Abstract
The stromal-vascular fraction (SVF), comprising heterogeneous cell populations and adipose-derived stromal cells (ADSCs), has therapeutic potential against osteoarthritis (OA); however, the underlying mechanism remains elusive. This study aimed to investigate the therapeutic effects of heterogeneous cells in rabbit SVF on rabbit chondrocytes. Rabbit SVF and ADSCs were autografted into knees at OA onset. The SVF (1 × 105) and low-dose ADSCs (lADSC; 1 × 104) groups adjusted for their stromal cell content were compared. Animals were euthanized 8 and 12 weeks after OA onset for macroscopic and histological analyses of OA progression and synovitis. Immunohistochemical and real-time polymerase chain reaction assessments were conducted. In vitro, immune-fluorescent double staining was performed for SVF to stain macrophages with F4/80, CD86(M1), and CD163(M2). OA progression was markedly suppressed, and synovitis was reduced in the SVF groups (OARSI histological score 8 W: 6.8 ± 0.75 vs. 3.8 ± 0.75, p = 0.001; 12 W: 8.8 ± 0.4 vs. 5.4 ± 0.49, p = 0.0002). The SVF groups had higher expression of collagen II and SOX9 in cartilage and TGF-β and IL-10 in the synovium, lower expression of MMP-13, and lower macrophage M1/M2 ratio than the lADSC groups. Immunofluorescent double staining revealed a markedly higher number of M2 than that of M1 macrophages in the SVF. The therapeutic effects of SVF on chondrocytes were superior than those of lADSCs, with enhanced anabolic and inhibited catabolic factors. Heterogeneous cells, mainly M2 macrophages in the SVF, enhanced growth factor secretion and chondrocyte-protective cytokines, thus benefiting chondrocytes and knee joint homeostasis. Overall, the SVF is a safe, relatively simple, and a useful treatment option for OA.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent years have witnessed progressive advances in the treatment of osteoarthritis (OA) owing to the advent of relatively new therapies that directly repair damaged tissue through the intra-articular injection of mesenchymal stromal/stem cells (MSCs) [1]. MSCs have therapeutic effects by suppressing inflammatory and immune-mediated responses through their paracrine effects on the host microenvironment and polarizing tissue-resident macrophages to an alternatively activated (M2) state. The significance of this existing paradigm is that the stem/progenitor function of MSC is independent of paracrine function and is not essential for anti-inflammatory or immunosuppressive function [2]. Therefore, in this study, we used the term “stromal cell” instead of “stem cell”. Adipose-derived stromal cells (ADSCs) are easily harvested from the adipose tissue in large quantities [3]. The therapeutic efficacy of ADSCs, as well as the potential of cell differentiation in adipogenesis, osteogenesis, chondrogenesis, and myogenesis, is comparable to that of bone marrow-derived mesenchymal stromal cells (BMSCs) against nerve injury and diabetic ulcers in animal models [3,4,5,6]. Therefore, the application of ADSCs in regenerative medicine has gained increased interest as an adjunctive therapy and showed promising results.
In addition, recent preclinical and clinical trials have reported the potential of the adipose-derived stromal-vascular fraction (SVF), comprising a heterogenous cell population in treating knee OA [7, 8]. SVF is obtained by digesting adipose tissues mechanically or enzymatically without the need for culturing, thus facilitating a one-step surgical process for regenerative treatment [9]. Additionally, SVF has been reported to be as effective as ADSCs in basic research studies [8,9,10,11,12]. Furthermore, the paracrine effects of SVF and ADSCs on chondrocytes determine their inhibitory effect on the development of OA [13, 14]. Moreover, recent systematic reviews and meta-analyses in clinical practice reported that SVF is a safe and useful treatment for OA, as it improved pain, functionality, and anatomy; however, small number of studies were conducted with different conditions [15,16,17,18]. However, the mechanisms underlying the effects of SVF on chondrocytes remain unclear.
SVF comprises heterogeneous cells, including ADSCs, macrophages, pericytes, fibroblasts, blood cells, endothelial cells, smooth muscle cells, and their progenitor cells [8]. The proportion of ADSCs in SVF varies widely, with values ranging from less than 1% to more than 16% [19]. Therefore, the therapeutic effects of SVF may be attributed to the functions of different cellular populations; however, the mechanisms of the paracrine effects of these heterogeneous cell populations on chondrocytes need to be explored [9, 20].
Among the heterogeneous cells in SVF, macrophages have received attention as a potential OA therapeutic target [21, 22]. Macrophages polarize into inflammation-induced (M1) or anti-inflammatory (M2) phenotypes. In particular, M2 macrophages induce the production of chondrogenic cytokines, including transforming growth factor (TGF)-β and interleukin (IL)-10, and play important roles in wound healing [23, 24]. The chondroprotective effect of IL-10 is mediated by the downregulation of inflammatory cytokines and chondrocyte apoptosis [25, 26]. Furthermore, articular chondrocytes secrete TGF-β and IL-10, and the expression of their respective receptor chains has been demonstrated [27, 28]. Macrophages comprise approximately 20% of SVF [29], and most macrophages in SVF belong to the M2 phenotype [30, 31]. Therefore, M2 macrophages are speculated to play an important role in determining the therapeutic potential of SVF on chondrocytes. However, there is a limited number of studies reporting on the paracrine effects of SVF or its macrophages on chondrocytes [32, 33]; these studies noted macrophage polarization and migration within the knee joint after intra-articular administration of SVF. However, they did not focus on macrophages as heterologous cells contained in SVF.
Therefore, this study primarily aimed to investigate the therapeutic effects of heterologous cells, including macrophages present in rabbit SVFs, on rabbit chondrocytes by comparing them to a control group and an ADSC group adjusted for ADSC content. The secondary objective was to investigate the mechanisms underlying the paracrine effects of SVF on chondrocytes compared to ADSCs. Our research question is “Is SVF more effective in promoting cartilage anabolism and inhibiting catabolism in a rabbit OA model compared to lADSCs containing the same amount of stem cells?” We hypothesized that treatment with SVF, in addition to the effect of ADSCs, promotes M2 polarization of macrophages in the synovium through the effect of M2 macrophages in heterologous cells and suppresses cartilage degeneration by promoting cartilage anabolism and inhibiting catabolism through the paracrine effect.
Materials and Methods
In Vivo Experiments
Establishment of Rabbit OA Model
Skeletally mature male New Zealand white rabbits (age: 6 months, body weight: 3.4 ± 0.2 kg) were used in this experiment. This study was approved by our institutional animal management and use committee. OA was surgically induced by anterior cruciate ligament (ACL) transection (ACLT) following the procedures described in previous studies [34, 35]. In the ACLT procedure, a 2 cm skin incision was made, and the ACL was exposed using the medial parapatellar approach. For optimal ACL visualization, the patella was moved laterally, and the knee was fully flexed. The tissue fragments between the upper and lower ligament stumps were removed as much as possible to prevent spontaneous ligament reattachment. To confirm that the ACL was completely transected, a gentle ACL test was performed. The joints were washed using sterile saline and closed. Surgical procedures were performed under sterile conditions and general anesthesia with isoflurane inhalation. Postoperative ACLT rabbits were allowed unrestricted cage activity. Rabbits were carefully observed for complications, such as infections. Rabbit OA models were established 8 weeks after ACLT following previous studies [34, 36]. Rabbits were euthanized at the onset of OA and at 8 and 12 weeks after onset of OA via intravenous injection of sodium pentobarbital to obtain knee-joint specimens. The study design is summarized in Supplementary Information 1. The independent variable was treatments of lADSC, hADSC, or SVF, while the dependent variable was their effect on OA progression.
Preparing SVF and ADSCs
SVF was isolated following the protocol described in a previous study [3, 37]. Rabbit adipose tissue (1.5 g) was collected from the adipose tissue pouch in the interscapular region along the dorsal line, which extends approximately 5 cm from the skull to the cranium. The obtained adipose tissue was washed using phosphate-buffered saline (PBS; Wako, Osaka, Japan) and shredded for 5 min. Afterward, collagenase D (Roche, Basel, Switzerland) was dissolved in 20 mL PBS (final concentration of 0.12%) and was added to the adipose tissue; digestion was then carried out in an incubator at 37 °C for 45 min. The mixture was infiltrated every 15 min during the digestion period. As soon as the reaction was complete, 20 mL Dulbecco’s modified Eagle’s Medium (DMEM; Sigma-Aldrich, St Louis, MO, USA) was added to stop collagenase activity and filtered using a cell strainer (BD Falcon™, Aichi, Japan). The resulting filtrate was centrifuged at 1,300 rpm for 6 min at 25 °C, the supernatant was removed, and the cell populations in the pellet were counted under a microscope.
SVF pellets were then seeded at a density of 5 × 104 cells/cm2 in tissue culture plates in DMEM complete medium supplemented with 10% fetal bovine serum (FBS), 100 units/mL penicillin (Sigma-Aldrich), and 100 µg/mL streptomycin (Sigma-Aldrich) in a humidified atmosphere of 5% CO2 and 95% air. According to previous reports, after culturing for 1 week, the cells were collected with trypsin-EDTA, centrifuged at 1,300 rpm for 6 min, and washed twice with PBS to obtain ADSCs [3, 38]. Cell populations in the pellets were counted using a microscope.
Cell counts of 1 × 105 SVFs and 1 × 105 and 1 × 104 ADSCs were prepared under sterile conditions in 1 mL rabbit serum albumin (RSA, 4%; Sigma-Aldrich) in a 1 mL syringe. The rabbits were divided into four groups and injected with 1 × 105 SVFs (SVF group), 1 × 105 ADSCs (high-dose ADSC; hADSC group), 1 × 104 ADSCs (low-dose ADSC; lADSC group), and 1 mL 4% RSA (control group). As SVF contains heterogeneous cells in addition to ADSCs, its therapeutic effect is thought to be mainly due to the synergistic effect of the functions of ADSCs and other cell populations [19, 39]. Therefore, based on previous reports [19] and the results of the colony-forming unit-fibroblast (CFU-F) assay (described later), in this study, the SVF/ADSC ratio was set at 10% and included an amount of ADSCs equivalent to that in the SVF and lADSC groups to determine the therapeutic potential of the heterogeneous cells in SVFs. To prevent articular cartilage damage, a needle was inserted into the knee joint, specifically behind the lateral edge of the patella at the femur-tibia junction, for sample injection into the joint capsule. This procedure was performed 8 weeks after ACL resection when the subject transitioned into an OA model. Subsequently, the knee was bent, and the rabbit was held in the same position for several minutes. Comparisons were made between the control, lADSC, hADSC, and SVF groups.
CFU-F Assay
SVF at 2 × 103 cells/cm2 were seeded in tissue culture plates containing DMEM supplemented with 10% FBS, 100 µg/mL streptomycin, 5 ng/mL fibroblast growth factor-2 (FGF-2; R&D Systems, Minneapolis, MN, USA), and 100 units/mL penicillin. The medium was replaced every 2–3 days to eliminate nonadherent cells. The cells were grown for 10–14 days, and the adherent cells were obtained from the cultures (n = 5). Once colonies were formed, the cells were stained with 0.5% crystal violet in methanol (Kanto Chemical Co., Ltd., Tokyo, Japan) for 10 min after removing the medium. Colonies comprised from more than 40 cells were sorted and counted under a microscope, and the number of colonies was normalized to that of the seeded cells [40].
Macroscopic Analysis
Macroscopic photographs were acquired using a Nikon D3000 camera (Nikon, Tokyo, Japan). Cartilage lesions of the rabbits were classified following the Osteoarthritis Research Society International (OARSI) OA Cartilage Histopathologic Assessment System and scored as reported in previous studies (n = 6) [41]. Two separate examiners (AK, YK) then performed a blind evaluation of each, and the average score was considered final.
Histological Analysis
For histological analysis, the femoral joint specimens from the four groups of rabbits were placed in 10% neutral buffered formalin (n = 5). The specimens were then decalcified using 4% ethylenediaminetetraacetic acid at room temperature (20–25℃) for 3 weeks. Specimens were then embedded with paraffin and cut into sagittal sections to generate thin sections of approximately 8 μm. The general morphology and proteoglycan content of cartilage tissue were assessed by safranin-O/fast green (Sigma-Aldrich) staining. Hematoxylin & eosin (H&E) staining was also performed to evaluate synovitis. Histological sections were visualized under a BZ-X700 microscope (Keyence, Osaka, Japan), evaluated by two separate examiners (AK, YK) in a blinded fashion, and quantified according to the OA Cartilage Histopathologic Assessment System of the OARSI [41]. The synovium was scored for synovitis using the modified OARSI score [41, 42].
Immunohistochemistry
Immunohistochemical examinations of the four groups were performed after deparaffinization (n = 5). To block endogenous peroxidase activity, the sections were incubated with 3% hydrogen peroxide (Wako Pure Chemicals, Osaka, Japan) for 30 min. Knee cartilage was evaluated using collagen type II (Collagen II) (1:25; Novus Biological, Littleton, CO, USA), SRY box (SOX)-9 (1:50; Santa Cruz Biotechnology, Santa Cruz, CA, USA), and matrix metalloproteinase (MMP)-13 (1:25; Thermo Fisher Scientific, Waltham, MA, USA) mouse monoclonal antibodies. Knee synovium was evaluated using CD86 (M1 macrophage marker) (1:50; Abcam, Tokyo, Japan) and CD163 (M2 macrophage marker) (1:50; Abcam). All antibody dilutions were prepared in PBS; after overnight incubation with primary antibodies at 4 °C, the sections were stained with horseradish peroxidase-conjugated anti-mouse immunoglobulin G antibody (N-Histofine Simple Stain MAXPO; Nichirei Bioscience, Tokyo, Japan) and incubated at room temperature for 30 min. Signals were detected using 3,3′-diaminobenzidine (Histofine Simple Stain DAB solution; Nichirei Bioscience) and generated as a brown reaction product.
Semi-quantitative immunohistochemistry analysis was performed using six microscopic fields of view (×100 magnification) on the anterior, central, and posterior regions of cartilage tissue. For complete protein expression evaluation, a semi-quantitative method of assigning immunohistochemical values as a percentage of positive regions (collagen II) or positive cells (SOX-9 and MMP-13) was employed with a maximum value of 100%. The M1/M2 (CD86/163) ratio was used to evaluate macrophage counts in the synovium. The average of the gray values normalized by the number of nuclei was estimated to determine the expression levels, as described in a previous study [43]. Analyses were performed by two investigators (KA and YK) in a blinded manner.
RT-PCR
For RT-PCR analysis, knee joint specimens were collected from the control, lADSC, hADSC, and SVF groups; knee joint cartilage tissue and synovial membrane were harvested. Articular cartilage was obtained by exposing the femoro-tibial joint and scraping off the surrounding articular cartilage causing OA using a scalpel. Total RNA was extracted from chondrocytes and synovium using the Trizol®LS reagent (Thermo Fisher Scientific) and the RNeasy® Mini Kit (Qiagen, Valencia, CA, USA) and reverse transcribed using the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA). RT-PCR amplification of cDNA was performed in duplicate on an Applied Biosystems 7500 RT-PCR system (Thermo Fisher Scientific). Primers used in the RT-PCR (Table 1) were synthesized by Thermo Fisher Scientific Inc. The mRNA expression levels in chondrocytes and synovium in the four groups were evaluated using RT-PCR and compared to the glyceraldehyde 3-phosphate dehydrogenase levels (n = 6).
In Vitro Experiments
Pellet Co-Culture
Isolation and culture of primary cultured chondrocytes were performed using knee articular cartilage tissue harvested from a rabbit OA model 8 weeks after the ACLT. Surgeries were performed under sterile conditions and general anesthesia. After harvesting, the joints were washed with sterile saline and closed. Subsequently, sliced thin cartilage tissue was stripped, diced, and digested in DMEM containing 0.2% collagenase D for 2 h 30 min. A nylon filter (70 mm) was used to remove undigested cartilage. Subsequently, the pellet was harvested by removing the supernatant after centrifuging at 1,200 rpm for 5 min at 25 °C. The chondrocyte pellets were resuspended in DMEM, including 10% FBS supplemented with 100 units/mL penicillin, 100 mg/mL streptomycin solution, and 0.1 mM dexamethasone (Sigma-Aldrich). The chondrocytes were then incubated at 37 °C in a humidified atmosphere of 5% CO2/95% air. Chondrocytes were grown in a monolayer and passaged when confluence was reached— the chondrocyte cells after two passages were used for the assay. Additionally, a separate co-culture system was used to confirm the paracrine effects of SVF and lADSCs on chondrocytes. SVF and ADSCs were isolated from rabbits whose cartilages had previously been harvested. Chondrocyte pellets (1 × 105 cells) were converted to a chondrogenic medium by adding DMEM containing 15% FBS, 100 U/mL penicillin, and 100 mg/mL streptomycin. The medium was converted to a chondrogenic medium by adding DMEM containing 0.1 mM dexamethasone, 0.4 mM proline (Sigma-Aldrich), 1% insulin-transferrin-sodium selenite (Sigma-Aldrich), 50 mM ascorbic acid-2-phosphate (Sigma-Aldrich), and 500 ng/mL osteogenic protein-6 (Sigma-Aldrich). Chondrocyte aliquots were centrifuged at 1,200 rpm for 5 min into pellets and were collected at the bottom of a 15 mL tube. Pellets and SVF (1 × 105 cells) or lADSC (1 × 104 cells) were separated in sterile culture plate inserts (Millicell; Millipore, Burlington, MA, USA). A control group was established with no cells in membrane plates and only OA chondrocytes in 15 mL tubes. To clearly confirm the therapeutic effect of heterologous cells contained in SVF, in vitro experiments and comparison with lADSC containing the same amount of stromal cells were performed; consequently, the hADSC group was excluded. Pellets were incubated at 37 °C under 5% CO2; the medium was changed every 2–3 days (n = 5). After 3 weeks, pellet sizes were evaluated and stained using safranin-O.
Enzyme-Linked Immunosorbent Assay (ELISA)
After 48 h of pellet co-culture, supernatants from the first exchange were collected. The concentrations of growth factors and cytokines released in control, lADSC, and SVF groups were determined following the manufacturer’s protocol provided along with sandwich ELISA kits (TGF-β: LifeSpan Biosciences, Seattle, USA; IL-10: Novus Biologicals, Colorado, USA). IL-10 was five-fold concentrated using Amicon Ultra® centrifugal filters (Merck, Darmstadt, Germany) and measured (n = 5). Results were normalized to the amount of DNA in the control group.
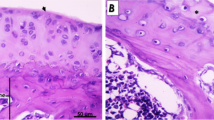
Immunohistochemical Staining of Macrophages
Fresh SVF (1 × 105 cells) and ADSCs (1 × 105 cells) were washed with PBS for 5 min and treated with 0.3% H2O2 and methanol for 20 min. Cells were treated with 5% normal goat serum prepared in PBS and 0.3% Triton X-100 (blocking buffer) for 1 h at 37 °C. Immunohistochemistry was performed with anti-F4/80 (1:200; Synaptic Systems, Göttingen, Germany) and anti-CD86 (1:200; Abcam, Tokyo, Japan) antibodies. In addition, double staining with anti-F4/80 and anti-CD163 antibodies (1:200, Abcam, Tokyo, Japan) was performed. F4/80 was used as pan-macrophage, CD86 as M1 macrophage phenotype, and CD163 as M2 macrophage phenotype marker. After incubation with primary antibodies for 1 h at room temperature, samples were incubated with Alexa Fluor® 488-conjugated donkey anti-rat IgG (1:1000; Bethyl Laboratories, Montgomery, AL, USA) or Alexa Fluor® 594-conjugated goat anti-mouse (1:1000; A90-131D4, Bethyl Laboratories) for 2 h at room temperature. Cells were finally counterstained with DAPI (Thermo Fisher Scientific), and fluorescent signals were captured using fluorescence microscopy. The percentage of CD163-positive cells compared to CD86-positive cells among F4/80-positive cells was also evaluated. Cell counts were examined by two blinded observers (KA and YK) in five fields of view. The average percentage of CD86- and CD163-positive cells relative to F4/80-positive cells was calculated (n = 5).
Statistical Analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) software (version 16.0, IBM Corp., Armonk, NY, USA). Results are presented as the mean ± standard deviation (SD). The chi-square test or one-way analysis of variance followed by a posteriori Tukey’s test was performed to compare the results between the groups. Statistical significance was set at p < 0.05.
Results
In Vivo Experiments
SVF Suppressed OA Progression More Effectively Compared to ADSC Adjusted to the Same Amount of Stromal Cells
In macroscopic analysis, control group demonstrated severe progression of cartilage erosion during twelve weeks after OA onset. lADSC group showed moderate progression of macroscopic cartilage fibrillation at eight and twelve weeks after OA onset, with lower OARSI score compared to control groups. However, cartilages treated with SVF showed mild macroscopic progression of cartilage degeneration compared to IADSC group with lower OARSI score at 8 and 12 weeks post OA onset. Besides, the OARSI score in the hADSC and SVF groups did not differ significantly (Fig. 1a).
a Macroscopic analysis of femoral condyles. Typical specimens at the onset of osteoarthritis (OA) (8 weeks after ACLT) and 8 and 12 weeks after OA onset. The surface of the cartilage was stained with India ink to confirm fibrosis and erosion. Macroscopic OA score at 8 weeks and 12 weeks after OA onset in each group. b Histological analysis of femoral condyles. Safranin-O/fast green staining of a typical specimen at OA onset (8 weeks after ACLT) and 8 and 12 weeks after OA onset. Scale bar = 100 μm. OARSI scores at 8 weeks and 12 weeks after OA onset in each group. c Histological analysis of synovium. H&E staining of a typical specimen 8 weeks after OA onset. Modified OARSI synovitis scores at 8 weeks after OA onset for each group
In histological evaluation, articular cartilage at 8 and 12 weeks showed the same trend as macroscopic evaluation. Importantly, histological findings in the control group showed the progression of OA changes, including the loss of proteoglycans and chondrocyte density in the superficial and intermediate layers of the cartilage layer. The lADSC group also showed a progression of OA changes, including the loss of proteoglycans in the intermediate zone and the loss of chondrocyte density in the midzone, with lower OARSI score compared to control groups, although to a lesser extent. However, hADSCs and SVF prevented the development of OA with retention of cartilage matrix. The OARSI scores in lADSC, hADSC, and SVF groups were markedly lower than those in the control group at both 8 and 12 weeks after OA onset. Moreover, the OARSI scores were considerably lower in the SVF group than those in the lADSC group; however, no significant differences were observed between the OARSI scores in the hADSC and SVF groups (Fig. 1b). In the synovium, the control group showed synovitis with lymphocytic infiltration and multilayering. In contrast, the lADSC group showed synovitis with mild multilayering, and the hADSC and SVF groups showed only mild synovitis. The modified OARSI scores for synovitis were also considerably lower in the lADSC, hADSC, and SVF groups than in the control group at 8 weeks after the onset of OA. In addition, the score was considerably lower in the SVF group than in the lADSC group at 8 weeks after the onset of OA, but the modified OARSI scores in the hADSC and SVF groups did not show significant differences (Fig. 1c).
SVF Promoted Cartilage Anabolism and Inhibited Cartilage Catabolism
In immunohistochemical analysis, lADSC, hADSC and SVF treatments showed evidence of a chondroprotective effect, with the control group scoring markedly higher than the control group at 8 and 12 weeks in the immunohistochemical staining of collagen II after the onset of OA. They promoted the expression of large amounts of collagen II in cartilage tissues compared to the control group. In addition, a remarkably greater positive area was detected in the SVF group than in the lADSC group. In contrast, no significant differences were observed in the positive areas between the hADSC and SVF groups (Fig. 2a). At 8 and 12 weeks after OA onset, lADSC, hADSC and SVF groups promoted higher SOX9 expression in cartilage tissue than in the control group, with the control group showing a marked reduction in chondroprotection in the immunohistochemical staining. In addition, a considerably higher percentage of positive regions were detected in the SVF group than in the lADSC group. No significant difference in positive cell ration was observed between the hADSC and SVF groups (Fig. 2b). The expression of MMP-13 was relatively high in the control group compared to that in the other three groups at 8 and 12 weeks. Moreover, a considerably lower percentage of positive cells was detected in the SVF group than in the lADSC group, whereas hADSC and SVF groups did not show significant differences in positive cell ratio (Fig. 2c). Furthermore, In RT-PCR of chondrocytes, Collagen II and SOX9 expression was extensively higher and MMP-13 expression was considerably lower in chondrocytes from the lADSC, hADSC and SVF groups than those in chondrocytes from the control group at 8 and 12 weeks after OA onset. In addition, collagen II and SOX9 expression was considerably higher and MMP-13 expression was lower in the SVF group than in the lADSC group. In contrast, no significant differences were observed in collagen II, SOX9, and MMP-13 expression between the hADSC and SVF groups (Fig. 2d).
a Immunohistochemical analysis of collagen II in cartilage. Representative samples at 8 and 12 weeks after OA onset. Scale bar = 100 mm. Percentage of collagen II positive areas at 8 weeks and 12 weeks after OA onset in each group. b Immunohistochemical analysis of SOX-9 in cartilage. Representative samples at 8 and 12 weeks after OA onset. Scale bar = 100 mm. Percentage of SOX-9 positive cells at e 8 weeks and 12 weeks after OA onset in each group. c Immunohistochemical analysis of MMP-13 in cartilage. Representative samples at 8 and 12 weeks after OA onset. Scale bar = 100 mm. Percentage of MMP-13 positive cells 8 weeks and 12 weeks after OA onset in each group. d Real-time PCR (RT-PCR) of collagen II, SOX9, MMP13. RT-PCR of collagen II, SOX9, and MMP13 expression performed using total RNA extracted from rabbit chondrocytes 8 and 12 weeks after OA onset
SVF Increased M2 Macrophage Polarization in Synovium
Immunohistochemical findings in synovial tissues showed that the CD86/CD163 expression ratio (M1/M2 ratio) was considerably lower in the lADSC, hADSC and SVF groups than that in the control group at 8 weeks post-OA onset, indicating increased M2 macrophage infiltration. Moreover, the M1/M2 ratio was remarkably lower in the SVF group than that in the lADSC group, while no significant difference was observed in M1/M2 ratio between the hADSC and SVF groups (Fig. 3a). Additionally, in RT-PCR of synovial cells, the expression of TGF-β and IL10 was remarkably higher, and MMP-13 was remarkably lower in the lADSC, hADSC and SVF groups than in the control group at 8 and 12 weeks after OA onset. In addition, the expression of TGF-β and IL10 was extensively higher, and that of MMP-13 was extensively lower in the SVF group than in the lADSC group, whereas no significant differences were observed between the hADSC and SVF groups (Fig. 3b).
a Immunohistochemical analysis of CD86 and CD163 in synovial tissue. Representative samples 8 weeks after OA onset. Scale bar = 100 mm. CD86/CD163 expression ratio (M1/M2 ratio) in each group. The sections were counterstained with hematoxylin. b Real-time PCR (RT-PCR) of TGF-β, IL-10 and MMP13 expression. RT-PCR of TGF-β, IL-10, and MMP13 using total RNA extracted from rabbit synovial cells 8 and 12 weeks after OA onset
In Vitro Experiments
SVF Contained M2 Polalyzed Macrophages, Secreted Significantly More Growth and Anti-Inflammatory Factors, and Increased Chondrogenesis Compared to lADSC Adjusted to the Same Amount of Stromal Cells
Pellet Co-Culture
Pellet co-cultures were performed to evaluate the proliferation of chondrocytes when cultured in the presence of SVF and ADSC paracrine factor (Fig. 4a). Pellets from all groups stained positive for safranin-O and exhibited a vitreous extracellular matrix containing round chondrocytes. Pellet size analysis revealed that the co-cultured chondrocytes formed markedly larger pellets in the lADSC and SVF groups than in the control group, with the pellet size of the SVF group being markedly larger than that of the lADSC group (Fig. 4b).
a Separated pellet co-culture system. ADSC and SVF groups were established between each administered cell in membrane plates and OA chondrocytes in 15 mL tubes. A control group was established with no cells in membrane plates and only OA chondrocytes in 15-mL tubes. b Gross photographs and safranin-O staining of the resulting pellets in each group. Pellet size in each group. c Representative double immunostaining of rabbit F4/80 (green) and rabbit CD86 (red) in ADSC and SVF groups. Scale bar: 20 μm for the right panel and 50 μm for the other panels. Representative double immunostaining of rabbit F4/80 (green) and rabbit CD163 (red) in the two groups. Scale bar: 20 μm for the right panel and 50 μm for the other panel. Comparison of the ratio of CD86-positive to CD163-positive cells in F4/80-positive cells by immunohistochemical staining
ELISA in the Co-Culture Medium
TGF-β and IL-10 levels between the three groups differed extensively in the co-culture medium. They were the highest in the SVF group, followed by the lADSC group, and the lowest in the control group (TGF-β: Mean ± SD; control:386.3 ± 54.6, lADSC:773.0 ± 129.0, SVF:1108.0 ± 147.8, SVF vs. lADSC: p = 0.0044, SVF vs. control: p < 0.0001, lADSC vs. control: p = 0.0015; IL-10: Mean ± SD; control:9.3 ± 1.28, lADSC:23.7 ± 3.5, SVF:49.0 ± 4.6, SVF vs. lADSC: p < 0.0001, SVF vs. control: p < 0.0001, lADSC vs. control: p = 0.0002).
Immunohistochemistry of Macrophages in SVF
Macrophages in fresh SVF were labeled with F4/80. The number of macrophages in SVF double-stained with F4/80 and CD163 was higher than those stained with either F4/80 or CD86. However, in ADSCs, no cells were labeled with F4/80, CD86, or CD163. The percentage of CD163-positive cells in SVF relative to F4/80-positive cells was markedly higher than for CD86-positive cells (Fig. 4c).
Discussion
In the present study, macroscopic, histological, and molecular analyses were performed in vivo using a rabbit experimental OA model to assess the therapeutic effect of SVF and ADSCs on OA. Macroscopic and histological analysis revealed that the SVF group was superior to the lADSC group in inhibiting OA progression and synovitis and was almost equivalent to the hADSC group. In addition, the immunohistochemical staining and expression of collagen II and SOX9 was the highest in the hADSC and SVF groups, followed by the lADSC group, and was the lowest in the control group at 8 and 12 weeks post-OA onset. Sox-9, a chondrogenic transcription factor, plays a crucial role in increasing chondrogenesis, particularly by activating the co-expression of collagen II [44, 45]. Taken together, the findings of the previous [14, 46] and the present studies suggest that intra-articularly injected SVF and ADSCs promote the secretion of anabolic factors in chondrocytes. In contrast, the immunohistochemical staining and mRNA expression of MMP-13 was low in the lADSC-, hADSC-, and SVF-injected knees compared to 4% RSA-injected knees; the suppression of its expression was higher in the SVF group than in the control and lADSC groups but was comparable to that of the hADSC group. MMP-13 has been reported to be involved in cartilage damage in OA [47] and is used as an indicator of OA treatment efficacy in OA models in vivo [38]. In summary, in vivo, the SVF treatment showed considerably increased anabolic and reduced catabolic effects on the cartilage compared to the control and lADSC treatments; however, these effects of SVF treatment were comparable to those of hADSC.
Next, we explored the involvement of macrophage in the synovium in the in vivo experimental OA model to understand the underlying mechanism of the OA-alleviating effects of SVF and ADSCs on chondrocytes. Recent studies suggest that macrophages in the synovium play a key role in OA pathogenesis [21, 22, 48]. In vivo, M1 macrophages in the synovium aggravate experimental OA, while M2 macrophages reduce its progression [21, 49]. In particular, an increased M1/M2 ratio is associated with increased expression of inflammatory cytokines and has been shown to induce OA [50]. In this study, lADSCs, hADSCs, and SVF treatments extensively ameliorated synovitis in the synovium and reduced the M1/M2 ratio at 8 weeks after OA onset compared to control treatment. Previous studies reported that ADSCs had an anti-inflammatory effect due to the M2 macrophage polarization [51, 52]. The translocation of intra-articularly administered SVF to the synovium was reported to increase the number of M2-like macrophages in the synovium in an OA mouse model [33]. The co-culture of macrophages with SVF markedly increased the percentage of M2 macrophage-positive markers [33]. In the present study, the synovitis, M1/M2 macrophage ratio, and M2 macrophage polarization were markedly improved in the SVF group compared to those in the control and lADSC groups. Taken together, we inferred that immunomodulation via macrophage polarization to the synovium induced by intra-articular injections of SVF and ADSCs contributes to the attenuation of OA in rabbits. In addition, the present study also demonstrated that at 8 and 12 weeks post-OA onset, expression of TGF-β and IL-10, which are expected to be secreted by M2 macrophages, was considerably increased, while that of MMP-13, a catabolic factor, was considerably suppressed in the synovial cells of lADSC, hADSC, and SVF groups compared to those in the synovial cells of the control group. These results suggest that the OA-alleviating effect of SVF is also attributed to the paracrine effect of M2 macrophages, which may improve synovial membrane and knee joint homeostasis and cartilage protection.
Furthermore, we performed in vitro experiments to confirm the findings of our in vivo experiments. Previous studies reporting the paracrine effects of SVF and ADSCs demonstrated an increase in chondrogenesis in the co-culture of chondrocytes with SVF and ADSCs [14, 53], thus confirming that SVF and ADSCs can promote the release of collagen II and SOX-9 expression in chondrocytes [13]. In this study, the separated pellet co-culture had a markedly larger pellet size in the SVF group than that in the control and lADSC groups. In addition, the levels of TGF-β and IL-10, the paracrine factors in ADSCs [54, 55], were higher in the SVF group than in the lADSC group, as detected via ELISA using the culture medium at the first exchange. These results indicate that SVF paracrine factors may be secreted not only by ADSCs, but also by other heterogeneous cells in SVF. Immunohistochemical staining also confirmed the anti-inflammatory phenotype of most macrophages in SVF by double staining with F4/80 and CD163. However, cells were not stained with F4/80 in the ADSC group, which may be attributed to the fact that ADSCs are pure stem cells. Macrophages comprise approximately 20% of the SVF [28], and approximately 80% of these macrophages were also positive for F4/80, a pan-macrophage cell surface marker, and approximately 70% for the M2 anti-inflammatory marker [30, 31]. These results are similar to what we obtained in this study. M2 macrophages secrete TGF-β and IL-10, induce collagen II expression in chondrocytes, and decrease MMP-13 expression [56]. Additionally, TGF-β has been reported to contribute to chondrocyte regeneration partially through the Smad2/3 signaling pathway [57]. Macrophages that have acquired the M2 phenotype upregulated the expression of anti-inflammatory cytokines, including IL-10 and TGF-β, upon coculture with MSCs and ADSCs [58]. In summary, a comparison of SVF and lADSCs suggests that the effect of SVF may be attributed to its heterogeneous cell composition, mainly comprising M2 macrophages, which are responsible for the secretion of growth factors and cartilage-protective cytokines, such as TGF-β and IL-10, which may contribute to the therapeutic effect of SVF on chondrocytes.
In addition, SVF has advantages in clinical use. In terms of cell harvesting, both SVF and ADSC have a lower donor site morbidity than BMSC [2,3,4,5,6,7]. Furthermore, SVF is obtained by mechanical or enzymatic digestion of adipose tissues, without the need for culture, thus making it easier and safer to use than ADSCs, which require weeks of cell culture [59, 60]. SVF is safe, feasible, and advantageous compared to ADSCs because it provides adequate cell numbers without culture or multiple passages [61]. Recently, the usefulness of intraoperative cell isolation and seeding techniques for creating scaffolds for in situ tissue-engineered grafts directly in the operating room has been reported for the treatment of bone defects [62, 63]. These techniques may also be applicable to the treatment of OA, and it is possible that SVF harvested during surgery, encapsulated in the scaffold, and implanted in situ in cartilage defects may be more effective than intra-articular injection of SVF. However, in dermatology, limited efficacy of MSCs alone in the treatment of diabetic skin ulcers and failure to achieve complete recovery have been reported [64]. A better therapeutic effect may be achieved by using adjuvant therapy such as the aforementioned scaffold in combination with SVF [62, 63].
Our study had some limitations. First, we administered SVF and ADSC in fixed doses via single injection; however, the optimal dose in the rabbit model has not yet been determined. Second, we used a rabbit OA model for this experiment. Because rabbits are quadrupeds, the established OA model may not necessarily translate to a human model owing to differences in postural and gait dynamics between rabbits and humans. Third, although the normal lifespan of a New Zealand rabbit is approximately 5 years, the New Zealand rabbits used in this study were only 6 months old; thus, they may not correspond to the changes in OA in middle-aged humans. Fourth, adding a healthy group as a control group may lead to a more accurate judgment of the therapeutic effect in each group. Lastly, histological and immunohistochemical evaluations in this study were performed primarily using semi-quantitative methods; therefore, more objective and accurate quantitative methods should be taken into consideration in future research.
Conclusion
Both SVF and hADSCs promoted chondrocyte anabolism and inhibited catabolism compared to controls and lADSCs; however, no significant differences were observed between them. The therapeutic effect of SVF was superior to that of lADSCs containing the same amount of stromal cells. Heterogeneous cells in SVF, particularly the M2 macrophages, promoted the secretion of growth factors and chondrocyte-protective cytokines, which could have contributed to the therapeutic effect of SVF on chondrocytes and maintenance of homeostasis in the knee joint. Moreover, the method of SVF collection was simpler than that used for ADSCs. Collectively, we concluded that SVF has some advantages over ADSC and may be a useful treatment option for OA.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
References
Agarwal, N., Mak, C., Bojanic, C., To, K., & Khan, W. (2021). Meta-analysis of adipose tissue derived cell-based therapy for the treatment of knee osteoarthritis. Cells,10(6), 1365. https://doi.org/10.3390/cells10061365
Phinney, D. G., Lee, H., & Boregowda, S. V. (2023). Revisiting the mesenchymal “stem vs. stromal” cell dichotomy and its implications for development of improved potency metrics. Stem Cells,41(5), 444–452. https://doi.org/10.1093/stmcls/sxad019
Zuk, P. A., Zhu, M., Mizuno, H., Huang, J., Futrell, J. W., Katz, A. J., et al. (2001). Multilineage cells from human adipose tissue: Implications for cell-based therapies. Tissue Engineering,7(2), 211–228. https://doi.org/10.1089/107632701300062859
Feng, Z., Ting, J., Alfonso, Z., Strem, B. M., Fraser, J. K., Rutenberg, J., Kuo, H. C., & Pinkernell, K. (2010). Fresh and cryopreserved, uncultured adipose tissue-derived stem and regenerative cells ameliorate ischemia-reperfusion-induced acute kidney injury. Nephrology Dialysis Transplantation: Official Publication of the European Dialysis and Transplant Association – European Renal Association,25(12), 3874–3884. https://doi.org/10.1093/ndt/gfq603
Li, M., Lei, H., Xu, Y., Li, H., Yang, B., Yu, C., et al. (2018). Exosomes derived from mesenchymal stem cells exert therapeutic effect in a rat model of cavernous nerves injury. Andrology,6(6), 927–935. https://doi.org/10.1111/andr.12519
Pomatto, M., Gai, C., Negro, F., Cedrino, M., Grange, C., Ceccotti, E., et al. (2021). Differential therapeutic effect of extracellular vesicles derived by bone marrow and adipose mesenchymal stem cells on wound healing of diabetic ulcers and correlation to their cargoes. International Journal of Molecular Sciences,22(8), 3851. https://doi.org/10.3390/ijms22083851
Hong, Z., Chen, J., Zhang, S., Zhao, C., Bi, M., Chen, X., & Bi, Q. (2019). Intra-articular injection of autologous adipose-derived stromal vascular fractions for knee osteoarthritis: A double-blind randomized self-controlled trial. International Orthopaedics,43(5), 1123–1134. https://doi.org/10.1007/s00264-018-4099-0
Biazzo, A., D’Ambrosi, R., Masia, F., Izzo, V., & Verde, F. (2020). Autologous adipose stem cell therapy for knee osteoarthritis: Where are we now? Physician and Sportsmedicine,48(4), 392–399. https://doi.org/10.1080/00913847.2020.1758001
van Dijk, A., Naaijkens, B. A., Jurgens, W. J. F. M., Nalliah, K., Sairras, S., van der Pijl, R. J., et al. (2011). Reduction of infarct size by intravenous injection of uncultured adipose derived stromal cells in a rat model is dependent on the time point of application. Stem Cell Research,7(3), 219–229. https://doi.org/10.1016/j.scr.2011.06.003
You, D., Jang, M. J., Kim, B. H., Song, G., Lee, C., Suh, N., et al. (2015). Comparative study of autologous stromal vascular fraction and adipose-derived stem cells for erectile function recovery in a rat model of cavernous nerve injury. Stem Cells Translational Medicine,4(4), 351–358. https://doi.org/10.5966/sctm.2014-0161
Domergue, S., Bony, C., Maumus, M., Toupet, K., Frouin, E., Rigau, V., et al. (2016). Comparison between stromal vascular fraction and adipose mesenchymal stem cells in remodeling hypertrophic scars. PLOS ONE,11(5), e0156161. https://doi.org/10.1371/journal.pone.0156161
Shimizu, M., Matsumine, H., Osaki, H., Ueta, Y., Tsunoda, S., Kamei, W., et al. (2018). Adipose-derived stem cells and the stromal vascular fraction in polyglycolic acid-collagen nerve conduits promote rat facial nerve regeneration. Wound Repair and Regeneration: Official Publication of the Wound Healing Society [And] the European Tissue Repair Society,26(6), 446–455. https://doi.org/10.1111/wrr.12665
Shi, J., Liang, J., Guo, B., Zhang, Y., Hui, Q., Chang, P., & Tao, K. (2017). Adipose-derived stem cells cocultured with chondrocytes promote the proliferation of chondrocytes. Stem Cells International,2017, 1709582. https://doi.org/10.1155/2017/1709582
Kuroda, Y., Matsumoto, T., Hayashi, S., Hashimoto, S., Takayama, K., Kirizuki, S., et al. (2019). Intra-articular autologous uncultured adipose-derived stromal cell transplantation inhibited the progression of cartilage degeneration. Journal of Orthopaedic Research: Official Publication of the Orthopaedic Research Society,37(6), 1376–1386. https://doi.org/10.1002/jor.24174
Boada-Pladellorens, A., Avellanet, M., Pages-Bolibar, E., & Veiga, A. (2022). Stromal vascular fraction therapy for knee osteoarthritis: A systematic review. Therapeutic Advances in Musculoskeletal Disease,14, 1759720X221117879. https://doi.org/10.1177/1759720X221117879
Bolia, I. K., Bougioukli, S., Hill, W. J., Trasolini, N. A., Petrigliano, F. A., Lieberman, J. R., & Weber, A. E. (2022). Clinical efficacy of bone marrow aspirate concentrate versus stromal vascular fraction injection in patients with knee osteoarthritis: A systematic review and meta-analysis. American Journal of Sports Medicine,50(5), 1451–1461. https://doi.org/10.1177/03635465211014500
Shah, S., Otsuka, T., Bhattacharjee, M., & Laurencin, C. T. (2021). Minimally invasive cellular therapies for osteoarthritis treatment. Regenerative Engineering and Translational Medicine,7(1), 76–90. https://doi.org/10.1007/s40883-020-00184-w
Schmitz, C., Alt, C., Pearce, D. A., Furia, J. P., Maffulli, N., & Alt, E. U. (2022). Methodological flaws in meta-analyses of clinical studies on the management of knee osteoarthritis with stem cells: A systematic review. Cells,11(6), 965. https://doi.org/10.3390/cells11060965
Aronowitz, J. A., Lockhart, R. A., & Hakakian, C. S. (2015). Mechanical versus enzymatic isolation of stromal vascular fraction cells from adipose tissue. Springerplus,4, 713. https://doi.org/10.1186/s40064-015-1509-2
Semon, J. A., Zhang, X., Pandey, A. C., Alandete, S. M., Maness, C., Zhang, S., et al. (2013). Administration of murine stromal vascular fraction ameliorates chronic experimental autoimmune encephalomyelitis. Stem Cells Translational Medicine,2(10), 789–796. https://doi.org/10.5966/sctm.2013-0032
Zhang, H., Lin, C., Zeng, C., Wang, Z., Wang, H., Lu, J., et al. (2018). Synovial macrophage M1 polarisation exacerbates experimental osteoarthritis partially through R-spondin-2. Annals of the Rheumatic Diseases,77(10), 1524–1534. https://doi.org/10.1136/annrheumdis-2018-213450
Sun, Y., Zuo, Z., & Kuang, Y. (2020). An emerging target in the battle against osteoarthritis: Macrophage polarization. International Journal of Molecular Sciences,21(22), 1–19. https://doi.org/10.3390/ijms21228513
Fernandes, T. L., Gomoll, A. H., Lattermann, C., Hernandez, A. J., Bueno, D. F., & Amano, M. T. (2020). Macrophage: A potential target on cartilage regeneration. Frontiers in Immunology,11, 111. https://doi.org/10.3389/fimmu.2020.00111
Qureshi, H. Y., Sylvester, J., el Mabrouk, M., & Zafarullah, M. (2005). TGF-beta-induced expression of tissue inhibitor of metalloproteinases-3 gene in chondrocytes is mediated by extracellular signal-regulated kinase pathway and Sp1 transcription factor. Journal of Cellular Physiology,203(2), 345–352. https://doi.org/10.1002/jcp.20228
Wang, Y., & Lou, S. (2001). Direct protective effect of interleukin-10 on articular chondrocytes in vitro. Chinese Medical Journal,114(7), 723–725.
Wojdasiewicz, P., Poniatowski, ŁA., & Szukiewicz, D. (2014). The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of osteoarthritis. Mediators of Inflammation,2014, 561459. https://doi.org/10.1155/2014/561459
Iannone, F., de Bari, C., Dell’Accio, F., Covelli, M., Patella, V., lo Bianco, G., & Lapadula, G. (2002). Increased expression of nerve growth factor (NGF) and high affinity NGF receptor (p140 TrkA) in human osteoarthritic chondrocytes. Rheumatology,41(12), 1413–1418. https://doi.org/10.1093/rheumatology/41.12.1413
Parker, W. L., Finnson, K. W., Soe-Lin, H., Knaus, P., & Philip, A. (2007). Expression and function of TbetaRII-B, a variant of the type II TGF-beta receptor, in human chondrocytes. Osteoarthritis and Cartilage,15(4), 442–453. https://doi.org/10.1016/j.joca.2006.10.006
Morris, M. E., Beare, J. E., Reed, R. M., Dale, J. R., LeBlanc, A. J., Kaufman, C. L., et al. (2015). Systemically delivered adipose stromal vascular fraction cells disseminate to peripheral artery walls and reduce vasomotor tone through a CD11b + cell-dependent mechanism. Stem Cells Translational Medicine,4(4), 369–380. https://doi.org/10.5966/sctm.2014-0252
Lumeng, C. N., Delproposto, J. B., Westcott, D. J., & Saltiel, A. R. (2008). Phenotypic switching of adipose tissue macrophages with obesity is generated by spatiotemporal differences in macrophage subtypes. Diabetes,57(12), 3239–3246. https://doi.org/10.2337/db08-0872
Potente, M., Gerhardt, H., & Carmeliet, P. (2011). Basic and therapeutic aspects of angiogenesis. Cell,146(6), 873–887. https://doi.org/10.1016/j.cell.2011.08.039
Desando, G., Bartolotti, I., Martini, L., Giavaresi, G., Nicoli Aldini, N., Fini, M., et al. (2019). Regenerative features of adipose tissue for osteoarthritis treatment in a rabbit model: Enzymatic digestion versus mechanical disruption. International Journal of Molecular Sciences,20(11), 2636. https://doi.org/10.3390/ijms20112636
Kamada, K., Matsushita, T., Yamashita, T., Matsumoto, T., Iwaguro, H., Sobajima, S., & Kuroda, R. (2021). Attenuation of knee osteoarthritis progression in mice through polarization of M2 macrophages by intra-articular transplantation of non-cultured human adipose-derived regenerative cells. Journal of Clinical Medicine,10(19), 4309. https://doi.org/10.3390/jcm10194309
Grigolo, B., Lisignoli, G., Desando, G., Cavallo, C., Marconi, E., Tschon, M., et al. (2009). Osteoarthritis treated with mesenchymal stem cells on hyaluronan-based scaffold in rabbit. Tissue Engineering Part C Methods,15(4), 647–658. https://doi.org/10.1089/ten.TEC.2008.0569
Vignon, E., Bejui, J., Mathieu, P., Hartmann, J. D., Ville, G., Evreux, J. C., & Descotes, J. (1987). Histological cartilage changes in a rabbit model of osteoarthritis. Journal of Rheumatology, 14, Spec No, 104–106.
Desando, G., Cavallo, C., Sartoni, F., Martini, L., Parrilli, A., Veronesi, F., et al. (2013). Intra-articular delivery of adipose derived stromal cells attenuates osteoarthritis progression in an experimental rabbit model. Arthritis Research and Therapy,15(1), R22. https://doi.org/10.1186/ar4156
Kosaka, M., Nakase, J., Hayashi, K., & Tsuchiya, H. (2016). Adipose-derived regenerative cells promote tendon-bone healing in a rabbit model. Arthroscopy: the Journal of Arthroscopic and Related Surgery: Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association,32(5), 851–859. https://doi.org/10.1016/j.arthro.2015.10.012
Kuroda, K., Kabata, T., Hayashi, K., Maeda, T., Kajino, Y., Iwai, S., et al. (2015). The paracrine effect of adipose-derived stem cells inhibits osteoarthritis progression. BMC Musculoskeletal Disorders,16, 236. https://doi.org/10.1186/s12891-015-0701-4
Bourin, P., Bunnell, B. A., Casteilla, L., Dominici, M., Katz, A. J., March, K. L., et al. (2013). Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: A joint statement of the International Federation for Adipose therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy,15(6), 641–648. https://doi.org/10.1016/j.jcyt.2013.02.006
Güven, S., Karagianni, M., Schwalbe, M., Schreiner, S., Farhadi, J., Bula, S., et al. (2012). Validation of an automated procedure to isolate human adipose tissue-derived cells by using the Sepax® technology. Tissue Engineering Part C Methods,18(8), 575–582. https://doi.org/10.1089/ten.TEC.2011.0617
Laverty, S., Girard, C. A., Williams, J. M., Hunziker, E. B., & Pritzker, K. P. H. (2010). The OARSI histopathology initiative – recommendations for histological assessments of osteoarthritis in the rabbit. Osteoarthritis and Cartilage,18(Suppl 3), S53-65. https://doi.org/10.1016/j.joca.2010.05.029
Heard, B. J., Barton, K. I., Chung, M., Achari, Y., Shrive, N. G., Frank, C. B., & Hart, D. A. (2015). Single intra-articular dexamethasone injection immediately post-surgery in a rabbit model mitigates early inflammatory responses and post-traumatic osteoarthritis-like alterations. Journal of Orthopaedic Research: Official Publication of the Orthopaedic Research Society,33(12), 1826–1834. https://doi.org/10.1002/jor.22972
Crowe, A., Zheng, W., Miller, J., Pahwa, S., Alam, K., Fung, K. M., et al. (2019). Characterization of plasma membrane localization and phosphorylation status of organic anion transporting polypeptide (OATP) 1B1 c.521 T > C nonsynonymous single-nucleotide polymorphism. Pharmaceutical Research,36(7), 101. https://doi.org/10.1007/s11095-019-2634-3
Shi, S., Wang, C., Acton, A. J., Eckert, G. J., & Trippel, S. B. (2015). Role of sox9 in growth factor regulation of articular chondrocytes. Journal of Cellular Biochemistry,116(7), 1391–1400. https://doi.org/10.1002/jcb.25099
Zamani, S., Hashemibeni, B., Esfandiari, E., Kabiri, A., Rabbani, H., & Abutorabi, R. (2014). Assessment of TGF-β3 on production of aggrecan by human articular chondrocytes in pellet culture system. Advanced Biomedical Research,3, 54. https://doi.org/10.4103/2277-9175.125799
Asai, K., Nakase, J., Yoshioka, K., Yoshimizu, R., Kimura, M., & Tsuchiya, H. (2022). Adipose-derived stem cell sheets promote meniscus regeneration regardless of whether the defect involves the inner half or the whole width of the anterior half of the medial meniscus in a rabbit model. Arthroscopy,38(9), 2672–2683. https://doi.org/10.1016/j.arthro.2022.02.020
Shirai, T., Kobayashi, M., Nishitani, K., Satake, T., Kuroki, H., Nakagawa, Y., & Nakamura, T. (2011). Chondroprotective effect of alendronate in a rabbit model of osteoarthritis. Journal of Orthopaedic Research: Official Publication of the Orthopaedic Research Society,29(10), 1572–1577. https://doi.org/10.1002/jor.21394
Utomo, L., Fahy, N., Kops, N., van Tiel, S. T., Waarsing, J., Verhaar, J. A. N., et al. (2021). Macrophage phenotypes and monocyte subsets after destabilization of the medial meniscus in mice. Journal of Orthopaedic Research: Official Publication of the Orthopaedic Research Society,39(10), 2270–2280. https://doi.org/10.1002/jor.24958
O’Brien, K., Tailor, P., Leonard, C., Difrancesco, L. M., Hart, D. A., Matyas, J. R., Frank, C. B., & Krawetz, R. J. (2017). Enumeration and localization of mesenchymal progenitor cells and macrophages in synovium from normal individuals and patients with pre-osteoarthritis or clinically diagnosed osteoarthritis. International Journal of Molecular Sciences,18(4), 774. https://doi.org/10.3390/ijms18040774
Zhang, H., Cai, D., & Bai, X. (2020). Macrophages regulate the progression of osteoarthritis. Osteoarthritis and Cartilage,28(5), 555–561. https://doi.org/10.1016/j.joca.2020.01.007
Manferdini, C., Maumus, M., Gabusi, E., Piacentini, A., Filardo, G., Peyrafitte, J. A., et al. (2013). Adipose-derived mesenchymal stem cells exert antiinflammatory effects on chondrocytes and synoviocytes from osteoarthritis patients through prostaglandin E2. Arthritis and Rheumatism,65(5), 1271–1281. https://doi.org/10.1002/art.37908
Manferdini, C., Paolella, F., Gabusi, E., Gambari, L., Piacentini, A., Filardo, G., et al. (2017). Adipose stromal cells mediated switching of the pro-inflammatory profile of M1-like macrophages is facilitated by PGE2: In vitro evaluation. Osteoarthritis and Cartilage,25(7), 1161–1171. https://doi.org/10.1016/j.joca.2017.01.011
Hildner, F., Concaro, S., Peterbauer, A., Wolbank, S., Danzer, M., Lindahl, A., et al. (2009). Human adipose-derived stem cells contribute to chondrogenesis in coculture with human articular chondrocytes. Tissue Engineering Part A,15(12), 3961–3969. https://doi.org/10.1089/ten.TEA.2009.0002
Dykstra, J. A., Blue, E. D., de Assis, N., Weimer, P. L., & Kota, D. J. (2020). Human adipose-derived stromal vascular fraction: Characterization, safety and therapeutic potential in an experimental mouse model of articular injury. Journal of Stem Cells and Regenerative Medicine,16(1), 16–25. https://doi.org/10.46582/jsrm.1601004
Laidding, S. R., Josh, F., Francisca, F. M., Faruk, M., Palissei, A. S., Satria, B., et al. (2020). Combination of platelet-rich plasma and stromal vascular fraction on the level of transforming growth factor-β in rat subjects experiencing deep dermal burn injury. Annals of Medicine and Surgery,60, 737–742. https://doi.org/10.1016/j.amsu.2020.11.088
Dai, M., Sui, B., Xue, Y., Liu, X., & Sun, J. (2018). Cartilage repair in degenerative osteoarthritis mediated by squid type II collagen via immunomodulating activation of M2 macrophages, inhibiting apoptosis and hypertrophy of chondrocytes. Biomaterials,180, 91–103. https://doi.org/10.1016/j.biomaterials.2018.07.011
Fujita, M., Matsumoto, T., Hayashi, S., Hashimoto, S., Nakano, N., Maeda, T., et al. (2022). Paracrine effect of the stromal vascular fraction containing M2 macrophages on human chondrocytes through the Smad2/3 signaling pathway. Journal of Cellular Physiology,237(9), 3627–3639. https://doi.org/10.1002/jcp.30823
Jiang, D., Qi, Y., Walker, N. G., Sindrilaru, A., Hainzl, A., Wlaschek, M., MacNeil, S., & Scharffetter-Kochanek, K. (2013). The effect of adipose tissue derived MSCs delivered by a chemically defined carrier on full-thickness cutaneous wound healing. Biomaterials,34(10), 2501–2515. https://doi.org/10.1016/j.biomaterials.2012.12.014
Bora, P., & Majumdar, A. S. (2017). Adipose tissue-derived stromal vascular fraction in regenerative medicine: A brief review on biology and translation. Stem Cell Research and Therapy,8(1), 145. https://doi.org/10.1186/s13287-017-0598-y
Zhu, M., Zhou, Z., Chen, Y., Schreiber, R., Ransom, J. T., Fraser, J. K., et al. (2010). Supplementation of fat grafts with adipose-derived regenerative cells improves long-term graft retention. Annals of Plastic Surgery,64(2), 222–228. https://doi.org/10.1097/SAP.0b013e31819ae05c
Mizushima, T., Takahashi, H., Takeyama, H., Naito, A., Haraguchi, N., Uemura, M., et al. (2016). A clinical trial of autologous adipose-derived regenerative cell transplantation for a postoperative enterocutaneous fistula. Surgery Today,46(7), 835–842. https://doi.org/10.1007/s00595-015-1246-8
Krasilnikova, O. A., Baranovskii, D. S., Yakimova, A. O., Arguchinskaya, N., Kisel, A., Sosin, D., et al. (2022). Intraoperative creation of tissue-engineered grafts with minimally manipulated cells: New concept of bone tissue engineering in situ. Bioengineering,9(11), 704. https://doi.org/10.3390/bioengineering9110704
Cao, S., Zhao, Y., Hu, Y., Zou, L., & Chen, J. (2020). New perspectives: In-situ tissue engineering for bone repair scaffold. Engineering,202, 108445. https://doi.org/10.1016/j.compositesb.2020.108445
Maksimova, N. V., Michenko, A. V., Krasilnikova, O. A., Klabukov, I. D., Gadaev, I. Y., Krasheninnikov, M. E., Belkov, P. A., & Lyundup, A. V. (2022). Mesenchymal stromal cell therapy alone does not lead to complete restoration of skin parameters in diabetic foot patients within a 3-year follow-up period. BioImpacts: BI,12(1), 51–55. https://doi.org/10.34172/bi.2021.22167
Acknowledgements
We thank Ms. Minako Nagata, Ms. Maya Yasuda, and Ms. Kyoko Tanaka for their expert technical assistance. We would like to thank Editage for the English language editing.
Funding
This work was supported by JSPS KAKENHI.
Author information
Authors and Affiliations
Contributions
T. Matsumoto designed this experiment. K. Anjiki, Y. Kuroda, M. Fujita, and Y. Onoi performed all procedures of experiments. R. Kuroda supervised the project. M. Tsubosaka, Y. Takashima, M. Fujita, K. Kikuchi, K. Ikuta, S. Tachibana, Y. Suda, K. Wada, and K. Anjiki analyzed the data. K. Anjiki wrote the original manuscript. T. Kamenaga, N. Nakano, S. Hayashi, T. Matsushita, and T. Matsumoto reviewed and edited the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All procedures involving animals were approved by the Institutional Animal Care and Use committee at Kobe University and were conducted in accordance with the national guidelines on animal care (Therapeutic effects of the stromal vascular fraction and adipose-derived stem cells on osteoarthritis in an experimental rabbit model: The Ethical Committee of Kobe University; approval number: P200705; date of approval: July 13, 2020).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 142 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anjiki, K., Matsumoto, T., Kuroda, Y. et al. Heterogeneous Cells as well as Adipose-Derived Stromal Cells in Stromal Vascular Fraction Contribute to Enhance Anabolic and Inhibit Catabolic Factors in Osteoarthritis. Stem Cell Rev and Rep 19, 2407–2419 (2023). https://doi.org/10.1007/s12015-023-10589-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-023-10589-z