Abstract
Due to their potential to enhance therapeutic results and enable targeted drug administration, polymer-drug conjugates that use polyethylene glycol (PEG) as both the polymer and the linker for drug conjugation have attracted much research. This study seeks to investigate recent developments in the design and synthesis of PEG-based polymer-drug conjugates, emphasizing fresh ideas that fill in existing knowledge gaps and satisfy the increasing need for more potent drug delivery methods. Through an extensive review of the existing literature, this study identifies key challenges and proposes innovative strategies for future investigations. The paper presents a comprehensive framework for designing and synthesizing PEG-based polymer-drug conjugates, including rational molecular design, linker selection, conjugation methods, and characterization techniques. To further emphasize the importance and adaptability of PEG-based polymer-drug conjugates, prospective applications are highlighted, including cancer treatment, infectious disorders, and chronic ailments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A potential method for increasing the therapeutic effectiveness of medications and permitting tailored drug administration is the use of polymer-drug conjugates [1,2,3]. Researchers can get around problems with low drug solubility, short half-life, lack of selectivity, and quick removal from the body by conjugating medicines to polymeric carriers [4]. Polyethylene glycol (PEG), one of the many polymers used for drug conjugation, has drawn a lot of interest because of its advantageous traits, which include great biocompatibility, water solubility, and little immunogenicity [5, 6].
Drug delivery technologies have undergone a revolution thanks to the development and manufacture of PEG-based polymer-drug conjugates [7]. PEG provides stability, increased circulation duration, less immunogenicity, and the ability to control drug release kinetics, making it the perfect polymer backbone for drug conjugation [8, 9]. Additionally, PEG is easily functionalized with various linkers to enable site-specific targeting and promote drug attachment [10].
The capacity of PEG-based polymer-drug conjugates to improve therapeutic results is one of their main benefits [11]. Drugs can be shielded from enzymatic breakdown by using PEG as a carrier, enabling extended circulation in the bloodstream [12]. Through increased exposure to the target region during this prolonged circulation time, the drug’s effectiveness is enhanced. Additionally, PEG-based conjugates can minimize off-target effects, as the polymer can shield the drug from interacting with non-target tissues, resulting in reduced toxicity and improved safety profiles [13].
Another critical aspect of PEG-based polymer-drug conjugates is their capacity for targeted drug delivery [14]. By incorporating specific ligands or antibodies onto the PEG backbone, conjugates can be designed to selectively recognize and bind to receptors or antigens expressed on the surface of target cells or tissues [15]. This active targeting strategy improves drug accumulation at the desired site, enhancing therapeutic efficacy while minimizing systemic side effects [16].
Despite the significant progress made in the design and synthesis of PEG-based polymer-drug conjugates, several challenges remain [17]. These include achieving optimal drug loading, maintaining stability during circulation, achieving controlled drug release profiles, and ensuring sufficient conjugation efficiency [18, 19]. Additionally, translating these conjugates from the laboratory to clinical settings requires addressing regulatory considerations and developing scalable manufacturing processes [20].
In light of these challenges and the growing need for more effective drug delivery systems, this research paper aims to explore recent advancements in the design and synthesis of PEG-based polymer-drug conjugates. This study highlights significant research gaps and suggests cutting-edge methodologies for further research through a thorough analysis of the body of existing literature. The article will offer a thorough framework for linker selection and design tactics, conjugation procedures, characterization approaches, and prospective therapeutic applications for rational molecular design of PEG-based conjugates. We want to help promote PEG-based polymer-drug conjugates, which can have a big influence on drug delivery systems, improve therapeutic efficacy, and provide tailored treatment choices for different illnesses, by tackling these important issues.
Rational Molecular Design
The therapeutic effectiveness and targeted drug delivery of polymer-drug conjugates based on polyethylene glycol (PEG) are greatly enhanced by rational molecular design. The choice of PEG as the polymer’s backbone, optimisation of PEG’s molecular weight and architecture, medication compatibility, and therapeutic goals are only a few of the crucial aspects that must be taken into account.
Due to its advantageous characteristics, PEG, a biocompatible and water-soluble polymer, has been widely employed in drug delivery systems [5]. The molecular weight of PEG is a significant factor that affects the pharmacokinetics and biodistribution of the conjugates. The accumulation and circulation time at the target location can be managed by selecting the ideal molecular weight with attention [9]. Recent studies have shown that PEGylation with longer PEG chains, such as PEG 2000, can increase the duration of systemic circulation and enhance therapeutic outcomes [21].
A further crucial component of rational molecular design is the architecture of PEG. A benefit of the creation of branching or multi-arm PEG designs is that they are more stable, have a higher drug loading capacity, and have better targeting efficiency [22]. Higher drug payloads and regulated release kinetics are possible thanks to the many attachment sites that branched PEG designs, such as dendritic PEG, may afford for drug conjugation [23]. Additionally, the PEG backbone’s addition of functional groups makes it easier to conjugate medicines or target ligands, enabling site-specific delivery [24].
The compatibility between the drug and PEG backbone is crucial for ensuring efficient conjugation and maintaining the drug’s stability and activity. Considerations such as drug solubility, chemical reactivity, and drug-polymer interaction should guide the selection of appropriate drug candidates for conjugation with PEG. Recent advances have demonstrated successful PEGylation of various classes of drugs, including small molecules, peptides, and proteins, leading to improved pharmacokinetics and therapeutic outcomes [2, 25].
Linker Selection and Design
The effective production of polymer-drug conjugates based on polyethylene glycol (PEG) depends on the choice and design of an acceptable linker. Linkers are essential for assuring the stability of the conjugates, providing regulated drug release, and promoting effective drug conjugation. The stability of the linker under physiological settings, the intended release kinetics, and the unique needs of the medication and target site must all be taken into account when choosing a linker.
For the polymer-drug combination to remain intact during circulation and to guarantee targeted drug release, the linker’s stability is crucial. Depending on the intended release mechanism, different linkers, such as cleavable and non-cleavable, can be used. Disulfide bonds, hydrazone bonds, and ester linkages are examples of cleavable linkers that have the benefit of causing drug release in response to particular stimuli, such as the intracellular reducing environment or enzyme activity [26]. For long-lasting therapeutic effects, non-cleavable linkers such as amide bonds or stable coordination bonds offer stability and sustained release patterns [27].
The unique characteristics of the medication and the target site should be taken into account while designing linkers. For instance, linkers having functional groups capable of conjugating with certain moieties or ligands can be included if the medicine requires a site-specific release or targeting [28]. Selective conjugation with thiol or amino groups present on the medication or targeted ligands is made possible by the insertion of reactive groups, such as maleimide or NHS ester, on the linker [29]. The development of click chemistry–based linkers, made possible by recent developments in linker design, has facilitated the production of very stable and site-specific polymer-drug conjugates. Click chemistry–based linkers enable efficient and selective conjugation operations [30].
Moreover, the linker length and flexibility should be carefully considered to ensure optimal drug loading and release kinetics. The linker should be long enough to prevent steric hindrance between the polymer and the drug, allowing for efficient drug conjugation and preserving drug activity. Additionally, linker flexibility can influence the release rate of the drug, with more flexible linkers generally promoting faster drug release [31]. The rational design of the linker structure and its attachment to the PEG backbone can provide control over drug release kinetics, maximizing therapeutic efficacy. The common structure of the polymer-drug conjugate can be seen in Fig. 1 (where the polymer-drug conjugate is represented with a clear representation of the polymer backbone, drug molecule, and linker). Various linkers are used in design for the design of various polyethylene glycol-linker-dug conjugated drug delivery systems and have been enlisted in Table 1, where their key features have also been reported.
Representation of polymer-drug conjugate for multipurpose use [32]
Conjugation Methods
The synthesis of polyethylene glycol (PEG)–based polymer-drug conjugates involves efficient and selective conjugation methods that ensure robust attachment of the drug to the PEG polymer backbone. Various conjugation strategies have been developed, offering versatility in terms of drug compatibility, conjugation efficiency, and control over drug loading (Fig. 2 shows the overview of the preparation of polymer-drug conjugate based on theranostic nanoparticles). The selection of the conjugation method depends on the chemical properties of the drug, the desired linker chemistry, and the specific requirements of the target application.
A general overview of the preparation of polymer-drug conjugate-based theranostic nanoparticles [55]
One commonly employed conjugation method is direct chemical conjugation, where the drug and PEG are functionalized with reactive groups that undergo a specific chemical reaction to form a covalent bond. For example, thiol groups on the drug can react with maleimide groups on the PEG backbone through a thiol-maleimide coupling reaction, resulting in stable drug attachment [9, 56]. Similarly, amine groups on the drug can react with carboxyl or NHS ester groups on the PEG backbone through amide bond formation [29]. Recent advancements have also utilized bioorthogonal reactions (Fig. 3 depicts the bioorthogonal chemistry reactions which is a set of high-yielding chemical reactions that occur in biological contexts quickly, selectively, and without causing negative side effects to endogenous functional groups.), such as click chemistry, to achieve selective and efficient conjugation [57, 58].
Bioorthogonal chemical reactions [57]
Another approach for conjugation is the use of activated PEG derivatives. PEG can be modified with specific reactive groups, such as succinimidyl ester or isocyanate, which react directly with nucleophilic groups on the drug to form stable conjugates. This method allows for efficient and site-specific drug attachment, ensuring high conjugation efficiency and minimal loss of drug activity. Additionally, the insertion of targeted ligands or other capabilities to improve the conjugate’s therapeutic qualities is possible when using activated PEG derivatives (see Fig. 4 which shows different linkers to create PEG derivatives) [59].
Different linkers are used to activate polyethylene glycol to create its active PEG derivatives [6]. Where (1) trichloro-s-triazine (cyanuric chloride) method; (2) a variation on the cyanuric chloride method;(3a) method of PEG-succinimidyl succinate; (3b) glutarate substitution by succinate residue; (3c) adding an amide bond to replace the aliphatic ester in 3a; (4) imidazolyl formate method; (5) and (6) are variations using phenyl carbonates of PEG; (7) succinimidyl carbonates of PEG; (8) succinimidyl active esters of PEG
Enzymatic conjugation methods have also gained attention in recent years. Enzymes, such as transglutaminases, can catalyse the formation of covalent bonds between the drug and PEG through enzymatic reactions, providing a mild and selective approach to conjugation [59]. Enzymatic conjugation allows for site-specific drug attachment, preserving the drug’s activity and minimizing non-specific interactions (see Fig. 5 which shows different groups that are catalysing the conjugation which is very crucial for the activity).
mTGase is an enzyme that catalyses conjugation. a The free amine group and the acyl donor. By releasing an ammonia group, the isopeptide link between these two molecules is created. b Water and an acyl donor when there are no free amine groups. c The mTGase crystal structure from S. mobaraensis (PDB ID 3IU0). (Left) Due to the pro sequence, the zymogen form of mTGase folds into a helix that covers the active site (C64). (Right) This is essential for activity, the active form of mTGase exposing the active site (C64) of proteases [60]
The choice of the conjugation method should consider factors such as the stability of the drug, reaction kinetics, and the desired control over drug loading. Additionally, the scalability and reproducibility of the conjugation process should be taken into account to facilitate translation from the laboratory to clinical settings. A few of the reported methods of conjugation have been tabulated in Table 2 with different drugs conjugated with different linkers with their key features and applications.
Characterization Techniques
Characterization techniques play a crucial role in evaluating the physicochemical properties and performance of polymer-drug conjugates and ensuring their successful development and effective drug delivery. Various techniques are employed which provide valuable insights into the structural characteristics, stability, drug loading, release kinetics, and biocompatibility of the conjugates. Several advanced techniques have been employed to assess the key parameters of polymer-drug conjugates, including the following.
Nuclear Magnetic Resonance (NMR)
NMR spectroscopy is widely used to confirm the successful conjugation of drugs to polymer carriers. It enables the identification and quantification of drug-polymer interactions, confirms the successful conjugation of the drug to the polymer backbone, and determines the degree of drug incorporation [106].
Fourier Transform Infrared Spectroscopy (FTIR)
FTIR is commonly used to identify the functional group and confirm the chemical bonding between the polymer and drug by analysing the characteristic peaks of functional groups involved in the conjugation process it provides information on the chemical structure and compatibility of the conjugates [107].
Dynamic Light Scattering (DLS)
DLS is used to measure the size distribution and stability of polymer-drug conjugates in solution as well as the size distribution of polymer-drug conjugates in solution. It provides insights into their stability, aggregation behaviour, and potential for controlled drug release valuable information on the hydrodynamic diameter, polydispersity, and aggregation behaviour of the conjugates [108].
Transmission Electron Microscopy (TEM)
TEM allows for the visualization of polymer-drug conjugates at the nanoscale level. It provides insights into the morphology, shape, and size of the conjugates, confirming the formation of desired nanostructures [109].
In Vitro Release Studies
To assess the release kinetics and drug release patterns from polymer-drug conjugates, in vitro release experiments are carried out. To simulate the drug release behaviour in the target region, these experiments are often conducted in physiologically realistic settings. To examine the drug release profiles, several techniques including dialysis, dissolution, or Franz diffusion cells are used [110].
Size Exclusion Chromatography (SEC)
The molecular weight distribution and homogeneity of polymer-drug conjugates are assessed using SEC. It aids in determining how conjugation affects the size and stability of the polymer [109].
Mass Spectrometry (MS)
The molecular mass and structural integrity of polymer-drug conjugates are determined by MS analysis. It gives details on purity, the ratio of drug to polymer, and if any degradation products are present [111].
Differential Scanning Calorimetry (DSC)
Polymer-drug conjugates’ thermal behaviour and phase transitions are assessed using DSC. Any modifications in the melting point or thermal stability brought on by drug conjugation can be detected [112].
X-ray Diffraction (XRD)
The degree of drug incorporation and crystallinity within the polymer matrix are investigated using XRD analysis. It aids in determining the drug’s physicochemical condition and diffusion throughout the circulatory system [111].
Thermal Analysis
The thermal behaviour, melting point, and thermal stability of polymer-drug conjugates are evaluated using methods like differential scanning calorimetry (DSC) and thermogravimetric analysis (TGA). They aid in comprehending medication stability and release patterns in varied environments [113].
Biological Assays
The biological activity and biocompatibility of polymer-drug conjugates are evaluated using a variety of biological tests, such as cell viability, cytotoxicity, and cell uptake studies. These tests give information on the conjugates’ therapeutic effectiveness and safety [62, 114,115,116].
It is essential to remember that the choice of characterization methods depends on the unique characteristics and needs of the polymer-drug conjugates under investigation. Combining these methods provides a thorough understanding of the properties and performance of the conjugates, helping their development and improvement for therapeutic uses.
Applications in Therapeutics
Due to their capacity to increase drug delivery, enhance pharmacokinetics, and target certain tissues or cells, polymer-drug conjugates have demonstrated tremendous promise in a variety of medicinal applications. Some significant uses for polymer-drug conjugates include the following.
Cancer Therapy
By increasing the selectivity and effectiveness of anti-cancer medications, polymer-drug conjugates have revolutionized cancer therapy. PEGylated liposomal doxorubicin (Doxil®) is one example [15]. Paclitaxel that has been PEGylated (Genexol-PM®) [117] (Fig. 6 displays many polymeric conjugates that are utilised for anti-cancer therapy) demonstrates improved tumour accumulation, extended circulation, and lower systemic toxicity.
Conjugate delivers medications into the body’s systemic circulation in a certain sequence [118]
Targeted Drug Delivery
Targeting certain tissues or cells can be done actively or passively with polymer-drug conjugates. Active targeting involves attaching ligands or antibodies to the polymer backbone, while passive targeting relies on the enhanced permeability and retention (EPR) effect. These strategies improve drug concentration at the desired site and minimize off-target effects [21].
Controlled Drug Release
Polymer-drug conjugates offer the advantage of controlled drug release, allowing sustained and localized delivery of therapeutic agents. Stimuli-responsive polymers, such as temperature, pH, or enzyme-sensitive linkers, enable triggered drug release at specific sites (Fig. 7 illustrates the process of transporting and releasing activity of pH-sensitive linkers in the delivery system) [119].
Using pH-sensitive linkers, PDCs are delivered into cancer cells and released [120]
Gene Delivery
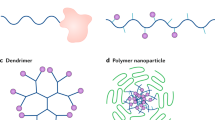
Polymer-drug conjugates have also been explored for gene delivery applications (see Fig. 8 exhibits the different drug delivery systems, which have been designed using PDCs). PEGylated polymeric nanoparticles can efficiently encapsulate and protect nucleic acids, enabling their delivery to target cells for gene therapy or RNA interference [121].
Polymeric drug conjugates for drug delivery [2]
Anti-inflammatory and Immunomodulatory Therapy
Polymer-drug conjugates can be designed to deliver anti-inflammatory or immunomodulatory drugs to treat various inflammatory and autoimmune diseases [122, 123]. Examples include PEGylated glucocorticoids for the treatment of rheumatoid arthritis [105] and PEGylated cytokines for immunotherapy (see Fig. 9 where methods for managing the inflammatory cascade and inflammation through neutrophils, monocytes, lymphocytes, macrophages, etc. are conveyed) [124].
a Recruitment of neutrophils and their roles in inflammation. By expressing P-selectin glycoprotein ligand 1 (PSGL1) and L-selectin, which bind to their respective ligands on the endothelium, neutrophils gently roll along the endothelium. Once at the region of inflammation, intercellular adhesion molecule 1 (ICAM1) on the endothelium and lymphocyte function-associated antigen 1 (LFA1) expressed on the neutrophil lock to start transmigration to the infected or inflammatory tissue area. To stop the spread of infection, neutrophils at the site of infection either phagocytose pathogens or release granules, reactive oxygen species (ROS), or neutrophil extracellular traps (NETs). After that, neutrophils commit to apoptosis, which starts other immune cell types migrating. By using efferocytosis, monocytes and macrophages eliminate dead cellular materials (pathogens and neutrophils), and they eventually go to the liver and lymph nodes to eliminate and deal with pathogenic materials. Furthermore, in order to support tissue repair, post-efferocytosis monocytes change to a pro-resolution phenotype. b Therapies not dependent on particles that control inflammation. stem cell therapies: mesenchymal stem cells (MSCs) that have been transplanted have the ability to generate cytokines that suppress the immune system, which can reduce immune cell recruitment and activation, increase the creation of regulatory T (Treg) cells, and block the development of T helper 1 (TH1) and T helper 2 (TH2) cells. Cytokines and antibody-based treatments: inflammatory cytokines attach to blocking antibodies or decoy receptors, which prevents their activation and reduces systemic inflammation. Vascular endothelial cells are the target of biological treatments that block certain leukocyte adhesion molecules, preventing immune cells from transmigrating and so inhibiting the inflammatory response. Targeted blocking of immune cells: by preventing certain receptors on the surface of immune cells, medications can directly revent immune cells from becoming pathologically activated. Monoclonal antibodies, or mAbs [125]
These applications (Table 3) demonstrate the versatility and potential of polymer-drug conjugates in improving therapeutic outcomes and addressing the limitations associated with conventional drug delivery systems.
Delivery Systems Designed from PEGylated Polymer-Drug Conjugates (PEG-PDCs)
Polymer-drug conjugates (PDCs) have emerged as a revolutionary platform for drug delivery, offering numerous advantages over conventional drug delivery systems [120, 144]. These advantages include improved solubility, enhanced pharmacokinetics, controlled drug release, and targeted delivery [145]. This review critically analyses various delivery systems designed by PEG-PDCs, highlighting their key features, advantages, and limitations.
Types of Delivery Systems from PEG-PDCs
PEG-PDCs can be utilized to design various delivery systems, catering to diverse therapeutic needs. Some of the prominent types include:
-
1.
Micelles: Amphiphilic PEG-PDCs can self-assemble into micellar structures, encapsulating drugs within the hydrophobic core. Micelles offer improved drug solubility and controlled release, making them suitable for hydrophobic drugs and sustained drug delivery [146,147,148].
-
2.
Liposomes: PEG-PDCs can be incorporated into the phospholipid bilayer of liposomes, providing them with enhanced stability, prolonged circulation times, and improved drug delivery. Liposomes enable targeted delivery through surface modifications with ligands [36, 149, 150].
-
3.
Nanoparticles: Polymeric nanoparticles loaded with drugs offer enhanced bioavailability, controlled release, and targeted delivery. PEG-PDCs can be used to design nanoparticles with specific sizes, surface properties, and drug release profiles for tailored therapeutic applications [12, 151,152,153].
-
4.
Hydrogels: PEG-PDCs can be incorporated into hydrogels for sustained and localized delivery of drugs. Hydrogels offer excellent biocompatibility and can provide a controlled release environment for sensitive drugs [30, 43, 69, 154, 155].
-
5.
Conjugates with targeting ligands: PEG-PDCs can be conjugated with targeting ligands, such as antibodies or peptides, to specifically target diseased tissues. This approach reduces systemic exposure and enhances therapeutic efficacy while minimizing side effects [66].
Research Examples of Delivery Systems Derived from PEG-PDCs
The following table (Table 4) summarizes recent research on delivery systems designed from PEG-PDCs, highlighting key aspects of each study.
Current Challenges and Future Perspectives
PEG-PDC-based delivery systems offer significant advantages over conventional drug delivery methods [55, 163]. They can improve the therapeutic efficacy and safety of various drugs while providing controlled release and targeted delivery [32, 164]. However, further research is needed to address certain challenges, including:
-
Development of more efficient and cost-effective synthesis methods [163].
-
Improved targeting strategies for specific diseases and tissues [25].
-
Overcoming potential immunogenicity concerns of PEGylation [116].
-
Developing strategies to control and optimize drug release profiles [110, 165, 166].
Despite these challenges, PEG-PDC-based delivery systems hold immense potential for revolutionizing drug delivery and improving patient outcomes. Future research efforts focused on addressing the existing challenges and exploring new applications will further propel the advancement of this promising technology.
Overcoming Limitations in PEG-Based Polymer-Drug Conjugation
Despite the significant progress in the field of PEG-based polymer-drug conjugates, several challenges still need to be addressed. One of the challenges is the efficient and selective conjugation of drugs to PEG polymers. The development of novel linker chemistries and conjugation strategies that provide controlled and site-specific drug attachment to PEG can enhance the stability and therapeutic efficacy of the conjugates [9, 167]. Additionally, optimizing the ratio of drug to polymer and the polymer size can further improve the drug loading capacity and release kinetics of the conjugates [168, 169]. Overcoming these limitations will contribute to the development of more effective PEG-based polymer-drug conjugates.
Limited In Vitro Validation
The study primarily relies on in vitro experiments [165, 170, 171]. While these experiments provide valuable insights into the basic mechanisms of action of the PEG-PDC-based delivery systems, they cannot fully predict the complex biological environment in vivo [172]. Further studies involving animal models and clinical trials are crucial to assess the safety and efficacy of these systems in humans.
Potential for Off-Target Toxicity
While PEG-PDCs are generally considered biocompatible, there is still a risk of off-target accumulation and potential side effects [173]. This is particularly concerning for nanoparticles that accumulate in organs such as the liver and spleen. Future research should focus on optimizing targeting strategies, such as by incorporating specific ligands or antibodies, to minimize off-target delivery.
Limited Drug Loading Capacity
Some PEG-PDC-based delivery systems may have limited drug loading capacity, restricting their effectiveness for certain therapeutic applications [152]. This is especially true for hydrophobic drugs that are difficult to encapsulate efficiently. Developing strategies to enhance drug loading without compromising stability and biocompatibility is crucial for realizing the full potential of these systems.
Scalability and Cost-Effectiveness
Scaling up the production of some PEG-PDCs can be challenging and expensive, limiting their widespread clinical use [174]. This is a major hurdle that needs to be overcome before PEG-PDC-based therapies can be made available to patients on a large scale. Future research should focus on developing cost-effective and scalable methods for PEG-PDCs production, such as continuous flow synthesis or microfluidic technologies.
Limited Understanding of Long-Term Effects
The long-term effects of PEG-PDC-based delivery systems are not fully understood [172, 175]. This is a significant concern, as nanoparticles can potentially accumulate in the body and cause long-term toxicity. Further studies are needed to investigate the potential for long-term effects and bioaccumulation of PEG-PDC-based systems before they can be widely adopted in clinical practice.
Regulatory Considerations and Clinical Translation of PEG-Based Systems
The clinical translation of PEG-based polymer-drug conjugates requires careful consideration of regulatory aspects. Understanding the regulatory requirements for the development, manufacturing, and clinical evaluation of PEG-based conjugates is crucial for their successful translation into the clinic. Issues related to the safety, toxicity, pharmacokinetics, and immunogenicity of the conjugates need to be thoroughly investigated [39, 176]. Moreover, scalability and reproducibility of the synthesis and manufacturing processes should be addressed to ensure consistent product quality. Collaboration between researchers, clinicians, regulatory authorities, and industry partners is essential to navigate these regulatory challenges and facilitate the clinical translation of PEG-based polymer-drug conjugates [130, 151].
Emerging Trends and Future Directions for PEG-Based Research
The field of PEG-based polymer-drug conjugates is continuously evolving, and several promising trends and future directions can be identified. One such trend is the development of multifunctional conjugates that combine therapeutic agents with imaging probes or targeting ligands to enable personalized medicine and improve treatment outcomes [177, 178]. Furthermore, the integration of stimuli-responsive properties into PEG-based systems allows for on-demand drug release at specific disease sites, enhancing therapeutic efficacy and minimizing off-target effects [179, 180]. Exploring new polymers, such as dendrimers, hyperbranched polymers, or supramolecular polymers, holds promise for expanding the versatility and functionality of PEG-based conjugates [22]. Additionally, advances in nanotechnology and nanomedicine can offer innovative strategies for the delivery of PEG-based conjugates, including the development of novel nano-carriers or combination therapies [22, 181]. The development and clinical use of PEG-based polymer-drug conjugates will be aided by continued research efforts in these fields.
Future Scopes
Development of Novel PEG-PDC-based Platforms
New PEG-PDC-based systems with improved functionalities, such as stimuli-responsive release, multimodality imaging, and combined drug delivery, can be developed to address specific therapeutic needs. These advanced systems can offer greater control over drug delivery and improve therapeutic efficacy.
Integration with Advanced Technologies
PEG-PDCs can be integrated with nanotechnologies, biomaterials, and artificial intelligence to create more sophisticated and personalized delivery systems. This integration can lead to the development of smart and responsive systems that can tailor their delivery behaviour to the specific needs of each patient.
Exploration of New Therapeutic Applications
PEG-PDCs can be explored for the delivery of various therapeutic agents, including gene editing tools, nucleic acids, and cell-based therapies. This opens up a wide range of potential applications for PEG-PDC-based systems in treating various diseases.
Improved In Vivo Studies
More comprehensive preclinical studies using relevant animal models are essential to assess the safety and efficacy of PEG-PDC-based systems in vivo. These studies should involve testing the systems in various disease models and evaluating their long-term effects.
Clinical Translation
The successful translation of PEG-PDC-based delivery systems into clinical practice requires robust clinical trials to demonstrate their safety and efficacy in humans. These trials should be well-designed and conducted following ethical guidelines to ensure the safety and well-being of patients.
Discussion and Conclusion
The design and production of PEG-based polymer-drug conjugates and their therapeutic uses, as well as the existing difficulties and promising future directions in this sector, have all been covered in this article. The discussion has highlighted the significance of PEGylation as a tactic to improve drug delivery system effectiveness and get around the drawbacks of traditional formulations.
The benefits of PEG-based polymer-drug conjugates include better solubility, longer circulation times, less immunogenicity, and tailored drug delivery. These conjugates have proven to improve drug stability, controlled release, and selective targeting of particular tissues or cells through logical molecular design, linker selection, and conjugation techniques [130, 150, 182,183,184]. The effectiveness and specificity of drug conjugation are greatly influenced by the choice of linker and conjugation technique. The intended release kinetics, stability, and biocompatibility of the conjugates should be taken into account while choosing and designing suitable linkers and conjugation techniques [120, 123, 185]. Characterization methods are essential for evaluating the physicochemical properties, stability, and efficacy of PEG-based polymer-drug conjugates. Numerous techniques, including spectroscopy, chromatography, and microscopy, may be used to analyse the structural characterization of the conjugates, release kinetics, and efficiency of drug loading. These techniques help to guarantee the consistency and quality of the conjugates for use in clinical trials and additional research [153, 180, 184, 186]. The conjugates have enhanced treatment outcomes, decreased systemic toxicity, and patient compliance. They might be designed to specifically target cancer cells or tumour microenvironments, enabling site-specific drug delivery and minimizing adverse effects. PEG-based conjugates can be changed to add other capabilities, such as imaging agents or stimuli-responsive components, expanding their potential for application in diagnostic and therapy monitoring [187,188,189,190]. PEG-based polymer-drug conjugates have demonstrated great potential, but there are still several problems that need to be fixed. Overcoming limitations in conjugation efficiency, stability, and scalability is crucial for their successful translation into clinical use. Regulatory considerations play a significant role in the development and approval of PEG-based systems for therapeutic applications, necessitating rigorous preclinical and clinical evaluations. Future research should focus on developing more advanced and multifunctional conjugates, exploring novel polymers, optimizing drug loading and release kinetics, and addressing potential immunogenicity issues.
In conclusion, PEG-based polymer-drug conjugates represent a promising approach for improving drug delivery in various therapeutic areas. Their rational design, selection of appropriate linkers and conjugation methods, and comprehensive characterization enable enhanced therapeutic efficacy and reduced toxicity. The applications of these conjugates in cancer therapy and other diseases highlight their potential impact in the field of therapeutics. However, further research and development efforts are required to overcome existing challenges and realize the full potential of PEG-based polymer.
Data Availability
Not applicable.
Abbreviations
- PEG:
-
Poly ethylene glycol
- PDC:
-
Polymer Drug conjugates
- DSPE-PEG:
-
1,2-Distearyl-sn-glycero-3-phosphoethanolamine-Poly(ethylene glycol)
- SiRNA:
-
Small interfering RNA
- PEG-PCL:
-
Poly(ethylene glycol)-Poly(ε-caprolactone)copolymers
- RNA:
-
Ribonucleic acid
- DNA:
-
Deoxy ribonucleic acid
- PEG-PLA:
-
Poly(ethylene glycol)-polyactide-poly(ethylene glycol)
References
Liechty, W. B., Kryscio, D. R., Slaughter, B. V., & Peppas, N. A. (2010). Polymers for drug delivery systems. Annual Review of Chemical and Biomolecular Engineering, 1, 149–173. https://doi.org/10.1146/ANNUREV-CHEMBIOENG-073009-100847
Larson, N., & Ghandehari, H. (2012). Polymeric conjugates for drug delivery. Chemistry of Materials: A Publication of the American Chemical Society, 24(5), 840. https://doi.org/10.1021/CM2031569
Thakor, P., Bhavana, V., Sharma, R., Srivastava, S., Singh, S. B., & Mehra, N. K. (2020). Polymer–drug conjugates recent advances and future perspectives. Drug Discovery Today, 25(9), 1718–1726. https://doi.org/10.1016/J.DRUDIS.2020.06.028
Negut, I., & Bita, B. (2023). Polymeric Micellar Systems—A special emphasis on Smart. Drug Delivery Pharmaceutics, 15(976), 1–49. https://doi.org/10.3390/pharmaceutics15030976
Greenwald, R. B., Conover, C. D., & Choe, Y. H. (2000). Poly(ethylene glycol) conjugated drugs and prodrugs: A comprehensive review. Critical Reviews in Therapeutic Drug Carrier Systems, 17(2), 61–101. Retrieved from https://pubmed.ncbi.nlm.nih.gov/10820646/
Milton Harris, J., & Chess, R. B. (2003). Effect of pegylation on pharmaceuticals. Nature Reviews Drug Discovery, 2(3), 214–221. https://doi.org/10.1038/nrd1033
Torchilin, V. P. (2001). Structure and design of polymeric surfactant-based drug delivery systems. Journal of Controlled Release, 73(2–3), 137–172. https://doi.org/10.1016/S0168-3659(01)00299-1
Kumari, A., Yadav, S. K., & Yadav, S. C. (2010). Biodegradable polymeric nanoparticle-based based drug delivery systems. Colloids and Surfaces B Biointerfaces, 75(1), 1–18. https://doi.org/10.1016/J.COLSURFB.2009.09.001
Veronese, F. M., & Pasut, G. (2005). PEGylation, successful approach to drug delivery. Drug Discovery Today, 10(21), 1451–1458. https://doi.org/10.1016/S1359-6446(05)03575-0
Ibeanu, N., Egbu, R., Onyekuru, L., Javaheri, H., Khaw, P. T., Williams, G. R., … Awwad, S. (2020). Injectables and depots to prolong drug action of proteins and peptides. Pharmaceutics, 12(10), 1–42. https://doi.org/10.3390/PHARMACEUTICS12100999
Kratz, F. (2008). Albumin as a drug carrier: Design of prodrugs, drug conjugates and nanoparticles. Journal of Controlled Release: Official Journal of the Controlled Release Society, 132(3), 171–183. https://doi.org/10.1016/J.JCONREL.2008.05.010
Moghimi, S. M., Hunter, A. C., & Murray, J. C. (2001). Long-circulating and target-specific nanoparticles: Theory to practice. Pharmacological Reviews, 53(2), 283–318. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11356986
Duncan, R. (2014). Polymer therapeutics: Top 10 selling pharmaceuticals - what next? Journal of Controlled Release: Official Journal of the Controlled Release Society, 190, 371–380. https://doi.org/10.1016/J.JCONREL.2014.05.001
Torchilin, V. P. (2010). Passive and active drug targeting: Drug delivery to tumours as an example. Handbook of Experimental Pharmacology, 197(197), 3–53. https://doi.org/10.1007/978-3-642-00477-3_1
Peer, D., Karp, J. M., Hong, S., Farokhzad, O. C., Margalit, R., & Langer, R. (2007). Nanocarriers as an emerging platform for cancer therapy. Nature Nanotechnology, 2(12), 751–760. https://doi.org/10.1038/NNANO.2007.387
Shi, J., Kantoff, P. W., Wooster, R., & Farokhzad, O. C. (2017). Cancer nanomedicine: Progress, challenges and opportunities. Nature Reviews Cancer, 17(1), 20–37. https://doi.org/10.1038/nrc.2016.108
Feng, Q., & Tong, R. (2016). Anticancer nanoparticulate polymer-drug conjugate. Bioengineering & Translational Medicine, 1(3), 277–296. https://doi.org/10.1002/btm2.10033
Duncan, R. (2003). The dawning era of polymer therapeutics. Nature Reviews Drug Discovery, 2(5), 347–360. https://doi.org/10.1038/NRD1088
Anselmo, A. C., & Mitragotri, S. (2016). Nanoparticles in the clinic. Bioengineering & Translational Medicine, 1(1), 10–29. https://doi.org/10.1002/btm2.10003
Etrych, T., Šubr, V., Laga, R., Říhová, B., & Ulbrich, K. (2014). Polymer conjugates of doxorubicin bound through an amide and hydrazone bond: Impact of the carrier structure onto synergistic action in the treatment of solid tumours. European Journal of Pharmaceutical Sciences, 58, 1–12. https://doi.org/10.1016/j.ejps.2014.02.016
Maeda, H. (2001). The enhanced permeability and retention (EPR) effect in tumour vasculature: The key role of tumor-selective macromolecular drug targeting. Advances in Enzyme Regulation, 41(1), 189–207. https://doi.org/10.1016/S0065-2571(00)00013-3
Dozier, J. K., & Distefano, M. D. (2015). Site-specific PEGylation of therapeutic proteins. International Journal of Molecular Sciences, 16(10), 25831–25864. https://doi.org/10.3390/IJMS161025831
Zelphati, O., Wang, Y., Kitada, S., Reed, J. C., Felgner, P. L., & Corbeil, J. (2001). Intracellular delivery of proteins with a new lipid-mediated delivery system. Journal of Biological Chemistry, 276(37), 35103–35110. https://doi.org/10.1074/JBC.M104920200
Lee, E. S., Oh, K. T., Kim, D., Youn, Y. S., & Bae, Y. H. (2007). Tumor pH-responsive flower-like micelles of poly(l-lactic acid)-b-poly(ethylene glycol)-b-poly(l-histidine). Journal of Controlled Release, 123(1), 19–26. https://doi.org/10.1016/J.JCONREL.2007.08.006
Polyak, D., Eldar-Boock, A., Baabur-Cohen, H., & Satchi-Fainaro, R. (2013). Polymer conjugates for focal and targeted delivery of drugs. Polymers for Advanced Technologies, 24(9), 777–790. https://doi.org/10.1002/PAT.3158
Tsuchikama, K., & An, Z. (2018). Antibody-drug conjugates recent advances in conjugation and linker chemistries. Protein & Cell, 9(1), 33–46. https://doi.org/10.1007/s13238-016-0323-0
Duncan, R., Vicent, M. J., Greco, F., & Nicholson, R. I. (2005). Polymer-drug conjugates: Towards a novel approach for the treatment of endocrine-related cancer. Endocrine-Related Cancer, 12(SUPPL. 1), 189–199. https://doi.org/10.1677/erc.1.01045
Aldewachi, H., Al-Zidan, R. N., Conner, M. T., & Salman, M. M. (2021). High-throughput screening platforms in the Discovery of Novel drugs for neurodegenerative diseases. Bioengineering, 8(2), 30. https://doi.org/10.3390/bioengineering8020030
Begines, B., Ortiz, T., Pérez-Aranda, M., Martínez, G., Merinero, M., Argüelles-Arias, F., & Alcudia, A. (2020). Polymeric nanoparticles for drug delivery: Recent developments and future prospects. Nanomaterials, 10(7), 1403(1–38). https://doi.org/10.3390/nano10071403
Auriemma, G., Russo, P., Del Gaudio, P., García-González, C. A., Landín, M., & Aquino, R. P. (2020). Technologies and formulation design of polysaccharide-based hydrogels for drug delivery. Molecules, 25(14), 3156. https://doi.org/10.3390/molecules25143156
Lallana, E., Sousa-Herves, A., Fernandez-Trillo, F., Riguera, R., & Fernandez-Megia, E. (2011). Click chemistry for drug delivery nanosystems. Pharmaceutical Research, 29:1(1), 1–34. https://doi.org/10.1007/S11095-011-0568-5
Javia, A., Vanza, J., Bardoliwala, D., Ghosh, S., Misra, L. A., Patel, M., & Thakkar, H. (2022). Polymer-drug conjugates design principles, emerging synthetic strategies and clinical overview. International Journal of Pharmaceutics, 623, 121863. https://doi.org/10.1016/J.IJPHARM.2022.121863
Li, J., & Kao, W. J. (2003). Synthesis of polyethylene glycol (PEG) derivatives and PEGylated - peptide biopolymer conjugates. Biomacromolecules, 4(4), 1055–1067. https://doi.org/10.1021/BM034069L
Kharkar, P. M., Rehmann, M. S., Skeens, K. M., Maverakis, E., & Kloxin, A. M. (2016). Thiol-ene click hydrogels for therapeutic delivery. ACS Biomaterials Science & Engineering, 2(2), 165–179. https://doi.org/10.1021/ACSBIOMATERIALS.5B00420
Hossen, S., Hossain, M. K., Basher, M. K., Mia, M. N. H., Rahman, M. T., & Uddin, M. J. (2019). Smart nanocarrier-based drug delivery systems for cancer therapy and toxicity studies: A review. Journal of Advanced Research, 15, 1–18. https://doi.org/10.1016/j.jare.2018.06.005
Milla, P., Dosio, F., & Cattel, L. (2011). PEGylation of proteins and liposomes: A powerful and flexible strategy to improve the drug delivery. Current Drug Metabolism, 13, 105–119. https://doi.org/10.2174/138920012798356934
Cai, K., Wang, A. Z., Yin, L., & Cheng, J. (2017). Bio-nano interface: the impact of biological environment on nanomaterials and their delivery properties. Journal of Controlled Release, 263, 211–222. https://doi.org/10.1016/j.jconrel.2016.11.034
Kondengadan, S. M., Bansal, S., Yang, C., Liu, D., Fultz, Z., & Wang, B. (2023). Click chemistry and drug delivery: A bird’s-eye view. Acta Pharmaceutica Sinica B, 13(5), 1990–2016. https://doi.org/10.1016/j.apsb.2022.10.015
Torchilin, V. P. (2012). Multifunctional nanocarriers. Advanced Drug Delivery Reviews, 64(SUPPL.), 302–315. https://doi.org/10.1016/j.addr.2012.09.031
Kadam, R. U., Bergmann, M., Hurley, M., Garg, D., Cacciarini, M., Swiderska, M. A., … Reymond, J. L. (2011). A glycopeptide dendrimer inhibitor of the galactose-specific lectin LecA and pseudomonas aeruginosa biofilms. Angewandte Chemie - International Edition, 50(45), 10631–10635. https://doi.org/10.1002/anie.201104342
Dhaneshwar, S., Kandpal, M., Gairola, N., & Kadam, S. (2006). Dextran: A promising macromolecular drug carrier. Indian Journal of Pharmaceutical Sciences, 68(6), 705–714. https://doi.org/10.4103/0250-474X.31000
Fu, C., Zhu, C., Synatschke, C. V., & Zhang, X. (2021). Editorial: design, synthesis and biomedical applications of functional polymers. Frontiers in Chemistry, 9, 1–2. https://doi.org/10.3389/fchem.2021.681189
Widjaja, L. K., Bora, M., Chan, P. N. P. H., Lipik, V., Wong, T. T. L., & Venkatraman, S. S. (2014). Hyaluronic acid-based nanocomposite hydrogels for ocular drug delivery applications. Journal of Biomedical Materials Research - Part A, 102(9), 3056–3065. https://doi.org/10.1002/jbm.a.34976
Qi, R., Gao, Y., Tang, Y., He, R. R., Liu, T. Le, He, Y., … Liu, G. (2009). PEG-conjugated PAMAM dendrimers mediate efficient intramuscular gene expression. AAPS Journal, 11(3), 395–405. https://doi.org/10.1208/s12248-009-9116-1
De Paula, D., Bentley, M. V. L. B., & Mahato, R. I. (2007). Hydrophobization and bioconjugation for enhanced siRNA delivery and targeting. RNA, 13(4), 431–456. https://doi.org/10.1261/rna.459807
Duncan, R. (2011). Polymer therapeutics as nanomedicines: New perspectives. Current Opinion in Biotechnology, 22(4), 492–501. https://doi.org/10.1016/j.copbio.2011.05.507
Alley, S. C., Okeley, N. M., & Senter, P. D. (2010). Antibody–drug conjugates: Targeted drug delivery for cancer. Current Opinion in Chemical Biology, 14(4), 529–537. https://doi.org/10.1016/j.cbpa.2010.06.170
Sahu, A., Bora, U., Kasoju, N., & Goswami, P. (2008). Synthesis of novel biodegradable and self-assembling methoxy poly(ethylene glycol)-palmitate nanocarrier for curcumin delivery to cancer cells. Acta Biomaterialia, 4(6), 1752–1761. https://doi.org/10.1016/j.actbio.2008.04.021
Gao, W., Chan, J. M., & Farokhzad, O. C. (2010). pH-Responsive nanoparticles for drug delivery. Molecular Pharmaceutics, 7(6), 1913–1920. https://doi.org/10.1021/mp100253e
Junutula, J. R., Raab, H., Clark, S., Bhakta, S., Leipold, D. D., Weir, S., … Mallet, W. (2008). Site-specific conjugation of a cytotoxic drug to an antibody improves the therapeutic index. Nature Biotechnology, 26(8), 925–932. https://doi.org/10.1038/nbt.1480
Kopeček, J. (2013). Polymer–drug conjugates: Origins, progress to date and future directions. Advanced Drug Delivery Reviews, 65(1), 49–59. https://doi.org/10.1016/j.addr.2012.10.014
Jao, D., Xue, Y., Medina, J., & Hu, X. (2017). Protein-based drug-delivery materials. Materials (Basel), 10(5), 517(1–24). https://doi.org/10.3390/ma10050517
Hale, C. R., Zhao, P., Olson, S., Duff, M. O., Graveley, B. R., Wells, L., … Terns, M. P. (2009). RNA-Guided RNA Cleavage by a CRISPR RNA-Cas Protein Complex. Cell, 139(5), 945–956. https://doi.org/10.1016/j.cell.2009.07.040
Zhang, Y., Hsu, B. Y. W., Ren, C., Li, X., & Wang, J. (2014). Silica-based nanocapsules: Synthesis, structure control and biomedical applications. Chemical Society Reviews, 44(1), 315–335. https://doi.org/10.1039/C4CS00199K
Manandhar, S., Sjöholm, E., Bobacka, J., Rosenholm, J. M., & Bansal, K. K. (2021). Polymer-drug conjugates as Nanotheranostic agents. Journal of Nanotheranostics, 2(1), 63–81. https://doi.org/10.3390/jnt2010005
Pasut, G., & Veronese, F. M. (2012). State of the art in PEGylation: The great versatility achieved after forty years of research. Journal of Controlled Release: Official Journal of the Controlled Release Society, 161(2), 461–472. https://doi.org/10.1016/J.JCONREL.2011.10.037
Hartung, K. M., & Sletten, E. M. (2023). Bioorthogonal chemistry: Bridging chemistry, biology, and medicine. Chem, 9(8), 2095–2109. https://doi.org/10.1016/j.chempr.2023.05.016
Qin, L. H., Hu, W., & Long, Y. Q. (2018). Bioorthogonal chemistry: Optimization and application updates during 2013–2017. Tetrahedron Letters, 59(23), 2214–2228. https://doi.org/10.1016/j.tetlet.2018.04.058
Mehvar, R. (2000). Modulation of the pharmacokinetics and pharmacodynamics of proteins by polyethylene glycol conjugation. Journal of Pharmacy & Pharmaceutical Sciences: a publication of the Canadian Society for Pharmaceutical Sciences, Societe canadienne des sciences pharmaceutiques, 3(1), 125–36. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10954682
Chan, S. K., & Lim, T. S. (2019). Bioengineering of microbial transglutaminase for biomedical applications. Applied Microbiology and Biotechnology, 103(7), 2973–2984. https://doi.org/10.1007/s00253-019-09669-3
Roberts, M. J., Bentley, M. D., & Harris, J. M. (2002). Chemistry for peptide and protein PEGylation. Advanced Drug Delivery Reviews, 54(4), 459–476. https://doi.org/10.1016/S0169-409X(02)00022-4
Banerjee, S. S., Aher, N., Patil, R., & Khandare, J. (2012). Poly(ethylene glycol)-prodrug conjugates: Concept, design, and applications. Journal of Drug Delivery, 2012, 1–17. https://doi.org/10.1155/2012/103973
Belén, L. H., Rangel-Yagui, C. de O., Beltrán Lissabet, J. F., Effer, B., Lee-Estevez, M., Pessoa, A., … Farías, J. G. (2019). From synthesis to characterization of site-selective PEGylated proteins. Frontiers in Pharmacology, 10, 1450. https://doi.org/10.3389/fphar.2019.01450
Zacchigna, M., Cateni, F., Drioli, S., & Bonora, G. M. (2011). Multimeric, multifunctional derivatives of poly(ethylene glycol). Polymers, 3(3), 1076–1090. https://doi.org/10.3390/polym3031076
Yan, J., Marina, P. F., & Blencowe, A. (2021). A facile strategy for the high yielding, quantitative conversion of polyglycol end-groups to amines. Polymers, 13(9), 1403. https://doi.org/10.3390/polym13091403
Hoppenz, P., Els-Heindl, S., & Beck-Sickinger, A. G. (2020). Peptide-drug conjugates and their targets in advanced cancer therapies. Frontiers in Chemistry, 8. https://doi.org/10.3389/fchem.2020.00571
Hoffman, A. S. (2012). Hydrogels for biomedical applications. Advanced Drug Delivery Reviews, 64(SUPPL.), 18–23. https://doi.org/10.1016/J.ADDR.2012.09.010
Arseneault, M., Wafer, C., & Morin, J. F. (2015). Recent advances in click chemistry applied to dendrimer synthesis. Molecules, 20(5), 9263–9294. https://doi.org/10.3390/molecules20059263
Lee, J. H. (2018). Injectable hydrogels deliver therapeutic agents for disease treatment and tissue engineering. Biomaterials Research, 22(1), 27. https://doi.org/10.1186/s40824-018-0138-6
Cicalese, M. P., Ferrua, F., Castagnaro, L., Pajno, R., Barzaghi, F., Giannelli, S., … Aiuti, A. (2016). Update on the safety and efficacy of retroviral gene therapy for immunodeficiency due to adenosine deaminase deficiency. Blood, 128(1), 45–54. https://doi.org/10.1182/blood-2016-01-688226
Wang, Z., Li, H., Gou, L., Li, W., & Wang, Y. (2023). Antibody–drug conjugates: Recent advances in payloads. Acta Pharmaceutica Sinica B, 13(10), 4025–4059. https://doi.org/10.1016/j.apsb.2023.06.015
Raza, F., Zafar, H., Zhu, Y., Ren, Y., Ullah, A., Khan, A. U., … Ge, L. (2018). A review of recent advances in stabilizing peptides/proteins upon fabrication in hydrogels from biodegradable polymers. Pharmaceutics, 10(1), 16. https://doi.org/10.3390/PHARMACEUTICS10010016
Butt, H., Eid, A., Ali, Z., Atia, M. A. M., Mokhtar, M. M., Hassan, N., … Mahfouz, M. M. (2017). Efficient CRISPR/Cas9-mediated genome editing using a chimeric single-guide RNA molecule. Frontiers in Plant Science, 8, 1441. https://doi.org/10.3389/fpls.2017.01441
Jasinski, D., Haque, F., Binzel, D. W., & Guo, P. (2017). Advancement of the emerging field of RNA nanotechnology. ACS Nano, 11(2), 1142–1164. https://doi.org/10.1021/acsnano.6b05737
Vargason, A. M., Anselmo, A. C., & Mitragotri, S. (2021). The evolution of commercial drug delivery technologies. Nature Biomedical Engineering, 5(9), 951–967. https://doi.org/10.1038/S41551-021-00698-W
Yao, Y., Zhou, Y., Liu, L., Xu, Y., Chen, Q., Wang, Y., … Shao, A. (2020). Nanoparticle-based drug delivery in cancer therapy and its role in overcoming drug resistance. Frontiers in Molecular Biosciences, 7, 193. https://doi.org/10.3389/fmolb.2020.00193
Mukherjee, A., Waters, A. K., Kalyan, P., Achrol, A. S., Kesari, S., & Yenugonda, V. M. (2019). Lipid-polymer hybrid nanoparticles as a next-generation drug delivery platform: State of the art, emerging technologies, and perspectives. International Journal of Nanomedicine, 14, 1937–1952. https://doi.org/10.2147/IJN.S198353
Bhattacharya, S., Prajapati, B. G., & Singh, S. (2023). A critical review on the dissemination of PH and stimuli-responsive polymeric nanoparticular systems to improve drug delivery in cancer therapy. Critical Reviews in Oncology/Hematology, 185, 103961. https://doi.org/10.1016/J.CRITREVONC.2023.103961
Cheng, X., Xie, Q., & Sun, Y. (2023). Advances in nanomaterial-based targeted drug delivery systems. Frontiers in Bioengineering and Biotechnology, 11, 1177151. https://doi.org/10.3389/fbioe.2023.1177151
Miao, Y., Yang, T., Yang, S., Yang, M., & Mao, C. (2022). Protein nanoparticles directed cancer imaging and therapy. Nano Convergence, 9(1), 2. https://doi.org/10.1186/s40580-021-00293-4
Xia, W., Tao, Z., Zhu, B., Zhang, W., Liu, C., Chen, S., & Song, M. (2021). Targeted delivery of drugs and genes using polymer nanocarriers for Cancer Therapy. International Journal of Molecular Sciences, 22(17), 9118. https://doi.org/10.3390/ijms22179118
Diamantis, N., & Banerji, U. (2016). Antibody-drug conjugates—an emerging class of cancer treatment. British Journal of Cancer, 114(4), 362. https://doi.org/10.1038/BJC.2015.435
Rassu, G., Sorrenti, M., Catenacci, L., Pavan, B., Ferraro, L., Gavini, E., … Dalpiaz, A. (2023). Conjugation, prodrug, and co-administration strategies in support of nanotechnologies to improve the therapeutic efficacy of phytochemicals in the central nervous system. Pharmaceutics, 15(6), 1–42. https://doi.org/10.3390/pharmaceutics15061578
Haney, M. J., Klyachko, N. L., Zhao, Y., Gupta, R., Plotnikova, E. G., He, Z., … Batrakova, E. V. (2015). Exosomes as drug delivery vehicles for Parkinson’s disease therapy. Journal of Controlled Release, 207, 18–30. https://doi.org/10.1016/j.jconrel.2015.03.033
Xu, M., Yang, Q., Sun, X., & Wang, Y. (2020). Recent advancements in the loading and modification of therapeutic exosomes. Frontiers in Bioengineering and Biotechnology, 8, 586130. https://doi.org/10.3389/FBIOE.2020.586130
Hu, Y., Liu, C., & Muyldermans, S. (2017). Nanobody-based delivery systems for diagnosis and targeted tumour therapy. Frontiers in Immunology, 8(NOV), 1442. https://doi.org/10.3389/FIMMU.2017.01442
Neeraj Agrawal, R., & Alok Mukerji, A. J. (2013). Polymeric prodrugs: Recent achievements and general strategies. Journal of Antivirals & Antiretrovirals, s15, 1–12. https://doi.org/10.4172/jaa.S15-007
Habault, J., & Poyet, J. L. (2019). Recent advances in cell penetrating peptide-based Anticancer therapies. Molecules (Basel Switzerland), 24(5), 927. https://doi.org/10.3390/MOLECULES24050927
Bechara, C., & Sagan, S. (2013). Cell-penetrating peptides: 20 years later, where do we stand? FEBS Letters, 587(12), 1693–1702. https://doi.org/10.1016/J.FEBSLET.2013.04.031
Materón, E. M., Miyazaki, C. M., Carr, O., Joshi, N., Picciani, P. H. S., Dalmaschio, C. J., … Shimizu, F. M. (2021). Magnetic nanoparticles in biomedical applications: A review. Applied Surface Science Advances, 6, 100163. https://doi.org/10.1016/J.APSADV.2021.100163
Siddique, S., & Chow, J. C. L. (2020). Gold nanoparticles for drug delivery and cancer therapy. Applied Sciences, 10(11), 3824. https://doi.org/10.3390/APP10113824
Tiwari, P. M., Vig, K., Dennis, V. A., & Singh, S. R. (2011). Functionalized Gold nanoparticles and their biomedical applications. Nanomaterials (Basel Switzerland), 1(1), 31–63. https://doi.org/10.3390/NANO1010031
Vardaxi, A., Kafetzi, M., & Pispas, S. (2022). Polymeric nanostructures containing proteins and peptides for Pharmaceutical Applications. Polymers, 14(4), 1–22. https://doi.org/10.3390/polym14040777
Verhoef, J. J. F., & Anchordoquy, T. J. (2013). Questioning the use of PEGylation for drug delivery. Drug Delivery and Translational Research, 3(6), 499. https://doi.org/10.1007/S13346-013-0176-5
Liu, Z., Tabakman, S., Welsher, K., & Dai, H. (2009). Carbon nanotubes in biology and medicine: In vitro and in vivo detection, imaging and drug delivery. Nano Research, 2(2), 85–120. https://doi.org/10.1007/s12274-009-9009-8
Pei, B., Wang, W., Dunne, N., & Li, X. (2019). Applications of Carbon nanotubes in Bone tissue regeneration and Engineering: Superiority, concerns, current advancements, and prospects. Nanomaterials, 9(10), 1501. https://doi.org/10.3390/nano9101501
Florkiewicz, W., Słota, D., Placek, A., Pluta, K., Tyliszczak, B., Douglas, T. E. L., & Sobczak-Kupiec, A. (2021). Synthesis and characterization of polymer-based Coatings modified with Bioactive ceramic and bovine serum albumin. Journal of Functional Biomaterials, 12(2), 21. https://doi.org/10.3390/JFB12020021
Fu, C.-P., Cai, X.-Y., Chen, S.-L., Yu, H.-W., Fang, Y., Feng, X.-C., … Li, C.-Y. (2023). Hyaluronic acid-based nanocarriers for anticancer drug delivery. Polymers, 15(10), 2317. https://doi.org/10.3390/polym15102317
Pathak, P., Zarandi, M. A., Zhou, X., & Jayawickramarajah, J. (2021). Synthesis and applications of porphyrin-biomacromolecule conjugates. Frontiers in Chemistry, 9, 764137. https://doi.org/10.3389/FCHEM.2021.764137
Sarbadhikary, P., George, B. P., & Abrahamse, H. (2021). Recent advances in Photosensitizers as multifunctional theranostic agents for imaging-guided photodynamic therapy of Cancer. Theranostics, 11(18), 9054–9088. https://doi.org/10.7150/THNO.62479
Markovic, M., Ben-Shabat, S., & Dahan, A. (2020). Prodrugs for Improved Drug Delivery: Lessons learned from recently developed and marketed products. Pharmaceutics, 12(11), 1–12. https://doi.org/10.3390/PHARMACEUTICS12111031
Suk, J. S., Xu, Q., Kim, N., Hanes, J., & Ensign, L. M. (2016). PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Advanced Drug Delivery Reviews, 99, 28–51. https://doi.org/10.1016/J.ADDR.2015.09.012
Salih, S., Alkatheeri, A., Alomaim, W., & Elliyanti, A. (2022). Radiopharmaceutical treatments for cancer therapy, radionuclides characteristics, applications, and challenges. Molecules, 27(16), 5231. https://doi.org/10.3390/molecules27165231
Holz, E., Darwish, M., Tesar, D. B., & Shatz-Binder, W. (2023). A review of protein- and peptide-based chemical conjugates: past, present, and future. Pharmaceutics, 15(2), 600. https://doi.org/10.3390/pharmaceutics15020600
Hussain, Z., Khan, S., Imran, M., Sohail, M., Shah, S. W. A., & de Matas, M. (2019). PEGylation: A promising strategy to overcome challenges to cancer-targeted nanomedicines: A review of challenges to clinical transition and promising resolution. Drug Delivery and Translational Research, 9(3), 721–734. https://doi.org/10.1007/s13346-019-00631-4
Zloh, M. (2019). NMR spectroscopy in drug discovery and development: Evaluation of physico-chemical properties. ADMET & DMPK, 7(4), 242. https://doi.org/10.5599/ADMET.737
Campanale, C., Savino, I., Massarelli, C., & Uricchio, V. F. (2023). Fourier transform infrared spectroscopy to assess the degree of alteration of artificially aged and environmentally weathered microplastics. Polymers, 15(4), 1–16. https://doi.org/10.3390/polym15040911
Stetefeld, J., McKenna, S. A., & Patel, T. R. (2016). Dynamic light scattering: A practical guide and applications in biomedical sciences. Biophysical Reviews, 8(4), 409. https://doi.org/10.1007/S12551-016-0218-6
Iwamoto, C., Ohtani, Y., & Hamada, K. (2023). Microstructure variation in the ultrasonic bonding process between Al sheets observed by in-situ transmission electron microscopy. Scripta Materialia, 234. https://doi.org/10.1016/j.scriptamat.2023.115560
Geraili, A., Xing, M., & Mequanint, K. (2021). Design and fabrication of drug-delivery systems toward adjustable release profiles for personalized treatment. Polymers, 2(5), 20200126. https://doi.org/10.1002/VIW.20200126
Messner, C. B., Demichev, V., Wang, Z., Hartl, J., Kustatscher, G., Mülleder, M., & Ralser, M. (2023). Mass spectrometry-based high-throughput proteomics and its role in biomedical studies and systems biology. Proteomics, 23(7–8), 1–15. https://doi.org/10.1002/PMIC.202200013
Dikecoglu, F. B., Topal, A. E., Ozkan, A. D., Tekin, E. D., Tekinay, A. B., Guler, M. O., & Dana, A. (2018). Force and time-dependent self-assembly, disruption and recovery of supramolecular peptide amphiphile nanofibers. Nanotechnology, 29(28), 285701. https://doi.org/10.1088/1361-6528/AABEB4
Fu, Y., & Kao, W. J. (2010). Drug release kinetics and transport mechanisms of non-degradable and degradable polymeric delivery systems. Expert Opinion on drug Delivery, 7(4), 429–444. https://doi.org/10.1517/17425241003602259
Elvira, C., Gallardo, A., San Roman, J., & Cifuentes, A. (2005). Covalent polymer-drug conjugates. Molecules 2005, 10(1), 114–125. https://doi.org/10.3390/10010114
Harbers, G. M., Emoto, K., Greef, C., Metzger, S. W., Woodward, H. N., Mascali, J. J., … Lochhead, M. J. (2007). A functionalized poly(ethylene glycol)-based bioassay surface chemistry that facilitates bio-immobilization and inhibits non-specific protein, bacterial, and mammalian cell adhesion. Chemistry of materials: a publication of the American Chemical Society, 19(18), 4405. https://doi.org/10.1021/CM070509U
Chen, B. M., Cheng, T. L., & Roffler, S. R. (2021). Polyethylene glycol immunogenicity: Theoretical, clinical, and practical aspects of Anti-polyethylene Glycol antibodies. Acs Nano, 15(9), 14022–14048. https://doi.org/10.1021/acsnano.1c05922
Luo, T., Magnusson, J., Préat, V., Frédérick, R., Alexander, C., Bosquillon, C., & Vanbever, R. (2016). Synthesis and in vitro evaluation of polyethylene glycol-paclitaxel conjugates for lung cancer therapy. Pharmaceutical Research, 33(7), 1671–1681. https://doi.org/10.1007/s11095-016-1908-2
Khan, J., Alexander, A., Ajazuddin, Saraf, S., & Saraf, S. (2018). Exploring the role of polymeric conjugates toward anti-cancer drug delivery: Current trends and future projections. International Journal of Pharmaceutics, 548(1), 500–514. https://doi.org/10.1016/j.ijpharm.2018.06.060
Yang, K., Feng, L., & Liu, Z. (2016). Stimuli-responsive drug delivery systems based on nano-graphene for cancer therapy. Advanced Drug Delivery Reviews, 105, 228–241. https://doi.org/10.1016/J.ADDR.2016.05.015
Junyaprasert, V. B., & Thummarati, P. (2023). Innovative design of targeted nanoparticles: Polymer–drug conjugates for enhanced Cancer Therapy. Pharmaceutics, 15(9), 2216. https://doi.org/10.3390/pharmaceutics15092216
Wu, P., Chen, H., Jin, R., Weng, T., Ho, J. K., You, C., … Han, C. (2018). Non-viral gene delivery systems for tissue repair and regeneration. Journal of Translational Medicine. BioMed Central Ltd. https://doi.org/10.1186/s12967-018-1402-1
Sahu, P., Sharma, G., Sagar Verma, V., Mishra, A., Deshmukh, N., Pandey, A., … Chauhan, P. (2022). Statistical optimization of microwave assisted acrylamide grafting of Linum usitatissimum Gum. NeuroQuantology, 20(11), 4008–4026. https://doi.org/10.14704/NQ.2022.20.11.NQ66404
Verma, V. S., Mishra, A., Badwaik, H. R., Alexander, A., & Ajazuddin, A. (2022). Molecular docking for rationalizing the use of linkers in polymer-drug conjugates design for pegylated anti-inflammatory drug delivery. International Journal of Health Sciences, 6626–6646. https://doi.org/10.53730/IJHS.V6NS6.11216
Zhai, Y., Zhou, Y., Li, X., & Feng, G. (2015). Immune-enhancing effect of nano-DNA vaccine encoding a gene of the prME protein of Japanese encephalitis virus and BALB/c mouse granulocyte-macrophage colony-stimulating factor. Molecular Medicine Reports, 12(1), 199–209. https://doi.org/10.3892/mmr.2015.3419
Brannon, E. R., Guevara, M. V., Pacifici, N. J., Lee, J. K., Lewis, J. S., & Eniola-Adefeso, O. (2022). Polymeric particle-based therapies for acute inflammatory diseases. Nature Reviews Materials, 7:10(10), 796–813. https://doi.org/10.1038/s41578-022-00458-5
Fan, Y., & Zhang, Q. (2013). Development of liposomal formulations: From concept to clinical investigations. Asian Journal of Pharmaceutical Sciences, 8(2), 81–87. https://doi.org/10.1016/j.ajps.2013.07.010
Paranjpe, P. V., Stein, S., & Sinko, P. J. (2005). Tumor-targeted and activated bioconjugates for improved camptothecin delivery. Anti-cancer Drugs, 16(7), 763–775. https://doi.org/10.1097/01.CAD.0000172834.78068.7C
Song, B., Liu, X., Dong, H., & Roy, R. (2023). Mir-140-3P induces chemotherapy resistance in esophageal carcinoma by targeting the NFYA-MDR1 axis. Applied Biochemistry and Biotechnology, 195(2), 973–991. https://doi.org/10.1007/S12010-022-04139-5
Maradana, M. R., Thomas, R., & O’Sullivan, B. J. (2013). Targeted delivery of curcumin for treating type 2 diabetes. Molecular Nutrition & food Research, 57(9), 1550–1556. https://doi.org/10.1002/MNFR.201200791
Alven, S., Nqoro, X., Buyana, B., & Aderibigbe, B. A. (2020). Polymer-drug conjugate, a potential therapeutic to combat breast and lung cancer. Pharmaceutics, 12(5), 406. https://doi.org/10.3390/pharmaceutics12050406
Novio, F. (2020). Design of targeted nanostructured coordination polymers (NCPs) for Cancer Therapy. Molecules, 25(15), 3449. https://doi.org/10.3390/MOLECULES25153449
van der Meel, R., Vehmeijer, L., Kok, R., Storm, G., & van Gaal, E. (2013). Ligand-targeted particulate nanomedicines undergoing clinical evaluation: Current status. Advanced Drug Delivery Reviews, 65(10), 163–200. https://doi.org/10.1016/j.addr.2013.08.012
Wang, Y. C., Wang, F., Sun, T. M., & Wang, J. (2011). Redox-responsive nanoparticles from the single disulfide bond-bridged block copolymer as drug carriers for overcoming multidrug resistance in cancer cells. Bioconjugate Chemistry, 22(10), 1939–1945. https://doi.org/10.1021/bc200139n
Santos-Carballal, B., Fernández Fernández, E., & Goycoolea, F. (2018). Chitosan in non-viral gene delivery: role of structure, characterization methods, and insights in cancer and rare diseases therapies. Polymers, 10(4), 444. https://doi.org/10.3390/polym10040444
Barua, S., Ramos, J., Potta, T., Taylor, D., Huang, H. C., Montanez, G., & Rege, K. (2011). Discovery of Cationic polymers for non-viral gene delivery using combinatorial approaches. Combinatorial Chemistry & High Throughput Screening, 14, 908–932. https://doi.org/10.2174/138620711797537076
Janakiraman, K., Krishnaswami, V., Rajendran, V., Natesan, S., & Kandasamy, R. (2018). Novel nano therapeutic materials for the effective treatment of rheumatoid arthritis-recent insights. Materials Today Communications, 17, 200–213. https://doi.org/10.1016/j.mtcomm.2018.09.011
Holley, A. K., Bakthavatchalu, V., Velez-Roman, J. M., & Clair, S. (2011). Manganese superoxide dismutase: Guardian of the powerhouse. International Journal of Molecular Sciences, 12(10), 7114–7162. https://doi.org/10.3390/IJMS12107114
Su, Q., Dong, J., Zhang, D., Yang, L., & Roy, R. (2022). Protective effects of the Bilobalide on Retinal oxidative stress and inflammation in Streptozotocin-Induced Diabetic rats. Applied Biochemistry and Biotechnology, 194(12), 6407–6422. https://doi.org/10.1007/S12010-022-04012-5
Cremolini, C., Vitale, E., Rastaldo, R., & Giachino, C. (2021). Advanced nanotechnology for enhancing immune checkpoint blockade therapy. Nanomaterials, 11(3), 1–26. https://doi.org/10.3390/NANO11030661
Siedenbiedel, F., & Tiller, J. C. (2012). Antimicrobial polymers in solution and on surfaces: Overview and functional principles. Polymers, 4(1), 46–71. https://doi.org/10.3390/polym4010046
Deslouches, B., Montelaro, R. C., Urish, K. L., & Di, Y. P. (2020). Engineered Cationic antimicrobial peptides (eCAPs) to combat multidrug-resistant bacteria. Pharmaceutics, 12(6), 501. https://doi.org/10.3390/pharmaceutics12060501
Parveen, S., Sur, T., Sarkar, S., & Roy, R. (2023). Antagonist impact of selenium-based nanoparticles against Mycobacterium tuberculosis. Applied Biochemistry and Biotechnology, 195(6), 3606–3614. https://doi.org/10.1007/S12010-023-04315-1
Zenych, A., Fournier, L., & Chauvierre, C. (2020). Nanomedicine progress in thrombolytic therapy. Biomaterials, 258, 120297. https://doi.org/10.1016/J.BIOMATERIALS.2020.120297
Sun, Y., & Davis, E. (2021). Nanoplatforms for targeted stimuli-responsive drug delivery: A review of platform materials and stimuli-responsive release and targeting mechanisms. Nanomaterials, 11(3), 746. https://doi.org/10.3390/nano11030746
Bajwa, N., Mahal, S., Singh, P. A., Jyoti, K., Dewangan, P., Madan, J., & Baldi, A. (2023). Drug–polymer conjugates: Challenges, opportunities, and prospects in clinical trials. Polymer-Drug Conjugates: Linker Chemistry Protocols and Applications, 389–469. https://doi.org/10.1016/B978-0-323-91663-9.00011-4
Chaudhuri, A., Ramesh, K., Kumar, D. N., Dehari, D., Singh, S., Kumar, D., & Agrawal, A. K. (2022). Polymeric micelles: A novel drug delivery system for the treatment of breast cancer. Journal of Drug Delivery Science and Technology, 77, 103886. https://doi.org/10.1016/J.JDDST.2022.103886
Ordanini, S., & Cellesi, F. (2018). Complex polymeric architectures self-assembling in unimolecular micelles: Preparation, characterization and drug nanoencapsulation. Pharmaceutics, 10(4), 209. https://doi.org/10.3390/pharmaceutics10040209
Gong, J., Chen, M., Zheng, Y., Wang, S., & Wang, Y. (2012). Polymeric micelles drug delivery system in oncology. Journal of Controlled Release: Official Journal of the Controlled Release Society, 159(3), 312–323. https://doi.org/10.1016/J.JCONREL.2011.12.012
Yadav, D., Sandeep, K., Pandey, D., & Dutta, R. K. (2017). Liposomes for drug delivery. Journal of Biotechnology & Biomaterials, 7(4), 1–8. https://doi.org/10.4172/2155-952X.1000276
Biswas, S., Kumari, P., Lakhani, P. M., & Ghosh, B. (2016). Recent advances in polymeric micelles for anti-cancer drug delivery. European Journal of Pharmaceutical Sciences: Official Journal of the European Federation for Pharmaceutical Sciences, 83, 184–202. https://doi.org/10.1016/J.EJPS.2015.12.031
Danhier, F., Ansorena, E., Silva, J. M., Coco, R., Le Breton, A., & Préat, V. (2012). PLGA-based nanoparticles: An overview of biomedical applications. Journal of Controlled Release: Official Journal of the Controlled Release Society, 161(2), 505–522. https://doi.org/10.1016/J.JCONREL.2012.01.043
Dristant, U., Mukherjee, K., Saha, S., & Maity, D. (2023). An overview of polymeric nanoparticles-based drug delivery system in Cancer Treatment. Technology in Cancer Research & Treatment, 22, 153303382311520. https://doi.org/10.1177/15330338231152083
Mudigunda, S. V., Pemmaraju, D. B., Paradkar, S., Puppala, E. R., Gawali, B., Upadhyayula, S. M., … Rengan, A. K. (2022). Multifunctional polymeric nanoparticles for chemo/phototheranostics of retinoblastoma. ACS Biomaterials Science & Engineering, 8(1), 151–160. https://doi.org/10.1021/acsbiomaterials.1c01234
Coolich, M. K., Lanier, O. L., Cisneros, E., & Peppas, N. A. (2023). PEGylated insulin-loaded complexation hydrogels for protected oral delivery. Journal of Controlled Release: Official Journal of the Controlled Release Society, 364, 216–226. https://doi.org/10.1016/J.JCONREL.2023.10.020
Phelps, E. A., Enemchukwu, N. O., Fiore, V. F., Sy, J. C., Murthy, N., Sulchek, T. A., … García, A. J. (2012). Maleimide cross‐linked bioactive PEG hydrogel exhibits improved reaction kinetics and cross‐linking for cell encapsulation and in situ delivery. Advanced Materials, 24(1), 64–70. https://doi.org/10.1002/adma.201103574
Biswas, S., Dodwadkar, N. S., Deshpande, P. P., & Torchilin, V. P. (2012). Liposomes loaded with paclitaxel and modified with novel triphenylphosphonium-PEG-PE conjugate possess low toxicity, target mitochondria and demonstrate enhanced antitumor effects in vitro and in vivo. Journal of Controlled Release, 159(3), 393–402. https://doi.org/10.1016/J.JCONREL.2012.01.009
Ashtary-Larky, D., Rezaei Kelishadi, M., Bagheri, R., Moosavian, S. P., Wong, A., Davoodi, S. H., … Asbaghi, O. (2021). The effects of nano-curcumin supplementation on risk factors for cardiovascular disease: A GRADE-assessed systematic review and meta-analysis of clinical trials. Antioxidants, 10(7), 1015. https://doi.org/10.3390/antiox10071015
Ang, M. J., Kang, S., & Moon, C. (2020). Melatonin alters neuronal architecture and increases cysteine-rich protein 1 signalling in the male mouse hippocampus. Journal of Neuroscience Research, 98(11), 2333–2348. https://doi.org/10.1002/JNR.24708
Anushiravani, M., Bakhshaee, M., Taghipour, A., & Mehri, M. R. (2018). Comparison of the therapeutic effect of the Persian Medicine Protocol with the common treatment of chronic rhinosinusitis: A randomized clinical trial. Electronic Physician, 10(7), 7017. https://doi.org/10.19082/7017
Chaisi, M. E., Osinubi, S. T., Dalton, D. L., & Suleman, E. (2019). Occurrence and diversity of avian haemosporidia in afrotropical landbirds. International Journal for Parasitology: Parasites and Wildlife, 8, 36. https://doi.org/10.1016/J.IJPPAW.2018.12.002
Hossain, S., Imai, Y., Suzuki, D., Choi, W., Chen, Z., Suzuki, T., … Negishi, Y. (2019). Elucidating ligand effects in thiolate-protected metal clusters using Au24Pt(TBBT)18 as a model cluster. Nanoscale, 11(45), 22089–22098. https://doi.org/10.1039/C9NR07117B
Shellmer, D. A., Dabbs, A. D., & Dew, M. A. (2011). Medical adherence in pediatric organ transplantation: What are the next steps? Current Opinion in Organ Transplantation, 16(5), 509. https://doi.org/10.1097/MOT.0B013E32834A8C89
Cen, J., Hou, M., & Liu, S. (2023). Discrete polyethylene glycol derivatives as a potent impetus for next-generation biomedicines. Giant, 15, 100169. https://doi.org/10.1016/j.giant.2023.100169
Duncan, R., Ringsdorf, H., & Satchi-Fainaro, R. (2008). Polymer therapeutics—Polymers as drugs, drug and protein conjugates and gene delivery systems: Past, present and future opportunities. Journal of Drug Targeting, 14(6), 337–341. https://doi.org/10.1080/10611860600833856
Shaik, B. B., Katari, N. K., & Jonnalagadda, S. B. (2023). Internal stimuli-responsive nanocarriers for controlled anti-cancer drug release: A review. Therapeutic Delivery, 14(9), 595–613. https://doi.org/10.4155/tde-2023-0041
Bai, X., Smith, Z., Wang, Y., Butterworth, S., & Tirella, A. (2022). Sustained drug release from Smart nanoparticles in Cancer Therapy: A comprehensive review. Micromachines, 13(10), 1623. https://doi.org/10.3390/mi13101623
Molineux, G. (2004). The design and development of Pegfilgrastim (PEG-rmetHuG-CSF, Neulasta ®). Current Pharmaceutical Design, 10(11), 1235–1244.
Farokhzad, O. C., Cheng, J., Teply, B. A., Sherifi, I., Jon, S., Kantoff, P. W., … Langer, R. (2006). Targeted nanoparticle-aptamer bioconjugates for cancer chemotherapy in vivo. Proceedings of the National Academy of Sciences of the United States of America, 103(16), 6315–6320. https://doi.org/10.1073/PNAS.0601755103
Bobo, D., Robinson, K. J., Islam, J., Thurecht, K. J., & Corrie, S. R. (2016). Nanoparticle-based medicines: a review of FDA-approved materials and clinical trials to date. Pharmaceutical Research, 33(10), 2373–2387. https://doi.org/10.1007/S11095-016-1958-5/METRICS
Sebak, A. A. (2018). Limitations of Pegylated nanocarriers: unfavourable physicochemical properties, biodistribution patterns and cellular and subcellular fates. International Journal of Applied Pharmaceutics, 10(5), 6. https://doi.org/10.22159/ijap.2018v10i5.27568
Bae, Y. H., & Park, K. (2020). Advanced drug delivery 2020 and beyond perspectives on the future. Advanced Drug Delivery Reviews, 158, 4–16. https://doi.org/10.1016/J.ADDR.2020.06.018
Hatakeyama, H., Akita, H., & Harashima, H. (2013). The Polyethyleneglycol Dilemma: Advantage and disadvantage of PEGylation of liposomes for systemic genes and nucleic acids delivery to tumors. Biological and Pharmaceutical Bulletin, 36(6), 892–899. https://doi.org/10.1248/bpb.b13-00059
Sanchez Armengol, E., Unterweger, A., & Laffleur, F. (2022). PEGylated drug delivery systems in the pharmaceutical field: Past, present and future perspective. Drug Development and Industrial Pharmacy, 48(4), 129–139. https://doi.org/10.1080/03639045.2022.2101062
Cheng, C. C., Lee, D. J., Liao, Z. S., & Huang, J. J. (2016). Stimuli-responsive single-chain polymeric nanoparticles towards the development of efficient drug delivery systems. Polymer Chemistry, 7(40), 6164–6169. https://doi.org/10.1039/C6PY01623E
Grewal, I. K., Singh, S., Arora, S., & Sharma, N. (2020). Polymeric nanoparticles for breast Cancer therapy: A Comprehensive Review. Biointerface Research in Applied Chemistry, 11(4), 11151–11171. https://doi.org/10.33263/BRIAC114.1115111171
Molineux, G. (2003). Pegylation: Engineering improved biopharmaceuticals for oncology. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 23(8P2). https://doi.org/10.1592/phco.23.9.3S.32886
Tarentino, A. L., Phelan, A. W., & Plummer, T. H. (1993). 2-Iminothiolane: A reagent for the introduction of sulphydryl groups into oligosaccharides derived from asparagine-linked glycans. Glycobiology, 3(3), 279–285. https://doi.org/10.1093/GLYCOB/3.3.279
Shao, Y., Huang, W., Shi, C., Atkinson, S. T., & Luo, J. (2012). Reversibly crosslinked nanocarriers for on-demand drug delivery in cancer treatment. Therapeutic Delivery, 3(12), 1409–1427. https://doi.org/10.4155/tde.12.106
Chauhan, A. S. (2018). Dendrimers for drug delivery. Molecules, 23(4), 1–9. https://doi.org/10.3390/molecules23040938
Zheng, Y., Li, S., Weng, Z., & Gao, C. (2015). Hyperbranched polymers: Advances from synthesis to applications. Chemical Society Reviews, 44(12), 4091–4130. https://doi.org/10.1039/C4CS00528G
Wang, X., Li, C., Wang, Y., Chen, H., Zhang, X., Luo, C., … Wang, J. (2022). Smart drug delivery systems for precise cancer therapy. Acta Pharmaceutica Sinica. B, 12(11), 4098. https://doi.org/10.1016/J.APSB.2022.08.013
Courrier, H. M., Butz, N., & Vandamme, T. F. (2002). Pulmonary drug delivery systems: recent developments and prospects. Critical Reviews™ in Therapeutic Drug Carrier Systems, 19(4–5), 425–498. https://doi.org/10.1615/CRITREVTHERDRUGCARRIERSYST.V19.I45.40
Sutanto, F., Konstantinidou, M., & Dömling, A. (2020). Covalent inhibitors: A rational approach to drug discovery. RSC Medicinal Chemistry, 11(8), 876. https://doi.org/10.1039/D0MD00154F
Xiao, R. Z., Zeng, Z. W., Zhou, G. L., Wang, J. J., Li, F. Z., & Wang, A. M. (2010). Recent advances in PEG–PLA block copolymer nanoparticles. International Journal of Nanomedicine, 5(1), 1057. https://doi.org/10.2147/IJN.S14912
Eras, A., Castillo, D., Suárez, M., Vispo, N. S., Albericio, F., & Rodriguez, H. (2022). Chemical Conjugation in Drug Delivery systems. Frontiers in Chemistry, 10, 889083. https://doi.org/10.3389/fchem.2022.889083
Ezike, T. C., Okpala, U. S., Onoja, U. L., Nwike, C. P., Ezeako, E. C., Okpara, O. J., … Nwanguma, B. C. (2023). Advances in drug delivery systems, challenges and future directions. Heliyon, 9(6), e17488. https://doi.org/10.1016/J.HELIYON.2023.E17488
Pacheco, C., Baião, A., Ding, T., Cui, W., & Sarmento, B. (2023). Recent advances in long-acting drug delivery systems for anticancer drugs. Advanced Drug Delivery Reviews, 194, 114724. https://doi.org/10.1016/j.addr.2023.114724
Sung, Y. K., & Kim, S. W. (2020). Recent advances in polymeric drug delivery systems. Biomaterials Research, 24(1), 12. https://doi.org/10.1186/s40824-020-00190-7
Hong, L., Li, W., Li, Y., & Yin, S. (2023). Nanoparticle-based drug delivery systems targeting cancer cell surfaces. RSC Advances, 13(31), 21365–21382. https://doi.org/10.1039/D3RA02969G
Verma, V. S., Sakure, K., & Badwaik, H. R. (2017). Xanthan Gum a Versatile Biopolymer: Current status and future Prospectus in Hydro Gel Drug Delivery. Current Chemical Biology, 11(1), 10–20. https://doi.org/10.2174/2212796810666161110152815
Acknowledgements
One author wish to acknowledge DST FIST project Level-0 (SR/FST/College-2018-431-C) for providing infrastructural facility.
Author information
Authors and Affiliations
Contributions
All the authors have equal contributions to the reported study.
Corresponding authors
Ethics declarations
Ethical Approval
Not applicable.
Consent to Participation
All the authors had their consent for participation in the reported study.
Consent for Publication
All the authors had their consent for the publication of the reported study.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Verma, V.S., Pandey, A., Jha, A.K. et al. Polyethylene Glycol–Based Polymer-Drug Conjugates: Novel Design and Synthesis Strategies for Enhanced Therapeutic Efficacy and Targeted Drug Delivery. Appl Biochem Biotechnol (2024). https://doi.org/10.1007/s12010-024-04895-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s12010-024-04895-6