Abstract
Natural substances have been demonstrated to be an unrivalled source of anticancer drugs in the present era of pharmacological development. Plant-based substances, together with their derivatives through analogues, play a significant character in the treatment of cancer by altering the tumor microenvironment and several signaling pathways. In this study, it was investigated whether the natural drugs, formononetin (FN) and sulforaphane (SFN), when combined, assess the efficacy of inhibiting cervical cancer cell proliferation by impeding the PI3K/Akt/mTOR signaling pathway in HeLa cells. The cells were treated with the combination of FN and SFN (FN + SFN) in various concentrations (0–50 µM) for 24 h and then analyzed for various experiments. The combination of FN + SFN-mediated cytotoxicity was analyzed by MTT assay. DCFH-DA staining was used to assess the ROS measurement, and apoptotic changes were studied by dual (AO/EtBr) staining assays. Protein expressions of cell survival, cell cycle, proliferation, and apoptosis protein were evaluated by flow cytometry and western blotting. Results showed that the cytotoxicity of FN and SFN was determined to be around 23.7 µM and 26.92 µM, respectively. Combining FN and SFN causes considerable cytotoxicity in HeLa cells, with an IC50 of 21.6 µM after 24-h incubation. Additionally, HeLa cells treated with FN and SFN together showed increased apoptotic signals and considerable ROS generation. Consequently, by preventing the production of PI3K, AKT, and mToR-mediated regulation of proliferation and cell cycle-regulating proteins, the combined use of FN + SFN has been regarded as a chemotherapeutic medication. Further research will need to be done shortly to determine how effectively the co-treatment promotes apoptosis to employ them economically.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is the second most powerful cause of death, based on the report from GLOBOCAN 2020, which predicted that, globally, cancer-related cases and deaths will be approximately 19.3 million annually and 10 million in the year 2020 correspondingly. Cervical cancer is the third most general factor in death in women globally out of all cancers. As one of the most common gynecological malignancies, cervical cancer will affect over six million women in 2020 and cause 342,000 deaths [1]. Cervical cancer begins to develop earlier in life. Unavoidable attention must be paid to it [2, 3].
Human papillomavirus (HPV) infection that persists is a contributing factor of cervical cancer, which infects the cervix’s epithelial cells. High-risk HPV causes uncontrollably multiplying infected cells by interfering with the processes of cell division, replication, and communication once it infects cervical cells [4]. Viral oncoproteins E6 and E7 suppress TP53 and RB1 proteins, changing DNA repair processes, apoptosis, and the cell cycle. Eventually, an HPV infection with oncogenic HPV types can persist and transform healthy cells into abnormal cells, if the body’s immune system is unable to eradicate the virus, ultimately leading to cancer [5]. Further, multiple investigations have revealed that extremely dangerous HPV infection, particularly HPV16 and HPV18, which are responsible for above 70% of metastatic cervical malignancies, is linked to about 90% of cervical carcinomas. The main reasons and optimal environment for HPV infection are dysfunction of the cervical-vaginal microbiota and an inflammatory reaction [6]. Additionally, as studies progress, bacteria might also have a role in cervical cancer. They also enhance the likelihood of chronic HPV infection and they cause local inflammatory responses [7, 8].
According to Small et al. [9], cisplatin-based therapy, brachytherapy, and surgical excision are frequently used techniques to treat those diagnosed with cervical carcinoma. Development of neoadjuvant therapies is needed [9]. Due to the dismal prognosis, however, treatment resistance and high toxicity are equally concerning [10]. Therefore, it is necessary to discover novel treatment molecules that suppress carcinogenesis to improve chemotherapy results and upsurge the general survival probability of people with cervical cancer.
Tumor suppressor p16INK4a is up-regulated by HPVs, and this is linked to the PI3K/Akt/mTOR pathway. When there is a strong chance that HPVs will inactivate the pRb protein, cervical cancer frequently expresses p16INK4a at high levels [11]. Cervical cancer HPV16 infection is linked to S6K phosphorylation. Moreover, the regulation of cell survival, growth, and proliferation is significantly influenced by the phosphatidylinositol 3-kinase (PI3K)/AKT/mammalian target of the rapamycin (mTOR) signaling pathway. Human malignancies frequently include abnormalities in the main PI3K/AKT/mTOR signaling pathway modules. The PI3K/Akt/mTOR circuit is one of many signaling cascades that control numerous cellular and molecular processes that are essential during the initiation, invasion, as well as metastasis of tumors [12]. Elevation of the signaling pathway consisting of PI3K and Akt has been interconnected to an assortment of human tumors, including cancers of the breast, ovary, endometrial, and malignant glioma, according to some research. Additionally, activation of the PI3K/Akt pathway is associated with a subpar response in cervical cancer [13]. According to this study, cervical cancers could be treated by targeting the PI3K/Akt/mTOR signaling system using a combination of dual natural drugs. Natural compounds originating from plants may be exploited as potential novel therapies for cancer. Phytochemicals can combine with a variety of molecular targets in tumor tissues and increase the effectiveness of conventional anticancer medications.
As indicators for cancer diagnosis, combinatorial epigenetic markings are becoming more significant [14]. To synergistically activate tumor suppressors, the best dietary combination that can lower the level of DNA methylation and deacetylation levels could be chosen [15]. As a result of their success in treating as well as avoiding cancer, combination strategies are growing in prominence in the field of cancer research. A quantifiable metric known as the Combination Index (CI) has been used to demonstrate that, in many situations, the combination of two or more drugs is better than the combination of chemicals operating alone [16, 17]. The Combination Index evaluates the extent of drug synergism or antagonistic interactions for a certain endpoint of impact assessment [18]. Too frequently, very large dosages of one compound are used to test for efficiency, which may result in side effects. Combining lower doses of the individual drugs may improve their chemopreventive capability and translational effects.
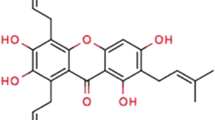
More and more natural compounds are being researched as potential novel medications [19, 20]. The isoflavone compound formononetin (C16H12O4) is mostly found in red clovers and the Chinese plant Astragalus membranaceus. The substance goes into a category of 4-position methoxy-substituted 7-hydroisoflavones. By modifying several signaling channels, formononetin induces cell death and the cell cycle, inhibits cell invasion, and suppresses tumor-promoting qualities both in vitro and in vivo. Through a synergistic effect, the use of formononetin in combination with other chemotherapeutic medications (such as bortezomib, sunitinib, epirubicin, doxorubicin, temozolomide, and metformin) increases its anticancer potency. Before this study, it showed that the bulk of the trials investigating formononetin’s anticancer properties used concentrations between 0.3 and 53.7 µg/ml (or 1–200 µM). Formononetin displays an IC50 between 10 and 300 µM, demonstrating its effectiveness in suppressing a variety of cancer cells [21]. Formononetin has an anticancer effect; however, the exact mechanism is still unknown. So, the structural alteration of formononetin was crucial in the search for stronger anti-tumor drugs based on the natural substance.
An isothiocyanate (ITC) molecule called sulforaphane is generated from cruciferous plants. Its effectiveness against a variety of cancer types has been demonstrated in several trials. Sulforaphane acts therapeutically in an assortment of ways, including cell cycle arrest in the G2/M and G1 phases to reduce cell growth and detoxify oxidants and carcinogens by blocking phase I metabolic enzymes [22]. The stimulation of apoptosis, cell cycle arrest, and inhibition of angiogenesis and metastasis are only a few of the anticancer properties that SFN has been related to [23, 24]. According to multiple studies, adding SFN to a common chemotherapeutic drug (such as paclitaxel, docetaxel, or gemcitabine) boosts apoptosis. The fact that numerous articles have addressed how sulforaphane works to prevent cancer [25,26,27]. Even thorough, evaluation of sulforaphane’s synergistic effects and delivery methods is absent. However, there is no scientific proof that a combination of FN and SFN has an anticancer effect on cervical cancer especially in target-specific pathways. In order to investigate their potential synergistic chemopreventive effect against cervical cancer cells, FN and SFN were employed simultaneously in the current investigation. This work focused on molecular processes involved in the PI3K/AKT pathways, which may reflect the suppression at the initial phase of cervical cancer development.
Materials and Methods
Reagents
The RPMI 1640 medium, tetrazolium bromide (MTT), fetal bovine serum (FBS), and phosphate-buffered saline (PBS) were obtained from Lonza Pvt Ltd. in China, along with other cell culture ingredients. Dimethyl sulfoxide (DMSO), formononetin (FN), and sulforaphane were purchased from Merck Sigma Aldrich Co. Ltd., St. Louis, USA. We obtained anti-PI3K, AKT, mTOR, cyclin-D1, PCNA, and CDK6 antibodies from Santa Cruz Biotechnology in the USA. The remaining scientific reagents and solutions had all molecular and sterile grades.
Cell Culture and Maintenance
HeLa, a cell line from a patient with cervical cancer, normal cervical cell line H8 were grown in Dulbecco’s modified Eagle’s medium (DMEM) media supplemented with L-glutamine and balanced salt solution (BSS) adjusted to contain glucose, 0.1 mm non-essential amino acids, 1 mm sodium pyruvate, and 1% penicillin/streptomycin/amphotericin B at 37 °C in a humid incubator with 5% CO2.
Cell Viability
After treatment with different concentrations of FN and SFN as well as chosen concentrations of the combination drugs, cell viability was assessed using the MTT test [28]. HeLa and H8 cells (1 × 104/ well) were trypsinized, placed in a 96-well plate, and given the night to adhere. They were subsequently given treatment for 24 h with specific chemicals. Following that, 10 µL of MTT was added to all wells, and the plates underwent another 4 h of incubation at 37 °C. The formazan crystals were removed from the MTT-containing medium, liquefied in 100 µL of DMSO, and added to every well, and the plates were then stirred at 37 °C for 10 min. A microplate reader was then used to detect the absorbance of the colored solution at 550 nm. The following formula was used to compute the cell viability:
Drug Combinations Assay
The effectiveness of combinatorial therapies and their interactions were evaluated using CompuSyn software [18]. Combination Index (CI) values under 1 indicate drug synergism, over 1 indicates drug additive activity, and more than 1 indicates drug antagonistic behavior.
Morphological Analysis
The morphological changes of HeLa cells were examined using a combination of FN and SFN. The 6-well culture plates with seeded cells were incubated for 24 h. A trinocular inverted phase contrast microscope (Lawrence & Mayo) was used to examine the cells after incubation to check for alterations in their morphological changes.
Dual Staining with Ethidium Bromide and Acridine Orange (AO/EB)
The proportion of cell apoptosis in HeLa cells treated with FN and SFN was assessed using AO/EtBr staining [29]. In a nutshell, HeLa cells (1 × 104 per well) were planted, and the cells were incubated at 37 °C for 24 h. Cells were then treated with FN and SFN and permissible to incubate for 24 h at 37° C. The treated cells were then stained for 10 min with 100 µg/mL of AO/EtBr stain at a 1:1 ratio as part of the treatment step. The amount of apoptotic cell death in the treated cells was quantified using a fluorescence microscope (3501, Lawrence and Mayo India Pvt, Ltd).
DAPI Staining
To analyze the HeLa cells treated with FN and SFN, the nuclei were stained with DAPI (4,6-diamidino-2-phenylindole), and then fluorescence image analysis (blue fluorescence in living cells) was performed. After 24 h of incubation, the HeLa cells were seeded at a density of 1 × 104 cells/mL on a sample that had been sterilized. The cell morphology was then stained with DAPI and examined under a fluorescence microscope (3501, Lawrence and Mayo India Pvt, Ltd).
Intracellular Generation of ROS
By using DCFH-DA staining on HeLa cells treated with FN and SFN, the level of reactive oxygen species (ROS) production in the control group was determined [30, 31]. In a nutshell, DMEM was used to seed HeLa cells (1 × 104), which were subsequently exposed to FN and SFN for 24 h at 37 °C. After the treatment period, 10 µL of DCFH-DA dye was added to each well and left to stain the cells for 1 h. A fluorescence microscope (3501, Lawrence and Mayo India Pvt, Ltd) was then used to assess the level of ROS formation in control and treated cells.
Measurement of Apoptosis by Flow Cytometry
HeLa cells (1 × 104) were sown in every well and incubated for 24 h at 37 °C in the groups receiving treatment FN and SFN that received medium supplements. HeLa cells were separated using three times diluted trypsin before being twice-washed in PBS and resuspended in the binding buffer in an icy setting. A commercial apoptosis detection kit (Ebioscience, USA) was used to detect the addition of FITC and PI, which completed the technique.
Cell Cycle Arrest Analysis
HeLa cells (1 × 104) were seeded in each well, and after 24 h of treatment with FN and SFN, the cells were trypsinized, recovered, and washed twice in ice-cold PBS. The cells were then fixed by adding 70% ice-cold ethanol and were then incubated at 4 °C overnight. Cells were then exposed to PI and ribonuclease A for 30 min. To count the number of cells at each step of the cell cycle, a flow cytometer was employed.
Western Blot Analysis
Western blotting was employed to examine the effects of the FN and SFN combination on the apoptotic and anti-apoptotic proteins in the treated and control cells [32]. HeLa cells were given 24 h of treatment with the selected drug combinations of FN and SFN in a 100-mm culture dish. After removing the medium, PBS was used to repeatedly wash the cells. After that, lysis buffer was applied to the cells for more than 20 min. The supernatant was then centrifuged and utilized to extract the proteins from the cells. The same quantity of protein was electrophoretically separated on a 12% SDS-polyacrylamide gel from each concentration of the sample. Following each transfer, the proteins were blocked for an hour with 10% skim milk in water before being released. After washing with PBS containing 0.1% Tween-20, the primary antibodies against PI3K, AKT, mTOR, cyclin-D1, PCNA, and CDK6 as well as β-actin were added at a v/v ratio of 1:1000. After overnight incubation at 4 °C, the primary antibodies were removed by washing, and the secondary antibodies were added. The protein bands were visible after 1 h of incubation at room temperature.
Analysis of Statistics
The mean and standard deviation are used to represent the results from three distinct experiments. To assess the significance of the difference between the untreated and treated groups, the GraphPad Prism program V6.0 (GraphPad Software 215 Inc., San Diego, CA, USA) was used using the t-test (p < 0.05).
Results
Effects of Treatment with FN and SFN on the Viability of HeLa Cell Line
The effects of the combination of FN and SFN on the viability of cervical cancer and normal cervical cells were assessed using the MTT (3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide) test. The effects of various doses of the therapy combination on HeLa cancer cell and normal H8 cell lines are depicted in Fig. 1a. The impact of FN and SFN on cervical cancer cells was investigated in both solo therapy and combo. We detected a dose-related diminution in the proliferation of treated cancer cells when compared to the standard and independent therapies; this effect was also found to be stronger when drug combinations were administered. Table 1 and Fig. 1 display the viability of cells at the chosen as well as treated dosages, whereas the combination of FN and SFN did not exhibit any appreciable alteration in the viability of normal H8 cells (Fig. 1b). Furthermore, the crystal violet assay, which is illustrated in Fig. 1c, was used to study the combination treatment of FN- and SFN-related cell proliferation. Crystal violet staining is more pronounced in control cells, indicating a high level of cell proliferation. However, cervical cancer cell’s rate of multiplication was dramatically reduced by the combination of FN and SFN treatment.
a Cytotoxicity study of FN and SFN against a HeLa cells and b H8 cells. Cell viability was examined using the MTT assay; subsequently, the cells had been treated for 24 h. The presented data were the means ± SD. Compared to the untreated group, *P < 0.05. c The combination of FN and SF-treated HeLa cells were stained with crystal violet. The studies were done in triplicate
Evaluation of Drug Interactions
The Combination Index (CI) was calculated using the CompuSyn program. In cervical cancer cell lines, it was discovered that the doses of 10 µM, 20 µM, and 30 µM FN and SFN simultaneously decreased cellular viability. The CI indices in certain of the combinations are displayed in Table 2. The value of CI > 1 indicates that there is antagonism between the two compounds. The values of CI = 1 and < 1 suggest that there is synergy among the two components. The CI value in HeLa cells is in the region of synergism at 10 µM FN and 10 µM SFN (CI 0.5), whereas at 30 µM FN and 20 µM SFN, the CI values indicate significant synergism (CI 0.57). We consequently reached the decision to continue using based on the IC50 values for our additional studies to investigate their impact at the molecular level.
Morphological Analysis
Using a phase contrast microscope, the morphological examination of HeLa cells was evaluated, and the effectiveness of delivering compounds at various concentrations was examined. As can be observed in Fig. 2, the control cells have morphological appearances which are regular, whereas those receiving treatment have undergone considerable morphological alterations that include cell contraction, blebbing, as well as separation from the exterior. In the treatment groups with larger concentrations, or in a concentration-reliant way of combinatorial treatment, these alterations were found to be more substantial. As a result, it has been demonstrated that the combination of FN and SFN had a dose-dependent ameliorative effect on cervical cancer.
Activation of Apoptosis by Combination of FN and SFN
Here, we used AO/EtBr staining to show how the interaction of FN and SFN affects the capacity of cervical cancer cells to undergo apoptosis. AO/EtBr labelling is a popular method for viewing chromatin abridgement during apoptosis under a fluorescent microscope. The apoptotic cells in HeLa cells received treatments with FN, SFN, and a combination of FN and SFN for 24 h, according to fluorescence microscopy (Fig. 3). The nucleus of the control cell fluoresced consistently green. Fluorescent microscopy, on the other hand, demonstrated that the treated HeLa’s nucleus structure was irregular as a result of a loss of membrane integrity. In formulations where cells received both FN and SFN treatment, apoptosis bodies, involving nuclear constriction and bulging, were observed as red-orange bodies. Therefore, the results of the current investigation showed that the combination of FN and SFN treatment had superior anti-tumor effects on cervical carcinoma cells in a concentration-based manner. The ratio of apoptotic cells was 74.45, 76.23, and 87.46% respectively at the various concentrations (10, 20, and 30 µM/mL) of the FN- and SFN-treated groups (Fig. 3b).
a The cells were stained with AO/EtBr to check the apoptosis stage with a combination of FN and SFN. b The bar diagram represents the % apoptosis in control, FN, SFN, and combination uses of FN + SFN-treated cells. White arrows indicate live cells, dashed arrows show apoptosis. Magnification bar, 50 μm
DAPI Staining
Additionally, DAPI staining was used to examine nuclear fragmentation as a marker of FN and SFN combination therapy (Fig. 4). The outcome shown in Fig. 4 illustrates how the combination treatment of FN and SFN caused nuclear disintegration and condensation. DAPI staining in control cells had decreased intensity at an excitation wavelength of 488 nm, whereas combination therapy cells displayed greater intensity, indicating the influence of FN and SFN in breaking down DNA in a dose-dependent way. Therefore, it has been demonstrated that these responses have simultaneously increased with the combination treatment of FN and SFN, as shown in Fig. 4.
HeLa cells treated with FN and SFN at various doses and control nuclei stained with DAPI. Untreated control cells display less strong blue coloration and spherical nuclei. Cells that had been exposed to both FN and SFN exhibited nuclear fragmentation and significantly stronger blue emission light in apoptotic cells (indicated by arrow). Scale bar, 50 μm
Production of Significant ROS by the Combination of FN and SFN
DCFH-DA staining was used to measure the generation of ROS by HeLa cells following FN and SFN therapy. Over 24 h, HeLa cells were detectable by FN and SFN in combination in a dose-dependent manner. HeLa significantly increased ROS production and fluorescence intensity (Fig. 5a). The amount of green fluorescence significantly increased after being exposed to FN and SFN for 24 h, as shown in (Fig. 5a); the ROS levels in these cells were calculated to be 50 (control), 190, 210, and 270, respectively (Fig. 5b). After receiving treatment with both FN and SFN, HeLa cells produced more ROS, and this increase was dose-dependent. These findings demonstrated the HeLa cells’ innate apoptotic signaling pathways.
Using 2,7-dichlorofluorescein diacetate labelling, it was possible to study in HeLa cells the effects of both FN and SFN on the formation of intracellular ROS. a Fluorescence microscopic image demonstrating the effect of FN, SFN, and FN + SFN on the generation of intracellular ROS (indicated by arrow). b The percentage of reactive oxygen species (ROS) generation was found using a spectrofluorometer. For comparison to the control group, the statistics are the mean and standard deviation of triplicates with a *p < 0.05 significance level. Scale bar, 50 μm
Combination of FN- and SFN-Induced Apoptosis Along with Cell Cycle Arrest in HeLa Cancer Cells
The percentage of apoptotic and necrotic cells shown in Fig. 6 was calculated using an apoptosis kit that included FITC-labelled annexin V and PI Staining. The comparison of the HeLa cells treated with control and combination FN and SFN and the results showed substantial differences. FN, SFN, and FN with SFN showed apoptotic cell percentages of 14.26 ± 2.3 and 24.49 ± 1.6%, and 30.41 ± 1.8, respectively. Our research showed that combination therapy of FN and SFN improved the number of cells in the Q2 phase of apoptosis. It was found that when HeLa cells were treated with a mixture of FN and SFN, the proportion of apoptotic cells increased in respective concentration manner. This investigation was conducted to find out the effectiveness of composites FN and SFN in cell cycle inhibition. The findings of the cell cycle analysis performed on the treated cells are displayed in Fig. 7. The cells were dispersed across the untreated control in the S and G1 phases of the cell cycle. Because of this, at higher concentrations (55.48%), the proportion of cells in the G0/G1 phase had suggestively decreased subsequently co-treating with FN and SFN at different concentrations. These findings show how the FN and SFN interfere with the cell cycle’s S-phase, perhaps causing cancer cell death.
Analysis of the cell cycle using flow cytometry. a FITC and Annexin V-stained flow cytometry were used to assess the apoptotic cells connected to FN and SFN therapy. b The proportion of cells in the G0/G1 phase is shown on a histogram; the information is from three associated investigations. Employing the Student’s t-test, (*p < 0.05 **p < 0.01) was compared to the control
Combination of FN and SFN Impede PI3K/AKT/mTOR Phosphorylation in HeLa Cells
To comprehend the impact of FN and SFN combination therapy on the phosphorylation of PI3K/AKT/mTOR in HeLa cells, western blot analysis was performed (Fig. 8). HeLa cells severely decreased the phosphorylation of cell survival indicators (PI3K, AKT, and mTOR) when exposed to the combination of FN and SFN (10, 20, 30 µM) for 24 h. These findings showed that FN and SFN together suppress PI3K/AKT/mTOR signaling in HeLa cells (Fig. 8a, b). Furthermore, when FN and SFN were used in conjunction, the overexpression of cell cycle-directing proteins such as cyclin-D1, PCNA, and CDK6 in HeLa cells was severely suppressed (Fig. 8c, d). Thus, by inhibiting or down-regulating the PI3K/AKT/mTOR signaling pathway, the co-treatment of FN and SFN on HeLa cells has synergistically inhibited cell propagation and promoted apoptosis, suggesting that this novel combination could be a promising potential therapeutic tactic for the management of cervical cancer.
Effect of FN + SFN on HeLa cells’ PI3K/AKT/mTOR pathway. a Western blotting tests on the combination FN + SFN therapy caused the expression of p-PI3K, p-AKT, and p-mTOR in HeLa cells. b PI3K/AKT/mTOR densitometric measurements were evaluated using the Image Studio software. β-actin expression is regarded as a housekeeping gene to ensure that proteins are loaded equally. The mean ± SD of three separate sets of data was used as a representation for the variables. **p < 0.01 and *p < 0.05 compared to the untreated group. c Western blotting tests on the effects of FN + SFN treatment on the expression of the proteins cyclin-D1, PCNA, and CDK6 in HeLa cells. d The image Studio program evaluated the densitometric study of the proteins mentioned previously. The equal loading of proteins was confirmed by the production of the housekeeping gene—actin. Three different experiments’ mean and standard deviation data were evaluated. *p < 0.05 and *p < 0.05 after associated to the control group
Discussion
Globally, cervical carcinoma continues to be one of the main causes of significant morbidity and mortality in women. Chemotherapy can help cervical cancer patients live longer, but it also increases drug resistance and has harmful side effects and consequences that put patients through a lot of pain. The use of natural substances produced by plants, such as alkaloids, flavonoids, phenols, and terpenoids, as a novel anticancer therapy for cervical cancer has garnered interest. The natural flavonoids found in FN and SFN are shown to have therapeutic benefits on the growth and spread of several malignancies. Increasing evidence suggests that dysregulation of numerous signaling pathways that encourage proliferating, prevent apoptosis, and trigger metastasis is linked to the development and spread of many malignancies, including cervical cancer [33]. Identification of prognostic and predictive biomarkers is required for risk categorization. The PI3K/Akt/mTOR (phosphatidylinositol 3-kinase/protein kinase B/mammalian target of rapamycin) pathway is frequently abnormal in cervical carcinoma, suggesting that it can be a possible target for therapy for the cure of this malignancy. It could also be used as an innovative biomarker in the evaluation of the risk of creating cervical carcinoma [12, 34]. In this work, we discovered that combinations of natural medications, such as FN and SFN, reduced cell development and caused cell death in cervical cancer, helping to establish a realistic therapy efficacy against the disease.
Therapy with an individual agent is not recommended over combination therapy including multiple therapeutic agents, each of which has a unique mechanism of action [35]. The numerous processes for cell survival are targeted by combination therapy, which promotes synergism and offers a viable remedy for tumor heterogeneity and drug resistance [36, 37]. According to numerous researches, sulforaphane boosts the effectiveness of medications and has a synergistic impact when given along with other drugs [36, 38,39,40,41]. Further, formononetin acts as an isoflavone derived from A. membranaceus which can promote tumor metastasis, inhibit cell cycle progression, and anti-angiogenesis. Additionally, it has been indicated to possess tumor-suppressive qualities in instances involving breast, colorectal, and lung cancer [42]. The above outcomes were shown to be associated with our results when given as a single therapy. Our findings further show that although FN and SFN each exhibit anti-carcinogenic characteristics on their own [41, 43, 21, 44], when delivered together, their efficacy is marginally stronger with a lower concentration. In the current investigation, it was shown that FN and SFN co-treatment, when compared to a single treatment, synergistically boosted the induction of apoptosis and inhibited growth in HeLa cells in vitro.
Inhibiting apoptosis is necessary for tumor development. Researcher’s interest in the mechanisms driving apoptosis-mediated cell death, which is linked to a number of human illnesses, has increased recently [45]. According to DAPI staining, cervical cancer cells exposed to a combination of FN and SFN showed a significant amount of blue fluorescence, but control calls exhibited a very low level of blue fluorescence. These findings demonstrated that the combination of FN and SFN significantly worsened nuclear damage in HeLa cells. Employing the AO/EtBr dye and a dual staining method, the apoptotic response of the combination of FN and SFN against HeLa was investigated. The AO stain could be accessible to live cells (green), in contrast to EtBr, which leaves cell debris stained with a reddish-orange color. The combined use of FN and SFN promoted apoptosis in the cervical cancer cell line, as evidenced by the red intensity fluorescence of the combination-treated cells being greater than that of control cells. Genistein and sulforaphane are effective in preventing breast cancer cells in previous studies [43], while formononetin significantly inhibits cervical cancer cells by reducing the expression of the MYC protein and inhibiting STAT3 activation via the JAK1/STAT3 pathway [44].
One of the most important organelles for controlling cell death is the mitochondria, which also includes other apoptosis-related markers. ROS, sometimes referred to as free radicals, are extremely active molecules with unattached valence shell electrons that cause a lot of oxidative damage to the cell [46, 47]. Elevated ROS concentrations are thought to be the primary cause of cell death. Additionally, the production of ROS in cancer cells is one of the ways through which the combination of FN and SFN has an anticancer impact. To calculate the quantities of intracellular ROS, fluorescence intensities of FN and SFN might be combined. According to the results of the ROS experiment, HeLa cells co-treated with FN and SFN are known to create more ROS when compared to the control group.
Many different proteins have been suggested to play a significant part in metastatic malignancies. The current work discovered an innovative compound that serves as a significant anticancer target by preferentially destroying cancer cells in HeLa cells by blocking the PI3K/AKT/mTOR signaling pathway [48]. Furthermore, because distinct PI3K isoforms play distinctly different roles in cellular signaling, proliferation, and neoplastic transformation, targeting one isoform through removal will impact downstream signaling in its own right [49]. In this instance, FN and SFN together dramatically reduced the expression of p-PI3K, p-AKT, and p-mTOR in the HeLa cancer cell line in comparison to the control. AKT contains multiple downstream targets which could play a role in transforming tumors and is the main modulator of PI3K-initiated signaling [50]. Once Akt is phosphorylated, mTOR is activated. Moreover, p-AKT and p-mTOR were found in 50% and 53% of adenocarcinomas, accordingly, based on expression evaluation of activating AKT and mTOR in patients who had cervix cancer [51]. Therefore, the combination of FN and SFN significantly reduced the expression of p-AKT in all HeLa cancer cell lines in a dose-responsive manner. This additionally clarifies why considerable inhibition of PI3K/AKT/mTOR boosted apoptosis promoted by the combination of FN and SFN in the cervical cancer cell line. Inhibition of p-AKT induced by the combination of FN + SFN on HeLa was noticeable.
Given that the PI3K/AKT/mTOR pathway is known to promote cell cycle progression [52]. Many different proteins, such as cyclins, CDKs, and CDKis, control the cell cycle [53]. It inspired us to investigate the cyclin expression defined in the current work, which ultimately found that FN + SFN caused cell cycle arrest by inhibiting the levels of cyclins D1 and CDK6 in HeLa cells, indicating that these kinds of proteins have been implicated in the development of the cell cycle in the cervical cancer cell line used. All things considered, these findings suggest that cyclin expression reductions have a role in the PI3K/AKT-mediated G0/G1 arrest. Crucially, suppression of cyclins and PCNA mediates the combination of FN- and SFN-induced cell cycle arrest, which could therefore lead to a reduction in CDK enzyme activity. We demonstrated the fact that strong repression of the PI3K/AKT/mTOR pathway can encourage apoptosis and impede the growth of tumors by controlling the expression of cell cycle regulatory proteins. This suggests that the combined use of FN and SFN may be a valuable cancer prevention therapeutic prospective applicant.
Conclusion
FN and SFN together form an effective combinatorial regimen that can improve cervical cancer’s translational chemopreventive capacity, according to the current study’s result. The combination of FN and SFN therapy had an anticancer impact on cervical cancer in vitro for the first time owing to our work. By inhibiting the cell cycle and triggering caspase-mediated intrinsic apoptosis, the combination of FN and SFN significantly decreased the viability of cervical cancer cells. After reducing the expression of cyclin-D1, PCNA, and CDK6 proteins, FN and SFN therapy down regulated the PI3K, AKT, and mTOR signaling pathways, which had an anticancer impact on cervical cancer. Therefore, by inducing cell death, the combination of FN and SFN offers promise as an effective chemopreventive strategy for preventing cervical carcinogenesis. Indeed, FN and SFN combination treatment might be used in clinical medicine with more studies to create regulated doses.
Data Availability
The data generated and the materials used in the study are available with the corresponding author and available on reasonable request.
References
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. C Ca: A Cancer Journal for Clinicians, 71, 209–249.
Zhou, Z. W., Long, H. Z., Xu, S. G., Li, F. J., Cheng, Y., Luo, H. Y., & Gao, L. C. (2022). Therapeutic effects of natural products on cervical cancer: Based on inflammatory pathways. Frontiers in Pharmacology, 13, 899208.
Olusola, P., Banerjee, H. N., Philley, J. V., & Dasgupta, S. (2019). Human papilloma virus-associated cervical cancer and health disparities. Cells, 8, 622.
Xu, B., Chotewutmontri, S., Wolf, S., Klos, U., Schmitz, M., Dürst, M., & Schwarz, E. (2013). Multiplex identification of human papillomavirus 16 DNA integration sites in cervical carcinomas. PloS One, 8(6), e66693.
Guan, P., Howell-Jones, R., Li, N., Bruni, L., de Sanjose, S., Franceschi, S., & Clifford, G. M. (2012). Human papillomavirus types in 115,789 HPV-positive women: A meta-analysis from cervical infection to cancer. International Journal of Cancer, 131(10), 2349–2359.
Zhou, Z. W., Long, H. Z., Cheng, Y., Luo, H. Y., Wen, D. D., & Gao, L. C. (2021). From microbiome to inflammation: The key drivers of cervical cancer. Frontiers in Microbiology, 12, 767931.
Golais, F., & Mrázová, V. (2020). Human alpha and beta herpesviruses and cancer: Passengers or foes? Folia Microbiol (Praha), 65, 439–449.
Sudomová, M., Berchová-Bímová, K., Marzocco, S., Liskova, A., Kubatka, P., & Hassan, S. T. S. (2021). Berberine in human oncogenic herpesvirus infections and their linked cancers. Viruses, 13, 1014.
Small, W., Jr., Bacon, M. A., Bajaj, A., Chuang, L. T., Fisher, B. J., Harkenrider, M. M., et al. (2017). Cervical cancer: A global health crisis. Cancer, 123, 2404–2412.
Kamran, S., Sinniah, A., Abdulghani, M. A. M., & Alshawsh, M. A. (2022). Therapeutic potential of certain terpenoids as anticancer agents: A scoping review. Cancers (Basel), 14, 1100. https://doi.org/10.3390/cancers14051100
Haręża, D. A., Jacek, R., & Wilczyński. (2022). Human papillomaviruses as infectious agents in gynecological cancers. Oncogenic Properties of Viral Proteins International Journal of Molecular Sciences, 23, 1818.
Afsane Bahrami, M., Hasanzadeh, S. M., Hassanian, S., ShahidSales, M., Ghayour-Mobarhan, G. A., Ferns, & Amir, A. (2017). The potential value of the PI3K/Akt/mTOR signaling pathway for assessing prognosis in cervical cancer and as a target for therapy. Journal of Cellular Biochemistry, 118, 4163–4169.
Schwarz, J. K., Payton, J. E., Rashmi, R., Xiang, T., Jia, Y., Huettner, P., Rogers, B. E., Yang, Q., Watson, M., & Rader, J. S. (2012). Pathway-specific analysis of gene expression data identifies the PI3K/Akt pathway as a novel therapeutic target in cervical cancer. Clinical Cancer Research, 18(5), 1464–1471.
Murrell, A. (2016). What lies beneath the epigenetic signatures associated with breast cancer and how do we find out? In Proceedings of the UK Breast Cancer Research Symposium, London, UK, 22–23.
Park, J. H., Kim, S. H., Lee, M. S., & Kim, M. S. (2017). Epigenetic modification by dietary factors: Implications in metabolic syndrome. Molecular Aspects of Medicine, 54, 58–70.
Tahir, A. A., Sani, N. F. A., Murad, N. A., Makpol, S., Ngah, W. Z. W., & Yusof, Y. A. M. (2015). Combined ginger extract & gelam honey modulate Ras/ERK and PI3K/AKT pathway genes in colon cancer HT29 cells. Nutrition Journal, 14, 31.
Kotecha, R., Takami, A., & Espinoza, J. L. (2016). Dietary phytochemicals and cancer chemoprevention: A review of the clinical evidence. Oncotarget, 7, 52517.
Chou, T. C. (2010). Drug combination studies and their synergy quantification using the Chou-Talalay method. Cancer Research, 70, 440–446.
Han, X., Cui, Z. Y., Song, J., Piao, H. Q., Lian, L. H., & Hou, L. S. (2019). Acanthoic acid modulates lipogenesis in nonalcoholic fatty liver disease via FXR/LXRs-dependent manner. Chemico-Biological Interactions, 311, 108794.
Li, X., Zhang, Y., Jin, Q., Xia, K. L., Jiang, M., & Cui, B. W. (2018). Liver kinase B1/AMP-activated protein kinase-mediated regulation by gentiopicroside ame liorates P2 × 7 receptor-dependent alcoholic hepatosteatosis. British Journal of Pharmacology, 175, 1451–1470.
Tay, K., C, Tan, L. T., Chan, C. K., Hong, S. L., Chan, K. G., & Yap, W. H. (2019). Formononetin: A review of its anicancer potentials and mechanisms. Frontiers in Pharmacology, 10, 820.
Kamal, M. M., & Nazzal, S. (2018b). Novel sulforaphane-enabled selfmicroemulsifying delivery systems (SFN-SMEDDS) of taxanes: Formulation development and in vitro cytotoxicity against breast cancer cells. International Journal of Pharmaceutics, 536(1), 187–198.
Tian, G., Li, Y., Cheng, L., Yuan, Q., Tang, P., Kuang, P., & Hu, J. (2016). The mechanism of sulforaphene degradation to different water contents. Food Chemistry, 194, 1022–1027.
Geng, Y., Zhou, Y., Wu, S., Hu, Y., Lin, K., Wang, Y., & Wu, W. (2017). Sulforaphane induced apoptosis via promotion of mitochondrial fusion and ERK1/2-mediated 26s proteasome degradation of novel pro-survival bim and upregulation of bax in human non-small cell lung cancer cells. Journal of Cancer, 8(13), 2456–2470.
Kim, S. H., Park, H. J., & Moon, D. O. (2017). Sulforaphane sensitizes human breast cancer cells to paclitaxel-induced apoptosis by downregulating the NF–κB signaling pathway. Oncology Letters, 13(6), 4427–4432.
Burnett, J. P., Lim, G., Li, Y., Shah, R. B., Lim, R., Paholak, H. J., McDermott, S. P., Sun, L., Tsume, Y., Bai, S., & Wicha, M. S. (2017). Sulforaphane enhances the anticancer activity of taxanes against triple negative breast cancer by killing cancer stem cells. Cancer Letters, 394, 52–64.
Tomooka, F., Kaji, K., Nishimura, N., Kubo, T., Iwai, S., Shibamoto, A., Suzuki, J., Kitagawa, K., Namisaki, T., Akahane, T., & Mitoro, A. (2023). Sulforaphane potentiates gemcitabine-mediated anti-cancer effects against intrahepatic cholangiocarcinoma by inhibiting HDAC activity. Cells, 12(5), 687.
Wang, S., Jiang, K., Muthusamy, R., Kalaimani, S., Selvababu, A. P., Balupillai, A., Narenkumar, J., Jeeva, J., & Jeevakaruniyam, S. (2022). Protosappanin-B suppresses human melanoma cancer cell growth through impeding cell survival, inflammation and proliferative signaling pathways. Process Biochemistry, 122, 78–85.
Karthikeyan, R., Kanimozhi, G., Prasad, N. R., Agilan, B., Ganesan, M., & Srithar, G. (2018). Alpha pinene modulates UVA-induced oxidative stress, DNA damage and apoptosis in human skin epidermal keratinocytes. Life Sciences, 212, 150–158.
Ramachandran, V., Arokia Vijaya Anand, M., David, E., Venkatachalam, K., Vijayakumar, S., Sankaran, V., Balupillai, A., Sangeetha, C. C., Gothandam, K. M., Kotakadi, V. S., & Ghidan, A. (2019). Antidiabetic activity of gold nanoparticles synthesized using wedelolactone in RIN-5F cell line. Antioxidants, 9(1), 8.
Subramaniyan, S., Kamaraj, Y., Kumaresan, V., Kannaiyan, M., David, E., Ranganathan, B., Selvaraj, V., & Balupillai, A. (2022). Green synthesized zinc oxide nanoparticles induce apoptosis by suppressing PI3K/Akt/mTOR signaling pathway in osteosarcoma MG63 cells. Global Translational Medicine, 1(1), 1–2.
Das, R. N., Balupillai, A., David, E., Santhoshkumar, M., & Muruhan, S. (2020). Naringin, a natural flavonoid, modulates UVB radiation-induced DNA damage and photoaging by modulating NER repair and MMPS expression in mouse embryonic fibroblast cells. Journal of Environmental Pathology Toxicology and Oncology, 39(2), 191–199.
Neophytou, C. M., Trougakos, I. P., Erin, N., & Papageorgis, P. (2020). Apoptosis deregulation and the development of cancer multi-drug resistance. Cancers, 13, 4363.
Aguayo, F., Perez-Dominguez, F., Osorio, J. C., Oliva, C., & Calaf, G. M. (2023). PI3K/AKT/mTOR signaling pathway in HPV-driven head and neck carcinogenesis: Therapeutic implications. Biology, 12, 672.
Desale, S. S., Soni, K. S., Romanova, S., Cohen, S. M., & Bronich, T. K. (2015). Targeted delivery of platinum-taxane combination therapy in ovarian cancer. Journal of Controlled Release: Official Journal of the Controlled Release Society, 220(Pt B), 651–659.
Kamal, M. M., Akter, S., Lin, C. N., & Nazzal, S. (2020). Sulforaphane as an anticancer molecule: Mechanisms of action, synergistic effects, enhancement of drug safety, and delivery systems. Archives of Pharmacal Research, 43, 371–384.
Yamada, R., Suda, H., Sadanari, H., Matsubara, K., Tuchida, Y., & Murayama, T. (2016). Synergistic effects by combination of ganciclovir and tricin on human cytomegalovirus replication in vitro. Antiviral Research, 125, 79–83.
Wang, X. F., Wu, D. M., Li, B. X., Lu, Y. J., & Yang, B. F. (2009). Synergistic inhibitory effect of sulforaphane and 5-fluorouracil in high and low metastasis cell lines of salivary gland adenoid cystic carcinoma. Phytotherapy Research: Ptr, 23(3), 303–307.
Kallifatidis, G., Labsch, S., Rausch, V., Mattern, J., Gladkich, J., Moldenhauer, G., Büchler, M. W., Salnikov, A. V., & Herr, I. (2011). Sulforaphane increases drug-mediated cytotoxicity toward cancer stem-like cells of pancreas and prostate. Molecular Therapy, 19(1), 188–195.
Kaminski, B. M., Weigert, A., Brune, B., Schumacher, M., Wenzel, U., Steinhilber, D., Stein, J., & Ulrich, S. (2011). Sulforaphane potentiates oxaliplatin-induced cell growth inhibition in colorectal cancer cells via induction of different modes of cell death. Cancer Chemotherapy and Pharmacology, 67(5), 1167–1178.
Li, J., Junqin, X., Yuxin, S., Ruolan, F., & Dan, Y. (2023). An insight on synergistic anti-cancer efficacy of biochanin A and sulforaphane combination against breast cancer. Applied Biochemistry and Biotechnology. https://doi.org/10.1007/s12010-023-04584-w
Ong, S. K. L., Shanmugam, M. K., Fan, L., Fraser, S. E., Arfuso, F., & Ahn, K. S. (2019). Focus on formononetin: Anticancer potential and molecular targets. Cancers (Basel), 11(5), 611.
Bidisha, P., Yuanyuan, L., & Trygve, O. (2018). The effects of combinatorial genistein and sulforaphane in breast tumor inhibition: Role in epigenetic regulation. International Journal of Molecular Sciences, 19, 1754.
Jing, Y. W., Ming, W. J., Ming, Y. L., Zhi, H. Z., Yue, X., Myong, H. R., Cheng, H. J., Guang, H. X., Lian, X. P., Hong, L. J., Juan, M., Yong, J., Hong, X. Z., & Xuejun, J. (2022). Formononetin represses cervical tumorigenesis by interfering with the activation of PD-L1 through MYC and STAT3 downregulation. Journal of Nutritional Biochemistry, 100, 108899.
Jan, R., & Chaudhry, G. S. (2019). Understanding apoptosis and apoptotic pathways targeted cancer therapeutics. Advanced Pharmaceutical Bulletin, 9(2), 205–218.
Chenyang, Z., Xin, W., Jiangfeng, D., Zhanjun, G., & Yuliang, Z. (2021). Reactive oxygen species-regulating strategies based on nanomaterials for disease treatment. Advanced Science, 8(3), 1–34.
Giovanni, M., Ciro, C., Michele, M., Luca, D., Pasquale, N., & Angela, G. (2022). Free radical properties, source and targets, antioxidant consumption and health. Oxygen, 2, 48–78.
Majeed, R., Hamid, A., Sangwan, P. L., Chinthakindi, P. K., Koul, S., Rayees, S., Singh, G., Mondhe, D. M., Mintoo, M. J., Singh, S. K., Rath, S. K., & Saxena, A. K. (2014). Inhibition of phosphotidylinositol-3 kinase pathway by a novel naphthol derivative of betulinic acid induces cell cycle arrest and apoptosis in cancer cells of different origin. Cell Death and Disease, 5(10), e1459.
Yang, J., Nie, J., Ma, X., Wei, Y., Peng, Y., & Wei, X. (2019). Targeting PI3K in cancer: Mechanisms and advances in clinical trials. Molecular Cancer, 18(1), 1–28.
He, Y., Sun, M. M., Zhang, G. G., Yang, J., Chen, K. S., Xu, W. W., & Li, B. (2021). Targeting PI3K/Akt signal transduction for cancer therapy. Signal Transduction and Targeted Therapy, 6(1), 425.
Lu, J., Zang, H., Zheng, H., Zhan, Y., Yang, Y., Zhang, Y., & Fan, S. (2020). Overexpression of p-Akt, p-mTOR and p-eIF4E proteins associates with metastasis and unfavorable prognosis in non-small cell lung cancer. PLoS One, 15(2), e0227768.
Glaviano, A., Foo, A. S., Lam, H. Y., Yap, K. C., Jacot, W., Jones, R. H., & Kumar, A. P. (2023). PI3K/AKT/mTOR signaling transduction pathway and targeted therapies in cancer. Molecular Cancer, 22(1), 138.
Zhong, L., Li, Y., Xiong, L., Wang, W., Wu, M., Yuan, T., & Yang, S. (2021). Small molecules in targeted cancer therapy: Advances, challenges, and future perspectives. Signal Transduction and Targeted Therapy, 6(1), 201.
Author information
Authors and Affiliations
Contributions
P.J.: conceptualization, methodology, original draft preparation; W.J.: writting and data curation; X.L.: review and editing; Q.Z.: supervision. Overall, all authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
All authors agreed to publish this paper in this journal.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, P., Jiang, W., Li, X. et al. Combination of Formononetin and Sulforaphane Natural Drug Repress the Proliferation of Cervical Cancer Cells via Impeding PI3K/AKT/mTOR Pathway. Appl Biochem Biotechnol (2024). https://doi.org/10.1007/s12010-024-04873-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s12010-024-04873-y