Opinion statement
Arteriovenous malformations (AVMs) pose a risk of morbidity and mortality throughout an affected patient’s lifetime. Over the course of a patient’s life, the risk of hemorrhage is approximately 1–4 % per year, and after an initial hemorrhage occurs, this risk may be higher. Other causes of morbidity include seizures, headaches, or progressive neurologic deficits. Once an AVM has been discovered, the utility of attempted obliteration or surgical resection compared to the risk of intervention should be entertained. The characteristics of the malformation as well as the patient’s overall health status contribute to the decision to intervene on these lesions. For small lesions located in superficial areas without high-risk surgical characteristics (low-grade Spetzler-Martin grades), it is reasonable to consider surgical resection. In lesions that pose high-risk of complications from surgical removal, intra-arterial embolization, radiosurgery, or a combination of the two may be reasonable treatment options. Some AVMs at traditional high surgical risk may be amenable to partial embolization, allowing initially high-risk lesions to become better candidates for surgical resection. In some patients, particularly those who are older or who have multiple medical comorbidities, the risk of intervention as compared to the annual hemorrhage risk may warrant conservative management as opposed to intervention. The overall treatment strategy must be based on patient and AVM characteristics and careful risk-benefit ratio analysis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An arteriovenous malformation (AVM) is a collection of abnormal blood vessels that can occur in multiple locations in the body, including the nervous system. When AVMs become symptomatic, these anomalies can result in significant morbidity and mortality. In this article, we will focus exclusively on management of AVMs occurring within the brain.
AVMs are classically thought to be congenital lesions, and pathologically demonstrate abnormal fistulous connections of arteries and veins that lack intervening capillary beds. As a result, the high-pressure flow from the arterial system communicates directly with the draining veins through a connection referred to as the nidus of the AVM (Fig. 1). On pathological examination, the arterioles feeding the malformation may demonstrate abnormalities of the muscular layer [1]. The abrupt transition from artery to vein causes fibroblast proliferation and thickened, “arterialized” walls in the venous system, along with significant venous distension and occasional venous pseudoaneurysmal development [2]. Aneurysms can also develop on the arterial side or within the nidus itself.
With the passage of high-pressure flow directly into the venous system, intracerebral hemorrhage can occur at any age and may be the initial clinical presentation of an AVM [3]. The overall estimated risk of hemorrhage of an unruptured AVM is between 1.3 and 4.1 % per year [4–8, 9••, 10].
Spetzler and Martin developed a grading system based on the size, location, and venous drainage of the malformation to estimate the risk associated with surgical resection [11]. This classification has become the primary means to indicate the severity of the malformation and risk assessment for intervention. The Spetzler-Ponce classification (SP) has also been used to estimate surgical risk and is a simplification of the Spetzler-Martin (SM) scale [12] but requires independent validation.
Once an AVM has bled, the risk of rebleeding is significantly increased in the first year but declines over time and eventually matches the risk of bleeding for unruptured AVMs [13]. A recent meta-analysis identified prior hemorrhage, deep location, deep venous drainage, and AVM-associated aneurysms as risk factors that predispose to hemorrhage [14]. In addition to hemorrhage, brain AVMs can cause headache, seizures, and progressive, disabling neurologic symptoms.
Once an AVM is discovered, either due to symptoms or incidentally on neuroimaging, patients are considered for definitive management or optimal medical management without intervention. Several studies, most recently the “Medical management with or without interventional therapy for unruptured brain arteriovenous malformations” (ARUBA) trial [9••] have attempted to identify optimal treatment regimens for these patients. Interventional procedures used to obliterate AVMs include endovascular embolization, stereotactic radiosurgery, or open neurosurgical procedures, used alone or in combination. In some cases, conservative management with close monitoring of chronic medical conditions along with symptomatic treatment is preferred.
Treatment
Patients with AVMs can come to the attention of neurologists or neurosurgeons after the onset of symptoms (e.g., headache, seizure, or focal neurological deficit) or by incidental radiological detection of the AVM. Most brain AVMs present symptomatically. In population-based studies, 43–71 % of brain AVMs present with intracranial hemorrhage (ICH) [5, 10, 15–19]. Other presentations include seizures (18–40 %), headaches (5–14 %), and focal neurological deficits. Approximately 20 % of patients with an AVM have had no related symptoms upon its discovery [20].
Ruptured AVMs confer high morbidity and mortality and thus justify treatment in almost all cases. Deciding whether to treat unruptured AVMs, however, is more challenging given relatively low annual hemorrhage rates and incomplete understanding of natural history. An important factor in the decision to treat is the surgical risk. Large or multiple lesions, those in eloquent brain regions, and those with deep venous drainage are characteristically more difficult to resect safely, and this is reflected in the SM grading system.
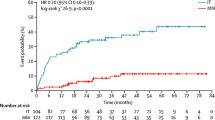
The recently published ARUBA trial aimed to identify the optimal therapy for patients with unruptured brain AVMs [9••]. Patients were randomized to interventional therapy (neurosurgery, embolization, radiotherapy, or a combination thereof) with medical management or medical management alone. This study was halted due to the apparent superiority of the medical management group, and the analysis included 223 patients. There was a higher prevalence of adverse events, including death, in the interventional group. However, the study has been criticized because a substantial proportion of eligible patients were treated outside of the trial and the types of interventions varied widely, with some receiving surgery, radiotherapy, or embolization alone and others receiving surgery with pre-treatment embolization or radiotherapy with preceding embolization. No patients received the combination of surgery and radiotherapy, so it is unclear whether results of ARUBA can be extrapolated to this population. There are also other populations not included in ARUBA. The majority of patients were white and had high pre-randomization functional status, the majority had low SM grade lesions that were supratentorial, few had associated aneurysms, and most had superficial venous drainage. Given this, it is difficult to extrapolate the results of this study to all patients with brain AVMs [9••]. A recent study evaluated a subset of ARUBA-eligible patients and found that the risk of stroke or death in patients undergoing intervention was less than reported in ARUBA (14.8 vs 30.7 %), raising some question to the generalizability of the trial [21••]. Nonetheless, the results of ARUBA substantiated previous findings from some observational studies suggesting that intervening on unruptured AVMS was associated with worse outcomes compared to no treatment [22]. In contrast, other observational studies, however, have found benefit for surgical intervention on subsets of patients, typically those with low SM grade AVMs [23••, 24••]. The optimal treatment regimen for an individual patient can be difficult to determine, and treatment is dependent on characteristics of the patient, the AVM, and the expertise at the treating medical center. Age is the most important patient-related factor in estimating the cumulative risk of AVM rupture (typically 2–4 % per year). Younger patients typically deserve a more aggressive approach given the higher lifetime risk of hemorrhage without treatment. The most recent recommendation from the American Heart Association (AHA) was published in 2001, before the more recent ARUBA trial, among others, was completed [9••, 21••, 23••, 24••]. The AHA recommended consideration of surgery for low SM grade lesions unless lesion location or draining vein characteristics precluded safe resection, where radiosurgery may be more appropriate. High-grade (SM IV or V) may pose excess procedural risk, and surgery is typically not recommended as monotherapy, but a combined approach may be beneficial in select cases. For intermediate (grade III) lesions, multimodality treatment was suggested. In all cases, with the exception of palliative treatment, the goal should be eradication of the lesion, as the risk of hemorrhage is increased with partial treatment [25].
Once it is determined to treat an AVM, there are multiple options. Surgery has been the mainstay of treatment. Radiosurgery is a useful option, particularly for lesions at high surgical risk, and endovascular embolization can be a valuable adjunct to these procedures. The goal of all therapies should be obliteration of the malformation, though embolization can also be used in a palliative capacity to attempt to limit further neurologic decline when the AVM is not amenable to definitive management. Outside of a palliative approach, partial obliteration of an AVM confers the risk of a procedure without reducing the risk of hemorrhage.
Endovascular embolization
Endovascular embolization of an AVM is most often used in combination with other treatment modalities. As part of combination therapy, the goal may be to reduce the overall size of the nidus prior to surgery or radiosurgery or to target specific high-risk characteristics (e.g., nidal or pre-nidal aneurysms and fistulas) prior to treatment with other modalities. This method can also be used as a palliative measure in an attempt to prevent further neurologic decline when the AVM is not amenable to other treatment modalities.
Standard procedure
Selective cerebral angiography is performed and should usually include bilateral carotid and vertebral artery injections as well as assessment of pial and dural territories. Microcatheters and distal access catheters have been developed to facilitate delivery of embolic agents to small feeding vessels of the malformation. Improvements in microcatheters have allowed superselective catheterization of most pial AVM feeders. Embolysates either liquid based (e.g., n-butyl cyanoacrylate) or ethylene-vinyl alcohol (e.g., Onyx) that will solidify shortly after release are administered into the feeding vessels of the malformation in an effort to decrease the size, target high-risk characteristics (aneurysm or fistula), or—more rarely—completely obliterate the malformation [26].
Complications
For patients who undergo endovascular treatment without adjuvant therapy, those with incomplete or <90 % obliteration of the malformation have demonstrated increased hemorrhage rates and mortality as compared to the expected natural history of these malformations [27]. Some studies have found that approximately 10–14 % of patients suffer complications of the procedure, with disabling neurologic deficits occurring in 2–5 %. Predisposing factors to worsening neurologic deficits after embolization include multiple embolization procedures, nidus size <3 or >6 cm, presence of deep venous drainage, eloquent location of the malformation, increasing patient age, and absence of symptoms pre-procedurally [28, 29]. The most serious complication is hemorrhage, whether intraprocedural or delayed. Brain ischemia can also more rarely occur and may result from migration of embolysates obstructing the normal vascular supply [28]. The overall mortality rate of embolization is 1–3.7 % [28, 30–32].
During the procedure, the embolysate may adhere to the microcatheter from which it is being delivered; however, newer devices now have detachable tips that allow for “breakaway” of the tip and removal of the remainder of the catheter, which has been shown to be a successful means of embolization without leading to further complication [33].
Stereotactic radiosurgery
The use of radiosurgery is often considered in patients with AVMs, either alone or in combination with neoadjuvant embolization, and can be combined with microsurgery as well. The success of radiosurgery is dependent on several factors. One study identified factors predictive of complete obliteration, and these included a low-flow pattern on angiography, absence of arterial enlargement, and no peri-nidal angiogenesis [34]. Additionally, low AVM volume and higher minimum radiation dose have been associated with increased obliteration rates [35, 36]. The use of Gamma knife compared to linear accelerator radiosurgery has not been shown to affect outcomes, with similar obliteration rates being reported between the two modalities in a prior study [34].
Following stereotactic radiosurgery, there is a delay to lesion obliteration, with a median obliteration rate measured between 3 and 5 years [37, 38]. Obliteration rates have been reported between 75 and 80 % of patients and are inversely proportional to AVM size [35, 38–40]. AVMs with a diameter less than 3 cm treated with 20–25 Gy equivalents have a 3-year obliteration rate of 80–95 %. However, larger AVMs have a much lower obliteration rate (33–60 %) [41]. Radiation dose has also been shown to be predictive, with a direct correlation of increasing dose and increased obliteration rates [35, 40].
Standard procedure
Planning for stereotactic radiosurgery requires pre-procedural imaging, with digital subtraction angiography (DSA) and brain imaging to ensure accurate characterization of the malformation in a 3D reconstruction [42]. MRI is typically preferred. Technologies utilizing 3D conventional angiography have further assisted in treatment planning as well [43]. After baseline imaging is obtained, the treatment field and dose is determined by a multidisciplinary team which typically consists of a neurosurgeon, radiation oncologist, and medical physicist. The lowest effective radiation dose is planned so as to prevent adverse side effects [44].
Treatment is delivered in a single fraction, or in cases of large AVMs where a large single dose of radiation may increase the risk of adverse side effects, a staged procedure with several sessions of targeted radiotherapy can be completed [45, 46]. Baseline DSA images are overlaid with source images from CT or MRI completed with fiducial markers. Once the source images with the angiographic images are uploaded into the delivery system, the pre-determined radiation dose is administered to the patient.
Complications
Obliteration following radiosurgery is delayed from months to several years, and in this interval, the risk of hemorrhage remains. The post-treatment annual hemorrhage risk was found to be 1.1 % in previously unruptured AVMs, compared to 2.3 % in previously ruptured AVMs in one study comparing those receiving single-dose treatment [47], however was much higher in a review comparing dose-staged versus volume-staged treatment (12.3 vs 17.8 %) [48]. The finding of increased hemorrhage risk in patients requiring multi-stage treatment may also be a function of a larger and more complex malformation at baseline. Additionally, a persistent risk of hemorrhage will exist in patients with partial obliteration of the AVM.
Nearby normal brain tissue is at risk for radiation-induced changes (RIC), leading to additional neurologic symptoms. The risk of permanent symptoms in pre-treatment unruptured and ruptured AVMs undergoing single radiosurgery treatment is reported to be 2.2 and 1.9 %, respectively [47]. The risk is higher (approximately 13 %) in patients treated with a multi-staged plan, whether based on volume-staged or dose-staged treatment [48].
Microsurgery
Microsurgical excision is the most definitive treatment of brain AVMs. This can be performed as the only treatment or can be preceded by embolization or radiosurgery in an effort to reduce the nidus size. Surgery is often elective for brain AVMs, except in patients who present with acute intracranial hemorrhage requiring hematoma evacuation. The SM grading scale [11] was developed to help stratify the risk of AVM resection and incorporates three lesional characteristics: size, venous drainage, and location of the malformation within an eloquent area of the brain. Grade I lesions are classically small, superficial, and in non-eloquent areas of the brain, while grade VI lesions have high-risk characteristics and are considered to carry prohibitive surgical risk. Surgical risk is also associated with lenticulostriate arterial supply, deep meningeal supply, and a diffuse nidus [41].
A simplified three-tiered classification has been proposed by Spetzler and Ponce and is derived from combining SM grades I and II into the top tier (A) and grades IV and V into the bottom tier (C) [12]. The SP classification has not been widely used or validated, but in a few observational studies, it has been shown that AVM grades A and B can be surgically treated with low risks of permanent morbidity [12, 49].
Standard procedure
Specific procedures for surgical resection are dependent on the size and location of the malformation. Lesions are typically approached with a craniotomy with careful opening of the dura to identify superficial draining veins so that they are not injured. Superficial arterial feeders are identified and coagulated. Aneurysm clips can be used for larger feeding arteries if they cannot be completely coagulated due to the high blood flow. Arterialized veins are often preserved, but occasionally small superficial veins are sacrificed to facilitate dissection. The operator dissects down to the nidus until its deepest aspect is reached. Coagulation of the AVM itself early in the procedure is avoided because it is under high pressure and more prone to rupture if manipulated. The draining veins are then targeted and transected. Once all arterial feeders and venous drainage have been controlled, the nidus is removed. Complete resection is confirmed with intraoperative angiography [41].
Complications
Intraoperative hemorrhage is a potential complication and most commonly a result of AVM bleeding during dissection. Parenchymal injury can occur if the margin of resection is too generous. Additionally, traversing arteries can be mistaken for arterial feeders and inadvertently ligated, causing ischemic injury [21••, 41]. Postoperative complications such as hemorrhage, seizures, infection, and vasospasm are possible, as they are after craniotomy for any indication. New-onset seizures have been reported in up to 15 % of patients. In patients who had seizures preoperatively, seizure frequency may worsen in 10 %, stay unchanged in 35 %, and improve in 55 % [41]. Many surgeons, therefore, prescribe prophylactic antiepileptic medications in the perioperative period.
Combination therapy
For the management of AVMs, the specific treatments listed above can be used alone but are commonly used in combination, particularly with intermediate- and high-grade lesions. Pre-surgical or pre-radiotherapy embolization may be completed to decrease the size of the nidus by targeting arterial feeders in an attempt to decrease the field of radiation or size of surgical resection. Treatment decisions are made by multidisciplinary teams and are often highly individualized.
Lee and colleagues reviewed cases in whom patients underwent embolization prior to stereotactic radiosurgery compared to those undergoing radiosurgery alone and found no statistically significant differences among obliteration rates or complications [50]. Another study found similar results and additionally no increase in long-term complications between combined treatment or radiation alone [51]. Other studies have suggested that the obliteration rate is significantly decreased in patients undergoing embolization prior to radiosurgery when compared to those undergoing radiosurgery alone, without a significant difference in the long-term complications of the procedures [46, 52, 53].
Embolization prior to surgery is typically done in patients with high SM grade lesions in an effort to decrease the size of the malformation and to eliminate high-risk characteristics, including aneurysms and fistulas. The risk of hemorrhage, mortality, or other post-operative complications between patients undergoing embolization and surgery compared to those undergoing surgery alone was shown to be no different in a retrospective review, with 91 % of patients having a good neurologic outcome [54]. However, in another study, the risk of any neurologic decline in patients undergoing combined endovascular and surgical management was shown to be >40 %, with 5 % having disabling deficits [55]. This highly complex group of patients is difficult to analyze systematically because of such heterogeneity in AVM anatomy, procedural expertise, comorbidities, and clinical context. A multimodality approach to high-grade lesions is recommended by the most recent AHA guideline [25].
Management of AVMs during pregnancy
There is limited data available regarding AVM management during pregnancy. The hemorrhage risk may be increased (10.8 vs 1.1 % per year), as shown in a prior retrospective review [14], but this has not been consistent in other studies [56, 57]. For patients who became pregnant during the latency period from stereotactic radiosurgery to confirmed lesion obliteration, the hemorrhage risk may be increased compared to non-pregnant patients [58].
A small series from Japan documented good outcomes with either Cesarean section or vaginal delivery in patients with known AVMs. During pregnancy, three of the identified patients suffered intracranial hemorrhage but did not have worsening of symptoms during or after delivery [59].
The general recommendation in pregnant patients who present with a symptomatic AVM has been to treat if the patient decompensates. The decision to otherwise treat the malformation while a patient is pregnant is dependent on a risk-benefit analysis; however, it is felt that the risk will likely outweigh the benefit in this scenario [25]. There is no standard recommendation for the method of obstetric delivery. The delivery method has not been shown to impact clinical outcomes, but there are few studies available.
Pediatric considerations
Most data regarding AVM management is limited to the adult population. The ARUBA trial did not include patients younger than 18 years of age. Young patients are exposed to a yearly hemorrhage risk, presumably for a much longer period of time as compared to their adult counterparts, conferring a theoretical increased hemorrhage risk over their lifetime.
Given the high lifetime hemorrhage risk, intervention may be justified if the risk-benefit analysis is reasonable and is the most recent recommendation from the AHA [25].
Multiple studies have found that stereotactic radiosurgery leads to generally good outcomes with a reasonable risk profile [37, 60]. Patients receiving a marginal radiation dose of 18–20 Gy had increased obliteration rates when compared to patients receiving <18 Gy of marginal dose radiation [61]. Obliteration rates were shown to be increased after stereotactic radiosurgery with patients receiving a higher marginal radiation dose (at least 22 Gy), two or fewer draining veins, and a lower score on the Virginia Radiosurgery AVM Scale in another study [37]. Additionally, in a retrospective review, microsurgery has also been shown to be well-tolerated in patients treated with this modality with a 94 % obliteration rate, if the lesion characteristics are amenable to such intervention [62]. Embolization using a detachable microcatheter was evaluated in a small cohort of patients to determine safety of this device in the pediatric population. Of 27 total injections, 7 microcatheters detached, more commonly when using NBCA as an embolysate, and no aberrant catheter migration or other complications were identified during a short follow-up period [63].
Multimodality treatment is also common in the pediatric population, and outcomes may be improved with this approach [64].
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Mandybur TI, Nazek M. Cerebral arteriovenous malformations. A detailed morphological and immunohistochemical study using actin. Arch Pathol Lab Med. 1990;114(9):970–3.
Challa VR, Moody DM, Brown WR. Vascular malformations of the central nervous system. J Neuropathol Exp Neurol. 1995;54(5):609–21.
Stapf C et al. Effect of age on clinical and morphological characteristics in patients with brain arteriovenous malformation. Stroke; J Cereb Circ. 2003;34(11):2664–9.
Brown Jr RD et al. The natural history of unruptured intracranial arteriovenous malformations. J Neurosurg. 1988;68(3):352–7.
Crawford PM et al. Arteriovenous malformations of the brain: natural history in unoperated patients. J Neurol Neurosurg Psychiatry. 1986;49(1):1–10.
Graf CJ, Perret GE, Torner JC. Bleeding from cerebral arteriovenous malformations as part of their natural history. J Neurosurg. 1983;58(3):331–7.
Kim H et al. Untreated brain arteriovenous malformation: patient-level meta-analysis of hemorrhage predictors. Neurology. 2014;83(7):590–7.
Mast H et al. Risk of spontaneous haemorrhage after diagnosis of cerebral arteriovenous malformation. Lancet. 1997;350(9084):1065–8.
Mohr JP et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet. 2014;383(9917):614–21. Randomized, prospective trial evaluating treatment of unruptured AVMs. This study had several significant limitations making application to other populations challenging.
Ondra SL et al. The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. J Neurosurg. 1990;73(3):387–91.
Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986;65(4):476–83.
Spetzler RF, Ponce FA. A 3-tier classification of cerebral arteriovenous malformations. Clin Artic J Neurosurg. 2011;114(3):842–9.
Halim AX et al. Longitudinal risk of intracranial hemorrhage in patients with arteriovenous malformation of the brain within a defined population. Stroke; J Cereb Circ. 2004;35(7):1697–702.
Gross BA, Du R. Natural history of cerebral arteriovenous malformations: a meta-analysis. J Neurosurg. 2013;118(2):437–43.
Brown Jr RD et al. Frequency of intracranial hemorrhage as a presenting symptom and subtype analysis: a population-based study of intracranial vascular malformations in Olmsted Country, Minnesota. J Neurosurg. 1996;85(1):29–32.
da Costa L et al. The natural history and predictive features of hemorrhage from brain arteriovenous malformations. Stroke; J Cereb Circ. 2009;40(1):100–5.
Fults D, Kelly Jr DL. Natural history of arteriovenous malformations of the brain: a clinical study. Neurosurgery. 1984;15(5):658–62.
Hofmeister C et al. Demographic, morphological, and clinical characteristics of 1289 patients with brain arteriovenous malformation. Stroke; J Cereb Circ. 2000;31(6):1307–10.
Stapf C et al. Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. Neurology. 2006;66(9):1350–5.
Al-Shahi R et al. Prospective, population-based detection of intracranial vascular malformations in adults: the Scottish Intracranial Vascular Malformation Study (SIVMS). Stroke; J Cereb Circ. 2003;34(5):1163–9.
Rutledge WC et al. Treatment and outcomes of ARUBA-eligible patients with unruptured brain arteriovenous malformations at a single institution. Neurosurg Focus. 2014;37(3), E8. Review of a single center of ARUBA-eligible patients demonstrating improved outcomes as compared to the entire ARUBA cohort.
Wedderburn CJ et al. Outcome after interventional or conservative management of unruptured brain arteriovenous malformations: a prospective, population-based cohort study. Lancet Neurol. 2008;7(3):223–30.
Bervini D et al. Surgery for unruptured arteriovenous malformations of the brain is better than conservative management for selected cases: a prospective cohort study. J Neurosurg. 2014;121(4):878–90. Database review of unruptured AVMs and complications from operative intervention. Patients with Spetzler-Ponce class A lesions tolerated surgery will without significant morbidity.
Potts MB et al. Current surgical results with low-grade brain arteriovenous malformations. J Neurosurg. 2015;122(4):912–20. Reviewed an existing database of low-grade AVMs treated with surgery to evaluate outcomes. Most patients had improved or stable neurologic deficits following surgery. Pre-operative embolization was used in nearly half of patients.
Ogilvy CS et al. AHA scientific statement: recommendations for the management of intracranial arteriovenous malformations: a statement for healthcare professionals from a special writing group of the Stroke Council, American Stroke Association. Stroke; J Cereb Circ. 2001;32(6):1458–71.
Crowley RW et al. Endovascular advances for brain arteriovenous malformations. Neurosurgery. 2014;74 Suppl 1:S74–82.
Wikholm G, Lundqvist C, Svendsen P. The Goteborg cohort of embolized cerebral arteriovenous malformations: a 6-year follow-up. Neurosurgery. 2001;49(4):799–805. discussion 805–6.
Hartmann A et al. Risk of endovascular treatment of brain arteriovenous malformations. Stroke; J Cereb Circ. 2002;33(7):1816–20.
Starke RM et al. Adjuvant embolization with N-butyl cyanoacrylate in the treatment of cerebral arteriovenous malformations: outcomes, complications, and predictors of neurologic deficits. Stroke; J Cereb Circ. 2009;40(8):2783–90.
Debrun GM et al. Embolization of the nidus of brain arteriovenous malformations with n-butyl cyanoacrylate. Neurosurgery. 1997;40(1):112–20. discussion 120–1.
Jayaraman MV et al. Neurologic complications of arteriovenous malformation embolization using liquid embolic agents. AJNR Am J Neuroradiol. 2008;29(2):242–6.
Ledezma CJ et al. Complications of cerebral arteriovenous malformation embolization: multivariate analysis of predictive factors. Neurosurgery. 2006;58(4):602–11. discussion 602–11.
Paramasivam S et al. O-026 safety and efficacy of detachable tip microcatheter for embolization of brain arteriovenous malformation. J Neurointerv Surgery. 2014;6 Suppl 1:A14.
Taeshineetanakul P et al. Angioarchitecture determines obliteration rate after radiosurgery in brain arteriovenous malformations. Neurosurgery. 2012;71(6):1071–8. discussion 1079.
Karlsson B, Lindquist C, Steiner L. Prediction of obliteration after gamma knife surgery for cerebral arteriovenous malformations. Neurosurgery. 1997;40(3):425–30. discussion 430–1.
Zacest AC et al. LINAC radiosurgery for cerebral arteriovenous malformations: a single centre prospective analysis and review of the literature. J Clin Neurosci: Off J Neurosurg Soc Australas. 2014;21(2):241–5.
Ding D et al. Radiosurgery for unruptured cerebral arteriovenous malformations in pediatric patients. Acta Neurochir. 2015;157(2):281–91.
Pollock BE, Link MJ, Brown RD. The risk of stroke or clinical impairment after stereotactic radiosurgery for ARUBA-eligible patients. Stroke; J Cereb Circ. 2013;44(2):437–41.
Lunsford LD et al. Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg. 1991;75(4):512–24.
Flickinger JC et al. An analysis of the dose-response for arteriovenous malformation radiosurgery and other factors affecting obliteration. Radiother Oncol: J Eur Soc Ther Radiol Oncol. 2002;63(3):347–54.
Youmans JR, Winn HR. Youmans neurological surgery. 6th ed. Philadelphia: Saunders/Elsevier; 2011.
Hamm KD et al. Special aspects of diagnostic imaging for radiosurgery of arteriovenous malformations. Neurosurgery. 2008;62(5 Suppl):A44–52. discussion A52.
Colombo F et al. Three-dimensional angiography for radiosurgical treatment planning for arteriovenous malformations. J Neurosurg. 2003;98(3):536–43.
Flickinger JC et al. Dose selection in stereotactic radiosurgery. Prog Neurol Surg. 2013;27:49–57.
Ding C et al. Multi-staged robotic stereotactic radiosurgery for large cerebral arteriovenous malformations. Radiother Oncol: J Eur Soc Ther Radiol Oncol. 2013;109(3):452–6.
Kano H et al. Stereotactic radiosurgery for arteriovenous malformations, Part 6: multistaged volumetric management of large arteriovenous malformations. J Neurosurg. 2012;116(1):54–65.
Ding D et al. Effect of prior hemorrhage on intracranial arteriovenous malformation radiosurgery outcomes. Cerebrovasc Dis. 2014;39(1):53–62.
Moosa S et al. Volume-staged versus dose-staged radiosurgery outcomes for large intracranial arteriovenous malformations. Neurosurg Focus. 2014;37(3), E18.
Korja M et al. Role of surgery in the management of brain arteriovenous malformations: prospective cohort study. Stroke; J Cereb Circ. 2014;45(12):3549–55.
Lee CC, et al. Stereotactic radiosurgery for arteriovenous malformations after Onyx embolization: a case-control study. J Neurosurg. 2015;1–10.
Izawa M et al. Combined management of intracranial arteriovenous malformations with embolization and gamma knife radiosurgery: comparative evaluation of the long-term results. Surg Neurol. 2009;71(1):43–52. discussion 52–3.
Andrade-Souza YM et al. Embolization before radiosurgery reduces the obliteration rate of arteriovenous malformations. Neurosurgery. 2007;60(3):443–51. discussion 451–2.
Schwyzer L et al. Long-term results of gamma knife surgery for partially embolized arteriovenous malformations. Neurosurgery. 2012;71(6):1139–47. discussion 1147–8.
Jafar JJ et al. The effect of embolization with N-butyl cyanoacrylate prior to surgical resection of cerebral arteriovenous malformations. J Neurosurg. 1993;78(1):60–9.
Hartmann A et al. Determinants of staged endovascular and surgical treatment outcome of brain arteriovenous malformations. Stroke; J Cereb Circ. 2005;36(11):2431–5.
Liu XJ et al. Risk of cerebral arteriovenous malformation rupture during pregnancy and puerperium. Neurology. 2014;82(20):1798–803.
Horton JC et al. Pregnancy and the risk of hemorrhage from cerebral arteriovenous malformations. Neurosurgery. 1990;27(6):867–71. discussion 871–2.
Tonetti D et al. Hemorrhage during pregnancy in the latency interval after stereotactic radiosurgery for arteriovenous malformations. J Neurosurg. 2014;121(Suppl):226–31.
Fukuda K et al. Pregnancy and delivery management in patients with cerebral arteriovenous malformation: a single-center experience. Neurol Med Chir. 2013;53(8):565–70.
Borcek AO et al. Gamma knife radiosurgery for arteriovenous malformations in pediatric patients. Childs Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg. 2014;30(9):1485–92.
Potts MB et al. Stereotactic radiosurgery at a low marginal dose for the treatment of pediatric arteriovenous malformations: obliteration, complications, and functional outcomes. J Neurosurg Pediatr. 2014;14(1):1–11.
Gross BA et al. Microsurgical treatment of arteriovenous malformations in pediatric patients: the Boston Children’s Hospital experience. J Neurosurg Pediatr. 2015;15(1):71–7.
Altschul D et al. Safety and efficacy using a detachable tip microcatheter in the embolization of pediatric arteriovenous malformations. Childs Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg. 2014;30(6):1099–107.
Darsaut TE et al. Management of pediatric intracranial arteriovenous malformations: experience with multimodality therapy. Neurosurgery. 2011;69(3):540–56. discussion 556.
Compliance with Ethics Guidelines
Conflict of Interest
Sherri A. Braksick and Jennifer E. Fugate declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Critical Care Neurology
Rights and permissions
About this article
Cite this article
Braksick, S.A., Fugate, J.E. Management of Brain Arteriovenous Malformations. Curr Treat Options Neurol 17, 32 (2015). https://doi.org/10.1007/s11940-015-0358-1
Published:
DOI: https://doi.org/10.1007/s11940-015-0358-1