Opinion statement
The increased number of patients with coronary artery disease (CAD) in developed countries is of great clinical relevance and involves a large burden of the healthcare system. The management of these patients is focused on relieving symptoms and improving clinical outcomes. Therefore the ideal test would provide the correct diagnosis and actionable information. To this aim, several non-invasive functional imaging modalities are usually used as gatekeeper to invasive coronary angiography (ICA), but their diagnostic yield remains low with limited accuracy when compared to obstructive CAD at the time of ICA or invasive fractional flow reserve (FFR). Invasive FFR is considered the gold standard for the evaluation of functionally relevant CAD. Therefore, an urgent need for non-invasive techniques that evaluate both the functional and morphological severity of CAD is growing. Coronary computed tomography angiography (CCTA) has emerged as a unique non-invasive technique providing coronary artery anatomic imaging. More recently, the evaluation of FFR with CCTA (FFRCT) has demonstrated high diagnostic performance compared to invasive FFR. Additionally, stress myocardial computed tomography perfusion (CTP) represents a novel tool for the diagnosis of ischemia with high diagnostic accuracy. Compared to nuclear imaging and cardiac magnetic resonance imaging, both FFRCT and stress-CTP, allow us to integrate the anatomical evaluation of coronary arteries with the functional relevance of coronary artery lesions having the potential to revolutionize the diagnostic paradigm of suspected CAD. FFRCT and stress-CTP could be assimilated in diagnostic pathways of patients with stable CAD and will likely result in a decrease of invasive diagnostic procedures and costs. The current review evaluates the technical aspects and clinical experience of FFRCT and stress-CTP in the evaluation of functionally relevant CAD discussing the strengths and weaknesses of each approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is a major cause of morbidity and mortality and consumes a large proportion of health care spending. The related cost of invasive coronary angiography (ICA) and revascularization has resulted in a great interest on how to select patients with known or suspected CAD who will receive the greatest benefit from these invasive procedures. For this reason, different diagnostic strategies based on the pre-test likelihood of CAD as gatekeeper for ICA are usually employed suggesting a conservative observational approach in the case of patients with low risk, non-invasive stress testing to detect ischemic burden in intermediate risk patients, and direct referral for ICA in high risk patients for CAD.
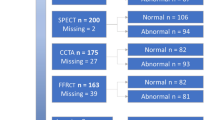
Myocardial ischemia detection has played a pivotal role in the identification of symptomatic intermediate risk patients who could receive benefit from invasive evaluation [1–4]. Myocardial ischemia can manifest with symptoms of shortness of breath or chest pain and even myocardial infarction and cardiac death. Although the role of coronary revascularization in acute ST and non-ST-segment elevation myocardial infarction is crucial for beneficial outcomes, in patients with stable CAD, the widespread use of revascularization is debated [5–7]. Therefore, the choice between a conservative or invasive approach in stable CAD is oftentimes challenging and mainly based on the severity of the hemodynamic effects associated with atherosclerotic lesions. To this regard, the combination of an anatomical evaluation of CAD with ICA bridged with the functional relevance of specific coronary artery lesions by invasive fractional flow reserve (FFR) is now considered the gold standard test in therapeutic decision making. FFR, the ratio of maximal hyperemic blood flow of a stenosis divided by normal hyperemic blood flow in the absence of stenosis, determines the functional significance of CAD in a lesion-specific manner. FFR-guided revascularization has been shown to improve outcomes and reduce health care costs [8••, 9••]. Although, both ICA and FFR provide combined anatomical and functional information regarding the severity of CAD, they are invasive and expensive techniques employing the use of ionizing radiation. With this understanding, there are several non-invasive modalities used in clinical practice for the functional assessment of CAD including exercise-ECG, stress echocardiography (Echo) [10], single-photon emission computed tomography (SPECT), or advanced non-invasive techniques such as stress cardiac magnetic resonance (CMR) and positron emission tomography (PET) [11]. However, recent literature has reported the low diagnostic yield of obstructive CAD at the time of ICA after undergoing standard-of-care non-invasive functional stress testing [12••, 13].
The role of coronary computed tomography angiography (CCTA) in the assessment of functionally significant CAD is debated as there is discordance between anatomic severity of disease and hemodynamic significance [14, 15].
In the EVINCI trial, Neglia et al. [16••] showed that CCTA is more accurate as compared to functional imaging in patients with suspected CAD. However, whether the superior diagnostic performance translates into improved outcomes is still issue of concern. Large registries note that early detection of sub-clinical CAD is correlated with worst outcomes [17••, 18]. Recently, data from the SCOT-HEART trial concluded that a CCTA diagnostic strategy alters therapeutic interventions which translated into reduced hard clinical endpoints such as myocardial infarction [19••]. On the other side, Douglas et al. [20••] showed that CCTA, as compared to a functional stress testing strategy was associated with a lower rate of non-obstructive CAD at ICA evaluation (3.4 vs. 4.3 %, p = 0.02) with a trend of higher number of patients referred to catheterization (12.2 vs. 8.0 %) and revascularization procedures (6.2 vs. 3.2 %) with equivalent clinical outcomes. For this reason, an urgent need for non-invasive techniques that evaluate both the functional and morphological severity of CAD is growing. CCTA has emerged as unique modality providing coronary artery anatomy and, more recently, due to the introduction of stress myocardial computed tomography perfusion (stress-CTP) and non-invasive fractional flow reserve (FFRCT), functional relevance of CAD in a single scan. The current review evaluates the technical aspects and clinical experience of FFRCT and stress-CTP in the evaluation of functionally relevant CAD discussing the strength and weakness of each approach.
Fractional flow reserve CCTA derived (FFRCT)
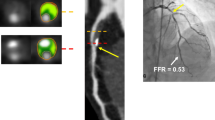
Studies of anatomical imaging, whether it be quantitative coronary angiography, CCTA or intravascular ultrasound, have consistently demonstrated an unreliable relationship between anatomic measures of stenosis and lesion-specific ischemia [15]. The ability to evaluate the functional significance of stenosis using FFR during ICA improves outcomes and reduces health care cost [8••, 9••]. However, considering the invasiveness of ICA, a new non-invasive approach to calculate total vessel FFR based on CCTA has been developed [21]. FFRCT applies computational fluid dynamics (CFD) to calculate FFR values in all epicardial coronary arteries without the need for additional imaging, medications, or change in imaging protocol [22]. FFRCT is based on three steps (Fig. 1): (1) reconstruction of a 3D model that includes the aortic root and coronaries, (2) identification of inflow and outflow boundary conditions that mimic coronary physiology during maximal hyperemia, and (3) performing a numerical solution of the laws governing fluid dynamics [21]. The color-coded 3D model is obtained from a standard CCTA acquisition in accordance with Society of Cardiovascular Computed Tomography guidelines [22].
FFRCT analysis. From a standard CCTA (Panel a), a quantitative 3-dimensional anatomic model of coronary arteries is generated. b A physiological model of the coronary microcirculation is derived from patient-specific characteristics and physical laws of fluid dynamics is applied (c) to calculate FFRCT for each point in the coronary tree (d). CCTA coronary computed tomography angiography, FFRCT: fractional flow reserve CCTA derived, LAD left anterior descending coronary artery, LCx left circumflex coronary artery, RCA right coronary artery. Modified by Pontone et al. [61••].
FFRCT has been extensively validated against invasive FFR (Table 1). In the DeFACTO study, diagnostic accuracy of FFRCT + CCTA was superior to CCTA alone compared with invasive FFR (73 % vs. 64 %, respectively) [23]. In addition, FFRCT demonstrated greater discrimination of lesion-specific ischemia compared to CCTA (area under the curve (AUC) of 0.81 vs 0.68) [23]. Despite the significant improvement in diagnostic accuracy of CCTA when integrated with FFRCT, a partial discrepancy between invasive FFR and FFRCT in the DeFACTO study was observed. This result could be attributed to nitroglycerin and beta-blockers not being mandatory in the protocol translating into a degradation in image quality [24]. In a sub-study of DeFACTO, for individuals with intermediate coronary stenosis, FFRCT had a negative predictive value of 90 %, allowing the clinician to rule-out intermediate lesions that cause ischemia [25]. A limitation of DISCOVER-FLOW was that it was powered to evaluate the diagnostic accuracy in a per-vessel model rather than a per-patient model. The latter point was evaluated in the DE-FACTO trial [26] where, in a larger study population, FFRCT showed a diagnostic accuracy, sensitivity, specificity, positive predictive value, and negative predictive value of 73, 90, 54, 67, and 84 %, respectively, improving the AUC from 0.68 to 0.81 when compared with CCTA alone. More recently, the NXT trial [27••] demonstrated per patient sensitivity and specificity of 86 and 79 %, respectively, with an even better AUC of 0.9 as compared to invasive FFR. In contrast to the two previous studies, in the NXT trial, a new generation of FFRCT software was employed, nitrates were administered in 99 % versus only 75 % of DEFACTO study population, and an intermediate risk population was included rather than patients with a higher risk as in DEFACTO and DISCOVER-FLOW. Importantly, in patients with intermediate stenosis [27••] and in patients with high Agatston score [28] the diagnostic performance of FFRCT remained unchanged. Of note, FFRCT was not-evaluable in 13 % of the NXT-trial patients due to poor image quality [27••].
In a real-world feasibility study, Nørgaard et al. [29] proposed the “Aarhus” algorithm in which patients with FFRCT lower than 0.75 were referred to ICA, patients with FFRCT ranging between 0.75 to 0.80 were followed clinically for symptom evolution and patients with FFRCT > 0.80 were deferred from ICA. In the same study, a conclusive FFRCT result was obtained in 98 % of patients [29]. One of the great advantages of FFRCT is that it does not increase radiation dose as it is quantified from standard CCTA datasets [30]. Several CCTA imaging protocol strategies have been described in the literature to decrease radiation dose while maintaining good image quality. Interestingly, Bilbey et al. [30] calculated the differential radiation dose simulating various common diagnostic pathways based on the first non-invasive diagnostic test performed. The population was divided in four groups: dobutamine echo, SPECT, CCTA, and CCTA+ FFRCT. Radiation dose exposure for CTA + FFRCT was lower than for SPECT, and the CTA + FFRCT pathway resulted in the lowest projected death or myocardial infarction rate at 1 year (2.33 %). Although the radiation dose was lowest in the pathway that used dobutamine echo, the dobutamine stress pathway had the highest 1-year event rate [30].
The ability to identify a specific plaque that causes ischemia utilizing FFRCT is proving to be cost-effective. The PLATFORM trial (Prospective LongitudinAl Trial of FFRCT: Outcome and Resource IMpacts) compared the rate of ICA documenting non-obstructive CAD, clinical outcomes, quality of life, and resource utilization following standard practice versus incorporating FFRCT [31]. The PLATFORM investigators demonstrated that in patients with planned ICA, the approach using FFRCT safely canceled 61 % of ICA, reduced ICAs with no obstructive CAD by a dramatic 83 %, improved quality of life for patients, and reduced healthcare cost [32••, 33]. Finally, exciting data from the EMERALD study was recently presented using CFD-based non-invasive hemodynamics for the prediction of acute coronary syndromes. Culprit lesions had significantly lower FFRCT and higher delta FFRCT (across lesions), axial plaque and wall shear stress compared to non-culprit lesions. The ability of these non-invasive hemodynamic parameters to better identify culprit lesions causing acute coronary syndrome as compared to anatomic stenosis severity or high risk plaque features could help fill the ambitious gap to diagnose the vulnerable lesion and patient.
Stress myocardial computed tomography perfusion (Stress-CTP)
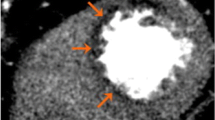
Despite studies in the field of stress-CTP starting a few decades ago, the clinical use of this technique was slow to emerge for several technical limitations such as limited temporal, spatial, and contrast resolution, and the z-axis coverage. During a stress-CTP, the contrast agent reaches the myocardial wall and attenuates the X-ray based on its concentration. In this way, the area with a perfusion defect is detectable as a region with hypo-attenuation. However, the highest concentration of iodine in the myocardium and its washout is a very rapid phenomenon. Therefore, a high temporal resolution is mandatory. High temporal resolution scans need to be matched with a very fast scan time which can be reached by two strategies to improve the scan time: (1) a higher craniocaudal coverage by increasing the number of slices or (2) a higher pitch scan or a combination of the two. The development of wide area detector CCTA with the introduction of 320-detector row systems has enabled whole heart coverage in one beat. Similarly, the scan time can be reduced by increasing the pitch. In one type of techniqueknown as “Flash CT,” a complete image acquisition within one cardiac cycle is achievable with the X-ray tube and detector rotating around the patient without overlap and with a very short scan time. Finally, beyond temporal resolution, another challenge in stress-CTP is to improve the contrast resolution in the myocardiumas the difference in contrast attenuation between normal and hypoperfused myocardial regions ranges in the order of 50 HU. To this regard, beam hardening artifacts related to contrast agent concentration in the left ventricle can mimic a false positive perfusion defect. Recently, dual energy computed tomography (DECT) has been introduced to overcome this limitation. This technique simultaneously acquires 2 sets of projections using 2 different X-ray energy spectra. In this way, DECT is more effective for correcting beam hardening artifacts due to the ability to reconstruct monochromatic CCTA images.
Stress-CTP can be acquired using two different approaches: static or dynamic protocol acquisitions [34]. Moreover, static stress-CTP can be further acquired using single or DECT [34]. Sample protocols are briefly summarized below and illustrated in Fig. 2.
Stress-CTP protocol. Patient is asked to refrain from smoking and caffeine for 24 h and to fast for 6 h before the scan. The patient is continuously monitored with blood pressure measurements and ECG. In patients with a resting HR >65 bpm before the scan, β-blockers are administered and all patients receive sublingual nitrates. Then, a single dataset at rest is acquired. After at least 15 min, vasodilatation is induced with i.v. adenosine injection (0.14 mg/Kg/min over 4 min). At the end of the third minute of adenosine infusion, a single (static CTP) or multiple (dynamic CTP) pass enhancements are acquired. ECG electrocardiogram, CTP , HR heart rate. Modified by Pontone et al. [61••].
-
(1)
Single energy static stress-CTP acquisition: Single energy static stress-CTP allows a qualitative evaluation of a single snapshot of the myocardium. Images are acquired covering the entire left ventricle at the time of the maximum peak of iodine based contrast agent in the coronaries [35]. The acquisition can be reached at rest and stress condition, and the images obtained at rest can be useful for coronary artery imaging as well.
-
(2)
Dual energy static stress-CTP acquisition: In the DECT protocol, different voltages can be obtained using two detectors that operate separately with high (140 kV) and low energy (80–100 kV) or with a single detector that rapidly switches from low to high energies (80-140 kV) [36, 37]. Merging the first-pass images of low and high energies is possible to visualize a colored map. The hypoattenuated areas are suggestive of perfusion defects [34]. Similar to static single energy protocols, static dual energy techniques are influenced by appropriate timing of scan acquisition as only a single snapshot is acquired [34].
-
(3)
Dynamic stress-CTP: Dynamic stress-CTP protocols are based on several computed tomography dataset acquisitions that sample the attenuation of the whole myocardium during first pass perfusion. Considering high temporal resolution required for this protocol, two different techniques have been developed. The first technique is based on wide coverage scanners to acquire the whole cardiac muscle in one single rotation without movement of the table. Alternatively, for scanners with high temporal resolution but lower coverage, the shuttle mode acquisition can be performed [38–40]. The real advantage of dynamic stress-CTP as compared to the other acquisition protocols is the ability to provide quantitative evaluation of perfusion by the estimation of myocardial blood flow (MBF) [34].
Regardless of the acquisition protocol used, stress-CTP requires the administration of pharmaceutical stressors [41] and double exposure to contrast agents and X-ray. A comparison of FFRCT versus stress-CTP is summarized in Table 2.
The diagnostic accuracy of stress-CTP has been studied by using several reference techniques such as SPECT, invasive FFR, ICA and stress CMR.
In a large cohort of patients from the CORE320 study, a combined approach of CCTA plus static single-energy stress-CTP reported high diagnostic accuracy with an AUC of 0.87 in the identification of flow limiting disease defined as a ≥50 % coronary stenosis by ICA causing a perfusion defect by SPECT [42••].. Similarly, Osawa et al., evaluated the performance of static single-energy stress-CTP compared to CCTA alone and demonstrated a significantly higher AUC of 0.89 versus 0.84 for the detection of CADThe negative predictive value of CCTA alone versus stress CTP increased from 63 to 96 %, respectively [43]. Several other studies have noted the high diagnostic accuracy of static single energy stress-CTP to detect functionally significant CAD [44–46].
There is less data evaluating the diagnostic performance of static dual energy stress-CTP [47–53]. Ko et al. showed improved diagnostic accuracy with CCTA + stress CTP compared to CCTA alone with an AUC of 0.89 versus 0.79, respectively [49].. Furthermore, in high-risk patients, the combined approach of CCTA and stress-CTP acquired in dual energy mode reported diagnostic performance which was superior to SPECT [50]. With the added value of providing quantitative perfusion from dynamic stress-CTP, a MBF cut-off value of 75 ml/100 ml/min has been reported to identify hemodynamically significant CAD [54, 55].. Quantitative MBF on stress-CTPreported a diagnostic accuracy of 82 % when compared to invasive FFR for the detection of hemodynamically significant stenosis [56].
Despite its diagnostic robustness, concerns remain regarding the lack of prognostic data of stress-CTP [57] and the non-negligible radiation exposure. Regarding the latter point, it is well known that in static acquisition the radiation dose is lower compared to dynamic acquisition [34] with a mean radiation dose, in a liberal scenario, of 12 mSv that is quite comparable, if not lower than the standard effective radiation dose of nuclear testing [42••, 58].
To the best of our knowledge, only one article in the literature analyzed the economic impact of stress-CTP as compared to standard nuclear stress imaging. Meyer et al. [59] demonstrated that a diagnostic strategy of stress-CTP had gains in quality-adjusted-life-years while lowering costs compared to SPECT.
Conclusion
Cardiac CT provides us with a unique non-invasive imaging modality offering fast diagnostic testing that is cost efficient and accurate at providing both anatomic and functional information. Although both FFRCT and stress-CTP represent two excellent techniques for non-invasive assessment of myocardial ischemia, it is important to consider their differences includingprognostic value, radiation dose, and cost-effectiveness. Ongoing studies such as DECIDE gold (ClinicalTrials.gov identifier NCT02178904) will analyze the diagnostic accuracy of dual energy stress-CTP as compared to FFR [60], while in CREDENCE trial (ClinicalTrials.gov identifier NCT02173275) a comparison of FFRCT versus other perfusion imaging modalities such as SPECT and stress-CMR will be studied. Finally, in the PERFECTION study, an intra-patient head to head comparison of per-vessel diagnostic accuracy of FFRCT versus stress-CTP will be performed [61••].
We have entered a new era in our diagnostic pathway of suspected CAD. Both FFRCT and stress-CTP could be very disruptive to standard practice diagnosis and management of CAD. Further studies are needed to recognize their full value and appreciate their extraordinary potential.
Abbreviations
- AUC:
-
Area under the curve
- CAD:
-
Coronary artery disease
- CCTA:
-
Coronary computed tomography angiography
- CFD:
-
Computational fluid dynamic
- CMR:
-
Cardiac magnetic resonance
- CTP:
-
Computed tomography perfusion
- DECT:
-
Dual energy computed tomography
- ECG:
-
Electrocardiogram
- Echo:
-
Echocardiography
- FFR:
-
Fractional flow reserve
- ICA:
-
Invasive coronary angiography
- MBF:
-
Myocardial blood flow
- PCI:
-
Percutaneous coronary intervention
- PET:
-
Positron emission tomography
- SPECT:
-
Single photon emission computed tomography
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Taylor J. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2506–7.
Crossman DC. The pathophysiology of myocardial ischaemia. Heart. 2004;90:576–80.
Tesche C, De Cecco CN, Caruso D, Baumann S, Renker M, Mangold S, et al. Coronary CT angiography derived morphological and functional quantitative plaque markers correlated with invasive fractional flow reserve for detecting hemodynamically significant stenosis. J Cardiovasc Comput Tomogr. 2016. doi:10.1016/j.jcct.2016.03.002.
Pontone G, Andreini D, Baggiano A, Bertella E, Mushtaq S, Conte E, et al. Functional relevance of coronary artery disease by cardiac magnetic resonance and cardiac computed tomography: myocardial perfusion and fractional flow reserve. Biomed Res Int. 2015;2015:297696.
Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–16.
Sedlis SP, Hartigan PM, Teo KK, Maron DJ, Spertus JA, Mancini GB, et al. Effect of PCI on long-term survival in patients with stable ischemic heart disease. N Engl J Med. 2015;373:1937–46.
Choi AD, Joly JM, Chen MY, Weigold WG. Physiologic evaluation of ischemia using cardiac CT: current status of CT myocardial perfusion and CT fractional flow reserve. J Cardiovasc Comput Tomogr. 2014;8:272–81.
••Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’ t Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–24. A invasive FFR strategy is more effective as compared to a invasive angiographic strategy.
••De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991–1001. The coronary revascularization in patients with invasive FFR < 0.8 is more effective than medical therapy alone.
Banerjee A, Newman DR, Van den Bruel A, Heneghan C. Diagnostic accuracy of exercise stress testing for coronary artery disease: a systematic review and meta-analysis of prospective studies. Int J Clin Pract. 2012;66:477–92.
Yang Z, Zheng H, Zhou T, Yang LF, Hu XF, Peng ZH, et al. Diagnostic performance of myocardial perfusion imaging with SPECT, CT and MR compared to fractional flow reserve as reference standard. Int J Cardiol. 2015;190:103–5.
••Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362:886–95. The diagnostic yeld of invasive coronary angiography is low despite the use of non-invasive diagnostic test as gatekeeper.
Patel MR, Dai D, Hernandez AF, Douglas PS, Messenger J, Garratt KN, et al. Prevalence and predictors of nonobstructive coronary artery disease identified with coronary angiography in contemporary clinical practice. Am Heart J. 2014;167:846–52.
Gonzalez JA, Lipinski MJ, Flors L, Shaw PW, Kramer CM, Salerno M. Meta-analysis of diagnostic performance of coronary computed tomography angiography, computed tomography perfusion, and computed tomography-fractional flow reserve in functional myocardial ischemia assessment versus invasive fractional flow reserve. Am J Cardiol. 2015;116:1469–78.
Min JK, Taylor CA, Achenbach S, Koo BK, Leipsic J, Norgaard BL, et al. Noninvasive fractional flow reserve derived from coronary CT angiography: clinical data and scientific principles. JACC Cardiovasc Imaging. 2015;8:1209–22.
••Neglia D, Rovai D, Caselli C, Pietila M, Teresinska A, Aguade-Bruix S, et al. Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging. 2015;8:e002179. In a low to intermediate risk population computed tomography coronary angiuography showed a higher accuracy as compared to other imaging modalities.
••Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah M, Budoff MJ, et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol. 2011;58:849–60. The coronary computed tomography angiography findings provided prognostic stratification of patients.
Cho I, Chang HJ BOH, Shin S, Sung JM, Lin FY, et al. Incremental prognostic utility of coronary CT angiography for asymptomatic patients based upon extent and severity of coronary artery calcium: results from the COronary CT Angiography EvaluatioN For Clinical Outcomes InteRnational Multicenter (CONFIRM) study. Eur Heart J. 2015;36:501–8.
••investigators S-H. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet. 2015;385:2383–91. The coronary computed tomography angiography in addition of standard of care positively reclassify patients with suspected coronary artery disease.
••Douglas PS, Hoffmann U, Lee KL, Mark DB, Al-Khalidi HR, Anstrom K, et al. PROspective Multicenter Imaging Study for Evaluation of chest pain: rationale and design of the PROMISE trial. Am Heart J. 2014;167:796–803. A anatomical strategy with coronary computed tomography angiography is associated with higher invasive procedures and revascularization with similaroutcomes when compared to a functional strategy.
Zarins CK, Taylor CA, Min JK. Computed fractional flow reserve (FFTCT) derived from coronary CT angiography. J Cardiovasc Transl Res. 2013;6:708–14.
Hulten E, Ahmadi A, Blankstein R. CT assessment of myocardial perfusion and fractional flow reserve. Prog Cardiovasc Dis. 2015;57:623–31.
Min JK, Leipsic J, Pencina MJ, Berman DS, Koo BK, van Mieghem C, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 2012;308:1237–45.
Norgaard BL, Leipsic J, Koo BK, Zarins CK, Jensen JM, Sand NP, et al. Coronary computed tomography angiography derived fractional flow reserve and plaque stress. Curr Cardiovasc Imaging Rep. 2016;9:2.
Nakazato R, Park HB, Berman DS, Gransar H, Koo BK, Erglis A, et al. Noninvasive fractional flow reserve derived from computed tomography angiography for coronary lesions of intermediate stenosis severity: results from the DeFACTO study. Circ Cardiovasc Imaging. 2013;6:881–9.
Koo BK, Erglis A, Doh JH, Daniels DV, Jegere S, Kim HS, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol. 2011;58:1989–97.
••Norgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol. 2014;63:1145–55. Fractional flow reserve measured by coronary computed tomography angiography is accurate when compared to invasive fractional flow reserve.
Norgaard BL, Gaur S, Leipsic J, Ito H, Miyoshi T, Park SJ, et al. Influence of coronary calcification on the diagnostic performance of CT angiography derived FFR in coronary artery disease: a substudy of the NXT trial. JACC Cardiovasc Imaging. 2015;8:1045–55.
Norgaard BL, Hjort J, Gaur S, Hansson N, Botker HE, Leipsic J, et al. Clinical use of coronary CTA-derived FFR for decision-making in stable CAD. JACC Cardiovasc Imaging. 2016;S1936-878X(16):30040–7.
Bilbey NB, P Naoum C, Dey Arepalli C, Norgaard BL, Leipsic J. Potential impact of clinical use of non-invasive FFRCT on radiation dose exposure and downstream clinical event rate. J Clin Imaging. 2016;40:1055–60.
Pontone G, Patel MR, Hlatky MA, Chiswell K, Andreini D, Norgaard BL, et al. Rationale and design of the Prospective LongitudinAl Trial of FFRCT: Outcome and Resource IMpacts study. Am Heart J. 2015;170:438–46.
••Douglas PS, Pontone G, Hlatky MA, Patel MR, Norgaard BL, Byrne RA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J. 2015;36:3359–67.
Hlatky MA, De Bruyne B, Pontone G, Patel MR, Norgaard BL, Byrne RA, et al. Quality-of-life and economic outcomes of assessing fractional flow reserve with computed tomography angiography: PLATFORM. J Am Coll Cardiol. 2015;66:2315–23. A strategy based on fractional flow reserve derived by coronary computed tomography angiography is able to reduce the number of invasuifve coronary angiography and rerlated cost.
Varga-Szemes A, Meinel FG, De Cecco CN, Fuller SR, Bayer 2nd RR, Schoepf UJ. CT myocardial perfusion imaging. AJR Am J Roentgenol. 2015;204:487–97.
Bischoff B, Bamberg F, Marcus R, Schwarz F, Becker HC, Becker A, et al. Optimal timing for first-pass stress CT myocardial perfusion imaging. Int J Cardiovasc Imaging. 2013;29:435–42.
Matsumoto K, Jinzaki M, Tanami Y, Ueno A, Yamada M, Kuribayashi S. Virtual monochromatic spectral imaging with fast kilovoltage switching: improved image quality as compared with that obtained with conventional 120-kVp CT. Radiology. 2011;259:257–62.
So A, Hsieh J, Imai Y, Narayanan S, Kramer J, Procknow K, et al. Prospectively ECG-triggered rapid kV-switching dual-energy CT for quantitative imaging of myocardial perfusion. JACC Cardiovasc Imaging. 2012;5:829–36.
Hsiao EM, Rybicki FJ, Steigner M. CT coronary angiography: 256-slice and 320-detector row scanners. Curr Cardiol Rep. 2010;12:68–75.
Bastarrika G, Ramos-Duran L, Rosenblum MA, Kang DK, Rowe GW, Schoepf UJ. Adenosine-stress dynamic myocardial CT perfusion imaging: initial clinical experience. Invest Radiol. 2010;45:306–13.
Cannao PM, Schoepf UJ, Muscogiuri G, Wichmann JL, Fuller SR, Secchi F, et al. Technical prerequisites and imaging protocols for dynamic and dual energy myocardial perfusion imaging. Eur J Radiol. 2015;84:2401–10.
Kim SM, Kim YN, Choe YH. Adenosine-stress dynamic myocardial perfusion imaging using 128-slice dual-source CT: optimization of the CT protocol to reduce the radiation dose. Int J Cardiovasc Imaging. 2013;29:875–84.
••Rochitte CE, George RT, Chen MY, Arbab-Zadeh A, Dewey M, Miller JM, et al. Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J. 2014;35:1120–30. The stress computed tomography perfusion showed a higher diagnostic accuracy when compared to the combination of invasive coronary angiography and single photon emission computed tomography.
Osawa K, Miyoshi T, Koyama Y, Hashimoto K, Sato S, Nakamura K, et al. Additional diagnostic value of first-pass myocardial perfusion imaging without stress when combined with 64-row detector coronary CT angiography in patients with coronary artery disease. Heart. 2014;100:1008–15.
George RT, Arbab-Zadeh A, Miller JM, Vavere AL, Bengel FM, Lardo AC, et al. Computed tomography myocardial perfusion imaging with 320-row detector computed tomography accurately detects myocardial ischemia in patients with obstructive coronary artery disease. Circ Cardiovasc Imaging. 2012;5:333–40.
Ko BS, Cameron JD, Meredith IT, Leung M, Antonis PR, Nasis A, et al. Computed tomography stress myocardial perfusion imaging in patients considered for revascularization: a comparison with fractional flow reserve. Eur Heart J. 2012;33:67–77.
Feuchtner G, Goetti R, Plass A, Wieser M, Scheffel H, Wyss C, et al. Adenosine stress high-pitch 128-slice dual-source myocardial computed tomography perfusion for imaging of reversible myocardial ischemia: comparison with magnetic resonance imaging. Circ Cardiovasc Imaging. 2011;4:540–9.
Ruzsics B, Schwarz F, Schoepf UJ, Lee YS, Bastarrika G, Chiaramida SA, et al. Comparison of dual-energy computed tomography of the heart with single photon emission computed tomography for assessment of coronary artery stenosis and of the myocardial blood supply. Am J Cardiol. 2009;104:318–26.
Wang R, Yu W, Wang Y, He Y, Yang L, Bi T, et al. Incremental value of dual-energy CT to coronary CT angiography for the detection of significant coronary stenosis: comparison with quantitative coronary angiography and single photon emission computed tomography. Int J Cardiovasc Imaging. 2011;27:647–56.
Ko SM, Choi JW, Hwang HK, Song MG, Shin JK, Chee HK. Diagnostic performance of combined noninvasive anatomic and functional assessment with dual-source CT and adenosine-induced stress dual-energy CT for detection of significant coronary stenosis. AJR Am J Roentgenol. 2012;198:512–20.
De Cecco CN, Harris BS, Schoepf UJ, Silverman JR, McWhite CB, Krazinski AW, et al. Incremental value of pharmacological stress cardiac dual-energy CT over coronary CT angiography alone for the assessment of coronary artery disease in a high-risk population. AJR Am J Roentgenol. 2014;203:W70–7.
Wang Y, Qin L, Shi X, Zeng Y, Jing H, Schoepf UJ, et al. Adenosine-stress dynamic myocardial perfusion imaging with second-generation dual-source CT: comparison with conventional catheter coronary angiography and SPECT nuclear myocardial perfusion imaging. AJR Am J Roentgenol. 2012;198:521–9.
Bamberg F, Marcus RP, Becker A, Hildebrandt K, Bauner K, Schwarz F, et al. Dynamic myocardial CT perfusion imaging for evaluation of myocardial ischemia as determined by MR imaging. JACC Cardiovasc Imaging. 2014;7:267–77.
Wichmann JL, Meinel FG, Schoepf UJ, Lo GG, Choe YH, Wang Y, et al. Absolute versus relative myocardial blood flow by dynamic CT myocardial perfusion imaging in patients with anatomic coronary artery disease. AJR Am J Roentgenol. 2015;205:W67–72.
Bamberg F, Becker A, Schwarz F, Marcus RP, Greif M, von Ziegler F, et al. Detection of hemodynamically significant coronary artery stenosis: incremental diagnostic value of dynamic CT-based myocardial perfusion imaging. Radiology. 2011;260:689–98.
Rossi A, Dharampal A, Wragg A, Davies LC, van Geuns RJ, Anagnostopoulos C, et al. Diagnostic performance of hyperaemic myocardial blood flow index obtained by dynamic computed tomography: does it predict functionally significant coronary lesions? Eur Heart J Cardiovasc Imaging. 2014;15:85–94.
Greif M, von Ziegler F, Bamberg F, Tittus J, Schwarz F, D’Anastasi M, et al. CT stress perfusion imaging for detection of haemodynamically relevant coronary stenosis as defined by FFR. Heart. 2013;99:1004–11.
Vliegenthart R, De Cecco CN, Wichmann JL, Meinel FG, Pelgrim GJ, Tesche C, et al. Dynamic CT myocardial perfusion imaging identifies early perfusion abnormalities in diabetes and hypertension: insights from a multicenter registry. J Cardiovasc Comput Tomogr. 2016;10:301–8.
Okada DR, Ghoshhajra BB, Blankstein R, Rocha-Filho JA, Shturman LD, Rogers IS, et al. Direct comparison of rest and adenosine stress myocardial perfusion CT with rest and stress SPECT. J Nucl Cardiol. 2010;17:27–37.
Meyer M, Nance Jr JW, Schoepf UJ, Moscariello A, Weininger M, Rowe GW, et al. Cost-effectiveness of substituting dual-energy CT for SPECT in the assessment of myocardial perfusion for the workup of coronary artery disease. Eur J Radiol. 2012;81:3719–25.
Truong QA, Knaapen P, Pontone G, Andreini D, Leipsic J, Carrascosa P, et al. Rationale and design of the dual-energy computed tomography for ischemia determination compared to “gold standard” non-invasive and invasive techniques (DECIDE-Gold): A multicenter international efficacy diagnostic study of rest-stress dual-energy computed tomography angiography with perfusion. J Nucl Cardiol. 2015;22:1031–40.
••Pontone G, Andreini D, Guaricci AI, Guglielmo M, Mushtaq S, Baggiano A, et al. Rationale and design of the PERFECTION (comparison between stress cardiac computed tomography PERfusion versus Fractional flow rEserve measured by Computed Tomography angiography In the evaluation of suspected cOroNary artery disease) prospective study. J Cardiovasc Comput Tomogr. 2016;10:330–4. This aim of this study is to have a intra-patient head to head comparisioon between fractional flow reserve derived by computed tomography versus stress myocardial computed tomography perfusion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Imaging
Gianluca Pontone MD, PhD, FESC, FSCCT and Giuseppe Muscogiuri MD contributed equally to this work.
Rights and permissions
About this article
Cite this article
Pontone, G., Muscogiuri, G., Andreini, D. et al. The New Frontier of Cardiac Computed Tomography Angiography: Fractional Flow Reserve and Stress Myocardial Perfusion. Curr Treat Options Cardio Med 18, 74 (2016). https://doi.org/10.1007/s11936-016-0493-3
Published:
DOI: https://doi.org/10.1007/s11936-016-0493-3