Abstract
Purpose of review
The purpose of this review is to discuss the therapeutic options available in the treatment of traumatic injuries involving peripheral nerves.
Recent findings
For nerve gap repair, synthetic nerve tubes are limited to gaps below 3 cm in length and to small-diameter nerve repairs, whereas the dependency on proliferating host Schwann cell limits the size of acellularized autografts. Thus, in most situations, nerve autografts remain superior for nerve gap correction.
Summary
When conservative treatment is either not indicated or ineffective, surgical intervention may be employed. The ideal timing of surgical intervention is often unclear and determined by a number of factors, including the circumstances surrounding the injury, the timing of the symptoms, the type and severity of the injury, the completeness of the lesion, the required regenerative distance, the degree of fascicular disruption, and the degree of concomitant tissue trauma and contamination, as well as the morbidity and mortality of the procedure, and the age and comorbidities of the patient. The most common nonsurgical error is unnecessary surgical delay. To avoid losing the opportunity to achieve successful motor recovery, it is important to involve a peripheral nerve surgeon early.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When neurologists encounter patients with traumatic peripheral nerve injuries, the initial step is to accurately localize and characterize the lesion because this information helps dictate patient management, including the timing of any surgical intervention. When inaccurately assessed, improper management may result, thereby diminishing the chance of a good functional outcome. Even when ideally managed, for a number of reasons, the functional outcome of peripheral nerve injuries may be suboptimal, including lesion severity, long distance between the lesion and the denervated target organs (muscle fibers, sensory receptors), and significant connective tissue proliferation at the lesion site. This manuscript reviews the more common types of traumatic nerve injuries and the major neurosurgical interventions available. In all situations, a neurosurgeon with experience in peripheral nerve trauma should be involved early.
Demographics
The majority of peripheral nerve injuries are traumatic, and the incidence of traumatic nerve injuries is approximately 350,000/year [1]. Traumatic nerve injuries involve a single upper extremity nerve in a young male. In a large series of 456 patients, 74% were male, the mean age was 32.4 years, the upper extremity was involved in 73.5%, and 83% were mononeuropathies [2]. Among traumatic upper extremity mononeuropathies, the radial nerve is the most frequently involved, followed by the ulnar nerve, and then, the median nerve; the sciatic nerve is the most frequently involved lower extremity nerve, followed by the peroneal nerve [3, 4]. During peacetime, most peripheral nerve injuries follow motor vehicle accidents [5].
Nerve injury types
Peripheral nerve injuries follow any force capable of disrupting the neuron cell body, its protoplasmic projections (axons), or their coverings (myelin). Although neurons may be injured in a large number of ways (e.g., traction, compression, transection, electrical, radiation, thermal, and injection), the pathologic outcomes are limited to demyelination and Wallerian degeneration. With focal demyelination, there are no distant pathological effects, whereas with axon disruption, the distal segment undergoes Wallerian degeneration (axon loss).
Most nerve injuries are mechanical in nature (compression, traction, transection). Of these, traction injuries predominate in the civilian sector [6]. Less common mechanisms include friction (dynamic compression of the nerve against another structure), pressure (injuries related to pressure changes within an enclosed space through which the nerve passes), and ischemic injuries, as well as traumatic injuries related to thermal, electrical, or radiation insults.
The anatomic location of an extremity nerve within a limb correlates with the type of injury to which it is most susceptible. For example, due to its course around the humerus, the axillary nerve is most susceptible to traction injuries from shoulder dislocation [5, 7]. The fascicular composition of a nerve also dictates its vulnerability to traction or compression injury. Because different segments of the same nerve have differing fascicular structure, segmental susceptibilities also occur. Hence, one segment may be more susceptible to traction, another to compression, and another to both forces. Nerve roots are susceptible to both traction and compression because of their lack of epineurium and perineurium, a lesser number of collagen fibers within the endoneurium, and the organization of their nerve fibers into parallel bundles [8].
Traction injuries
Nerves are somewhat resistant to stretch injury, a reflection of their tensile strength and elasticity. The tensile strength of a nerve reflects its ability to withstand loads that elongate it. The structural features than generate resistance to stretch injury include the undulating course of the nerve through the limb and the undulating course of its nerve fibers through the fascicle (the undulatory features provide slack), as well as the tensile properties of the perineurium [8]. As tension is applied to a nerve, its undulatory features are lost first, at which point, further resistance to stretch is provided by the perineurium. As the tension increases further, the perineurium ruptures. The point at which perineurial rupture occurs reflects the magnitude, duration, and rate of application of the traction force [8].
Compression injuries
The compressive strength of a nerve reflects its ability to withstand loads that reduce its diameter. Whereas the perineurium provided resistance against traction injury, the epineurium provides resistance against compression injury by dissipating external pressure applied to it. Therefore, nerves with more epineurial tissue are able to resist larger compressive forces. Fascicular structure also contributes to compressive force resistance. A larger number of smaller fascicles dissipates compressive force better than a smaller number of larger fascicles [8]. For example, the peroneal division of the sciatic nerve has a smaller number of larger fascicles and less epineurial tissue than does the tibial division, accounting for its greater vulnerability to compression. Other reasons for its greater susceptibility include less epineurial adipose tissue [8], a poorer blood supply, and nerve anchoring at two sites (the sciatic notch and the fibular head) [9•].
Compressive forces produce nerve injury in two ways—damage to the nerve fiber (axon or myelin) and endoneurial edema formation [10]. Endoneurial edema impedes nerve function by increasing the endoneurial fluid pressure (e.g., compartment syndrome), which reduces axon transport, may impede the intraneural microcirculation, and may generate fibrosis. Concomitant stretch injuries (from nerve fiber angulation) and ischemic injuries (from vascular compromise) may be present.
When compressive forces are short in duration (e.g., sitting on a hard toilet seat, leg crossing), the resultant neurological features are typically transient and positive (tingling) and reflect ischemia (when the external pressure on the blood vessels exceeds the systolic blood pressure). When compressive forces are of longer duration, negative features (numbness, weakness) may occur from myelin or axon disruption. With compressive injuries, because the basement membrane surrounding the Schwann cell is unaffected and because the connective tissue elements are not disrupted, reinnervation is favored and, hence, the prognosis tends to be good. Body sites more susceptible to nerve compression include those areas where the nerve passes through a narrow opening, passes across the edge of another structure, or is superficial. Nerves are more susceptible to external compressive forces where they pass over a bone (radial nerve/spiral groove, common peroneal nerve/fibular neck, ulnar nerve/ulnar groove). Compressive force susceptibility may also be genetic (tomaculous neuropathy).
Transection injuries
With transection injuries, because the nerve fibers (and connective tissue elements) are severed, these disorders are axon loss in type. They are categorized as complete or incomplete and, depending on the mechanism of transection, as sharp or blunt. With complete injuries, the severed ends pull away from each other, creating a gap that prevents reinnervation by proximodistal axon regrowth. Thus, transection injuries have a worse prognosis.
Lesion assessment
The pathophysiology of the lesion dictates its clinical and electrodiagnostic (EDX) manifestations. With demyelinating conduction slowing (DMCS), positive symptoms (e.g., tingling) occur because the action potentials are able to traverse the lesion site, albeit at a slower rate. When the fibers are demyelinated to differing degrees, there is a resultant loss of synchrony among the propagating action potentials. As a result, vibratory perception and muscle stretch reflexes are diminished or absent because they require the synchronous arrival of action potential volleys. With demyelinating conduction block (DMCB) and axon loss, the clinical manifestations are negative (numbness, weakness) because the action potentials cannot traverse the lesion. With DMCB, because the affected motor axons remain in contact with the muscle fibers, there is no associated muscle atrophy. Also, because DMCB primarily involves the larger diameter, more heavily myelinated nerve fibers, large fiber sensory modalities (vibration, proprioception, discriminative touch) are affected out of proportion to the small fiber modalities (pain, temperature, crude touch). With axon loss, muscle atrophy is evident because denervated muscle fibers decrease in their transverse diameter. With axon loss, the associated sensory loss involves the large and small fiber sensory modalities more evenly.
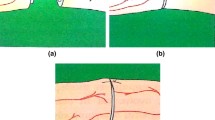
With axon loss lesions, the EDX abnormalities observed depend on lesion severity and the timing of the study. With mild axon disruption, isolated fibrillation potentials may be the only abnormality. Because of the high innervation ratio (muscle fibers innervated per motor neuron) of the skeletal muscle, a large number of fibrillation potentials (typically hundreds) are generated per motor axon disrupted, rendering the needle electromyogram (EMG) examination the most sensitive EDX study for motor axon loss. Unfortunately, fibrillation potentials typically do not appear until day 21 (and as late as day 35). With more severe lesions, low-amplitude sensory responses are observed. The sensory response amplitude decrement from Wallerian degeneration begins around day 6 (as some of the sensory axons fail to conduct action potentials) and is complete by day 10 (when there is uniform conduction failure among the affected axons). With lesions of even greater severity, low-amplitude motor responses appear. The motor response amplitude decrement begins around days 2–3 and is complete by day 6. This reflects the fact that neuromuscular junction (NMJ) degeneration precedes axon degeneration and the motor responses are dependent on NMJ transmission (see Fig. 1).
With axon disruption, Wallerian degeneration ensues and causes the motor and sensory responses to decrease, as shown in this illustration of a complete lesion involving a mixed nerve. Because the neuromuscular junctions degenerate before the axons, the motor responses (assess the motor axons, muscle fibers, and the intervening neuromuscular junctions) decrement earlier than the sensory responses (assess the sensory axons).
Because the motor response amplitude value (and the negative area under the curve value) reflects the number of functioning muscle fibers, it is useful in severity assessment. Because the latency and conduction velocity values only reflect the fastest conducting nerve fiber, these measurements are insensitive to axon loss. Even when all of the fastest fibers are involved and the latency and conduction velocity values become abnormal, their degree of abnormality is small in comparison to the degree of amplitude decrement. In general, once the motor response falls to about 50% of its normal size, the sensory response from the nerve becomes absent (or nearly so) and a neurogenic MUAP recruitment pattern may be observable [11]. The latter becomes more obvious as the severity increases further. Focal demyelination and neurogenic recruitment do not require time to mature and, thus, are apparent at lesion onset, assuming the lesion is severe enough to manifest them.
Most abrupt-onset lesions are traumatic in origin and axon loss in nature [5]. With traumatic median neuropathy, DMCB or axon loss (or a combination) is observed. Conversely, with slowly progressive entrapment of the median nerve (i.e., carpal tunnel syndrome), the earliest pathophysiology is focal DMCS. As the disorder becomes more severe, axon loss appears. Consequently, traumatic median neuropathies have a completely different pathophysiology (and natural history) than median neuropathies from carpal tunnel syndrome. For this reason, median nerve trauma occurring at the carpal tunnel should never be referred to as acute carpal tunnel syndrome [12].
Severity assessment by strength assessment
The Medical Research Council (MRC) scale is a nonlinear scale for grading muscle strength that was first published in 1941, revised in 1943, and republished in a document entitled “Aids to the Investigation of Peripheral Nerve Injuries (War Memorandum No. 45)” [13]. Grade 0 indicates no visible muscle movement; grade 1 indicates muscle movement without joint movement; grade 2 indicates contractile force unable to overcome gravity; grade 3 indicates that the generated contractile force is able to overcome gravity without added resistance; grade 4 indicates that the generated contractile force overcomes gravity plus added resistance (provided by the examiner); and grade 5 indicates normal contractile force against full resistance. Based on these definitions, grade 4 represents about 70% of the scale, extending from grade 3 to grade 5. Because of the wide range of muscle strength represented by grade 4, a plus or minus sign is typically used to subdivide it into mild, moderate, and severe weakness (4+, 4, and 4−, respectively) (see Table 1).
Severity assessment by EDX assessment
In general, when patients with traumatic peripheral neuropathies are initially followed (e.g., blunt trauma), EDX testing is typically performed after post-trauma day 21. It is important that EDX providers appropriately apply the various EDX studies so that the lesion is ideally localized and characterized. The basic concepts of lesion localization and characterization are reviewed in most standard EDX textbooks [11]. The following discussion is a summary of the most important concepts and an EDX example demonstrating the determination of the associated pathophysiologies.
Motor NCS
Unlike the MRC scale, which estimates muscle power using a nonlinear 6-point scale (0–5), the motor NCS are much more specific, providing a linear 100-point scale. This is accomplished by comparing the motor response recorded from the weak muscle to the one recorded from the homologous muscle on the contralateral (asymptomatic) side, expressed as a percentage.
The innervation ratio of a muscle (i.e., the number of muscle fibers innervated per anterior horn cell) is constant. Thus, the percentage of denervated muscle fibers within the muscle correlates with percentage of disrupted motor axons within the nerve. Following muscle fiber denervation, motor axons adjacent to the denervated fibers sprout collaterals and reinnervate the denervated muscle fibers. As a result of this mechanism of reinnervation, termed collateral sprouting, the innervation ratio of the adopting motor neuron increases. Thus, following reinnervation by collateral sprouting, the percentage calculation underestimates lesion severity. Prior to collateral sprouting, the distal motor response amplitude values of the symptomatic and asymptomatic sides can be compared to provide an estimate of severity. In the setting of DMCB lesions, the percentage of blocked motor nerve fibers can be calculated by comparing the motor response amplitude values of the motor responses recorded with stimulation below and above the lesion. Mixed lesions are calculated using both techniques in sequence, starting with the axon loss determination. An example of this is provided here.
Example. A 48-year-old man presents on day 28 for EDX assessment of a traumatic right peroneal neuropathy. The right superficial peroneal sensory and peroneal motor (recording EDB) responses are absent, the right peroneal distal motor response (recording TA) is low in amplitude and shows a DMCB across the fibular head, and the needle EMG show 3+ fibrillation potentials with neurogenic motor unit action potential (MUAP) recruitment in a right common peroneal nerve distribution. There are no chronic changes (e.g., increased MUAP duration). Thus, this is a mixed lesion (DMCB and axon loss) localized to the fibular head. The amplitude values of the right and left common peroneal motor responses can be used to semi-quantify the underlying pathophysiologies.
For example, when the amplitude of the peroneal motor response recording TA is 3.0 mV with ipsilateral below-fibular head stimulation, 1.5 mV with ipsilateral above-fibular head stimulation, and 6.0 mV with contralateral below-fibular head stimulation, the responsible pathophysiologies are easily determined. The percentage of axon loss is calculated by comparing the distal motor response amplitude values of the two sides using the formula, 1 − symptomatic side / asymptomatic side × 100%, as follows:
The percentage of DMCB is calculated using the formula, 1 − proximal response / distal response × 100%, as follows:
Thus, of the motor axons not affected by axon loss, 50% are affected by DMCB. Hence, 50% are axon loss, 25% are DMCB (half of 50%), and 25% are normal. When only the ipsilateral values are used, the erroneous impression that there is a DMCB affecting 50% of the fibers results. When the motor responses show response dispersion, the amplitude values are unreliable. In this setting, the negative area-under-the-curve values should be utilized. In summary, because reinnervation via collateral sprouting increases the innervation ratio, the calculated percentage of axon loss represents an underestimate. Consequently, beyond three months, it is more accurate to state that the axon loss involves at least the calculated percentage.
Sensory NCS
Because of their low amplitude, short negative phase duration, greater number of phases, and wider range of conduction velocities, sensory responses are quite susceptible to physiological temporal dispersion and, thus, overestimate the severity of axon loss. In general, after Wallerian degeneration has occurred and before reinnervation through collateral sprouting has occurred, when the nerve is about 50% disrupted, the motor responses are about 50% decreased and the sensory responses are about 90% decreased (or absent) [11]. Although sensory responses are not helpful for lesion severity estimation, their susceptibility makes them better for the initial localization of axon loss lesions.
Needle EMG examination
The needle EMG study cannot approximate the percentage of motor axon involvement and, thus, is of limited value in grading lesion severity. The quantity of fibrillation potentials observed primarily reflects the timing of the study, not the severity of the lesion. Also, the grading scale (1+ to 4+) is nonlinear (i.e., a grade of 2+ does not represent twice as many fibrillation potentials as a grade of 1+). The presence of a neurogenic MUAP recruitment pattern indicates that at least 50% of the motor nerve fibers are unable to transmit action potentials. However, it does not differentiate between axon loss and DMCB. In general, the observation of an MUAP firing at a rate of 20 Hz or more is abnormal because this rate is 3 standard deviations above the mean firing rate for a 30% maximum isometric contraction [14, 15].
Nerve injury classification
With the Seddon [16, 17] and Sunderland [18, 19] nerve injury classification systems, the degree of connective tissue disruption dictates lesion severity. Because this is a histological determination, it cannot be employed in the acute setting. Nonetheless, it is important to be familiar with these two systems.
The Seddon classification system
With the Seddon system, there are three grades of severity: neurapraxia (myelin disruption), axonotmesis (axon disruption), and neurotmesis (nerve disruption).
Neurapraxia
Neurapraxia, the mildest grade, consists of focal myelin disruption that blocks action potential propagation (DMCB). EDX testing identifies neurapraxia and, after day 6, differentiates it from axon loss. Neurapraxia has an excellent prognosis, with full motor recovery following remyelination. The production of voltage-gated sodium channels along the demyelinated segment may restore action potential propagation through the lesion prior to remyelination [20].
Axonotmesis
With axonotmesis (tmesis, a cutting), there is axon disruption and resultant Wallerian degeneration. Because the connective tissue elements (endoneurium, perineurium, epineurium) are unaffected, the neural tubes (endoneurium) are spared. Thus, the prognosis is excellent because the regenerating axons are able to advance unimpeded within their original endoneurial sheath. Because collateral sprouting occurs within the muscle, in the setting of incomplete axon loss, reinnervation via collateral sprouting is the primary mechanism of reinnervation.
Neurotmesis
With neurotmesis, the nerve is divided and recovery cannot occur without surgical intervention. In general, unless there is exclusionary evidence, it is best to assume that focal nerve trauma represents a neurotmetic injury so that the opportunity for surgical intervention is not lost [21].
The Sunderland classification system
The Sunderland system employs 5 grades of nerve injury. With this system, the degree of connective tissue involvement is better defined and, thus, provides more accurate prognostication. Sunderland grade 1 is equivalent to neurapraxia and Sunderland grade 2 is equivalent to axonotmesis.
Sunderland grades 3–5
With lesions more severe than axonotmesis, recovery through proximodistal axonal advancement primarily reflects two factors: (1) the ability of the regenerating axons to advance across the lesion site and (2) their ability to enter the proper endoneurial tubes within the distal stump. These factors depend on certain characteristics of the lesion, including its severity, degree of connective tissue disruption and proliferation, presence of a gap or debris between the proximal and distal stumps, underlying etiology, and patient’s age [5, 22].
Sunderland grade 3
With grade 3 lesions, which often follow severe traction or compression, the endoneurium is disrupted. This permits axon misdirection—the advancing axons enter the wrong endoneurial tube (aberrant reinnervation). The outcome depends on the tube entered and may be asymptomatic (a motor axon enters an endoneurial tube leading to the same muscle) or symptomatic (when it leads to an alternative end organ (sensory receptor, autonomic gland, different muscle)). Examples of nerve fiber–receptor mismatch with seventh nerve lesions include crocodile tears (lacrimation during eating when a motor axon advances to the lacrimal gland) and synkinesis (when a motor axon advances to a different facial muscle). Because axons are more intermingled proximally, the likelihood of aberrant reinnervation is greater with proximal nerve lesions.
The outcome of Sunderland third-degree lesions varies widely (from good to negligible), depending on the number of endoneurial tubes disrupted, the degree of associated fibrosis (bleeding and intrafascicular edema lead to intrafascicular fibrosis and possible neuroma formation), the level of the lesion along the nerve, the distance between the lesion and the denervated end organs, and the completeness of the lesion. Without surgical intervention, incomplete recovery frequently occurs.
Sunderland grade 4
With grade 4 injuries, there is perineurial disruption and, hence, fascicular structural damage. Thus, there is greater axonal misdirection and greater fibrosis. As a result of the perineurial disruption, advancing axons may exit the fascicle or they may form a neuroma within the nerve (neuroma-in-continuity). Surgical intervention is required.
Sunderland grade 5
With grade 5 injuries, there is epineurial disruption and the nerve trunk may be severed (neurotmesis in the Seddon system). Like fourth-degree injuries, surgical intervention is mandatory.
Sunderland grade 6
Mackinnon popularized the term sixth-degree injury (nerve injuries of mixed grade), which are the most challenging to treat [23]. With these lesions, fascicular treatment is individually based.
It is important to distinguish axon loss lesions that might recover spontaneously (second- and some third-degree) from those that require surgical intervention (most third-degree and all fourth-degree and fifth-degree). Acutely, their clinical features are identical and, thus, they cannot be differentiated noninvasively.
In addition to lesion severity, functional outcome also reflects time to operative repair and the age of the patient. Regarding the former, although satisfactory outcomes may follow surgical intervention after 12 months [24], the best motor outcomes are associated with surgical intervention before 6 months, with less ideal outcomes between 6 and 12 months and the poorest outcomes after 12 months. Because denervated sensory receptors do not undergo degeneration, sensory recovery may occur up to 48 months later [25, 26]. Regarding age, operative outcomes are better for younger individuals (under 20) than for older persons (over 50) [22, 25].
Neuromuscular imaging
Introduction
Clinical and EDX testing are useful initially for lesion localization, after which neuromuscular imaging using high-resolution US or magnetic resonance (MR) imaging are employed for lesion visualization and characterization. As stated previously, the basic unit of a peripheral nerve is the axon (either myelinated or unmyelinated), the fluid between the Schwann cell membrane and the axolemma is the endoneurial fluid, and the interfascicular epineurial tissue of larger nerves contains various amounts of adipose.
Neuromuscular ultrasound
Neuromuscular ultrasonography (US) began in the 1980s and, through technical advancements, led to the development of high-resolution US (12–18 MHz transducer) and the enhanced ability to quickly identify and noninvasively and painlessly assess long lengths of specific nerves. Of the measured parameters (e.g., echotexture, vascularity), nerve cross-sectional area (CSA) is most commonly reported [27]. To avoid overestimating the CSA, the transducer is oriented perpendicular to the longitudinal axis of the nerve. The hyperechoic (bright) signal of the epineurial tissue is manually outlined or estimated by placement of an ellipse of best fit. By providing anatomical details, neuromuscular US compliments EDX testing. One major disadvantage of the US is its dependence on the skills and experience of the operator.
Magnetic resonance neurography
Specialized RF receiver coils (phased-array coils), which are flexible and specific to each body region, integrate the data from individual coils into a single image, thereby mimicking a single, much larger coil [28]. This technique maintains the high signal-to-noise ratio (SNR) of smaller coils and overcomes their small field of view (FOV). Nonetheless, the FOV is still small and requires lesion localization (clinically or electrodiagnostically) prior to imaging. The degree of spatial resolution is proportional to the size of the matrix (e.g., 512 × 512 provides a larger FOV than 256 × 256), and the SNR is increased by imaging with higher field strengths. Standard spin-echo T1-weighting imaging (T1WI) best displays regional anatomy, whereas fast spin-echo T2-weighted imaging (T2WI) best demonstrates intraneural pathology. Fat suppression techniques (e.g., STIR) are required so that adjacent extraneural fat does not obscure the desired intraneural signal. As with the US, at least two planes of imaging are required. With nerves, parallel (in-plane) images and perpendicular (cross-sectional) images are collected. In-plane imaging identifies nerve displacement and caliber changes, whereas perpendicular imaging permits fascicular pattern assessment and better nerve caliber assessment [28]. Because nerve caliber varies along its length, contralateral comparison studies are helpful. Contrast is helpful when neoplastic, inflammatory, post-XRT, or infectious processes are suspected, but otherwise is typically unnecessary. Abnormal findings include loss of perineural fat, diffuse or focal enlargement, diffuse or focal T2 hyperintensity, abnormal fascicular patterns, and T1 enhancement [28]. With nerve trauma, MRI helps characterize the lesion (e.g., intraneural hematoma, neuroma, loss of continuity, diffuse or focal perineural fibrosis). The muscles innervated by the affected nerve may show features of denervation or fibrofatty changes.
Magnetic resonance neurography (MRN)
Recent advancements in MR imaging, especially diffusion-weighted imaging (DWI) and diffusion tensor imaging (DTI), have significantly increased the utility of MR neurography for assessing peripheral nerve injuries, including the connective tissue elements [29, 30•].
DWI neurography (DWIN)
Peripheral nerves are highly anisotropic (i.e., water diffusivity is markedly limited along its perpendicular axis and facilitated along its longitudinal axis). DWN provides predominantly qualitative information about axonal integrity; quantitative information is derived through the apparent diffusion coefficient (ADC). The ADC reflects water displacement into the extracellular space, with high values usually representing edema [30•, 31, 32]. The advantages of DWN include high background signal contrast ratio, large FOV, short acquisition times, and quantification through ADC; disadvantages include low spatial resolution, contamination by other DWI hyperintense structures, T2-shine-through effect, and the low specificity of ADC [30•].
DTI neurography (DTIN)
Normally, diffusion of free water along the longitudinal axis is facilitated and movement transversely is restricted. Measured parameters include fractional anisotropy (FA, the most important measurement), mean diffusivity (MD), axial diffusivity (AD), and radial diffusivity (RD). DTIN data are also reconstructed to create 3D images. The advantages of DTIN include high anatomical detail and quantification (FA and diffusivity); disadvantages include artifact susceptibility, small FOV, and long acquisition times [30•]. The FA value reflects fascicular integrity and water movement direction. A low FA value suggests isotropic diffusion and, hence, neural disruption, whereas a higher value suggests greater anisotropy and, thus, neural integrity. AD reflects longitudinal diffusion, RD reflects transverse diffusion along the two axes perpendicular to axial flow, and MD reflects the average of these three movements.
Nerve trauma
With nerve trauma, there is increased water in the extracellular space and various degrees of connective tissue disruption. At the injury site, DWIN may show DWI hyperintensity, nerve thickening, increased ADC, and increased MD. Potential DTIN findings include decreased FA (loss of fiber anisotropy), increased RD (due to disruption of myelin sheaths and connective tissue elements), and edema.
Thus, the FA and RD values change along a continuum as the Sunderland grade increases from grade 2 (minimal FA decrease and minimal RD increase) to grade 5 (large FA decrease and large RD increase); conversely, following regeneration, the FA value progressively increases and the RD value progressively decreases. As the edema lessens, the ADC and MD values normalize [33]. With compressive forces, such as with carpal tunnel syndrome, there is enlargement of the extracellular space (increased CSA on US and MRN), increased ADC (edema), and loss of nerve anisotropy (FA value reduction and diffusivity changes) [34]. Following surgical release, the FA value increases, typically within 6 months, and the RD value decreases [35]. Standardization studies are required to determine the exact role of these newer MRN techniques in the assessment and management of peripheral nerve trauma.
Surgical management
Introduction
Despite incredible advances in peripheral nerve repair, the ideal timing of surgical intervention is often unclear and reflects a number of factors, including the following: the circumstances surrounding the injury, the timing of the symptoms, the type and severity of the injury, the required regeneration distance, the degree of fascicular disruption, the morbidity and mortality risks of the procedure, the degree of concomitant tissue trauma and contamination, and the age and comorbidities of the patient [21, 36]. Among these, nerve injury type and severity primarily dictate management.
In general, immediate surgical exploration is usually employed when neurological deficits develop in the distribution of a nerve following sharp penetrating injury, when nerve transection is suspected, and with severe or open trauma, injection injury, or following surgery, whereas with less severe or closed trauma or suspected neurapraxia, conservative treatment (e.g., splinting, physical therapy, and neuropathic pain medications) with serial clinical and EDX assessments for evidence of improvement, worsening, or new symptoms is typically employed. When evidence of worsening, features suggestive of a neuroma (neuromas may be identified by ultrasound or magnetic resonance neurography), or failure to recover as expected occurs, surgical intervention is considered. Unfortunately, the ideal observation period is not always clear. Although a number of factors contribute to this determination, in general, motor function recovery is best when surgical intervention is undertaken within the first three months by an experienced peripheral nerve surgeon. Consequently, many authors recommend exploration during the first 3–6 months when recovery is absent or minimal [22]. Shorter observation periods (e.g., 3 weeks) are frequently employed with high-energy injuries or those producing total or near-total paralysis [37]. Although an advancing Tinel sign indicates distal nerve regeneration, it may reflect advancing sensory axons, in which case the time delay may eliminate the opportunity to achieve successful motor recovery through surgical intervention.
Approach to axon loss (grades 2–5)
Distinguishing grades 2–5 is important because their management differs: second-degree injuries have an excellent prognosis without surgical intervention, fourth- and fifth-degree lesions require surgical intervention, and third-degree injuries often benefit from surgical intervention (spontaneous recovery is less frequent). Again, as stated previously, these are histological grades.
Two major issues are relevant—the completeness of the lesion and the distance between the lesion site and the denervated muscle fibers (i.e., the regenerative distance). With incomplete lesions, reinnervation via collateral sprouting occurs through the intramuscular motor branches of the unaffected motor axons. With complete lesions, reinnervation must occur through proximodistal axon advancement. When the regenerative distance exceeds 20 in, even when the axons successfully reach their target, they are too late because denervated muscle fibers undergo fibrofatty degeneration at 20–24 months. This is referred to as the Rule of 20 [38]. Thus, with an incomplete lesion and a 4-in regenerative distance, both mechanisms of reinnervation are available, spontaneous improvement is expected, and an observation period is employed. Should improvement not occur at the expected time, enough time still remains for successful surgical intervention. Conversely, with a complete lesion located more than 20 in from the denervated muscle fibers, neither mechanism is available. For situations between these extremes, management must be individualized. Importantly, unnecessary surgical delay is the most common nonsurgical error and, hence, early surgical consultation is mandatory so that all options remain available to the patient.
Surgical interventions
Although a number of surgical interventions are available, only a brief discussion of the major ones is provided here. As expected, the underlying injury mechanism contributes to initial management. In addition, whether the injury is open or closed is important. With open injuries, surgical exploration is required, whereas with closed injuries, clinical and EDX monitoring is employed [39•]. In general, with closed injuries, EDX testing is performed at 3 weeks and repeated every three months for evidence of recovery or worsening.
With compression injuries, timing plays a role. Most acute-onset compressive lesions (e.g., Saturday night palsy) are associated with DMCB and axon loss, whereas with chronic compression (e.g., carpal tunnel syndrome), demyelinating conduction slowing (DMCS) predominates. With these lesions, the nerve fibers closest to the compressive force and those with the thickest myelin tend to be more extensively involved [40]. EDX testing can help tease out the various percentages and dictate management. The sensory and motor NCS and the needle EMG studies should be performed bilaterally.
Most closed traction injuries are associated with lesions in continuity and are treated conservatively because, at least initially, there is no way to determine the likelihood of recovery, the need for surgery, or the type of surgical intervention required [41]. At day 7, motor NCS can differentiate grade 1 lesions (DMCB) from axon loss lesions (grades 2–5), but the latter grades cannot be differentiated from each other. As a result, with axon loss, a period of watchful waiting may be employed and, when signs of recovery fail to appear, surgical exploration is considered. The duration of the observation period must be individualized and varies with the circumstances of the injury (e.g., it is much shorter in the setting of high-energy injuries or those associated with total or near-total paralysis) [37].
With sharp transection injuries, the ends of the transected nerve can often be reattached, whereas with blunt transection injuries, the damaged portions of each end can be removed and a cable graft placed. The term, cable graft, refers to a nerve graft composed of several sections of nerve, similar to a cable, used for repair of nerve injuries involving multiple fascicles. Sharp transections are usually repaired within 72 h, when they are easier to assess (prior to scarring), easier to repair (prior to retraction), and the motor fascicles are still identifiable [37, 39•, 41, 42], whereas blunt transection repairs are usually delayed for 3–4 weeks, at which point the nonconducting fibrotic segments of both stumps are appreciable (termed the zone of injury) [41, 42]. When repaired prior to this time, failure rates of 100% have been reported [43].
When transection injuries result in nerve gaps, a number of approaches may be used, depending on the distance between the nerve stumps, the diameter of the nerve, the location of the lesion along the nerve, and the availability of a proximal stump. Nerve mobilization helps to approximate the two stumps. When the gap is less than 1 cm and stump approximation does not generate excessive tension on the nerve, end-to-end repair (also known as end-to-end suturing, end-to-end neurorrhaphy, and direct repair) is preferred because it allows the severed fascicles to be matched and reconnected [44]. Because the axons composing a fascicle change as the axons advance, lengthy lesions do not permit fascicular matching. With end-to-end suturing of monofascicular lesions (or polyfascicular lesions in which the severed fascicles cannot be matched), the epineurium is usually sutured to avoid trauma to the perineurium (termed an epineurial or epineural repair), whereas when individual fascicles are repaired, the perineurium is sutured (termed fascicular repair). When some fascicles can be matched and others cannot, both techniques are employed. Unfortunately, even with proper alignment, only about 50% of individuals demonstrate functional recovery [45].
Following removal of the fibrotic segments, when the ends cannot be approximated in a tension-free manner or when there is a gap between the two ends exceeding 1 cm, an end-to-end repair is not performed. Thus, either a nerve conduit or a nerve graft must be interposed. A nerve conduit is a synthetic nerve tube that may be resorbable or nonresorbable. With nerve tube repairs, the nerve stumps are inserted into the ends of the tube and sutured in place. Nerve conduits collect the axoplasm and other neural stump fluids, from which a fibrin-based scaffold forms, thereby permitting cell migration [39•]. Schwann cells grow into the tube at both ends and axonal advancement occurs from the proximal stump [36, 46]. Because the concentration of neurotrophic factors (released from the nerve ending after injury) within the conduit is critical in assisting nerve regeneration, based on the formula for the volume of a cylinder (V = πr2L), conduits are limited to thinner-diameter nerve repairs and lengths not exceeding 3 cm [47, 48]. Also, a small portion of proximal nerve can be minced and placed in the center of the conduit for additional neurotrophic support [48].
Nerve grafts may be autografts or allografts and are useful for gaps in the 1–5 cm range [39•]. For a number of reasons, nerve autografts are considered superior. They provide endoneurial tubes, Schwann cells, and neurotrophic factors; have inherent flexibility and strength; and are immune-compatible, inexpensive, and their ready availability [39•, 49]. Sensory nerves are more frequently used for autografting (e.g., sural, superficial peroneal, intercostal, lateral, and medial antebrachial cutaneous, dorsal ulnar cutaneous). The sural nerve is often chosen because of its ease of harvest, limited morbidity, moderate dispensability, and length of nerve available (30–50 cm) [50]. Multiple sural nerve segments may be required for large-diameter nerve repairs. It is interposed using an end-to-end suturing technique. To avoid postoperative recoil and tension, donor nerve length should exceed gap length by about 20% [36]. The primary disadvantage of autografting is the loss of donor nerve function and possible neuroma formation.
These two disadvantages are eliminated through the use of an allograft. Cellular allografts (nonprocessed cadaver nerve grafts) are used for extensive injuries that require long lengths of nerve graft material. With cellular allografts, immunosuppression is required until native cells incorporate the graft (e.g., 18–24 months) [39•, 51].
Acellular allografts (processed cadaver nerve grafts) are treated to eliminate the immunogenicity of the donor tissue and to provide an extracellular matrix to help direct axonal advancement. Although superior to conduits, acellularized autografts depend on proliferating host Schwann cells to support axonal regeneration and, consequently, the proliferative demand is greater with autografts of longer lengths, thereby also limiting this approach for large defects [52]. Thus, they are inferior to nerve autografts [53].
For gaps exceeding 5 cm, vascularized nerve grafts and nerve transfers are utilized. Vascularized nerve grafts are used for long gaps among large nerve trunks when the recipient region is ischemic or scarred. For proximal injuries where the proximal stump is not available (avulsions) or not identifiable, devastating brachial plexus injuries, injuries with lengthy regenerative distances, or injuries in which the presentation has been delayed, a healthy adjacent nerve (the donor) can be attached to the distal stump of the severed nerve (the recipient) [36]. With this technique, termed nerve transfer or neurotization, the donor nerve may be used in its entirety or the transfer may be limited to one or more of its fascicles. Because the donor nerve is coapted to the recipient nerve near the motor endplate region of the affected nerve, reinnervation occurs earlier.
Finally, it is also possible to perform an end-to-side neurorrhaphy for long-gap injuries. With this technique, the donor function is not lost. In a recent study of this technique in a rodent model, it was shown that axon regrowth from the donor nerve to the recipient nerve is more efficient when the donor nerve undergoes a 50% cross-section at the coaptation site (greater axonal sprouting) and the recipient nerve is degenerated (better attracts the axonal sprouts).
A large number of procedures are currently available for the surgical treatment of traumatic nerve injuries, each of which has its limitations. In the future, techniques to enhance axon regeneration, such as the application of devices for the sustained delivery of nerve growth factors, the implantation of Schwann cells at the injury site, and the delivery of stem cells able to differentiate into Schwann cells, will undoubtedly improve the outcome of those patients undergoing nerve grafting procedures [39•].
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Fowler JR, Lavasani M, Huard J, Goitz RJ. Biologic strategies to improve nerve regeneration after peripheral nerve repair. J Reconstr Microsurg. 2015;31:243–8.
Kouyourmdjian JA. Peripheral nerve injuries: a retrospective survey of 456 cases. Muscle Nerve. 2006;34:785–8.
Noble J, Munro CA, Prasad VS, Midha R. Analysis of upper and lower extremity peripheral nerve injuries in a population of patients with multiple injuries. J Trauma. 1998;45:116–22.
Robinson LR. Traumatic injury to peripheral nerves. Muscle Nerve. 2000;23:863–73.
Ferrante MA, Wilbourn AJ. The electrodiagnostic examination with peripheral nerve injuries. In: Mackinnon SE, editor. Nerve surgery. New York: Thieme; 2015. p. 59–74.
Campbell WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol. 2008;119:1951–65.
Wilbourn AJ, Ferrante MA. Clinical electromyography. In: Joynt RJ, Griggs RC, editors. Baker’s clinical neurology [book on CD-ROM]. Philadelphia: WB Saunders; 2000. record 7592-8248.
Sunderland S. The anatomy and physiology of nerve injury. Muscle Nerve. 1990;13:771–84.
• Robinson LR. How electrodiagnosis predicts clinical outcome of focal peripheral nerve lesions. Muscle Nerve. 2015;52:321–33. This article reviews the electrodiagnostic prognostic factors for traumatic peripheral nerve injuries, including general concepts related to peripheral nerve injury.
Sunderland S. The nerve lesion in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 1976;39:615–26.
Ferrante MA. Comprehensive electrodiagnostic medicine: principles and concepts with clinical correlations and case studies. New York: Cambridge University Press; 2018.
Holmlund T, Wilbourn AJ. Acute median neuropathy at the wrist is not carpal tunnel syndrome. Muscle Nerve. 1993;16:1092.
Aids to the examination of the peripheral nervous system (memorandum no. 45), Medical Research Council, 1970/6].
Dorfman LJ, Howard JE, McGill KC. Influence of contractile force on properties of motor unit action potentials: ADEMG analysis. J Neurol Sci. 1988;86:125–36.
Petajan JH, Phillip BA. Frequency control of motor unit action potentials. Electroencephalogr Clin Neurophysiol. 1969;27:66–72.
Seddon HJ. A classification of nerve injuries. BMJ. 1942;2:237–9.
Seddon HJ. Three types of nerve injury. Brain. 1943;66:237–88.
Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain. 1951;74:491–516.
Sunderland S. Nerve and nerve injuries. 2nd ed. Edinburgh: Churchill Livingstone; 1978.
Waxman SG, Brill MH. Conduction through demyelinated plaques in multiple sclerosis: computer simulations of facilitation by short internodes. J Neurol Neurosurg Psychiatry. 1978;41:408–17.
Ditty BJ, Omar NB, Rozelle CJ. Surgery for peripheral nerve trauma. In: Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ, editors. Nerves and nerve injuries. Amsterdam: Elsevier; 2015. p. 373–81.
Goubier J-N, Teboul F. Grading of nerve injuries. In: Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ, editors. Nerves and nerve injuries. Amsterdam: Elsevier; 2015. p. 603–10.
Farber SF, Saheb-Al-Zamani M, Zieske L, Laurido-Soto O, Bery A, Hunter D, et al. Peripheral nerve surgery after local anesthetic injection. Anesth Analg. 2013;117:731–9.
Khalifa H, Belkheyar Z, Diverrez JP, Oberlin C. Results of 24 nerve repairs at more than one year post-injury. Chir Main. 2012;31:318–23.
Mailander P, Berger A, Schaller E, Rube K. Results of primary nerve repair in the upper extremity. Microsurgery. 1989;10:147–50.
Weinzweig N, Chin G, Mead M, Stone A, Nagle D, Gonzalez M, et al. Recovery of sensibility after digital neurorrhaphy: a clinical investigation of prognostic factors. Ann Plast Surg. 2000;44:610–7.
Shen J, Cartwright MS. Neuromuscular ultrasound in the assessment of polyneuropathies and motor neuron disease. J Clin Neurophysiol. 2016;33:86–93.
Maravilla KR, Bowen BC. Imaging of the peripheral nervous system: evaluation of peripheral neuropathy and plexopathy. AJNR. 1998;19:1011–23.
Lehmann HC, Zhang J, Mori S, Sheikh KA. Diffusion tensor imaging to assess axonal regeneration in peripheral nerves. Exp Neurol. 2010;223:238–44.
• Noguerol TM, Barousse R, Socolovsky M, Luna A. Quantitative magnetic resonance (MR) neurography for evaluation of peripheral nerves and plexus injuries. Quant Imaging Med Surg. 2017;7:398–421. This is an excellent review of the mechanics underlying quantitative magnetic resonance neurography in relation to various types of nerve injury.
Anderson AW, Xie J, Pizzonia J, Bronen RA, Spencer DD, Gore JC. Effects of cell volume fraction changes on apparent diffusion in human cells. Magn Reson Imaging. 2000;18:689–95.
Eguchi Y, Ohtori S, Yamashita M, Yamauchi K, Suzuki M, Orita S, et al. Clinical applications of diffusion magnetic resonance imaging of the lumbar foraminal nerve root entrapment. Eur Spine J. 2010;19:1874–82.
Simon NG, Kliot M. Diffusion weighted MRI and tractography for evaluating peripheral nerve degeneration and regeneration. Neural Regen Res. 2014;9:2122–4.
Heckel A, Weiler M, Xia A, Ruetters M, Pham M, Bendszus M, et al. Peripheral nerve diffusion tensor imaging: assessment of axon and myelin sheath integrity. PLoS One. 2015;10:e0130833.
Naraghi A, da Gama LL, Menezes R, Khanna M, Sussman M, Anastakis D, et al. Diffusion tensor imaging of the median nerve before and after carpal tunnel release in patients with carpal tunnel syndrome: feasibility study. Skelet Radiol. 2013;42:1403–12.
Midha R, Alaqeel A. Technical aspects of nerve repair. In: Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ, editors. Nerves and nerve injuries. Amsterdam: Elsevier; 2015. p. 225–36.
Hentz VR. Brachial plexus injuries. In: Omer Jr GE, Spinner M, Van Beek AL, editors. Management of peripheral nerve problems. 2nd ed. Philadelphia: WB Saunders; 1998. p. 445–53.
Scarrf JE. Peripheral nerve injuries: principles of treatment. Med Clin. 1958;42:611–40.
• Habre SB, Bond G, Jing XL, Kostopoulos E, Wallace RD, Konofaos P. The surgical management of nerve gaps: present and future. Ann Plast Surg. 2018;80:252–61. This excellent review is written for the non-neurosurgeon and discusses the various surgical options in a manner that is easily comprehended.
Aguayo A, Nair CP, Midgley R. Experimental progressive compression neuropathy in the rabbit: histologic and electrophysiologic studies. Arch Neurol. 1971;24:358–64.
Spinner RJ, Kline DG. Surgery for peripheral nerve and brachial plexus injuries or other nerve lesions. Muscle Nerve. 2000;23:680–95.
Kline DG, Hudson AR. Nerve injuries: operative results for major nerve injuries, entrapments, and tumors. Philadelphia: WB Saunders Company; 1995.
Ring D, Chin K, Jupiter JB. Radial nerve palsy associated with high-energy humeral shaft fractures. J Hand Surg Am. 2004;29:144–7.
Meadows RM, Sengelaub DR, Jones KJ. Cellular aspects of nerve injury and regeneration. In: Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ, editors. Nerves and nerve injuries. Amsterdam: Elsevier; 2015. p. 433–49.
Kallio PK, Vastamaki M. An analysis of the results of late reconstruction of 132 median nerves. J Hand Surg (Br Vol). 1993;18:97–105.
Heath CA, Rutkowski GE. The development of bioartificial nerve grafts for peripheral nerve regeneration. Trends Biotechnol. 1998;16:163–8.
Weber RA, Breidenbach WC, Brown RE, Jabaley ME, Mass DP. A randomized prospective study of polyglycolic acid conduits for digital nerve reconstruction in humans. Plast Reconstr Surg. 2000;106:1036–45.
Mackinnon SE. Technical use of synthetic conduits for nerve repair. J Hand Surg Am. 2011;36:183. (letter to the editor)
Ng SS, Kwan MK, Ahmad TS. Quantitative and qualitative evaluation of sural nerve graft donor site. Med J Malaysia. 2006;61(suppl B):13–7.
Lee SK, Wolfe SW. Peripheral nerve injury and repair. J Am Acad Orthop Surg. 2000;8:243–52.
Mackinnon SE, Doolabh VB, Novak CB, Trulock EP. Clinical outcome following nerve allograft transplantation. Plast Reconstr Surg. 2001;107:1419–29.
Saheb-Al-Zamani M, Yan Y, Farber SJ, Hunter DA, Newton P, Wood MD, et al. Limited regeneration in long acellular nerve allografts is associated with increased Schwann cell senescence. Exp Neurol. 2013;247:165–77.
Moore AM, Kasukurthi R, Magill CK, Farhadi HF, Borschel GH, Mackinnon SE. Limitations of conduits in peripheral nerve repairs. Hand. 2009;4:180–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mark A. Ferrante declares that he has no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Neuromuscular Disorders
Rights and permissions
About this article
Cite this article
Ferrante, M.A. The Assessment and Management of Peripheral Nerve Trauma. Curr Treat Options Neurol 20, 25 (2018). https://doi.org/10.1007/s11940-018-0507-4
Published:
DOI: https://doi.org/10.1007/s11940-018-0507-4