Abstract
Vascularization is a major hurdle in complex tissue and organ engineering. Tissues greater than 200 μm in diameter cannot rely on simple diffusion to obtain nutrients and remove waste. Therefore, an integrated vascular network is required for clinical translation of engineered tissues. Microvessels have been described as <150 μm in diameter, but clinically they are defined as <1 mm. With new advances in super microsurgery, vessels less than 1 mm can be anastomosed to the recipient circulation. However, this technical advancement still relies on the creation of a stable engineered microcirculation that is amenable to surgical manipulation and is readily perfusable. Microvascular engineering lays on the crossroads of microfabrication, microfluidics, and tissue engineering strategies that utilize various cellular constituents. Early research focused on vascularization by co-culture and cellular interactions, with the addition of angiogenic growth factors to promote vascular growth. Since then, multiple strategies have been utilized taking advantage of innovations in additive manufacturing, biomaterials, and cell biology. However, the anatomy and dynamics of native blood vessels has not been consistently replicated. Inconsistent results can be partially attributed to cell sourcing which remains an enigma for microvascular engineering. Variations of endothelial cells, endothelial progenitor cells, and stem cells have all been used for microvascular network fabrication along with various mural cells. As each source offers advantages and disadvantages, there continues to be a lack of consensus. Furthermore, discord may be attributed to incomplete understanding about cell isolation and characterization without considering the microvascular architecture of the desired tissue/organ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the aims of tissue engineering is to create replacement parts for damaged tissue and organs. This achievement would have profound clinical implications, especially in the disciplines of reconstructive surgery, transplant medicine and vascular surgery. Over 110,000 patients are currently waiting for an organ transplant and thousands of others could benefit from a vascularized composite allograft [1]. However, clinical translation of engineered tissue has been limited by the insufficient diffusion of oxygen and nutrients [2] into the graft. At diffusion distances greater than 150–200 μm, tissue constructs without a perfusable vascular network undergo rapid cell death and necrosis [3]. Therefore, in order to achieve successful implantation, the engineered replacement mandates rapid perfusion and integration with the recipient vasculature [4]. This typically requires a surgical anastomosis between the vascularized construct and recipient vasculature. Parameters such as size of the vascular connection and perfusion rate can affect patency [5]. Therefore, an engineered construct that contains a vascular tree from the capillary level (~5 μm diameter) to one that permits surgical anastomosis (~1 mm diameter) wound be welcomed. Advances in microvascular engineering would also be embraced by any medical or surgical field in which microvascular dysfunction is present, such as diabetic retinopathy [6], microvascular myocardial angina [7], and critical limb ischemia. For example, it is estimated that 1% of Americans over 50 years will develop critical limb ischemia [8]. While surgical advances have reduced the incidence of patients that ultimately require amputation, they are not feasible in all situations. This is particularly true when the blood flow limiting pathology occurs in the microvascular segment, as typically seen in diabetic patients [9].
Current approaches for vascularization rely on a variety of cell sources and approaches [10], with endothelial cells (EC) being a foundation. However, as ECs are significant in the rejection of allografts [11], it is imperative that cells used for microvascular engineering are compatible with the planned recipient. Therefore, cell sourcing must account for immunogenicity, in addition to other factors such as ease of isolation, reliable characterization, and vasculogenic/angiogenic potential. This has led to the investigation of mature endothelial cells, endothelial progenitor cells (EPCs), and other stem cell sources for the formation of microvascular networks in tissue engineered constructs and the treatment of critical ischemia.
Microvascular Development, Angiogenesis, and Revascularization
Embryologically, vascular development occurs through the processes of vasculogenesis and angiogenesis (Fig. 1) [12] . Vasculogenesis is the process of vessel formation in the early stage of development during which de novo blood vessels are formed from endothelial progenitor cells [13]. The lateral and posterior mesoderm in the gastrulating embryo express vascular endothelial growth factor receptor-2 (VEGFR2), the receptor for VEGF, which is the most crucial signal for embryonic vascular formation [14]. This receptor tyrosine kinase is encoded by the KDR (kinase insert domain receptor) gene, which is also known as fetal liver kinase-1 (FLK-1). The VEGFR2 expressing cells cluster to form hemangioblastic aggregates [15]. The peripheral cells (angioblasts) flatten and differentiate into ECs, while the central cells form hematopoietic precursors. These progenitor cells migrate in response to endoderm derived signals, such as FGF (fibroblast growth factor) and BMP4 (bone morphogenic protein), to the sites of vascularization [16]. Following this, the ECs rapidly anastomose to form capillaries/primary vascular plexus and serve as a scaffold for the circulation. After the onset of heartbeat and blood flow, the capillary plexus is rapidly remodeled into a functional circulatory system [14]. Angiogenesis begins on embryonic day 8.5 in the mouse yolk sac [17, 18] and occurs through a coordinated series of events where vascular sprouts grow from specialized endothelial “tip cells” in response to angiogenic stimuli [19]. Initially, local destruction of the basement membrane occurs, followed by sprouting, proliferation, and alignment of endothelial cells into a tube. Angiogenesis is responsible for vascular remodeling through both sprouting and intussusceptive mechanisms with VEGF maintaining a critical role. Once the definitive vascular network is established, ECs remain quiescent until physiological or pathological events occur that require neovascularization. Neovascularization is achieved by both vasculogenesis (EPCs) and angiogenesis (adult ECs) [20] through gene expression, transcriptional factors, and microRNA (miRNA) regulation. Growth factors, cytokines and proteins play a major role in endothelial differentiation (Table 1; Figure 2) with VEGF and it’s receptors (VEGFR1 and VEGFR2) indispensable for blood vessel development and remodeling [46]. However, numerous signals/proteins are involved including Notch, Ephrin, Sonic hedgehog, and angiopoietin (Ang)-Tie. Notch signaling regulates both cellular proliferation and development, and in association with delta-like 4 (Dll4) modulates sprouting angiogenesis [47] via tip cells [48]. Ang-Tie is an EC specific signaling system that is necessary in both embryonic vascular development and regulation of postnatal angiogenesis [49]. Transcription factors regulate these critical gene expressions to modulate angiogenesis (Table 2). The ETS (E26 transformation-specific) transcription factor family plays a significant role in angiogenesis by targeting genes such as von Willebrand factor (vWF), Endoglin, Ang-Tie, VEGFR2, eNOS (endothelial nitric oxide synthase), and VE-cadherin [72]. For example, the ETS transcription factor Erg is required for endothelial tube formation through its association with VE-cadherin [36].
Vasculogenesis and angiogenesis: Two distinct mechanisms of blood vessel formation. Vasculogenesis gives rise to the primitive vascular plexus during embryogenesis. Stimulated by tumors and hypoxic conditions, angiogenesis remodels and expands the vascular network [12]
STRING analysis of functional protein association networks in vasculogenesis: Key proteins and transcription factors that are involved in vasculogenesis were identified by a literature search. Protein-protein interactions were evalauted using STRING analysis. The interactions between proteins and transcriptional factors within major Biological Processes (GO) such as vasculature development (blue color), blood vessel development (red color) and morphogenesis (green color) are highlighted
Gene expression is also controlled by miRNAs, which are small non-coding RNA molecules containing approximately 17-25 nucleotides that negatively regulate gene expression either by reducing translational efficiency or transcript degradation. A single miRNA has the ability to regulate hundreds of genes and affect the downstream transcriptome and proteome. Therefore, they have a profound ability to affect multiple biological processes, such as development, differentiation and growth. Recent studies have highlighted their involvement in vascular development (Table 3), with many studies focusing on their involvement in the VEGF signaling pathway. MicroRNAs affect vascular development by playing substantial modulatory roles, both at the ligand level and further downstream through intracellular signaling pathways, such as phosphoinositide-3-kinase (PI3K) and MAPK/ERK [87]. Their importance in embryonic angiogenesis has further been verified though Dicer-knockout mice which die mid-gestation [88]. However, miRNA involvement has also been suggested in post-natal vascular pathologies, including critical limb ischemia. Spinetti et al. have suggested that miRNA-15a and miRNA-16 impair circulating proangiogenic cell function and are increased in patients with critical limb ischemia [89]. Additionally, the authors further demonstrated that ex vivo inhibition of these miRNAs improved post-ischemia blood flow and muscular arteriole density in a murine model of critical limb ischemia [89]. Therefore, it is not surprising that miRNA modulation has emerged as a technology to facilitate vascular engineering [90], both in vivo and ex vivo. However, as the vascular system is diverse in size, architecture, and functionality, multiple engineering approaches may need to be considered in a coordinated fashion Table 4.
Histology and Anatomy
The vasculature can be apportioned between the microvasculature and the macrovasculature. The microvasculature cannot be seen with the naked eye and is typically defined anatomically as having a luminal diameter <150 μm and functionally as regulating the total peripheral resistance in the vascular tree [102]. This includes arterioles, capillaries, and venules. Arterioles originate from arteries to arborize into capillaries which coalesce into venules that drain into veins. All constituents of the vascular tree are lined by endothelial cells (tunica intima) with varying degrees of stromal cells. Arterioles (100 to 300 μm diameter) have muscular walls (tunica media) that consist of a few layers of smooth muscle cells surrounded by a collagen layer (tunica adventitia). Capillaries (5 to 10 μm diameter) only have a single EC layer without any other distinct layers. This allows efficient material exchange between the blood and interstitium. Venules (7 μm to 1 mm diameter) contain a middle layer of muscle/elastic tissue and an outer layer of connective tissue. The ECs in capillaries and venules are enveloped by pericytes which are located in the basement membrane. Pericytes regulate microvascular morphogenesis and homeostasis while exhibiting some mesenchymal stem/progenitor cell functionality [103]. However, these cellular behaviors and interactions are also profoundly affected by the surrounding extracellular matrix (ECM).
The ECM is a structural support system that provides a matrix for cell adhesion and serves as a storage depot for growth factors [104]. Therefore, it is not surprising that it plays a large role in coordinating the angiogenic process through pro- and anti-angiogenic factor regulation , matrix- degrading proteases, and cell-ECM interactions [105]. The ECM is synthesized by fibroblasts and includes structural proteins (e.g. collagen), adhesive glycoproteins (e.g. fibronectin, laminin), glycosaminoglycans (e.g. hyaluronan), and proteoglycans (e.g. heparin sulfate) [104, 105]. It can broadly be subdivided into the interstitial matrix and the extracellular basement membrane, with the former consisting of collagen, fibronectin, elastin, and proteoglycans and the latter consisting of collagen IV, laminin, entactin, and heparin sulfate which binds to VEGF [106]. These ECM molecules/fragments can function in either a pro-angiogenic (e.g. collagen I, fibronectin, laminin-1) or anti-angiogenic fashion (e.g. arresten, endostatin) [106]. Angiogenesis occurs in ischemic tissues when oxygen sensing mechanisms detect a level of hypoxia that requires new blood vessel formation to satisfy metabolic demands. The most common form occurs in stages through a sprouting mechanism (Fig. 3) as follows: enzymatic degradation of the capillary basement membrane, endothelial cell proliferation, directed migration, tubulogenesis, vessel fusion; and pericyte [107], smooth muscle, and fibroblast stabilization [108]. This coordinated activity is orchestrated by the mechanical forces in the ECM along with cell-cell and cell-matrix interactions, bound proteins, and soluble growth factors. For example, αVβ3 integrin present on ECs allows for binding to ECM vitronectin which augments the EC responsiveness to soluble factors, such as VEGF [104]. This intricate interplay allows for varied angiogenic responses depending on the initiating factors and anatomic site.
Sprouting angiogenesis: After stimulation with angiogenic factors of a quiescent vessel (a), basement membrane degradation, pericyte detachment, and loosening of endothelial cell junctions occur (b). Endothelial cells begin to proliferate, migrate, and take part in forming an immature capillary structure and depositing a new basement membrane (c). Finally, pericytes are recruited thereby providing stabilization of the new vessel (d) [106]
Variability in the microcirculatory bed across different tissues and organs is secondary to differences in cellular composition leading to adaptable physiology. For example, the microcirculation of the skin is distinct from that seen in the pancreatic islets as the skin microvasculature contains a large number of post-capillary venules that aid in preventing unwanted external elements from entering the body and thermoregulation [109]. The endocrine pancreatic islets are arranged around a central capillary that allows blood to first pass through centrally located β-cells and initiate an insulin response to circulating glucose prior to encountering α-cells and δ-cells that are responsible for appropriate counter-regulatory hormone secretion [110]. These subtle differences in microvascular anatomy and cell subtype are paramount in the regulation of blood flow to diverse tissues and organs. Therefore, specific cellular starting materials will be required to generate the desired microvascular bed for the engineered replacement tissue.
Cell Source and Type
ECs and mural cells (pericytes and smooth muscle cells) are the mainstay of engineering strategies, as they play essential developmental roles of the vascular tree [111]. However, varied cell sources have been utilized with each having innate advantages and disadvantages in microvascular network assembly.
Endothelial Cells
ECs typically express von Willebrand factor, vascular endothelial (VE)-cadherin, and platelet endothelial cell adhesion molecule-1 (PECAM-1/CD31) [112]. They are instrumental in diapedesis, vascular tone, and smooth muscle cell proliferation [113]. As they are ubiquitous to the entire vascular tree, they have been investigated extensively for in vitro vascular engineering. It has long been appreciated that vascular graft failure is mediated by platelet initiated thrombosis and mitigated by an intact EC monolayer [114]. However, grafts less than 6 mm are still unreliable and not routinely used in clinical practice [115]. This limitation is problematic for the development of engineered and immediately perfusable tissues as they require the integration of vessels ranging from 5 μm to 1 mm to permit both physiologic functionality and the ability for surgical anastomosis. However, there have been substantial advances in in vitro microvascular engineering, especially with the generation of prevascularized tissues. Both macrovascular and microvascular endothelial cells have been utilized for this purpose. Differences do exist between them and are further amplified depending on the tissue source. As such, macrovascular cells include those originating from the pulmonary artery, coronaries, aorta, saphenous vein, umbilical cord, and dermis. Likewise, microvascular cells from virtually all these locations are available as well. Human umbilical vein endothelial cells (HUVECs) are the most widely used type of macrovascular cell for the purpose of forming a neovasculature. HUVECs have been demonstrated to undergo self-assembly into capillary structures in a variety of studies, especially when used in the presence of a basement-membrane matrix, such as Matrigel [91]. Although Matrigel is useful for microvascular engineering and study, its disadvantages are its sarcoma cell origin and lot-to-lot variability [116]. These factors may limit its potential for clinical translation and other scaffolds have been established using HUVECs. Nakatsu et al. described a fibrin gel based bead assay where Cytodex (Sigma-Aldrich, St. Louis, MO) beads were coated with ECs prior to being embedded in a fibrin gel that was subsequently coated with fibroblasts [117]. The fibroblasts provide the soluble factors that allow for angiogenesis. This model has been replicated with various EC and feeder cell sources and has been used extensively in the study of microvascular engineering. Rioja et al., described a modular approach to microvascular engineering where HUVECs/fibroblast loaded fibrin or collagen-fibrin composite microbeads were embedded in a fibrin hydrogel (Fig. 4a) [92]. The authors demonstrated that endothelial networks formed and anastomosis between microbeads was established. However, in order to recapitulate the desired native microvascular anatomy, a patterning strategy may need to be employed that can optimize incorporation and physiologic function. Baranski et al., utilized a micropatterning technique to organize HUVECs into cords which following implantation acted as a guide for capillary formation [119]. When implanted with hepatocytes, prevascularized constructs with cords integrated and survived better than constructs that had randomly organized microvascular networks [119] . However, even with this approach it takes 5 to 14 days for mature capillaries to develop, which is still suboptimal to prevent necrosis of the innermost cell mass. Angiogenic integration of a prevascularized construct following implantation still requires progression through several stages as follows: enzymatic degradation of the capillary basement membrane, endothelial cell proliferation, directed migration, tubulogenesis, vessel fusion, and pericyte stabilization [107]. Specifically, the initial step of angiogenesis is controlled ECM degradation by matrix metalloproteinases (MMPs) that are secreted by ECs and other cells. As angiogenesis occurs in the microvasculature, differences in the expression of MMPs has been demonstrated between microvascular and macrovascular ECs, with substantially more MMP9 being secreted by microvascular cells [120]. Therefore, it may be worthwhile to revascularize grafts with microvascular cells to hasten angiogenic integration. It is also known that microvascular cells are critical to the formation of new blood vessels through sprouting mechanisms and may not require exogenous pro-angiogenic growth factors when used in specific co-cultures [121]. This may have significant implications for engraftment and rapid perfusion of prevascularized tissues upon implantation. Dermal microvascular endothelial cells (DMVECs) represent a type of microvascular cell that have been used extensively [93]. However, there have been concerns that mature ECs lack significant regenerative potential [122], autologous sources may be problematic to obtain in ample quantities, and that phenotype expression is tissue dependent [123, 124]. These concerns have prompted the examination of other cell sources for microvascular engineering.
Various cell sources for microvascular engineering: Microvascular bioengineering from various cell types: a HUVECs labeled with UEA-1 (red) were loaded onto microbeads (green) and demonstrated sprouting at 14 days [92], b iPSC→ECs were cultured for 3 days on PEG hydrogels and stained for CD31 (green), VE-Cadherin (red) and DAPI (blue) [98], c human adipose derived EPCs (CD34+/CD31-) loaded with CellTracker Red (Thermo Fisher, Eugene, OR) cultured on a 3D collagen gel demonstrating tube formation at 24 hours (our laboratory unpublished work) and d cross section of microvascular fragments seeded onto a porous scaffold and stained with hematoxylin and eosin [118]
Embryonic Stem Cells
Embryonic stem cells (ESCs) were first reported in the mouse in 1981 followed by identification in humans in 1998 [125, 126, 127]. ESCs are located in the inner cell mass of the embryo [126] and are true pluripotent stem cells. As such, they can proliferate indefinitely and differentiate into any cell type while imparting low immunogenicity. These characteristics makes them especially appropriate for tissue engineering strategies, including microvascular replacement [128]. Levenberg et al., described the differentiation of human ESCs into endothelial cells in 2002 [94]. Following the formation of embryoid bodies (EBs), cells expressing PECAM-1 were isolated and sorted. After six passages, cells displayed CD34 and FLK-1 markers similar to that seen in HUVECs. Cords with lumens developed following seeding onto Matrigel. Furthermore, after a week of animal implantation an ESC→EC coated scaffold integrated with the host vasculature and had evidence of perfusion [94]. In a follow-up study the same group utilized ESC derived ECs to engineer vascularized skeletal muscle [95]. This was accomplished by co-culturing human ESC→ECs with mouse skeletal myoblast cells and mouse embryonic fibroblasts on a highly porous, biodegradable polymer scaffold. It was shown that the addition of fibroblasts increased the expression of VEGF and promoted microvessel stability following a month-long in vitro culture. Animal implantation demonstrated vigorous anastomosis with the host vasculature which was similar to that seen with HUVECs. Most interestingly, the vessels were completely integrated with the differentiating skeletal muscles fibers [95]. While the therapeutic advantages of ESCs are sizable, it is unfortunate that their downsides may be greater. The mechanisms that regulate ESC pluripotency and differentiation are still poorly understood with the contribution of various transcription factors, cofactors, chromatin regulators, and noncoding RNAs still imprecise [129]. Additionally, as ESCs are derived from the inner cell mass of a pre-implantation embryo, there are significant ethical concerns with cell retrieval. These considerations significantly hinder the potential for clinical translation. As such, other stem cell and progenitor cell sources are continuously being explored.
Induced Pluripotent Stem Cells
Advances in cellular reprograming has led to the detection of a noteworthy alternative cell source for therapeutic vascularization, induced pluripotent stem cells (iPSCs). iPSCs have the capacity for pluripotency and self-renewal, much like ESCs [130]. When initially described by Yamanaka in 2006, they were generated from mouse embryonic or adult fibroblasts (somatic cells) through the introduction of four transcription factors; OCT 3/4, SOX2, KLF4, and c-MYC via integrative retroviral delivery [130, 131]. The subsequent year, production using human fibroblasts was described using the same transcription factors [132], while a separate group used OCT4, NANOG, SOX2, and LIN28 [133] for reprogramming. These early efforts were hampered by low reprogramming efficiency, viral integration, and severe genomic modifications [134]. However, since then programming efficiency has been improved and the use of DNA-free vectors [135], non-integrating vectors, or vector excision has mitigated the incorporation of viral transgenes [136], improving safety. As such, the use of iPSCs has expanded across multiple disciplines, including microvascular engineering. Ikuno et al., utilized human iPSC lines for differentiation into endothelial cells. The authors utilized a 2D monolayer serum-free culture system and ordered differentiation using stage-specific stimulation with VEGF and cAMP while removing non-responder cells early in the process [96]. iPSC derived ECs demonstrated CD31, VE-Cadherin, and endothelial nitric oxide synthase (eNOS) similar to HUVECs but with increased CD34 and CD133 expression. CD34 and CD133 are markers of both ECs and multipotent progenitor cells; therefore, it is not surprising that they were expressed on iPSC derived ECs. Additionally, these cells exhibited tube forming ability and morphology similar to the gold-standard HUVECs [96] when cultured on Matrigel. However, their propensity for capillary morphogenesis has also been evaluated in fibrin-based scaffolds. Bezenah et al., employed a coated bead approach to assess the ability of iPSC→ECs to form microvascular networks in fibrin 3D culture in the presence of fibroblasts [97]. However, the authors discovered that although iPSC→ECs formed mature capillary-like vessels they also a revealed a five-fold reduction in capillary network creation when compared to HUVECs. The authors concluded that differences in EC phenotypes must be better understood, especially when considering iPSCs for clinical use [97]. Zanotelli et al., encapsulated human iPSCs derived ECs in peptide-functionalized polyethylene glycol (PEG) hydrogels to engineer a microvascular network in vitro using either well-culture or a microfluidic device (Fig. 4b) [98]. The PEG hydrogels functioned as a synthetic ECM and allowed for stable capillary lumens over a two-week period. The in vitro differentiation of iPSCs to ECs has been described using a variety of selective medias [137] and platforms. For example, Kurokawa et al., have shown microvascular development in an organ-on-a-chip platform using iPSC→ECs and polydimethylsiloxane [138].
Adult Stem Cells
For decades angiogenesis through vascular sprouting and intussusception followed by vascular myogenesis was believed to be the sole mechanism for the development of new vascular networks [139]. Since the 1930s, endothelial/capillary-like formations were observed in leukocyte cultures [140]; these and other reports suggested uncharacterized circulating precursor cells with roles in blood vessel formation. In 1997, Asahara et al., described the first putative isolation of bone-marrow derived, circulating endothelial progenitor cells from human peripheral blood using surface marker CD34 and a polyclonal antibody to endothelial cell marker VEGFR-2 [141]. Since then, EPC isolation has been widely reported from human and other animal sources, including bone marrow and adipose tissue (data from our lab; Fig. 4c and Fig. 5). However, despite great interest and ongoing work, significant controversy has surrounded the precise definition and function of EPCs. It is now widely accepted that EPCs represent heterogeneous cells that exhibit differing functions depending on isolation and culture methodology. A comprehensive account of this still unfolding story and specific cell makers is left to dedicated reviews [140, 141, 142,142,143,144,145,146,147,148,149,150,151,152,153,153,155]. The acknowledged CD34+/VEGFR-2+ EPC initially isolated by Asahara incorporated en-masse into sites of neovascularization due to induced ischemia, whereas CD34-/VEGFR-2- cells only rarely incorporated [140]. By 2000, Gehling et al., reported that CD133+ cells from granulocyte colony stimulating factor-mobilized peripheral blood differentiated to exhibit various endothelial markers when cultured with VEGF and stem cell growth factors [156], implicating CD133 as a strong selective marker for EPC identification. Also, in 2000, Peichev et al., reported that a small subset of CD34+/AC133+/VEGFR-2+ cells were found in several different hematopoietic sources. When incubated with VEGF, FGF-2, and collagen, these cells differentiated into CD133-/VEGFR-2+ mature endothelial cells, suggesting that EPCs with angioblast potential may be marked selectively through CD133 [157]. In 2005, Romagnani et al., reported CD34+ cells also expressing either CD133 or CD14 additionally express embryonic stem cell markers Nanog and Oct-4. Accordingly, they proliferated in response to stem cell growth factors, and could differentiate into endothelial cells, adipocytes, osteoblasts, and neural cell lineages [158]. To date, there is no exclusive EPC marker, and it is impossible to differentiate immature EPCs from primitive hematopoietic stem cells due to overlapping surface markers [140]. However, ‘early’ EPCs and ‘late’ EPCs have been distinguished, with the former being spindle-shaped with peak culture growth at 2-3 weeks and secreting many angiogenic and neuroregulatory cytokines prior to dying after approximately four weeks in culture. These ‘early’ EPCs have been characterized as being myeloid angiogenic cells – hematopoietic lineage and the ‘late’ cells being endothelial colony forming cells (ECFC) [155]. ECFCs appear as cobblestone-shaped cells after 2-3 weeks in culture which can be maintained for up to 12 weeks [140]. Clinically, ECFCs are characterized by a high proliferative potential and vasculogenic capacity as was recently documented by Reid et al. in a model of ischemic retinopathy [159]. Despite nomenclature discrepancies, their potential application in the formation of new blood vessels has spawned much enthusiasm among researchers and clinicians. Recently, Liang et al., utilized human bone marrow derived EPCs which expressed CD133, CD34, VEGFR2, VE-cadherin, E-selectin, and vWF to demonstrate enhanced angiogenesis when co-cultured in the presence of mesenchymal stem cells (MSCs). The effects were mediated through PDGF (platelet derived growth factor) and Notch signaling [100]. Liu et al., used cell sheets to co-culture EPCs and MSCs which proved advantageous for integration into an irradiated field [160]. In this study, EPCs emerged as cobblestone colonies in primary culture and expressed CD31, VE-Cadherin, and VEGFR2 [160]. In addition to surface marker expression the source of EPC isolation may affect vasculogenic potential. For example, it has been suggested that adult peripheral blood derived EPCs may have lower vasculogenic potentials when compared to other sources [161]. However, Melero-Martin et al., demonstrated that postnatal EPCs have an inherent vasculogenic ability when co-cultured with mesenchymal progenitor cells [162]. The authors utilized both cord blood derived EPCs and adult peripheral blood EPCs which were purified by CD31 selection and formed EC colonies with a cobblestone appearance. EPCs expressed CD31, CD105, CD44, CD29, and VEGFR2 but failed to express CD90 and CD45 with flow cytometry characterization. In the presence of mesenchymal stem cells (60%), EPCs from either source demonstrated robust vascularization [162]. MSCs are known as being able to differentiate into pericytes through EC influences and paracrine effects [163]. However, the isolation and culture of EPCs from blood is time consuming and inefficient. In 2004, Planat-Benard et al., described using adipose tissue for EPC isolation, with their procedure being the same as for isolation of MSCs from adipose [164]. In 2013, Hager et al., described using magnetic activated cell sorting with CD133, CD34, and CD31 cell markers to isolate EPCs from human lipoaspirate [165]. Zhou et al., showed that adipose derived EPCs (adEPCs) formed capillary-like structures in Matrigel []. Other groups have differentiated ADSCs into EPCs by pretreating them with endothelial media for three days then subjecting them to laminar shear stress [166]. These cells had significantly increased expression of endothelial markers and formed tube-like structures in Matrigel. However, some studies reject this theory suggesting that ADSCs do not differentiate into EPCs, but rather the SVF including EPCs [167]. Amerion et al., showed that rat adEPCs change morphology over time [168], which is consistent with other studies describing early and late EPCs [169]. They showed that cells grew more rapidly after seven days in endothelial induction medium, which led to formation of a cell sheet after three weeks. VEGFR2 expression was significantly increased in the early stage and continued; whereas, TIE-2 (tyrosine kinase with immunoglobulin-like and epidermal growth factor-like domains 2) signaling increased in the third week and other genes had fluctuating expression. Our laboratory has demonstrated that human adipose derived EPCs can organize into tubule formation within 24 hours in 3D collagen culture (Fig. 5) without any pretreatment. ECM production appears to be vital to the structural integrity of engineered tissues including the stabilization of the microvascular network. It has been shown that EPCs demonstrate superior ECM deposition and assembly when compared to mature ECs and should be considered for microvascular engineering [170]. The importance of ECM deposition for microvascular network stabilization can further be witnessed that co-culture with mural cells offers significant advantages.
Human adipose tissue isolated endothelial progenitor cells: EPCs (CD34+/CD31-) cultured on 3D collagen scaffolds in endothelial microvascular media (MV media) demonstrated vasculogenesis. a Live imaging was performed using an Evos FL Auto (ThermoFisher) microscope with arrows showing early tube formation (A1) and excessive growth at 21 hours (A2). b A Cytodex 3 microcarrier bead coated with EPCs for 12 hours and cultured in collagen demonstrating sprouts (arrows) at 72 hours using live imaging and z-stack reconstruction. c EPCs stained with CellTracker dye and coated on Cytodex 3 beads demonstrating network/tube formation (arrows) after six days in 3D collagen culture (Unpublished work from our lab)
Mural and Perivascular Cells
The absence of pericytes is a limiting factor in maintaining engineered microvessels in culture for an extended period. However, pericytes themselves are a rare occurrence and their isolation and characterization is imprecise. First discovered in the late 19th century as contractile cells surrounding the endothelium of small blood vessels, the term “pericyte” was ascribed by Zimmerman in 1923 [103]. Since then their wide-ranging importance has been documented in vascular development, stabilization, maturation, and remodeling [171], along with ECs. Transforming growth factor beta 1 (TGF-β1) has been shown to play a central role in the pericyte-EC interaction, especially in regards to mesenchymal→mural cell differentiation and the suppression of EC proliferation and migration [172]. Additionally, recent studies have suggested pericyte similarities to multipotent stem cells and progenitor cells [173]. Validated pericyte markers include PDGFR-β, NG2 (chondroitin sulfate proteoglycan 4), CD13 (alanyl aminopeptidase), α-SMA (alpha-smooth muscle actin), and desmin. However, these markers are dependent on multiple factors and are dynamic in their expression [103]. Angiopoietin-1 (ANG1) is expressed on pericytes and its interaction with the TIE-2 receptor on ECs provides vessel stabilization and maturation. Therefore, its importance to vascularization of engineered tissues has been probed [174]. Morin et al., used human brain pericytes and HUVECs to fabricate aligned microvessels in a 3D fibrin gel by day three [175]. The authors noted that both pericytes and a defined medium were required to achieve a highly interconnected microvasculature with the presence of pericytes increasing the total vessel length [175]. Chen et al., used pericytes with HUVECs in Matrigel to generate capillary like structures [176]. The authors isolated microvascular pericytes (CD146+/CD34-/45-/56-) from human skeletal muscle. Pericytes were combined with an equal number of HUVECs in either 2D or 3D culture. Co-culture with pericytes significantly improved and hastened microvascular formation in both culture conditions [176]. Cultured pericytes exhibited sustained high inflammatory gene expression, including HIF-1α (hypoxia-inducible factor 1-alpha). HIF-1α is a subunit transcriptional factor that has been demonstrated to play a significant role in angiogenesis. The peri-endothelial location of pericytes is frequently confused with other adjacent mesenchymal cells including vascular smooth muscle cells and fibroblasts. Secondary to the difficulty in pericyte isolation and the importance of supporting cells in the developing microcirculation other perivascular cells have been used for microvascular engineering endeavors.
The utility of fibroblasts in microvascular tissue engineering has been well documented. They are ubiquitous in connective tissue and therefore are located throughout the body. Since they are responsible for the generation of extracellular matrix and collagen, they contribute to the structural support of tissues, including the vascular tree. Additionally, they have been shown to be vital to angiogenesis through the secretion of soluble mediators, such as tissue inhibitor of metalloproteinase-1 (TIMP-1) [177]. However, unlike pericytes, they are relatively easy to isolate and are present in large numbers. This has led to their extensive investigation in tissue engineering endeavors. Chen et al., co-cultured normal human lung fibroblasts (NHLFs) and HUVECs in fibrin gels to generate in vitro prevascularized constructs [178]. Furthermore, a high density of fibroblasts accelerated functional anastomosis following animal implantation by 2-3 days. Costa-Almeida et al., co-cultured human dermal fibroblasts with ECs and showed that they promoted vascularization, which was thought to be due to their higher expression of α-SMA and podoplanin as well as increased synthesis of ECM [179]. Newman et al., also showed that fibroblast-derived ECM components play a critical role in EC lumen formation via expression of five genes: collagen I, procollagen C endopeptidase enhancer I, secreted protein acidic and rich in cysteine, TGF-β-induced protein Ig-h3, and insulin growth factor-binding protein 7 [180]. Other groups have also shown that growth factors and matrix proteins from fibroblasts modulate EC sprouting into capillary networks in vitro [181, 182].
Likewise, MSCs have also been shown to support vascular tube formation. They can serve as a source of vasculogenic growth factors and have the ability to differentiate into mural cells via communication with ECs [183]. HUVECs cultured with BM-MSCs versus fibroblasts showed a higher number of cell junctions and slower vessel formation with a higher number of branches, simulating physiological vessel growth [184]. Pill et al., showed that MSCs from both adipose and bone marrow promotes tubulogenesis in co-culture with ECs, although via distinct mechanisms [185]. Verseijden et al., showed that prevascularized HUVEC/ADSC constructs resulted in significantly higher vessel formation after in vivo implantation in mice [186]. Melero-Martin et al., showed combination of EPCs and MSCs from blood or bone marrow allowed rapid formation of functional anastomoses in vivo, which remained patent at four weeks [163]. Rao et al., found that a high ratio of EC:BM-MSCs (5:1) led to unstable vessel formation compared to lower ratios [187]. Other groups have also shown that both BM-MSCs [188,189,190] and ADSCs [191,192,193] co-cultured with ECs support vascular formation.
Microvascular Fragments
The uncertainty of cellular isolates and their correct ratios for microvascular engineering has led to an interest in the utility of multicellular vessel segments. Hoying et al. reported that microvascular fragments (MF) isolated from adipose tissue undergo expansion and sprouting when placed in a collagen gel [194]. These features have been demonstrated in mouse, rat, and human sources [195]. MF retrieval relies on the isolation of intact short vessel segments that includes arterioles, capillaries, and venules. In addition to luminal ECs, these fragments are rich in smooth muscle cells, progenitors, and perivascular cells. By containing native cell ratios, MFs eliminate the uncertainty of recombining the correct cellular portions (e.g. ECs, MSCs, fibroblasts) in vitro while offering a simpler isolation protocol than that of individual cells. This can be appreciated where the retrieval of cell subpopulations from adipose tissue involves extensive collagen digestion but MF isolation only requires a fraction of time [196]. Although, it has been demonstrated that angiogenic MFs can be isolated from a variety of tissues [197], the ubiquity and accessibility of adipose tissue has made it a preferred choice. Specifically, MFs can be obtained from patients via minimally invasive liposuction techniques that can performed under local anesthesia in a clinic setting. In culture, MFs have been shown to release proangiogenic mediators, such as VEGF [118], potentially obviating the need for exogenous angiogenic supplementaion. Furthermore, they have demonstrated the ability for inosculation and perfusion following animal implantation. Laschke et al. demonstrated that the incorporation of adipose derived MFs into porous scaffolds contributed to enhanced inosculation following implantation (Fig. 4d) [118]. Shepard et al. engineered prevascularized cardiac patches in vitro using microvascular fragments which demonstrated inosculation with the coronary microcirculation in a mouse myocardial infarct model within seven days [198]. It is has also been suggested that MFs demonstrate substantial plasticity with microvessels of arterial identity being able to give rise to both arterial and venous phenotypes [199] despite the luminal dimensions becoming somewhat uniform in culture with an average diameter of ~23 μm [200]. While the maintenance of native cell ratios in a multicellular fragment is advantageous, the large size of MFs may limit their utility in additive manufacturing technologies, such as vascular bioprinting. Furthermore, directed manipulation with miRNAs may prove cumbersome in a multicellular fragment [201]. However, continued investigation of MFs is warranted to determine if their heterogeneous cell populations offer an advantage to the in vitro recombination of ECs and mural cells for microvascular engineering.
Cell Seeding
Cell-based therapies were the earliest approaches in healing damaged tissue in which single cell suspensions were injected into defect areas to help regeneration and organ recovery. However, this approach has limitations such as difficulties in retaining cells at the target site [202]. As microvascular dysfunction is generally not limited to a confined region, as is the case in diabetes [203], direct cellular injections for microvascular regeneration may not prove beneficial. Additionally, engineered tissues need to rapidly integrate upon implantation. Therefore, other approaches have been developed to optimize engraftment upon implantation.
In Vitro Prevascularization
Prevascularization is a concept in which engineered tissue has an established microvasculature prior to implantation facilitating vascular integration and perfusion prior to the onset of hypoxia induced cell damage. Current strategies generally rely on random cell/spheroid seeding, cell sheets, and bioprinting technologies.
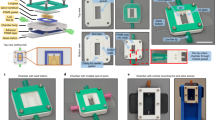
Seeding cells onto scaffolds has been widely used for in vitro prevascularization, using all the cellular sources outlined above. The scaffold chosen must consider material biocompatibility, biodegradability, mechanical properties, and scaffold architecture. Numerous scaffold materials have been utilized in tissue engineering with the general goal of imitating the native ECM [204] required for native cell function. Most of the scaffolds used in microvascular engineering endeavors can be broadly grouped as hydrogels. Hydrogels are a group of natural (e.g. polysaccharide or polypeptide-based) or synthetic (e.g. polyethylene glycol, polyacrylamide) polymeric materials whose hydrophilic structure allows them to hold large amounts of water [205]. Natural hydrogels such as fibrin, collagen, and alginate have all been used as ECM mimics in tissue engineering. Fibrin is formed during wound coagulation and is used extensively in clinical applications for hemostasis. It can either be obtained whole or separately in its fibrinogen and thrombin components which can increase tunability of its final application. While useful in angiogenic assays, its susceptibility to protease mediated degradation mitigates its utility in in vitro prevascularization approaches. Collagen based hydrogels have a deep history in 3D culture applications [206] with Matrigel being extensively used in microvascular engineering as it best resembles the complex ECM found in living tissues. It is unique in that in addition to collagen type IV it contains laminin, entactin, and various other proteoglycans and growth factors [206]. While it robustly supports cell growth and vascular network formation it is derived from mouse sarcoma cells, thereby potentially limiting clinical translation. This has led to a variety of other collagen sources being investigated (e.g. type 1 bovine) [207] that can be fashioned in different concentrations allowing for mechanical stability at the expense of porosity. To further expand the hydrogel-based scaffold platform, sourcing has also transitioned from natural to synthetic sources such as poly ethylene glycol (PEG), dimethacrylate, methacrylated gelatin [208] and poly(lactide-coglycolide) [209]. Scaffolds have been fashioned in various patterns to reproduce microcirculatory architecture [208] and into cylindrical shapes (Fig. 6) [209]. Likewise, scaffolds have also widely been used as a platform for cell seeding and random tubulogenesis. While each scaffold has its own advantages and disadvantages, the materials which best resemble native ECM have fragile mechanical properties which complicate the transfer of in vitro prevascularized constructs into an in vivo model. This further muddles the cell seeding process in addition to the optimal ratio of vascular and mural/stromal cells remaining ill-defined [210]. Furthermore, the ability to precisely control the complex microvascular architecture is not possible yet.
Cylindrical scaffold fabrication approach for microvascular engineering: a Schematic diagram adopted from Tung et al. [209], demonstrating HUVEC culture on a degradable cylindrical PLGA scaffold for microvessel formation. b Cylidrical PLGA scaffolds were made from a PDMS mold that had been generated using soft-lithography. c HUVEC-cultured cylindrical scaffold stained for F-actin (red) and nucleus (blue) using 3D confocal microscopy [209]
Cell sheet engineering is a new scaffold-free method that overcomes the drawbacks of scaffold-based techniques [211]. In this method, cell aggregates can be harvested without proteolytic enzymes, allowing cells to be manipulated without disrupting their native ECM [212, 213]. Intact cell sheets, including the deposited ECM, can be harvested using thermoresponsive hydrogels, such as poly n-isopropyl acrylamide (PNIPAAm) and methylcellulose (MC), simply by changing the temperature. In these systems, cells adhere and proliferate on the substrate at 37°C and when the temperature is decreased to room temperature, confluent cells can be released as an intact sheet. MC and PNIPAAm hydrogels have been utilized in many studies for cell sheet fabrication. Shimizu et al., showed that cell sheets can be stacked to create a thick construct with vascularity [214]. Sekiya et al., showed that layered EC sheets produced lumens and vascular structures [215]. Asakawa also showed that stacked cell sheets of HUVECs and dermal fibroblasts created vascular networks [216]. Another study described vessel formation in a five-layer myoblast sheet construct by stacking HUVECs and myoblast cells [217]. They observed the anastomosis of the endothelial network in the stacked construct to host vessels after transplantation in vivo. These studies clearly indicate the potential for cell sheet engineering techniques in microvascular endeavors. While manipulation of the engineered microvascular network may prove more stable with this approach, it offers limited benefit over traditional scaffold cell seeding with regards to controlling the vascular architecture.
Bioprinting is one of the recently described techniques that allows direct fabrication and preparation of complex 3D vascular networks [218]. The major advantage of this technique is the ability to fabricate a complex tissue construct with fine spatial control over the cell pattern and requisite growth factor deposition [219] with both scaffold-based and scaffold-free techniques. In bioprinting, living cells are delivered in a bioink, which forms the initial ECM following either extrusion-, droplet-, or laser-based bioprinting. Ideal bioinks remain stable during the bioprinting process while exhibiting a viscosity in the range of 10-150 mPa, which eases deposition and prevents nozzle clogging [220]. Natural biopolymers such as gelatin, collagen, agarose, alginate; and synthetic materials such as poly ethylene glycol have been used as bioinks [221]. Bioinks with thermally reversible gelation, such as gelatin-based hydrogels, are preferred due to their ability to demonstrate both solid and semisolid states [222]. Kolesky et al., used a cell laden ink composed of gelatin and fibrinogen to bioprint thick vascularized tissues which could eventually be perfused with growth factors to promote osteogenic differentiation of human MSCs in situ [222]. Byambaa et al., developed a bone-like construct by arranging individual bioprinted rods including VEGF-functionalized gelatin-methylated rods and hMSC laden gels loaded with silicate nanoparticle cylinder rods in the form of a pyramidal construct [223]. Ozbolat and co-workers introduced co-axial bioprinting to directly extrude perfusable vasculatures in the range of 1 mm in external diameter, which was then further advanced by other groups [224,225,226,227]. While patterned vascular formations can be formed, bioprinting still lacks the resolution to print an intact vasculature from the capillary level (~5μm diameter) to one that permits reliable surgical anastomosis (~1mm diameter). Therefore, without the ability for rapid perfusion prevascularized scaffolds still suffer from some degree of ischemia following implantation. To limit this, it may be beneficial to incorporate growth factors into the implanted construct or recipient sites.
Angiogenic factors play critical roles in vascularization after implantation when incorporated into biomaterial scaffolds [2, 123, 228, 229]. Angiogenic growth factors accelerate vascularization by activating and stimulating ECs/ EPCs, which results in migration of these cells toward the factor gradient. These factors not only cause vascular organization and network formation, but they have great impact on vessel maturation by recruiting mural cells and stabilizing the implanted ECs [229]. The main growth factors involved in upregulating angiogenesis and vascular formation include: VEGF, basic fibroblast growth factor and hepatocyte growth factor (HGF). Other cytokines such as platelet-derived growth factor, TGF-β, and angiopoietin also affect angiogenesis indirectly and are involved in the stabilization of newly formed vessels. The major drawback of these factors is that they are not highly stable and have high degradation rates in vivo, which makes delivery challenging. Therefore, spatial and temporal release of cytokines is essential. Immobilizing these factors within the scaffold and tissue engineered construct is a promising approach which can provide fine control over the delivery of angiogenic growth factors [123, 229]. In one study, Poldervaart et al., investigated temporally controlled release of VEGF from gelatin microspheres which resulted in prolonged release of VEGF for three weeks in vitro [230]. In another study, Campagnolo et al., investigated how conjugating polycaprolactone (PCL) constructs with heparin binding peptide increases accumulation of vascular endothelial growth factor [231]. Growth factor incorporation may prove useful in further augmenting the potential of cell stacking and bioprinting technologies for functional microvascular creation.
In Vivo Prevascularization
In vivo prevascularization is an approach where the engineered construct is implanted into well vascularized tissue in order to induce ingrowth of surrounding blood vessels into the scaffold prior to final transfer into the defect site [232]. Inducing vascularization in vivo using arteriovenous loops (AVLs) was first described by Erol in 1980 [233]. In this technique, grafts (e.g. skin) are implanted adjacent to a large caliber vascular conduit (1-3 mm) that has been fashioned into a loop shape. Following a week of implantation, the AV-loop has inosculated the implanted graft through vascular ingrowth. The entire AV-loop/graft can now be transferred into a desired remote site with the AV-loop permitting a direct anastomosis to the final vascular bed. This approach has been used clinically when there is no free-flap option to reconstruct challenging wounds [234]. AVLs have also be used to lengthen the vascular pedicle [235], decrease risk of thrombotic events at the anastomosis [236], and reduce ischemia time [237], which all improve the chance of tissue transfer survival. This has prompted its utility in the vascularization of prevascularized engineered tissue, utilizing either autogenic or allogenic vascular grafts. For this purpose, tissue constructs and arteriovenous loops are placed into a chamber which could be empty or filled with ECM. After vascular formation the construct can be surgically anastomosed at the site of the defect [238]. Arkudas et al., used an AVL model to asses vascular formation of sintered 45S5 Bioglass [239]. They observed a dense network of capillaries three weeks after implantation in the medial thigh of rats. In another study by Beier et al., hydroxyapatite-beta tri-calcium phosphate (HA/β-TCP) constructs were vascularized by implanting ceramic constructs placed in an AVL into the groins of merino sheep after six and 12 weeks [240]. A drawback of this strategy is the number of operations that are needed to complete the process. However, when integrated with cellular based strategies and novel microfabrication techniques, it may demonstrate utility in the rapid perfusion of an engineered microvasculature.
Conclusions
Tremendous advances in stem cell biology, materials science, and additive manufacturing have drastically propelled the field of tissue engineering recently. A major limiting factor towards clinical translation remains vascularization and immediate or near-immediate perfusion. However, endothelial cell-based co-cultures or microvessel fragments have demonstrated significant potential in replicating the vasculogenic process. It is interesting that with both approaches adipose tissue has emerged as a substantial donor depot for cellular based strategies for microvascular engineering. Advances in in vitro prevascularization strategies have led to more rapid perfusion upon implantation. This has led to promising platforms such as vascularized organ-on-a chip with direct surgical anastomosis (Fig. 7) as was recently detailed by Zhang et al. [241]. The authors of this study highlighted the importance of a cross-disciplinary collaboration with input from materials science, cell biology, additive manufacturing, and surgery. This is particularly exciting as it represents a step forward in the clinical translation of engineered tissues. However, it is likely that both the vasculogenic and angiogenic processes of engineered tissue will need to be optimized for large volume tissue transfer or the correction of microvascular dysfunction. In clinical surgery, it is well established that a period of warm ischemia greater than four hours will lead to significant tissue necrosis and poorer patient outcomes. Therefore, we are not only challenged with the task of striving for perfusion within this time frame but in also fabricating a microcirculatory bed that will function appropriately for the engineered tissue or organ.
Direct surgical anastomosis of engineered cardiac tissue: The AngioChip is a citric acid-based scaffold that suppports the assembly of parenchymal cells (e.g. cardiac, hepatic) adjacent to a perfusable, branched 3D microchannel network that can be coated with endothelial cells. Furthermore, the AngioChip can be surgically anastamosed for rapid perfusion. Schematic diagram adopted from Zhang et al. [241] demonstrating surgical anastomosis of the AngioChip cardiac tissue on the rat femoral vessels in the configuration of an artery-to-artery graft (a) and artery-to-vein graft (b) exhibiting a rapidly perfused engineered microcirculation
Adult ECs along with multipotent and pluripotent stem cells have been cultured in various scaffolds and conditions to demonstrate in vitro and in vivo possibilities
Abbreviations
- AdEPC:
-
Adipose derived EPC
- ANG:
-
Angiopoietin
- AVL:
-
Arteriovenous loop
- bFGF:
-
Basic fibroblast growth factor
- BM:
-
Bone marrow
- Dll4:
-
Delta-like 4
- DMVEC:
-
Dermal microvascular endothelial cell
- EB:
-
Embryoid body
- EC:
-
Endothelial cell
- ECFC:
-
Endothelial colony forming cell
- ECM:
-
Extracellular membrane
- eNOS:
-
Endothelial nitric oxide synthase
- EPC:
-
Endothelial progenitor cell
- ESC:
-
Embryonic stem cell
- FGF:
-
Fibroblast growth factor
- FLK-1:
-
Fetal liver kinase-1
- HA:
-
Hydroxyapatite
- HGF:
-
Hepatocyte growth factor
- HIF:
-
Hypoxia-inducible factor
- HUVEC:
-
Human umbilical vein umbilical cell
- iPSC:
-
Induced pluripotent stem cell
- MC:
-
Methylcellulose
- MF:
-
Microvessel fragment
- MMP:
-
Matrix metalloproteinase
- MSC:
-
Mesenchymal stem cell
- NHLF:
-
Normal human lung fibroblast
- PCL:
-
Polycaprolactone
- PDMS:
-
Polydimethylsiloxane
- PECAM:
-
Platelet endothelial cell adhesion molecule
- PEG:
-
Poly ethylene glycol
- PLGA:
-
Poly(lactide-co-glycolide)
- PNIPAAm:
-
Poly n-isopropyl acrylamide
- SMA:
-
Smooth muscle actin
- SVF:
-
Stromal vascular fraction
- TCP:
-
Tri-calcium phosphate
- TGF:
-
Transforming growth factor
- TIMP:
-
Tissue inhibitor of metalloproteinase
- VE:
-
Vascular endothelial
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
- vWF:
-
von Willebrand factor
References
Chim, H., Amer, H., Mardini, S., & Moran, S. L. (2014). Vascularized composite allotransplant in the realm of regenerative plastic surgery. Mayo Clinic Proceedings, 89, 1009–1020.
Rouwkema, J., Rivron, N. C., & van Blitterswijk, C. A. (2008). Vascularization in tissue engineering. Trends in Biotechnology, 26, 434–441.
Shanbhag, S., Pandis, N., Mustafa, K., Nyengaard, J. R., & Stavropoulos, A. (2017). Cell Cotransplantation Strategies for Vascularized Craniofacial Bone Tissue Engineering: A Systematic Review and Meta-Analysis of Preclinical In Vivo Studies. Tissue Engineering Part B: Reviews, 23, 11–117.
Phelps, E. A., & García, A. J. (2010). Engineering more than a cell: vascularization strategies in tissue engineering. Current Opinion in Biotechnology, 21, 704–709.
Lovett, M., Lee, K., Edwards, A., & Kaplan, D. L. (2009). Vascularization strategies for tissue engineering. Tissue engineering Part B, Reviews, 15, 353–370.
Cade, W. T. (2008). Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Physical Therapy, 88, 1322–1335.
Marinescu, M. A., Löffler, A. I., Ouellette, M., Smith, L., Kramer, C. M., & Bourque, J. M. (2015). Coronary microvascular dysfunction, microvascular angina, and treatment strategies. JACC: Cardiovascular Imaging, 8, 210–220.
Weitz, J. I., Byrne, J., Clagett, G. P., et al. (1996). Diagnosis and treatment of chronic arterial insufficiency of the lower extremities: a critical review. Circulation, 94, 3026–3049.
Freisinger, E., Malyar, N. M., Reinecke, H., & Lawall, H. (2017). Impact of diabetes on outcome in critical limb ischemia with tissue loss: a large-scaled routine data analysis. Cardiovascular Diabetology, 16, 41.
Sun, X., Altalhi, W., & Nunes, S. S. (2016). Vascularization strategies of engineered tissues and their application in cardiac regeneration. Advanced Drug Delivery Reviews, 96, 183–194.
Al-Lamki, R. S., Bradley, J. R., & Pober, J. S. (2008). Endothelial cells in allograft rejection. Transplantation, 86, 1340–1348.
Bae, H., Puranik, A. S., Gauvin, R., et al. (2012). Building vascular networks. Science Translational Medicine, 4, 160ps23.
Risau, W., & Lemmon, V. (1988). Changes in the vascular extracellular matrix during embryonic vasculogenesis and angiogenesis. Developmental Biology, 125, 441–450.
Eichmann A, Bouvrée K, Pardanaud L. Vasculogenesis and Angiogenesis in Development. In: Marmé D, Fusenig N, (Ed) Tumor Angiogenesis: Basic Mechanisms and Cancer Therapy. Berlin, Heidelberg: Springer Berlin Heidelberg; 2008:31-45.
Chung, A. S., & Ferrara, N. (2011). Developmental and pathological angiogenesis. Annual Review of Cell and Developmental Biology, 27, 563–584.
Goldie, L. C., Nix, M. K., & Hirschi, K. K. (2008). Embryonic vasculogenesis and hematopoietic specification. Organogenesis, 4, 257–263.
Patel-Hett, S., & D’Amore, P. A. (2011). Signal transduction in vasculogenesis and developmental angiogenesis. The International Journal of Developmental Biology, 55, 353.
Garcia, M. D., & Larina, I. V. (2014). Vascular development and hemodynamic force in the mouse yolk sac. Frontiers in Physiology, 5, 308.
Gerhardt, H., Golding, M., Fruttiger, M., et al. (2003). VEGF guides angiogenic sprouting utilizing endothelial tip cell filopodia. The Journal of Cell Biology, 161, 1163–1177.
Urbich, C., & Dimmeler, S. (2004). Endothelial progenitor cells: characterization and role in vascular biology. Circulation Research, 95, 343–353.
Lee, S., Chen, T. T., Barber, C. L., et al. (2007). Autocrine VEGF signaling is required for vascular homeostasis. Cell, 130, 691–703.
Shibuya, M. (2006). Vascular endothelial growth factor receptor-1 (VEGFR-1/Flt-1): a dual regulator for angiogenesis. Angiogenesis, 9, 225–230.
Zhang, Z., Neiva, K. G., Lingen, M. W., Ellis, L. M., & Nör, J. E. (2010). VEGF-dependent tumor angiogenesis requires inverse and reciprocal regulation of VEGFR1 and VEGFR2. Cell Death and Differentiation, 17, 499.
Carmeliet, P. (2000). Mechanisms of angiogenesis and arteriogenesis. Nature Medicine, 6, 389.
Sato, T. N., Tozawa, Y., Deutsch, U., et al. (1995). Distinct roles of the receptor tyrosine kinases Tie-1 and Tie-2 in blood vessel formation. Nature, 376, 70.
Partanen, J., & Dumont, D. (1999). Functions of Tie1 and Tie2 receptor tyrosine kinases in vascular development. Vascular Growth Factors and Angiogenesis: Springer, 159–172.
Savant, S., La Porta, S., Budnik, A., et al. (2015). The orphan receptor Tie1 controls angiogenesis and vascular remodeling by differentially regulating Tie2 in tip and stalk cells. Cell Reports, 12, 1761–1773.
Lyden, D., Young, A. Z., Zagzag, D., et al. (1999). Id1 and Id3 are required for neurogenesis, angiogenesis and vascularization of tumour xenografts. Nature, 401, 670.
Kroll, J., & Waltenberger, J. (1998). VEGF-A induces expression of eNOS and iNOS in endothelial cells via VEGF receptor-2 (KDR). Biochemical and Biophysical Research Communications, 252, 743–746.
Kim, Y.-M., Namkoong, S., Yun, Y.-G., et al. (2007). Water extract of Korean red ginseng stimulates angiogenesis by activating the PI3K/Akt-dependent ERK1/2 and eNOS pathways in human umbilical vein endothelial cells. Biological and Pharmaceutical Bulletin, 30, 1674–1679.
Chen, J., Somanath, P. R., Razorenova, O., et al. (2005). Akt1 regulates pathological angiogenesis, vascular maturation and permeability in vivo. Nature Medicine, 11, 1188.
Somanath, P. R., Razorenova, O. V., Chen, J., & Byzova, T. V. (2006). Akt1 in endothelial cell and angiogenesis. Cell Cycle, 5, 512–518.
Kim, H.-M., Kang, D.-K., Kim, H. Y., Kang, S. S., & Chang, S.-I. (2007). Angiogenin-induced protein kinase B/Akt activation is necessary for angiogenesis but is independent of nuclear translocation of angiogenin in HUVE cells. Biochemical and Biophysical Research Communications, 352, 509–513.
DeLisser, H. M., Christofidou-Solomidou, M., Strieter, R. M., et al. (1997). Involvement of endothelial PECAM-1/CD31 in angiogenesis. The American Journal of Pathology, 151, 671.
Jakobsson, L., Franco, C. A., Bentley, K., et al. (2010). Endothelial cells dynamically compete for the tip cell position during angiogenic sprouting. Nature Cell Biology, 12, 943.
Birdsey, G. M., Dryden, N. H., Amsellem, V., et al. (2008). Transcription factor Erg regulates angiogenesis and endothelial apoptosis through VE-cadherin. Blood, 111, 3498–3506.
Dejana, E., Orsenigo, F., & Lampugnani, M. G. (2008). The role of adherens junctions and VE-cadherin in the control of vascular permeability. Journal of Cell Science, 121, 2115–2122.
Forghany, Z., Robertson, F., Lundby, A., Olsen, J. V., & Baker, D. A. (2017). Control of endothelial cell tube formation by Notch ligand intracellular domain interactions with activator protein 1 (AP-1). Journal of Biological Chemistry.
Leslie, J. D., Ariza-McNaughton, L., Bermange, A. L., McAdow, R., Johnson, S. L., & Lewis, J. (2007). Endothelial signalling by the Notch ligand Delta-like 4 restricts angiogenesis. Development, 134, 839–844.
Suzuma, K., Naruse, K., Suzuma, I., et al. (2000). Vascular endothelial growth factor induces expression of connective tissue growth factor via KDR, Flt1, and phosphatidylinositol 3-kinase-akt-dependent pathways in retinal vascular cells. Journal of Biological Chemistry, 275, 40725–40731.
Doughervermazen, M., Hulmes, J. D., Bohlen, P., & Terman, B. I. (1994). Biological activity and phosphorylation sites of the bacterially expressed cytosolic domain of the KDR VEGF-receptor. Biochemical and Biophysical Research Communications, 205, 728–738.
Moroianu, J., & Riordan, J. F. (1994). Nuclear translocation of angiogenin in proliferating endothelial cells is essential to its angiogenic activity. Proceedings of the National Academy of Sciences, 91, 1677–1681.
Koblizek, T. I., Weiss, C., Yancopoulos, G. D., Deutsch, U., & Risau, W. (1998). Angiopoietin-1 induces sprouting angiogenesis in vitro. Current Biology, 8, 529–532.
Kishimoto, K., Liu, S., Tsuji, T., Olson, K. A., & Hu, G.-F. (2005). Endogenous angiogenin in endothelial cells is a general requirement for cell proliferation and angiogenesis. Oncogene, 24, 445.
Pavlov, N., Frendo, J.-L., Guibourdenche, J., Degrelle, S. A., Evain-Brion, D., & Badet, J. (2014). Angiogenin expression during early human placental development; association with blood vessel formation. BioMed Research International, 2014.
Shibuya, M. (2011). Vascular Endothelial Growth Factor (VEGF) and Its Receptor (VEGFR) Signaling in Angiogenesis: A Crucial Target for Anti- and Pro-Angiogenic Therapies. Genes & Cancer, 2, 1097–1105.
Pitulescu, M. E., Schmidt, I., Giaimo, B. D., et al. (2017). Dll4 and Notch signalling couples sprouting angiogenesis and artery formation. Nature Cell Biology, 19, 915.
Hellstrom, M., Phng, L. K., Hofmann, J. J., et al. (2007). Dll4 signalling through Notch1 regulates formation of tip cells during angiogenesis. Nature, 445, 776–780.
Eklund, L., Kangas, J., & Saharinen, P. (2017). Angiopoietin-Tie signalling in the cardiovascular and lymphatic systems. Clinical Science (London, England), 131, 87–103.
Jośko, J., & Mazurek, M. (2004). Transcription factors having impact on vascular endothelial growth factor (VEGF) gene expression in angiogenesis. Medical Science Monitor, 10, RA89–RA98.
Craig, M. P., Grajevskaja, V., Liao, H.-K., et al. (2015). Etv2 and Fli1b Function Together as Key Regulators of Vasculogenesis and Angiogenesis. Arteriosclerosis, Thrombosis, and Vascular Biology, 35, 865–876.
Baltrunaite, K., Craig, M. P., Palencia Desai, S., et al. (2017). ETS transcription factors Etv2 and Fli1b are required for tumor angiogenesis. Angiogenesis, 20, 307–323.
Sato, Y., Teruyama, K., Nakano, T., et al. (2006). Role of Transcription Factors in Angiogenesis. Annals of the New York Academy of Sciences, 947, 117–123.
Randi Anna, M., Sperone, A., Dryden Nicola, H., & Birdsey, G. M. (2009). Regulation of angiogenesis by ETS transcription factors. Biochemical Society Transactions, 37, 1248.
Hashiya, N., Jo, N., Aoki, M., et al. (2004). In vivo evidence of angiogenesis induced by transcription factor Ets-1: Ets-1 is located upstream of angiogenesis cascade. Circulation, 109, 3035–3041.
McLaughlin, F., Ludbrook, V. J., Cox, J., von Carlowitz, I., Brown, S., & Randi, A. M. (2001). Combined genomic and antisense analysis reveals that the transcription factor Erg is implicated in endothelial cell differentiation. Blood, 98, 3332–3339.
Rudders, S., Gaspar, J., Madore, R., et al. (2001). ESE-1 is a novel transcriptional mediator of inflammation that interacts with NF-κB to regulate the inducible nitric-oxide synthase gene. Journal of Biological Chemistry, 276, 3302–3309.
Christensen, R. A., Fujikawa, K., Madore, R., Oettgen, P., & Varticovski, L. (2002). NERF2, a member of the Ets family of transcription factors, is increased in response to hypoxia and angiopoietin-1: A potential mechanism for Tie2 regulation during hypoxia. Journal of Cellular Biochemistry, 85, 505–515.
Edel, M. (1999). Analysis of the TEL protein during tumour angiogenesis. Anticancer Research, 19, 2945–2951.
Spyropoulos, D. D., Pharr, P. N., Lavenburg, K. R., et al. (2000). Hemorrhage, Impaired Hematopoiesis, and Lethality in Mouse Embryos Carrying a Targeted Disruption of the Fli1Transcription Factor. Molecular and Cellular Biology, 20, 5643–5652.
Zheng, H., Wasylyk, C., Ayadi, A., et al. (2003). The transcription factor Net regulates the angiogenic switch. Genes & Development, 17, 2283–2297.
Xu, L., & Komatsu, M. (2009). Promoter Cloning and Characterization of the Anti-vascular Proliferation Gene, R-ras ROLE OF ETS-AND SP-BINDING MOTIFS. Journal of Biological Chemistry, 284, 2706–2718.
Dube, A., Thai, S., Gaspar, J., et al. (2001). Elf-1 is a transcriptional regulator of the Tie2 gene during vascular development. Circulation Research, 88, 237–244.
Khachigian, L. M., Resnick, N., Gimbrone, M. A., & Collins, T. (1995). Nuclear factor-kappa B interacts functionally with the platelet-derived growth factor B-chain shear-stress response element in vascular endothelial cells exposed to fluid shear stress. The Journal of Clinical Investigation, 96, 1169–1175.
De Val, S. (2011). Key transcriptional regulators of early vascular development. Arteriosclerosis, Thrombosis, and Vascular Biology, 31, 1469–1475.
Potente, M., Urbich, C., K-i, S., et al. (2005). Involvement of Foxo transcription factors in angiogenesis and postnatal neovascularization. The Journal of Clinical Investigation, 115, 2382–2392.
Alabdi, L., He, M., Yang, Q., Norvil, A. B., & Gowher, H. (2018). The transcription factor Vezf1 represses the expression of the antiangiogenic factor Cited2 in endothelial cells. Journal of Biological Chemistry.
Sacilotto, N., Chouliaras, K. M., Nikitenko, L. L., et al. (2016). MEF2 transcription factors are key regulators of sprouting angiogenesis. Genes & Development, 30, 2297–2309.
Henderson, A. M., Wang, S.-J., Taylor, A. C., Aitkenhead, M., & Hughes, C. C. W. (2001). The Basic Helix-Loop-Helix Transcription Factor HESR1 Regulates Endothelial Cell Tube Formation. Journal of Biological Chemistry, 276, 6169–6176.
Esser, J. S., Charlet, A., Schmidt, M., et al. (2017). The neuronal transcription factor NPAS4 is a strong inducer of sprouting angiogenesis and tip cell formation. Cardiovascular Research, 113, 222–223.
Winnik, S., Klinkert, M., Kurz, H., et al. (2009). HoxB5 induces endothelial sprouting in vitro and modifies intussusceptive angiogenesis in vivo involving angiopoietin-2. Cardiovascular Research, 83, 558–565.
Randi, A. M., Sperone, A., Dryden, N. H., & Birdsey, G. M. (2009). Regulation of angiogenesis by ETS transcription factors. Biochemical Society Transactions, 37, 1248–1253.
Sakai, E., Miura, Y., Suzuki-Kouyama, E., et al. (2017). A mammalian mirtron miR-1224 promotes tube-formation of human primary endothelial cells by targeting anti-angiogenic factor epsin2. Scientific Reports, 7, 5541.
Qian, Q., Wenkui, S., Wen, Z., et al. (2017). The role of microRNA-93 regulating angiopoietin2 in the formation of malignant pleural effusion. Cancer Medicine, 6, 1036–1048.
Yang, Q., Jia, C., Wang, P., et al. (2014). MicroRNA-505 identified from patients with essential hypertension impairs endothelial cell migration and tube formation. International Journal of Cardiology, 177, 925–934.
Wang, P., Luo, Y., Duan, H., et al. (2013). MicroRNA 329 Suppresses Angiogenesis by Targeting CD146. Molecular and Cellular Biology, 33, 3689–3699.
Wang, S., Aurora, A. B., Johnson, B. A., et al. (2008). The Endothelial-Specific MicroRNA miR-126 Governs Vascular Integrity and Angiogenesis. Developmental Cell, 15, 261–271.
Chistiakov, D. A., Orekhov, A. N., & Bobryshev, Y. V. (2016). The role of miR-126 in embryonic angiogenesis, adult vascular homeostasis, and vascular repair and its alterations in atherosclerotic disease. Journal of Molecular and Cellular Cardiology, 97, 47–55.
Chen, Y., & Gorski, D. H. (2008). Regulation of angiogenesis through a microRNA (miR-130a) that down-regulates antiangiogenic homeobox genes GAX and HOXA5. Blood, 111, 1217–1226.
Fasanaro, P., D'Alessandra, Y., Di Stefano, V., et al. (2008). MicroRNA-210 modulates endothelial cell response to hypoxia and inhibits the receptor tyrosine kinase ligand Ephrin-A3. Journal of Biological Chemistry, 283, 15878–15883.
Suárez, Y., Fernández-Hernando, C., Yu, J., et al. (2008). Dicer-dependent endothelial microRNAs are necessary for postnatal angiogenesis. Proceedings of the National Academy of Sciences, 105, 14082–14087.
Li, Y., Song, Y.-H., Li, F., Yang, T., Lu, Y. W., & Geng, Y.-J. (2009). MicroRNA-221 regulates high glucose-induced endothelial dysfunction. Biochemical and Biophysical Research Communications, 381, 81–83.
Suárez, Y., Fernández-Hernando, C., Pober, J. S., & Sessa, W. C. (2007). Dicer Dependent MicroRNAs Regulate Gene Expression and Functions in Human Endothelial Cells. Circulation Research, 100, 1164.
Poliseno, L., Tuccoli, A., Mariani, L., et al. (2006). MicroRNAs modulate the angiogenic properties of HUVECs. Blood, 108, 3068.
Kuehbacher, A., Urbich, C., Zeiher, A. M., & Dimmeler, S. (2007). Role of Dicer and Drosha for endothelial microRNA expression and angiogenesis. Circulation Research, 101, 59–68.
Otsuka, M., Zheng, M., Hayashi, M., et al. (2008). Impaired microRNA processing causes corpus luteum insufficiency and infertility in mice. The Journal of Clinical Investigation, 118, 1944–1954.
Dang, L. T., Lawson, N. D., & Fish, J. E. (2013). MicroRNA control of vascular endothelial growth factor signaling output during vascular development. Arteriosclerosis, Thrombosis, and Vascular Biology, 33, 193–200.
Yang, W. J., Yang, D. D., Na, S., Sandusky, G. E., Zhang, Q., & Zhao, G. (2005). Dicer is required for embryonic angiogenesis during mouse development. The Journal of Biological Chemistry, 280, 9330–9335.
Spinetti, G., Fortunato, O., Caporali, A., et al. (2013). MicroRNA-15a and microRNA-16 impair human circulating proangiogenic cell functions and are increased in the proangiogenic cells and serum of patients with critical limb ischemia. Circulation Research, 112, 335–346.
Gori, M., Trombetta, M., Santini, D., & Rainer, A. (2015). Tissue engineering and microRNAs: future perspectives in regenerative medicine. Expert Opinion on Biological Therapy, 15, 1601–1622.
Haralabopoulos, G. C., Grant, D. S., Kleinman, H. K., & Maragoudakis, M. E. (1997). Thrombin promotes endothelial cell alignment in Matrigel in vitro and angiogenesis in vivo. The American Journal of Physiology, 273, C239–C245.
Rioja, A. Y., Tiruvannamalai Annamalai, R., Paris, S., Putnam, A. J., & Stegemann, J. P. (2016). Endothelial sprouting and network formation in collagen- and fibrin-based modular microbeads. Acta Biomaterialia, 29, 33–41.
Nor, J. E., Peters, M. C., Christensen, J. B., et al. (2001). Engineering and characterization of functional human microvessels in immunodeficient mice. Laboratory Investigation, 81, 453–463.
Levenberg, S., Golub, J. S., Amit, M., Itskovitz-Eldor, J., & Langer, R. (2002). Endothelial cells derived from human embryonic stem cells. Proceedings of the National Academy of Sciences of the United States of America, 99, 4391–4396.
Levenberg, S., Rouwkema, J., Macdonald, M., et al. (2005). Engineering vascularized skeletal muscle tissue. Nature Biotechnology, 23, 879–884.
Ikuno, T., Masumoto, H., Yamamizu, K., et al. (2017). Efficient and robust differentiation of endothelial cells from human induced pluripotent stem cells via lineage control with VEGF and cyclic AMP. PLoS One, 12, e0173271.
Bezenah, J. R., Kong, Y. P., & Putnam, A. J. (2018). Evaluating the potential of endothelial cells derived from human induced pluripotent stem cells to form microvascular networks in 3D cultures. Scientific Reports, 8, 2671.
Zanotelli, M. R., Ardalani, H., Zhang, J., et al. (2016). Stable engineered vascular networks from human induced pluripotent stem cell-derived endothelial cells cultured in synthetic hydrogels. Acta Biomaterialia, 35, 32–41.
Asahara, T., & Kawamoto, A. (2004). Endothelial progenitor cells for postnatal vasculogenesis. American Journal of Physiology. Cell Physiology, 287, C572–C579.
Liang, T. Z., Zhu, L., Gao, W. L., et al. (2017). Coculture of endothelial progenitor cells and mesenchymal stem cells enhanced their proliferation and angiogenesis through PDGF and Notch signaling. FEBS Open Bio, 7, 1722–1736.
Zhou, L., Xia, J., Qiu, X., et al. (2015). In vitro evaluation of endothelial progenitor cells from adipose tissue as potential angiogenic cell sources for bladder angiogenesis. PLoS One, 10, e0117644.
Levy, B., Ambrosio, G., Pries, A., & Struijker-Boudier, H. (2001). Microcirculation in hypertension: a new target for treatment? Circulation, 104, 735–740.
Armulik, A., Genove, G., & Betsholtz, C. (2011). Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Developmental Cell, 21, 193–215.
Wilgus, T. A. (2012). Growth Factor-Extracellular Matrix Interactions Regulate Wound Repair. Adv Wound Care (New Rochelle), 1, 249–254.
Sottile, J. (1654). Regulation of angiogenesis by extracellular matrix. Biochimica et Biophysica Acta, 2004, 13–22.
Neve, A., Cantatore, F. P., Maruotti, N., Corrado, A., & Ribatti, D. (2014). Extracellular matrix modulates angiogenesis in physiological and pathological conditions. BioMed Research International, 2014, 756078.
Ghajar, C. M., George, S. C., & Putnam, A. J. (2008). Matrix metalloproteinase control of capillary morphogenesis. Critical Reviews in Eukaryotic Gene Expression, 18, 251–278.
Grant, D. S., & Kleinman, H. K. (1997). Regulation of capillary formation by laminin and other components of the extracellular matrix. EXS, 79, 317–333.
Shepro D. Microvascular research: biology and pathology: Elsevier; 2005.
Jansson, L. (1994). The regulation of pancreatic islet blood flow. Diabetes/Metabolism Reviews, 10, 407–416.
Stratman, A. N., Pezoa, S. A., Farrelly, O. M., et al. (2017). Interactions between mural cells and endothelial cells stabilize the developing zebrafish dorsal aorta. Development, 144, 115–127.
Costa-Almeida, R., Granja, P. L., Soares, R., & Guerreiro, S. G. (2014). Cellular strategies to promote vascularisation in tissue engineering applications. European Cells & Materials, 28, 51–66 discussion -7.
Cines, D. B., Pollak, E. S., Buck, C. A., et al. (1998). Endothelial cells in physiology and in the pathophysiology of vascular disorders. Blood, 91, 3527–3561.
Hubbell, J. A., Massia, S. P., Desai, N. P., & Drumheller, P. D. (1991). Endothelial cell-selective materials for tissue engineering in the vascular graft via a new receptor. Biotechnology (N Y), 9, 568–572.
Hiob, M. A., She, S., Muiznieks, L. D., & Weiss, A. S. (2017). Biomaterials and Modifications in the Development of Small-Diameter Vascular Grafts. ACS Biomaterials Science & Engineering, 3, 712–723.
Fang, Y., & Eglen, R. M. (2017). Three-Dimensional Cell Cultures in Drug Discovery and Development. SLAS Discov, 22, 456–472.
Nakatsu, M. N., Davis, J., & Hughes, C. C. (2007). Optimized fibrin gel bead assay for the study of angiogenesis. Journal of Visualized Experiments, 186.
Laschke, M. W., Kleer, S., Scheuer, C., et al. (2012). Vascularisation of porous scaffolds is improved by incorporation of adipose tissue-derived microvascular fragments. European Cells & Materials, 24, 266–277.
Baranski, J. D., Chaturvedi, R. R., Stevens, K. R., et al. (2013). Geometric control of vascular networks to enhance engineered tissue integration and function. Proceedings of the National Academy of Sciences of the United States of America, 110, 7586–7591.
Jackson, C. J., & Nguyen, M. (1997). Human microvascular endothelial cells differ from macrovascular endothelial cells in their expression of matrix metalloproteinases. Int J Biochem Cell B, 29, 1167–1177.
Unger, R. E., Sartoris, A., Peters, K., et al. (2007). Tissue-like self-assembly in cocultures of endothelial cells and osteoblasts and the formation of microcapillary-like structures on three-dimensional porous biomaterials. Biomaterials, 28, 3965–3976.
Sieveking, D. P., Buckle, A., Celermajer, D. S., & Ng, M. K. (2008). Strikingly different angiogenic properties of endothelial progenitor cell subpopulations: insights from a novel human angiogenesis assay. Journal of the American College of Cardiology, 51, 660–668.
Novosel, E. C., Kleinhans, C., & Kluger, P. J. (2011). Vascularization is the key challenge in tissue engineering. Advanced Drug Delivery Reviews, 63, 300–311.
Kim, S., & Von Recum, H. (2008). Endothelial stem cells and precursors for tissue engineering: Cell source, differentiation, selection, and application. Tissue Engineering Part B-Reviews, 14, 133–147.
Martin, G. R. (1981). Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells. Proceedings of the National Academy of Sciences, 78, 7634–7638.
Thomson, J. A., Itskovitz-Eldor, J., Shapiro, S. S., et al. (1998). Embryonic stem cell lines derived from human blastocysts. Science, 282, 1145–1147.
Evans, M. J., & Kaufman, M. H. (1981). Establishment in culture of pluripotential cells from mouse embryos. Nature, 292, 154–156.
Donny, H. P., & Sharon, G. (2009). Vascular engineering using human embryonic stem cells. Biotechnology Progress, 25, 2–9.
Young, R. A. (2011). Control of the embryonic stem cell state. Cell, 144, 940–954.
Rodolfa, K. T., & Eggan, K. (2006). A transcriptional logic for nuclear reprogramming. Cell, 126, 652–655.
Takahashi, K., & Yamanaka, S. (2006). Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell, 126, 663–676.
Takahashi, K., Tanabe, K., Ohnuki, M., et al. (2007). Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell, 131, 861–872.
Yu, J., Vodyanik, M. A., Smuga-Otto, K., et al. (2007). Induced pluripotent stem cell lines derived from human somatic cells. Science, 318, 1917–1920.
Shao, L., & Wu, W. S. (2010). Gene-delivery systems for iPS cell generation. Expert Opinion on Biological Therapy, 10, 231–242.
Yoshioka, N., Gros, E., Li, H. R., et al. (2013). Efficient generation of human iPSCs by a synthetic self-replicative RNA. Cell Stem Cell, 13, 246–254.
Zhou, Y. Y., & Zeng, F. (2013). Integration-free methods for generating induced pluripotent stem cells. Genomics, Proteomics & Bioinformatics, 11, 284–287.
Song, H.-H. G., Rumma, R. T., Ozaki, C. K., Edelman, E. R., & Chen, C. S. (2018). Vascular Tissue Engineering: Progress, Challenges, and Clinical Promise. Cell Stem Cell, 22, 340–354.
Kurokawa, Y. K., Yin, R. T., Shang, M. R., Shirure, V. S., Moya, M. L., & George, S. C. (2017). Human Induced Pluripotent Stem Cell-Derived Endothelial Cells for Three-Dimensional Microphysiological Systems. Tissue Engineering Part C: Methods, 23, 474–484.
Khakoo, A. Y., & Finkel, T. (2005). Endothelial progenitor cells. Annual Review of Medicine, 56, 79–101.
Ribatti, D. (2007). The discovery of endothelial progenitor cells. An historical review. Leukemia Research, 31, 439–444.
Asahara, T., Murohara, T., Sullivan, A., et al. (1997). Isolation of putative progenitor endothelial cells for angiogenesis. Science, 275, 964–967.
Pearson, J. D. (2009). Endothelial progenitor cells - hype or hope? Journal of Thrombosis and Haemostasis, 7, 255–262.
Pearson, J. D. (2010). Endothelial progenitor cells--an evolving story. Microvascular Research, 79, 162–168.
Asahara, T., Kawamoto, A., & Masuda, H. (2011). Concise review: Circulating endothelial progenitor cells for vascular medicine. Stem Cells, 29, 1650–1655.
Long, D. A., Norman, J. T., & Fine, L. G. (2012). Restoring the renal microvasculature to treat chronic kidney disease. Nature Reviews. Nephrology, 8, 244–250.
Weiss, D. J. (2014). Concise review: current status of stem cells and regenerative medicine in lung biology and diseases. Stem Cells, 32, 16–25.
Menegazzo, L., Albiero, M., Avogaro, A., & Fadini, G. P. (2012). Endothelial progenitor cells in diabetes mellitus. Biofactors, 38, 194–202.
Wu, X., Rabkin-Aikawa, E., Guleserian, K. J., et al. (2004). Tissue-engineered microvessels on three-dimensional biodegradable scaffolds using human endothelial progenitor cells. American Journal of Physiology. Heart and Circulatory Physiology, 287, H480–H487.
Young, P. P., Vaughan, D. E., & Hatzopoulos, A. K. (2007). Biologic properties of endothelial progenitor cells and their potential for cell therapy. Progress in Cardiovascular Diseases, 49, 421–429.
Critser, P. J., Voytik-Harbin, S. L., & Yoder, M. C. (2011). Isolating and defining cells to engineer human blood vessels. Cell Proliferation, 44(Suppl 1), 15–21.
Yoder, M. C. (2012). Human endothelial progenitor cells. Cold Spring Harbor Perspectives in Medicine, 2, a006692.
Peters, E. B., Christoforou, N., Leong, K. W., Truskey, G. A., & West, J. L. (2016). Poly(ethylene glycol) Hydrogel Scaffolds Containing Cell-Adhesive and Protease-Sensitive Peptides Support Microvessel Formation by Endothelial Progenitor Cells. Cellular and Molecular Bioengineering, 9, 38–54.
Chong, M. S., Ng, W. K., & Chan, J. K. (2016). Concise Review: Endothelial Progenitor Cells in Regenerative Medicine: Applications and Challenges. Stem Cells Translational Medicine, 5, 530–538.
Peters, E. B. (2017). Endothelial Progenitor Cells for the Vascularization of Engineered Tissues. Tissue Engineering. Part B, Reviews.
Medina, R. J., Barber, C. L., Sabatier, F., et al. (2017). Endothelial Progenitors: A Consensus Statement on Nomenclature. Stem Cells Translational Medicine, 6, 1316–1320.
Gehling, U. M., Ergun, S., Schumacher, U., et al. (2000). In vitro differentiation of endothelial cells from AC133-positive progenitor cells. Blood, 95, 3106–3112.
Peichev, M., Naiyer, A. J., Pereira, D., et al. (2000). Expression of VEGFR-2 and AC133 by circulating human CD34(+) cells identifies a population of functional endothelial precursors. Blood, 95, 952–958.
Romagnani, P., Annunziato, F., Liotta, F., et al. (2005). CD14+CD34low cells with stem cell phenotypic and functional features are the major source of circulating endothelial progenitors. Circulation Research, 97, 314–322.
Reid, E., Guduric-Fuchs, J., O'Neill, C. L., et al. (2018). Preclinical Evaluation and Optimization of a Cell Therapy Using Human Cord Blood-Derived Endothelial Colony-Forming Cells for Ischemic Retinopathies. Stem Cells Translational Medicine, 7, 59–67.
Liu, H., Zhou, W., Ren, N., et al. (2017). Cell Sheets of Co-cultured Endothelial Progenitor Cells and Mesenchymal Stromal Cells Promote Osseointegration in Irradiated Rat Bone. Science Reporter, 7, 3038.
Au, P., Daheron, L. M., Duda, D. G., et al. (2008). Differential in vivo potential of endothelial progenitor cells from human umbilical cord blood and adult peripheral blood to form functional long-lasting vessels. Blood, 111, 1302–1305.
Melero-Martin, J. M., De Obaldia, M. E., Kang, S. Y., et al. (2008). Engineering robust and functional vascular networks in vivo with human adult and cord blood-derived progenitor cells. Circulation Research, 103, 194–202.
Xu, J., Gong, T., Heng, B. C., & Zhang, C. F. (2017). A systematic review: differentiation of stem cells into functional pericytes. FASEB Journal, 31, 1775–1786.
Planat-Benard, V., Silvestre, J.-S., Cousin, B., et al. (2004). Plasticity of human adipose lineage cells toward endothelial cells: physiological and therapeutic perspectives. Circulation, 109, 656–663.
Hager, G., Holnthoner, W., Wolbank, S., et al. (2013). Three specific antigens to isolate endothelial progenitor cells from human liposuction material. Cytotherapy, 15, 1426–1435.
Hsueh, Y.-Y., Chang, Y.-J., Huang, C.-W., et al. (2015). Synergy of endothelial and neural progenitor cells from adipose-derived stem cells to preserve neurovascular structures in rat hypoxic-ischemic brain injury. Scientific Reports, 5, 14985.
Kondo, K., Shintani, S., Shibata, R., et al. (2009). Implantation of adipose-derived regenerative cells enhances ischemia-induced angiogenesis. Arteriosclerosis, Thrombosis, and Vascular Biology, 29, 61–66.
Amerion, M., Valojerdi, M. R., Abroun, S., & Totonchi, M. (2017). Long term culture and differentiation of endothelial progenitor like cells from rat adipose derived stem cells. Cytotechnology, 1–17.
Hur, J., Yoon, C.-H., Kim, H.-S., et al. (2004). Characterization of two types of endothelial progenitor cells and their different contributions to neovasculogenesis. Arteriosclerosis, Thrombosis, and Vascular Biology, 24, 288–293.
Kusuma, S., Zhao, S., & Gerecht, S. (2012). The extracellular matrix is a novel attribute of endothelial progenitors and of hypoxic mature endothelial cells. The FASEB Journal, 26, 4925–4936.
Gokcinar-Yagci, B., Uckan-Cetinkaya, D., & Celebi-Saltik, B. (2015). Pericytes: Properties, Functions and Applications in Tissue Engineering. Stem Cell Reviews, 11, 549–559.
Walshe, T. E., Saint-Geniez, M., Maharaj, A. S., Sekiyama, E., Maldonado, A. E., & D'Amore, P. A. (2009). TGF-beta is required for vascular barrier function, endothelial survival and homeostasis of the adult microvasculature. PLoS One, 4, e5149.
Crisan, M., Yap, S., Casteilla, L., et al. (2008). A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell, 3, 301–313.
Mravic, M., Asatrian, G., Soo, C., et al. (2014). From pericytes to perivascular tumours: correlation between pathology, stem cell biology, and tissue engineering. International Orthopaedics, 38, 1819–1824.
Morin, K. T., Smith, A. O., Davis, G. E., & Tranquillo, R. T. (2013). Aligned human microvessels formed in 3D fibrin gel by constraint of gel contraction. Microvascular Research, 90, 12–22.
Chen, C. W., Okada, M., Proto, J. D., et al. (2013). Human pericytes for ischemic heart repair. Stem Cells, 31, 305–316.
Liu, H., Chen, B., & Lilly, B. (2008). Fibroblasts potentiate blood vessel formation partially through secreted factor TIMP-1. Angiogenesis, 11, 223–234.
Chen, X., Aledia, A. S., Popson, S. A., Him, L., Hughes, C. C., & George, S. C. (2010). Rapid anastomosis of endothelial progenitor cell-derived vessels with host vasculature is promoted by a high density of cotransplanted fibroblasts. Tissue Engineering. Part A, 16, 585–594.
Costa-Almeida, R., Gomez-Lazaro, M., Ramalho, C., Granja, P. L., Soares, R., & Guerreiro, S. G. (2014). Fibroblast-endothelial partners for vascularization strategies in tissue engineering. Tissue Engineering Part A, 21, 1055–1065.
Newman, A. C., Nakatsu, M. N., Chou, W., Gershon, P. D., & Hughes, C. C. (2011). The requirement for fibroblasts in angiogenesis: fibroblast-derived matrix proteins are essential for endothelial cell lumen formation. Molecular Biology of the Cell, 22, 3791–3800.
Berthod, F., Germain, L., Tremblay, N., & Auger, F. A. (2006). Extracellular matrix deposition by fibroblasts is necessary to promote capillary-like tube formation in vitro. Journal of Cellular Physiology, 207, 491–498.
Kunz-Schughart, L. A., Schroeder, J. A., Wondrak, M., et al. (2006). Potential of fibroblasts to regulate the formation of three-dimensional vessel-like structures from endothelial cells in vitro. American Journal of Physiology-Cell Physiology, 290, C1385–C1C98.
Hirschi, K. K., Burt, J. M., Hirschi, K. D., & Dai, C. (2003). Gap junction communication mediates transforming growth factor-β activation and endothelial-induced mural cell differentiation. Circulation Research, 93, 429–437.
Grainger, S. J., & Putnam, A. J. (2011). Assessing the permeability of engineered capillary networks in a 3D culture. PLoS One, 6, e22086.
Pill, K., Hofmann, S., Redl, H., & Holnthoner, W. (2015). Vascularization mediated by mesenchymal stem cells from bone marrow and adipose tissue: a comparison. Cell Regeneration, 4, 8.
Verseijden, F., Sluijs, S. J. P.-V., Farrell, E., et al. (2010). Prevascular structures promote vascularization in engineered human adipose tissue constructs upon implantation. Cell Transplantation, 19, 1007–1020.
Rao, R. R., Peterson, A. W., Ceccarelli, J., Putnam, A. J., & Stegemann, J. P. (2012). Matrix composition regulates three-dimensional network formation by endothelial cells and mesenchymal stem cells in collagen/fibrin materials. Angiogenesis, 15, 253–264.
Duttenhoefer, F., Lara de Freitas, R., Meury, T., et al. (2013). 3D scaffolds co-seeded with human endothelial progenitor and mesenchymal stem cells: evidence of prevascularisation within 7 days. European Cells & Materials ECM, 26, 64–65.
Ghajar, C. M., Kachgal, S., Kniazeva, E., et al. (2010). Mesenchymal cells stimulate capillary morphogenesis via distinct proteolytic mechanisms. Experimental Cell Research, 316, 813–825.
Kachgal, S., Carrion, B., Janson, I. A., & Putnam, A. J. (2012). Bone marrow stromal cells stimulate an angiogenic program that requires endothelial MT1-MMP. Journal of Cellular Physiology, 227, 3546–3555.
Rohringer, S., Hofbauer, P., Schneider, K. H., et al. (2014). Mechanisms of vasculogenesis in 3D fibrin matrices mediated by the interaction of adipose-derived stem cells and endothelial cells. Angiogenesis, 17, 921–933.
Holnthoner, W., Hohenegger, K., Husa, A. M., et al. (2015). Adipose-derived stem cells induce vascular tube formation of outgrowth endothelial cells in a fibrin matrix. Journal of Tissue Engineering and Regenerative Medicine, 9, 127–136.
Merfeld-Clauss, S., Gollahalli, N., March, K. L., & Traktuev, D. O. (2010). Adipose tissue progenitor cells directly interact with endothelial cells to induce vascular network formation. Tissue Engineering Part A, 16, 2953–2966.
Hoying, J. B., Boswell, C. A., & Williams, S. K. (1996). Angiogenic potential of microvessel fragments established in three-dimensional collagen gels. In Vitro Cellular & Developmental Biology. Animal, 32, 409–419.
Sun, X., Altalhi, W., & Nunes, S. S. (2016). Vascularization strategies of engineered tissues and their application in cardiac regeneration. Advanced Drug Delivery Reviews, 96, 183–194.
Frueh, F. S., & Spater, T. (2017). Scheuer C. Laschke MW. Isolation of Murine Adipose Tissue-derived Microvascular Fragments as Vascularization Units for Tissue Engineering. J Vis Exp: Menger MD.
Nunes, S. S., Krishnan, L., Gerard, C. S., et al. (2010). Angiogenic potential of microvessel fragments is independent of the tissue of origin and can be influenced by the cellular composition of the implants. Microcirculation, 17, 557–567.
Shepherd, B. R., Hoying, J. B., & Williams, S. K. (2007). Microvascular transplantation after acute myocardial infarction. Tissue Engineering, 13, 2871–2879.
Nunes, S. S., Rekapally, H., Chang, C. C., & Hoying, J. B. (2011). Vessel arterial-venous plasticity in adult neovascularization. PLoS One, 6, e27332.
Chang, C. C., & Hoying, J. B. (2006). Directed three-dimensional growth of microvascular cells and isolated microvessel fragments. Cell Transplantation, 15, 533–540.
Fish JE, Srivastava D. MicroRNAs: opening a new vein in angiogenesis research. Sci Signal 2009;2:pe1.
Matsuda, N., Shimizu, T., Yamato, M., & Okano, T. (2007). Tissue Engineering Based on Cell Sheet Technology. Advanced Materials, 19, 3089–3099.
Chao, C. Y., & Cheing, G. L. (2009). Microvascular dysfunction in diabetic foot disease and ulceration. Diabetes/Metabolism Research and Reviews, 25, 604–614.
Chan, B. P., & Leong, K. W. (2008). Scaffolding in tissue engineering: general approaches and tissue-specific considerations. European Spine Journal, 17(Suppl 4), 467–479.
Ahmed, E. M. (2015). Hydrogel: Preparation, characterization, and applications: A review. Journal of Advanced Research, 6, 105–121.
Caliari, S. R., & Burdick, J. A. (2016). A practical guide to hydrogels for cell culture. Nature Methods, 13, 405–414.
Chan, E. C., Kuo, S. M., Kong, A. M., et al. (2016). Three Dimensional Collagen Scaffold Promotes Intrinsic Vascularisation for Tissue Engineering Applications. PLoS One, 11, e0149799.
Rayner, S. G., & Zheng, Y. (2016). Engineered Microvessels for the Study of Human Disease. Journal of Biomechanical Engineering, 138.
Tung, Y. T., Chang, C. C., Ju, J. C., & Wang, G. J. (2017). Fabrication of a reticular poly(lactide-co-glycolide) cylindrical scaffold for the in vitro development of microvascular networks. Science and Technology of Advanced Materials, 18, 163–171.
Koike, N., Fukumura, D., Gralla, O., Au, P., Schechner, J. S., & Jain, R. K. (2004). Tissue engineering: creation of long-lasting blood vessels. Nature, 428, 138–139.
Ma, D., Ren, L., Liu, Y., et al. (2010). Engineering scaffold-free bone tissue using bone marrow stromal cell sheets. Journal of Orthopaedic Research : Official Publication of the Orthopaedic Research Society, 28, 697–n/a.
Akahane, M., Shigematsu, H., Tadokoro, M., et al. (2010). Scaffold-free cell sheet injection results in bone formation. Journal of Tissue Engineering and Regenerative Medicine, 4, 404–411.
Elloumi-Hannachi, I., Yamato, M., & Okano, T. (2010). Cell sheet engineering: a unique nanotechnology for scaffold-free tissue reconstruction with clinical applications in regenerative medicine. Journal of Internal Medicine, 267, 54.
Shimizu, T., Sekine, H., Yang, J., et al. (2006). Polysurgery of cell sheet grafts overcomes diffusion limits to produce thick, vascularized myocardial tissues. The FASEB Journal, 20, 708–710.
Sekiya, S., Shimizu, T., & Okano, T. (2013). Vascularization in 3D tissue using cell sheet technology. Regenerative Medicine, 8, 371–377.
Asakawa, N., Shimizu, T., Tsuda, Y., et al. (2010). Pre-vascularization of in vitro three-dimensional tissues created by cell sheet engineering. Biomaterials, 31, 3903–3909.
Sasagawa, T., Shimizu, T., Sekiya, S., et al. (2010). Design of prevascularized three-dimensional cell-dense tissues using a cell sheet stacking manipulation technology. Biomaterials, 31, 1646–1654.
Ravnic, D. J., Leberfinger, A. N., Koduru, S. V., et al. (2017). Transplantation of Bioprinted Tissues and Organs: Technical and Clinical Challenges and Future Perspectives. Annals of Surgery, 266, 48–58.
Cui, X., & Boland, T. (2009). Human microvasculature fabrication using thermal inkjet printing technology. Biomaterials, 30, 6221–6227.
Datta, P., Ayan, B., & Ozbolat, I. T. (2017). Bioprinting for vascular and vascularized tissue biofabrication. Acta Biomaterialia, 51, 1–20.
Zhang, Y. S., Yue, K., Aleman, J., et al. (2017). 3D Bioprinting for Tissue and Organ Fabrication. Annals of Biomedical Engineering, 45, 148–163.
Kolesky, D. B., Homan, K. A., Skylar-Scott, M. A., & Lewis, J. A. (2016). Three-dimensional bioprinting of thick vascularized tissues. Proceedings of the National Academy of Sciences, 113, 3179–3184.
Byambaa, B., Annabi, N., Yue, K., et al. (2017). Bioprinted Osteogenic and Vasculogenic Patterns for Engineering 3D Bone Tissue. Advanced Healthcare Materials, 6, n/a–n/a.
Yahui, Z., Yin, Y., Howard, C., & Ibrahim TO. (2013). Characterization of printable cellular micro-fluidic channels for tissue engineering. Biofabrication, 5, 025004.
Zhang, Y., Yu, Y., Akkouch, A., Dababneh, A., Dolati, F., & Ozbolat, I. T. (2015). In vitro study of directly bioprinted perfusable vasculature conduits. Biomaterials Science, 3, 134–143.
Yu, Y., Zhang, Y., Martin, J. A., & Ozbolat, I. T. (2013). Evaluation of Cell Viability and Functionality in Vessel-like Bioprintable Cell-Laden Tubular Channels. Journal of Biomechanical Engineering, 135, 091011–091019.
Yu, Y., Zhang, Y., & Ozbolat, I. T. (2014). A hybrid bioprinting approach for scale-up tissue fabrication. Journal of Manufacturing Science and Engineering, 136, 061013.
Mishra, R., Roux, B. M., Posukonis, M., et al. (2015). Effect of prevascularization on in vivo vascularization of poly(propylene fumarate)/fibrin scaffolds. Biomaterials, 77, 255–266.
Rouwkema, J., & Khademhosseini, A. (2016). Vascularization and Angiogenesis in Tissue Engineering: Beyond Creating Static Networks. Trends in Biotechnology, 34, 733–745.
Poldervaart, M. T., Gremmels, H., van Deventer, K., et al. (2014). Prolonged presence of VEGF promotes vascularization in 3D bioprinted scaffolds with defined architecture. Journal of Controlled Release, 184, 58–66.
Campagnolo, P., Gormley, A. J., Chow, L. W., et al. (2016). Pericyte Seeded Dual Peptide Scaffold with Improved Endothelialization for Vascular Graft Tissue Engineering. Advanced Healthcare Materials, 5, 3046–3055.
Koepple, C., Kneser, U., & Schmidt, V. J. (2017). Microsurgical Approaches for In Vivo Prevascularization. In W. Holnthoner, A. Banfi, J. Kirkpatrick, & H. Redl (Eds.), Vascularization for Tissue Engineering and Regenerative Medicine (pp. 1–18). Cham: Springer International Publishing.
Erol, O. O., & Sira, M. (1980). New capillary bed formation with a surgically constructed arteriovenous fistula. Plastic and Reconstructive Surgery, 66, 109–115.
Mambally, S. R. T., & Santha, K. K. (2015). Utility of arteriovenous loops before free tissue transfer for post-traumatic leg defects. Indian Journal of Plastic Surgery: Official Publication of the Association of Plastic Surgeons of India, 48, 38.
Taub, P. J., Chun, J. K., Zhang, W. X., Pham, N. D., Weinberg, H., & Silver, L. (1999). Staging arteriovenous fistula loops for lengthening of free-flap pedicles. Journal of Reconstructive Microsurgery, 15, 123–125.
Lin, C.-H., Mardini, S., Lin, Y.-T., Yeh, J.-T., Wei, F.-C., & Chen, H.-C. (2004). Sixty-five clinical cases of free tissue transfer using long arteriovenous fistulas or vein grafts. Journal of Trauma and Acute Care Surgery, 56, 1107–1117.
Atiyeh, B. S., Sfeir, R. E., Hussein, M. M., & Husami, T. (1995). Preliminary arteriovenous fistula for free-flap reconstruction in the diabetic foot. Plastic and Reconstructive Surgery, 95, 1062–1069.
Arkudas, A., Tjiawi, J., Bleiziffer, O., et al. (2007). Fibrin gel-immobilized VEGF and bFGF efficiently stimulate angiogenesis in the AV loop model. Molecular Medicine, 13, 480–487.
Arkudas, A., Balzer, A., Buehrer, G., et al. (2013). Evaluation of Angiogenesis of Bioactive Glass in the Arteriovenous Loop Model. Tissue Engineering Part C: Methods, 19, 479–486.
Beier, J. P., Horch, R. E., Hess, A., et al. (2010). Axial vascularization of a large volume calcium phosphate ceramic bone substitute in the sheep AV loop model. Journal of Tissue Engineering and Regenerative Medicine, 4, 216–223.
Zhang, B., Montgomery, M., Chamberlain, M. D., et al. (2016). Biodegradable scaffold with built-in vasculature for organ-on-a-chip engineering and direct surgical anastomosis. Nature Materials, 15, 669–678.
Acknowledgements
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under BIRCWH award # K12HD055882 “Career Development Program in Women’s Health Research at Penn State”, the American Association of Plastic Surgeons Research Scholar Award, and a Penn State Junior Faculty Research Scholar Award (PA Tobacco Settlement Fund).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interests
Authors declare no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koduru, S.V., Leberfinger, A.N., Pasic, D. et al. Cellular Based Strategies for Microvascular Engineering. Stem Cell Rev and Rep 15, 218–240 (2019). https://doi.org/10.1007/s12015-019-09877-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-019-09877-4