Abstract
Polymer-drug conjugates are nanosized drug delivery systems, which comprise several drug molecules covalently attached to a polymeric carrier. This chapter provides an overview of this technology in the context of drug delivery. Particular emphasis is given to different approaches and techniques used to synthesise and characterise polymer-drug conjugates. In the final part of the chapter current applications of this technology are also discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- High Performance Liquid Chromatography
- Drug Release
- Free Drug
- Amide Bond
- Nuclear Magnetic Resonance Spectroscopy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Materials Chemistry
1.1 Definition of Polymer-Drug Conjugates and General Background to This Technology
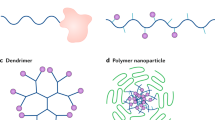
Polymer-drug conjugates are a drug delivery technology where a polymer carrier is used to improve the performance of a drug (e.g. improve drug selectivity towards the target site). Unlike other systems, such as liposomes or nanoparticles where the drug is physically entrapped within the carrier, in a polymer-drug conjugate the drug is covalently attached to the polymer via a biodegradable linker (Fig. 7.1).
The concept of conjugation of a drug to a polymeric carrier was first introduced in the 70s by Helmut Ringsdorf as a strategy to enhance the selectivity, cellular uptake and solubility of a drug (Ringsdorf 1975). Since then, extensive work has been carried out which has resulted in polymer-drug conjugates reaching clinical evaluation (Vasey et al. 1999; Seymour et al. 2009, also reviewed in Duncan 2006; Canal et al. 2011).
The rationale for conjugating a drug to a polymer stems from the fact that the biological behaviour of the drug can be significantly altered by increasing its molecular weight (MW). Covalent conjugation to a polymer results in:
-
Prolonged circulation time of the drug. The polymer can protect the conjugated drug from premature inactivation during its delivery to the site of action; in addition, the macromolecular size of the conjugate prevents the early elimination of the drug through renal filtration.
-
Restricted body distribution. An intravenously administered drug is generally able to diffuse throughout the body, with no selectivity towards the target tissue. On the other hand, the macromolecular size of a conjugate prevents extravasation of the drugs in areas where the vascular endothelium is continuous. In fact, conjugation to a polymer restricts drug access to those tissues where the vasculature presents fenestrations and gaps of appropriate size (>20 nm). The tumour tissue, for instance, is characterised by a defective vasculature which is permeable to the conjugate. This and other features (discussed in Sect. 7.4.1) make the tumour tissue an ideal target for polymer-drug conjugates.
-
Selective drug release. Polymer conjugation can also alter the cellular pharmacokinetics of the drug. Because of its size, the conjugate is taken up by cells exclusively by endocytosis, firstly into endosomes, then into lysosomes. The lysosomal compartment has two peculiar characteristics: an acidic pH (4–5) and a high concentration of proteolytic enzymes (e.g. cathepsin B). This unique environment can be turned into a useful trigger for drug release from the conjugate. Indeed, polymer-drug conjugates have been designed with biodegradable linkers either sensitive to acidic pH or selectively degraded by proteolytic enzymes. This allows the drug to be released exclusively intracellularly and to effectively reach its biological target (generally the nucleus and the DNA in case of anticancer drugs).
The biological behaviour of a polymer-drug conjugate is strongly affected by each of its constituents and by the overall physico-chemical properties of the system (e.g. water solubility). The next section will look at each component of a polymer-drug conjugate.
1.2 Composition of a Polymer-Drug Conjugate.
As previously described, a polymer-drug conjugate is constituted by three (to four) components: a drug, a polymeric carrier, a linker and, optionally, a targeting group. In this section we will look at each component individually.
1.2.1 Drug
The vast majority of the polymer-drug conjugates that have been proposed to date have been designed for application in cancer therapy (see Sect. 7.4). Therefore, most of the drugs used in polymer-drug conjugates are anticancer agents; examples include: doxorubicin, paclitaxel and camptothecin.
With the help of an example (doxorubicin) we are now going to look at what characteristics make a drug suitable for conjugation to a polymeric system (also summarised in Fig. 7.2).
Doxorubicin is a potent anticancer agent, used for the treatment of metastatic breast cancer (Paridaens et al. 2000). The main issue with the therapeutic use of doxorubicin is its cardiotoxicity, which is a result of the lack of selectivity of this drug (Jensen 2006). Such lack of selectivity makes it an ideal candidate for polymer conjugation, as the polymer will promote drug accumulation in the tumour tissue. The chemical structure of doxorubicin also makes it a suitable candidate for conjugation. In particular, this molecule contains a primary amino group and a hydroxyl group. Both these functional groups can be exploited for linking the drug onto a polymer (e.g. via formation of an amide bond or an ester bond for the amino group or hydroxyl group, respectively). In addition, doxorubicin absorbs UV–vis light and is inherently fluorescent. These are two favourable properties as the presence of the drug can be detected using appropriate instruments (see Sect. 7.3).
1.2.2 Polymer
Many polymeric carriers have been suggested for use within the context of polymer-drug conjugates. In particular, four of them have been tested clinically: N-(2-hydroxypropyl)-methacrylamide (HPMA) copolymers, polyethylene glycol (PEG), polyglutamic acid (PGA) and oxidised dextran (Duncan 2006).
With the help of an example (PGA) we are now going to look at what characteristics make a polymer suitable for use in a polymer-drug conjugate system (also summarised in Fig. 7.3).
PGA is a polymer constituted by units of glutamic acid linked together via amide bonds. PGA is water-soluble and this is an important characteristic for intravenous drug delivery as biological fluids, such as the blood, are essentially water-based systems.
PGA is biodegradable, which means that in biological systems it is degraded to smaller fragments. This is an advantage for a polymeric carrier as it ensures that the carrier is eliminated from the body after drug release. Non-biodegradable polymers, such as PEG, can also be used, but their size has to be such that allows excretion via the kidneys (typically lower than 40,000 Da).
Each monomer of PGA has a pendant side chain, which terminates with a carboxyl group. These carboxyl groups can be exploited for conjugation to a drug, for instance, to an amino group to produce an amide bond or to a hydroxyl group to produce an ester bond. All polymers suggested for use as a carrier need to have a functional group that allows conjugation to a drug. If a polymer has multiple conjugation sites (such as PGA), each polymer chain will be able to carry several drug molecules. In the case of PGA, each polymeric chain could carry one drug molecule per monomer (i.e. 200 drug molecules per chain, for 30,000 Da PGA). This property of a polymeric carrier (i.e. the ability to carry drug molecules) is called ‘loading capacity’. In general, a higher loading capacity is to be preferred, as less of the carrier needs to be used in order to administer a therapeutic dose of the drug.
Finally, PGA is non-toxic and non-immunogenic (i.e. does not stimulate an immune response). These are key properties, as toxicity from a drug delivery carrier would not be considered acceptable.
1.2.3 Linker
In a polymer-drug conjugate the linker is the part that connects the drug to the polymeric carrier. Many types of linkers have been suggested, which includes peptidyl linkers and pH-labile linkers (Duncan 2006).
With the help of an example (the peptidyl linker Gly-Phe-Leu-Gly) we are now going to look at what characteristics make a linker suitable for use in a polymer-drug conjugate system (also summarised in Fig. 7.4).
Early studies on a series of HPMA copolymer-doxorubicin conjugates compared different peptidyl linkers, including Gly-Phe-Leu-Gly. The conjugate containing this linker was then progressed for evaluation into clinical trials (Vasey et al. 1999; Seymour et al. 2009). Stability tests carried out in plasma showed that the linker was stable (i.e. did not release the drug) in these conditions. This was a positive finding, as a good linker needs to be stable in the blood to avoid premature drug release. Other studies carried out on a mixture of lysosomal enzymes (mimicking the environment found by the conjugate in the lysosomes) showed drug release in these experimental settings. Biodegradability at the target site is also an important characteristic as drug release is necessary to drug activity.
1.2.4 Targeting Group
The targeting group is the fourth (but optional) structural component of a polymer-drug conjugate. Its role is to actively direct the conjugate towards the desired tissue. With the help of an example (galactosamine) we are now going to look at what characteristics make a targeting group suitable for use in a polymer-drug conjugate (also summarised in Fig. 7.5).
Galactosamine is an amino sugar able to bind selectively to the hepatocyte galactose receptor, a liver-specific receptor (Ashwell and Harford 1982). The ability to bind to tissue-specific markers (which are generally proteins associated to a certain tissue and not expressed elsewhere in the body) is an essential requirement for a targeting group. In addition, galactosamine presents a primary amino group, which can be used for linking this molecule to the polymer (as for the conjugated drug). These features make galactosamine a suitable targeting group to be exploited in the context of drug delivery. Galactosamine was covalently bound to an HPMA copolymer-doxorubicin conjugate designed for the treatment of liver cancer (Seymour et al. 1991; Pimm et al. 1993; Julyan et al. 1999). This conjugate was investigated clinically (Phase I and Phase II) and clinical imaging confirmed preferential accumulation in the liver (Seymour et al. 2002).
In this chapter we have already discussed the ability of a conjugate to target the tumour tissue with a passive mechanism based on its physico-chemical properties (i.e. its molecular weight, see Sect. 7.1.1). For this reason, the targeting group is an optional component in a polymer-drug conjugate designed for anticancer therapy.
2 Polymer-Drug Conjugates Synthesis
2.1 Synthetic Strategies
There are two main synthetic approaches that can be used to produce a polymer-drug conjugate: polymer-analogous reaction and copolymerisation of appropriate monomers (Fig. 7.6).
-
Polymer-analogous reaction. This synthetic strategy starts with a polymeric precursor in which the sites of conjugation are chemically modified to increase their reactivity (e.g. a carboxylic acid converted into an ester containing an appropriate leaving group) and to produce a reaction with the drug (Fig. 7.6a).
-
Copolymerization of appropriate monomers. This approach involves two steps: (1) coupling of the drug to the monomer; (2) polymerization of such drug-monomer derivatives with the monomers, to yield the conjugate (Fig. 7.6b).
The copolymerisation strategy presents the advantage that, at least theoretically, drug loading can be increased or decreased by adjusting the ratio between the monomers containing the drug and the other monomers. However, the polymer-analogous reaction is by far the most commonly used approach, as it normally requires milder reaction conditions compared to those used in polymerisation reactions. Hence, with this strategy there is generally less of a chance to degrade the drug during the conjugation process.
Conjugation of a drug to a polymeric carrier can also be defined in relation to the position of the conjugation site within the polymer chain. This is largely driven by the chemical structure of the polymeric carrier used. Two types of conjugation can be identified: terminal conjugation and pendant chain conjugation (Fig. 7.7).
-
Terminal conjugation: this is typical of polymers with functional groups present only at the end termini (e.g. unmodified PEG). For unmodified linear polymers, this type of conjugation results in a conjugate with a low carrying capacity, as a maximum of two drug molecules can be carried by each polymeric chain. More recently, however, polymers with regular branching at the termini have been developed (dendronised systems) to accommodate additional drug molecules in each polymer chain (see Fig. 7.7a).
-
Pendant chain conjugation: this refers to the conjugation to polymers with suitable functional groups present along the chain (see Fig. 7.7b). This is the case with polymers such as the HPMA copolymer, where side chains are attached to the main polymeric backbone, or PGA that naturally contains a side carboxyl group per monomer and allows a theoretical maximum loading of one drug molecule per monomer. Pendant chain conjugation has the advantage that the loading capacity is typically higher than that achievable with terminal conjugation.
With regard to the actual conjugation reaction, the choice is primarily driven by the functional groups present on the drug and on the polymeric carrier, but standard synthetic reactions can be employed. For instance, an amino group present in the drug can be linked to a carboxylic acid group on the polymer after appropriate activation of the carboxylic acid group via standard coupling reactions (e.g. N,Nʹ-dicyclohexylcarbodiimide (DCC) or 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC) coupling).
2.2 Purification
Once the conjugation reaction has been carried out, the conjugate needs to be purified from reaction by-products and from residual reagents, as these might present unwanted biological activity (e.g. they might be toxic). Standard purification techniques routinely used for purifying small molecules can be applied to the purification of the conjugates (e.g. precipitation, filtration). In addition, as the conjugate and the reagents differ significantly in size, size-exclusion chromatography is typically used in this context.
One type of impurity that needs particular attention is residual, unreacted free drug, as it will have a different biological activity and a different pharmacokinetic profile compared to the conjugated drug. This aspect is further discussed in Sect. 7.3.1.
3 Polymer-Drug Conjugates Characterisation
After preparation, polymer-drug conjugates must be carefully characterised. Thorough characterisation prior to any testing is essential to correctly interpret biological behaviours observed for the conjugate. In addition, as conjugates progress into clinical trials, it is important to guarantee the reproducibility of their preparation and the overall quality of the final products. Because the drug is covalently attached to the polymeric carrier, polymer-drug conjugates cannot be treated simply as a new formulation of the drug (even if they carry a well-known and clinically established drug). In fact, these technologies are considered by the regulatory authorities as ‘new chemical entities’ (i.e. as completely new drugs) and, as such, they need to undergo extensive testing to ensure their safety and efficacy. Both European (i.e. EMA) and American (i.e. FDA) regulatory authorities have set the standards for the quality of medicines in order to guarantee their efficacy and safety.
3.1 Characterisation Parameters
Proof of conjugation. The initial characterisation of a polymer-drug conjugate includes finding evidence that a covalent bond between the drug and the polymer has been formed (i.e. that the drug is attached to the polymer and not physically ‘entrapped’ within the polymer). Several techniques have been used to achieve this purpose and, in many cases, different techniques have to be used in conjunction of one with the other (see Sect. 7.3.2).
Total drug content. When the formation of the conjugate is confirmed, it is essential to understand how much drug is bound to the polymer. The total drug content can be expressed in two different ways: (i) as the percentage in weight of the whole conjugate; (ii) as the percentage of functional groups contained in the polymer that have been conjugated to the drug. (i) and (ii) are strictly related but convey different information. In particular, (i) gives an immediate measure of total drug content. For example, a PGA-paclitaxel conjugate was synthesised that contained approximately 37 % w/w of paclitaxel (e.g. 100 mg of conjugate contain 37 mg of paclitaxel) (Li et al. 1998). Conversely, (ii) is often used to indicate how efficient a conjugation reaction was (e.g. 80 % of the functional groups available on a polymer reacted with the drug or, in other words, the drug loading was 80 % of the maximum theoretical loading). Different techniques can be used to assess the drug content of a conjugate, as described in more detail in Sect. 7.3.2.
Impurities and residual-free drug content. We have already discussed the importance of an accurate purification of the conjugate from excess reagents and reaction by-products (Sect. 7.2.2). One type of impurity that needs particular attention is residual, unreacted free drug. As the free drug will have biological activity and a different pharmacokinetic profile compared to the conjugated drug, removing it is particularly key. To this end, size-exclusion chromatography is the technique most frequently used, as the free and conjugated drug differ significantly in size. The content of residual-free drug is typically expressed as a percentage of the total drug content and, in general, the purification of the conjugate should aim to achieve levels below 1 %.
Size. Determining the size of the conjugate is very important, as this is arguably the key parameter that drives the distribution of the conjugate in the body and determines how quickly the conjugate (or the unloaded polymer) will be excreted from the body. However, it should be highlighted that most polymeric systems are polydisperse (i.e. polymers are constituted by a range of polymeric chains varying in length, depending on the number of monomers per chain). This means that most polymer-drug conjugates are polydispersed systems too. Therefore, the molecular weight stated is an average of the molecular weight of the various chains and should always be accompanied by the polydispersity value for that system.
3.2 Techniques Employed to Characterise Conjugates
To achieve the information described above, a variety of analytical techniques can be used.
3.2.1 Thin Layer Chromatography (TLC)
TLC is a very simple technique that is routinely used during conjugation reactions to obtain an indication of how the reaction is progressing. A sample from the reaction mixture is spotted onto a TLC plate and run with an appropriate mobile phase. Typically, the TLC plate is then viewed under a UV lamp (if, the drug absorbs at UV). Alternatively, specific stains are used to detect functional groups present in the drug and make the TLC spot visible (e.g. ninhydrin stain, which turns the spot pink in presence of compounds containing primary amino groups). The mobile phase can be modified to ensure that the free drug and the conjugated drug have different retention times (Fig. 7.8). As the reaction progresses, the drug starts to get detected at the retention factor of the polymer (see Fig. 7.8).
Schematic representation of how to monitor a conjugation reaction by TLC. In this example, the TLC plate is placed under an UV lamp. The drug (in D) can be detected by UV, while the polymer (in P) does not absorb UV light, therefore is not visible; lane (R) contains the reaction mixture (the change in colour of the spot on the baseline refers to the drug being conjugated to the polymer; as a consequence the spot of the free drug tends to disappear); lane (M) contains the mixture of the polymer and the drug in absence of activators of the reaction
3.2.2 UV–vis Spectroscopy
Many drugs have a chemical structure that absorbs light in the UV–vis region of the electromagnetic spectrum. As such, these drugs can be detected and quantified in solution by a UV–vis spectrophotometer. On the other hand, the most common polymers used in conjugation (PEG, PGA, HPMA copolymers) do not absorb UV–vis light. These represent very useful features when characterising a polymer-drug conjugate, as the UV–vis spectrum of the polymer is expected to change dramatically after conjugation. However, for a correct interpretation of the conjugate’s spectrum, it is important to remember the following considerations:
-
UV–vis is a useful technique to identify and quantify the total drug content of the conjugate, but it cannot normally discriminate between bound and free drug as, typically, both absorb at the same wavelength; therefore UV–vis spectroscopy alone is not a valid proof of conjugation and it becomes meaningful only when supported by other techniques.
-
Polymer conjugation often alters the extinction coefficient of a drug (i.e. the free drug and the conjugated drug might have different extinction coefficients; Vicent et al. 2005), which can lead to errors. In particular, if the drug content in a conjugate was estimated using a calibration curve of the free drug, this could result in an over- or under-estimation of the total drug content.
3.2.3 Nuclear Magnetic Resonance (NMR) Spectroscopy
NMR spectroscopy is a technique commonly used to prove that conjugation has occurred. The presence of signals belonging to the drug in the spectrum of the conjugate is not an indication of conjugation per se, as they might belong to the unbound drug. However, a shift in the resonance of the protons and carbons adjacent to the conjugation site is an indication that their electronic environment has changed and this might be due to conjugation. In addition, the sharp peaks typical of the spectrum of small molecules become broad after conjugation to macromolecules, as a consequence of the slower molecular tumbling of the polymeric chains. A shift in resonance combined with the broadening of the peaks represents an indication of successful conjugation of the drug.
In some cases the overlapping of crucial peaks does not allow a complete interpretation of the spectrum. In these cases, 2D NMR spectroscopic analyses represent a valid and powerful alternative to the usual spectrum. For instance, the nuclear overhauser effect spectroscopy (NOESY) and the total correlation spectroscopy (TOCSY) have been used to prove the formation of the amide bond between HPMA copolymer and doxorubicin (Pinciroli et al. 1997).
NMR spectroscopy can also be used to determine drug content within the conjugate. This can be achieved by relative integration of the signals from the drug and those from the polymeric backbone. This allows the calculation of a molecular ratio between drug molecules and polymer monomers, which can be converted into drug content expressed as percentage in weight.
3.2.4 Infrared Spectroscopy (IR)
IR is a technique very useful to identify functional groups. Polymer conjugation often results in the formation of new bonds (e.g. ester or amide bonds) between the drug and the polymer, which can be detected in an IR spectrum. A comparison of the spectrum of the conjugate with the spectra of the unbound drug and polymer can reveal the formation of the new bond. However, this might result in a challenging task when the newly formed bond is a functional group already present in the polymer. For example, PGA is constituted by monomers of glutamic acid joined together via amide bonds. If the drug is joined to the polymer via an amide bond, it might be difficult to discriminate which component of the IR signal is due to the amide bonds of the polymer and which is due to the conjugated drug. Conversely, formation of an amide bond in a PEG-based conjugate would be easier to detect as unmodified PEG does not contain this type of bond.
3.2.5 Matrix-Assisted Laser Desorption/Ionisation Time of Flight (MALDI-TOF)
MALDI-TOF analysis is a particular type of mass spectrometry that has been employed to characterise polymer-drug conjugates (Wu and Odom 1998). In particular, this technique can detect the shift in the mass of the conjugate due to conjugation with a drug. A mass increase in the polymer, which matches the added mass due to the presence of the drug, constitutes strong proof of conjugation. Therefore, MALDI-TOF is useful in the context of confirming covalent linkage and also in determining the molecular weight and the polydispersity of the conjugate.
3.2.6 Gel Permeation Chromatography (GPC)
GPC is a type of size-exclusion chromatography in which compounds are separated according to their size (or, more precisely, to the volume they occupy in solution, i.e. hydrodynamic volume): bigger molecules elute from the column faster (have shorter retention times) than smaller molecules. After conjugation to a drug, the hydrodynamic volume of a polymer may change significantly depending on the type of drug used (Fig. 7.9). The conjugate could adsorb molecules of water within its structure and adopt an extended conformation, which would result in a shorter retention time compared to the free polymer. On the other hand, the conjugate may adopt a more compact conformation and display a smaller hydrodynamic volume than that of the corresponding free polymer, which would result in a prolonged retention time.
3.2.7 High Performance Liquid Chromatography (HPLC)
HPLC is a technique widely employed in the synthesis and characterisation of polymer-drug conjugates. The use of HPLC within the context of polymer-drug conjugates relies on the fact that the free drug and the conjugated drug are likely to interact differently with the stationary phase and the mobile phase, and therefore are likely to elute from an HPLC column at different times. Preparatory HPLC can be used to isolate and purify the conjugate from the free drug. Columns for preparative HPLC are relatively large (internal diameter: 5–20 mm) and allow loading of large amounts of a compound (up to milligrams of compounds). In a similar manner, analytical HPLC can be used to check that the conjugate is free from unconjugated drug or to quantify the total drug content and the content of residual-free drug. Columns for analytical HPLC are smaller (internal diameter typically 4.6 mm) and allow loading of small amounts of compound (up to few micrograms).
In addition, HPLC is often employed during stability studies, to verify that the conjugate is stable, and no drug is released from the conjugate during storage. Finally, HPLC can also be used to measure drug release under different physiological conditions. For example, samples from the blood or the urine of a patient can be analysed by HPLC to detect the stability of the conjugate in biological fluids and the rate of drug release.
3.2.8 Small Angle Neutron Scattering (SANS)
SANS is a technique that has been used to investigate the behaviour of the conjugates in solution (Paul et al. 2007). This type of analysis can provide key information about the conformation of the polymer (e.g. radius of gyration). A comparison between the scattering behaviour of different conjugates can also provide information about structure-activity relationships.
4 Application of Polymer-Drug Conjugates
This section describes the different therapeutic areas to which the concept of polymer-drug conjugates has been applied (Sects. 7.4.1 and 7.4.2). A recent development in the field (the use of polymer-drug conjugates to deliver drug combinations) is also reported (Sect. 7.4.3). The final section (Sect. 7.4.4) provides an update on the current status of polymer-drug conjugates.
4.1 Treatment of Cancer
The vast majority of polymer-drug conjugates that have been developed to date and that have undergone clinical evaluation are designed for application to cancer treatment. The tumour tissue represents an ideal target for polymer-drug conjugates. Firstly, it is characterised by a leaky vasculature, which allows extravasation of the conjugate from the capillaries feeding the tumour tissue to the tumour tissue itself. Conversely, the large size of the conjugate prevents extravasation of this system into normal tissues. In addition, the tumour tissue is also characterised by a poor lymphatic system, which is unable to effectively clear the extracellular fluid. As a consequence, the conjugate is retained in the tumour tissue for longer. The combination of these two factors (leaky vasculature and poor drainage) has been called ‘enhanced permeability and retention (EPR) effect’ and is a phenomenon typical of solid tumours (Matsumura and Maeda 1986; reviewed in Maeda et al. 2013).
The EPR effect results in the passive accumulation of macromolecules into the tumour tissue and makes polymer conjugation an ideal strategy to selectively target this disease. Unconjugated drugs are unable to take advantage of the EPR effect for the following reasons: (1) they are low MW molecules, able to diffuse throughout the body with no selectivity (i.e. size exclusion) for a specific tissue; (2) their clearance from the biological fluids does not rely on the lymphatic system, therefore they do not accumulate in the tumour tissue.
As the EPR effect promotes an improved selectivity towards the tumour tissue, the toxicity of polymer-drug conjugates compared to their parent-free drug is generally lower. For example, the maximum tolerated dose (a parameter indicating the toxicity of a therapeutic agent) of free doxorubicin is 60–80 mg/m2 (Muzykantov and Torchilin 2003), while that of an HPMA copolymer-doxorubicin is 320 mg/m2 (Vasey et al. 1999).
Within the context of cancer treatment, many established anticancer agents (e.g. paclitaxel and doxorubicin) have been proposed in the form of polymer-drug conjugates. More recently, the concept of polymer-drug conjugates has also been applied to experimental anticancer agents that had shown promising anticancer activity, but that had failed to progress into the market due to toxicity or other unfavourable properties. For instance, the antiangiogenic agent TNP-470 has been conjugated to an HPMA copolymer with a view to maintaining the anticancer activity while reducing its toxicity (TNP-470 is neurotoxic when administered as a free drug) (Satchi-Fainaro et al. 2004, 2005).
4.2 Polymer-Drug Conjugates in Diseases Other Than Cancer
Traditionally polymer-drug conjugates have been developed for the treatment of cancer, but recently the versatility of this approach has been exploited also in other therapy areas. Representative examples of different therapeutic areas to which the concept of polymer-drug conjugates has been applied are described here.
Rheumatoid arthritis is a chronic inflammatory disease of the joints. Chronic inflammation is associated with leaky vasculature and enhanced vascular permeability. Therefore, the ability of macromolecules to selectively extravasate in correspondence of the inflamed tissue has supported the development of polymer-drug conjugates specific for this disease (e.g. PEG-dexamethasone, Liu et al. 2010; linear cyclodextrin-α-methylprednisolone, Hwang et al. 2008).
Leishmaniasis is a protozoal infection transmitted by the bite of a certain type of sand fly. The visceral form of the disease is caused by the migration of the parasite to vital organs and is often lethal. In order to improve the treatment of the disease, two HPMA copolymer conjugates of the anti-leishmanial drug 8-aminoquinoline have been developed (with and without the targeting moiety mannose) and have shown promising results in pre-clinical studies (Roy et al. 2012; Nan et al. 2001, 2004).
Polymer-drug conjugation is a relatively new concept and its development has focused on the use of well-known drugs, with the aim of proving the advantages of the new approach by comparison. With conjugation becoming a more established approach, innovative drugs targeting new molecular mechanisms have also been conjugated. For instance, it is now clear that cardiovascular and neurodegenerative disorders are often associated with increased apoptosis (i.e. the mechanism of programmed cell death) (Haunstetter and Izumo 1998; Mattson 2000). Consequently, anti-apoptotic agents have been investigated to limit inappropriate apoptosis and arrest the progression of the disease (Malet et al. 2006). One of these drugs (called ‘peptoid 1’) was shown to achieve only limited efficacy in cellular models because of its poor ability to permeate the cell membrane. A lysosomotropic delivery of the drug was then needed to improve its performance and polymer conjugation was the strategy selected. Indeed, conjugation to PGA resulted in enhanced uptake and intracellular trafficking of the anti-apoptotic drug (Vicent and Perez-Paya 2006).
4.3 Combination Therapy
Many diseases (e.g. cancer and HIV) are treated with cocktails of drugs rather than with a single therapeutic agent. The overall aim of this type of therapeutic regimen (combination therapy) is to maximise efficacy while decreasing toxicity. For instance, in the case of anticancer treatment, different chemotherapeutic agents are administered jointly over repetitive treatment cycles. The development of drug delivery platforms able to carry multiple types of drugs could allow the simultaneous administration of the drugs in combination, resulting in improved patient compliance and simplified therapies. To this purpose, in recent years, polymer-drug conjugates carrying two types of drugs have been developed and tested pre-clinically. Examples of this approach are reported in Table 7.1.
4.4 Current Status of Polymer-Drug Conjugates
Polymer-drug conjugates have shown promise for cancer therapy, but to date, no polymer-drug conjugate has reached the market. However, an increasing number of polymer-drug conjugates have entered and are progressing through clinical evaluation. Table 7.2 summarises the polymer-drug conjugates that have undergone clinical evaluation.
5 Conclusions
Polymer-drug conjugates are a drug delivery technology based on the covalent conjugation of drug molecules to a polymeric carrier. Conjugation to a polymer prolongs the circulation time of the drug, increases its selectivity for the target tissue (e.g. the tumour tissue) and allows selective drug release. The development of a polymer-drug conjugate requires a careful design and an accurate choice of its components (polymer, linker, drug and optional targeting moiety). Optimised synthetic conditions and extensive characterization are necessary to make a reproducible and ‘high quality’ polymer-drug conjugate. The application of this concept has mainly focused on the treatment of cancer, with encouraging clinical results. While the first marketed polymer-drug conjugate is still awaited, research is ongoing to further develop this concept. Progress in polymer chemistry is leading to innovative polymer architectures and new molecular targets are being investigated to extend this technology to new applications.
Problem Box
Question 1.
Calculate the drug loading (expressed as % w/w) for a linear polymer-drug conjugate and for its dendronised derivative (schematic representation of the structures and the MWs of the various components are reported in figure below). Briefly discuss the importance of drug loading within the context of polymer-drug conjugates.
Important note. In your calculation assume that conjugation of the drug to the polymer or to the branching unit results in the loss of a molecule of water (loss of an H from the drug and loss of an OH from the polymer/branching unit). Addition of each branching unit also results in a loss of a molecule of water.

Answer 1.
Step 1. Calculate the % w/w of the linear polymer-drug conjugate.
-
(a)
Calculate the drug content:
(543.98 × 2) − 2 = 1,085.96
-
(b)
Calculate the total weight of the conjugate
(543.98 × 2) + 3,500 − (18 × 2) = 4,551.96
-
(c)
Calculate the % w/w:
(1085.96/4551.96) * 100 = 23.8%
Step 2. Calculate the % w/w of the dendronised polymer-drug conjugate.
-
(a)
Calculate the drug content:
(543.98 × 8) − 8 = 4,343.84
-
(b)
Calculate the total weight of the conjugate
(543.98 × 8) + 3,500 + (161 × 6) − (18 × 14) = 8,565.84
-
(c)
Calculate the % w/w:
(4,343.84/8,565.84) × 100 = 50.7 %
Question 2.
The anticancer agent paclitaxel has been considered a promising candidate for delivery via polymer-drug conjugate technology. Indicate what characteristics of this drug molecule make it suitable for applications with this technology.
Answer 2.
(a) Paclitaxel is an anticancer drug with toxicity due to non-selective delivery (conjugation to a polymer can improve selectivity); (b) paclitaxel is poorly water-soluble and has to be administered in a oil-based formulation (Cremophor), which has a certain toxicity; conjugation to a polymer can improve solubility in biological fluids; (c) paclitaxel contains an hydroxyl group (this can be used for conjugation via, for instance, an ester linkage); (d) paclitaxel has a short plasma half-life (which can be prolonged by conjugation to a polymer).
References
Albain KS, Belani CP, Bonomi P, O’Byrne KJ, Schiller JH, Socinski M (2006) PIONEER: a phase III randomized trial of paclitaxel poliglumex versus paclitaxel in chemotherapy-naïve women with advanced-stage non-small-cell lung cancer and performance status of 2. Clin Lung Cancer 7:417–419
Ashwell G, Harford J (1982) Carbohydrate-specific receptors of the liver. Annu Rev Biochem 51:531–554
Beeram M, Rowinsky EK, Hammond LA, Patnaik A, Schwartz GH, de Bono JS, Forero L, Forouzesh B, Berg KE, Rubin EH, Beers S, Killian A, Kwiatek J, McGuire J, Spivey L, Takimoto CH (2002) A phase I and pharmacokinetic (PK) study of PEG-paclitaxel in patients with advanced solid tumors. Proc Am Soc Clin Oncol 21:405
Borad MJ, Hamm JT, Rosen LS, Jameson GS, Utz J, Mulay M, Eldon M, Dhar S, Acosta L, Von Hoff DD (2008) Phase I dose finding and pharmacokinetic study of NKTR-102 (PEGylated irinotecan): early evidence of anti-tumor activity. J Clin Oncol 26:13518
Calvo E, Hoch U, Maslyar DJ, Tolcher AW (2010) Dose-escalation phase I study of NKTR-105, a novel pegylated form of docetaxel. J Clin Oncol 28:TPS160
Campone M, Rademaker-Lakhai JM, Bennouna J, Howell SB, Nowotnik DP, Beijnen JH, Schellens JHM (2007) Phase I and pharmacokinetic trial of AP5346, a DACH–platinum–polymer conjugate, administered weekly for three out of every 4 weeks to advanced solid tumor patients. Cancer Chemother Pharmacol 60:523–533
Canal F, Sanchis J, Vicent MJ (2011) Polymer-drug conjugates as nano-sized medicines. Curr Opin Biotechnol 22:894–900
Clementi C, Miller K, Mero A, Satchi-Fainaro R, Pasut G (2011) Dendritic poly(ethylene glycol) bearing paclitaxel and alendronate for targeting bone neoplasms. Mol Pharm 8:1063–1072
Danhauser-Riedl S, Hausmann E, Schick HD, Bender R, Dietzfelbinger H, Rastetter J, Hanauske AR (1993) Phase I clinical and pharmacokinetic trial of dextran conjugated doxorubicin (AD-70, DOX-OXD). Invest New Drugs 11:187–195
Daud A, Garrett C, Simon GR, Munster P, Sullivan D, Stromatt S, Allevi C, Bernareggi B (2006) Phase I trial of CT-2106 (polyglutamated camptothecin) administered weekly in patients with advanced solid tumors. In: ASCO annual meeting proceedings. J Clin Oncol 24:2015
Duncan R (2006) Polymer conjugates as anticancer nanomedicines. Nat Rev Cancer 6:688–701
Greco F, Vicent MJ, Gee S, Jones AT, Gee J, Nicholson RI, Duncan R (2007) Investigating the mechanism of enhanced cytotoxicity of HPMA copolymer–Dox–AGM in breast cancer cells. J Control Release 117:28–39
Guo Z, Wheler JJ, Naing A, Mani S, Goel S, Mulcahy M, Gamza F, Longley C, Buchbinder A, Kurzrock R (2008) Clinical pharmacokinetics (PK) of EZN-2208, a novel anticancer agent, in patients (pts) with advanced malignancies: a phase I, first-in-human, dose-escalation study. J Clin Oncol 26:2556
Hamm JT, Richards D, Ramanathan RK, Becerra C, Jameson G, Walling J, Gribben D, Dhar S, Eldon M, Von Hoff D (2009) Dose-finding study of NKTR-102 in combination with cetuximab. J Clin Oncol 27:13503
Haunstetter A, Izumo S (1998) Apoptosis: basic mechanisms and implications for cardiovascular disease. Circ Res 82:1111–1129
Homsi J, Simon GR, Garret CR, Springett G, De Conti R, Chiappori AA, Munster PN, Burton MK, Stromatt S, Allievi C, Angiuli P, Eisenfeld A, Sullivan DM, Daud AI (2007) Phase I trial of poly-L-glutamate camptothecin (CT-2106) administered weekly in patients with advanced solid malignancies. Clin Cancer Res 13:5855–5861
Hwang J, Rodgers K, Oliver JC, Schluep T (2008) Alpha-methylprednisolone conjugated cyclodextrin polymer-based nanoparticles for rheumatoid arthritis therapy. Int J Nanomed 3:359–371
Jensen BV (2006) Cardiotoxic consequences of anthracycline-containing therapy in patients with breast cancer. Semin Oncol 33:S15–S21
Julyan PJ, Seymour LW, Ferry DR, Daryani S, Boivin CM, Doran J, David M, Anderson D, Christodoulou C, Young AM, Hesslewood S, Kerr DJ (1999) Preliminary clinical study of the distribution of HPMA copolymers bearing doxorubicin and galactosamine. J Control Release 22:281–290
Kostkova H, Etrych T, Rihova B, Ulbrich K (2011) Synergistic effect of HPMA copolymer-bound doxorubicin and dexamethasone in vivo on mouse lymphomas. J Bioactive Compatible Polym 26:270–286
Langer CJ, O’Byrne KJ, Socinski MA, Mikhailov SM, Lesniewski-Kmak K, Smakal M, Ciuleanu TE, Orlov SV, Dediu M, Heigener D, Eisenfeld AJ, Sandalic L, Oldham FB, Singer JW, Ross HJ (2008) Phase III trial comparing paclitaxel poliglumex (CT-2103, PPX) in combination with carboplatin versus standard paclitaxel and carboplatin in the treatment of PS 2 patients with chemotherapy-naıve advanced non-small cell lung cancer. J Thorac Oncol 3:623–630
Li C, Yu DF, Newman RA, Cabrai F, Stephens LC, Hunter N, Milas L, Wallace S (1998) Complete regression of well-established tumors using a novel water-soluble poly(L-glutamic acid)-paclitaxel conjugate. Cancer Res 58:2404–2409
Liu XM, Quan LD, Tian J, Laquer FC, Ciborowski P, Wang D (2010) Synthesis of click PEG-dexamethasone conjugates for the treatment of rheumatoid arthritis. Biomacromolecules 11:2621–2628
Maeda H, Nakamura H, Fang J (2013) The EPR effect for macromolecular drug delivery to solid tumours: improvement of tumour uptake, lowering of systemic toxicity, and distinct tumour imaging in vivo. Adv Drug Deliv Rev 65:71–79
Malet G, Martín AG, Orzáez M, Vicent MJ, Masip I, Sanclimens G, Ferrer-Montiel A, Mingarro I, Messeguer A, Fearnhead HO, Pérez-Payá E (2006) Small molecule inhibitors of Apaf-1-related caspase-activation that control mitochondrial-dependent apoptosis. Cell Death Differ 13:1523–1532
Matsumura Y, Maeda H (1986) A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumour agent SMANCS. Cancer Res 46:6387–6392
Mattson MP (2000) Apoptosis in neurodegenerative disorders. Nat Rev Mol Cell Biol 1:120–129
Meerum Terwogt JM, ten Bokkel Huinink WW, Schellens JH, Schot M, Mandjes IA, Zurlo MG, Rocchetti M, Rosing H, Koopman FJ, Beijnen JH (2001) Phase I clinical and pharmacokinetic study of PNU166945, a novel water-soluble polymer-conjugated prodrug of paclitaxel. Anticancer Drug 12:315–323
Miller K, Eldar-Boock A, Polyak D, Segal E, Benayoun L, Shaked Y, Satchi-Fainaro R (2011) Antiangiogenic antitumor activity of HPMA copolymer-paclitaxel-alendronate conjugate on breast cancer bone metastasis mouse model. Mol Pharm 8:1052–1062
Muzykantov VR, Torchilin VP (2003) Biomedical aspects of drug targeting. Springer, New York
Nan A, Nanayakkara D, Larry A, Walker LA, Yardley V, Croft SL, Ghandehari H (2001) N-(2-hydroxypropyl)methacrylamide (HPMA) copolymers for targeted delivery of 8-aminoquinoline antileishmanial drugs. J Control Release 77:233–243
Nan A, Croft SL, Yardley V, Ghandehari H (2004) Targetable watersoluble polymer-drug conjugates for the treatment of visceral leishmaniasis. J Control Release 94:115–127
Neumann TA, Van Patischen H, Marcantonio A, Song D, Morrison P, Eldon MA (2007) Evaluation of single oral doses of NKTR118 (PEG-naloxol) as a peripheral opioid antagonist (POA): a double-blind placebo-controlled study in healthy male subjects. J Clin Pharmacol 47:1210
O’Brien M, Oldham E (2005) Paclitaxel poliglumex vs. gemcitabine or vinorelbine for the treatment of performance status (PS) 2 patients with chemotherapy-naïve advanced non-small cell lung cancer (NSCLC): the STELLAR 4 phase III study. In: 2005 ASCO annual meeting, p 1122
O’Brien M, Socinski MA, Popovich AY, Bondarenko IN, Tomova A, Bilynskyi BT, Hotko YS, Ganul VL, Kostinsky IY, Eisenfeld AJ, Sandalic L, Oldham FB, Bandstra B, Sandler AB, Singer JW (2008) Randomized phase III trial comparing single-agent paclitaxel poliglumex (CT-2103, PPX) with single-agent gemcitabine or vinorelbine for the treatment of PS 2 patients with chemotherapy-naive advanced non-small cell lung cancer. J Thorac Oncol 3:728–734
Oliver JC, Yen Y, Synold TW, Schluep T, Davis M (2008) A dose-finding pharmacokinetic study of IT-101, the first de novo designed nanoparticle therapeutic in refractory solid tumors. J Clin Oncol 26:14538
Paridaens R, Biganzoli L, Bruning P, Klijn JGM, Gamucci T, Houston S, Coleman R, Schachter J, Van Vreckem A, Sylvester R, Awada A, Wildiers J, Piccart M (2000) Paclitaxel versus doxorubicin as first-line single-agent chemotherapy for metastatic breast cancer: a European organization for research and treatment of cancer randomized study with cross-over. J Clin Oncol 18:724–733
Pasut G, Greco F, Mero A, Mendichi R, Fante C, Green RJ, Veronese FM (2009) Polymer-drug conjugates for combination anticancer therapy: investigating the mechanism of action. J Med Chem 52:6499–6502
Paul A, Vicent MJ, Duncan R (2007) Using small-angle neutron scattering to study the solution conformation of N-(2-hydroxypropyl)methacrylamide copolymer-doxorubicin conjugates. Biomacromolecules 8:1573–1579
Paz-Ares L, Ross H, O’Brien M, Riviere A, Gatzemeier U, Von Pawel J, Kaukel E, Freitag L, Digel W, Bischoff H, Garcìa-Campelo R, Iannotti N, Reiterer P, Bover I, Prendiville J, Eisenfeld AJ, Oldham FB, Bandstra B, Singer JW, Bonomi P (2008) Phase III trial comparing paclitaxel poliglumex vs docetaxel in the second-line treatment of non-small-cell lung cancer. Br J Cancer 98:1608–1613
Pimm MV, Perkins AC, Duncan R, Ulbrich K (1993) Targeting of N-(2-hydroxypropyl) methacrylamide copolymer-doxorubicin conjugate to the hepatocyte galactose-receptor in mice: visualisation and quantification by gamma scintigraphy as a basis for clinical targeting studies. J Drug Target 1:125–131
Pinciroli V, Rizzo V, Angelucci F, Tatò M, Vigevani A (1997) 1H NMR characterization of methacrylamide polymer conjugates with the anti-cancer drug doxorubicin. Magn Reson Chem 35:2–8
Rademaker-Lakhai JM, Terret C, Howell SB, Baud CM, de Boer RF, Pluim D, Beijnen JH, Schellens JHM, Droz JP (2004) A phase I and pharmacological study of the platinum polymer AP5280 given as an intravenous infusion once every 3 weeks in patients with solid tumors. Clin Cancer Res 10:3386–3395
Ringsdorf H (1975) Structure and properties of pharmacologically active polymers. J Polym Sci 51:135–153
Roy P, Das S, Auddy RG, Mukherjee A (2012) Biological targeting and drug delivery in control of Leishmaniasis. J Cell Anim Biol 6:73–87
Santucci L, Mencarelli A, Renga B, Pasut G, Veronese F, Zacheo A, Germani A, Fiorucci S (2006) Nitric oxide modulates proapoptotic and antiapoptotic properties of chemotherapy agents: the case of NO-pegylated epirubicin. FASEB J 20:765–767
Satchi-Fainaro R, Puder M, Davies JW, Tran HT, Sampson DA, Greene AK, Corfas G, Folkman J (2004) Targeting angiogenesis with a conjugate of HPMA copolymer and TNP-470. Nat Med 10:255–261
Satchi-Fainaro R, Mamluk R, Wang L, Short SM, Nagy JA, Feng D, Dvorak AM, Dvorak HF, Puder M, Mukhopadhyay D, Folkman J (2005) Inhibition of vessel permeability by TNP-470 and its polymer conjugate, caplostatin. Cancer Cell 7:251–261
Sausville EA, Garbo LE, Weiss GJ, Shkolny D, Yurkovetskiy AV, Bethune C, Ramanathan RK, Fram RJ (2010) Phase I study of XMT-1001 given IV every 3 weeks to patients with advanced solid tumors. J Clin Oncol 28:13121
Schoemaker NE, van Kesteren C, Rosing H, Jansen S, Swart M, Lieverst J, Fraier D, Breda M, Pellizzoni C, Spinelli R, Porro MG, Beijnen JH, Schellens JHM, Bokkel Huinink WW (2002) A phase I and pharmacokinetic study of MAG-CPT, a water-soluble polymer conjugate of camptothecin. Br J Cancer 87:608–614
Scott LC, Yao JC, Benson AB, Thomas AL, Falk S, Mena RR, Picus J, Wright J, Mulcahy MF, Ajani JA, Evans TRJ (2009) A phase II study of pegylated-camptothecin (pegamotecan) in the treatment of locally advanced and metastatic gastric and gastro-oesophageal junction adenocarcinoma. Cancer Chemother Pharmacol 63:363–370
Segal E, Pan H, Benayoun L, Kopečková P, Shaked Y, Kopeček J, Satchi-Fainaro R (2009) Enhanced anti-tumor activity and safety profile of targeted nano-scaled HPMA copolymer-alendronate-TNP-470 conjugate in the treatment of bone malignances. Biomaterials 32:4450–4463
Seymour LW, Ulbrich K, Wedge SR, Hume IC, Strohalm J, Duncan R (1991) N-(2-hydroxypropyl)methacrylamide copolymers targeted to the hepatocyte galactose-receptor: pharmacokinetics in DBA2 mice. Br J Cancer 63:859–866
Seymour LW, Ferry DR, Anderson D, Hesslewood S, Julyan PJ, Poyner R, Doran J, Young AM, Burtles S, Kerr DJ (2002) Hepatic drug targeting: phase I evaluation of polymer-bound doxorubicin. J Clin Oncol 15:1668–1676
Seymour LW, Ferry DR, Kerr DJ, Rea D, Whitlock M, Poiner R, Boivin C, Hesslewood S, Twelves C, Blackie R, Schatzlein A, Jodrell D, Bissett D, Calvert H, Lind M, Robbins A, Burtles S, Duncan R, Cassidy J (2009) Phase II studies of polymer-doxorubicin (PK1, FCE28068) in the treatment of breast, lung and colorectal cancer. Int J Oncol 34:1629–1636
Soepenberg O, de Jonge MJA, Sparreboom A, de Bruin P, Eskens FALM, de Heus G, Wanders J, Cheverton P, Ducharme MP, Verweij J (2005) Phase I and pharmacokinetic study of DE-310 in patients with advanced solid tumors. Clin Cancer Res 11:703–711
Vasey PA, Kaye SB, Morrison R, Twelves C, Wilson P, Duncan R, Thomson AH, Murray LS, Hilditch TE, Murray T, Burtles S, Fraier D, Frigerio E, Cassidy J (1999) Phase I clinical and pharmacokinetic study of PK1 [N-(2-hydroxypropyl)methacrylamide copolymer doxorubicin]: first member of a new class of chemotherapeutic agents-drug-polymer conjugates. Clin Cancer Res 5:83–94
Vicent MJ, Perez-Paya E (2006) Poly-l-glutamic acid (PGA) aided inhibitors of apoptotic protease activating factor 1 (Apaf-1): an antiapoptotic polymeric nanomedicine. J Med Chem 49:3763–3765
Vicent MJ, Greco F, Nicholson RI, Paul A, Griffiths PC, Duncan R (2005) Polymer therapeutics designed for a combination therapy of hormone-dependent cancer. Angew Chem Int Ed 44:4061–4066
Webster L, Dhar S (2009) NKTR-118 significantly reverses opioid-induced constipation poster. In: 20th AAPM annual clinical meeting
Wu KJ, Odom RW (1998) Characterizing synthetic polymers by MALDI MS. Anal Chem News Features 1:456–461
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Fante, C., Greco, F. (2013). Polymer-Drug Conjugates. In: Uchegbu, I., Schätzlein, A., Cheng, W., Lalatsa, A. (eds) Fundamentals of Pharmaceutical Nanoscience. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9164-4_7
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9164-4_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9163-7
Online ISBN: 978-1-4614-9164-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)