Abstract
Excessive exposure of iodine over a time is well known to cause thyroid dysfunction, which may be followed by different effects on body organs. The present study aimed to illustrate the impacts of exposure of rats to excess iodine (above the tolerable range) and the reversibility of any negative impacts on hormonal profile related to thyroid besides cortisol and the hematological and biochemical parameters along with the histopathological alterations in the thyroid gland, liver, kidneys, and heart. Seventy-five rats were divided equally into three groups: Group 1 was control animals. Groups 2 and 3 received sodium iodide (NaI) orally at a dose of (35 and 70 mg/kg BW), which corresponded to (500 and 1000) times excess iodine from the physiological dose, respectively for 30 days, then the NaI administration stopped in the treated groups for 15 consecutive days. Blood and tissue samples were collected twice for various experimental tests after 30 and 15 days of exposure to excess iodine and stopping the exposure, respectively. Overall results revealed that excess iodine in both tested groups developed a hyperthyroid condition, hypercortisolism, relative polycythemia, neutropenia, elevation in serum liver and cardiac enzymes activities, hyperprotenemia, hyperglobulinemia, elevation in serum urea, and cardiac troponin I concentrations (p < 0.05). It was concluded that the excess iodine caused hyperthyroidism, which was associated with significant changes in erythrogram and leukogram and alterations in hepatic, renal, and cardiac functions in an iodine dose-dependent damage relationship and the most of negative impacts continued after stopping the administration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
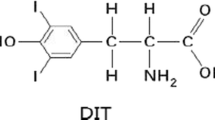
Iodine (I) is one of the essential trace elements for animals and humans, which is mainly found in ocean water in the form of highly water-soluble iodide ion (I−), where the oceans are the main repositories of iodine in the world. It is found in nature in different forms represent in inorganic potassium and sodium salts (iodides and iodates), inorganic diatomic iodine (molecular iodine), and organic monoatomic iodine. It is considered a main element for the production of thyroid hormones [1, 2]. Simply, the thyroid gland effectively takes up the iodine then starts the organification process for formation of the iodized compounds, which is utilized for thyroid hormones synthesis. These important hormones act to control a number of metabolic processes as well as induce the typical development of numerous organs and enhance the normal growth of the body. The relation between the level of iodine intake and the range of thyroid disease occurrence appears in the form of ‘U’ shaped curve, signifying that there is an increasing risk with both low and high iodine intake [3].
Since the implementation of the global strategy to the salt iodization policy over the last several decades, the iodine deficiency problem has remarkably improved worldwide. On the other hand, excess iodine exposure problems due to extensive environmental exposure and the poor monitoring of exposure levels, remains a concern [4, 5]. Excessive exposure of iodine for humans and animals has been linked to several sources. Dietary sources that are naturally rich in iodine in some world regions are the main cause of health problems related to iodine excess in some countries [6].The use of iodine-containing water-purification tablets is considered another source of excess exposure to iodine [7, 8]. Also, the high iodine content in animal feed (including grass) and/or the use of iodophor cleaners for milk cans lets dairy products become a potential source of health problems related to excess iodine in some countries where dairy products represent a main part of the human diet [9]. Another common source of exposure to excess iodine in the medical field is iodinated contrast agents used in diagnostic radiology, where a single dose of iodinated contrast usually contains hundreds of thousands of times the recommended daily dose of iodine, as well as taking supplements, which contain iodine without monitoring, and the use of antiseptics containing iodine [6]. On the other hand, the exposure to excess iodine in livestock may be due to the prolonged consumption of a feed containing several components supplemented with iodine compounds and the improper dealing with mineral feed admixtures for long time. Also, the prolonged use of iodine compounds for prevention and the treatment of different disease such as infectious podo-dermatitis, mastitis, actinomycosis, infertility cases, and complex of respiratory diseases may lead to exposure of animals to excess iodine [10]. In general, the slight or even moderate over exposure to most of the minerals relative to the essential body requirement does not cause deleterious effects on animal and human health, but excessive exposure for long durations can start to induce bad impacts on the health status [11, 12]. According to the literature, the exposure to iodine that are far in excess or above the physiological needs, but below the tolerable doses may produce deleterious effects, particularly on the thyroid gland, and thyroid hormones production and secretion. It was evidenced that the excess iodine intake involved risks manifesting as hypothyroidism, hyperthyroidism, development of goiter, cancer, and Jod-Basedow syndrome, a cause of thyrotoxicosis which is typically seen after exposure to exogenous iodine load [13,14,15,16]. This in turn can induce various impacts on different body organ systems, depending on the thyroid dysfunction, especially when the thyroid hormones have effects on virtually every organ in the body system [17]. Additionally, the extent and duration of exposure of excess iodine plays an important role in the severity of negative impacts.
Therefore, this study was carried out to investigate the impacts of exposure of experimental rats to excess iodine (above the tolerable range) on hormonal profile related to thyroid as well as erythrogram, leukogram, besides the various biochemical parameters related to different vital organs represented in the liver, kidneys, and heart and the possible histopathological alterations in the tested organs. Also, the reversibility of any negative impacts on body systems after stopping the exposure to excess iodine was investigated.
Material and Methods
Experimental Animals Maintenance
The present study was done on seventy-five healthy male Wistar albino rats (Rattus norvegicus) (2 months old and weighing 150 g ± 15) obtained from the laboratory animal house, Faculty of Veterinary Medicine, Zagazig University, Egypt, which were adapted for 1 week before starting the experiment. All the experimental rats were kept in standard cages and maintained on the standard feed formulated according to NRC [18] and details of which are given in (Table 1) and water ad libitum. NaI at the dose of 0.07 mg/kg BW was provided with the standard feed [19]. Standard laboratory conditions were provided for animals during the experiment (24 ± 2 C, relative humidity 40–60%, 12-h dark and light photoperiod). Rats were weighed at the beginning of the experiment and every week until the end of the experiment to adjust the dose of tested agent. Experimental animals were observed daily to monitor the general health status. The study was approved by Zagazig University Institutional Animal Care and Use Committee “ZU-IACUC”, Egypt (Approval no: ZU-IACUC/2/F/114/2019).
Tested Agent
Excess iodine was administered in this experiment in the form of sodium iodide (NaI). It was analytic reagent with 99% purity and procured from Techno pharmchem, Bahadurgarh, India (CAS No. 7681-82-5). It was in the form of white crystalline powder and was stored in a suitable condition.
Experimental Pattern
A total of 75 rats were randomly divided into three groups, each group included 25 rats. Group 1 kept as a normal control. Group 2 (500 EI) was administered NaI at a dose of 35 mg/kg BW dissolved in distilled water, which corresponded to 500 times excess iodine (EI) from the physiological daily dose. Group 3 (1000 EI) was administered NaI at a dose of 70 mg/kg BW daily dissolved in distilled water, which corresponded to 1000 times excess iodine from the physiological daily dose. The doses were given daily for 30 days continuously via oral gavage needle, then stopped in the treated groups for 15 consecutive days. The physiological daily dose of iodine was referred to the published literature [19]. Bearing in mind that, median lethal dose (LD50) of NaI in rats (oral treatment) is 4340 mg/kg [20].The used doses in this study are above the iodine tolerable range for rats according to Chakraborty et al. [21].
Blood and Organs Collection
Sampling occurred twice during the course of the experiment, after 30 days from starting the administration of NaI and after 15 days of stopping administration of NaI from the experimental groups. Blood samples were collected by puncturing retro-orbital venous sinus from anesthetized rats with sodium pentobarbital after overnight fasting period. The first portion (1 ml) of blood samples was collected into clean Wasserman tubes containing dipotassium salt of ethylenediaminetetraacetic acid (EDTA) for doing the different hematological tests. The second portion (1.5 ml) of blood samples was collected into ordinary tubes for centrifugation and isolation of serum for doing the different hormonal and biochemical assays. Rats were euthanized after anesthesia by decapitation, and thyroid, the liver, kidneys, and heart were quickly excised for histopathological examination.
Hormonal Assay
The RT-2100C microplate reader (Rayto Life and Analytical Sciences, China) was used to measure thyroid-stimulating hormone (TSH) (Catalogue No. RTC007R), thyroxine (T4) (Catalogue No. MBS704309), free thyroxine (FT4) (Catalogue No. ER0962), triiodothyronine (T3) (Catalogue No. MBS261285), free triiodothyonine (FT3) (Catalogue No. CSB-E05076r), and cortisol (Catalogue No. MBS9424757). These parameters were measured using ELISA kits purchased commercially from BioVendor, MyBioSource, FineTest and Cusabio by following of the manufacturer’s instructions.
Hematological and Biochemical Assays
The hematological parameters were measured by using an automated blood cell analyzer (Rayto-7200, Germany), including red blood cells (RBCs) count, hemoglobin (Hb) concentration, packed cell volume (PCV) value and total and differential leukocyte counts.
The semi-auto chemistry analyzer (Chem-7 manufactured by Erba Diagnostics, Germany) was used to measure the serum biochemical parameters, including alanine aminotransferase (ALT), aspartate transaminase (AST), gamma-glutamyltransferase (GGT), total proteins, albumin, creatinine, urea, lactate dehydrogenase (LDH), and creatine kinase-myocardial band (CK-MB).All biochemical markers were measured by using commercial diagnostic kits purchased from Spinreact, following of the manufacturer instructions. Subtracting albumin from total proteins produces globulins concentration.
The RT-2100C microplate reader (Rayto Life and Analytical Sciences, China) was used to measure cardiac troponin I (cTn I) by using an available ELISA kit (Catalogue No. ER0870) purchased from FineTest according to the kit guidelines.
Histopathological Examination
In order to detect the histopathological alterations in the thyroid, liver, kidneys, and heart, the different organs were collected then fixed by using of 10% buffered formalin. The fixed tissues were cut then washed with distilled water and dehydrated in ascending degrees of alcohol, then cleared in xylene, after that, paraffinized and sectioned into 5-μm thin pieces. Finally, the prepared slides were stained with hematoxylin and eosin (H&E) [22]. All slides were examined under a light microscope and photomicrographs were captured.
Statistical Evaluation
In the present study, the obtained data were analyzed by using SPSS software (V21.0) and subjected to statistical processing by using the method of one-way analysis of variance (ANOVA), and Tukey’s HSD post-hoc descriptive was used to test the significance differences between the mean values [23]. A significant change was considered if p < 0.05.
Results
Hormonal Assay
In the current research, serum TSH level showed a significant decrease in both NaI-exposed groups, and the lowest values were observed in (1000 EI) group (p < 0.05) after 30 days from the exposure to NaI and 15 days of stopping NaI-exposure compared with the control group. Serum T4, FT4, T3, FT3, and cortisol levels showed a significant increase in both NaI-exposed groups when compared with the control group, and the highest values were observed in (1000 EI) group (p < 0.05) after 30 days from the exposure to NaI and 15 days of stopping NaI-exposure (Figs. 1, 2, and 3a, b)
a Serum thyroid-stimulating hormone (TSH) and b thyroxine (T4) concentrations after 30 days of starting sodium iodide exposure and 15 days of stopping the exposure in the different groups. Data are expressed in the form of mean ± SE. Bars with different letters are significantly different (p < 0.05) and the highest value was represented by the letter (a). EI excess iodine
a Serum-free thyroxine (FT4) and b triiodothyronine (T3) concentrations after 30 days of starting sodium iodide exposure and 15 days of stopping the exposure in the different groups. Data are expressed in the form of mean ± SE. Bars with different letters are significantly different (p < 0.05) and the highest value was represented by the letter (a). EI excess iodine
a Serum-free triiodothyonine (FT3) and b cortisol concentrations after 30 days of starting sodium iodide exposure and 15 days of stopping the exposure in the different groups. Data are expressed in the form of mean ± SE. Bars with different letters are significantly different (p < 0.05) and the highest value was represented by the letter (a). EI excess iodine
Hematological and Biochemical Assays
Concerning the results of hematological parameters (Tables 2 and 3), a significant increase in RBCs count, Hb concentration, and PCV value in all NaI-exposed groups with regard to the control group (p < 0.05) was observed, and the highest values were observed in (1000 EI) group after 30 days of exposure to NaI, while there were no statistically significant differences in these hematological parameters in all experimental groups after 15 days of stopping NaI-exposure (p > 0.05). A significant reduction and elevation in the total leukocytes count was noted in (500 EI) and (1000 EI) groups, respectively compared with the control group (p < 0.05). Neutrophils count showed a significant decrease in both NaI-exposed groups in comparison with the control group (p < 0.05). Lymphocytic, monocytic, and esinophilic counts exhibited non-significant change and significant increase in (500 EI) and (1000 EI) groups, respectively, when compared with control group (p < 0.05). Basophilic count showed non-statistical significant difference in all tested groups (p > 0.05). All these changes in leukogram were observed after 30 days of the exposure to NaI. On the other hand, non-statistical significant differences were observed in all tested groups in leukogram parameters after 15 days of stopping NaI- exposure (p > 0.05).
As for the results of biochemical tests (Tables 4 and 5), after 30 days of the exposure to NaI, a significant increase in serum ALT, AST, GGT, LDH, and CK-MB activities and levels of total proteins, globulins, urea, and cTn I was remarked in both NaI-exposed groups in comparison with the control group; and the highest values were observed in (1000 EI) group (p < 0.05),while the serum albumin level showed a significant increase in (500 EI) group and non-significant change in (1000 EI) group when compared with control group (p < 0.05); and lastly, serum creatinine showed non-statistical significant difference in all tested groups (p > 0.05). Furthermore, after 15 days of stopping NaI-exposure, a significant increase in serum ALT, AST, GGT, LDH, and CK-MB activities and levels of total proteins, albumin, globulins, urea, and cTn I was observed in (500 EI) and (1000 EI) groups in comparison with the control group; and the highest values were observed in (1000 EI) group except in the values of albumin (p < 0.05), ultimately, serum creatinine, showed non-statistical significant difference in all tested groups (p > 0.05).
Histopathological Examination
Photomicrograph of the rat thyroid gland of the control group showed regular contoured follicles lined by bland-looking cuboidal epithelial cells; large round parafollicular C cells are seen distributed in the follicular wall and in between follicles (Fig. 4a). The histopathological changes in the thyroid gland of the 500 EI group 30 days post NaI-exposure appeared in the form of focal follicular cells proliferation, nuclear enlargement with ground glass appearance, parafollicular cellular proliferation, and cystification (Fig. 4b). Lastly, the most evident histopathological changes in the thyroid gland of the 1000 EI group 30 days post NaI-exposure appeared in the form of focal follicular cells proliferation, nuclear enlargement with ground glass appearance, cystification and capillary hyperemia and intervening capillary network, and associated parathyroid tissue (Fig. 4c,d). Regarding the histopathological alterations in thyroid gland after 15 days of stopping NaI-exposure, the pathological changes in thyroid follicles, follicular cells, and parafollicular cells tend to be lower compared to those found after 30 days of exposure to NaI in this study. Colloid scalloping was also seen in some follicles as a manifestation of previous hyperfunctional activity.
Photomicrograph of H&E stained sections after 30 days of starting sodium iodide exposure. a Thyroid gland tissue section of control group showing regular contoured follicles lined by bland-looking cuboidal epithelial cells (yellow arrows), large round parafollicular C cells are seen distributed in the follicular wall and in between follicles (black star and arrow). b Thyroid gland tissue section of 500 EI group showing focal follicular cells proliferation, nuclear enlargement with ground glass appearance (yellow arrow), parafollicular cellular proliferation (red arrow) and cystification (black arrow). c, d Thyroid gland tissue sections of 1000 EI group showing focal follicular cells proliferation, nuclear enlargement with ground glass appearance (yellow arrow), cystification (green arrows), capillary hyperemia (blue arrow), and intervening capillary network and associated parathyroid tissue (yellow star)
A photomicrograph of rat liver of the control group showed preserved lobular arrangement, hepatic cords orientations, portal tirades structural components, sinusoids, Von-Kupffer cells, and stroma (Fig. 5a). The histopathological alterations in the liver of the 500 EI group 30 days post NaI-exposure were observed in the form of congested blood vessels and (lymphocytes, plasma cells, and macrophages) infiltration (Fig. 5b). On the other hand, liver histopathological findings in the 1000 EI group 30 days post NaI-exposure revealed marked congestion, edema, biliary proliferation, round cells (lymphocytes, plasma cells, and macrophages) infiltration, hepatocellular degeneration (cloudy swelling and hydropic degeneration), besides periportal round cells aggregation, and congested blood vessels (Fig. 5c,d). By looking at the histopathological changes in hepatic tissue after 15 days of stopping NaI-exposure showed generally hepatic parenchymal, vascular, biliary, and stromal structures tend towards normal condition, a part of mild portal vascular dilatation and mild biliary proliferation or chronic cholangitis, which are more pronounced in 1000 EI group.
Photomicrograph of H&E stained sections after 30 days of starting sodium iodide exposure. a Liver tissue section of control group showing preserved lobular arrangement, hepatic cords orientations, portal tirades structural components, sinusoids, Von-Kupffer cells, and stroma (yellow arrow and star). b Liver tissue section of 500 EI group showing congested blood vessels (yellow star) and (lymphocytes, plasma cells and macrophages) infiltration (yellow arrow). c, d Liver tissue sections of 1000 EI group showing marked congestion, edema, biliary proliferation (red arrow), round cells (lymphocytes, plasma cells, and macrophages), infiltration (yellow arrow), hepatocellular degeneration (cloudy swelling and hydropic degeneration) (dark blue arrows), besides periportal round cells aggregation (black arrow), and congested blood vessels (yellow stars)
In the kidney tissue section of the control group, apparently normal cortical and medullary counterparts were observed (Fig. 6a). Microscopic examination of the renal tissue section of the 500 EI group 30 days post NaI-exposure showed mild nephrotoxic changes represented by congestion of renal blood vessels, perivascular edema, and interstitial round cell infiltration (Fig. 6b). The histopathological observations on the kidney of the 1000 EI group 30 days post NaI-exposure showed moderate nephrotoxic changes represented by degenerative changes in renal tubular epithelium (cloudy swelling and hydropic degeneration), interstitial round cell infiltration, cystically dilated renal tubules, hypercellular glomerulous, and intratubular hyaline casts (Figs. 6c, d). On the other hand, the histopathological results after 15 days of stopping NaI-exposure revealed relatively apparent normal renal structures. Mild glomerular shrinkage and renal tubular epithelial degeneration were observed in the 1000 EI group.
Photomicrograph of H&E stained sections after 30 days of starting sodium iodide exposure. a Kidney tissue section of control group showing apparently normal cortical and medullary counterparts (yellow arrows and star). b Kidney tissue section of 500 EI group showing mild nephrotoxic changes represented by congestion of renal blood vessels, perivascular edema (yellow arrow), interstitial round cell infiltration (red arrow). c, d Kidney tissue sections of 1000 EI group showing moderate nephrotoxic changes represented by degenerative changes in renal tubular epithelium (cloudy swelling and hydropic degeneration) (yellow star), interstitial round cell infiltration (red arrow), cystically dilated renal tubules (blue arrow), and hypercellular glomerulous (black arrow)
Heart tissue section of the control group showed apparently normal and healthy cardiomyocytes, sarcolemmal membranes, intercalated discs, coronary and intermuscular blood vessels, and capillaries (Fig. 7a). Inspections of the cardiac tissue sections of the 500 EI group 30 days post NaI-exposure showed congestion of the coronary and intermuscular blood vessels, perivascular, and intermuscular edema (Fig. 7b, c). Histopathological examination of cardiac tissue sections of the 1000 EI group 30 days post NaI-exposure showed cardiotoxic changes represented by congestion of the coronary and intermuscular blood vessels (Fig. 7d), cardiomyocytic degenerative, necrotic, and malacic changes, besides intermascular hemorrhage (Fig. 8a–c). With regard to the histopathological findings of cardiac tissue after 15 days of stopping NaI-exposure, the reduction in the most of cardiac pathological changes previously observed in this study upon exposure to NaI towards normal status was observed.
Photomicrograph of H&E stained sections after 30 days of starting sodium iodide exposure. a Heart tissue section of control group showing apparently normal and healthy cardiomyocytes, sarcolemmal membranes, intercalated discs, coronary and intermuscular blood vessels, and capillaries (yellow arrows). b, c Heart tissue sections of 500 EI group showing congestion of the coronary and intermuscular blood vessels (black arrow), perivascular and intermuscular edema (brown arrow). d Heart tissue sections of 1000 EI group showing cardiotoxic changes represented by congestion of the coronary and intermuscular blood vessels (black arrow)
Discussion
The thyroid gland has a hand over in a large extent on the various activities of the body, where the thyroid hormones act on organs’ physiological functions as well as the metabolic rate, and the activity of different enzymes in the body [24]. Thyroid imbalances can lead to serious disturbances of chemical and morphological structure of different organs [25].
Iodine is a fundamental constituent of the thyroid hormones, so receiving the normal bodily requirement of iodine is an important for normal thyroid function. Thyroxine (T4) and triiodothyronine (T3) are the important hormones produced by the thyroid gland, and T3 is the active form and the majority of it comes from the peripheral conversion of T4 to T3, while it represents 20% of the produced and secreted hormone from the thyroid. On the other hand, T4 constitutes more than 80% of the synthesized and secreted hormone from the thyroid. The production and release of thyroid hormones are regulated by thyroid-stimulating hormone (TSH) under a feedback loop effect [26, 27]. Free forms of thyroid hormones (0.02% of T4 and 0.04% of T3) are considered the biologically active forms, while protein-bound thyroid hormones are considered inactive and unavailable to peripheral tissues. The laboratory screening for the evaluation of thyroid function includes TSH, T4, T3, FT4, and FT3; and the measurement of FT4 and FT3 considers the most clinically relevant for the assessment of thyroid disturbances, where the total thyroid hormones’ measurement is influenced by changes in the concentration of the binding protein [28]. The current study showed a significant decrease in the serum TSH level and significant increase in serum T4, FT4, T3, and FT3 concentrations in in both groups exposed to NaI in excess with the marked alterations in (1000 EI) group compared to the control group. These obtained results may be due to that the excess iodine provides high substrate for thyroid hormones production. Also, it is possible for iodine to act as an immune stimulator, which leading to autoimmune thyroid disease and subsequent hyperthyroidism. TSH level depression in the present study is the most sensitive indicator of hyperthyroidism case [26, 29]. According to Fradkin and Wolff [30], the iodine-induced hyperthyroidism may relate also to faults in autoregulation of hormones biosynthesis. These detected results are confirmed by the histopathological changes of thyroid gland tissue of rats in the experimental groups (Fig. 4b–d). Cortisol is the fundamental hormone responsible for the unfavorable effects of stress. Also, it has an important role in the regulation of different physiological processes inside the body varies from metabolic activities to memory formation and behavior [31, 32]. Concerning the serum cortisol level in the existing study, hypercortisolism was observed in rats groups which exposed to NaI in excess with the highest value in (1000 EI) group in comparison with the control group and that can be due to the significant alterations (hyperactivity) in hypothalamic-pituitary-adrenal axis (HPA) function under the influence of hyperthyroidism. Also, high levels of thyroid hormones have a direct effect on the development and function of the adrenal cortex, where hyperthyroidism accelerates the adrenal cortex morphogenesis and stimulates its hypertrophy and occurrence of hypercortisolism subsequently. Moreover, the severity and duration of the hyperthyroid case may play an important role in determining the adrenal functional capacity level and the HPA axis [33, 34].
The hematological laboratory tests as well as the serum biochemical tests play an important role as health monitoring [35]. In this experiment, exposure of experimental animals to iodine in excess (500 and 1000 EI) markedly increased RBCs count, Hb concentration, and PCV value after 30 days of the exposure compared to control group, and these changes can be attributed to increase production of thyroid hormones as a consequence to an excess iodine load, where the thyroid hormones play an important role in erythropoiesis. They promote erythropoiesis via hyperproliferation of immature erythroid progenitors as well as increase the secretion of erythropoietin hormone by stimulating the erythropoietin gene expression [36].The relationship between thyroid hormones and leukocytes biology is relatively important, where the thyroid hormones effect on the physiological leukocytes activities [37]. In the present work, leukocytosis which was observed in the (1000 EI) group after 30 days of the exposure to NaI may be related to lymphocytosis, monocytosis, and eosinophilia. This may happen as a result of the influence of the hyperthyroidism which induces lymphoid hyperplasia with a corresponding lymphocytosis occurrence [38], as well as the hyperplasia of the myeloid lineages in the bone marrow which leads to increase the number of eosinophils and monocytes [37]. While these changes were not observed in (500 EI) group, this may indicate that the changes in these parameters are taking place in a dose-dependent manner. On the other hand, neutropenia was observed in both NaI-exposed groups in comparison with control group after 30 days of the exposure may be due to decreased neutrophil circulation time or the development of antineutrophil autoantibodies [39, 40].
A complex relationship exists between the thyroid gland and the liver in both health and disease conditions [41]. Liver enzymes are considered as one of the determining factors of liver functional status, where the hepatic impairment is characterized by the abnormality in serum levels of hepatic enzymes and metabolic products in comparison with the normal levels [42]. There are a many of enzymes with different sensitivities and diagnostic indications for the liver injury, such as ALT that is predominantly found in the liver as well as AST and LDH that are somewhat nonspecific for liver injury since their presence in serum can also reflect injury to extrahepatic tissues and GGT which appears to reflect cholestatic injury [43]. The conducted study revealed a significant increase in serum ALT, AST, and LDH activities in both groups exposed to NaI in excess with the highest values in (1000 EI) group compared to the control group of animals. These changes can be probably attributed to induced oxidative damage, which is associated with hyperthyroidism condition resulting from the exposure to excess NaI as well as the hepatocytes apoptosis and subsequent escape of hepatic enzymes to the blood stream [44,45,46]. The produced apoptosis may activate by a direct effect of triiodothyronine hormones on hepatocytes mitochondria and/or as a result of the activation of death receptor-mediated pathways in liver according to Upadhyay et al. and Kumar et al. [44, 45]. On the other hand, increased serum GGT activity indicated hepatic cholestasis condition after exposure to excess iodine [46, 47]. These results are confirmed by the histopathological lesions of the hepatic tissue of rats in the experimental groups (Fig. 5b–d).
Serum proteins measurement is considered an important diagnostic and monitoring tool for different diseases and pathological conditions [48]. Nearly all serum proteins are produced by hepatocytes; the considerable exception is the immunoglobulins that are produced by plasma cell [49]. Concerning the protein profile in this experiment, hyperproteinemia combined with hyperalbuminemia and hyperglobulinemia was noticed in (500 EI) group after 30 days of the exposure to NaI and 15 days of stopping NaI-exposure when compared with the control group. Hyperalbuminemia in this case may be associated with excessive water loss and dehydration associated with hyperthyroidism which recorded by Wudeveld and Jansen [50]. On the other hand, hyperglobulinemia may be associated with high levels of serum immunoglobulins due to impact of thyroid hormone on the immune system, wherein the hyperthyroid case, autoimmune thyroiditis is found to be accentuated [51, 52]. As for the (1000 EI) group, non-significant change in serum albumin level after 30 days of the exposure to NaI may due to rapid catabolism of albumin as well as the hepatic injury in this group at a degree higher than (500 EI) group, which may lead to a degree of hypoalbuminemia and in the same time there are excessive water loss and dehydration in this group, so finally the net resultant non-significant change in albumin value [53, 54]. After 15 days of stopping NaI-exposure, the serum albumin level increased significantly in (1000 EI) group may be due to decrease in the effect of factors, which cause hypoalbuminemia in comparison to other factors which increased it. Hyperglobulinemia was observed in (1000 EI) group after 30 days of the exposure to NaI and 15 days of stopping NaI- exposure for the same previously mentioned causes for (500 EI) group.
Observing some markers of kidney function in this study revealed that non-significant change in the level of serum creatinine in both groups exposed to NaI in excess as well as a significant increase in the value of serum urea after exposure of both groups of animals to excess NaI with the highest values in (1000 EI) group in comparison to the control group. According to some previous studies, the resulted hyperthyroidism condition may cause alterations in renal tubular function and electrolyte homeostasis as well as the increasing in the glomerular filtration rate (GFR), which in turn leads to decrease circulating creatinine and urea concentrations and underlying masked renal dysfunction, and this explains the non-significant change in the values of serum creatinine in the experimental animals. In this condition, creatinine clearance increased and muscle bulk decreased, which in turn leads to decrease creatinine production and level in serum; and in contrast, the mild to moderate renal injury may be occur and induces the increase of serum creatinine level and the net result, masked normal creatinine level [55, 56]. As for the serum urea concentration, several factors may influence its values such as dehydration condition and catabolic state which may be induced by hyperthyroidism and finally leads to increase serum urea concentration in testing animals, besides the renal injury which leads to incomplete removal of urea from the circulation by the kidney [57,58,59]. The histopathological changes of the renal tissue supported these findings in the experimental groups (Fig. 6b–d).
Myocardial cell injury can be determined by releasing of various proteins into the blood circulation from injured myocytes including cardiac troponin I, CK-MB, LDH, and myoglobin [59]. The current study showed that significant increase in serum LDH and CK-MB activities and cTn I level in both experimental groups exposed to excess NaI with the highest values in (1000 EI) group as compared to the respective control. The probable cause of these alterations may be associated with the production of reactive oxygen species (ROS) after the exposure of animals to excess NaI where the iodide reacts exceedingly with all main biomolecules and building bases of proteins, lipids, and nucleic acids and produces intermediary compounds, which can begin severe peroxidative and apoptotic processes and finally leading to disruptive and degenerative changes in the fundamental organs such as the heart [60]. Also, excessive thyroid hormones have a thyrotoxic cardiomyopathy effect, more specifically, is defined as myocardial damage caused by toxic effects of excessive thyroid hormone, resulting in altered myocyte energy production, intracellular metabolism, and myofibril contractile function [61]. These alterations were confirmed and supported by the histopathological findings of the cardiac tissue in the tested groups (Fig. 7b–d and Fig. 8a–c).
Looking at the results of most of the measured parameters in this study, it was found that despite the stopping exposure of experimental animals to NaI (500 and 1000 EI) for 15 days, most of the adverse effects on different organs and histopathological lesions were still observable. This indicates that the negative effects persist longer and may take some time to return to normal values. According to Ilker et al. [62], iodine-induced hyperthyroidism is self-limited considerably with a period of time (1–18) months after the cessation of iodine exposure, so the resolution of hyperthyroidism condition may return the different biological markers towards normal. The present results also stated that the negative impacts on different systems inside the body of experimental animals after exposure to excess iodine appeared to be increased in a dose-dependent manner in comparison to control.
Conclusions
To sum up, the results of this study indicated that the exposure of experimental animals to excess iodine above the tolerable range caused hyperthyroidism, which was associated with significant changes in erythrogram and leukogram and alterations in hepatic, renal, and cardiac functions in an iodine dose-dependent damage relationship, and most of these alterations take more than 15 days to show full change towards the normal status. Accordingly, the results of the present study elevate conception about the health problems after the exposure to excess iodine for considerably long periods.
References
Heyland A, Moroz LL (2005) Cross-kingdom hormonal signaling: an insight from thyroid hormone functions in marine larvae. J Exp Biol 208:4355–4361. https://doi.org/10.1242/jeb.01877
Patrick L (2008) Iodine: deficiency and therapeutic considerations. Altern Med Rev 13:116–127
Laurberg P, Pedersen IB, Knudsen N, Ovesen L, Andersen S (2001) Environmental iodine intake affects the type of non-malignant thyroid disease. Thyroid 11(5):457–469. https://doi.org/10.1089/105072501300176417
Delange F, Lecomte P (2000) Iodine supplementation: benefits outweigh risks. Drug Saf 22:89–95. https://doi.org/10.2165/00002018-200022020-00001
Liu D, Lin X, Yu F, Zhang M, Chen H, Bao W, Wang X (2015) Effects of 3,5-diiodotyrosine and potassium iodide on thyroid function and oxidative stress in iodine-excess Wistar rats. Biol Trace Elem Res 168(2):44752. https://doi.org/10.1007/s12011-015-0371-y
Luo Y, Kawashima A, Ishido Y, Yoshihara A, Oda K, Hiroi N, Ito T, Ishii N, Suzuki K (2014) Iodine excess as an environmental risk factor for autoimmune thyroid disease. Int J Mol Sci 15:12895–12912. https://doi.org/10.3390/ijms150712895
Georgitis WJ, McDermott MT, Kidd GS (1993) An iodine load from water-purification tablets alters thyroid function in humans. Mil Med 158:794–797. https://doi.org/10.1093/milmed/158.12.794
Zhao J, Chen Z, Maberly G (1998) Iodine-rich drinking water of natural origin in China. Lancet 352:2024. https://doi.org/10.1016/S0140-6736(05)61375-X
Franke K, Meyer U, Wagner H, Flachowsky G (2009) Influence of various iodine supplementation levels and two different iodine species on the iodine content of the milk of cows fed rapeseed meal or distillers dried grains with solubles as the protein source. J Dairy Sci 92:4514–4523. https://doi.org/10.3168/jds.2009-2027
Paulíková I, Kováč G, Bíreš J, Paulík Š, Seidel H, Nagy O (2002) Iodine toxicity in ruminants. Vet Med -Czech 47(12):343–350. https://doi.org/10.17221/5845-VETMED
William W (2008) Mineral tolerances of Animals. Tri-State Dairy Nutr Conf
Soetan K, Olaiya CO, Oyewole OE (2009) The importance of mineral elements for humans, domestic animals and plants: a review. Afr J Food Sci 4(5):200–222
Goa TS, Hu FN, Teng WP (2003) Effect of mild and moderate excessive iodine supplementation on thyroid function and morphology in non-iodine deficiency rat model. Zhonghua Nei Ke Za Zhi 42(10):705–708
Food Standards Australia New Zealand (FSANZ) (2008) Final assessment report-proposal P230: consideration of mandatory fortification with iodine for New Zealand. Food Standards Australia New Zealand, Wellington
Burgi H (2010) Iodine excess. Best Pract Res Clin Endocrinal 24:107–115. https://doi.org/10.1016/j.beem.2009.08.010
Rose HR, Zulfiqar H (2021) Jod Basedow syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
Shahid MA, Ashraf MA, Sharma S (2020) Physiology, thyroid hormone. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
NRC (1995) Nutrient requirements of laboratory animals, 4th edn. National Academy Press, Washington DC
Lupachik SV, Nadol'nik LI, Netsetskaya ZV, Vinogradov VV (2006) Effects of chronic administration of high doses of potassium iodide on iodine metabolism in the rat thyroid gland. Biomed Khim 52(2):161–168
Clayton GD, Clayton FE (1981) In: Patty’s industrial toxicology and hygiene. Clayton GD and Clayton FE (eds.), 3rd edn. Vol 2B, p 2975
Chakraborty A, Mandal J, Mondal C, Sinha S, Chandra AK (2016) Effect of excess iodine on oxidative stress markers, steroidogenic-enzyme activities, testicular morphology, and functions in adult male rats. Biol Trace Elem Res 172(2):380–394. https://doi.org/10.1007/s12011-015-0581-3
Suvarna KS, Layton C, Bancroft JD (2013) Bancroft’s theory and practice of histological techniques, 7th edn. Churchill Livingstone Elsevier, China
Snedecor GW, Cochran WG (1994) Statistical method, 8th edn. Iowa State University Press, Ames
Norman AW, Litwack G (1996) Thyroid hormones. In: Norman AW, Litwack G (eds) Hormones, 2nd edn. Academic Press, pp 169–191. https://doi.org/10.1016/B978-012521441-4/50007-9
Sarkar D, Chakraborty A, Saha A, Chandra AK (2018) Iodine in excess in the alterations of carbohydrate and lipid metabolic pattern as well as histomorphometric changes in associated organs. J Basic Clin Physiol Pharmacol 29(6):631–643. https://doi.org/10.1515/jbcpp-2017-0204
Brent GA (2010) Thyroid function testing. Springer, NY. https://doi.org/10.1007/978-1-4419-1485-9
Fitzgerald SP, Bean NG (2018) Thyroid stimulating hormone (TSH) autoregulation reduces variation in the TSH response to thyroid hormones. Temperature 5(4):380–389. https://doi.org/10.1080/23328940.2018.1513110
Welsh KJ, Soldin SJ (2016) How reliable are free thyroid and total T3 hormone assays? Eur J Endocrinol 175(6):R255–R263. https://doi.org/10.1530/EJE-16-0193
Willis GC (2014) Endocrine and metabolic emergencies, an issue of emergency medicine clinics of North America. Volume 32, Number 2. Elsevier, Philadelphia. https://doi.org/10.1016/j.emc.2014.03.001
Fradkin JE, Wolff J (1983) Iodide induced thyrotoxicosis. Medicine 62:1. https://doi.org/10.1097/00005792-198301000-00001
Christiansen JJ, Djurhuus CB, Gravholt CH, Iversen P, Christiansen JS, Schmitz O, Weeke J, Jørgensen JOL, Møller N (2007) Effects of cortisol on carbohydrate, lipid and protein metabolism: studies of acute cortisol withdrawal in adrenocortical failure. J Clin Endocrinol Metab 92:3553–3559. https://doi.org/10.1210/jc.2007-0445
Samidurai M, Kang H, Ramasamy VS, Jo J (2018) Impact of electrical stimulation on cortisol secretion in rat adrenal gland. BioChip J 12(3):216–221. https://doi.org/10.1007/s13206-017-2303-8
Johnson EO, Kamilaris TC, Calogero AE, Gold PW, Chrousos GP (2005) Experimentally induced hyperthyroidism is associated with activation of the rat hypothalamic-pituitary-adrenal axis. Eur J Endocrinol 153(1):177–185. https://doi.org/10.1530/eje.1.01923
Yashchenko A, Lutsyk S (2018) The influence of hypo- and hyperthyroidism on morphogenesis and histophysiology of adrenal glands. J Embryol Stem Cell Res 2(1):000107. https://doi.org/10.23880/JES-16000107
Suckow MA, Stevens KA, Wilson RP (2012) The laboratory rabbit, guinea pig, hamster, and other rodents, 1st edn. Academic press, Elsevier, San Diego, USA
Kandir S, Keskin E (2016) Effects of hypothyroidism and hyperthyroidism on hematological parameters in rats. Ankara Üniv Vet Fak Derg 63:371–376. https://doi.org/10.1501/Vetfak_0000002755
Díaz-Soto G (2014) Thyroid disorders: focus on hyperthyroidism. Rijeka, Croatia
Braverman LE, Cooper DS (2013) Werner and ingbar’s the thyroid: a fundamental and clinical text, 10th edn. Lippincott Williams and Wilkins, Philadelphia. https://doi.org/10.5772/57001
Eakin DL, Peake RL, Weiss GB (1983) Effect of therapy on the neutropenia of hyperthyroidism. South Med J 76(3):335–337. https://doi.org/10.1097/00007611-198303000-00017
Burrow GN, Oppenheimer JH, Volpe R (1990) Thyroid function and disease. W.B. Saunders Company, Philadelphia
Malik R, Hodgson H (2002) The relationship between the thyroid gland and the liver. QJM-Int J Med 95(9):559–569. https://doi.org/10.1093/qjmed/95.9.559
Ajayi AF, Akhigbe RE (2012) Implication of altered thyroid state on liver function. Thyroid Res Pract 9:84–87. https://doi.org/10.4103/0973-0354.99649
Arika WM, Nyamai DW, Osano KO, Ngugi MP, Njagi ENM (2016) Biochemical markers of in vivo hepatotoxicity. J Clin Toxicol 6:297
Upadhyay G, Singh R, Kumar A, Kumar S, Kapoor A, Godbole M (2004) Severe hyperthyroidism induces mitochondria-mediated apoptosis in rat liver. Hepatology 39:1120–1130. https://doi.org/10.1002/hep.20085
Kumar A, Sinha RA, Tiwari M, Singh R, Koji T, Manhas N, Rastogi L, Pal L, Shrivastava A, Sahu RP, Godbole M (2007) Hyperthyroidism induces apoptosis in rat liver through activation of death receptor-mediated pathways. Mayo Clin 46(5):888–898. https://doi.org/10.1016/j.jhep.2006.12.015
Kim SM, Kim SC, Chung IK, Cheon WH, Ku SK (2012) Antioxidant and protective effects of bupleurum falcatum on the l-thyroxine-induced hyperthyroidism in rats. Evid Based Complement Alternat Med 2012:1–12. https://doi.org/10.1155/2012/578497
Suckow MA, Weisbroth SH, Franklin CL (2006) The laboratory rat, 2nd edn. Elsevier, Boston
Tothova C, Nagy O, Kovac G (2016) Serum proteins and their diagnostic utility in veterinary medicine: a review. Vet Med 61(9):475–496. https://doi.org/10.17221/19/2016-VETMED
Eckersall PD (2008) Proteins, proteomics, and the dysproteinemias. In: Kaneko JJ, Harvey JW, Bruss ML (eds) Clinical biochemistry of domestic animals, 6th edn. Elsevier Academic Press, California. https://doi.org/10.1016/B978-0-12-370491-7.00005-2
Wudeveld PGAB, Jansen AP (1960) Renal concentrating and water-excreting capacity in hyperthyroidism. Clinica Chimica Acta 5:618–621. https://doi.org/10.1016/0009-8981(60)90002-4
Mariotti S, Caturegli P, Barbesino G, Del Prete GF, Chiovato L, Pinchera A (1991) Circulating soluble interleukin 2 receptor concentration is increased in both immunogenic and nonimmunogenic hyperthyroidism. J Endocrinol Invest 14:777–781. https://doi.org/10.1007/BF03347915
Nandakumara DN, Konera BC, Vinayagamoorthia R, Nandaa N, Negib VS, Goswamia K, Bobbya Z, Hamide A (2008) Activation of NF-jB in lymphocytes and increase in serum immunoglobulin in hyperthyroidism: possible role of oxidative stress. Immunobiology 213:409–415. https://doi.org/10.1016/j.imbio.2007.10.005
Müller MJ, Seitz H (1984) Thyroid hormone action on intermediary metabolism. Part III. Protein metabolism in hyper-and hypothyroidism. Klin Wochenschr 62:97–102. https://doi.org/10.1007/BF01738699
Thrall MA, Weiser G, Allison RW, Campbell TW (2012) Veterinary hematology and clinical chemistry, 2nd edn. John Wiley & Sons, Iowa
Birchard SJ, Sherding RG (2006) Saunders manual of small animal practice, 3rd edn. Saunders, Elsevier, Missouri, USA
Basu G, Mohapatra A (2013) Interactions between thyroid disorders and kidney disease. Indian J Endocrinol Metab 16(2):204–213. https://doi.org/10.4103/2230-8210.93737
Turakulov Ya K (1975) Thyroid hormones: biosynthesis, physiological effects, and mechanisms of action, 1st edn. Springer, NY
Loeb JN (1978) Metabolic changes: vitamin metabolism, renal function, body water and electrolytes. In: Werner SC, Ingbar SH (eds) The thyroid. Harper and Row Publishers Inc., Hagerstown, pp 705–715
Burtis CA, Ashwood ER, Bruns DE (2012) Tietz textbook of clinical chemistry and molecular diagnostics, 5th edn. Saunders, Elsevier
Joanta AE, Filip A, Clichici S, Andrei S, Cluj-Napoca Romania CN (2006) Iodide excess exerts oxidative stress in some target tissues of the thyroid hormones. Acta Physiol Hung 293:347–359. https://doi.org/10.1556/APhysiol.93.2006.4.11
Osuna PM, Udovcic M, Sharma MD (2017) Hyperthyroidism and the heart. MDCVJ XIII(2):60–63. https://doi.org/10.14797/mdcj-13-2-60
Ilker S, Demet S, Anton P (2020) Iodine-induced hyperthyroidism: do you mind? SANAMED 15(2):215–217. https://doi.org/10.24125/sanamed.v15i2.458
Acknowledgements
The author would like to thank Prof. Dr. Al-Sayed Al-Attar, Professor of Pathology, Faculty of Veterinary Medicine, Zagazig University, Egypt, for his generous help in examining and reading of histopathological slides.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ismail, H.T.H. The Impact of Iodine Exposure in Excess on Hormonal Aspects and Hemato-Biochemical Profile in Rats. Biol Trace Elem Res 200, 706–719 (2022). https://doi.org/10.1007/s12011-021-02681-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-02681-7