Abstract
The executive board of the Academy for Ethics in Medicine (AEM) and two AEM working groups formulated standards and recommendations for clinical ethics consultation in 2010, 2011, and 2013. These guidelines comply with the international standards like those set by the American Society for Bioethics and Humanities. There is no empirical data available yet that could indicate whether these standards and recommendations have been implemented in German hospitals. This desideratum is addressed in the present study. We contacted 1.858 German hospitals between September 2013 and January 2014. A follow-up survey was conducted between October 2014 and January 2015. The data of the initial survey and the follow-up survey were merged and evaluated. The statements of the participants were compared with the standards and recommendations. The standards of the AEM concerning the tasks of clinical ethics consultation (including ethics consultation, ethics training and the establishment of policy guidelines) are employed by a majority of participants of the study. Almost all of these participants document their consultation activities by means of protocols or entries in the patient file. There are deviations from the recommendations of the AEM working groups regarding the drafting of statutes, activity reports, and financial support. The activities of clinical ethics consultation predominantly comply with the standards of the AEM and recommendations for the documentation. The recommendations for evaluation should be improved in practice. This applies particularly for activity reports in order to evaluate the activities. Internal evaluation could take place accordingly.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 2010, the executive board of the Academy for Ethics in Medicine (AEM) published “Standards for Ethics consultation in health facilities” (AEM 2010). Herein, concrete tasks and goals of structured clinical ethics case consultation like the Healthcare Ethics Committee (HEC), Ethics Consultation or ethics forum were defined. The tasks included the implementation of ethics case consultation, ethics training, and the establishment of ethical guidelines. In defining these tasks, the AEM follows the internationally recognized standards for HECs (Hester and Schonfeld 2012) which are also recommended by the American Society for Bioethics and Humanities (ASBH 2011; Tarzian et al. 2015). Among others, a structured approach in ethics case consultation and the systematic reflection of ethical conflicts were formulated as targets by the AEM. Suggestions on behalf of the implementation and refinement of the tasks and goals were furthermore submitted (AEM 2010). The executive board of the AEM has also formulated standards for structures of clinical ethics consultation. As a result, “Recommendations for the documentation of ethics case consultation” were published by the AEM working group in 2011, which provided the preparation and subsequent retention of result reports of ethics case consultation among others (Fahr et al. 2011). In 2013, another AEM working group published “Recommendations for the evaluation of ethics case consultation in health facilities” (Neitzke et al. 2013). Statutes and activity reports are presented as part of the evaluation process in this publication. With these two recommendations (Fahr et al. 2011; Neitzke et al. 2013), the functioning of structures of clinical ethics case consultation is being specified. Since the publication of the standards by the AEM in 2010 (AEM 2010) and the recommendations of the working groups (Fahr et al. 2011; Neitzke et al. 2013), no nationwide empirical data was collected on the functioning of structures in terms of clinical ethics case consultation in Germany. A study like the widely recognized survey by Fox et al. (2007) for the USA was not available in the German context. This desideratum is addressed in this study. The present paper evaluates how these standards and recommendations have been implemented in German hospitals. We have analyzed quantitative data. In this paper we will answer four questions: (1) Which of the tasks defined by the AEM are accomplished in practice? (2) How are the goals established by the AEM put into practice? (3) How does the documentation of the clinical ethic consultations results’ look like? (4) What kind of instruments are used for evaluating these results?
Method
Between mid-August and October 2014, we contacted each of the 1.858 hospitals in Germany for the follow-up survey by phone (Schochow et al. 2015). We inquired whether a structure of clinical ethics consultation was already implemented or was about to be implemented. In addition to that we inquired whether the hospital had participated in the first survey. In cases where the hospital had not participated in the first survey, we inquired whether the hospital would participate in a follow-up survey in written form. If they agreed to do so, a questionnaire was sent to them. The follow-up survey in written form was structured according to the questionnaires that were used during the first survey. The questionnaire consisted of yes/no-questions, questions regarding grouping (single choice as well as multiple choices), rating scales, and free text entries. The questionnaire included 28 items and was both composed of a quantitative section (16 items) and a qualitative section (12 items). The data of the first study and the follow-up survey was merged and evaluated. The hospitals were divided into three categories: small hospitals (maximum number of beds 300), mid-size hospitals (number of beds between 301 and 700), and large hospitals (minimum number of beds 701). The statistical analysis was conducted by using SPSS-software for Windows version 20. Dependencies with a p value smaller than 5 % were considered to be statistically significant. In this paper, we focused exclusively on those statements of the participants that relate to the AEM-standards (AEM 2010) and the recommendations of the two working groups (Fahr et al. 2011; Neitzke et al. 2013). Our aim was to evaluate if and to what extent the standards and recommendation are applied in practice.
Results
545 out of the 1.858 contacted hospitals claimed to have implemented a structure of clinical ethics consultation. All further statements refer to this total of 545 participants. 90.8 % out of this participants implemented ethics consultations, 9.2 % did not. Trainings were offered by 71.9 % of the participants. We found a significant connection between the size of the hospitals and the provision of ethics trainings (p = 0.00): The larger the hospital, the more likely is the provision of ethics training. The type of hospital operation is of no significance in this regard (p = 0.94).
71.7 % of the participants were responsible for establishing ethical guidelines. There is a significant correlation between the size of the hospital and the responsibility for ethical guidelines (p = 0.02): The larger the hospital, the more likely the hospital is responsible for establishing ethical guidelines. There is no significant influence of the type of operation on the responsibility for establishing guidelines (p = 0.96).
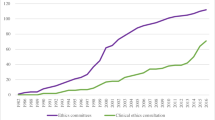
Instruments for structuring the clinical ethics consultation and systematic reflection were used by 64.9 % of the participants. Often the Nijmegen method (25 %) or own sheets (12 %) were being used. 19.5 % of the participants did not use structuring instruments (Fig. 1). Whether such an instrument is used depends on the size of the hospital (p = 0.00). 83.8 % of mid-size hospitals, 74.7 % of the large hospitals and 65.8 % of the small hospitals used instruments for structuring the clinical ethics consultation and systematic reflection. Out of the 471 hospitals which have implemented a HEC, 79.2 % used an instrument.
93.2 % of the participants documented the results of the ethics case consultation in the form of a protocol. The entry in the patient record was used as a form of documentation by 46.8 % of the participants. 42.6 % of the respondents documented twice (protocol and patient record). Amongst the mid-size hospitals, 53.9 % used this method.
Statutes were established especially for the Hospital Ethics Committee (HEC). 471 (86.4 %) of the participants had implemented a HEC. 84.7 % of the participants with a HEC have a statute. In this respect, the size of the hospital is of significance (p = 0.01): The larger the hospital, the more likely it is to establish a statute. 70.0 % of the small hospitals and 87.3 % of the large hospitals had a statute. There is no significant correlation between the type of hospital operation and the existence of a statute. Activity reports were created mainly by subscribers with a HEC. 34.2 % out of the 471 participants with a HEC have written an annual report and 23.4 % are planning to do so. The size of the hospital is significant in this regard (p = 0.03): The larger the hospital, the more likely it is to have written an annual report. In 24.5 % of the small hospitals and 41.8 % of the large hospitals an annual report had been written. We could not ascertain a significant connection between the type of hospital operation and the existence of annual reports.
A budget is available for 21.7 % of the participants who have implemented a structure of clinical ethics consultation. 17.8 % of the denominational hospitals and 24.4 % of the non-denominational hospitals reported to have such a budget. The type of hospital operation is of no significance here (p = 0.25). The size of the hospital correlates with the existence of a budget (p = 0.002). Whereas a budget is available in 16.0 % of the small hospitals, 22.2 % of the mid-size hospitals and 34.2 % of the large hospitals have one.
Discussion
One important task is the implementation of ethics case consultation (AEM 2010). A large majority (90.8 %) of the implemented structures of clinical ethics consultation conduct the same. It turns out however that 9.2 % of the participants did not conduct any clinical ethics consultation. This is partly due to lack of requests from the treatment team, the patients or the relatives. Further reasons might be the reservations among physicians (Schochow et al. 2015) or limited time resources.
The implementation of ethics training regarding issues of medical and nursing ethics is an essential task of structures of clinical ethics consultation (AEM 2010). Nevertheless, almost one third (28.1 %) of the participants with an implemented structure of clinical ethics consultation are not responsible for ethics training. This leaves opportunities to raise awareness for ethical issues unused (Kinlaw 2012). Not only are there ethical issues in clinical practice that cannot consequently be identified but skills in dealing with ethical conflicts are also lacking (AEM 2010). Furthermore, there is a preventive dimension to ethics education that has to be considered (Parsi 2012).
Ethical guidelines are recommendations for how to cope with recurring situations, such as dealing with living wills (AEM 2010; Flicker et al. 2014; Neitzke et al. 2015). Nearly one third (28.3 %) of the structures of clinical ethics consultation are not responsible for establishing ethical guidelines. As a result of this lack, guidance for both the treatment team and the team of clinical ethics consultants is not available. But ethical guidelines do not always provide answers in every individual situation. The treatment team and the team of clinical ethics consultants should therefore be notified of the terms of ethical issues in training (Roberts and Reicherter 2015).
Clinical ethics case consultation as defined by the AEM aims at structuring and reflecting the consultation process (AEM 2010). The application of a structure instrument can help to conduct a clinical ethics consultation (Steinkamp 2012). Only 64.9 % of the implemented structures of clinical ethics consultation actually use structure instruments. A critical attitude towards their usage is thus discernible. Moreover, it should be noted that the use of structure instruments cannot replace a qualification of the ethics consultants (Andereck et al. 2012; Wasson et al. 2015). The activities of clinical ethics consultation predominantly comply with the tasks and goals of the standards of the AEM.
According to the recommendations of the working group of the AEM, the results of an ethics case consultation should be documented in the medical records (Schochow et al. 2015). The documentation is important because the results of an ethics case consultation have a concrete impact on the further treatment or care of the patients. Result reports are often made using the form of a protocol. As our survey shows, the documentation is mainly implemented in the form of protocols (93.2 %) and registrations in the patient record (46.8 %). It should be noted that 42.6 % of the participants have two sets of documents. Against the background of these results, we can reconstruct that more than 90 % of the participants with a structure of clinical ethics consultation create the appropriate documents during practice.
According to the recommendations for the evaluation made by the working group of the AEM, a statute and/or rules of procedure is necessary for structures of clinical ethics consultation (Pfäfflin et al. 2009; Neitzke et al. 2013). The statute should especially regulate the goals and tasks, the composition, the reporting as well as documentation requirements. Statutes are created primarily for the HEC. Almost 85 % of the implemented HEC have a statute. Especially in large hospitals which had implemented a HEC, statutes existed, thus creating the foundations for quality and transparency. Most of the major hospitals with an implemented HEC have established statutes. This fulfils the crucial requirement for quality and transparency.
The various activities of the structure of clinical ethics case consultation should be documented in an appropriate manner in order to, for example, evaluate them for the purpose of quality assurance. A regular (e.g. annual) activity report is recommended by the working group of the AEM (Neitzke et al. 2013). Almost half of all HEC do not submit any annual reports (42.2 %). Annual reports are a possibility to document the activities of the structure of clinical ethics consultation for the hospital management. Regular activity reports are a part of assuring the quality. They should hence be submitted at least once a year. The recommendations for evaluation should be improved in practice.
In its recommendations, the AEM emphasizes that the financial endowment should be discussed with the management when appointing the members of a structure for clinical ethics consultation (Neitzke et al. 2013). Most structures of clinical ethics consultation do not have a budget so far. Large hospitals more often equip their structures for clinical ethics consultation with a budget compared to small hospitals. This has an impact on the staffing and the implementation of the tasks of clinical ethics consultation.
All of the 654 questionnaires that were received could be included in the evaluation. 15 participants did not provide information concerning hospital operations. The response rate of 35.2 % exceeds other hospital surveys by far (Dörries and Hespe-Jungesblut 2007). Especially the response rates of mid-size hospitals (58.9 %), large hospitals (66.9 %), and denominational hospitals (36.4 %) allow for generalizations. On the whole, the questions were answered fully and conclusively, whereby it cannot be determined to what extent ideas with regard to structures of clinical ethics consultation might vary.
References
AEM, Vorstand der Akademie für Ethik in der Medizin e.V. (2010). Standards für Ethikberatung in Einrichtungen des Gesundheitswesens. Ethik in der Medizin, 22, 149–153.
Andereck, W. S., McGaughey, J. W., & Jonsen, A. R. (2012). The clinical ethics consultant: verifying the qualifications of a new type of practitioner in a community hospital. Journal of Healthcare Management/American College of Healthcare Executives, 57(4), 264–273.
ASBH, American Society for Bioethics and Humanities. (2011). Core competencies for healthcare ethics consultation (2nd ed.). Glenview: ASBH.
Dörries, A., & Hespe-Jungesblut, K. (2007). Die Implementierung Klinischer Ethikberatung in Deutschland. Ergebnisse einer bundesweiten Umfrage bei Krankenhäusern. Ethik in der Medizin, 19, 148–156.
Fahr, U., Herrmann, B., May, A. T., Reinhardt-Gilmour, A., & Winkler, E. C. (2011). Empfehlungen für die Dokumentation von Ethik-Fallberatungen. Ethik in der Medizin, 23, 155–159.
Flicker, L. S., Rose, S. L., Eves, M. M., Flamm, A. L., Sanghani, R., & Smith, M. L. (2014). Developing and testing a checklist to enhance quality in clinical ethics consultation. The Journal of Clinical Ethics, 25(4), 281–290.
Fox, E., Myers, S., & Pearlman, R. A. (2007). Ethics consultation in United States hospitals: A national survey. American Journal of Bioethics, 7, 13–25.
Hester, D. M., & Schonfeld, T. (2012). Introduction to healthcare ethics committees. In D. M. Hester & T. Schonfeld (Eds.), Guidance for healthcare ethics committees (pp. 1–8). Cambridge: Cambridge University Press.
Kinlaw, K. (2012). The healthcare ethics committee as educator. In D. M. Hester & T. Schonfeld (Eds.), Guidance for healthcare ethics committees (pp. 155–163). Cambridge: Cambridge University Press.
Neitzke, G., Riedel, A., Brombacher, L., Heinemann, W., & Herrmann, B. (2015). Empfehlungen zur Erstellung von Ethikleitlinien in Einrichtungen des Gesundheitswesens. Ethik in der Medizin, 27, 241–248.
Neitzke, G., Riedel, A., Dinges, S., Fahr, U., & May, A. T. (2013). Empfehlungen zur Evaluation von Ethikberatung in Einrichtungen des Gesundheitswesens. Ethik in der Medizin, 25, 149–156.
Parsi, K. (2012). Education as prevention. In D. M. Hester & T. Schonfeld (Eds.), Guidance for healthcare ethics committees (pp. 164–171). Cambridge: Cambridge University Press.
Pfäfflin, M., Kobert, K., & Reiter-Theil, S. (2009). Evaluating clinical ethics consultation. A European perspective. Cambridge Quarterly of Healthcare Ethics, 18(4), 406–419.
Roberts, L. W., & Reicherter, D. (Eds.). (2015). Professionalism and ethics in medicine. A study guide for physicians and physicians-in-training. New York, NY: Springer.
Schochow, M., Schnell, D., & Steger, F. (2015). Implementation of clinical ethics consultation in German hospitals. Science and Engineering Ethics. doi:10.1007/s11948-015-9709-2.
Steinkamp, N. (2012). Methoden ethischer Entscheidung im Pflegealltag. In S. Monteverde (Ed.), Handbuch Pflegeethik. Ethisch denken und handeln in den Praxisfeldern der Pflege (pp. 175–192). Stuttgart: Kohlhammer.
Tarzian, A. J., Wocial, L. D., & The ASBH Clinical Ethics Consultation Affairs Committee. (2015). A code of ethics for health care ethics consultants. Journey to the present and implications for the field. The American Journal of Bioethics, 15, 38–51.
Wasson, K., Parsi, K., McCarthy, M., Siddall, V. J., & Kuczewski, M. (2015). Developing an evaluation tool for assessing clinical ethics consultation skills in simulation based education: The ACES project. HealthCare Ethics Committee Forum, 28, 103–113.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schochow, M., Rubeis, G. & Steger, F. The Application of Standards and Recommendations to Clinical Ethics Consultation in Practice: An Evaluation at German Hospitals. Sci Eng Ethics 23, 793–799 (2017). https://doi.org/10.1007/s11948-016-9805-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11948-016-9805-y