Abstract
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease that mainly affects the motor system. It is a very heterogeneous disorder, so far more than 40 genes have been described as responsible for ALS. The cause of motor neuron degeneration is not yet fully understood, but there is consensus in the literature that it is the result of a complex interplay of several pathogenic processes, which include alterations in nucleocytoplasmic transport, defects in transcription and splicing, altered formation and/or disassembly of stress granules and impaired proteostasis. These defects result in protein aggregation, impaired DNA repair, mitochondrial dysfunction and oxidative stress, neuroinflammation, impaired axonal transport, impaired vesicular transport, excitotoxicity, as well as impaired calcium influx. We argue here that all the above functions ultimately lead to defects in protein synthesis. Fused in Sarcoma (FUS) is one of the genes associated with ALS. It causes ALS type 6 when mutated and is found mislocalized to the cytoplasm in the motor neurons of sporadic ALS patients (without FUS mutations). In addition, FUS plays a role in all cellular functions that are impaired in degenerating motor neurons. Moreover, ALS patients with FUS mutations present the first symptoms significantly earlier than in other forms of the disease. Therefore, the aim of this review is to further discuss ALS6, detail the cellular functions of FUS, and suggest that the localization of FUS, as well as protein synthesis rates, could be hallmarks of the ALS phenotype and thus good therapeutic targets.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
ALS
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative devastating disease with currently no efficient treatment. It affects superior motor neurons from the motor cortex and inferior motor neurons from the brainstem and spinal cord. It was first discovered in 1869 by the neurologist Jean-Martin Charcot [1] but was brought to attention in 1939 when Lou Gehrig, one of the most beloved baseball players of all time, ended his career because of symptoms of the disease [2].
ALS patients can be separated into two categories depending on the etiology of the disease: sporadic (SALS) or familial (FALS). 90% of the cases fall into the SALS group, where the cause or causes of the disease are unknown. The remaining 10%, in which more than one family member may be affected by the disease, have been linked to hereditary mutations. Familial cases of ALS are mostly inherited in a dominant pattern and are numbered according to the gene which is found mutated in each patient and currently, mutations in more than 40 genes such as superoxide dismutase 1 (SOD1) in ALS1, Vesicle-associated membrane protein (VAPB) in ALS8, TAR DNA binding protein 43 (TARDBP) in ALS10, and fused in sarcoma (FUS) in ALS6 have been identified in familial forms of ALS [3].
The estimated worldwide mortality is about 30,000 patients a year [4]but the incidence rate varies across continents. It is estimated to be 2–3 per 100,000 individuals in Europe and 0.7–0.8 per 100,000 individuals in Asia [5]. The mean age of onset of ALS is 65, but younger patients may be affected [6], and is usually fatal within 2–5 years [7] after disease onset.
ALS symptoms occur due to the degeneration of the motor neurons (MNs). The usual clinical presentation in ALS patients involves the motor symptoms such as muscle twitching, cramping, stiffness, and weakness. Overall, the patient’s muscles become weaker as the disease progresses and muscle tissue atrophies. However, non-motor signs can be associated as well (as cognitive dysfunction, frontotemporal dementia, extrapyramidal features, among others). Therefore, ALS is currently widely considered as a multisystem degeneration [3].
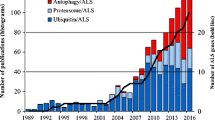
The causes of motor neuron degeneration are not completely understood, but it is agreed across literature that is a consequence of a complex interplay between multiple pathogenic processes. Amongst these processes, there are some features considered as ALS hallmarks (Fig. 1). They include alterations in nucleocytoplasmic transport, defects in transcription and splicing, altered stress granule (SG) formation and/or disassembly, impaired proteostasis that results in aggregating proteins, impaired DNA repair, mitochondrial dysfunction and oxidative stress, oligodendrocyte degeneration, neuroinflammation, defective axonal transport, defective vesicular transport, excitotoxicity, and disturbed calcium influx [8].The result is a multifactorial disorder caused by a combination of multiple genes effects as well as by interactions between genes activity and the environment.
One key feature found in 90% of ALS cases is ubiquitinated protein inclusions, in which TAR DNA-binding protein 43 (TDP-43) is a major constituent [9]. TDP-43, besides being intrinsically predisposed to aggregation, is also normally involved in mRNA processing. In this way, ALS-linked mutations intensify aggregates formation and increase their toxicity, which emphasizes the relation between disease onset and severity and cell proteostasis defects.
Due to its heterogeneity in diverse aspects, such as causative mutations, age at onset, progression rate and local of first symptoms initiation, researchers have been failing to find new therapeutic approaches.
In 2009, the first mutations in the FUS gene, also known as translocated in liposarcoma (TLS), an RNA-processing protein, were identified in ALS families, which was classified as ALS type six (ALS6). FUS mutations have also been described in sporadic cases linked to chromosome 16q12. [10,11,12].
Importantly, ALS patients harboring FUS mutations present the first symptoms significantly earlier than in other forms of the disease. Indeed, more than 60% of FUS mutant patients present the first signs of disease before 45 years of age. Moreover, many ALS6 juvenile cases have been described with disease onset in the early twenties [13, 14].
FUS is also found mislocalized on MNs cytoplasm from SALS patients. Moreover, FUS is associated to all cellular functions found to be disturbed in the degenerating MNs. Therefore, the main objective of this review is to further discuss ALS6, detail FUS cellular functions, and suggest that FUS localization, as well as protein synthesis rates, might be hallmarks of the ALS phenotype and hence, potentially good therapy targets.
ALS 6
The clinical features of ALS6 are alike the classical ALS phenotype. Symptoms include progressive muscular atrophy, dysphagia, dysarthria, ultimately leading to respiratory failure. The neuropathological characteristics of these patients are upper and lower motor neurons degeneration, neuronal degeneration on the anterior horn of the spinal cord, mild pyramidal neuronal loss, dystrophic neurites, astrogliosis, and microglial activation. They generally present TDP43-negative and FUS-positive cytoplasmic inclusions in the motor neurons [9].
FUS was first identified in malignant human myxoid liposarcoma (a form of malignant tumor affecting adipose tissue), as a fused protein with CHOP (C/EBP homologous protein) a dominant transcription inhibitor. It was only in 2009 that the first cases of ALS with FUS mutations were described [12].
Mutations in the FUS gene are responsible for both familial (4% of the cases) and sporadic forms of ALS (1% of the cases) [15]. To date, more than 50 different mutations within the FUS gene were described to cause ALS. Most familial ALS mutations are found in the FUS C-terminal nuclear localization sequence (NLS), causing the mislocalization of the normally nuclear protein to the cytoplasm. Consequently, this leads to the accumulation of cytoplasmic protein inclusions [16]. This suggests that either loss of FUS function in the nucleus or gain of toxic function in the cytoplasm are the disease-causing mechanisms [17], although both mechanisms are most likely acting together. However, to enhance our comprehension on the pathobiology underlying FUS mutations in ALS patients, understanding the role of wild-type (wt) FUS is crucial.
FUS Protein
FUS is a 526 amino acid RNA binding protein (RBP) of the FET family that contains several functional domains including: Gln-Gly-Ser-Tyr-rich (or prion-like) domain; Gly-rich domain; Arg-Gly-Gly-rich domain; RNA recognition motif; zinc finger domain and a C-terminal nuclear localization signal (NLS) [18].
Under physiological conditions, FUS is mostly localized in the nucleus in neurons and is exclusively nuclear in glia[19]. Yet, FUS can be transported between the nucleus and cytoplasm [20].
The exact function of FUS under normal physiological conditions is unclear. Some established roles include transcriptional control [21], RNA processing through splicing regulation of pre-mRNAs [22], and DNA repair [23], thus defining FUS as a pleiotropic protein. Concerning FUS structure, the N-terminus is most likely involved in transcriptional activation and C-terminus in protein and RNA binding.
There is evidence that FUS might have distinct roles during different stages throughout development. It was previously observed that FUS is ubiquitously expressed postnatally in mice and rats, but its expression decreases on most tissues by adult age, except in neuronal tissues [14]. This suggests a role for FUS that is linked to neurodevelopment and neuronal homeostasis and highlights possible mechanisms of action of mutant FUS in ALS pathogenesis.
However, FUS was described as a ubiquitous expressed protein and an endogenous nuclear expression of FUS in adult myoblasts and myotubes was previously reported [24]. Furthermore, the expression of mutant FUS only in muscle cells was sufficient to exert degenerative effects in motor neurons [25]. It has also been reported that expression of mutant FUS exclusively in astrocytes is sufficient to induce death of spinal motor neurons [26]. Further work is needed to better understand FUS functions in other types of cells and how they contribute to the motor neuron death and disease phenotype. However, most importantly, these results highlight a non-cell-autonomous mechanism that seems to be of relevance for the progression of ALS pathology.
In addition to FUS function in multiple cells, numerous studies report the role of FUS on diverse cellular processes, as summarized below.
FUS Models
There are many available models to study FUS functions, which are reviewed in greater detail elsewhere [27]. Here we detail each model system used and try to give emphasis on results using patient derived cells, as Induced Pluripotent Stem Cells-derived motor neurons. However, independently of the model itself, being drosophila, yeast, mice, or human cells, there is a particularly conserved characteristic of most FUS models that needs to be highlighted.
When overexpressed, wild-type human FUS induces cytoplasmic inclusions formation. The latter being a hallmark of ALS6 patients and, therefore, one of the putative causes of neuronal degeneration. Indeed, ALS phenotypes were recapitulated in a transgenic mouse model generated by using the pronuclear injection of wild type human FUS cloned into a modified mouse prion gene. The mice ended up overexpressing ubiquitously and constitutively wild type human FUS. These animals developed an aggressive ALS phenotype with early tremor outbreak followed by progressive posterior members paralysis and death after 12 weeks [28]. The presence of neurological symptoms in a ubiquitously expressed system suggests that FUS plays an essential role in neural compartment ontogenesis which deserves further attention.
Cellular Functions
FUS Functions During Embryonal Development
When FUS is knocked down from frog embryos they fail to gastrulate and show mesodermal differentiation defects. In these embryos, it was demonstrated that intron retention in pre-mRNA occurs in 3–5% of all transcripts when FUS levels are decreased [29]. Beyond that, it was shown that the C-terminal domain of FUS is not required for correct splicing, since embryos in which the FUS C-terminal part was missing developed normally and do not show miss splicing [29].
The consequences of disrupting Fus were also investigated in mice. Mice that are heterozygous for Fus mutation are indistinguishable from wild-type mice. On the other hand, homozygous Fus mutant mice fail to suckle and die within 16 h of birth. Despite these Fus–/– mice develop normally (what the authors confirm with histology examination of major organs and tissues), Fus mutant mice do display genomic instability in their lymphocytes [30].
Furthermore, Fus expression was previously analyzed in a longitudinal study in C57BL6 mice and Sprague-Dawley rats. High and ubiquitous levels of Fus mRNA were detected in neonate mice and rats but were significantly lower in most tissues in the adult rodents. Meanwhile, in adult individuals, FUS protein was undetectable in some peripheral organs such as skeletal muscles, liver, and kidney, but was constantly highly expressed in the central nervous system [14].
In summary, the studies discussed above suggest that during embryogenesis and in newborn developing tissues, FUS has an important role in mesoderm development due to its function in splicing. Of note, one copy of wild-type Fus is enough to sustain normal cellular functions during development as the heterozygotes show a wild type-like phenotype in neonatal rodents. However, homozygous mutations of Fus are lethal in mice.
Finally, Fus expression is maintained in the adult nervous tissue, and its functions are linked to neuronal homeostasis. FUS roles in adult cells are summarized below.
Genome Maintenance
One of the reported roles for FUS is in the maintenance of genome integrity by having a role in DNA damage repair (DDR).
Previous reports provided evidence that FUS is recruited to sites of laser-induced DNA double-strand breaks (DSBs). This recruitment needs poly ADP-ribose polymerase (PARP) activity. The arginine/glycine-rich domains of FUS are responsible for the protein redistribution to the sites of DNA damage once these domains directly interact with PARP. In addition, depletion of FUS diminished DSB repair, decreasing both homologous recombination (HR) and non-homologous end-joining (NHEJ), implicating FUS as an upstream effector in both pathways [23].
Furthermore, FUS localization after laser-induced DNA damage showed that recruitment of FUS to the damaged sites occurs earlier than for proteins with well-known roles in the DNA-repair process, including NBS1 (Nijmegen breakage syndrome-1), p-ATM (phosphorylated-ataxia telangiectasia mutated), γH2AX (phosphorylated histone 2 A.X), and Ku70 [31].
Specifically, in neurons, wildtype FUS facilitates recruitment of XRCC1/DNA Ligase IIIα (LigIII) complex to oxidized genome sites and allow for base excision repair (BER). Consequently, insufficient nucleic FUS causes DNA nick ligation defects, which are toxic to MNs [32].
Many reports linked DNA repair defects to neurodegenerative diseases [33,34,35]. ALS patients display increased levels of the DNA damage marker γH2AX in cortical MNs [36]. Similarly, MNs derived from induced pluripotent stem cells (IPSCs) with endogenous FUS mutations showed signs of DNA damage [37].
When NHEJ and HR-mediated DNA repair capacity was measured in U2OS cells bearing different ALS-linked mutations, all the FUS mutants tested (R244C, R514S, H517Q, and R521C) had impaired HR-mediated DNA repair compared to wild- type FUS. However, localization of FUS variants either in the nucleus or in the cytoplasm did not correlate with HR activity. For example, the mutant FUS R244C was mostly identified in the nucleus, but exhibited a considerable decrease in HR, indicating that the loss of function of mutant FUS that caused defective HR is not simply a consequence of its absence from the nucleus. Overall, FUS mutants affected the HR DNA repair pathway more pronouncedly than NHEJ [36].
Familial cases of ALS that present mutations in the FUS gene show a reduced interaction within mutant FUS and HDAC1, causing defects in DNA repair [36].Indeed, in a transgenic mouse model expressing a frequent familial ALS-associated FUS mutation (FUS-R521C), mutant FUS proteins stably interact with wild type FUS, competing with HDAC1 and inhibiting HDAC1-FUS interactions. Consequently, FUS-R521C mice displayed increased DNA damage and a substantial decrease in dendritic growth and synaptic functions in the brain and spinal cord[38].
FUS also participates in the cellular response to topoisomerase I (TOP1)-induced DNA breakage. When RNA polymerase II (Pol II) stops at sites of TOP1-induced DNA breaks, FUS relocalizes to the nucleolus. In this setting, FUS-mutant patient fibroblasts are more sensitive to TOP1-induced DNA breakage than wild type-FUS control fibroblasts [39].
Overall, there is consistent evidence that FUS plays an important upstream role in the cellular response to diverse types of DNA damage induction (being TOP1, laser, or oxidative stress) and that it can recruit many DNA repair proteins. However, there is no consensus of whether FUS is more significant to the HR or NHEJ dependent DNA damage repair, but it seems to be enrolled in both pathways.
Regulation of Gene Expression
FUS and Post Translation Modifications on Histone Residues
Availability of DNA- therefore packing of nucleosomes- is expected to be important to transcription initiation. Post-translation modifications (PTMs) on histone residues can modulate nucleosome stability and dynamics and is one of the major mechanisms of gene expression control. Histone acetylation, methylation, and phosphorylation act in concert to modulate chromatin accessibility and FUS has been associated with deposition of all the mentioned modifications[40].Recent evidence shows that alteration of the epigenetic landscape is one of the features that result in ALS pathology [40,41,42].
Histone acetyl transferases (HATs) and histone deacetylases (HDACs) control histone acetylation in an antagonistic fashion. In a FUS overexpression model using HeLa cells, FUS was found binding to CBP/p300- a major HAT - and inhibiting its histone acetylation activity. This results in hypoacetylation of a region in proximity to the CCND1 gene with reduction of cyclin D1expression, impairing progression through the cell cycle [43].
In a yeast model overexpressing human FUS, significantly reduced histone H3 lysine 14 and 56 (H3K14 and H3K56) acetylation levels were observed. These modifications are preserved in humans and acetylation of H3K14 is specifically found at actively transcribed genes promoters [41]. Accordingly, FUS overexpression in this model presented reduced global RNA levels, another indication that histone hypoacetylation may reduce transcription [44].
Interestingly, HDAC inhibitors are arising as promising therapeutic strategies for ALS patients. Drugs inhibiting HDAC activity are used in the clinic as anticancer agents, showing that its administration is safe as a treatment for human diseases [45]. Specifically for ALS, research is still ongoing, and several steps are needed before clinical trials, but pre-clinical studies observed that treatment with different HDAC inhibitors decreased motor neuron degeneration in a SOD1 mouse model [46, 47].
Regarding ALS6, an in-vitro model using IPSC-derived MNs demonstrates that the genetic silencing and pharmacological inhibition of HDAC6 were able to recover axonal transport problems caused by mutant FUS [48]. Accordingly, transgenic mice overexpressing wild-type FUS (“TgFUS+/+”) had reduced histone acetylation. Continuous ACY-738 treatment (an HDAC inhibitor able to surpass the blood-brain barrier) in these mice reestablished global histone acetylation, ameliorated the motor degeneration, and significantly extended transgenic mice life span [49].
FUS overexpression also caused asymmetric dimethylation on arginine 3 ofhistone 4, which is known to promote histone acetylation and gene transcription [50]. This feature is possibly related to the Protein arginine N-methyltransferase 1 (PRMT1), which is responsible for H4R3me2asym [51]. In a mouse model of ALS with FUS-R521C mutation, the interaction of mutant FUS with PRMT1 was responsible for PRMT1 activity inhibition. It was observed a reduction of H4R3me2asym in this model, ultimately leading to transcriptional silencing. When PRMT1 was overexpressed, the phenotype caused by the mutation was decreased [52].
FUS is also capable of modulating phosphorylation on histone residues. In NSC-34 and HEK-293T cells, FUS knockdown (KD) through RNA interference induced H3 phosphorylation. FUS-KD decreased cell proliferation and modulated expression levels of genes involved in cell cycle regulation, cytoskeletal organization, and oxidative stress [53].
Results relating FUS to the regulation of PTMs on histone residues seem to agree with the literature. Overall, mutations result in changes in patterns of PTMs and the downregulation in global gene transcription compared to controls.
FUS and miRNA Regulation
Another mechanism by which FUS influences gene expression is through micro-RNA regulation. Micro RNAs (miRNAs) are small non-coding RNAs that can change the expression of many different mRNAs with high specificity [54]. The miRNA base pairing to mRNA untranslated region (UTR) sequences is responsible for target specificity. This binding results in mRNA destabilization or translation inhibition [55].
One of the first pieces of evidence that FUS is capable of regulating miRNAs was demonstrated when FUS was identified as a protein that contributes to the biogenesis of a subset of miRNAs, including miRNAs with neuronal functions, differentiation, and synaptogenesis. FUS is recruited to the chromatin at miRNA transcription sites and binds their pre-miRNAs. Moreover, depletion of FUS leads to a decrease in Drosha (the main nuclease responsible for miRNA processing initiation step in the nucleus) levels at chromatin loci [56].
ALS mutations were also recognized as responsible for general miRNA deregulation [57, 58]. Analysis of the whole transcriptome of isogenic IPSC-derived human motor neurons expressing either FUS wild-type or mutant identified several miRNAs deregulated on the mutant MNs, including miR-375, previously related to motor neuron survival [57]. Another ALS-related FUS mutation, FUS- R495X, also impairs miRNA-mediated gene silencing [58]. One mechanism by which FUS interferes with miRNA gene expression regulation is by directly binding the core miRNA-induced silencing complex (miRISC) component AGO2 and by directly interacting with miRNA and mRNA targets [58].
Collectively, literature results strongly suggest a role of FUS in regulating the activity of miRNA-mediated gene silencing by directly binding miRISC components and consequently playing an important part in neuronal differentiation and maintenance in ALS patients.
FUS and Splicing
Finally, one important feature of FUS regarding the regulation of gene expression is its role in splicing. FUS binds to several transcripts within the brain [59]. The exact mechanism by which it regulates splicing is unknown, although crosslinking and immunoprecipitation (iCLIP) in mouse brains showed that FUS binds along the full length of emerging RNAs and persist bound to the pre-mRNAs until splicing termination [60].
FUS also binds important spliceosome components. U1 snRNP is one of the most abundant FUS interactors. Components of U1 snRNP core particle (as Sm proteins and U1 snRNA) mislocalize with FUS to the cytoplasm in fibroblast of ALS6 patients with FUS NLS mutations. The mislocalization of snRNP core proteins seems to be dependent on the RRM domain of FUS. Moreover, FUS and U1 snRNP proteins KD caused motor axon truncations in zebrafish [61]. FUS binding to U11 snRNP regulates the removal mainly of minor introns. In neuroblastoma cells, a FUS knockout (KO) disturbed the splicing of minor intron-containing mRNAs. Moreover, cytoplasmic aggregates formed by an ALS-associated FUS mutant traps U11 and U12 snRNAs in these aggregates, inhibiting the splicing of minor introns [17]. Additionally, association of FUS to RNA polymerase II (RNAP II) is indispensable to U1 snRNP and RNAP II interaction: It was shown that proper splicing requires FUS presence during RNAP II transcription reaction, thus, coupling transcription to splicing [62].
Regarding alternative splicing, FUS-binding sites are present around the alternatively spliced exons and tend to form stable secondary structures. Moreover, FUS is commonly present in the antisense RNA strand at the promoter regions, which downregulates transcription of the coding strand [63].
It is not clear whether mutations in the FUS gene causes gain or loss of functions on the FUS protein. To compare the mutation-induced changes to actual loss of function consequences (represented by the knockouts or knockdowns previously reported), knock-in models were created and high depth RNA-sequencing data on FUS mutants was performed in parallel to FUS KO. Still, a widespread loss of function on gene expression and splicing was caused by FUS ALS mutations, being RNA binding proteins preferential targets of this effect. Similarly, mutant FUS induces intron retention through RNA binding, even in FUS itself [64].
The brain proteomic diversity is a major consequence of alternative splicing spatial and temporal control [65], therefore highlighting the relevance of this mechanism to this specific tissue correct function. FUS is required for splicing events to occur but can also inhibit splicing and alternative splicing. Thus, it indicates that FUS might regulate splicing events and transcription in a position and interactor-dependent manner, which is of extreme importance for proper neuronal tissue homeostasis.
FUS and SG
ALS is considered to have multifactorial pathogenic mechanisms and SGs are one of the most well-studied hallmarks that can be influenced by epigenetic factors. Therefore, many modifiers of SG assembly are under research.
FUS is found within SGs and aggregation of FUS protein is believed to have a fundamental role in ALS pathogenesis, since FUS aggregates are found in the cytoplasm of motor neurons in postmortem sections of sporadic ALS patients [66].
The role of FUS in SGs was intensely studied and reviewed [18, 67,68,69]. The main conclusions to these analyses are mentioned below.
FUS is a member of ribonucleoprotein particles (RNPs), which are RNA and RNA-binding proteins (RBPs) complexes and can have different roles [70]. RBPs can form cytoplasmic granules, that are membraneless organelles and include different kinds of granules. Amongst them are processing bodies (p-bodies), transport and stress granules, (SGs), with the latter being RNA-containing cytoplasmic foci generated once the cell is exposed to stress. The SGs are assembled to allow the cell to handle cellular stresses by delaying mRNA translation and directing synthesis towards cytoprotective proteins. After the stress is relieved, these structures are disassembled [71]. Most of the proteins that have been described in these structures are RNA binding proteins (RBPs) or are proteins involved in RNA metabolism and translation[72].
FUS is one of these RBPs identified within both SGs and P-bodies and there is a consensus that the amount of FUS in granules depends on how much of the protein is mislocalized to the cytoplasm [73]. Both wild type and mutated forms of FUS are found in SGs [74]. However, FUS mutants are more present in these structures when compared to wild type [73, 75]. It is worth pointing out that FUS is not required for the SG assembly once it is not impaired by endogenous wild-type FUS knockdown [76]. However, many results indicate that mutations in FUS make the protein become aggregation prone and alter many aspects of SGs, including granule size [77], abundance, assembly and disassembly speed [68], and biophysical properties, such as viscosity and stiffness [68, 77]. Although it is not a consensus whether mutations on FUS make SG more or less dynamic.
Most studies use oxidative stress to induce SG assembly and compare wild-type to mutated FUS functions. Regarding FUSwt function in different cellular stress responses, FUS exhibits a vigorous response to hyperosmolar stress. Hyperosmolar stress causes an immediate nuclear FUS redistribution to the cytoplasm, with transient nuclear clearance and loss of function. When in the cytoplasm, it integrates into stress granules. But this redistribution is independent of SG formation, once FUS does not seem to migrate to the cytoplasm as a response to others stress granule assembly inducers, such as sodium arsenite, hydrogen peroxide, thapsigargin, or heat shock [78].
FUS translocation is also modulated by methyltransferase activity, Transportin 1, and is potentiated by transcriptional inhibition [79]. Interestingly, reduced FUS expression causes cell viability loss in response to hyperosmolar stress, indicating a protective role for FUS in this context [78].
The role of SG within the cells and how it can impact disease progression is not completely understood. How could a pro-survival trait maybe increase toxic protein aggregation? One accepted model is that SGs may aid the formation of cytoplasmic aggregates in ALS, while excessive SG assembly or defective SG clearance induced by mutations or cellular conditions increase SG persistence, consequently generating toxic aggregates [80]. It was previously shown that repetitive assembly of SGs is toxic to motor neurons and is succeeded by SGs alteration into cytoplasmic inclusions similar to those found on the ALS pathology [81]. On the other hand, there is the possibility that SGs do not play a role in the formation of persistent aggregates or even that SGs present a protective effect.
Pointing towards the latter hypothesis, when FUS domains responsible for RNA recognition and binding are disrupted, consequently decreasing SG assembly, it highly increases the formation of structures comparable to aggresomes [82]. Also, Protein ubiquilin 2 (UBQLN2) was shown to maintain the solubility of FUS in response to stress, increasing FUS–RNA complex formation and, therefore, acting as a negative regulator of SG formation [83]. FUS-mediated neurodegeneration is also modified by muscleblind (MBL) in an ALS6 drosophila model: MBL overexpression was able to decrease cytoplasmic mislocalization of mutant FUS and accumulation in stress granules [84]. This evidence leads us to believe that the stress granules act as a protective feature when cells are stressed by aggregating FUS because when FUS is soluble in the cytoplasm it is toxic for cells. However, when SGs become permanent aggregates, they become toxic for cells.
Besides these specific proteins that can modulate mutated FUS localization and solubility, studies report that enhancing autophagy reduces cytoplasmic FUS, decreases the number of stress granules, and rescues motor function [85].
Lastly, multiple viruses can induce SG assembly [86]. Several studies have reported epidemiological and clinical evidence connecting viral infection and ALS [87,88,89]. For example, it is known that individuals infected with HIV or human T cell leukemia virus 1 develop neurological disorders with clinical features of ALS [90]. Accordingly, synthetic dsRNA poly (I:C) (a viral mimic) or an SG-inducing virus causes the persistent presence of mutant FUS granules. These inclusions sequester the autophagy receptor optineurin and nucleocytoplasmic transport factors. Moreover, mutant FUS-expressing cells are more susceptible to dsRNA toxicity, suggesting that the antiviral immune response is likely a second hit for FUS pathological phenotype [91].
PTMs on FUS protein itself can also influence ALS pathology. Post-translational modifications of FUS can occur at different positions, affecting its localization and aggregation propensity. Although the roles of PTMs in FUS aggregation pathology remain unresolved and depends on the type of PTM and interactors, several putative PTM share overlapping sites with disease-associated mutations, which could indicate their relevance to the development of ALS phenotype [92].
In summary, wild-type FUS seems to have protective effects when cells suffer from stress exposure. While mutant-FUS seems to have a gain-of-toxic mechanism, modifying the dynamic properties of stress granules (Fig. 2) [77]. Overall, disease pathogenesis could be a result of the presence of FUS in the cytoplasm and the assembly of FUS protein into stress granules, acting as an interface between genetic susceptibility and environmental factors [93].
Protein Synthesis
Subcellular localization of proteins is essential to the establishment of the body axis, cell migration, synaptic plasticity, and other biological processes in neurons, the first affected cells in ALS. Three processes control protein localization: transport, localization of mRNAs, and local translation. A comparison between isolated cell bodies and neurites of neurons differentiated from mouse embryonic stem cells, identified with a global analysis of protein presence, RNA expression, and translation rates that mRNA position is the primary mechanism defining protein localization in neurites. [94].
Localization of mRNAs is highly conserved in eukaryotes [95] and mechanisms of axonal mRNA translation might be the link to axon guidance, survival, regeneration, and neurological disorders [96].
Protein synthesis, proteasome, or autophagy activation are energetically expensive processes and ribosome quality control can prevent unnecessary translation. Another way of avoiding this energetic waste is by nonsense-mediated decay (NMD), which distinguishes and erases mRNAs with premature termination codons (PTCs) [97]. In this way, the NMD pathway regulates protein translation. It was found that in N2a cells expressing mutant FUS, NMD was altered, meaning that NMD-promoting factors UPF1 and UPF3b were increased, while a negative NMD regulator, UPF3a, was decreased, resulting in hyperactivation of NMD [98], consequently decreasing protein synthesis due to lack of mRNA.
In mice, either expressing both mouse and human FUS or only full-length human FUS, ALS- related mutant FUS and not wild type accumulated in the axons in hippocampal neurons and sciatic nerves and caused decreased intra-axonal protein synthesis. Unlike in other models, this specific study showed that mutations did not cause FUS cytoplasmic aggregation, as well as did not alter FUS-bound pre-mRNAs splicing, but rather, induced a gain of toxic function that resulted in suppression of intra-axonal translation, synaptic dysfunction, and progressive motor degeneration [99].
In cultured neurons differentiated from mouse embryonic stem cells expressing human R495X FUS, analysis by CLIP-Seq and Ribo-seq showed that wildtype FUS binds on precursor mRNAs (pre-mRNAs), while mutated FUS binds mature mRNAs. Surprisingly, this binding did not change the translation levels of the attached mRNAs. However, it was found that R495X decreases mitochondria function-associated genes translation, resulting in an important decrease in mitochondrial size [100].
Beyond that, translation inhibition in both mouse and human MNs could be achieved by mutant FUS expression at physiological levels. Mutant FUS did not act directly on the translation machinery but was found to form cytoplasmic inclusions containing FMRP (a neurodegeneration-associated RBP involved in translation regulation). This causes the repression of translation in vitro and in vivo [101].
The role of wild-type FUS in protein synthesis is yet to be completely understood and it may be an exclusive function of the mutant forms due to their mislocalization in the cytoplasm. Nonetheless, protein synthesis suppression seems to be a common consequence of FUS mutations.
It is not clear whether the decreased translation is protective or harmful in the neurodegeneration context. However, the phosphorylation of eukaryotic initiation factor 2α (eIF2α) is one of the most consistent observations related to neurodegenerative diseases. eIF2α is a translation initiation factor, involved in cap-dependent protein translation and its phosphorylated form causes global translation suppression [102].
In summary, there is accumulating evidence about the importance of protein synthesis to the ALS disease onset and progression. Therefore, further investigation on the role of translation rates on ALS phenotypes can help increase understanding of the disease pathways and the development of further and more efficient therapeutics.
Discussion and Conclusion
There is a variety of molecular mechanisms underlying neurodegenerative pathogenesis, hampering the development of effective therapies for these disorders. This heterogeneity has been a challenge to enhance our understanding on the cellular phenotypes that might be happening to protect the motor neurons from insults or that are the direct causes that lead to motor neuron death. Hopefully, new technologies might help understand these differences. The single-cell transcriptomic resolution, for example, enables unraveling cell-specific disease states [103], and since ALS is a late-onset disease, it might point us to transcriptional patterns that keep cells functioning despite the initial stresses caused by the mutations [104]. Moreover, spatial transcriptomics permits finding the gene expression of resistant neurons in their microenvironment and with their interconnecting cells [105]. Recently, spatiotemporal transcriptomic atlas has been generated with ALS postmortem spinal cords and with mouse models [106, 107]. These techniques might help answer questions regarding the causes and consequences of neurodegeneration and each cellular phenotype leading to motor neuron death.
We argue that protein synthesis is a major process that controls cell behavior since proteins are the functional molecules that determine cell types and functions [108]. Accordingly, understanding and targeting protein synthesis defects might help stop disease progression.
All processes in which mutant FUS leads to aberrations ultimately change protein translation rates (Fig. 3):
-
Wild type FUS is relevant for the DNA damage repair mechanism and ALS patients have higher amount of damage in the DNA, as previously discussed. It is known that DNA damage inhibits protein translation. For example, damage in the DNA caused by UVB inhibits overall protein synthesis, and causes translational reprogramming, allowing the selective synthesis of DDR proteins, such as ERCC1, ERCC5, DDB1, XPA, XPD, and OGG1 mRNAs [109]. Also, ionizing radiation (IR) that causes DNA double-strand breaks (DSBs), results in changes in levels of proteins involved in autophagy, proteasome degradation, mitochondrial proteins, and a striking downregulation of ribosomal and translation factors that rapidly changes the translation pattern after IR [110].
-
FUS roles in transcription involving PTMs on histones decrease global RNA levels, which could also result in the decrease of global translation because of the lack of mRNA availability.
-
Disturbing splicing events can affect mRNA availability and localization, and rates of protein translation, consequently. It was previously shown that in mammalian cells, spliced mRNAs generate greater protein amounts per mRNA molecule than identical mRNAs not made by splicing. This correlates with augmented polysome association with spliced mRNAs, possibly due to exon junction complexes (EJCs) deposition [111].
-
Stress granules’ central role is changing synthesis towards cytoprotective proteins by delaying mRNA translation. Their permanent presence and translation suppression might be the trigger to cytotoxicity in a late-onset disease like ALS.
Many efforts were made to understand the main and common processes underlying the pathobiology of all ALS types. Synaptic loss is a crucial event in neurodegenerative disorders and should be considered as one of these overlapping processes. One of the several mechanisms involved in sustaining synapses integrity is local protein translation, as it can directly affect the synaptic formation, communication, and maintenance. Local protein synthesis is regulated by RNA-binding proteins and their association with RNA granules. Consequently, the loss of synapses in neurodegenerative diseases could be a result of RNA metabolism malfunction and further investigation into RBPs like FUS could lead to important insights into how their disruption can cause disease onset [112].
In conclusion, FUS is a protein related to many cellular processes, and there is growing evidence that its dysfunction might be involved in the mechanism of the pathogenesis of not only ALS6 but other types of familial and sporadic ALS [66]. Here we argue that the mechanisms disrupted by FUS mutations ultimately result in the decrease of protein synthesis. Further studies should focus on translational rates to better understand if they are a cause or a consequence of the ALS phenotype and propose alternative therapies aiming to delay the disease onset and increase patients’ survival.
Data Availability
Data analysed during this study are included and refered in this published article.
References
Charcot, J. M. (1869). Deux cas d’atrophie musculaire progressive: avec leÌ sions de la substance grise et des faisceaux anteÌ rolateÌ raux de la moelle eÌ pinieÌ€re. Paris: Masson.
Cook, C., & Petrucelli, L. (2019). Genetic convergence brings clarity to the enigmatic Red line in ALS. Neuron, 101, 1057–1069.
Mathis, S., Goizet, C., Soulages, A., Vallat, J. M., & Masson, G. (2019). le. Genetics of amyotrophic lateral sclerosis: A review. J Neurol Sci [Internet]. Elsevier; [cited 2019 Apr 10];399:217–26. Available from: https://www.sciencedirect.com/science/article/pii/S0022510X19301017?via%3Dihub#bb0025
Petrov, D., Mansfield, C., Moussy, A., & Hermine, O. (2017). ALS clinical trials review: 20 years of failure. Are we any closer to registering a new treatment? Front Aging Neurosci (p. 68). Frontiers Research Foundation.
Hardiman, O., Al-Chalabi, A., Chio, A., Corr, E. M., Logroscino, G., Robberecht, W., et al. (2017). Amyotrophic lateral sclerosis. Nat Rev Dis Primers. Nature Publishing Group.
van Es, M. A., Hardiman, O., Chio, A., Al-Chalabi, A., Pasterkamp, R. J., Veldink, J. H., et al. (2017). Amyotrophic lateral sclerosis. The Lancet (pp. 2084–2098). Lancet Publishing Group.
van den Berg, L. H. (2014). Therapy of amyotrophic lateral sclerosis remains a challenge. Lancet Neurol (pp. 1062–1063). Lancet Publishing Group.
Van Damme, P., Robberecht, W., & Van Den Bosch, L. (2017). Modelling amyotrophic lateral sclerosis: Progress and possibilities. DMM Disease Models and Mechanisms (pp. 537–549). Company of Biologists Ltd.
Blair, I. P., Williams, K. L., Warraich, S. T., Durnall, J. C., Thoeng, A. D., Manavis, J., et al. (2010). FUS mutations in amyotrophic lateral sclerosis: clinical, pathological, neurophysiological and genetic analysis. J Neurol Neurosurg Psychiatry BMJ Publishing Group Ltd, 81, 639–645.
Kwiatkowski, T. J., Bosco, D. A., LeClerc, A. L., Tamrazian, E., Vanderburg, C. R., Russ, C., et al. (1979). Mutations in the FUS/TLS Gene on Chromosome 16 Cause Familial Amyotrophic Lateral Sclerosis. Science 2009;323:1205–8.
Vance, C., Rogelj, B., Hortobágyi, T., de Vos, K. J., Nishimura, A. L., Sreedharan, J., et al. (1979). Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science 2009;323:1208–11.
Belzil, V. V., Valdmanis, P. N., Dion, P. A., Daoud, H., Kabashi, E., Noreau, A., et al. (2009). Mutations in FUS cause FALS and SALS in French and French Canadian populations. Neurology Lippincott Williams and Wilkins, 73, 1176–1179.
Bäumer, D., Hilton, D., Paine, S. M. L., Turner, M. R., Lowe, J., Talbot, K., et al. (2010). Juvenile ALS with basophilic inclusions is a FUS proteinopathy with FUS mutations. Neurology Lippincott Williams and Wilkins, 75, 611–618.
Huang, C., Zhou, H., Tong, J., Chen, H., Liu, Y. J., Wang, D., et al. (2011). FUS Transgenic Rats Develop the Phenotypes of Amyotrophic Lateral Sclerosis and Frontotemporal Lobar Degeneration. Cox GA, editor. PLoS Genet. Public Library of Science; ;7:e1002011.
Kiernan, M. C., Vucic, S., Cheah, B. C., Turner, M. R., Eisen, A., Hardiman, O., et al. (2011). Amyotrophic lateral sclerosis.The Lancet. p.942–55.
Gal, J., Zhang, J., Kwinter, D. M., Zhai, J., Jia, H., Jia, J., et al. (2011). Nuclear localization sequence of FUS and induction of stress granules by ALS mutants. Neurobiol Aging. ;32:2323.e27-2323.e40.
Reber, S., Stettler, J., Filosa, G., Colombo, M., Jutzi, D., Lenzken, S. C., et al. (2016). Minor intron splicing is regulated by FUS and affected by ALS-associated FUS mutants (35 vol., pp. 1504–1521). EMBO J. John Wiley & Sons, Ltd.
Sama, R. R., Ward, K., & Bosco, C. L. (2014). DA. Functions of FUS/TLS from DNA repair to stress response: implications for ALS. ASN Neuro: SAGE Publications.
Andersson, M. K., Ståhlberg, A., Arvidsson, Y., Olofsson, A., Semb, H., Stenman, G., et al. (2008). The multifunctional FUS, EWS and TAF15 proto-oncoproteins show cell type-specific expression patterns and involvement in cell spreading and stress response. Bmc Cell Biology, 9, 37.
Brelstaff, J., Lashley, T., Holton, J. L., Lees, A. J., Rossor, M. N., Bandopadhyay, R., et al. (2011). Transportin1: a marker of FTLD-FUS. Acta Neuropathologica, 122, 591–600.
Fujioka, Y., Ishigaki, S., Masuda, A., Iguchi, Y., Udagawa, T., Watanabe, H., et al. (2013). FUS-regulated region- and cell-type-specific transcriptome is associated with cell selectivity in ALS/FTLD. Sci Rep. Nature Publishing Group, 3, 2388.
Lagier-Tourenne, C., Polymenidou, M., Hutt, K. R., Vu, A. Q., Baughn, M., Huelga, S. C., et al. (2012). Divergent roles of ALS-linked proteins FUS/TLS and TDP-43 intersect in processing long pre-mRNAs. Nature Neuroscience, 15, 1488–1497.
Mastrocola, A. S., Kim, S. H., Trinh, A. T., Rodenkirch, L. A., & Tibbetts, R. S. (2013). The RNA-binding protein fused in sarcoma (FUS) functions downstream of poly(ADP-ribose) polymerase (PARP) in response to DNA damage. Journal of Biological Chemistry, 288, 24731–24741.
Prpar Mihevc, S., Pavlin, M., Darovic, S., Živin, M., Podbregar, M., Rogelj, B., et al. (2017). Modelling FUS Mislocalisation in an In Vitro Model of Innervated Human Muscle. Journal of Molecular Neuroscience [Internet]. Springer New York LLC; [cited 2022 Dec 4];62:318–28. Available from: https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s12031-017-0940-y
Wächter, N., Storch, A., & Hermann, A. (2015). Human TDP-43 and FUS selectively affect motor neuron maturation and survival in a murine cell model of ALS by non-cell-autonomous mechanisms. Amyotroph Lateral Scler Frontotemporal Degener [Internet]. Amyotroph Lateral Scler Frontotemporal Degener; [cited 2022 Dec 4];16:431–41. Available from: https://pubmed.ncbi.nlm.nih.gov/26174443/
Jensen, B. K., McAvoy, K. J., Heinsinger, N. M., Lepore, A. C., Ilieva, H., Haeusler, A. R., et al. (2022). Targeting TNFα produced by astrocytes expressing amyotrophic lateral sclerosis-linked mutant fused in sarcoma prevents neurodegeneration and motor dysfunction in mice. Glia [Internet]. John Wiley & Sons, Ltd; [cited 2022 Dec 4];70:1426–49. Available from: https://onlinelibrary.wiley.com/doi/full/https://doi.org/10.1002/glia.24183
Guerrero, E. N., Wang, H., Mitra, J., Hegde, P. M., Stowell, S. E., Liachko, N. F., et al. (2016). TDP-43/FUS in motor neuron disease: Complexity and challenges.Prog Neurobiol.
Mitchell, J. C., McGoldrick, P., Vance, C., Hortobagyi, T., Sreedharan, J., Rogelj, B., et al. (2013). Overexpression of human wild-type FUS causes progressive motor neuron degeneration in an age- and dose-dependent fashion. Acta Neuropathol Springer, 125, 273–288.
Dichmann, D. S., & Harland, R. M. (2012). fus/TLS orchestrates splicing of developmental regulators during gastrulation. Genes dev (26 vol., pp. 1351–1363). Cold Spring Harbor Laboratory Press.
Hicks, G. G., Singh, N., Nashabi, A., Mai, S., Bozek, G., Klewes, L., et al. (2000). Fus deficiency in mice results in defective B-lymphocyte development and activation, high levels of chromosomal instability and perinatal death. Nature Genetics, 24, 175–179.
R, S. L., R, A., G, R. L., G, G. J., D.A.Q. M, F., G-HG-H, et al. (2014). PARP-1 dependent recruitment of the amyotrophic lateral sclerosis-associated protein FUS/TLS to sites of oxidative DNA damage. Nucleic Acids Research, 42, 307–314.
Wang, H., Guo, W., Mitra, J., Hegde, P. M., Vandoorne, T., Eckelmann, B. J., et al. (2018). Mutant FUS causes DNA ligation defects to inhibit oxidative damage repair in Amyotrophic Lateral Sclerosis. Nat Commun [Internet]. Nature Publishing Group; [cited 2019 Nov 3];9:3683. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30206235
Kim, B. W., Jeong, Y. E., Wong, M., & Martin, L. J. (2020). DNA damage accumulates and responses are engaged in human ALS brain and spinal motor neurons and DNA repair is activatable in iPSC-derived motor neurons with SOD1 mutations.Acta Neuropathol Commun.
Mitra, J., Guerrero, E. N., Hegde, P. M., Liachko, N. F., Wang, H., Vasquez, V., et al. (2019). Motor neuron disease-associated loss of nuclear TDP-43 is linked to DNA double-strand break repair defects. Proc Natl Acad Sci U S A.
Walker, C., Herranz-Martin, S., Karyka, E., Liao, C., Lewis, K., Elsayed, W., et al. (2017). C9orf72 expansion disrupts ATM-mediated chromosomal break repair.Nat Neurosci.
Wang, W. Y., Pan, L., Su, S. C., Quinn, E. J., Sasaki, M., Jimenez, J. C., et al. (2013). Interaction of FUS and HDAC1 regulates DNA damage response and repair in neurons. Nature Neuroscience, 16, 1383–1391.
Higelin, J., Demestre, M., Putz, S., Delling, J. P., Jacob, C., Lutz, A. K., et al. (2016). FUS Mislocalization and Vulnerability to DNA Damage in ALS Patients Derived hiPSCs and Aging Motoneurons.Front Cell Neurosci. Frontiers Media SA; ;10.
Qiu, H., Lee, S., Shang, Y., Wang, W. Y., Au, K. F., Kamiya, S., et al. (2014). ALS-associated mutation FUS-R521C causes DNA damage and RNA splicing defects. Journal of Clinical Investigation, 124, 981–999.
Martinez-Macias, M. I., Moore, D. A., Green, R. L., Gomez-Herreros, F., Naumann, M., Hermann, A., et al. (2019). FUS (fused in sarcoma) is a component of the cellular response to topoisomerase I-induced DNA breakage and transcriptional stress.Life Sci Alliance. ;2.
Bennett, S. A., Tanaz, R., Cobos, S. N., Torrente, M. P., & Torrente Brooklyn, M. P. (2019 p). Epigenetics in amyotrophic lateral sclerosis: a role for histone post-translational modifications in neurodegenerative disease.Translational Research19–30.
Masala, A., Sanna, S., Esposito, S., Rassu, M., Galioto, M., Zinellu, A., et al. (2018). Epigenetic changes Associated with the expression of amyotrophic lateral sclerosis (ALS) causing genes. Neuroscience (390 vol., pp. 1–11). Elsevier Ltd.
Berson, A., Nativio, R., Berger, S. L., & Bonini, N. M. (2018). Epigenetic Regulation in Neurodegenerative Diseases.Trends Neurosci.
Cui, W., Yoneda, R., Ueda, N., & Kurokawa, R. (2018). Arginine methylation of translocated in liposarcoma (TLS) inhibits its binding to long noncoding RNA, abrogating TLS-mediated repression of CBP/p300 activity. Journal of Biological Chemistry. American Society for Biochemistry and Molecular Biology Inc.; ;293:10937–48.
Chen, K., Bennett, S. A., Rana, N., Yousuf, H., Said, M., Taaseen, S., et al. (2018). Neurodegenerative Disease Proteinopathies are connected to distinct histone post-translational modification landscapes. ACS Chem Neurosci American Chemical Society, 9, 938–948.
McClure, J. J., Li, X., & Chou, C. J. (2018). Advances and Challenges of HDAC Inhibitors in Cancer Therapeutics.Adv Cancer Res.
Ryu, H., Smith, K., Camelo, S. I., Carreras, I., Lee, J., Iglesias, A. H., et al. (2005). Sodium phenylbutyrate prolongs survival and regulates expression of anti-apoptotic genes in transgenic amyotrophic lateral sclerosis mice. J Neurochem. John Wiley & Sons, Ltd; ;93:1087–98.
Yoo, Y. E., & Ko, C. P. (2011). Treatment with trichostatin A initiated after disease onset delays disease progression and increases survival in a mouse model of amyotrophic lateral sclerosis. Exp Neurol Academic Press, 231, 147–159.
Guo, W., Naujock, M., Fumagalli, L., Vandoorne, T., Baatsen, P., Boon, R., et al. (2017). HDAC6 inhibition reverses axonal transport defects in motor neurons derived from FUS-ALS patients. Nat Commun Nature Publishing Group, 8, 861.
Rossaert, E., Pollari, E., Jaspers, T., Van Helleputte, L., Jarpe, M., Van Damme, P., et al. (2019). Restoration of histone acetylation ameliorates disease and metabolic abnormalities in a FUS mouse model. Acta Neuropathol Commun NLM (Medline), 7, 107.
Litt, M., Qiu, Y., & Huang, S. (2009). Histone arginine methylations: their roles in chromatin dynamics and transcriptional regulation (pp. 131–141). Biosci Rep. Portland Press.
Scaramuzzino, C., Monaghan, J., Milioto, C., Lanson, N. A., Maltare, A., Aggarwal, T., et al. (2013). Protein Arginine Methyltransferase 1 and 8 Interact with FUS to Modify Its Sub-Cellular Distribution and Toxicity In Vitro and In Vivo.PLoS One. ;8.
Tibshirani, M., Tradewell, M. L., Mattina, K. R., Minotti, S., Yang, W., Zhou, H., et al. Cytoplasmic sequestration of FUS/TLS associated with ALS alters histone marks through loss of nuclear protein arginine methyltransferase 1.
Ward, C. L., Boggio, K. J., Johnson, B. N., Boyd, J. B., Douthwright, S., Shaffer, S. A., et al. (2014). A loss of FUS/TLS function leads to impaired cellular proliferation.Cell Death Dis. Nature Publishing Group; ;5.
Rusk, N. (2008). When microRNAs activate translation. Nat Methods Nature Publishing Group, 5, 122–123.
Vasudevan, S., Tong, Y., & Steitz, J. A. (1979). Switching from Repression to Activation: MicroRNAs Can Up-Regulate Translation. Science 2007;318:1931–4.
Morlando, M., Dini Modigliani, S., Torrelli, G., Rosa, A., Di Carlo, V., Caffarelli, E., et al. (2012). FUS stimulates microRNA biogenesis by facilitating co-transcriptional Drosha recruitment. EMBO Journal, 31, 4502–4510.
De Santis, R., Santini, L., Colantoni, A., Peruzzi, G., de Turris, V., Alfano, V., et al. (2017). FUS Mutant Human Motoneurons Display altered transcriptome and microRNA pathways with implications for ALS Pathogenesis. Stem Cell Reports Cell Press, 9, 1450–1462.
Zhang, T., Wu, Y. C. C., Mullane, P., Ji, Y. J., Liu, H., He, L., et al. (2018). FUS regulates activity of MicroRNA-Mediated gene silencing. Mol Cell Cell Press, 69, 787–801e8.
Orozco, D., & Edbauer, D. (2013). FUS-mediated alternative splicing in the nervous system: Consequences for ALS and FTLD. J Mol Med. Springer; p. 1343–54.
Rogelj, B., Easton, L. E., Bogu, G. K., Stanton, L. W., Rot, G., Curk, T. T., et al. (2012). Widespread binding of FUS along nascent RNA regulates alternative splicing in the brain.Sci Rep. Nature Publishing Group; ;2.
Yu, Y., Chi, B., Xia, W., Gangopadhyay, J., Yamazaki, T., Winkelbauer-Hurt, M. E., et al. (2015). U1 snRNP is mislocalized in ALS patient fibroblasts bearing NLS mutations in FUS and is required for motor neuron outgrowth in zebrafish. Nucleic Acids Research, 43, 3208–3218.
Yu, Y., & Reed, R. (2015). FUS functions in coupling transcription to splicing by mediating an interaction between RNAP II and U1 snRNP. Proc Natl Acad Sci U S A National Academy of Sciences, 112, 8608–8613.
Ishigaki, S., Masuda, A., Fujioka, Y., Iguchi, Y., Katsuno, M., Shibata, A., et al. (2012). Position-dependent FUS-RNA interactions regulate alternative splicing events and transcriptions.Sci Rep. Nature Publishing Group; ;2.
Humphrey, J., Birsa, N., Milioto, C., Robaldo, D., Eberle, A. B., Kräuchi, R., et al. (2019). FUS ALS-causative mutations impact FUS autoregulation and the processing of RNA-binding proteins through intron retention. bioRxiv (p. 567735). Cold Spring Harbor Laboratory.
Grabowski, P. (2011). Alternative splicing takes shape during neuronal development.Curr Opin Genet Dev.
Tyzack, G. E., Luisier, R., Taha, D. M., Neeves, J., Modic, M., Mitchell, J. S., et al. (2019). Widespread FUS mislocalization is a molecular hallmark of amyotrophic lateral sclerosis.Brain.
Japtok, J., Lojewksi, X., Naumann, M., Klingenstein, M., Reinhardt, P., Sterneckert, J., et al. (2015). Stepwise acquirement of hallmark neuropathology in FUS-ALS iPSC models depends on mutation type and neuronal aging. Neurobiol Dis Academic Press Inc, 82, 420–429.
Marrone, L., Poser, I., Casci, I., Japtok, J., Reinhardt, P., Janosch, A., et al. (2018). Isogenic FUS-eGFP iPSC reporter lines enable quantification of FUS stress Granule Pathology that is rescued by drugs inducing Autophagy. Stem Cell Reports Elsevier, 10, 375–389.
Birsa, N., Bentham, M. P., & Fratta, P. (2020). Cytoplasmic functions of TDP-43 and FUS and their role in ALS. Semin Cell Dev Biol (pp. 193–201). Elsevier Ltd.
Stefl, R., Skrisovska, L., & Allain, F. H. T. (2005). RNA sequence- and shape-dependent recognition by proteins in the ribonucleoprotein particle.EMBO Rep.
Nostramo, R., Xing, S., Zhang, B., & Herman, P. K. (2019). Insights into the role of P-bodies and stress granules in protein quality control.Genetics.
Anderson, P., & Kedersha, N. (2008). Stress granules: the Tao of RNA triage.Trends Biochem Sci.
Lenzi, J., De Santis, R., De Turris, V., Morlando, M., Laneve, P., Calvo, A., et al. (2015). ALS mutant FUS proteins are recruited into stress granules in induced pluripotent stem cell-derived motoneurons. Company of Biologists Ltd, 8, 755–766.
Jain, S., Wheeler, J. R., Walters, R. W., Agrawal, A., Barsic, A., & Parker, R. (2016). ATPase-Modulated Stress Granules Contain a Diverse Proteome and Substructure.Cell.
Bosco, D. A., Lemay, N., Ko, H. K., Zhou, H., Burke, C., Kwiatkowski, T. J., et al. (2010). Mutant FUS proteins that cause amyotrophic lateral sclerosis incorporate into stress granules.Hum Mol Genet.
Aulas, A., Stabile, S., Vande Velde, C., & Endogenous (2012). TDP-43, but not FUS, contributes to stress granule assembly via G3BP.Mol Neurodegener.
Baron, D. M., Kaushansky, L. J., Ward, C. L., Sama, R. R. K., Chian, R. J., Boggio, K. J., et al. (2013). Amyotrophic lateral sclerosis-linked FUS/TLS alters stress granule assembly and dynamics. Mol Neurodegener [Internet]. BioMed Central; [cited 2020 May 23];8:30. Available from: http://molecularneurodegeneration.biomedcentral.com/articles/https://doi.org/10.1186/1750-1326-8-30
Sama, R. R. K., Ward, C. L., Kaushansky, L. J., Lemay, N., Ishigaki, S., Urano, F., et al. (2013). FUS/TLS assembles into stress granules and is a prosurvival factor during hyperosmolar stress. Journal Of Cellular Physiology, 228, 2222–2231.
Dormann, D., Rodde, R., Edbauer, D., Bentmann, E., Fischer, I., Hruscha, A., et al. (2010). ALS-associated fused in sarcoma (FUS) mutations disrupt transportin-mediated nuclear import.EMBO Journal.
Sweeney, P., Park, H., Baumann, M., Dunlop, J., Frydman, J., Kopito, R., et al. (2017). Protein misfolding in neurodegenerative diseases: implications and strategies.Transl Neurodegener. Transl Neurodegener; ;6.
Zhang, P., Fan, B., Yang, P., Temirov, J., Messing, J., Kim, H. J., et al. (2019). Chronic optogenetic induction of stress granules is cytotoxic and reveals the evolution of ALS-FTD pathology (p. 8). Elife: eLife Sciences Publications Ltd.
Shelkovnikova, T. A., Robinson, H. K., Connor-Robson, N., & Buchman, V. L. (2013). Recruitment into stress granules prevents irreversible aggregation of FUS protein mislocalized to the cytoplasm. Cell Cycle Taylor and Francis Inc, 12, 3383–3391.
Alexander, E. J., Niaki, A. G., Zhang, T., Sarkar, J., Liu, Y., Nirujogi, R. S., et al. (2018). Ubiquilin 2 modulates ALS/FTD-linked FUS–RNA complex dynamics and stress granule formation (115 vol., pp. E11485–E11494). Proc Natl Acad Sci U S A. National Academy of Sciences.
Casci, I., Krishnamurthy, K., Kour, S., Tripathy, V., Ramesh, N., Anderson, E. N., et al. (2019). Muscleblind acts as a modifier of FUS toxicity by modulating stress granule dynamics and SMN localization.Nat Commun. Nature Research; ;10.
Ryu, H. H., Jun, M. H., Min, K. J., Jang, D. J., Lee, Y. S., Kim, H. K., et al. (2014). Autophagy regulates amyotrophic lateral sclerosis-linked fused in sarcoma-positive stress granules in neurons. Neurobiol Aging Elsevier Inc, 35, 2822–2831.
McCormick, C., & Khaperskyy, D. A. (2017). Translation inhibition and stress granules in the antiviral immune response.Nat Rev Immunol.
Limongi, D., & Baldelli, S. (2016). Redox Imbalance and Viral Infections in Neurodegenerative Diseases.Oxid Med Cell Longev.
Xue, Y. C., Feuer, R., Cashman, N., & Luo, H. (2018). Enteroviral infection: The forgotten link to amyotrophic lateral sclerosis?Front Mol Neurosci.
Celeste, D. B., & Miller, M. S. (2018). Reviewing the evidence for viruses as environmental risk factors for ALS: a new perspective. Cytokine (pp. 173–178). Academic Press.
Verma, A., & Berger, J. R. (2006). ALS syndrome in patients with HIV-1 infection.J Neurol Sci.
Shelkovnikova, T. A., An, H., Skelt, L., Tregoning, J. S., Humphreys, I. R., & Buchman, V. L. (2019). Antiviral Immune response as a trigger of FUS Proteinopathy in Amyotrophic lateral sclerosis. Cell Rep Elsevier B V, 29, 4496–4508e4.
Rhoads, S. N., Monahan, Z. T., Yee, D. S., & Shewmaker, F. P. (2018). The Role of Post-Translational Modifications on Prion-Like Aggregation and Liquid-Phase Separation of FUS. Int J Mol Sci. Multidisciplinary Digital Publishing Institute; p. 886.
Aulas, A., Velde, C., & Vande (2015). Alterations in stress granule dynamics driven by TDP-43 and FUS: A link to pathological inclusions in ALS? Front Cell Neurosci.Frontiers Research Foundation; ;9.
Zappulo, A., van den Bruck, D., Ciolli Mattioli, C., Franke, V., Imami, K., McShane, E., et al. (2017). RNA localization is a key determinant of neurite-enriched proteome. Nature Communications, 8, 583.
Eliscovich, C., & Singer, R. H. (2017). RNP transport in cell biology: the long and winding road.Curr Opin Cell Biol.
Jung, H., Yoon, B. C., & Holt, C. E. (2012). Axonal mRNA localization and local protein synthesis in nervous system assembly, maintenance and repair.Nat Rev Neurosci.
Karamyshev, A. L., & Karamysheva, Z. N. (2018). Lost in translation: Ribosome-associated mRNA and protein quality controls.Front Genet.
Kamelgarn, M., Chen, J., Kuang, L., Jin, H., Kasarskis, E. J., Zhu, H., & S A [Internet]. (2018). ALS mutations of FUS suppress protein translation and disrupt the regulation of nonsense-mediated decay. Proc Natl Acad Sci U. National Academy of Sciences; [cited 2019 Feb 15];115:E11904–13. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30455313
López-Erauskin, J., Tadokoro, T., Baughn, M. W., Myers, B., McAlonis-Downes, M., Chillon-Marinas, C., et al. (2018). ALS/FTD-Linked Mutation in FUS Suppresses Intra-axonal Protein Synthesis and Drives Disease Without Nuclear Loss-of-Function of FUS. Neuron [Internet]. Cell Press; [cited 2019 Feb 15];100:816–830.e7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0896627318308468
Nakaya, T., & Maragkakis, M. (2018). Amyotrophic lateral sclerosis associated FUS mutation shortens mitochondria and induces neurotoxicity. Sci Rep Nature Publishing Group, 8, 1–15.
de la Fuente, F. R., & Emc, F. (2020). FUS-ALS mutants alter FMRP phase separation equilibrium and impair protein translation Birsa N. bioRxiv [Internet]. Cold Spring Harbor Laboratory; [cited 2020 Sep 22];2020.09.14.296038. Available from: https://doi.org/10.1101/2020.09.14.296038
Bond, S., Lopez-Lloreda, C., Gannon, P. J., Akay-Espinoza, C., & Jordan-Sciutto, K. L. (2020). The integrated stress response and phosphorylated eukaryotic initiation factor 2α in neurodegeneration.J Neuropathol Exp Neurol.
Blum, J. A., & Gitler, A. D. (2022). Singling out motor neurons in the age of single-cell transcriptomics. Trends in Genetics Elsevier Current Trends, 38, 904–919.
Nichterwitz, S., Nijssen, J., Storvall, H., Schweingruber, C., Comley, L. H., Allodi, I., et al. (2020). LCM-seq reveals unique transcriptional adaptation mechanisms of resistant neurons and identifies protective pathways in spinal muscular atrophy. Genome Res [Internet]. Cold Spring Harbor Laboratory Press; [cited 2022 Dec 4];30:1083–96. Available from: https://pubmed.ncbi.nlm.nih.gov/32820007/
Lee, J., Yoo, M., & Choi, J. (2022). Recent advances in spatially resolved transcriptomics: challenges and opportunities. BMB Rep [Internet]. Korean Society for Biochemistry and Molecular Biology; [cited 2022 Dec 4];55:113. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8972138/
Russ, D. E., Cross, R. B. P., Li, L., Koch, S. C., Matson, K. J. E., Yadav, A., et al. (2021). A harmonized atlas of mouse spinal cord cell types and their spatial organization. Nature Communications 2021 12:1 [Internet]. Nature Publishing Group; [cited 2022 Dec 4];12:1–20. Available from: https://www.nature.com/articles/s41467-021-25125-1
Maniatis, S., Äijö, T., Vickovic, S., Braine, C., Kang, K., Mollbrink, A., et al. (2019). Spatiotemporal dynamics of molecular pathology in amyotrophic lateral sclerosis. Science [Internet]. Science; [cited 2022 Dec 4];364:89–93. Available from: https://pubmed.ncbi.nlm.nih.gov/30948552/
Kim, H. J. (2019). Cell fate control by translation: MRNA translation initiation as a therapeutic target for cancer development and stem cell fate control. Biomolecules. MDPI AG.
Powley, I. R., Kondrashov, A., Young, L. A., Dobbyn, H. C., Hill, K., Cannell, I. G., et al. (2009). Translational reprogramming following UVB irradiation is mediated by DNA-PKcs and allows selective recruitment to the polysomes of mRNAs encoding DNA repair enzymes. Genes dev (23 vol., pp. 1207–1220). Cold Spring Harbor Laboratory Press.
Bennetzen, M. V., Kosar, M., Bunkenborg, J., Payne, M. R., Bartkova, J., Lindström, M. S., et al. (2018). DNA damage-induced dynamic changes in abundance and cytosol-nuclear translocation of proteins involved in translational processes, metabolism, and autophagy (17 vol., pp. 2146–2163). Cell Cycle. Taylor and Francis Inc.
Nott, A., Le Hir, H., & Moore, M. J. (2004). Splicing enhances translation in mammalian cells: an additional function of the exon junction complex. Genes dev (18 vol., pp. 210–222). Cold Spring Harbor Laboratory Press.
Sephton, C. F., & Yu, G. (2015). The function of RNA-binding proteins at the synapse: implications for neurodegeneration. Cellular and Molecular Life Sciences.
Acknowledgements
We thank the people in the Foijer and Zatz labs for fruitful discussions.
Funding
This work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and an Abel Tasman fellowship to AA awarded by the University of Groningen. The funding agencies had no role in the design of the study and collection, analysis, and interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Amanda F. Assoni: Conceptualization; literature search; data curation; writing – original draft; writing – review and editing. Floris Foijer: Conceptualization; resources; data curation; writing – review and editing. Mayana Zatz: Conceptualization; supervision; resources; writing – review and editing.
Corresponding author
Ethics declarations
Ethics approval
Not Aplicable.
Consent for Publication
Not Aplicable.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Assoni, A.F., Foijer, F. & Zatz, M. Amyotrophic Lateral Sclerosis, FUS and Protein Synthesis Defects. Stem Cell Rev and Rep 19, 625–638 (2023). https://doi.org/10.1007/s12015-022-10489-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-022-10489-8