Opinion statement
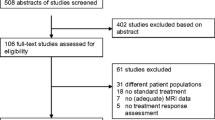
With advances in treatments and survival of patients with glioblastoma (GBM), it has become apparent that conventional imaging sequences have significant limitations both in terms of assessing response to treatment and monitoring disease progression. Both ‘pseudoprogression’ after chemoradiation for newly diagnosed GBM and ‘pseudoresponse’ after anti-angiogenesis treatment for relapsed GBM are well-recognised radiological entities. This in turn has led to revision of response criteria away from the standard MacDonald criteria, which depend on the two-dimensional measurement of contrast-enhancing tumour, and which have been the primary measure of radiological response for over three decades. A working party of experts published RANO (Response Assessment in Neuro-oncology Working Group) criteria in 2010 which take into account signal change on T2/FLAIR sequences as well as the contrast-enhancing component of the tumour. These have recently been modified for immune therapies, which are associated with specific issues related to the timing of radiological response. There has been increasing interest in quantification and validation of physiological and metabolic parameters in GBM over the last 10 years utilising the wide range of advanced imaging techniques available on standard MRI platforms. Previously, MRI would provide structural information only on the anatomical location of the tumour and the presence or absence of a disrupted blood-brain barrier. Advanced MRI sequences include proton magnetic resonance spectroscopy (MRS), vascular imaging (perfusion/permeability) and diffusion imaging (diffusion weighted imaging/diffusion tensor imaging) and are now routinely available. They provide biologically relevant functional, haemodynamic, cellular, metabolic and cytoarchitectural information and are being evaluated in clinical trials to determine whether they offer superior biomarkers of early treatment response than conventional imaging, when correlated with hard survival endpoints. Multiparametric imaging, incorporating different combinations of these modalities, improves accuracy over single imaging modalities but has not been widely adopted due to the amount of post-processing analysis required, lack of clinical trial data, lack of radiology training and wide variations in threshold values. New techniques including diffusion kurtosis and radiomics will offer a higher level of quantification but will require validation in clinical trial settings. Given all these considerations, it is clear that there is an urgent need to incorporate advanced techniques into clinical trial design to avoid the problems of under or over assessment of treatment response.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gliomas are the most common type of primary brain tumour in adults with an annual incidence of 4–5/100,000 people. For newly diagnosed glioblastoma (GBM), the most common and malignant of the gliomas, no treatment has yet been shown to be more effective than maximal safe surgical resection followed by chemoradiation and adjuvant chemotherapy with temozolomide [1]. There has been only a modest improvement in outcome over the last 10 years with 3-year survival increasing from about 4% in 1999–2000 to 10% in 2009–2010 [2].
Almost all GBMs will recur and no therapies currently exist that significantly prolong survival at relapse. Progress has been limited both by the paucity of effective treatments but also by the inherent difficulties in assessing treatment response in clinical trials. This review will discuss the advances and limitations of quantitative MRI techniques currently being implemented into clinical practice as well as emerging techniques that will become a standard part of clinical trial design over the next decade.
Challenges in monitoring treatment response with conventional MRI
It is essential that imaging is sufficiently accessible, technically reproducible and biologically meaningful to guide treatment decisions and assessment of efficacy of new treatments. Image evaluation with conventional MRI is limited to the assessment of disease bulk and morphology; it lacks information regarding the viability of residual tumour, crucial for response monitoring and the distinction between treatment effects on the brain and underlying disease status.
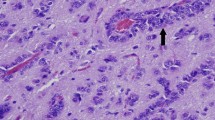
Although tumour dimensions are measurable within the millimetre range, microscopic infiltration remains occult on conventional imaging. Contrast enhancement is not a specific sign of active tumour, nor do all high-grade gliomas enhance [3]. Whilst harmonisation of imaging protocols can improve comparability, certain variations in technical parameters or patient position are difficult to completely eradicate, and can lead to overdiagnosis of disease progression [4, 5••]. Volumetric imaging is desirable, but may not be universally available, due to equipment or time constraints.
Pseudoprogression
Chemoradiation and radiotherapy of GBM can lead to an increase in tumour volume, oedema and enhancement, known as pseudoprogression (PsP), shortly after completion of treatment, which is often difficult to distinguish from progressive tumour [6, 7]. PsP occurs in 20–30% of patients and is defined as the appearance of new enhancing lesions and/or oedema in the absence of progressive disease (PD). These changes are followed by subsequent improvement or stabilisation without further treatment [8,9,10]. The precise mechanism remains poorly understood with most cases peaking within 3 months of completing chemoradiation, although some cases present well beyond the 12-week timeline [8]. PsP is thought to be due to a pronounced local tissue reaction involving an inflammatory component, oedema and abnormal vessel permeability. A variety of structural features have proven to be unreliable predictors of PsP, with the exception of subependymal enhancement, which according to one study may represent a relatively specific (93.3%) sign for GBM progression [6]. Studies have shown that there is a higher incidence of PsP in tumours with methylated MGMT and an association with increased survival, perhaps representing an active inflammatory response against the tumour [10,11,12]. PsP is not exclusive to treated GBM and has also been reported following radiotherapy for low-grade gliomas [13].
Pseudoresponse
Pseudoresponse is the radiological phenomenon whereby anti-angiogenic agents, e.g. bevacizumab, can produce early (within 1–2 days) and dramatic reduction of tumour enhancement and peri-tumoural oedema, as a result of reduced vascular permeability to contrast agents, known as vascular normalisation, rather than a true anti-tumour effect [14, 15] (Fig. 1). A subset of patients that initially experience reduction in tumour contrast enhancement subsequently develop non-enhancing tumour progression, best visualised on T2/FLAIR sequences [16, 17].
Multiparametric MRI of recurrent left frontotemporal GBM, treated with bevacizumab showing early pseudoresponse and vascular normalisation. Each column shows a different imaging biomarker derived from MRI at four timepoints. Column 1 shows long echo time MRSI with a high choline peak which remains stable up to 3 months after treatment. This is consistent with the absence of significant tumour cell kill. Column 2 shows a heterogeneous axial T2W image showing some reduction in the central cystic component with little change in mass effect. Columns 3 and 4 show DWI at b1000 and ADC images. There is no evidence of tumour cell kill. Vascular normalisation would be expected to decrease the extravascular space and so to reduce ADC values but this is not readily evident. Column 5 shows the axial T1W + Gadolinium in the equilibrium phase showing significant reduction of contrast enhancement which appears at the day 10 scan and is maintained for 3 months consistent with reductions in BBB permeability (pseudoresponse). Columns 6 and 7 show perfusion weighted imaging (rCBF and rCBV) showing an early reduction of rCBF and rCBV around the cyst accompanied by increases anteriorly consistent with vascular normalisation. (Figure kindly provided by Prof. Anwar Padhani, Paul Strickland Scanner Centre, Mount Vernon Cancer Centre, UK)
RANO criteria
Therapeutic trials use progression-free survival (PFS) as a surrogate for overall survival (OS), based on radiographic assessment of post-contrast T1-weighted and non-contrast T2-weighted/FLAIR MRI. As MRI parameters are used to define progression-free survival, this can confound assessments of treatment response and lead to erroneous conclusions being made either on the presumed efficacy or lack of efficacy of treatments. In recognition of this, an international working party was convened in 2008 to update the response assessment criteria for high-grade gliomas and produced a paper in 2010 known as the RANO criteria (Response Assessment in Neuro-oncology) (Table 1) [18]. These criteria were refined around the complexities of imaging following the advent of chemoradiotherapy for newly diagnosed GBM and anti-angiogenic agents for recurrent GBM. Prior to this, imaging response assessment tools used the Macdonald criteria [19], which originated in the era of cytotoxic chemotherapy where radiographic findings directly reflected anti-tumour effect.
Limitations of RANO criteria
The clinical application of the RANO criteria is that patients with progressive radiographic findings can continue current therapy pending follow-up imaging by defining true progression as occurring no sooner than 3 months following completion of chemoradiation, unless there is (i) new enhancement outside the main radiation field or (ii) pathological confirmation of unequivocal tumour progression.
Despite these considerations, the RANO criteria still rely on two-dimensional measurements of enhancing tissue and are operator dependent. These measurements can be challenging when the enhancement has ill-defined margins and/or an irregular shape. Single centre studies have shown promise in using semi-quantitative MR measures such as apparent diffusion coefficient ratios [20], choline, creatine and N-acetylaspartate ratios from MR spectroscopy [21] and perfusion imaging [22] for differentiating PsP from progressive disease (PD) but these techniques have not yet been incorporated into response criteria, as they are not universally available, are difficult to reproduce and increase the overall cost of the imaging examination. They are unlikely to gain widespread acceptance until they have been validated in clinical trials.
There are several therapeutic trials currently underway comparing conventional imaging with advanced MRI techniques to improve treatment response criteria. In the paediatric high-grade glioma population, the HERBY trial is comparing conventional MRI with perfusion/diffusion MRI for response assessment while investigating the practicality of obtaining high quality diffusion/perfusion scans in a multi-centre setting [23]. The recent publication of updated response assessment criteria for the evaluation of patients undergoing immunotherapy (iRANO) [24] demonstrates that imaging response criteria will continually evolve as newer treatments are developed and more sensitive MRI surrogates of tumour burden are evaluated (see below).
Diffusion weighted imaging
Diffusion weighted MRI (DWI) examines the movement of water molecules in brain parenchyma. In any area, in which water diffusion is focally impaired (‘restricted’), this is displayed as bright image signal. Through mathematical subtraction of unwanted T2 effects, the apparent diffusion coefficient (ADC) map is generated, on which dark signal must correspond in location to confirm restriction. ADC signal in glioma is partly influenced by cellularity, making DWI a technique of great interest for both grading and detecting disease recurrence [25, 26].
Numerous studies have reported a difference in the ADC values of PsP and PD [27,28,29], but variable ADC thresholds with no clear cutoff have made it difficult to extrapolate beyond a single institution level. It has been proposed that ADC histogram analysis, specifically the 5th percentile value of the cumulative ADC histogram, may be a better predictor of PsP versus PD (with 90% sensitivity and specificity) [30]. At low diffusion gradient strengths (‘b values’), perfusion effects can neutralise the reduced ADC signal of cellular neoplasms. Therefore, obtaining histograms from high b value (b3000) imaging may improve diagnostic power, and for this the 5th percentile of the cumulative ADC histogram achieved superior accuracy compared to the standard b1000 value [31•].
Diffusion tensor imaging (DTI) gathers data from a greater number (6–256) of diffusion directions than DWI (3 directions). Although used mainly for presurgical tractography, DTI has also been applied to the distinction between PsP and PD [32], but has not been widely validated for treatment monitoring. The clinically disseminated DWI assumes a Gaussian normal distribution of diffusion as this would be the case in water, and is therefore subject to inaccuracies. Diffusion kurtosis imaging (DKI) constitutes an innovative imaging method, which can be calculated from DTI data and describes the deviation of diffusion values in tissue from the Gaussian curve. There is evidence that DKI and related mathematical models can yield information on glioma cellularity and on tissue heterogeneity with a diagnostic precision superior to standard DWI and DTI [33]. The application of DKI in assessing treatment response is discussed below.
In respect of pseudoresponse, enlarging areas of diffusion restriction corresponding to non-enhancing tumour, occurring with anti-VEGF treatment, have long represented a diagnostic dilemma because it was unclear if these represent viable tumour or tissue necrosis due to treatment response. Two comprehensive studies correlating histology with areas of low ADC signal changes have shown that these areas were consistent with aggressive recurrent GBM, either throughout or as a tumour rim. This result was matched by poor outcomes in all subjects [34•, 35].
Perfusion weighted imaging
Perfusion weighted imaging (PWI) exploits the neoangiogenic properties of proliferating gliomas, and is able to identify areas of high-grade tumour with high accuracy [36]. PWI can be performed in a number of ways; the main techniques in clinical practice are dynamic susceptibility-weighted contrast-enhanced MRI (DSC), dynamic contrast-enhanced MRI (DCE) and arterial spin labelling (ASL).
Dynamic susceptibility contrast
DSC represents the most commonly used modality, with gradient echo (T2*) images obtained at rapid intervals during the first pass phase of a gadolinium bolus injection. Relative cerebral blood volume (rCBV) has become the most validated perfusion parameter and reliably correlates with tumour grade, vascularity and focal anaplastic transformation [37, 38]. Using a threshold value of 1.75, DSC has high (95%) sensitivity but relatively low (70%) specificity in distinguishing LGG from HGG, as certain LGG, particularly oligodendrogliomas, may contain areas of high rCBV [39].
DSC studies have consistently demonstrated high accuracy (>90%) in differentiating between PsP and PD [40,41,42]. In a systematic review summarising the evidence for DSC for the PsP/PD indication, the main issue of defining a ‘universal’ rCBV threshold was highlighted [43]. In a recent meta-analysis, the high accuracy of DSC was confirmed (pooled sensitivities and specificities for rCBVmean and rCBVmax in the region of 90%) but only in individual studies with highly variable cutoff values [44••]. Contrast dose, bolus timing and vendor software may all influence DSC signal, probably to a greater extent than interoperator variation, and are challenging to harmonise between institutions [22, 45].
Because of these considerations and the fact that it is not practical to biopsy all new lesions with an elevated rCBV, repeat PWI at a short interval can help clarify the situation: indeed, longitudinal trends in rCBV could be more useful than absolute rCBV in distinguishing PsP from PD [22]. Again, a multiparametric approach might be considered here, for example Wang et al. found high accuracy (area under the curve/AUC 0.91) for a model combined with DTI, which permitted distinction not only between PsP/PD but also for PD and mixed response [46].
The complexity of defining a rCBV threshold for PSP/PD distinction is exacerbated in patients receiving anti-angiogenic drugs, although PWI could still be useful for treatment monitoring [47]. In one study, pretreatment perfusion appears to be the principal determinant of likely response to bevacizumab in GBM, whereby tumours with higher rCBV values retain this feature during treatment despite a greater anti-angiogenic effect of the drug [48].
Dynamic contrast enhancement
Dynamic contrast enhancement (DCE), or permeability imaging, is a T1-based perfusion technique, which can be a useful adjunct for lesions in which susceptibility artefact from blood products or calcification prevents DSC quantification, or where rCBV values are indeterminate [49]. The pharmacokinetic modelling required for DCE quantification is challenging, whereby a diversity of methods of imaging and post-processing analysis are described in the literature, some with an unclear physiological basis [44••]. This has led to its less widespread use in daily practice. In individual studies, DCE parameters (most frequently the volume transfer constant ‘K trans’) have shown good correlation with tumour malignant potential and for the distinction between PsP and PD: DCE results to date include a higher K trans at baseline as a predictor of worse PFS and OS [48] and a higher K trans for recurrent glioma compared to radiation necrosis [50]. A combination of K trans and plasma volume (Vp) enabled the distinction between PsP and PD with 85% sensitivity and 79% specificity [51••]. Too few studies are available to carry out meta-analysis [44••].
Arterial spin labelling
ASL uses magnetically labelled blood and has the advantage of not requiring a gadolinium contrast injection. Because of its low signal to noise ratio (SNR) and need for specialist post-processing, it has not yet featured much in brain tumour clinical imaging [43].
MR spectroscopy
MR spectroscopy (MRS) examines the distribution of chemical metabolites within a chosen volume of brain tissue. It can be performed either as a single voxel technique (SVS) to obtain average metabolite values within the region of interest or through simultaneous analysis of several voxels (multi-voxel spectroscopy/MVS, chemical shift imaging/CSI). SVS is quick and readily available as a standard on most clinical MRI systems, but cannot capture spatial tissue heterogeneity, whereas multi-voxel techniques are more demanding in terms of preparatory steps and data post-processing. Ample evidence exists for the value of MRS in the distinction of glioma from non-neoplastic conditions and for glioma grading [51••], whereby the best validated ratios indicative of tumour are Cho/NAA (choline/N-acetyl-aspartate) and Cho/Cr (choline/creatine) ratios.
The utility of MRS in post-therapeutic imaging is less well validated. A single study analysis seeking to define a threshold for MRS and ADC in distinguishing PD from PsP reported a sensitivity and specificity >95%, but included less than 40 patients [52]. Other investigators observed a significant reduction in metabolite ratios (Cho/NAA and Cho/Cr) in 26 HGG patients comparing baseline to 2 months after radiotherapy (RT) which was associated with a worse outcome, possibly explained through reduced cell death (and thus choline liberation) in non-responders [53, 54]. A recent meta-analysis of 455 patients with suspected glioma recurrence after radiotherapy concluded that MRS alone has moderate diagnostic performance in differentiating glioma recurrence from radiation necrosis using Cho/Cr and Cho/NAA metabolite ratios, and strongly recommended its use only in combination with other advanced imaging technologies [55].
Multiparametric imaging
A multiparametric imaging approach may aid PsP/PD distinction. In one study, combining DWI, perfusion and spectroscopy data improved the diagnostic accuracy (from 84–87% for the single modalities to 93%) [56]. A multiparametric (structural, DTI and perfusion MRI) machine learning technique has been developed which can predict sites and severity of future GBM recurrence on preoperative images with >90% sensitivity and specificity [57]. Machine learning studies could be revolutionary, but require computational ‘big data modelling’, which at present confines them to engineering-supported research environments.
Emerging techniques
1. Novel MRI sequences
i. Advanced diffusion techniques
DWI examines the movement of water molecules in biological systems, whereby clinical DWI assumes a normal (‘Gaussian’) distribution of diffusion values, as this would be the case in free water. In reality, the complex intracellular and extracellular in vivo environment causes the diffusion of water molecules to deviate significantly from this pattern. DKI is an attempt to account for this variation by providing a more accurate model of diffusion and capturing the true diffusion behaviour as a marker of tissue heterogeneity [58], whereby steep (‘leptokurtotic’) curves have been associated with high-grade glioma. Several studies have shown that DKI can differentiate between different grade in gliomas [59, 60]. A recent study investigating DKI and the molecular profile of gliomas has shown that normalised mean kurtosis is significantly lower in tumours with IDH1/2 mutation than tumours with IDH 1/2 wild type [61].
Attempts at more accurate modelling of diffusion in tumour tissue has led to the development of a novel technique called VERDICT (Vascular, Extracellular and Restricted Diffusion for Cytometry in Tumours) which models three primary components: (i) intravascular, (ii) extracellular-extravascular space (EES) and (iii) intracellular water to DW-MRI datasets with various diffusion times and diffusion weightings [62]. The model allows the extraction of features such as cell size and has recently been applied to gliomas at our institution in a feasibility study and shows promise in mapping glioma microstructure which has important implications for presurgical planning and assessing treatment response.
ii. Chemical exchange saturation transfer
Chemical exchange saturation transfer (CEST) MRI is sensitive to the chemical exchange between exchangeable protons on functional metabolite groups (e.g. hydroxyls, amides, amines). The advantages of this technique are that endogenous proteins are used to create imaging contrast rather than exogenous contrast agents and that solute metabolites can be studied at very small concentrations (below what can be visualised with MRS). The majority of CEST imaging studies in GBM have used the amide group to generate CEST contrast, showing that amide proton transfer (APT) can stratify patients by tumour grade [63] and can differentiate between radiation necrosis and active tumour [64•]. A recent study has targeted the amine protons of glutamine for higher CEST contrast and has provided a novel imaging biomarker for mapping regions of low pH within tumour demonstrating a shorter time to progression for acidic lesions compared to tumours with relatively low acidity [65].
Creatine has also been investigated for CEST signal and a recent report has shown reduced creatine CEST contrast in tumours compared to normal brain in mouse glioma models that may be able to differentiate tumours of different aggressiveness [66]. Finally, D-glucose has been used as a potential biodegradable MR contrast agent for imaging glucose uptake in tumours and the first report in human glioma patients has recently been published [67]. This group demonstrated that dynamic glucose enhanced imaging is safe and feasible in humans with signal changes due to glucose uptake in vessels, the brain and tumour areas. Further work to establish this GlucoCEST technique is underway which may provide comparable information to FDG-PET.
iii. Hyperpolarised MRI
Whilst conventional proton MRS can inform on steady state levels of cellular metabolites, the emergence of hyperpolarized carbon MRS has also enabled imaging of metabolic fluxes in real time [68]. This technique has been used in early imaging of response to targeted therapies and chemotherapy in GBM. A decrease in the hyperpolarized lactate-to-pyruvate ratio has been observed in vivo in orthotopic GBM models treated with everolimus [69] and temozolomide [70]. The first-in-human hyperpolarized brain MRI study is currently underway at UCSF that aims to detect abnormal tumour metabolism in patients and to differentiate treatment-related changes from tumour recurrence (dana.org).
2. Radiomics
Radiomics refers to the extraction and analysis of large amounts of advanced quantitative imaging data with high throughput from conventional MRI sequences for correlation with clinical outcomes [71]. Standardised semantic feature sets such as the Visually Accessible Rembrandt Images (VASARI) are widely used in GBM radiomic studies and can be reproducibly scored by radiologists (wiki.cancerimagingarchive.net). This feature set comprises 30 semantic features including tumour location, proportion of enhancing tumour and definition of the enhancing margin and has been shown to predict survival and molecular subtype in GBMs [72•]. For radiogenomic studies in GBM, computational features have been derived from conventional MRI sequences (T2W/FLAIR/T1W+C) that correlate with the VASARI semantic feature set [73] and with mRNA expression [74], molecular subtype and survival [75]. In a recent study, radiomic features computed from MRIs of treatment-naïve GBMs were able to distinguish patients with long-term and short-term survival [76]. The application of this technique to distinguish radiation necrosis from tumour recurrence has shown that texture features which emphasise edge-related differences can discriminate tumour recurrence from radiation necrosis with one study showing that a machine classifier was superior to radiologists in identifying tumour necrosis in 11 primary and 4 metastatic brain tumour cases [77].
This technique provides reliable non-invasive quantitative measurements from routinely acquired MR brain imaging that could readily be applied in clinical practice to assist radiologists. The challenge for use of radiomics in clinical practice, particularly for multi-centre trials, includes the standardisation of image acquisition protocols across different sites, accurate image-registration and accurate tumour segmentation. Future studies incorporating advanced MRI sequences (such as DWI and MRS) and PET data into radiological datasets for more sensitive feature extraction may provide improved imaging response criteria in future GBM treatment trials.
Assessing treatment response to immunotherapy
There is considerable emerging interest in immune therapies in cancer and a number of phase III trials are underway with vaccines and immune checkpoint inhibitors for GBM. A recent report from our institution showed that the combination of ipilimumab (a monoclonal antibody against cytotoxic T-lymphocyte antigen 4) with bevacizumab was associated with a partial response in 31% of patients and stable disease in another 31%, by RANO criteria [78].
Studies of immunotherapies in other solid tumours have revealed specific issues associated with the radiological assessment of treatment response, reflecting delayed responses or therapy-induced inflammation. In particular, clinical improvement and prolonged survival with visible tumour regression can still occur following initial apparent progression or appearance of new lesions. It has therefore become necessary to refine the RANO criteria for patients undergoing immunotherapy, and iRANO criteria have now been published [24], to provide recommendations for management of patients with early progressive changes seen on imaging after initiation of immunotherapy. These changes can be caused by tumour growth that precedes the development of an anti-tumour immune response or by pseudoprogression associated with an inflammatory immune infiltrate. In such cases, early progressive imaging changes do not necessarily predict a poor outcome. The iRANO criteria will therefore permit continuation of treatment in patients who are clinically stable, even if they are progressing radiologically, and to obtain confirmation of true tumour progression on follow-up imaging.
Conclusions
Despite the plethora of advanced imaging techniques available in most neuro-oncology centres, the assessment of treatment response in clinical trials is still hampered by a number of factors including lack of standardised protocols, the level of post-processing analysis required and the lack of consensus over the most reliable and reproducible imaging modality. Imaging biomarkers must be meaningfully translatable across centres and provide reliable surrogate endpoints for multi-institutional studies and clinical trials.
Further studies are urgently needed to establish reproducibility and applicability of current semi-validated quantitative diffusion and perfusion measures across multiple sites and MRI systems, which in turn will lead to optimisation of patient management and future multi-centre trials.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stupp R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10:459–66.
deSouza RM, Shaweis H, Han C, et al. Has the survival of patients with glioblastoma changed over the years? Br J Cancer. 2016;114:146–50.
Metellus P, Coulibaly B, Colin C, et al. Absence of IDH mutation identifies a novel radiologic and molecular subtype of WHO grade II gliomas with dismal prognosis. Acta Neuropathol. 2010;120:719–29.
Reuter M, Gerstner ER, Rapalino O, Batchelor TT, Rosen B, Fischl B. Impact of MRI head placement on glioma response assessment. J Neurooncol. 2014;118:123–9.
•• Ellingson BM, Bendzhus M, Boxerman J, et al. Consensus recommendations for a standardized Brain Tumor Imaging Protocol in clinical trials. Neuro Oncol. 2015;17:1188–98. This recently published paper is the first to provide international consensus recommendations for glioma imaging in clinical trials, highlighting a need for standardisation that may also be relevant to clinical practice.
Young RJ, Gupta A, Shah AD, et al. Potential utility of conventional MRI signs in diagnosing pseudoprogression in glioblastoma. Neurology. 2011;76:1918–24.
Verma N, Cowperthwaite MC, Burnett MG, Markey MK. Differentiating tumor recurrence from treatment necrosis: a review of neuro-oncologic imaging strategies. Neuro Oncol. 2013;15:515–34.
Radbruch A, Fladt J, Kickingereder P, et al. Pseudoprogression in patients with glioblastoma: clinical relevance despite low incidence. Neuro Oncol. 2015;17:151–9.
de Wit MC, de Bruin HG, Eijkenboom W, Sillevis Smitt PA, van den Bent MJ. Immediate post-radiotherapy changes in malignant glioma can mimic tumor progression. Neurology. 2004;63:535–37.
Brandes AA, Franceschi E, Tosoni A, et al. MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J Clin Oncol. 2008;26:2192–97.
Da Cruz H, Rodriguez I, Domingues RC, Gasparetto EL, Sorensen AG. Pseudoprogression and pseudoresponse: imaging challenges in the assessment of posttreatment glioma. AJNR Am J Neuroradiol. 2011;32:1978–85.
Gerstner ER, McNamara MB, Norden AD, Lafrankie D, Wen PY. Effect of adding temozolomide to radiation therapy on the incidence of pseudo-progression. J Neurooncol. 2009;94:97–101.
van West SE, de Bruin HG, van de Langerijt B, Swaak-Kragten AT, van den Bent MJ, Taal W. Incidence of pseudoprogression in low-grade gliomas treated with radiotherapy. Neuro Oncol. 2016. pii: now194.
Batchelor T, Sorensen A, di Tomaso E, et al. AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell. 2007;11:83–95.
Vredenburgh JJ, Desjardins A, Herndon 2nd JE, et al. Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol. 2007;25:4722–29.
Norden AD, Young GS, Setayesh K, et al. Bevacizumab for recurrent malignant gliomas: efficacy, toxicity, and patterns of recurrence. Neurology. 2008;70:779–87.
Narayana A, Kelly P, Golfinos J, et al. Antiangiogenic therapy using bevacizumab in recurrent high-grade glioma: impact on local control and patient survival. J Neurosurg. 2009;110:173–80.
Wen PY, Macdonald DR, Reardon DA, et al. Updated response assessment criteria for high-grade gliomas: response assessment in Neuro-Oncology working group. J Clin Oncol. 2010;28:1963–72.
Macdonald DR, Cascino TL, Schold Jr SC, Cairncross JG. Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol. 1990;8:1277–80.
Pope WB, Kim HJ, Huo J, et al. Recurrent glioblastoma multiforme: ADC histogram analysis predicts response to bevacizumab treatment. Radiology. 2009;252:182–9.
Bulik M, Kazda T, Slampa P, Jancalek R. The diagnostic ability of follow-up imaging biomarkers after treatment of glioblastoma in the temozolomide era: implications from proton MR spectroscopy and apparent diffusion coefficient mapping. Biomed Res Int. 2015;2015:641023.
Boxerman JL, Ellingson BM, Jeyapalan S, Elinzano H, Harris RJ, Rogg JM, Pope WB, Safran H. Longitudinal DSC-MRI for distinguishing tumor recurrence from pseudoprogression in patients with a high-grade glioma. Am J Clin Oncol 2014.
Jaspan T, Morgan PS, Warmuth-Metz M, et al. Response assessment in pediatric neuro-oncology: implementation and expansion of the RANO criteria in a randomized phase II trial of pediatric patients with newly diagnosed high-grade gliomas. AJNR Am J Neuroradiol. 2016;37:1581–87.
Okada H, Weller M, Huang R, et al. Immunotherapy response assessment in neuro-oncology: a report of the RANO working group. Lancet Oncol. 2015;16:e534–42.
Simon D, Fritzsche KH, Thieke C, et al. Diffusion-weighted imaging-based probabilistic segmentation of high- and low-proliferative areas in high-grade gliomas. Cancer Imaging. 2012;12:89–99.
LaViolette PS, Mickevicius NJ, Cochran EJ, et al. Precise ex vivo histological validation of heightened cellularity and diffusion-restricted necrosis in regions of dark apparent diffusion coefficient in 7 cases of high-grade glioma. Neuro Oncol. 2014;16:1599–606.
Hein PA, Eskey CJ, Dunn JF, Hug EB. Diffusion-weighted imaging in the follow-up of treated high- grade gliomas: tumor recurrence versus radiation injury. AJNR Am J Neuroradiol. 2004;25:201–9.
Asao C, Korogi Y, Kitajima M, et al. Diffusion- weighted imaging of radiation-induced brain injury for differentiation from tumor recurrence. AJNR Am J Neuroradiol. 2005;26:1455–60.
Lee WJ, Choi SH, Park CK, et al. Diffusion-weighted MR imaging for the differentiation of true progression from pseudoprogression following concomitant radiotherapy with temozolomide in patients with newly diagnosed high-grade gliomas. Acad Radiol. 2012;19:1353–61.
Song YS, Choi SH, Park CK, et al. True progression versus pseudoprogression in the treatment of glioblastomas: a comparison study of normalized cerebral blood volume and apparent diffusion coefficient by histogram analysis. Korean J Radiol. 2013;14:662–72.
• Chu HH, Choi SH, Ryoo I, et al. Differentiation of true progression from pseudoprogression in glioblastoma treated with radiation therapy and concomitant temozolomide: comparison study of standard and high-b-value diffusion-weighted imaging. Radiology. 2013;269:831–40. This study examines the value of diffusion imaging to distinguish pseudoprogression from tumour, highlighting the potential benefit of high b value imaging and histogram analysis.
Sundgren PC, Fan X, Weybright P, et al. Differentiation of recurrent brain tumor versus radiation injury using diffusion tensor imaging in patients with new contrast-enhancing lesions. Magn Reson Imaging. 2006;24:1131–42.
Jiang R, Jiang J, Zhao L, et al. Diffusion kurtosis imaging can efficiently assess the glioma grade and cellular proliferation. Oncotarget. 2015;6(39):42380–93.
• Barajas Jr RF, Butowski NA, Phillips JJ, et al. The development of reduced diffusion following bevacizumab therapy identifies regions of recurrent disease in patients with high-grade glioma. Acad Radiol. 2016;23:1073–82. This research identified viable tumour corresponding to regions of low ADC signal following anti-angiogenic therapy by means of histological correlation.
Nguyen HS, Milbach N, Hurrell SL, Cochran E, Connelly J, Bovi A et al. Progressing bevacizumab-induced diffusion restriction is associated with coagulative necrosis surrounded by viable tumor and decreased overall survival in patients with recurrent glioblastoma. AJNR Am J Neuroradiol. 2016.
Law M, Yang S, Wang H, et al. Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. AJNR Am J Neuroradiol. 2003;24:1989–98.
Lacerda S, Law M. Magnetic resonance perfusion and permeability imaging in brain tumors. Neuroimaging Clin N Am. 2009;19:527–57.
Danchaivijitr N, Waldman AD, Tozer DJ, et al. Low-grade gliomas: do changes in rCBV measurements at longitudinal perfusion-weighted MR imaging predict malignant transformation? Radiology. 2008;247:170–8.
Lev MH, Ozsunar Y, Henson JW, Rasheed AA, Barest GD, Harsh 4th GR. Glial tumor grading and outcome prediction using dynamic spin-echo MR susceptibility mapping compared with conventional contrast-enhanced MR: confounding effect of elevated rCBV of oligodendrogliomas. AJNR Am J Neuroradiol. 2004;25:214–21.
Sugahara T, Korogi Y, Tomiguchi S, et al. Posttherapeutic intraaxial brain tumor: the value of perfusion-sensitive contrast-enhanced MR imaging for differentiating tumor recurrence from nonneoplastic contrast-enhancing tissue. AJNR Am J Neuroradiol. 2000;21:901–9.
Hu LS, Baxter LC, Smith KA, et al. Relative cerebral blood volume values to differentiate high-grade glioma recurrence from posttreatment radiation effect: direct correlation between image-guided tissue histopathology and localized dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging measurements. AJNR Am J Neuroradiol. 2009;30:552–8.
Gasparetto EL, Pawlak MA, Patel SH, et al. Posttreatment recurrence of malignant brain neoplasm: accuracy of relative cerebral blood volume fraction in discriminating low from high malignant histologic volume fraction. Radiology. 2009;250:887–96.
Fatterpekar GM, Galheigho D, Narayana A, Johnson G, Knopp E. Treatment-related change versus tumor recurrence in high-grade gliomas: a diagnostic conundrum—use of dynamic susceptibility contrast-enhanced (DSC) perfusion MRI. AJR Am J Roentgenol. 2012;198:19–26.
•• Patel P, Baradaran H, Delgado D, Askin G, Christos P, Tsiouris AJ, Gupta A. MRI perfusion imaging in the evaluation of high-grade gliomas after treatment: a systematic review and meta-analysis. Neuro Oncol. 2016. This systematic meta-analysis confirms the benefit of DSC to distinguish pseudoprogression from recurrent tumour, but highlights the problem of defining a widely applicable threshold value.
Kelm ZS, Korfiatis PD, Lingineni RK, Daniels JR, Buckner JC, Lachane DH et al. Variability and accuracy of different software packages for dynamic susceptibility contrast magnetic resonance imaging for distinguishing glioblastoma progression from pseudoprogression. J Med Imaging (Bellingham). 2015; 2: 026001
Wang S, Martinez-Lage M, Sakai Y, et al. Differentiating tumor progression from pseudoprogression in patients with glioblastomas using diffusion tensor imaging and dynamic susceptibility contrast MRI. AJNR Am J Neuroradiol. 2016;37:28–36.
Choi SH, Jung SC, Kim KW, et al. Perfusion MRI as the predictive/prognostic and pharmacodynamic biomarkers in recurrent malignant glioma treated with bevacizumab: a systematic review and a time-to-event meta-analysis. J Neurooncol. 2016;128:185–94.
Kickingereder P, Wiestler B, Graf M, et al. Evaluation of dynamic contrast-enhanced MRI derived microvascular permeability in recurrent glioblastoma treated with bevacizumab. J Neurooncol. 2015;121:373–80.
Thomas AA, Arevalo-Perez J, Kaley T, et al. Dynamic contrast enhanced T1 MRI perfusion differentiates pseudoprogression from recurrent glioblastoma. J Neurooncol. 2015;125:183–90.
Bisdas S, Naegele T, Ritz R, et al. Distinguishing recurrent high-grade gliomas from radiation injury: a pilot study using dynamic contrast-enhanced MR imaging. Acad Radiol. 2011;18:575–83.
•• Wang Q, Zhang H, Zhang J, Wu C, Zhu W, Li F et al. The diagnostic performance of magnetic resonance spectroscopy in differentiating high-from low-grade gliomas: a systematic review and meta-analysis. Eur Radiol. 2015 Oct 15. This meta-analysis suggests that MRS can contribute to glioma assessment, however, the study raises doubts regarding the accuracy of the technique when used in isolation.
Kazda T, Bulik M, Pospisil P, et al. Advanced MRI increased the diagnostic accuracy of recurrent glioblastoma: single institution thresholds and validation of MR spectroscopy. Neuroimage Clin. 2016;11:316–21.
Quon H, Brunet B, Alexander A, et al. Changes in serial magnetic resonance spectroscopy predict outcome in high-grade glioma during and after postoperative radiotherapy. Anticancer Res. 2011;31:3559–65.
Tolia M, Verganelakis D, Tsoukalas N, Kyrgias G, Papathanasiou M, Mosa E. Prognostic value of MRS metabolites in postoperative irradiated high grade gliomas. Biomed Res Int. 2015;2015:341042.
Zhang H, Ma L, Wang Q, Zheng X, Wu C, Xu BN. Role of magnetic resonance spectroscopy for the differentiation of recurrent glioma from radiation necrosis: a systematic review and meta-analysis. Eur J Radiol. 2014;83:2181–9.
Matsusue EI, Fink JR, Rockhill JK, Ogawa T, Maravilla KR. Distinction between glioma progression and post-radiation change by combined physiologic MR imaging. Neuroradiology. 2010;52:297–306.
Akbari H, Macyszyn L, Da X, et al. Imaging surrogates of infiltration obtained via multiparametric imaging pattern analysis predict subsequent location of recurrence of glioblastoma. Neurosurgery. 2016;78:572–80.
Wu EX, Cheung MM. MR diffusion kurtosis imaging for neural tissue characterization. NMR Biomed. 2010;23:836.
Van Cauter S, Veraart J, Sijbers J, et al. Gliomas: diffusion kurtosis MR imaging in grading. Radiology. 2012;263:492–501.
Raab P, Hattingen E, Frank K, Zanella FE, Lanfermann H. Cerebral gliomas: diffusional kurtosis imaging analysis of microstructural differences. Radiology. 2010;254:876–81.
Hempel JM, Bisdas S, Schittenhelm J, Brendle C, Bender B, Wassmann H et al. In vivo molecular profiling of human glioma using diffusion kurtosis imaging. J Neurooncol. 2016.
Panagiotaki E, Walker-Samuel S, Siow B, et al. Noninvasive quantification of solid tumor microstructure using VERDICT MRI. Cancer Res. 2014;74:1902–12.
Togao O, Yoshiura T, Keupp J, et al. Amide proton transfer imaging of adult diffuse gliomas: correlation with histopathological grades. Neuro Oncol. 2014;16(3):441–8.
• Zhou J, Tryggestad E, Wen Z, et al. Differentiation between glioma and radiation necrosis using molecular magnetic resonance imaging of endogenous proteins and peptides. Nat Med. 2011;17:130–34. Description of a novel MRI technique, amide proton transfer MRI, showing the ability to clearly differentiate gliomas and radiation necrosis in animal models.
Harris RJ, Cloughesy TF, Liau LM, et al. pH-weighted molecular imaging of gliomas using amine chemical exchange saturation transfer MRI. Neuro Oncol. 2015;17:1514–24.
Cai K, Tain RW, Zhou XJ, Damen FC, Scotti AM, Hanriharan H et al. Creatine CEST MRI for differentiating gliomas with different degrees of aggressiveness. Mol Imaging Biol 2016.
Xu X, Yadav NN, Knutsson L, et al. Dynamic glucose-enhanced (DGE) MRI: translation to human scanning and first results in glioma patients. Tomography. 2015;1:105–14.
Brindle KM, Bohndiek SE, Gallagher FA, Kettunen MI. Tumor imaging using hyperpolarized 13C magnetic resonance spectroscopy. Magn Reson Med. 2011;66:505–19.
Chaumeil MM, Ozawa T, Park I, et al. Hyperpolarized 13C MR spectroscopic imaging can be used to monitor everolimus treatment in vivo in an orthotopic rodent model of glioblastoma. NeuroImage. 2012;59:193–201.
Park I, Larson PE, Zierhut ML, et al. Hyperpolarized 13C magnetic resonance metabolic imaging: application to brain tumors. Neuro-Oncology. 2010;12:133–44.
Bai HX, Lee AM, Yang L, et al. Imaging genomics in cancer research: limitations and promises. Br J Radiol. 2016;89:20151030.
• Gutman DA, Cooper LA, Hwang SN, et al. MR imaging predictors of molecular profile and survival: multi institutional study of the TCGA glioblastoma data set. Radiology. 2013;267:560–9. Radiological analysis using the VASARI criteria on a large glioblastoma dataset showing high levels of inter-rater agreement of macroscopic imaging features, and correlating them with genetic expression and gene subtypes.
Gevaert O, Mitchell LA, Achrol AS, et al. Glioblastoma multiforme: exploratory radiogenomic analysis by using quantitative image features. Radiology. 2014;273:168–74.
Jamshidi N, Diehn M, Bredel M, Kuo MD. Illuminating radiogenomic characteristics of glioblastoma multiforme through integration of MR imaging, messenger RNA expression, and DNA copy number variation. Radiology. 2014;270:1–2.
Lee J, Narang S, Martinez J, Rao G, Rao A. Spatial habitat features derived from multiparametric magnetic resonance imaging data are associated with molecular subtype and 12-month survival status in glioblastoma multiforme. PLoS One. 2015;10:e0136557.
Yang D, Rao G, Martinez J, Veeraraghavan A, Rao A. Evaluation of tumor-derived MRI texture features for discrimination of molecular subtypes and prediction of 12-month survival status in glioblastoma. Med Phys. 2015;42:6725–35.
Tiwari P, Prasanna P, Wolansky L, Pinho M, Cohen M, Nayate AP et al. Computer-extracted texture features to distinguish cerebral radionecrosis from recurrent brain tumors on multiparametric MRI: a feasibility study. AJNR Am J Neuroradiol. 2016.
Carter T, Shaw H, Cohn-Brown D, Chester K, Mulholland P. Ipilimumab and bevacizumab in glioblastoma. Clin Oncol (R Coll Radiol). 2016;28:622–26.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Harpreet Hyare, Steffi Thust and Jeremy Rees declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neuro-oncology
Rights and permissions
About this article
Cite this article
Hyare, H., Thust, S. & Rees, J. Advanced MRI Techniques in the Monitoring of Treatment of Gliomas. Curr Treat Options Neurol 19, 11 (2017). https://doi.org/10.1007/s11940-017-0445-6
Published:
DOI: https://doi.org/10.1007/s11940-017-0445-6