fusion in osteoclasts [73]. DC-STAMP was recently shown to be an ITIM-signaling receptor [74]. However, antibody against DC-STAMP blocks OC formation in vitro suggesting DC-STAMP as a positive regulator of osteoclastogenesis. DC-STAMP (high) freshly isolated monocytes produce a higher number of OC in culture than DC-STAMP (low) cells [74]. DC-STAMP has been demonstrated to interact with SHP-1 and CD16 (FcγRIII) during osteoclastogenesis [74]. Perhaps this interaction also sequesters these negative regulators enabling promotion of osteoclastogenesis, but this was not directly examined.
PD-1
Programmed cell death protein 1 (PD-1 or CD279) is a cell surface receptor in the immunoglobulin superfamily. Deficiency of PD-1 leads to T cell activation, but surprisingly, the enhanced immune activation does not lead to bone loss. The cytoplasmic tail of PD-1 contains an ITIM domain and an immunoreceptor tyrosine-based switch motif that can link to additional signaling intermediates. PD-1 deficiency in mice leads to reduced osteoclastogenesis and an osteopetrotic phenotype [75]. Micro-CT analysis of PD-1−/− bones shows significant increases in trabecular and cortical bone mineral densities of the tibia, and histomorphometry reveals a 55 % decrease in osteoclast number on bone surfaces compared to WT mice. Bone formation indices are similar in both groups. The cells from PD-1-deficient mice show decreased osteoclastogenesis in vitro but do not demonstrate a significant change in functional bone resorption [75]. Thus, PD-1 positively regulates osteoclastogenesis, although the exact mechanism has not been demonstrated. Whether or not PD-1 promotes osteoclastogenesis by sequestering SHP-1 or SHIP phosphatases has not been examined.
ITIM-Signaling Receptors that Inhibit Osteoclastogenesis
Other ITIM-signaling receptors inhibit osteoclastogenesis. The phosphatases SHP-1 and SHIP-1 are known to associate with ITIM domains, and both of these phosphatases function as negative regulators of osteoclastogenesis. Mice expressing mutant SHP-1 show marked osteopenia with an increase in bone resorption. SHP-1-deficient mice have increased numbers of osteoclasts in vitro with increased bone resorption [76]. The SHIP-1 phosphatase also inhibits osteoclastogenesis, and SHIP-1-deficient mice are also osteopenic with increased in vitro formation of osteoclasts and increased bone resorption [77].
While less is known about ITIM-signaling receptors in osteoclastogenesis, those that inhibit osteoclastogenesis in vitro include TLT-1s, CMRF-35-like molecule-1 (CLM-1), and PIR-B. TLT-1s is an alternate transcript of triggering receptor expressed on myeloid cells like transcript-1 (TLT-1) and the only TREM receptor family member with a cytoplasmic ITIM domain [78]. TLT-1s is mainly expressed in macrophages and osteoclast precursor cells. Knockdown of TLT-1s strongly enhances the formation and resorption capacity of osteoclasts [78]. CLM-1 is expressed on osteoclast precursors and is downregulated by stimulation with RANKL. Overexpression of CLM-1 in the osteoclastogenic cell line RAW264.7 inhibits osteoclast differentiation induced by RANKL [79]. PIR-B and four isoforms of its human ortholog leukocyte Ig-like receptor LILR-B are present on cultured osteoclast precursor cells of mouse and human origin, respectively, and these ITIM-harboring inhibitory receptors constitutively recruit SHP-1 in the presence of RANKL and M-CSF. Both murine PIR-B and the human ortholog LILR-B1 suppress osteoclast development in vitro. These receptors are thought to interact with their MHC class I ligands on the same cell surface and then serve as a basal inhibitory stimulus for osteoclastogenesis [80]. While these receptors all can inhibit osteoclastogenesis, the exact in vivo role they play, particularly in pathological states has not been delineated.
FcγRIIB
FcγRIIB is an ITIM-containing Fc receptor that is highly expressed on osteoclast precursors and serves to chronically inhibit osteoclastogenesis. FcγRIIB−/− mice were recently found to have a markedly osteoporotic phenotype with enhanced osteoclastogenesis consistent with initial in vitro observations [64]. The enhanced osteoclast formation effect is not a cell autonomous change due to the deficiency of FcγRIIB but rather a response to immune complex stimulation enabled by FcγRIIB deficiency. When FcγRIIB−/− cells are cultured in the presence of serum from FcγRIIB−/− mice, enhanced osteoclastogenesis is observed due to the unusually high levels of immune complexes that stimulate activating FcRγ-associated receptors in the FcγRIIB−/− cells. Enhanced osteoclastogenesis is not observed in mice with combined FcγRIIB/FcγR deficiency confirming the requirement for activating FcRγ-associated receptors for the immune complex stimulation of osteoclastogenesis [64].
Bypassing Co-stimulation by ITAM-Associated Immunoreceptors
We note that the concept of ITAM-signaling as strictly activating and ITIM signaling as strictly inhibitory was overly simplistic and as these many studies have shown, co-stimulation in osteoclastogenesis is much more complex. In addition, while it is often stated that the ITAM-signaling co-receptors are required for osteoclastogenesis, we also note that this does not apply to all situations where osteoclastogenesis occurs. It is clear that there is a significant difference in the phenotype of the DAP12−/−/FcRγ−/− mice and the RANK-deficient mice [4–6]. The lack of RANK signaling leads to a global defect in all osteoclastogenesis, causing osteopetrosis in the long bones and lack of tooth eruption in the jaw. In contrast, while the DAP12−/−/FcRγ−/− mice have similar osteopetrosis in the long bones, they show normal tooth eruption [4–6]. In addition, despite the lack of osteoclasts in the long bones of DAP12-/-/FcRγ−/− mice at baseline, when these mice are estrogen deficient, post-ovariectomy, they are able to generate osteoclasts in vivo, with significant bone loss [9]. Thus, the requirement for specific ITAM-signaling adaptors to provide co-stimulation in osteoclastogenesis appears to be microenvironment specific and can be bypassed in specific locations and pathological conditions.
Recent studies of the transcriptional regulator recombination signal binding protein for immunoglobulin kappa J region (RBP-J) demonstrate that the deletion of RBP-J rescues the defect in osteoclastogenesis observed in the DAP12-/-/FcRγ−/− mice both in vivo and in vitro [81]. RBP-J deficiency allows RANK or TNFR signaling to induce osteoclastogenesis independent of ITAM-adapter signals. RBP-J deficiency potentiates cell responses to TGF-β by upregulating TGFβR1 and maintaining downstream PLCγ2/calcium-CaMKK/PYK2 activity in the absence of ITAM-signaling adaptors [81]. Whether or not specific other additional co-receptors are also required under these conditions is not yet clear. Nonetheless, deficiency of RBP-J results in increased PLCγ2 expression and activity as well as calcium oscillations that enable NFATc1 activation [81], indicating that osteoclastogenesis continues to require the master terminal regulators of osteoclastogenesis and verifies that pathways that bypass the ITAM-signaling adaptors can initiate the process.
Thus, all osteoclastogenesis is not likely identical, and like other immune cells, differences in co-receptor and/or cytokine stimulation during differentiation likely lead to functional heterogeneity among cells. While all osteoclasts share the function of bone resorption, the combination of enzymatic and acidic mechanisms used by osteoclasts at different sites has been suggested to vary [82], and it remains to be determined if this is a consequence of conditions of differentiation. Much remains to be determined to better delineate these regulatory mechanisms. However, the importance of a requirement for co-receptors in osteoclastogenesis is that it provides a mechanism by which osteoclastogenesis can be fine-tuned in response to specific microenvironments and holds potential for differential regulation of bone resorption in health and disease.
References
Mellis DJ, Itzstein C, Helfrich MH, Crockett JC (2011) The skeleton: a multi-functional complex organ: the role of key signalling pathways in osteoclast differentiation and in bone resorption. J Endocrinol 211:131–143
Long CL, Humphrey MB (2012) Osteoimmunology: the expanding role of immunoreceptors in osteoclasts and bone remodeling. Bonekey Rep 1
Wythe SE, Nicolaidou V, Horwood NJ (2014) Cells of the immune system orchestrate changes in bone cell function. Calcif Tissue Int 94:98–111
Boyce BF, Xing L (2007) Biology of RANK, RANKL, and osteoprotegerin. Arthritis Res Ther 9(Suppl 1):S1
Koga T, Inui M, Inoue K, Kim S, Suematsu A, Kobayashi E, Iwata T, Ohnishi H, Matozaki T, Kodama T, Taniguchi T, Takayanagi H, Takai T (2004) Costimulatory signals mediated by the ITAM motif cooperate with RANKL for bone homeostasis. Nature 428:758–763
Mocsai A, Humphrey MB, Van Ziffle JA, Hu Y, Burghardt A, Spusta SC, Majumdar S, Lanier LL, Lowell CA, Nakamura MC (2004) The immunomodulatory adapter proteins DAP12 and Fc receptor gamma-chain (FcRgamma) regulate development of functional osteoclasts through the Syk tyrosine kinase. Proc Natl Acad Sci U S A 101:6158–6163
Negishi-Koga T, Takayanagi H (2009) Ca2+-NFATc1 signaling is an essential axis of osteoclast differentiation. Immunol Rev 231:241–256
Humphrey MB, Lanier LL, Nakamura MC (2005) Role of ITAM-containing adapter proteins and their receptors in the immune system and bone. Immunol Rev 208:50–65
Wu Y, Torchia J, Yao W, Lane NE, Lanier LL, Nakamura MC, Humphrey MB (2007) Bone microenvironment specific roles of ITAM adapter signaling during bone remodeling induced by acute estrogen-deficiency. PLoS One 2, e586
Hamerman JA, Ni M, Killebrew JR, Chu CL, Lowell CA (2009) The expanding roles of ITAM adapters FcRgamma and DAP12 in myeloid cells. Immunol Rev 232:42–58
Lanier LL, Bakker AB (2000) The ITAM-bearing transmembrane adaptor DAP12 in lymphoid and myeloid cell function. Immunol Today 21:611–614
Zawawi MS, Dharmapatni AA, Cantley MD, McHugh KP, Haynes DR, Crotti TN (2012) Regulation of ITAM adaptor molecules and their receptors by inhibition of calcineurin-NFAT signalling during late stage osteoclast differentiation. Biochem Biophys Res Commun 427:404–409
Paloneva J, Kestila M, Wu J, Salminen A, Bohling T, Ruotsalainen V, Hakola P, Bakker AB, Phillips JH, Pekkarinen P, Lanier LL, Timonen T, Peltonen L (2000) Loss-of-function mutations in TYROBP (DAP12) result in a presenile dementia with bone cysts. Nat Genet 25:357–361
Paloneva J, Mandelin J, Kiialainen A, Bohling T, Prudlo J, Hakola P, Haltia M, Konttinen YT, Peltonen L (2003) DAP12/TREM2 deficiency results in impaired osteoclast differentiation and osteoporotic features. J Exp Med 198:669–675
Cella M, Buonsanti C, Strader C, Kondo T, Salmaggi A, Colonna M (2003) Impaired differentiation of osteoclasts in TREM-2-deficient individuals. J Exp Med 198:645–651
Humphrey MB, Ogasawara K, Yao W, Spusta SC, Daws MR, Lane NE, Lanier LL, Nakamura MC (2004) The signaling adapter protein DAP12 regulates multinucleation during osteoclast development. J Bone Miner Res 19:224–234
Zou W, Reeve JL, Liu Y, Teitelbaum SL, Ross FP (2008) DAP12 couples c-Fms activation to the osteoclast cytoskeleton by recruitment of Syk. Mol Cell 31:422–431
Zou W, Zhu T, Craft CS, Broekelmann TJ, Mecham RP, Teitelbaum SL (2010) Cytoskeletal dysfunction dominates in DAP12-deficient osteoclasts. J Cell Sci 123:2955–2963
Kaifu T, Nakahara J, Inui M, Mishima K, Momiyama T, Kaji M, Sugahara A, Koito H, Ujike-Asai A, Nakamura A, Kanazawa K, Tan-Takeuchi K, Iwasaki K, Yokoyama WM, Kudo A, Fujiwara M, Asou H, Takai T (2003) Osteopetrosis and thalamic hypomyelinosis with synaptic degeneration in DAP12-deficient mice. J Clin Invest 111:323–332
Nataf S, Anginot A, Vuaillat C, Malaval L, Fodil N, Chereul E, Langlois JB, Dumontel C, Cavillon G, Confavreux C, Mazzorana M, Vico L, Belin MF, Vivier E, Tomasello E, Jurdic P (2005) Brain and bone damage in KARAP/DAP12 loss-of-function mice correlate with alterations in microglia and osteoclast lineages. Am J Pathol 166:275–286
Kamimura M, Mori Y, Sugahara-Tobinai A, Takai T, Itoi E (2015) Impaired fracture healing caused by deficiency of the immunoreceptor adaptor protein DAP12. PLoS One 10, e0128210
Bouchon A, Hernandez-Munain C, Cella M, Colonna M (2001) A DAP12-mediated pathway regulates expression of CC chemokine receptor 7 and maturation of human dendritic cells. J Exp Med 194:1111–1122
Hamerman JA, Jarjoura JR, Humphrey MB, Nakamura MC, Seaman WE, Lanier LL (2006) Cutting edge: inhibition of TLR and FcR responses in macrophages by triggering receptor expressed on myeloid cells (TREM)-2 and DAP12. J Immunol 177:2051–2055
Ito H, Hamerman JA (2012) TREM-2, triggering receptor expressed on myeloid cell-2, negatively regulates TLR responses in dendritic cells. Eur J Immunol 42:176–185
Humphrey MB, Daws MR, Spusta SC, Niemi EC, Torchia JA, Lanier LL, Seaman WE, Nakamura MC (2006) TREM2, a DAP12-associated receptor, regulates osteoclast differentiation and function. J Bone Miner Res 21:237–245
Peng Q, Malhotra S, Torchia JA, Kerr WG, Coggeshall KM, Humphrey MB (2010) TREM2- and DAP12-dependent activation of PI3K requires DAP10 and is inhibited by SHIP1. Sci Signal 3:ra38
Colonna M, Turnbull I, Klesney-Tait J (2007) The enigmatic function of TREM-2 in osteoclastogenesis. Adv Exp Med Biol 602:97–105
Daws MR, Sullam PM, Niemi EC, Chen TT, Tchao NK, Seaman WE (2003) Pattern recognition by TREM-2: binding of anionic ligands. J Immunol 171:594–599
N’Diaye EN, Branda CS, Branda SS, Nevarez L, Colonna M, Lowell C, Hamerman JA, Seaman WE (2009) TREM-2 (triggering receptor expressed on myeloid cells 2) is a phagocytic receptor for bacteria. J Cell Biol 184:215–223
Stefano L, Racchetti G, Bianco F, Passini N, Gupta RS, Panina Bordignon P, Meldolesi J (2009) The surface-exposed chaperone, Hsp60, is an agonist of the microglial TREM2 receptor. J Neurochem 110:284–294
Hsieh CL, Koike M, Spusta SC, Niemi EC, Yenari M, Nakamura MC, Seaman WE (2009) A role for TREM2 ligands in the phagocytosis of apoptotic neuronal cells by microglia. J Neurochem 109:1144–1156
Takegahara N, Takamatsu H, Toyofuku T, Tsujimura T, Okuno T, Yukawa K, Mizui M, Yamamoto M, Prasad DV, Suzuki K, Ishii M, Terai K, Moriya M, Nakatsuji Y, Sakoda S, Sato S, Akira S, Takeda K, Inui M, Takai T, Ikawa M, Okabe M, Kumanogoh A, Kikutani H (2006) Plexin-A1 and its interaction with DAP12 in immune responses and bone homeostasis. Nat Cell Biol 8:615–622
Park-Min KH, Ji JD, Antoniv T, Reid AC, Silver RB, Humphrey MB, Nakamura M, Ivashkiv LB (2009) IL-10 suppresses calcium-mediated costimulation of receptor activator NF-kappa B signaling during human osteoclast differentiation by inhibiting TREM-2 expression. J Immunol 183:2444–2455
Crotti TN, Dharmapatni AA, Alias E, Zannettino AC, Smith MD, Haynes DR. (2012) The immunoreceptor tyrosine-based activation motif (ITAM)-related factors are increased in synovial tissue and vasculature of rheumatoid arthritic joints. Arthritis Res Ther 14(6):R245. doi:10.1186/ar4088
Otero K, Turnbull IR, Poliani PL, Vermi W, Cerutti E, Aoshi T, Tassi I, Takai T, Stanley SL, Miller M, Shaw AS, Colonna M (2009) Macrophage colony-stimulating factor induces the proliferation and survival of macrophages via a pathway involving DAP12 and beta-catenin. Nat Immunol 10:734–743
Bakker AB, Baker E, Sutherland GR, Phillips JH, Lanier LL (1999) Myeloid DAP12-associating lectin (MDL)-1 is a cell surface receptor involved in the activation of myeloid cells. Proc Natl Acad Sci U S A 96:9792–9796
Inui M, Kikuchi Y, Aoki N, Endo S, Maeda T, Sugahara-Tobinai A, Fujimura S, Nakamura A, Kumanogoh A, Colonna M, Takai T (2009) Signal adaptor DAP10 associates with MDL-1 and triggers osteoclastogenesis in cooperation with DAP12. Proc Natl Acad Sci U S A 106:4816–4821
Joyce-Shaikh B, Bigler ME, Chao CC, Murphy EE, Blumenschein WM, Adamopoulos IE, Heyworth PG, Antonenko S, Bowman EP, McClanahan TK, Phillips JH, Cua DJ (2010) Myeloid DAP12-associating lectin (MDL)-1 regulates synovial inflammation and bone erosion associated with autoimmune arthritis. J Exp Med 207:579–589
Shin HS, Sarin R, Dixit N, Wu J, Gershwin E, Bowman EP, Adamopoulos IE (2015) Crosstalk among IL-23 and DNAX activating protein of 12 kDa-dependent pathways promotes osteoclastogenesis. J Immunol 194:316–324
Watson AA, O’Callaghan CA (2010) Crystallization and X-ray diffraction analysis of human CLEC5A (MDL-1), a dengue virus receptor. Acta Crystallogr Sect F: Struct Biol Cryst Commun 66:29–31
Chen DY, Yao L, Chen YM, Lin CC, Huang KC, Chen ST, Lan JL, Hsieh SL (2014) A potential role of myeloid DAP12-associating lectin (MDL)-1 in the regulation of inflammation in rheumatoid arthritis patients. PLoS One 9, e86105
Crotti TN, Dharmapatni AA, Alias E, Haynes DR (2015) Osteoimmunology: major and costimulatory pathway expression associated with chronic inflammatory induced bone loss. J Immunol Res 2015:281287
Ishida-Kitagawa N, Tanaka K, Bao X, Kimura T, Miura T, Kitaoka Y, Hayashi K, Sato M, Maruoka M, Ogawa T, Miyoshi J, Takeya T (2012) Siglec-15 protein regulates formation of functional osteoclasts in concert with DNAX-activating protein of 12 kDa (DAP12). J Biol Chem 287:17493–17502
Angata T, Tabuchi Y, Nakamura K, Nakamura M (2007) Siglec-15: an immune system Siglec conserved throughout vertebrate evolution. Glycobiology 17:838–846
Hiruma Y, Hirai T, Tsuda E (2011) Siglec-15, a member of the sialic acid-binding lectin, is a novel regulator for osteoclast differentiation. Biochem Biophys Res Commun 409:424–429
Hiruma Y, Tsuda E, Maeda N, Okada A, Kabasawa N, Miyamoto M, Hattori H, Fukuda C (2013) Impaired osteoclast differentiation and function and mild osteopetrosis development in Siglec-15-deficient mice. Bone 53:87–93
Kameda Y, Takahata M, Komatsu M, Mikuni S, Hatakeyama S, Shimizu T, Angata T, Kinjo M, Minami A, Iwasaki N (2013) Siglec-15 regulates osteoclast differentiation by modulating RANKL-induced phosphatidylinositol 3-kinase/Akt and Erk pathways in association with signaling adaptor DAP12. J Bone Miner Res 28:2463–2475
Shimizu T, Takahata M, Kameda Y, Endo T, Hamano H, Hiratsuka S, Ota M, Iwasaki N (2015) Sialic acid-binding immunoglobulin-like lectin 15 (Siglec-15) mediates periarticular bone loss, but not joint destruction, in murine antigen-induced arthritis. Bone 79:65–70
Kameda Y, Takahata M, Mikuni S, Shimizu T, Hamano H, Angata T, Hatakeyama S, Kinjo M, Iwasaki N (2015) Siglec-15 is a potential therapeutic target for postmenopausal osteoporosis. Bone 71:217–226
Lanier LL (2009) DAP10- and DAP12-associated receptors in innate immunity. Immunol Rev 227:150–160
Zou W, Teitelbaum SL (2015) Absence of Dap12 and the alphavbeta3 integrin causes severe osteopetrosis. J Cell Biol 208:125–136
Faccio R, Zou W, Colaianni G, Teitelbaum SL, Ross FP (2003) High dose M-CSF partially rescues the Dap12−/− osteoclast phenotype. J Cell Biochem 90:871–883
Kim N, Takami M, Rho J, Josien R, Choi Y (2002) A novel member of the leukocyte receptor complex regulates osteoclast differentiation. J Exp Med 195:201–209
Merck E, Gaillard C, Gorman DM, Montero-Julian F, Durand I, Zurawski SM, Menetrier-Caux C, Carra G, Lebecque S, Trinchieri G, Bates EE (2004) OSCAR is an FcRgamma-associated receptor that is expressed by myeloid cells and is involved in antigen presentation and activation of human dendritic cells. Blood 104:1386–1395
Barrow AD, Raynal N, Andersen TL, Slatter DA, Bihan D, Pugh N, Cella M, Kim T, Rho J, Negishi-Koga T, Delaisse JM, Takayanagi H, Lorenzo J, Colonna M, Farndale RW, Choi Y, Trowsdale J (2011) OSCAR is a collagen receptor that costimulates osteoclastogenesis in DAP12-deficient humans and mice. J Clin Invest 121:3505–3516
Kim JH, Kim K, Jin HM, Youn BU, Song I, Choi HS, Kim N (2008) Upstream stimulatory factors regulate OSCAR gene expression in RANKL-mediated osteoclast differentiation. J Mol Biol 383:502–511
Kim GS, Koh JM, Chang JS, Park BL, Kim LH, Park EK, Kim SY, Shin HD (2005) Association of the OSCAR promoter polymorphism with BMD in postmenopausal women. J Bone Miner Res 20:1342–1348
Herman S, Muller RB, Kronke G, Zwerina J, Redlich K, Hueber AJ, Gelse H, Neumann E, Muller-Ladner U, Schett G (2008) Induction of osteoclast-associated receptor, a key osteoclast costimulation molecule, in rheumatoid arthritis. Arthritis Rheum 58:3041–3050
Ndongo-Thiam N, de Sallmard G, Kastrup J, Miossec P (2014) Levels of soluble osteoclast-associated receptor (sOSCAR) in rheumatoid arthritis: link to disease severity and cardiovascular risk. Ann Rheum Dis 73:1276–1277
Barrow AD, Palarasah Y, Bugatti M, Holehouse AS, Byers DE, Holtzman MJ, Vermi W, Skjodt K, Crouch E, Colonna M (2015) OSCAR is a receptor for surfactant protein D that activates TNF-alpha release from human CCR2+ inflammatory monocytes. J Immunol 194:3317–3326
Goettsch C, Rauner M, Sinningen K, Helas S, Al-Fakhri N, Nemeth K, Hamann C, Kopprasch S, Aikawa E, Bornstein SR, Schoppet M, Hofbauer LC (2011) The osteoclast-associated receptor (OSCAR) is a novel receptor regulated by oxidized low-density lipoprotein in human endothelial cells. Endocrinology 152:4915–4926
Ochi S, Shinohara M, Sato K, Gober HJ, Koga T, Kodama T, Takai T, Miyasaka N, Takayanagi H (2007) Pathological role of osteoclast costimulation in arthritis-induced bone loss. Proc Natl Acad Sci U S A 104:11394–11399
Dietrich J, Nakajima H, Colonna M (2000) Human inhibitory and activating Ig-like receptors which modulate the function of myeloid cells. Microbes Infect 2:323–329
Negishi-Koga T, Gober HJ, Sumiya E, Komatsu N, Okamoto K, Sawa S, Suematsu A, Suda T, Sato K, Takai T, Takayanagi H (2015) Immune complexes regulate bone metabolism through FcRgamma signalling. Nat Commun 6:6637
Grevers LC, de Vries TJ, Everts V, Verbeek JS, van den Berg WB, van Lent PL (2013) Immune complex-induced inhibition of osteoclastogenesis is mediated via activating but not inhibitory Fcgamma receptors on myeloid precursor cells. Ann Rheum Dis 72:278–285
MacLellan LM, Montgomery J, Sugiyama F, Kitson SM, Thummler K, Silverman GJ, Beers SA, Nibbs RJ, McInnes IB, Goodyear CS (2011) Co-opting endogenous immunoglobulin for the regulation of inflammation and osteoclastogenesis in humans and mice. Arthritis Rheum 63:3897–3907
Harre U, Georgess D, Bang H, Bozec A, Axmann R, Ossipova E, Jakobsson PJ, Baum W, Nimmerjahn F, Szarka E, Sarmay G, Krumbholz G, Neumann E, Toes R, Scherer HU, Catrina AI, Klareskog L, Jurdic P, Schett G (2012) Induction of osteoclastogenesis and bone loss by human autoantibodies against citrullinated vimentin. J Clin Invest 122:1791–1802
Harre U, Lang SC, Pfeifle R, Rombouts Y, Fruhbeisser S, Amara K, Bang H, Lux A, Koeleman CA, Baum W, Dietel K, Grohn F, Malmstrom V, Klareskog L, Kronke G, Kocijan R, Nimmerjahn F, Toes RE, Herrmann M, Scherer HU, Schett G (2015) Glycosylation of immunoglobulin G determines osteoclast differentiation and bone loss. Nat Commun 6:6651
Bohm S, Schwab I, Lux A, Nimmerjahn F (2012) The role of sialic acid as a modulator of the anti-inflammatory activity of IgG. Semin Immunopathol 34:443–453
Scherer HU, van der Woude D, Ioan-Facsinay A, el Bannoudi H, Trouw LA, Wang J, Haupl T, Burmester GR, Deelder AM, Huizinga TW, Wuhrer M, Toes RE (2010) Glycan profiling of anti-citrullinated protein antibodies isolated from human serum and synovial fluid. Arthritis Rheum 62:1620–1629
Daeron M, Jaeger S, Du Pasquier L, Vivier E (2008) Immunoreceptor tyrosine-based inhibition motifs: a quest in the past and future. Immunol Rev 224:11–43
Hayashi M, Nakashima T, Kodama T, Makrigiannis AP, Toyama-Sorimachi N, Takayanagi H (2010) Ly49Q, an ITIM-bearing NK receptor, positively regulates osteoclast differentiation. Biochem Biophys Res Commun 393:432–438
Yagi M, Miyamoto T, Sawatani Y, Iwamoto K, Hosogane N, Fujita N, Morita K, Ninomiya K, Suzuki T, Miyamoto K, Oike Y, Takeya M, Toyama Y, Suda T (2005) DC-STAMP is essential for cell-cell fusion in osteoclasts and foreign body giant cells. J Exp Med 202:345–351
Chiu YH, Mensah KA, Schwarz EM, Ju Y, Takahata M, Feng C, McMahon LA, Hicks DG, Panepento B, Keng PC, Ritchlin CT (2012) Regulation of human osteoclast development by dendritic cell-specific transmembrane protein (DC-STAMP). J Bone Miner Res 27:79–92
Nagahama K, Aoki K, Nonaka K, Saito H, Takahashi M, Varghese BJ, Shimokawa H, Azuma M, Ohya K, Ohyama K (2004) The deficiency of immunoregulatory receptor PD-1 causes mild osteopetrosis. Bone 35:1059–1068
Aoki K, Didomenico E, Sims NA, Mukhopadhyay K, Neff L, Houghton A, Amling M, Levy JB, Horne WC, Baron R (1999) The tyrosine phosphatase SHP-1 is a negative regulator of osteoclastogenesis and osteoclast resorbing activity: increased resorption and osteopenia in me(v)/me(v) mutant mice. Bone 25:261–267
Takeshita S, Namba N, Zhao JJ, Jiang Y, Genant HK, Silva MJ, Brodt MD, Helgason CD, Kalesnikoff J, Rauh MJ, Humphries RK, Krystal G, Teitelbaum SL, Ross FP (2002) SHIP-deficient mice are severely osteoporotic due to increased numbers of hyper-resorptive osteoclasts. Nat Med 8:943–949
Yoon SH, Lee YD, Ha J, Lee Y, Kim HH (2012) TLT-1s, alternative transcripts of triggering receptor expressed on myeloid cell-like transcript-1 (TLT-1), inhibits the triggering receptor expressed on myeloid cell-2 (TREM-2)-mediated signaling pathway during osteoclastogenesis. J Biol Chem 287:29620–29626
Chung DH, Humphrey MB, Nakamura MC, Ginzinger DG, Seaman WE, Daws MR (2003) CMRF-35-like molecule-1, a novel mouse myeloid receptor, can inhibit osteoclast formation. J Immunol 171:6541–6548
Mori Y, Tsuji S, Inui M, Sakamoto Y, Endo S, Ito Y, Fujimura S, Koga T, Nakamura A, Takayanagi H, Itoi E, Takai T (2008) Inhibitory immunoglobulin-like receptors LILRB and PIR-B negatively regulate osteoclast development. J Immunol 181:4742–4751
Li S, Miller CH, Giannopoulou E, Hu X, Ivashkiv LB, Zhao B (2014) RBP-J imposes a requirement for ITAM-mediated costimulation of osteoclastogenesis. J Clin Invest 124:5057–5073
Everts V, de Vries TJ, Helfrich MH (2009) Osteoclast heterogeneity: lessons from osteopetrosis and inflammatory conditions. Biochim Biophys Acta 1792:757–765
Acknowledgments
We thank T. P. Quinn for helpful suggestions and editing the manuscript. M. B. H. is supported by NIH grant AR064211. M. C. N. is supported by a VA Merit Review, NIH grant AG046282, the UCSF-Stanford Arthritis Center of Excellence funded by the Great Western Region of the Arthritis Foundation, the Rheumatology Research Foundation, and the Russell/Engleman Rheumatology Research Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mary Beth Humphrey and Mary C. Nakamura declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Humphrey, M.B., Nakamura, M.C. A Comprehensive Review of Immunoreceptor Regulation of Osteoclasts. Clinic Rev Allerg Immunol 51, 48–58 (2016). https://doi.org/10.1007/s12016-015-8521-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-015-8521-8