Abstract
Diabetes mellitus, which is the result of autoimmune destruction of the insulin-producing β cells, occurs by loss of insulin-secreting capacity. The insufficient source of insulin-producing cells (IPCs) is the major obstacle for using transplantation as diabetes treatment method. The present study suggests a method to form islet-like clusters of IPCs derived from mouse embryonic stem cells (mESCs). This protocol consists of several steps. Before starting this protocol, embryoid bodies (EBs) should be cultured in suspension in conditioned medium of isolated mouse pancreatic islet in combination with activing A to be induced. Then differentiated mESCs were replaced with dishes supplemented with basic fibroblast growth factor (bFGF). Next, bFGF was withdrawn, and cyclopamine and noggin were added. Then the cells were treated with B27, nicotinamide, and islet-conditioned medium for maturation. mESCs, as the control group, were cultured without any treatment. An enhanced expression of pancreatic-specific genes was detected by qRT-PCR and immunofluorescence in the differentiated mESCs. The differentiated mESCsco express other markers of pancreatic islet cells as well as insulin. This method exhibited higher insulin generation and further improvement in IPCs protocol that may result in an unlimited source of ES cells suitable for transplantation. The results indicated that conditioned medium, just as critical components of the stem cell niche associated with other factors, had high potential to differentiate mESCs into IPCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cell therapy, as a treatment strategy for many diseases and damaged organs, can enhance the biological function of body by replacing or repairing the impaired tissues. This approach can be achieved by obtaining favorite stem cells from various organs [2].
Embryonic stem cells (ESCs) with self-renewing capability are pluripotent cells established from the inner cell mass [33]. The major properties of these cells are their in vitro and in vivo differentiation ability into all of embryonic three-layer lineages [5, 18]. For differentiation, the isolated ESCs grow in suspension to form the embryoid bodies (EBs), which is an important step in differentiation process. According to the mentioned characteristics, mESCs are the desired candidates for transplantation therapies such as diabetes treatment [9, 16]. Diabetes mellitus is the most common metabolic disorder that is currently known as the dominant cause of death in the world [1, 27]. Diabetes is associated with different effects such as diabetic retinopathy, nephropathy, and neuropathy and currently, there is no effective cure for this disease [3, 15, 24, 29, 36]. Today, islet cell transplantation is considered as a treatment for diabetic patients. However, several problems might be induced due to the application of this procedure. Therefore, researchers try to use stem cells therapeutically [8, 13, 14, 29]. ESCs could potentially be accounted as the unbound number of IPCs for transplantation into patients with diabetes mellitus [13].
Pancreatic organogenesis is a complex and multistep process, which is controlled by genes, key transcriptional regulators, and environment. Among them, Pdx1, a pancreas duodenum homeodomain transcription factor; FOXA2, as a candidate gene for familial hyperinsulinism; Ptf1a, a bHLH transcription factor; Ngn3, a transiently expressed transcription factor; and C-peptide, as an indicator of beta cell secretary function, are important for pancreatic specification [12, 21, 35]. During embryogenesis, various signaling factors such as activing/nodal, beta fibroblast growth factor (bFGF), retonoic acid (RA), Shh, … engage in the development of pancreas, many of which are produced by pancreases itself and its surrounding environment [28, 32]. Furthermore, the use of co-culture techniques is considerably efficient in improving the differentiation of ES cells towards a desirable direction and also in studying the developmentally signaling interactions between two adjacent organs. Conditioned medium is prepared by collecting desirable secreted factors that can directly or indirectly play an effective role in cells specification [10, 11].
A co-culture system associated with signaling factors to generate insulin-producing cells (IPCs) from mESCs was described in the present study. The aim of this study was to demonstrate the protocol’s four steps for definitive endoderm (DE), primitive gut (PG), and pancreatic epithelium (PE) induction to simplify the IPCs protocols.
Materials and Methods
Laboratory Animals
Male NMRI mice (25–30 g) were purchased from the animal house of Ahvaz Jundishapur University of Medical Science (Ahvaz, Iran). Mice were housed in the standard cages on a 12:12-h light-dark cycle and were supplied with sterile feed and water.
Isolation and Culture of Mice Pancreatic Islets
Pancreatic islets were isolated from male NMRI mice and digested with collagenase. In summary, the pancreas was removed from an adult mouse and washed with PBS and floated in collagenase IV (ICN Biomedicals, USA) for 15 min. Then they were cultured in DMEM/F12 (Gibco, USA) with 3% FBS (Gibco), 100 U/ml pen/strep (Sigma, USA), and 5 mM D-glucose. Every day, the supernatant was collected and centrifuged with the 2000g (Hettich, Germany, Rotofix32A) for 5 min, and stored in − 80 0C [30].
Isolation and Culture MEF
In this study, the 13-day-old embryos of NMRI mice were used for isolating and culturing MEF by an enzymatic method. Isolated cells were cultured in a high-glucose Dulbecco’s modified Eagle’s medium (DMEM) containing 10% (vol/vol) FBS, 2 mM l glutamine, and pen/strep until passage 3. MEFs were inactivated by mitomycin C (Sigma) treatment and were used as a feeder layer for mESCs.
Embryonic Stem Cell Culture
Mouse ESCs were maintained on precoated gelatin (0.1%, Sigma) dishes containing mitomycin C-inactivated feeder layer of primary cultures of MEFs in DMEM supplemented with 15% FBS, 2 mM glutamine (Gibco, USA), 0.1 mM beta-mercaptoethanol (Sigma, USA), 1% nonessential amino acid stock (Gibco, USA), 1% penicillin and streptomycin stock, and 1000 IU/ml leukemia inhibitory factor (LIF, Chemicon, ESGRO). Cultures were grown and passaged in 5% CO2 and 95% humidity every 2 days.
In vitro Differentiation Procedure
Prior to differentiation, mESCs were subjected to EBs formation in 6-well nontreated plate at a density of 1 × 105 cells/well in DMEM supplemented with 3% FBS. After 2–4 days of culture, 40–50 EBs were plated in 24-well plate for differentiation. Differentiation of IPCs was carried out in four stages. The first stage was the induction of DE. For this purpose, the undifferentiated mESCs were induced by three different protocols: (a) mESCs were cultured in conditioned medium (obtained from pancreatic islets) containing 30 ng/ml activin A (R&D) for 6 days. (b) mESCs were cultured in DMEM containing 100 ng/ml activin A (R&D) associated 25 ng/ml Wnt3a for 6 days. (c) mESCs were only cultured in conditioned medium for 6 days. The second stage was PG induction. In this stage, the DE-induced cells (which earned from stage 1 by protocol A) were treated with DMEM supplemented with 2 ng/ml bFGF (Invitrogen) and the cells were fed with fresh medium every 2–3 days for 7 days. In stage 3, the PE induction was carried out. The cells (which were earned from stage 2) were cultured in suspension in DMEM supplemented with cyclopamine (0.2 μM) and noggin (50 ng/ml) for 7 days. IPCs maturity was the last stage. To do this, the cell clusters (which earned from stage 3) were cultured with condition medium containing B27 1% and nicotinamide (10 mM) for 6 days. Then the differentiated cells were analyzed.
Relative Reverse Transcription Polymerase Chain Reaction Analysis
The mRNA expression levels were measured by relative reverse transcription polymerase chain reaction (qRT-PCR). In sum, the extraction of total RNA was done by sinaclon (IRAN). Using the TaqMan Reverse Transcription Kit (Genall, Ampliqon, Denmark) containing random hexamer primer mix based on the manufacturer’s instructions, RNA (2–5 μg) was reverse transcribed. Briefly, RNA sample and primers were mixed in a sterile RNase-free microfuge tube and incubated 5 min at 65 °C. Then the buffer, reverse transcriptase enzyme, and RNase inhibitor were added and incubated at 42 °C for 1 hour. Quantitative RT-PCR reactions were carried out in the 48-well optical reaction plates on StepOne™ RT- PCR System. The resulting cDNA (30 ng) was subjected to qRT-PCR for each reaction through mixing with 10 μL of Power SYBER Green master mixture (Ampliqon, Denmark), 0.5 μM of each primer (Table 1) in a total volume of 20 μL at the annealing temperature. The threshold cycle (Ct) of each sample was obtained from StepOne software (Applied Biosystems). The samples were normalized via GAPDH as a housekeeping gene. QRT-PCR was performed on a master cycler (ABI 2720, Applied Biosystems, USA). In this study, the un-induced cells were presented as control samples.
Fluorescent Immunostaining
F immunostaining was initiated with rinsing of the differentiated cells by phosphate-buffered saline (PBS) and fixed for 20 min in 4% paraformaldehyde. Then the cells were permeabilized using 0.5% Triton X-100 in PBS/1% serum albumin and were incubated in 0.1 M PBS containing 10% normal goat serum as a blocking buffer for 45 and after that incubated overnight with the primary antibody mouse monoclonal anti-FoxA2 (1/100 dilution, Abcam; ab60721), mouse monoclonal anti-Sox17 (1/500, Abcam; ab191699), mouse monoclonal anti-Pdx1 (1/500, Abcam; ab47267), mouse monoclonal anti-HNF4a (1/500, Abcam; ab41898), mouse monoclonal anti-NKX2.2 (1/500, Abcam; ab191077), mouse monoclonal anti-Neurogenin3 (1/500, Abcam; ab38548), mouse monoclonal anti-Insulin (1/500, Abcam; ab8304), mouse monoclonal anti-C-peptide (1/500, Abcam; ab14181), and mouse monoclonal anti-Glucagon (1/500, Abcam; ab10988). After rinsing the secondary Donkey Anti-Rabbit IgG H&L Alexa Fluor (1/200 dilution, Abcam; 150108), Donkey Anti-Mouse IgG H&L Alexa Fluor (1/200 dilution, Abcam;150073) were added to the samples, which were then incubated for an additional hour. Finally, the cells’ nucleus were stained with DAPI (Sigma, USA) and then analyzed with the fluorescence microscope (Olympus, BX51, Japan).
DTZ Staining
A DTZ (Merck) stock solution was prepared with 50 mg of DTZ in 5 ml of DMSO and then this solution was diluted in culture medium and stored at − 20 °C. Briefly, the differentiated clusters were incubated at 37 °C for 15 min in the DTZ solution with the concentration of 10 mM. After that, the clusters were rinsed three times with PBS and observed by microscopy.
Statistical Analysis
Data expression is performed by SPSS as mean ± SEM. Following Tukey’s test, one-way analysis of variance (ANOVA) was applied to compare the data obtained from different groups. In fact, A p value < 0.05 was considered as a significant difference statistically.
Results
Condition Medium and Low Concentration of Activin A Induce Definitive Endoderm Formation from mESCs
In this study, we used three protocols for inducing DE populations. As shown in Fig. 1a, results of qRT-PCR show that among three protocols, condition medium plus activin A with the concentration of 30 ng/ml was significantly more effective than others. Also, activin A associated Wnt3a was significantly more effective than condition medium alone.
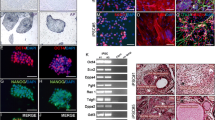
a Quantitative expression analysis of definitive endoderm derived from mESCs after 6 days. Results were collected from 3 independent experiments with 2 internal replicates per experiment. Differences were statistically significant if p ≤ 0.05. Increase in expression of the definitive endoderm marker (FoxA2 and Sox17) and decrease in expression of non-endodermal markers (Brachyury, Sox7 and Sox1) and pluripotency-related genes (Nanog and Oct4). b Differentiation of mESCs into DE cells. Immunofluorescence analysis of Sox17 (in green) and FoxA2 (in red) expression after 6 days. Scale bar = 50 μm. c Quantitative expression analysis of definitive endoderm derived from mESCs by three different protocols after 6 days; CM conditioned media, AA Activin A
Condition medium plus low concentration of activin A treatment of mESCs induced differentiation of DE populations, as assessed by marker gene analysis. qRT-PCR analysis of day 6 endoderm cells identified mRNAs including Foxa2, Sox17, and GSC, which were induced in activin A and condition medium-treated muk3 mESCs on day 6 (Fig. 1). In addition, we observed a significant decrease in the expression of Brachyury, a mesendoderm marker; Sox1, an ectoderm marker; and Sox7, a visceral endoderm marker; Nanog and Oct4, as pluripotent markers, were compared to a control experiment without any induction (Fig. 1b). In this study, the control group did not express mRNAs of the DE genes.
Also, we performed immunocytochemical analysis on the mESC derived from endoderm population. The majority of the endoderm cells expressed Foxa2 and Sox17 transcription factors, with expression localized within the nucleus. Taken together, these data indicated that treatment with low concentration of activin A and condition medium efficiently induced DE and other cells were rare in our differentiated endoderm population (Fig. 1c).
Survey Expression of Pdx1 in Pancreatic Endoderm After Stage 3
MESC-derived definitive endoderm cells were treated with bFGF, cyclopamine, and noggin supplement (stages 2 and 3) for 14 days. After that, the differentiated cells were tested for Pdx1 and Foxa2 by immunocytochemistry and qRT-PCR. Also, we verified high expression of pancreas-related genes including Hnf4α, Ngn3, and Nkx2.2 in pancreatic endoderm comparing with the control samples in this stage (Fig. 2). Also, Nanog and Oct4, as pluripotent markers, were drastically downregulated in comparison with nontreated cultures (Fig. 2). These results confirmed that treatment with this protocol could induce significant differentiation of mESCs into pancreatic endoderm cells in these stages.
a Quantitative expression analysis of pancreatic endoderm derived from DE cells after 7 days. Results were collected from 3 independent experiments with 2 internal replicates per experiment. Differences were statistically significant if p ≤ 0.05. Increase in expression of the pancreatic endoderm marker (Pdx1, Foxa2, HNF4α, Ngn3, Nkx2.2) and decrease in expression of pluripotency-related genes (Nanog and Oct4). b Differentiation of DE cells into pancreatic endoderm cells. b Immunofluorescence analysis of Pdx1 (in red), Foxa2 (in red), HNF4α (in red), Ngn3 (in green), and Nkx2.2 (in green) expression after 7 days. Scale bar = 50 μm
IPCs Maturity
In the final stage, differentiation of clusters was continued. Eventually, we harvested the cells that produced the pancreatic hormones including C-peptide, insulin, and glucagon after 26 days. These maturated cells were stained with immunocytochemistry and analyzed with qRT-PCR and these data are presented in Fig. 3. The results showed that the majority of maturated cells expressed C-peptide, insulin, and glucagon.
a Quantitative expression analysis of IPCs derived from pancreatic endoderm cells after 13 days. Results were collected from 3 independent experiments with 2 internal replicates per experiment. Differences were statistically significant if p ≤ 0.05. Increase in expression of the IPCs marker (C-peptide, insulin, and glucagon) and decrease in expression of pluripotency-related genes (Nanog and Oct4). b Differentiation of DE cells into IPCs. b Immunofluorescence analysis of glucagon (in red), C-peptide (in green), and insulin (in green) expression after 13 days. Scale bar = 50 μm
Light Microscopy of Cultured Islets and DTZ Staining
Cultured cells, EBs formation, and islets had regular cellular structures under the inverted microscope. In addition, no disintegrated islets were observed in islet preparations (Fig. 4). Owing to the presence of zinc in insulin-containing secretory granules, regions of pancreatic endocrine cells in the cultures could be specifically labeled with the zinc-chelating dye dithizone (DTZ), which efficiently stains beta cells in the islet (Latif et al. 1988). Using this characteristic of DTZ, IPCs were identified in differentiated cells derived from ESCs as cellular clusters. We observed discrete areas of DTZ staining in stage 4 cultures (Fig. 5).
Cell Viability
MTT results indicated that in the last stage, the IPCs had cell viability higher than 70%. As shown in Fig. 6, until day 7, cell viability of cells was around 98% and decreased into 81% on day 14, 74% on day 20, and eventually 70% on day 26.
Discussion
In this study, we have described an efficient protocol to differentiate mESCs through DE, PG, PE, and endocrine populations to ultimately generate IPCs expressing C-peptide, insulin, and glucagon. Taken together, our results showed that mESC-derived IPCs contained C-peptide, insulin, and glucagon-producing cells similar to pancreatic islets. Mature cells also express Pdx1, as a pancreas-specific transcription factor, which regulates expression of the insulin gene. In the current protocol, we choose a combination of various factors, including activin A and a transforming growth factor TGF-β gene family member, as well as bFGF, noggin, and condition medium at specific stages of differentiation.
We used a low concentration of activin A, in combination with conditioned medium, during the early stages of endoderm formation. Previous studies showed that high concentration of activin A required inducing differentiation of ES cells to IPCs [15, 19] and in this protocol, we could reduce the concentration of this factor. To date, we have observed considerable percentage of endoderm cells expressing Sox17 and Foxa2. In the present study, we used noggin to induce differentiation of pancreatic lineage by enhancing Pdx1 gene expression. As previous studies showed, treatment with inhibitors of bone morphogenetic protein (BMP) signaling such as noggin can induce Pdx1 cells from DE cells [17, 23]. In later steps, we removed bFGF to facilitate pancreatic differentiation and prevent hepatic differentiation [26]. We have chosen nicotinamide and condition medium, which could induce maturation of pancreatic endocrine cells. Condition medium alone was largely ineffective in inducing endoderm formation in mESCs [11]. Activin A treatment alone caused induction of endoderm-specific genes, but the condition medium and activin A combination induced higher levels of Sox17 and Foxa2 expression in muk3 mESCs.
Here, we declare that factors from the mouse pancreatic islets induced differentiation of mESCs into IPCs. The islets released soluble signals that are responsible for in vitro IPCs differentiation from mESCs. Similar to our study, Lee et al. demonstrated that the pancreatic extracts induced differentiation of human adipose tissue-derived stem cells into IPCs [20]. Also, Chang et al reported that BM-MSCs were differentiated into IPCs by the use of rabbit pancreatic pieces [4].
Here, we observed that under the current culture conditions, mESCs could directly differentiate into definitive endoderm and, later, into pancreatic endoderm cells with Pdx1 expression. Recently, D’Amour et al. have reported on generating pancreatic insulin-producing cells from hESCs [6, 7]. They and others declared that the formation of definitive endoderm cells, before induction of prepancreatic cells, plays an important role in pancreatic cells development [6, 25]. Therefore, we used this idea in our differentiation protocol.
Generally, during the in vitro experiment, the events related to real development have been followed up such as the expression pattern of transcription factor genes. In the present study, we analyzed sequential expression of transcription factors involved in pancreas development. The continuous appearance of Sox17, Foxa2, Pdx1, Hnf4a, Ngn3, and Nkx2.2, followed by islet hormones, insulin, glucagon, and C-peptide, clearly suggested that the mESCs followed a progression similar to that of in vivo pancreas development. We also have tested the expression of other developmentally regulated genes including sox7 as a visceral endodermal marker, Brachyury as a mesodermal marker, Sox1 as an ectodermal marker, Nanog and Oct4 as pluripotent markers, and AFP as a hepatocyte marker. Our results showed that these markers were downregulated following induction at various stages of IPCs generation. It is a further confirmation for the efficiency of this protocol.
So far, mESCs were used in various studies in order to obtain IPCs, as an example Soria et al. in 2000 introduced their insulin-secreting cell production which was made using the multistep differentiation protocol [31]. Also, Lumelsky et al. utilized a modified approach to generate nestin-positive cells and it was demonstrated that they induced islet-like clusters from mESCs. They declared that these clusters were able to secrete insulin but their efficiency was significantly lower than the normal cells [22]. Therefore, we tried to improve our efficiency, for example, we provided embryoid bodies (EBs) before initiation of differentiation. Previously, it has been demonstrated that cell to cell communication can improve cell viability and differentiation [34]. Therefore, the use of EBs is a helpful idea for long-term in vitro maintenance of embryonic cells. In addition, the formation of EBs in the nest steps can increase the percentage of the insulin expressing cells and can improve their survivability.
Conclusion
In this study, we utilized the pancreatic extract to differentiate mESCs into IPCs. The contact between cells and condition medium associated with signals initiated the differentiation. This approach and the other ones are useful in the development of considerable methods to generate functional IPCs from stem cells. It is worth mentioning that further changes of the protocol may lead to an increase in insulin expression and secretion.
References
Abu Bakar Sajak, A., Mediani, A., Maulidiani, Ismail, A., & Abas, F. (2017). Metabolite variation in lean and obese streptozotocin (STZ)-induced diabetic rats via (1)H NMR-based metabolomics approach. Applied Biochemistry and Biotechnology, 182(2), 653–668.
Ballas, C. B., Zielske, S. P., & Gerson, S. L. (2002). Adult bone marrow stem cells for cell and gene therapies: implications for greater use. Journal of Cellular Biochemistry. Supplement, 38, 20–28.
Bundhun, P. K., Bhurtu, A., & Yuan, J. (2017). Impact of type 2 diabetes mellitus on the long-term mortality in patients who were treated by coronary artery bypass surgery: a systematic review and meta-analysis. Medicine, 96(22), e7022.
Chang, C., Niu, D., Zhou, H., Li, F., & Gong, F. (2007). Mesenchymal stem cells contribute to insulin-producing cells upon microenvironmental manipulation in vitro. Transplantation Proceedings, 39(10), 3363–3368.
Chen, C. Y., Cheng, Y. Y., Yen, C. Y., & Hsieh, P. C. (2017). Mechanisms of pluripotency maintenance in mouse embryonic stem cells. Cellular and Molecular Life Sciences: CMLS, 74(10), 1805–1817.
D’Amour, K. A., Agulnick, A. D., Eliazer, S., Kelly, O. G., Kroon, E., & Baetge, E. E. (2005). Efficient differentiation of human embryonic stem cells to definitive endoderm. Nature Biotechnology, 23(12), 1534–1541.
D’Amour, K. A., Bang, A. G., Eliazer, S., Kelly, O. G., Agulnick, A. D., Smart, N. G., Moorman, M. A., Kroon, E., Carpenter, M. K., & Baetge, E. E. (2006). Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells. Nature Biotechnology, 24(11), 1392–1401.
Dave, S. D., Vanikar, A. V., & Trivedi, H. L. (2013). Extrinsic factors promoting in vitro differentiation of insulin-secreting cells from human adipose tissue-derived mesenchymal stem cells. Applied Biochemistry and Biotechnology, 170(4), 962–971.
De Felici, M., Farini, D., & Dolci, S. (2009). In or out stemness: comparing growth factor signalling in mouse embryonic stem cells and primordial germ cells. Current Stem Cell Research & Therapy, 4(2), 87–97.
Ebrahimi-Barough, S., Hoveizi, E., Norouzi Javidan, A., & Ai, J. (2015). Investigating the neuroglial differentiation effect of neuroblastoma conditioned medium in human endometrial stem cells cultured on 3D nanofibrous scaffold. Journal of Biomedical Materials Research. Part A., 103(8), 2621–2627.
Elham, H., Fardin, F., & Mahmod, H. (2017). The roles of the co-culture of mEScs with pancreatic islets and liver stromal cells in the differentiation of definitive endoderm cells. Biologicals: Journal of the International Association of Biological Standardization, 45, 9–14.
Fujitani, Y. (2017). Transcriptional regulation of pancreas development and beta-cell function [review]. Endocrine Journal, 64(5), 477–486.
Golden, S. H., Maruthur, N., Mathioudakis, N., Spanakis, E., Rubin, D., Zilbermint, M., & Hill-Briggs, F. (2017). The case for diabetes population health improvement: evidence-based programming for population outcomes in diabetes. Current Diabetes Reports, 17(7), 51.
Hoveizi, E., Khodadadi, S., Tavakol, S., Karima, O., & Nasiri-Khalili, M. A. (2014). Small molecules differentiate definitive endoderm from human induced pluripotent stem cells on PCL scaffold. Applied Biochemistry and Biotechnology, 173(7), 1727–1736.
Hoveizi, E., Massumi, M., Ebrahimi-barough, S., Tavakol, S., & Ai, J. (2015). Differential effect of Activin A and WNT3a on definitive endoderm differentiation on electrospun nanofibrous PCL scaffold. Cell Biology International, 39(5), 591–599.
Hoveizi, E., Nabiuni, M., Parivar, K., Ai, J. and Massumi, M. (2013) Definitive endoderm differentiation of human-induced pluripotent stem cells using signaling molecules and IDE1 in three-dimensional polymer scaffold. Journal of biomedical materials research. Part A, 102, 4027–36.
Jiang, J., Au, M., Lu, K., Eshpeter, A., Korbutt, G., Fisk, G., & Majumdar, A. S. (2007). Generation of insulin-producing islet-like clusters from human embryonic stem cells. Stem Cells, 25(8), 1940–1953.
Kang, X., Xie, Y., Powell, H. M., James Lee, L., Belury, M. A., Lannutti, J. J., & Kniss, D. A. (2007). Adipogenesis of murine embryonic stem cells in a three-dimensional culture system using electrospun polymer scaffolds. Biomaterials, 28(3), 450–458.
Kroon, E., Martinson, L. A., Kadoya, K., Bang, A. G., Kelly, O. G., Eliazer, S., Young, H., Richardson, M., Smart, N. G., Cunningham, J., Agulnick, A. D., D’Amour, K. A., Carpenter, M. K., & Baetge, E. E. (2008). Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nature Biotechnology, 26(4), 443–452.
Lee, J., Han, D. J., & Kim, S. C. (2008). In vitro differentiation of human adipose tissue-derived stem cells into cells with pancreatic phenotype by regenerating pancreas extract. Biochemical and Biophysical Research Communications, 375(4), 547–551.
Lee, S. H., Park, M. H., Park, S. J., Kim, J., Kim, Y. T., Oh, M. C., Jeong, Y., Kim, M., Han, J. S., & Jeon, Y. J. (2012). Bioactive compounds extracted from Ecklonia cava by using enzymatic hydrolysis protects high glucose-induced damage in INS-1 pancreatic beta-cells. Applied Biochemistry and Biotechnology, 167(7), 1973–1985.
Lumelsky, N., Blondel, O., Laeng, P., Velasco, I., Ravin, R., & McKay, R. (2001). Differentiation of embryonic stem cells to insulin-secreting structures similar to pancreatic islets. Science, 292(5520), 1389–1394.
Maehr, R., Chen, S., Snitow, M., Ludwig, T., Yagasaki, L., Goland, R., Leibel, R. L., & Melton, D. A. (2009). Generation of pluripotent stem cells from patients with type 1 diabetes. Proceedings of the National Academy of Sciences of the United States of America, 106(37), 15768–15773.
Massumi, M., Hoveizi, E., Baktash, P., Hooti, A., Ghazizadeh, L., Nadri, S., Pourasgari, F., Hajarizadeh, A., Soleimani, M., Nabiuni, M., & Khorramizadeh, M. R. (2014). Efficient programming of human eye conjunctiva-derived induced pluripotent stem (ECiPS) cells into definitive endoderm-like cells. Experimental Cell Research, 322(1), 51–61.
McLean, A. B., D’Amour, K. A., Jones, K. L., Krishnamoorthy, M., Kulik, M. J., Reynolds, D. M., Sheppard, A. M., Liu, H., Xu, Y., Baetge, E. E., & Dalton, S. (2007). Activin a efficiently specifies definitive endoderm from human embryonic stem cells only when phosphatidylinositol 3-kinase signaling is suppressed. Stem Cells, 25(1), 29–38.
Mfopou, J. K., Chen, B., Mateizel, I., Sermon, K., & Bouwens, L. (2010). Noggin, retinoids, and fibroblast growth factor regulate hepatic or pancreatic fate of human embryonic stem cells. Gastroenterology, 138, 2233–2245 2245 e2231–2214.
Ni, Z., Zhang, Y., Wang, H., Wei, Y., Ma, B., Hao, J., Tu, P., Duan, H., Li, X., Jiang, P., Ma, X., Wang, B., Wu, R., Zhu, J., & Li, M. (2016). Construction of a fusion peptide 5rolGLP-HV and analysis of its therapeutic effect on type 2 diabetes mellitus and thrombosis in mice. Applied Biochemistry and Biotechnology, 179(1), 59–74.
Prince, V. E., Anderson, R. M., & Dalgin, G. (2017). Zebrafish pancreas development and regeneration: fishing for diabetes therapies. Current Topics in Developmental Biology, 124, 235–276.
Shaer, A., Azarpira, N., & Karimi, M. H. (2014). Differentiation of human induced pluripotent stem cells into insulin-like cell clusters with miR-186 and miR-375 by using chemical transfection. Applied Biochemistry and Biotechnology, 174(1), 242–258.
Sherwood, R. I., Jitianu, C., Cleaver, O., Shaywitz, D. A., Lamenzo, J. O., Chen, A. E., Golub, T. R., & Melton, D. A. (2007). Prospective isolation and global gene expression analysis of definitive and visceral endoderm. Developmental Biology, 304(2), 541–555.
Soria, B., Roche, E., Berna, G., Leon-Quinto, T., Reig, J. A., & Martin, F. (2000). Insulin-secreting cells derived from embryonic stem cells normalize glycemia in streptozotocin-induced diabetic mice. Diabetes, 49(2), 157–162.
Spaeth, J. M., Walker, E. M., & Stein, R. (2016). Impact of Pdx1-associated chromatin modifiers on islet beta-cells. Diabetes, Obesity & Metabolism, 18(Suppl 1), 123–127.
Wang, Z., & Huang, J. (2014). Neuregulin-1 increases connexin-40 and connexin-45 expression in embryonic stem cell-derived cardiomyocytes. Applied Biochemistry and Biotechnology, 174(2), 483–493.
Yang, J., Wu, C., Stefanescu, I. and Horowitz, A. (2017) Analysis of Retinoic Acid-induced Neural Differentiation of Mouse Embryonic Stem Cells in Two and Three-dimensional Embryoid Bodies. Journal of visualized experiments, https://doi.org/10.3791/55621.
Zhou, G., Chiu, D., Qin, D., Niu, L., Cai, J., He, L., Huang, W., & Xu, K. (2012). Detection and clinical significance of CD44v6 and integrin-beta1 in pancreatic cancer patients using a triplex real-time RT-PCR assay. Applied Biochemistry and Biotechnology, 167(8), 2257–2268.
Zhu, R., Liu, H., Liu, C., Wang, L., Ma, R., Chen, B., Li, L., Niu, J., Fu, M., Zhang, D. and Gao, S. (2017) Cinnamaldehyde in diabetes: A review of pharmacology, pharmacokinetics and safety. Pharmacological research, 122, 78–89.
Funding
This study was financially supported by the vice chancellor of research affairs of Ahvaz Jondishapur University of Medical Science, Cellular and Molecular Research Center, Grant No: CMRC-9415 and Iranian Stem Cell Network.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Elham, H., Mahmoud, H. The Effect of Pancreas Islet-Releasing Factors on the Direction of Embryonic Stem Cells Towards Pdx1 Expressing Cells. Appl Biochem Biotechnol 186, 371–383 (2018). https://doi.org/10.1007/s12010-018-2733-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12010-018-2733-3