Abstract
Purpose of review
We investigate the complexities and interplay between the concepts of prognostic uncertainty and patient preferences as they relate to the delivery of goal-concordant care to patients with severe acute brain injuries (SABI) in the Neurological Intensive Care Unit (Neuro-ICU).
Recent findings
Patients with SABI in the Neuro-ICU have unique palliative care needs due to sudden, often unexpected changes in personhood and quality of life. A substantial amount of uncertainty is inherent and poses a challenge to both the patient’s prognosis and treatment preferences. The delivery of goal-concordant care can be difficult to achieve.
Summary
The uncertainty inherent to both prognosis and patient preferences challenges the provision of goal-concordant care to patients with SABI. The best case/worst case/most likely case scenario is a communication strategy that can aid clinicians when discussing the patient’s uncertain prognosis. A time-limited trial may provide a framework for families and clinicians to pursue aggressive life-sustaining treatment for a certain amount of time, in which prognosis may become more defined, patient goals may become clearer, and clinicians and families may establish a common ground. Although the delivery of goal-concordant care in the Neuro-ICU may be an unachievable, lofty goal, it is a level of care that we should continue to strive for and discuss.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Severe acute brain injuries (SABI), such as stroke, traumatic brain injury, and hypoxic-ischemic encephalopathy after cardiac arrest, present a unique challenge to patients, families, and clinicians given the sudden presentation of life-altering deficits, the threat to the patient’s personhood and quality of life, and the substantial prognostic uncertainty regarding mortality and morbidity. These patients are also typically unable to communicate their needs or to participate in decisions about their care, which places this important responsibility on their family members [1]. Although a spectrum of disease exists, patients often present acutely neurologically devastated, where life or death depends on immediate complex decisions including the utilization of life-saving treatments, surgical interventions, and transfers from community hospitals to urban or academic centers for higher levels of care. Even after early survival, patients in the Neurological Intensive Care Unit (Neuro-ICU) are frequently unable to participate in decisions in their care as prolonged life-sustaining treatments, including percutaneous endoscopic gastrostomy, tracheostomy, or ventriculoperitoneal shunt placement, are considered. Highly consequential treatment decisions are often time sensitive and must be made in a fast-paced environment, where clinicians and family members engage in a shared decision-making process that requires mutual trust and substituted judgment on the patient’s preferences and values as well as expected outcomes [2, 3].
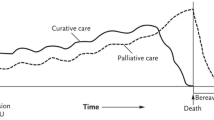
Due to these complexities, a palliative care approach, meaning the holistic and expert communication and management of the physical, psychosocial, and existential needs of patients and families, is fundamental to the care of patients with SABI in the Neuro-ICU.
In this chapter, we focus on concepts that are central to the palliative care approach and discuss challenges and opportunities to providing goal-concordant care in the Neuro-ICU. Goal-concordant care is the careful assessment of a patient’s goals, values, and personhood so that patients, their families and clinicians can develop a treatment plan that prioritizes and most likely supports what is most important to the patient [4]. We review relevant literature, discuss challenges, and provide suggestions to navigate prognostic uncertainty and patient preferences and the resulting family distress, as they relate to the delivery of goal-concordant care for patients with SABI.
Prognostic uncertainty
Prognostic uncertainty after SABI applies not only to a patient’s likelihood of surviving but, perhaps to even a larger extent, to their likelihood of recovering to a state that they might consider to be “a meaningful life.” We consider three aspects of this uncertainty: first, the uncertainty around the degree of functional recovery; second, the uncertainty around a patient’s presumed wishes about medical treatment; and third, the uncertainty about to what degree a patient and their loved ones may adapt to a future health state [5]. The lack of certainty in predicting a patients’ recovery course can lead to an emotionally difficult and ambiguity-filled decision-making process for families [6]. When substantial prognostic uncertainty persists, especially in the early stages of SABI, current guidelines recommend “aggressive” therapies for those without advance directives to the contrary [7]. Recently published guidelines by the Neurocritical Care Society highlight scales and scores to aid clinicians with predictions regarding the need for certain interventions and offering reasonably accurate chances of functional recovery [8, 9]. However, as the guidelines allude to, several limitations preclude the ability to provide a clear prognosis [8, 9]. Such limitations may include, among others, the lack of long-term follow-up as well as lack of patient-centered outcome assessments in most studies, the confounding effect of withdrawal of life-sustaining treatment practices and self-fulfilling prophecies [10, 11], and the impact of socioeconomic inequities and racism in healthcare. This lack of evidence and clear guidelines leads to substantial practice variation across clinicians, hospitals, and regions [12,13,14,15].
One method of addressing the prognostic uncertainty for SABI is the concept of a time-limited trial (TLT) [16]. Instead of providing treatment options as a dichotomous choice between the life-sustaining vs. the comfort-focused pathway, a TLT of certain and transient life-sustaining therapies may offer a structured compromise [17]: A TLT is an agreement between the clinician and the surrogate decision-makers that outlines specific treatments that may be pursued for an agreed upon amount of time and an agreed upon change in the patient’s condition [16]. If the patient’s recovery trajectory is promising as defined by previously agreed-on signs and symptoms, life-sustaining treatment would be continued; if their clinical condition worsens or prognosis becomes more certain towards an unacceptable health state due to lack of recovery or other signs, further escalations of care may be avoided, life-sustaining treatments stopped, and care transitioned towards an exclusive focus on comfort [16]. The clinician and surrogate decision-maker should also agree on what to do next if the patient’s clinical condition remains the same, or no clarity regarding prognosis is available [18]. It is important that the clinician provides objective measures for clinical improvement or decline and specifies endpoints to the family members to set expectations as they, too, monitor the patient, and to establish agreement as to whether clinical criteria of the TLT have been met. These trials include family meetings to allow exploration and revisiting of patient preferences and values, to provide the family with time to cope and adjust to the patient’s condition, to allow rapport- or trust-building between clinicians and surrogate decision-makers, to provide longitudinal support and continuity of care to the surrogate decision-makers, and to acknowledge and reassess the uncertainty that is inherently a part of the shared decision-making process [18]. A TLT can also provide the family with the temporary option to give the patient a chance at recovery without indefinitely prolonging suffering [16]. One multicenter, prospective quality improvement project in medical ICUs aimed to use TLTs to decrease the use of nonbeneficial ICU care [19•]. Their results suggested that family meetings during the postintervention period, when compared to the preintervention period, were more likely to include discussion about risk and benefits of treatment options, patient preferences and values, and clinical measures of improvement; ICU length of stay was decreased; and utilization of invasive ICU procedures was decreased [19•]. Possible barriers for clinicians to conducting a TLT include the following: clinicians and families are not able to agree upon a time limit; surrogate decision-makers request additional time; the lack of continuity due to clinicians’ rotating schedules; and unexpected fluctuations in the patient’s condition [20]. Also, surrogate decision-makers may adjust their expectations and refine the goals of care as they follow the patients’ trajectory. The shortage of guidelines regarding which clinical outcomes to track and the optimal length of a TLT based upon evidence about expected recovery time frames has been noted as a barrier to the use of TLTs by ICU clinicians [21]. Further investigation, specifically in patients with SABI, is needed to determine the effectiveness of well-structured TLTs on improving emotional and psychological well-being for family members and achieving goal-concordant care. Such investigation may also include evaluating the effectiveness of including palliative care or neuropalliative care specialist teams in these family meetings and in the structure and follow-up of TLTs.
Further complicating prognostic uncertainty is the concept of prognostic discordance, where clinicians and family members have different perceptions or expectations for the patient’s recovery. One observational cohort study of patients with SABI found that—early in the ICU course—the predictions of a patient’s likelihood for recovery to independence were substantially different between families, nurses, and physicians, with families tending to be more optimistic about recovery [22•]. Compared to families who identified as non-Hispanic White, prognostic discordance was significantly more common with families who self-reported as non-White or Hispanic [23•]. These studies also distinguished between different types of discordance: “misunderstanding” is the difference between what the clinician predicts and what the family thinks the clinician predicts and may be due to miscommunication. A potential disconnect between how clinicians deliver the prognosis and how the families wish to optimally receive the information could contribute to “misunderstanding.” For example, family members of patients with traumatic brain injury have indicated a preference towards number-based projections believing that it would be more concrete and limit the amount of uncertainty, whereas physicians avoided number estimates, as it may promote false hope, may be difficult for family to interpret, and may also be inaccurate or biased [24]. A recent cross-sectional, mixed-methods study analyzed the language used by clinicians when presenting a prognosis during a family meeting for patients in the Neuro-ICU [25]. Most of the statements made by clinicians about survival, physical function, cognition, and overall recovery (62%) did not include information about the likelihood of the outcome occurring, and only 2% of the statements included a numeric estimate [25]. “Belief discordance” is the difference between what the family thinks the clinician predicted and what the family predicts themselves and suggests that a person’s own beliefs influence their prognostic assessment to supersede the clinician’s estimate [22•, 23•, 26]. When formulating their own opinions of the patient’s prognosis, families consider “not just what the doctor tells” them, but also their beliefs regarding their loved one’s will to live, the patient’s or other loved ones’ past experiences surviving a poor prognosis, the patient’s physical appearance, the effect of having family at the patient’s side, and their own optimism, spirituality, and core beliefs [27]. Although they may contribute to prognostic discordance, none of these factors seems inappropriate for family members to consider in the acute or subacute phases of illness and should be incorporated into prognosis communication, supporting the family in the process of coping, and shared decision-making in the ICU.
One option that incorporates prognostic uncertainty into the communication model is the best case/worst case/most likely case framework [28]. In this framework, which is an adaptation of scenario planning, an illustration is used in conjunction with stories to describe what the patient may experience in the best case, worst case, and most likely case with each treatment option or throughout their clinical course [29]. Without knowing the likelihood of each, presenting the best anticipated recovery and the worst anticipated case for the patient’s prognosis can provide the family with a range of realistic expectations, where the “most likely case” is usually somewhere in between. As the patient’s hospital course progresses, the gap between the two scenarios should narrow and the “true/most likely” prognosis become clearer. This method has been described in numerous settings, including during the COVID-19 pandemic [30], when making decisions regarding potentially risky surgical interventions [29], and in the trauma ICU [31•]. Use of this framework resulted in a clearer presentation of treatment options, offered a variety of protentional clinical trajectories, created a more active discussion with family members, and resulted in significantly improved end-of-life communication scores [29, 31•]. However, a small randomized, double-blinded study comparing the use of the best case/worst case to the more traditional risk/benefit framework when presenting palliative surgical options to patients with advanced cancer found that patients had no difference in preference between the two models [32]. Potential downsides to the use of this model are that it is susceptible to increased subjectivity due to the potential biases of the clinician completing the discussion [33], and clinicians have found it monotonous to integrate into daily ICU rounds on every patient [31•]. Future research is needed to investigate if the framework can be successfully adapted for use with patients suffering from SABI.
Patient preferences
Identification of patient preference is a key element of the shared decision-making process. A qualitative analysis of recordings of ICU family meetings suggested that more than 88% of meetings contained no discourse regarding the patient’s desire for autonomy, independence, emotional well-being, relationships, physical function, cognitive function, or spirituality [34]. In a study assessing a different cohort of audio-recorded family meetings, the same research group found that clinicians used the patients’ values to make a treatment plan in only 8.2% of conferences [35]. Understanding patient preferences requires using information about a patient’s past-self to predict a patient’s comfort with a future-self with a new, likely poor, functional status [5]. Clinicians may want to explore who the patient was before the SABI and what was most important to them. It is also important to establish what the patient might be willing and able to endure in order to potentially achieve a recovery that allows them to at least some extent participate in what is important to them.
Ideally, discussions around artificial life support would have previously occurred in the primary care setting in the form of advance care planning documents. However, patients presenting with SABI rarely have advance directives [36, 37•], and even if an advance directive is present, it often fails to appropriately address the unique circumstances of SABI [36]. Therefore, clinicians often have to rely heavily on second-hand information about the patient provided by family members through their own lens. When eliciting patient preferences during family meetings, it is a key to gather an understanding of the patients’ priorities for their general health and well-being and not just regarding certain treatment options [38]. It is also important to consider the patient’s priorities within the context of their religious beliefs, cultural backgrounds, and prior experience with similar illnesses. This may take the form of conversations generally about desired future physical, cognitive, and social functional status that then become more focused on specific priorities or activities [35]. Preferences may include a desire to live until a particular date or event or as long as possible, or patients may draw the line at being able to live at home vs. a hospital or institution; they may prioritize the relief of pain over survival or even wakefulness and the ability to participate in certain activities that they previously enjoyed or valued or to communicate with others [39].
Few studies have focused on patient preferences specifically in the setting of SABI. In one single center, prospective, cohort study, over one half (55%) of families of patients with SABI perceived that their loved one would “prefer a plan of medical care that focuses on extending life as much as possible” vs. “a plan of medical care that focuses on comfort and would limit life-saving treatments” (33%) or “unsure” (12%) [37•]. Identifying comfort as a preference was more likely among non-Hispanic White patients and those with higher illness severity [37•]. The finding that patients categorized as non-White or Hispanic compared to non-Hispanic White patients were less likely to prefer comfort-focused care requires future investigation. Another large study randomized healthy adults to the role of surrogate decision-maker for a hypothetical patient with a recovery from SABI that either resulted in being in a severe functionally disabled state or staying in a vegetative state [40]. For the patients with severe functional disability, 15% of the surrogates chose life sustaining treatment; for the patients in a persistent vegetative state, 11.4% of families chose life sustaining treatment, which was not significantly different between the groups [40]. In both scenarios, surrogate decision-makers who chose life-sustaining treatment expressed more uncertainty about their choice than those who chose comfort-care measures [41].
Even in situations where the patient’s preferences are clearly understood and defined, devising a treatment plan that aligns with these preferences remains challenging. For example, some treatments may be viewed as both life-sustaining or comfort-focused depending on the clinical context and the patient’s underlying co-morbidities. Young et al. present a case of a gentleman with terminal cancer who underwent an emergent thrombectomy after suffering a devasting acute ischemic stroke [42]. Although thrombectomy is traditionally thought of as life-sustaining, in this case, the thrombectomy was considered “palliative,” as the goal was to minimize the amount of suffering for the patient near the end of his life [42]. Even when a patient with a neurological emergency has previous completed ACP documentation, surrogate decision-makers may reverse them in order to pursue what they believe aligns with the patient’s values regarding a specific disease process and treatment option. A small retrospective chart review suggests that reversals of ACP documentation can lead to a mixture of clinical outcomes, ranging from death to independent living, and may be necessary in order to provide goal-concordant care [43].
Family distress
As most patients with SABI are unable to participate in the formulation of their care plan, this vital role is filled by family members or other surrogate decision-makers. Fulfillment of this responsibility can have significant immediate and prolonged impacts on the individual. In one large prospective cohort study of family members of patients with SABI, one-half of the family members suffered from moderate anxiety or depression during the patient’s acute hospitalization, and 20% of family members continued with the same level of distress at 6-month follow-up [44]. In another study of patients who required prolonged mechanical ventilation, those with SABI vs. those with non-neurological critical illness had more severe symptoms of anxiety and depression 6 months after hospitalization [45]. After discharge from the hospital, family members often have difficulty adjusting to a new, often unexpected or undesired, normal and yearned for ongoing support from clinicians during the recovery phase, especially when the prospect of new treatment decisions arose [46]. Due to the documented severe effects of the patient’s condition on the family members, numerous family-centered interventions have been developed and tested with mixed results. Randomized clinical trials investigating multifaceted family-support interventions [47,48,49] have shown promising results that require further research. Unaddressed emotional and psychological distress can make the surrogate decision-maker’s already unthinkable task of formulating a goal-concordant treatment plan by navigating the uncertainty of the patient’s prognosis and preferences nearly impossible.
Goal-concordant care
Providing goal-concordant care requires that the entire healthcare team aligns a patient’s treatment options with their personal goals and values and gives them the potential for their personal optimal clinical course. Goal-concordant care is delivered when the treatment that a patient receives is directed at achieving what is most important to them while avoiding interventions or symptoms that are inconsistent with this patient’s values or goals. For instance, if a patient has stated that they would only want to live if they were able to communicate with their family and be cognitively reasonably intact, and 2 weeks into their hospital stay they have started to awaken and say a few words, then prolonged life support in terms of gastrostomy for continued artificial nutrition and hydration could appear goal-concordant at the time—they may, however, also have suggested “never” wanting to be in a nursing home, in which case a time-limited trial of gastrostomy and nursing home for a month or three could be considered but only with a clear agreement to revisit this pathway at follow-up visits over the ensuing months—is the patient continuing to recover and how realistic is it that they will regain the stated level of recovery? Has this goal changed? Not having an expected clinical course or knowing the exact outcome of the treatments that are being contemplated makes it incredibly difficult to develop a treatment plan that provides goal-concordant care and makes it an ongoing, iterative process. In fact, in one qualitative study, some surrogate decision-makers of patients with SABI felt that prognostic uncertainty caused them to feel that there was not even a decision for them to make [50]. Another qualitative study interviewed surrogate decision-makers of patients with SABI who had undergone tracheostomy. In retrospect, these family members did not seem to perceive the tracheostomy as a choice, because the only alternative would have been death [51]. In addition, research is needed to determine the role of clinician bias when attempting to provide goal-concordant care in the setting of uncertainty. Although it is important to acknowledge the overwhelming amount of uncertainty when discussing goal-concordant care with families, it is equally important to concretely address what is known with a reasonable amount of certainty in terms of both patient preferences and prognosis. This may include a certainty that a patient will require time in the nursing home before potentially reaching a level of recovery that will allow them to return home or a certainty that they will be dependent on artificial nutrition and hydration for a certain amount of time.
As difficult as goal-concordant care has been to achieve clinically, it has also proved difficult to quantitatively measure in research. Some studies have used surrogate end-points to measure goal-concordance, such as agreement between physician decision and patient preference for withholding care; duration of ICU admission, mechanical ventilation, and comatose state; and presence and severity of the patients’ pain [52]. In the fast-paced intensive care unit, where survival is priority, goal-discordant care may not always be inappropriate, if provided for a limited amount of time. When asked, many surrogates will say that their loved one would prioritize comfort over longevity, but will also recognize that the care their loved one is receiving is prioritizing longevity over comfort [37•]. These are important areas for clinicians and families to explore. Clinicians and patients or surrogate decision-makers may also have different definitions and concepts of goal-concordant care. In a large, multicenter, prospective, cohort study of older adult patients who were unable to participate in their treatment decisions on a general medical service and in the medical ICU, surrogates were asked to place the patient’s treatment preferences in one of three categories: comfort-focused, life-sustaining, or intermediate [53]. Almost half of the patients (46.6%) received at least one intervention that did not align with the surrogate’s stated goals-of-care [53]. One of the strengths of this study was the use of an intermediate group despite the fact that many in this group were still “full code” [53]. Future research should investigate further the preferences of this intermediate group and treatment options that they are willing to pursue.
Conclusion
The delivery of goal-concordant care in the neurocritical care unit may be a lofty goal that is unlikely to ever be fully achieved. However, improvements in communication, such as with the use of the “best case/worst case/most likely case” framework, and the use of TLTs may move us closer to providing goal-concordant care. Research specific to SABI is urgently needed to improve our ability to prognosticate, find better ways to support family members and shared decision-making, and better understand the importance of goal-concordant care.
Availability of data and materials
Not applicable.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Creutzfeldt CJ, Engelberg RA, Healey L, et al. Palliative care needs in the Neuro-ICU. Crit Care Med. 2015;43(8):1677–84. https://doi.org/10.1097/CCM.0000000000001018.
Curtis JR, White DB. Practical guidance for evidence-based ICU family conferences. Chest. 2008;134(4):835–43. https://doi.org/10.1378/chest.08-0235.
Curtis JR, Vincent JL. Ethics and end-of-life care for adults in the intensive care unit. Lancet. 2010;376(9749):1347–53. https://doi.org/10.1016/S0140-6736(10)60143-2.
Halpern SD. Goal-concordant care - searching for the holy grail. N Engl J Med. 2019;381(17):1603–6. https://doi.org/10.1056/NEJMp1908153.
Creutzfeldt CJ, Holloway RG. Treatment decisions for a future self: ethical obligations to guide truly informed choices. JAMA. 2020;323(2):115–6. https://doi.org/10.1001/jama.2019.19652.
Jones K, Quinn T, Mazor KM, Muehlschlegel S. Prognostic uncertainty in critically ill patients with traumatic brain injury: a multicenter qualitative study. Neurocrit Care. 2021;35(2):311–21. https://doi.org/10.1007/s12028-021-01230-3.
Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53(7):e282–361. https://doi.org/10.1161/STR.0000000000000407.
Busl KM, Fried H, Muehlschlegel S, et al. Guidelines for neuroprognostication in adults with guillain-barré syndrome [published correction appears in Neurocrit Care. Neurocrit Care. 2023;38(3):564–583. https://doi.org/10.1007/s12028-023-01707-3.
Rajajee V, Muehlschlegel S, Wartenberg KE, et al. Guidelines for neuroprognostication in comatose adult survivors of cardiac arrest. Neurocrit Care. 2023;38(3):533–63. https://doi.org/10.1007/s12028-023-01688-3.
Becker KJ, Baxter AB, Cohen WA, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56(6):766–72. https://doi.org/10.1212/wnl.56.6.766.
Creutzfeldt CJ, Becker KJ, Weinstein JR, et al. Do-not-attempt-resuscitation orders and prognostic models for intraparenchymal hemorrhage. Crit Care Med. 2011;39(1):158–62. https://doi.org/10.1097/CCM.0b013e3181fb7b49.
Huijben JA, Volovici V, Cnossen MC, et al. Variation in general supportive and preventive intensive care management of traumatic brain injury: a survey in 66 neurotrauma centers participating in the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) study. Crit Care. 2018;22(1):90. Published 2018 Apr 13. https://doi.org/10.1186/s13054-018-2000-6.
George BP, Kelly AG, Schneider EB, Holloway RG. Current practices in feeding tube placement for US acute ischemic stroke inpatients. Neurology. 2014;83(10):874–82. https://doi.org/10.1212/WNL.0000000000000764.
Krishnamoorthy V, Hough CL, Vavilala MS, et al. Tracheostomy after severe acute brain injury: trends and variability in the USA. Neurocrit Care. 2019;30(3):546–54. https://doi.org/10.1007/s12028-019-00697-5.
Kelly AG, Zahuranec DB, Holloway RG, Morgenstern LB, Burke JF. Variation in do-not-resuscitate orders for patients with ischemic stroke: implications for national hospital comparisons. Stroke. 2014;45(3):822–7. https://doi.org/10.1161/STROKEAHA.113.004573.
Quill TE, Holloway R. Time-limited trials near the end of life. JAMA. 2011;306(13):1483–4. https://doi.org/10.1001/jama.2011.1413.
VanKerkhoff TD, Viglianti EM, Detsky ME, Kruser JM. Time-limited trials in the intensive care unit to promote goal-concordant patient care. Clin Pulm Med. 2019;26(5):141–5. https://doi.org/10.1097/cpm.0000000000000323.
Leiter RE, Tulsky JA. Time-limited trials and potentially nonbeneficial treatment in the ICU-willing to wait for it. JAMA Intern Med. 2021;181(6):795–6. https://doi.org/10.1001/jamainternmed.2021.0988.
• Chang DW, Neville TH, Parrish J, et al. Evaluation of time-limited trials among critically ill patients with advanced medical illnesses and reduction of nonbeneficial ICU treatments. JAMA Intern Med. 2021;181(6):786–794. https://doi.org/10.1001/jamainternmed.2021.1000. A prospective quality improvement study aiming to evaluate if time-limited trials for patients in the medical intensive care unit was associated with decreased length of stay in the ICU and usage of certain therapies. The use of time-limited trials was associated with less frequent invasive procedures, shorter length of stay in the ICU, and more family meetings that included discourse regarding risk and benefits of treatment options, eliciting of patient values, and establishing signs of clinical improvement.
Bruce CR, Liang C, Blumenthal-Barby JS, et al. Barriers and facilitators to initiating and completing time-limited trials in critical care. Crit Care Med. 2015;43(12):2535–43. https://doi.org/10.1097/CCM.0000000000001307.
Viglianti EM, Ervin JN, Newton CA, Kruser JM, Iwashyna TJ, Valley TS. Time-limited trials in the ICU: a mixed-methods sequential explanatory study of intensivists at two academic centres. BMJ Open. 2022;12(4):e059325. Published 2022 Apr 4. https://doi.org/10.1136/bmjopen-2021-059325.
• Kiker WA, Voumard RR, Plinke W, Longstreth WT Jr, Curtis JR, Creutzfeldt CJ. Prognosis predictions by families, physicians, and nurses of patients with severe acute brain injury: agreement and accuracy. Neurocrit Care. 2022;37(1):38–46. https://doi.org/10.1007/s12028-022-01501-7. The goal of the study was to analyze the prognostic predictions regarding recovery of patients with severe acute brain injury made by families, clinicians, and nurses. Families had significantly more optimistic predictions of recovery compared to both clinicians and nurses.
• Kiker WA, Rutz Voumard R, Andrews LIB, et al. Assessment of discordance between physicians and family members regarding prognosis in patients with severe acute brain injury. JAMA Netw Open. 2021;4(10):e2128991. Published 2021 Oct 1. https://doi.org/10.1001/jamanetworkopen.2021.28991. The goal of the study was to investigate prognosis discordance between clinicians and families of patients with severe acute brain injury. Discordance occurred with 61% of patients and was more common in non-white families compared to white families.
Quinn T, Moskowitz J, Khan MW, et al. What families need and physicians deliver: contrasting communication preferences between surrogate decision-makers and physicians during outcome prognostication in critically ill TBI patients. Neurocrit Care. 2017;27(2):154–62. https://doi.org/10.1007/s12028-017-0427-2.
Goss A, Ge C, Crawford S, et al. Prognostic language in critical neurologic illness: a multicenter mixed-methods study. Neurology. 2023;101(5):e558–69. https://doi.org/10.1212/WNL.0000000000207462.
White DB, Ernecoff N, Buddadhumaruk P, et al. Prevalence of and factors related to discordance about prognosis between physicians and surrogate decision makers of critically ill patients. JAMA. 2016;315(19):2086–94. https://doi.org/10.1001/jama.2016.5351.
Boyd EA, Lo B, Evans LR, et al. “It’s not just what the doctor tells me:” factors that influence surrogate decision-makers’ perceptions of prognosis. Crit Care Med. 2010;38(5):1270–5. https://doi.org/10.1097/CCM.0b013e3181d8a217.
Schwarze ML, Kehler JM, Campbell TC. Navigating high risk procedures with more than just a street map. J Palliat Med. 2013;16(10):1169–71. https://doi.org/10.1089/jpm.2013.0221.
Taylor LJ, Nabozny MJ, Steffens NM, et al. A framework to improve surgeon communication in high-stakes surgical decisions: best case/worst case. JAMA Surg. 2017;152(6):531–8. https://doi.org/10.1001/jamasurg.2016.5674.
Schwarze ML, Zelenski A, Baggett ND, et al. Best case/worst case: ICU (COVID-19)-a tool to communicate with families of critically ill patients with COVID-19. Palliat Med Rep. 2020;1(1):3–4. Published 2020 Apr 30. https://doi.org/10.1089/pmr.2020.0038.
• Zimmermann CJ, Zelenski AB, Buffington A, et al. Best case/worst case for the trauma ICU: development and pilot testing of a communication tool for older adults with traumatic injury. J Trauma Acute Care Surg. 2021;91(3):542–51. https://doi.org/10.1097/TA.0000000000003281. The ‘best case/worst case’ communication tool was evaluated in a pre-post study for use with older adults in the trauma intensive care unit. Use of this tool was associated with significant improvement in end-of-life communication score and resulted in less clinicians endorsed providing false hope.
Blumenthaler AN, Robinson KA, Hodge C, et al. Communication frameworks for palliative surgical consultations: a randomized study of advanced cancer patients [published online ahead of print, 2023 Feb 21]. Ann Surg. 2023. https://doi.org/10.1097/SLA.0000000000005823.
Kruser JM, Nabozny MJ, Steffens NM, et al. “Best case/worst case”: qualitative evaluation of a novel communication tool for difficult in-the-moment surgical decisions. J Am Geriatr Soc. 2015;63(9):1805–11. https://doi.org/10.1111/jgs.13615.
Scheunemann LP, Cunningham TV, Arnold RM, Buddadhumaruk P, White DB. How clinicians discuss critically ill patients’ preferences and values with surrogates: an empirical analysis. Crit Care Med. 2015;43(4):757–64. https://doi.org/10.1097/CCM.0000000000000772.
Scheunemann LP, Ernecoff NC, Buddadhumaruk P, et al. Clinician-family communication about patients’ values and preferences in intensive care units. JAMA Intern Med. 2019;179(5):676–84. https://doi.org/10.1001/jamainternmed.2019.0027.
Alonso A, Dörr D, Szabo K. Critical appraisal of advance directives given by patients with fatal acute stroke: an observational cohort study. BMC Med Ethics. 2017;18(1):7. Published 2017 Feb 2. https://doi.org/10.1186/s12910-016-0166-5.
• Rutz Voumard R, Dugger KM, Kiker WA, et al. Goal-concordant care after severe acute brain injury. Front Neurol. 2021;12:710783. Published 2021 Sep 17. https://doi.org/10.3389/fneur.2021.710783. This study compared the goals-of-care of patients with severe acute brain injury with the treatment that they received in the intensive care unit. 88% of patients who had the goal of extending life were receiving care that was in line with this goal, while only 27% of patients who prioritized receiving care that optimized comfort and quality of life received such care.
Taylor LJ, Johnson SK, Nabozny MJ, et al. Barriers to goal-concordant care for older patients with acute surgical illness: communication patterns extrinsic to decision aids. Ann Surg. 2018;267(4):677–82. https://doi.org/10.1097/SLA.0000000000002282.
Ahmad SR, Tarabochia AD, Budahn L, et al. Determining goal concordant care in the intensive care unit using electronic health records. J Pain Symptom Manage. 2023;65(3):e199–205. https://doi.org/10.1016/j.jpainsymman.2022.11.002.
Hwang DY, Knies AK, Mampre D, et al. Concerns of surrogate decision makers for patients with acute brain injury: a US population survey. Neurology. 2020;94(19):e2054–68. https://doi.org/10.1212/WNL.0000000000009406.
Garg A, Soto AL, Knies AK, et al. Predictors of surrogate decision makers selecting life-sustaining therapy for severe acute brain injury patients: an analysis of US population survey data. Neurocrit Care. 2021;35(2):468–79. https://doi.org/10.1007/s12028-021-01200-9.
Young MJ, Regenhardt RW, Sokol LL, Leslie-Mazwi TM. When should neuroendovascular care for patients with acute stroke be palliative? AMA J Ethics. 2021;23(10):E783–E793. Published 2021 Oct 1. https://doi.org/10.1001/amajethics.2021.783.
McHugh DC, George BP, Bender MT, et al. Reversal of advanced directives in neurologic emergencies. Neurohospitalist. 2022;12(4):651–8. https://doi.org/10.1177/19418744221097348.
Plinke WV, Buchbinder SA, Brumback LC, et al. Identification of palliative care needs and mental health outcomes among family members of patients with severe acute brain injury. JAMA Netw Open. 2023;6(4):e239949. Published 2023 Apr 3. https://doi.org/10.1001/jamanetworkopen.2023.9949.
Wendlandt B, Olm-Shipman C, Ceppe A, et al. Surrogates of patients with severe acute brain injury experience persistent anxiety and depression over the 6 months after ICU admission. J Pain Symptom Manage. 2022;63(6):e633–9. https://doi.org/10.1016/j.jpainsymman.2022.02.336.
RutzVoumard R, Kiker WA, Dugger KM, et al. Adapting to a new normal after severe acute brain injury: an observational cohort using a sequential explanatory design. Crit Care Med. 2021;49(8):1322–32. https://doi.org/10.1097/CCM.0000000000004947.
White DB, Angus DC, Shields AM, et al. A randomized trial of a family-support intervention in intensive care units. N Engl J Med. 2018;378(25):2365–75. https://doi.org/10.1056/NEJMoa1802637.
Torke AM, Varner-Perez SE, Burke ES, et al. Effects of spiritual care on well-being of intensive care family surrogates: a clinical trial. J Pain Symptom Manage. 2023;65(4):296–307. https://doi.org/10.1016/j.jpainsymman.2022.12.007.
Curtis JR, Treece PD, Nielsen EL, et al. Randomized trial of communication facilitators to reduce family distress and intensity of end-of-life care. Am J Respir Crit Care Med. 2016;193(2):154–62. https://doi.org/10.1164/rccm.201505-0900OC.
Goss AL, Voumard RR, Engelberg RA, Curtis JR, Creutzfeldt CJ. Do they have a choice? Surrogate decision-making after severe acute brain injury. Crit Care Med. 2023;51(7):924–35. https://doi.org/10.1097/CCM.0000000000005850.
Lou W, Granstein JH, Wabl R, Singh A, Wahlster S, Creutzfeldt CJ. Taking a chance to recover: families look back on the decision to pursue tracheostomy after severe acute brain injury. Neurocrit Care. 2022;36(2):504–10. https://doi.org/10.1007/s12028-021-01335-9.
Connors AF, Dawson NV, Desbiens NA, et al. A controlled trial to improve care for seriously ill hospitalized patients: the study to understand prognoses and preferences for outcomes and risks of treatments (support). JAMA. 1995;274:1591–8. https://doi.org/10.1001/jama.1995.03530200027032.
Comer AR, Hickman SE, Slaven JE, et al. Assessment of discordance between surrogate care goals and medical treatment provided to older adults with serious illness. JAMA Netw Open. 2020;3(5):e205179. Published 2020 May 1. https://doi.org/10.1001/jamanetworkopen.2020.5179.
Funding
National Institutes of Health, R01 NR019268.
Author information
Authors and Affiliations
Contributions
KAH and CJC were responsible for the preparation and conceptualization of the first draft of the manuscript. All authors contributed equally to the revision of subsequent drafts and approval of the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Conflict of Interest
Kristopher A. Hendershot declares that he has no conflict of interest. Maya N. Elias declares that she has no conflict of interest. Breana L. Taylor declares that she has no conflict of interest. Sarah Wahlster declares that she has no conflict of interest. Claire J. Creutzfeldt declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subject performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hendershot, K.A., Elias, M.N., Taylor, B.L. et al. An Update on Palliative Care in Neurocritical Care: Providing Goal-Concordant Care in the Face of Prognostic Uncertainty. Curr Treat Options Neurol 25, 517–529 (2023). https://doi.org/10.1007/s11940-023-00778-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-023-00778-z