Abstract
Purpose of review
The purpose of this review is to analyze the long-term prognostic value of stress perfusion cardiovascular magnetic resonance (CMR) in patients with suspected or known coronary artery disease (CAD).
Recent findings
Stress perfusion CMR provides high diagnostic accuracy for detection of CAD, with high sensitivity and relatively lower specificity. A normal stress perfusion CMR examination is highly predictive of overall low patient risk. Conversely, abnormal stress perfusion CMR results are associated with mortality and increased risk for adverse cardiac-related events. Stress perfusion CMR is a useful and robust tool for risk reclassification across different CAD risk categories, and most significant for patients of intermediate risk. Stress CMR is reliable for excluding clinically significant coronary artery disease in patients presenting with low-risk acute chest pain. An ischemic burden threshold of less than 1.5 cardiac segments has been found to be most appropriate for safe deferral from revascularization therapy. A stress perfusion CMR-guided strategy has been shown to be noninferior compared to fractional flow reserve (FFR) for revascularization in patients with stable CAD. In clinical practice, CMR offers a multiplicity of useful techniques besides stress perfusion which may add significant prognostic value when combined with the findings of the stress test itself.
Summary
Stress perfusion CMR is an accurate noninvasive diagnostic test for patients with suspected CAD and provides strong prognostic value across different risk categories.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart disease continues to be the leading cause of death worldwide [1]. Of the cardiac diseases, obstructive coronary artery disease (CAD) is one of the most significant. Mortality from CAD is predicted to exceed 23 million by 2030 [2]. Due to the tremendous morbidity, mortality associated with this disease, early and accurate diagnosis and treatment is imperative. Of particular interest is diagnosis of stable obstructive coronary artery disease, which is often characterized by transient exertional episodes of chest pain secondary to demand-supply mismatch [3]. Conventional coronary angiography remains the gold standard for diagnosis of obstructive CAD. Over the past several decades, however, there have been substantial advances in the field of noninvasive cardiac imaging, and in particular cardiac magnetic resonance (CMR). Currently, CMR is widely used as a noninvasive assessment of cardiac function and myocardial viability. Furthermore, stress perfusion CMR imaging has also evolved into a widely utilized diagnostic measure for CAD.
We will briefly summarize the technical aspects of the stress perfusion CMR exam and outline the methods of its image analysis. The most common clinical application of stress perfusion CMR is diagnosis of CAD, and we will review data on its diagnostic performance. The emphasis of this work will be to analyze the long-term prognostic value of stress perfusion CMR. This will include analysis of the prognostic implications of a normal and abnormal stress perfusion CMR test as well as its utility in patient risk stratification. We will also explore how stress perfusion CMR can aid in clinical decision making and its role in guiding revascularization therapy in patients with stable CAD. Lastly, we compare CMR to SPECT, with emphasis on its ability to predict outcomes for patients with known or suspected CAD.
Description of technique and image analysis
Stress perfusion imaging with CMR has much in common with the coronary flow reserve. The test is performed during a physiologic resting state as well as during a “stress” state when there is maximal coronary vasodilation. In stress perfusion CMR, pharmacologic vasodilation is most commonly achieved with adenosine [4]. A typical stress/rest perfusion protocol consists of the following steps:
- 1.
Infusion of adenosine over 3 min at 140 μg/kg/min
- 2.
Administration of gadolinium contrast during final minute of adenosine infusion
- 3.
Dynamic T1-weighted imaging for 40–50 heartbeats (4–5 slices are obtained during each heartbeat)
- 4.
Continuous monitoring of ECG and BP at baseline, during and post-adenosine infusion.
Image interpretation in clinical practice is most commonly performed via simple qualitative visual assessment of the stress and rest perfusion images. Myocardial tissues which are adequately perfused demonstrate increased signal intensity on the dynamic T1-weighted images. Assessment for CAD is most effectively done when integrating interpretation of the stress/rest perfusion images with that of the late gadolinium enhancement images (LGE) to evaluate for ischemia and prior myocardial infarction [5]. A defect seen on the stress images which normalizes in intensity on the rest images without associated late gadolinium enhancement (LGE) is defined as ischemic. A perfusion defect which is matched with LGE images can be described as “fixed defect” or “scar” [6]. An alternative approach is quantitative image analysis. The advantage is that this potentially provides absolute computation of blood flow through the myocardium. Unfortunately, the required post-processing is significantly more labor-intensive, and thus this technique is less feasible in everyday clinical practice [4]. Moreover, the diagnostic accuracy of the quantitative approach was not found to be superior to that of visual interpretation [7].
Stress perfusion CMR for detection of CAD
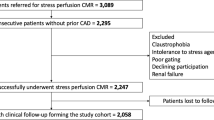
The most common and perhaps most applicable indication for stress perfusion CMR is to assess for hemodynamically significant CAD. Its diagnostic accuracy has been evaluated in numerous patient studies, both retrospective and prospective. In a 2008 multicenter study including 221 patients, Schwitter et al. were able to demonstrate at least equal diagnostic performance of adenosine stress CMR in a head to head comparison with SPECT, based on ROC analysis [8].
A multicenter meta-analysis of 1516 patients (24 datasets) demonstrated a sensitivity of 0.91 and specificity of 0.81 for diagnosis of CAD by stress perfusion CMR [9]. The sensitivity and specificity were attained from a patient population with a relatively high pretest probability of CAD, who had been referred to undergo X-ray angiography [9]. Overall, data shows that stress perfusion CMR provides high diagnostic accuracy for detection of CAD.
Prognosis of negative stress perfusion CMR
Data from multiple studies shows that stress perfusion CMR has high negative predictive value for adverse events. In a multicenter study including 9151 patients followed up for up to 10 years, Heitner et al. demonstrated that a normal stress perfusion CMR showed low overall patient risk. They found annual mortality rates of 0.8%, 1.4%, and 2.7% for patients with low, intermediate, and high Framingham risk, respectively, versus 2.7%, 4.0%, and 4.9% respectively for patients with abnormal stress perfusion CMR [10••]. Furthermore, the 9151 patients of this study were subdivided into 8 subpopulations based on presence of CAD and clinical history: ± history of CAD, normal vs abnormal LVEF (55% threshold), presence/absence of CMR LGE, and presence/absence of typical chest pain. Kaplan-Meier survival analysis was performed in each of these subpopulations with the results yielding significantly higher survival (P < 0.001) for patients with a normal stress perfusion CMR compared to those with an abnormal stress test [10••]. The same findings were observed with a Kaplan-Meier analysis of the whole study population, and accounting for age, sex, and cardiac risk factors [10••].
A separate meta-analysis performed by Gargiulo et al. including 14 studies and 12,178 patient reported a stress perfusion CMR negative predictive value for nonfatal myocardial infarction and cardiac death of 98.12% (95% CI of 97.26–98.33) [11]. This was equivalent to a pooled event rate after negative test (ERNT) of 1.88% and an annualized ERNT of 1.03% [11]. These values are similar to the annual mortality estimates of the meta-analysis by Heitner et al. and only marginally higher than the background event rate of individuals of low risk (< 1%) [12]. A subset of the studies selected in this meta-analysis utilized CMR stress wall motion imaging (dobutamine stress). No significant difference was found in the NPV of stress perfusion CMR and CMR dobutamine stress for prediction of adverse cardiac-related events. One of the main limitations of this meta-analysis, however, is that it provides limited evaluation of the NPV of stress perfusion CMR in relation to pretest risk. This was mainly due to lack of availability of relevant clinical data to perform the necessary subgroup analysis [11]. Overall, however, the data undeniably shows that CMR stress perfusion provides excellent negative predictive value.
In combination with LGE
A single CMR study offers a multiplicity of useful techniques besides stress perfusion which may add significant prognostic value when combined with the findings of the stress test itself. The value of LGE as an independent predictor has been well established [13]. LGE, however, offers complementary prognostic value when combined with stress perfusion CMR. In a study of 254 patients referred for CMR for symptoms of myocardial ischemia, the combination of negative stress perfusion and LGE were predictive of a 98.1% negative annual event rate for death or myocardial infarction [13]. When assessed individually, the negative annual event rates for negative stress perfusion CMR and LGE were 95.8% and 96.1% respectively [13].
Negative prognostic value of CMR stress in the acute setting
Acute chest pain is one of the most common reasons for visits to the emergency department (ED). Of particular interest are patients whose acute chest pain is classified as “low risk” based on a resolved pain syndrome, unremarkable serial electrocardiograms (ECGs), and negative biomarkers for myocardial necrosis [14]. Various types of stress tests are often utilized in deciding which of these patients are of high enough risk to qualify for an invasive coronary angiography and which can be safely discharged home. The predictive value of stress perfusion CMR in this acute context was evaluated in a retrospective study of 89 patients who had presented to the ED with “low-risk acute chest pain” and had undergone stress perfusion CMR for risk stratification [14]. A composite of cardiac death, nonfatal acute MI, obstructive CAD on invasive coronary angiography, or recurrent chest pain requiring hospital admission was used as the primary endpoint. Eighty-two of the 89 patients (92.1%) had negative stress perfusion CMR studies. The negative prognostic value for the primary endpoint was found to be 100%, after a median follow-up of 292 days [14]. Stress perfusion CMR is a reliable tool for excluding clinically significant coronary artery disease in patients presenting with low-risk acute chest pain.
Prognosis of abnormal stress CMR
Similar as in the case of a normal stress perfusion CMR, important prognostic information can be gleaned from an abnormal examination. This is clearly shown in the study by Heitner et al., which is the most recent and perhaps most powerful with a diverse cohort of over 9000 patients who were prospectively followed for up to 10 years [10••]. The prognostic value of stress CMR was evaluated in three main ways: analysis of patient mortality, multivariate analysis and net reclassification, and survival analysis. The annual mortality of the overall cohort was found to be 3.1% [10••]. Significantly higher mortality was found in patients who had a positive CMR stress test across all three Framingham risk categories in asymptomatic patients. Patients with positive stress perfusion CMR test results were found to have significantly higher annual mortality rates across all Framingham risk categories, compared to those with normal stress CMR test results [10••].
Next, multivariate analysis was performed with the main aim to determine whether CMR stress offered additive prognostic value. Proportional regression (Cox) was used to make distinct multivariable models. The first of these used a priori risk factors of age, sex, history of diabetes, history of hypertension, history of hyperlipidemia, smoking status, history of CAD, and history of myocardial infarction [10••]. The second model utilized programmatic stepwise selection of clinical variables resulting in a selection of risk factors similar to those in the first model. In both models, abnormal stress perfusion CMR was the variable with the highest hazard ratio (HR of 1.8 with 95% CI of 1.6–2.0), while history of diabetes was second highest (HR of 1.5). Additionally, both Cox regression models were performed with and without the inclusion of the variable of abnormal stress perfusion CMR. It was found that there was significant improvement (P < 0.001) in fit of both Cox regression models when abnormal stress perfusion CMR was included as a variable serving as evidence of its predictive value. Net reclassification analysis showed that stress perfusion CMR resulted in net improvement in prediction for the overall cohort of 11.4% (broken down as 6.5% improvement for patients who survived the follow-up period and 4.9% for those who did not) [10••].
Lastly, Kaplan-Meier survival analysis demonstrated a strong association between positive stress CMR and mortality in all patients (HR 1.883; 95% CI, 1.680–2.112) following adjustment for age, sex, and cardiac risk factors. The large number and broad spectrum of patients included in this study allowed for the investigators to perform survival analysis on various subpopulations such as those with and without history of CAD, normal (> 55%) and abnormal LVEF, presence/absence of LGE, and presence/absence of chest pain. In all 8 of these subpopulations, abnormal stress CMR demonstrated a strong association with mortality [10••].
Overall, this study provides strong evidence that abnormal stress CMR findings are associated with mortality. The overall large number and broad spectrum of patients followed in this study as well as the examination of multiple different subpopulations allow for significant reduction in selection bias.
Utility of stress perfusion CMR for risk reclassification
Shah et al. investigate the effectiveness of stress perfusion CMR as a tool to reclassify patient risk beyond standard clinical variables. A cohort of 815 consecutive patients referred for evaluation of myocardial ischemia with CMR was observed. The endpoint in this study, major of adverse cardiac event events (MACE), consisted of nonfatal myocardial infarction or cardiac death [15]. In the overall cohort, inducible ischemia, as assessed by stress perfusion CMR, was again found to be a very strong predictor of MACE (HR of 14.66; P < 0.0001). The most significant findings were however related to improvement of risk reclassification for MACE across ACC/AHA practice guideline recommended annualized risk categories (low, < 1%; moderate, 1–3%; high, > 3%). The addition of inducible ischemia resulted in a net reclassification of 91.5% (65.7% were reclassified to low risk and 25.8% to high risk) of the patients which had originally been placed in the moderate risk category. The annualized rate of MACE for those patients which were reclassified to high risk was 4.9% versus 0.3% for those who had been reclassified from intermediate to low risk [15]. A significant proportion (31.6%) of patients initially classified as high risk was reclassified to moderate risk. Only slightly less than 8% of the patients in the low-risk category were reclassified after the addition of stress perfusion CMR [15]. Overall, this study proves that stress perfusion CMR is a useful and robust tool for risk reclassification across CAD risk categories, and most significant for patients with intermediate risk.
Prognostic value of stress perfusion CMR based on sex
Many of the current noninvasive techniques have been reported to have lower overall accuracy for diagnosis of CAD in women as compared to in men [16]. Multiple causes have been suggested which may contribute to this including breast attenuation imaging artifacts, smaller heart size in women, atypical symptoms, and age-related comorbidities that limit exercise tolerance [16]. Coelho-Filho et al. evaluated the prognostic value of vasodilator stress perfusion CMR in women and compared it to its performance in male patients via a prospective study. The study included 405 patients (168 women) who were referred for ischemia assessment and underwent CMR which included vasodilator stress perfusion and LGE. The patients were followed for a median of 30 months with the main endpoint assessed being major adverse cardiac events (MACE) defined by cardiac death or new acute myocardial infarction [16]. Positive findings on stress perfusion CMR in women were found to be associated with an annual MACE rate of 15%, significantly higher than the MACE annual rate in women with a negative test of 0.3% [16]. Additionally, the ischemic burden as evaluated by stress perfusion CMR was found to be the strongest multivariable predictor of MACE, regardless of sex.
Prognosis of ischemic burden
The previously reviewed studies examined the predictive power of stress perfusion CMR based on an essentially binary stress test result—presence or absence of ischemia, serving as the outcome predictor. Vincenti et al. performed a prospective study with the aim to determine an ischemia threshold for safe patient deferral from revascularization [17]. This was a prospective study of consisting of 1024 patients with known or suspected CAD who were referred for stress perfusion CMR to assess for myocardial ischemia [17]. The CMR evaluation included both adenosine stress perfusion and LGE. The ischemic burden was evaluated quantitatively based on number of involved ischemic segments (16 segment model) [17]. The primary endpoint consisted of composite cardiac death, nonfatal myocardial infarction, and late coronary revascularization (> 90 days post-CMR) and was reached by 8.4% of patients after a mean follow-up of 2.5 years. The secondary endpoint was cardiac death and nonfatal MI and was reached by 3.1% of the patients [17]. ROC analysis was used to show that threshold of > 1.5 segments maximized accuracy for prediction of the primary endpoint with a sensitivity and specificity of 67% and 81% respectively and AUC of 0.77 [17].
Univariate Cox regression analysis showed that an ischemic burden of > 1.5 segments was associated with a greater than 8-fold increase in risk of occurrence of the primary outcome (HR of 8.57 [5.449–13.478]). This was the strongest predictor among multiple other dichotomized variables such as age, LV volumes, LVEF, and LV wall abnormality which were also significantly associated with occurrence of the primary outcome. Multivariate Cox regression analysis also yielded similar findings with ischemic burden of > 1.5 segments being the strongest predictor among the included variables after correction for covariates [17]. Kaplan-Meier analysis showed that patients with an ischemic burden of > 1.5 segments were significantly more likely to experience the primary and secondary outcome (p < 0.001). There was no significant difference between likelihood of occurrence of either the primary or secondary endpoints in patients with an ischemic burden < 1.5 segments versus patients without ischemia (normal stress perfusion CMR) [17]. The conclusion drawn from this study is that an ischemic burden of 2 or more segments on stress perfusion CMR is a very strong predictor of the adverse events described by the primary and secondary endpoints. Conversely, patients with zero or 1 ischemic segments can be safely deferred from revascularization.
Prognostic value of CMR compared to SPECT
Single-photon emission computed tomography (SPECT) has been a well-established technique for evaluating myocardial perfusion with good diagnostic accuracy for detection of CAD. Furthermore, multiple studies have shown that it offers incremental prognostic value for patients with known or suspected CAD [18]. Unfortunately, there is no data in the literature providing direct comparison between the prognostic value of SPECT and CMR myocardial perfusion imaging as independent techniques. There is however meaningful comparison between CMR and SPECT when each is viewed as a multiparametric examination (including stress and rest perfusion), as they are often performed in clinical practice. The CE-MARC study was a large prospective trial which served as a powerful source for direct comparison between CMR and SPECT [19]. A cohort of 628 patients with suspected angina prospectively underwent CMR, SPECT, and a coronary angiography (reference standard) within a period of 4 weeks and then followed for up to 5 years. The CMR examination included rest and stress (adenosine) perfusion, cine imaging, coronary MR angiography, and LGE. ECG-gated SPECT imaging provided rest and stress (adenosine) perfusion data, as well as ancillary findings such as regional wall motion, right ventricular uptake, and transient ischemic dilatation. Both the CMR and SPECT examinations were considered abnormal if any of their individual parameters were outside of normal limits [20]. As expected, primary analysis showed that both CMR and SPECT have a high diagnostic accuracy for CAD [20]. Additionally, by univariate analysis, abnormal findings by CMR and SPECT were both found to be independent predictors of MACE, with CMR demonstrating a significantly superior hazard ratio (2.77 vs 1.62) [20]. Furthermore, in a multivariable analysis, only CMR proved to be a significant predictor of MACE after adjustment for covariates such as cardiovascular risk factors, angiography results, and stratification by initial treatment [20]. Ultimately, these findings are evidence that CMR is a robust alternative to SPECT in predicting outcomes for patients with known or suspected CAD.
It should be highlighted that CMR offers several additional advantages over SPECT and PET. CMR provides superior spatial resolution compared to SPECT and PET. Second, CMR does not require patient exposure to radiation. Lastly, the CMR examination offers additional information such as evaluation of cardiac function and myocardial viability.
Stress perfusion CMR as a guide for revascularization in patients with stable CAD
There has been long-term controversy regarding the benefit provided by percutaneous coronary intervention (PCI) in treatment of patients with stable CAD. One of the established strategies for management of such patients with persistent symptoms or proven ischemia is invasive coronary angiography and the use of fractional flow reserve (FFR) to guide decision-making regarding revascularization [21••]. In brief, the findings of the FAME 2 Trial suggested that PCI therapy guided by fractional flow reserve (FFR) combined with optimal medical therapy (OPM) is associated with a superior clinical outcome compared to OPM therapy alone [22]. This superiority was manifested by a significantly reduced rate of urgent revascularization in patients treated with FFR-guided PCI and this ultimately led to a premature termination of the study [22]. The investigators of the MR-INFORM trial sought to compare an alternative strategy in which stress perfusion CMR is used to guide revascularization decision making as opposed to the FFR-guided strategy tested in the FAME 2 Trial [21••]. In this multicenter study, 918 patients with evidence of stable CAD were randomly assigned to either the CMR-based or FFR-based strategy. Revascularization was recommended for patients with at least 6% ischemia detected by stress perfusion in the CMR group, and FFR of 0.8 or less in the FFR-guided group [21••]. The primary endpoint was a composite of death, nonfatal MI, or target-vessel revascularization within 1 year. 40.5% of the patients in the CMR group met the criteria for recommended revascularization, compared to 45.9% of patients in the FFR-guided group. Significantly, less patients received revascularization therapy in the CMR group (35.7% versus 45.0%) [21••]. The primary endpoint occurred in 3.6% of the patients in the CMR-guided group versus in 3.7% in the FFR group [21••]. This difference was not deemed significant and met the noninferiority threshold (risk difference of 6%). Furthermore, there was no significant difference in patients free from angina after 12 months between the two groups. This is a significant study which establishes a noninvasive management strategy guided by stress perfusion CMR as noninferior to the invasive FFR-guided approach which had been previously evaluated in the FAME 2 Trial.
Conclusion
Stress perfusion CMR is an accurate noninvasive diagnostic test for patients with suspected CAD and provides strong prognostic value across different subpopulations and risk categories.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Torpy JM, Burke AE, Glass RM. JAMA patient page. Coronary heart disease risk factors. JAMA. 2009;302(7):2388.
Cassar A, Holmes DR Jr, Rihal CS, Gersh BJ. Chronic coronary artery disease: diagnosis and management. Mayo Clin Proc. 2009;84(12):1130–46.
Ford TJ, Corcoran D, Berry C. Stable coronary syndromes: pathophysiology, diagnostic advances and therapeutic need. Heart. 2018;104(4):284–92.
Grizzard JD, Judd RM, Kim RJ. Cardiovascular MRI in practice: a teaching file approach. London: Springer; 2008. xv, 299p. p.
Klem I, Heitner JF, Shah DJ, Sketch MH Jr, Behar V, Weinsaft J, et al. Improved detection of coronary artery disease by stress perfusion cardiovascular magnetic resonance with the use of delayed enhancement infarction imaging. J Am Coll Cardiol. 2006;47(8):1630–8.
Gerber BL, Raman SV, Nayak K, Epstein FH, Ferreira P, Axel L, et al. Myocardial first-pass perfusion cardiovascular magnetic resonance: history, theory, and current state of the art. J Cardiovasc Magn Reson. 2008;10:18.
Biglands JD, Ibraheem M, Magee DR, Radjenovic A, Plein S, Greenwood JP. Quantitative myocardial perfusion imaging versus visual analysis in diagnosing myocardial ischemia: A CE-MARC Substudy. JACC Cardiovasc Imaging. 2018;11(5):711–8.
Schwitter J, Wacker CM, van Rossum AC, Lombardi M, Al-Saadi N, Ahlstrom H, et al. MR-IMPACT: comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. Eur Heart J. 2008;29(4):480–9.
Nandalur KR, Dwamena BA, Choudhri AF, Nandalur MR, Carlos RC. Diagnostic performance of stress cardiac magnetic resonance imaging in the detection of coronary artery disease: a meta-analysis. J Am Coll Cardiol. 2007;50(14):1343–53.
•• Heitner JF, Kim RJ, Kim HW, Klem I, Shah DJ, Debs D, et al. Prognostic value of vasodilator stress cardiac magnetic resonance imaging: a multicenter study with 48000 patient-years of follow-up. JAMA Cardiol. 2019; A powerful multicenter study with over 9000 patients evaluating the prognostic value of stress perfusion CMR.
Gargiulo P, Dellegrottaglie S, Bruzzese D, Savarese G, Scala O, Ruggiero D, et al. The prognostic value of normal stress cardiac magnetic resonance in patients with known or suspected coronary artery disease: a meta-analysis. Circ Cardiovasc Imaging. 2013;6(4):574–82.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47.
Steel K, Broderick R, Gandla V, Larose E, Resnic F, Jerosch-Herold M, et al. Complementary prognostic values of stress myocardial perfusion and late gadolinium enhancement imaging by cardiac magnetic resonance in patients with known or suspected coronary artery disease. Circulation. 2009;120(14):1390–400.
Hartlage G, Janik M, Anadiotis A, Veledar E, Oshinski J, Kremastinos D, et al. Prognostic value of adenosine stress cardiovascular magnetic resonance and dobutamine stress echocardiography in patients with low-risk chest pain. Int J Cardiovasc Imaging. 2012;28(4):803–12.
Shah R, Heydari B, Coelho-Filho O, Murthy VL, Abbasi S, Feng JH, et al. Stress cardiac magnetic resonance imaging provides effective cardiac risk reclassification in patients with known or suspected stable coronary artery disease. Circulation. 2013;128(6):605–14.
Coelho-Filho OR, Seabra LF, Mongeon FP, Abdullah SM, Francis SA, Blankstein R, et al. Stress myocardial perfusion imaging by CMR provides strong prognostic value to cardiac events regardless of patient’s sex. JACC Cardiovasc Imaging. 2011;4(8):850–61.
Vincenti G, Masci PG, Monney P, Rutz T, Hugelshofer S, Gaxherri M, et al. Stress perfusion CMR in patients with known and suspected CAD: prognostic value and optimal ischemic threshold for revascularization. JACC Cardiovasc Imaging. 2017;10(5):526–37.
Cremer P, Hachamovitch R, Tamarappoo B. Clinical decision making with myocardial perfusion imaging in patients with known or suspected coronary artery disease. Semin Nucl Med. 2014;44(4):320–9.
Greenwood JP, Maredia N, Younger JF, Brown JM, Nixon J, Everett CC, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet. 2012;379(9814):453–60.
Greenwood JP, Herzog BA, Brown JM, Everett CC, Nixon J, Bijsterveld P, et al. Prognostic value of cardiovascular magnetic resonance and single-photon emission computed tomography in suspected coronary heart disease: long-term follow-up of a prospective, diagnostic accuracy cohort study. Ann Intern Med. 2016.
•• Nagel E, Greenwood JP, McCann GP, Bettencourt N, Shah AM, Hussain ST, et al. Magnetic resonance perfusion or fractional flow reserve in coronary disease. N Engl J Med. 2019;380(25):2418–28 A significant study which establishes a noninvasive management strategy guided by stress perfusion CMR as noninferior to the invasive FFR-guided approach.
De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367(11):991–1001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Filev, P.D., Stillman, A.E. Long-Term Prognostic Value of Stress Perfusion Cardiovascular Magnetic Resonance Imaging. Curr Treat Options Cardio Med 21, 51 (2019). https://doi.org/10.1007/s11936-019-0766-8
Published:
DOI: https://doi.org/10.1007/s11936-019-0766-8