Abstract
Purpose of Review
Despite effective available treatments, gout management is often unsuccessful in getting patients to target serum urate goal and in managing flares in the setting of comorbidities. Studies addressing future treatment options for short- and long-term management are reviewed.
Recent Findings
URAT-1 blocking agents have been helpful but have had limitations related to effects on renal function, lack of efficacy with renal impairment, and potential to increase renal stones. Dotinurad may function in the setting of decreased renal function. Arhalofenate has anti-URAT-1 activity and may also blunt gout flares. A new xanthine oxidase inhibitor (XOI), tigulixostat, is under study. New uricase treatments manufactured in combination with agents that can reduce immunogenicity may make uricase treatment simpler. A unique strategy of inhibiting gut uricase may offer the benefits of avoiding systemic absorption. For gout flares, IL-1β inhibitor studies in progress include different dosing schedules. Dapansutrile, an oral agent under investigation, inhibits activation of the NLRP3 inflammasome and may be an effective anti-inflammatory.
Summary
New treatments for gout that are under study may work in the setting of comorbidities, simplify management, utilize new mechanisms, or have reduced side effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
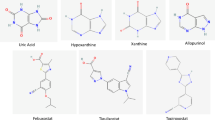
Although present treatments for gout are effective, there are many unmet needs remaining, for which the gout pipeline is expanding. The ever-growing list of associated comorbidities with gout (e.g., renal disease [1], hypertension [2], cardiovascular disease [3], type 2 diabetes mellitus [4], and venous thromboembolism [5]) requires an armamentarium that can avoid exacerbating these conditions. The remaining areas of concern include reducing the costs of care, offering more oral options, and approaching gout treatment via new mechanisms. It is also prudent to develop approaches that may limit the number of dose titrations presently required for a treat-to-target strategy with the use of allopurinol and febuxostat [10, 11].
Concerning uricosuric agents, the prevention of renal stone formation remains a concern. With uricase agents, such as pegloticase, recent FDA approval permits the co-administration of methotrexate to reduce immunogenicity. However, new strategies that can combine the immunosuppressive agent with the uricase agent may simplify management.
The pipeline of medications that may rectify shortcomings in gout treatment includes additional xanthine oxidase inhibitors (XOI). Since these medications are the cornerstone of gout treatment, having additional agents is important. Patients with the HLA-B*58:01 haplotype have an increased risk of allopurinol hypersensitivity syndrome; thus, their options are limited if they do not tolerate febuxostat. Newer XOI agents may also allow for less intensive drug titration compared with allopurinol.
The treatment of gout flares also has significant gaps that the gout pipeline is attempting to address. There are significant limitations to current treatments for acute gout flares, mainly related to contra-indications such as heart failure, renal disease, and active peptic ulcer disease. New approaches targeting the inflammasome and IL-1 activation are under active study.
Developing solutions to address current limitations in gout treatment can be extremely cost-effective. Research on patients with gout suggested an average of 25 missed workdays per year due to disease [6]. It is estimated that the total annual costs caused by uncontrolled gout add an individual financial burden of over $30,000 yearly, with gout patients being less likely to be active participants in the workforce compared to non-gout controls [7].
The new strategies we describe in this review have the potential to improve compliance with gout medications, allow treatment of patients with multiple comorbidities, simplify treatment strategies, and reduce the cost of care by controlling gout in expanded patient populations. Selected agents under study are listed in Table 1.
Urate Lowering Therapies (ULT)
URAT1 Agents
Human urate transporter 1 (URAT1) has been identified in the renal tubules as a key player in this process. Existing URAT1 inhibitors such as probenecid are hampered by the fact that kidney impairment may blunt its efficacy, and increase the risk of renal stones. Benzbromarone is a more potent URAT1 inhibitor but has been marred by concerns with potential hepatotoxicity [8].
A more recent agent, lesinurad, was the first selective uric acid resorption inhibitor (SURI) approved by the FDA. This URAT1 and organic anion transporter 4 (OAT4) inhibitor was found to be an effective agent when combined with allopurinol in the CLEAR1 and CLEAR2 trials [9, 10]. However, these studies found a transient elevation of creatinine greater than 1.5× above baseline among lesinurad-treated patients compared to standard therapy when dosed at 400 mg vs 200 mg. Due to the fear of the formation of micro-crystals in the kidney, lesinurad was approved for use only in conjunction with an XOI in an attempt to reduce renal risk and required frequent monitoring of creatinine clearance. Lesinurad was discontinued in both the US and European markets, with the manufacturer citing financial rather than medical concerns.
Dotinurad
Dotinurad is another SURI, approved in Japan in 2020 for gout and asymptomatic hyperuricemia, and is currently being evaluated in US and European markets. A double-blinded randomized phase 2 study showed promise when 200 hyperuricemic patients with or without gout were given dotinurad or placebo. In the highest (4 mg) dose group, 100% of treated patients achieved a goal urate less than 6.0 mg/dL by the final visit [11]. A phase 3 study with 201 patients comparing the efficacy of dotinurad to benzbromarone demonstrated non-inferiority of dotinurad, with 86.2% and 83.6% of patients, respectively, reaching goal level urate (p = 0.693) at the end of the trial with similar rates of adverse drug reactions [12]. A similar randomized double-blinded study comparing dotinurad to febuxostat once again showed non-inferiority, finding a 41.8% and 44% reduction in uric acid, respectively, after a 14-week period [13•]. In a larger study examining longer-term use, Hosoya et al. [14] titrated 330 hyperuricemic patients to a target dose of 2 or 4 mg daily dotinurad for a total of 34 or 58 weeks. Of note, several safety signals were raised, with an overall incidence of AE at 65.3% and ADRs at 21.8% leading to discontinuation in 4.5% and 3%, respectively. Most commonly, this included nasopharyngitis (17.9%) and gout flare (13.0%). More severe cases included an increased incidence of renal calculi (1.5%). Interestingly, there was a small but statistically significant increase in eGFR in the dotinurad arm, but a further study on dotinurad in CKD and diabetic kidney disease did not confirm significant changes in creatinine [15]. Overall, once-daily dotinurad appears to be at least as effective as existing ULTs. Notably, dotinurad did not cause the increase in creatinine that lesinurad showed. Like lesinurad, dotinurad appears to be effective in patients with moderate renal dysfunction, a potential advantage over probenecid.
Verinurad
Verinurad is a second-generation URAT1 inhibitor which, as with lesinurad, was found in early studies to increase the risk of renal functional decline. A pooled analysis of two phase II trials of 376 patients taking verinurad with gout or asymptomatic hyperuricemia found 17.1% of those in the treatment arm had creatinine elevations over 1.5× baseline with a substantial proportion not returning to baseline levels by the end of the studies [16]. Although found to be an effective ULT, the adverse renal effects of verinurad had been deemed a reason to avoid the agent as monotherapy, but more recent research has looked into its use as a combination therapy with an XOI. A phase II trial involving 60 adults with hyperuricemia, T2DM, and albuminuria found that combination therapy with verinurad and febuxostat against placebo not only lowered serum uric acid by 63.7% at 24 weeks but resulted in neither a clinically meaningful reduction in eGFR (the authors cited concerns over power to detect statistically significant differences), nor differences in incidence of renal calculi between active and control arms. However, 62.5% of patients suffered from treatment-related AEs, most commonly diarrhea (12.5%) and dizziness (9.4%) [17]. It is hoped that the phase IIa SAPPHIRE study (Study of verinurAd and alloPurinol in Patients with cHronic kIdney disease and hyperuRicaEmia; NCT03990363) will help elucidate the renal safety of allopurinol with combined verinurad [18].
Arhalofenate
Arhalofenate is the first medication shown to reduce not only serum uric acid but also a risk of flare, which would be of special interest when ULT is started. Arhalofenate inhibits both URAT1 and OAT4, thereby reducing urate reabsorption in the proximal tubule. It also decreases IL-1 beta and IL-6 release and inflammasome activation by interfering with the peroxisome proliferator-activated receptor (PPAR) gamma pathway [19]. Poiley et al. conducted a 12-week, phase IIb, double-blinded, randomized controlled trial (RCT) in which 239 gout patients were assigned, in a 2:2:2:2:1 ratio, to receive 600-mg arhalofenate, or 800-mg arhalofenate, or 300-mg allopurinol, or 300-mg allopurinol plus 0.6-mg colchicine, or placebo once a day [20•]. Although arhalofenate was found to be less effective as a ULT compared to 300-mg allopurinol, it did reduce incidence of flare by 46% compared to allopurinol. Similar rates of treatment-related AEs and no increase in baseline creatinine were found across all groups, and notably, no renal calculi were observed in the arhalofenate group. Data does not exist yet for patients with renal impairment, and phase III clinical trials in combination with febuxostat are currently underway.
Xanthine Oxidase Inhibitors
Tigulixostat
A disadvantage of existing ULTs includes the need for frequent dose titration to reach a serum uric acid (sUA) goal, especially in patients with renal dysfunction. In contrast, tigulixostat, a novel, non-purine, selective xanthine oxidase inhibitor appears to demonstrate promising sUA lowering efficacy at lower drug dosages with less need for dose titration. Potential adverse effects include elevations of creatine kinase (CK) and transaminase levels.
The phase II CLUE trial examined the safety and efficacy of tigulixostat in gout patients with hyperuricemia [21•]. This randomized, double-blinded, placebo-controlled multicenter study evaluated doses of 50 mg, 100 mg, and 200 mg daily. The primary endpoint was the proportion of patients with sUA < 5 mg/dL at week 12. All patients received colchicine prophylaxis. Out of 143 patients randomized, 62.2% of the 200 mg group, 44.7% of the 100 mg group, and 47.1% of the 50 mg group achieved the primary endpoint compared to 2.9% of the placebo group (p < 0.0001). A significant percentage of patients reached sUA level < 5 mg/dL as early as week 2 of the study. Notably, this rapid lowering of sUA was seen even in the lower-dose group receiving 100 mg. There was no effect on reducing gout flares, and flare rates across groups did not appear to have an association with dosage. Several cases of transaminase elevation developed after drug initiation, and low-grade CK elevation was seen, most specifically in the 200 mg group [21•]. The performance of tigulixostat compared to allopurinol will be the subject of future investigation. The EURELIA 1 and 2 studies will evaluate safety and efficacy of 6 months of treatment with tigulixostat compared to allopurinol in a randomized, double-blind, parallel-group placebo-controlled study [22, 23].
Uricases
The pathologic accumulation of serum urate is unique in that it results from a lack of the enzyme uricase in humans, which metabolizes uric acid into the easily soluble and excretable allantoin [24]. Pegloticase, a pegylated recombinant uricase, was designed to rectify this gap. However, pegloticase is contraindicated in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency and has been associated with infusion reactions secondary to a significant degree of immunogenicity [24]. Major resultant drawbacks to compliance and efficacy include strict pre-treatment monitoring of sUA levels. Treatment is promptly stopped for levels > 6.0 mg/dL, which suggests loss of efficacy due to neutralizing anti-drug antibodies (ADAs) to pegloticase. ADAs are also associated with subsequent infusion reactions [25].
SEL-212
Novel pegylated uricase SEL-212 has demonstrated a reduced risk of ADA formation in addition to efficacious serum urate control, without the need for a separate immunosuppressant. Recent research has shown that co-administration of pegloticase with immunosuppressants leads to better treatment response rates and fewer infusion reactions [26,27,28]. The FDA has approved the combined use of pegloticase and methotrexate to reduce immunogenicity based on the MIRROR trial [28]. In contrast, SEL-212 is a combination of SEL-037 and SEL-110, respectively, pegadricase (or pegsiticase) and a synthetic vaccine particle (SVP) encapsulating rapamycin (SVP-R, or ImmTOR) [29]. This design is unique in its incorporation of ImmTOR nanoparticles specifically to decrease the immunogenicity of the recombinant uricase [30]. Induction of immunological tolerance is achieved through the exposure to antigen together with encapsulated rapamycin and induction of a regulatory T-cell response specific to the antigen presented.
Phase I and II studies of SEL-212 have thus far shown a reduction in ADAs, achievement of sUA control with monthly infusion, and few adverse effects [31,32,33,34]. A phase I trial examined the safety of varying doses of SEL-212 administered as a single monthly infusion in patients with hyperuricemia [31]. Phase II results demonstrated a reduction in sUA through 30 days of post-administration monitoring, with undetectable sUA at day 30 in subjects receiving SVP-R at the highest dose [33, 34]. Adverse events consisted solely of skin rash, seen also at the lowest effective dose. Further dose studies evaluated the safety and tolerability of three, monthly, infusions of SEL-212 followed by monthly infusions of SEL-037 alone in patients with symptomatic gout and hyperuricemia [34]. Additional phase II trials showed that all patients in the study who achieved a sUA < 6 mg/dL at 3 months also maintained control at months 4 and 5. Sixty-six percent of patients maintained sUA control at week 20 with low or no ADAs present. Notably, the rate of gout flares remained relatively low (29–35%). Future studies with SEL-212 include the COMPARE phase II trial to compare the safety and efficacy of SEL-212 with pegloticase [35]. The DISSOLVE phase 3 trial will further investigate two different doses of SEL-212 [36]. Should SEL-212, which does not require administration with methotrexate to limit immunogenicity, demonstrate equal-to-superior safety and efficacy compared to methotrexate/pegloticase, it may offer a strong future alternative to the existing treatment option.
ALLN-346
A novel urate metabolizer, ALLN-346, is an oral bioengineered uricase for use in patients with impaired renal function. It acts locally in the gut without systemic absorption, potentially reducing the rate of systemic immunogenicity as compared to pegloticase. This oral agent takes advantage of the intestinal excretion pathway for urate reduction, which has yet to be utilized in strategies for sUA control (Fig. 1). In settings of reduced renal excretion, there is a corresponding physiologic adaptation of increased intestinal urate excretion. ALLN-346 has demonstrated potential effectiveness in published proof-of-concept mouse studies, two completed phase I trials, and one ongoing phase IIa study with preliminary data [37,38,39]. The phase II trial evaluated safety and bioactivity in a small group of patients with hyperuricemia and renal function ranging from normal to stage 2 chronic kidney disease (CKD) [39]. Results demonstrated a significant reduction in mean sUA in all patients receiving the study drug compared to placebo (p < 0.05). This reduction was especially prominent in patients with CKD, providing support for localized intestinal activity. Lack of systemic absorption was demonstrated by ELISA testing of serum before and after administration, and no serious adverse events were noted. A future phase II study, presently in recruitment, will evaluate safety and efficacy in patients with gout, hyperuricemia, and mild to moderate CKD [22].
Both endogenously synthesized and exogenously derived purines are metabolized into hypoxanthine, xanthine, and uric acid (urate) by the enzyme xanthine oxidase. Uric acid is excreted from the human body primarily by a renal mechanism and less predominantly by an intestinal pathway. In mammals other than humans and apes, the enzyme uricase further metabolizes uric acid into the soluble form of allantoin. Urate homeostasis within the kidney is controlled by ion transporters such as URAT1 and OAT4. Hyperuricemia can occur as a result of overproduction or underexcretion from derangements or imbalance in this metabolic pathway from a variety of factors, subsequently leading to tissue deposition and triggering of a pro-inflammatory signal cascade as illustrated further in Fig. 2. Newer agents are in red
Treatments for Gout Flares
The Inflammasome
IL-1β is a potent mediator of the innate immune response with pleiotropic effects throughout the body, including induction of fever, stimulation of the hypothalamic-pituitary-adrenal axis, endothelial activation, promotion of neutrophil trafficking, and differentiation of lymphoid cells [40]. Produced predominantly by monocytes and macrophages, its secretion is modulated by upstream intracellular signaling cascades that converge on the inflammasome, a molecular scaffold comprised of oligomerized pattern recognition receptors (PRRs). The most well-characterized of these is the nucleotide-binding domain and leucine-rich repeat pyrin-containing protein-3 (NLRP3) inflammasome. In acute gouty inflammation, MSU crystals engage cell-surface PRRs on synovial tissue macrophages, providing a priming signal that leads to increased pro-IL-1β transcription. Phagocytosis of crystals generates reactive oxygen species and decreases intracellular potassium levels. These markers of endogenous stress activate NLRP3 inflammasome assembly, with brisk secretion of IL-1β [41]. This inflammatory axis represents an exciting target for novel therapeutics and a promising focus of future investigative directions (Fig. 2).
Transcription of inactive pro-IL-1β is upregulated in response to “priming signals,” which are transmitted when cytosolic and cell surface germline-encoded pattern recognition receptors (PRRs) are engaged by evolutionarily conserved motifs on microbes and damaged host tissue fragments [66]. A secondary “activating signal” launches an intracellular cascade that converges on the formation of the inflammasome, a complex comprised of oligomerized PRRs associated with an adaptor protein thus activating IL-1 [67]. Newer agents are in red
Current Anti Il-1 Therapies
There are currently three FDA-approved anti-IL-1 therapies: anakinra, canakinumab, and rilonacept. Although none of these agents is labeled for gout in the USA, based on data reporting the superiority of canakinumab to triamcinolone in patients with intolerance, non-response, or contraindication to NSAIDs and/or colchicine [42], the European Medicines Agency in 2013 approved the use of canakinumab for acute gout.
Recent studies have demonstrated the efficacy of these agents in acute flare treatment. A 2019 multicenter RCT by Janssen et al. utilized a double-dummy, placebo-controlled design to evaluate the non-inferiority of anakinra compared to colchicine, naproxen, or prednisone, finding that anakinra was non-inferior to comparators without increased risk of serious adverse events [43•]. In another multicenter RCT, Saag et al. investigated the superiority of anakinra vs. triamcinolone. Anakinra failed to meet superiority for the primary endpoint, though select secondary endpoints were in its favor, with similar times to resolution of pain and equivalent rates of adverse effects between groups [44•].
Despite accumulating data on the effectiveness of IL-1 blockade, concerns about cost continue to limit real-world use. A model-based cost-effectiveness analysis in the Netherlands compared naproxen, prednisone, colchicine, or anakinra as flare treatment, stratified on concomitant use of backbone ULT [45]. Although anakinra-based strategies yielded marginally greater quality-adjusted life years (QALYs) vs. other agents, there was a near zero probability that anakinra was cost-effective as flare management at any willingness to pay up to €80,000.
Largely due to cost, ACR and EULAR recommend IL-1 blockage as a salvage therapy only when usual care has failed or is contraindicated [46, 47]. Colchicine, NSAID, and glucocorticoid use is often restricted by co-morbid medical conditions such as hypertension, chronic kidney disease (CKD), and heart failure. In hospitalized patients and highly selected outpatients, IL-1 blockade is a major addition to the therapeutic armamentarium given the class’s relative safety and tolerability [48].
Novel Investigative Directions
Several investigations into optimal dosing strategies, target patient populations, and novel formulations of drugs targeting the IL-1 pathway are currently underway. A phase II, blinded, double-dummy RCT comparing anakinra 100 mg vs. prednisone 30 mg for acute gout flare in patients with CKD stages 4, 5, or renal transplant began in June 2022 [49]. The findings of this research will be of particular relevance in the advanced CKD patient population, who typically were excluded from earlier anakinra trials.
IL-1 Inhibitors
SSGJ-613, a humanized monoclonal antibody against IL-1β, is currently recruiting for phase I/II multicenter trials and will be studied in a variety of dosing schemes [50]. A study of RPH-104, a heterodimeric fusion protein that binds and inactivates circulating IL-1β was terminated due to recruitment difficulties as well as the results of early interim analysis showing no significant difference between RPH-104 at any dose and NSAID therapy in reduction of pain intensity at the target joint [51]. AC-201, an oral caspase and IL-1β modulator whose active metabolite down-regulates IL-1R and up-regulates IL-1Ra, failed to demonstrate efficacy for flare prophylaxis compared to febuxostat in a double-blinded RCT. Nevertheless, further study of oral anti-IL-1 agents is still of great interest in light of many patients’ preferences for oral over injectable therapy [52].
NLRP3
Dapansutrile (OLT1177)
Upstream of IL-1β, NLRP3 inflammasome-directed research represents a promising area of inquiry. Dapansutrile (OLT1177), an oral small molecule that selectively binds and inhibits the NLRP3 inflammasome [53•], is under study in a phase II/III randomized, double-blind, placebo-controlled safety and efficacy trial. Patients with acute flare onset within 96 h will be randomized to receive dapansutrile tablets vs. placebo for 7 days without concurrent use of NSAID, colchicine, or steroid with the primary outcome defined as change in VAS in the target joint from baseline to 72 h after treatment. Much like AC-201, dapansutrile’s oral formulation makes it a particularly compelling therapeutic agent. Several other agents with NLRP3 inhibitory properties are currently under study in ex vivo and mouse models of gout, as well as in other inflammasome-driven diseases.
Discussion
An ideal agent for gout is fast-acting, effective as monotherapy, easy to titrate, well-tolerated, cost-efficient, and can be used without contraindication in the setting of the many comorbidities often found in gout patients.
So far, the URAT1 agents have shown the ability to lower urate, especially in combination with an XOI. They unfortunately have tended to raise creatinine levels and have the potential to increase renal stone formation. This may well be a class effect although they may have some use as a combination therapy. Dotinurad is highlighted as a potential monotherapy, so far appearing to be without major renal issues in comparison to the others mentioned in this group. Arhalofenate, despite its mild urate-lowering effects, may have utility in light of both its urate-lowering and flare-reduction properties.
As a new XOI agent, tigulixostat appeared to reach urate goals in many patients without the need for multiple dose titrations. Upcoming trials comparing tigulixostat in different doses (EURELIA 1—currently recruiting) and compared with allopurinol (EURELIA 2—not yet recruiting) will be of significant interest [22, 23].
Pegloticase can lose its uricase effectiveness due to neutralizing ADAs, and a number of immunosuppressive agents have been employed in combination to reduce its immunogenicity (61). The MIRROR trial and others showed success in reducing ADAs by administering pegloticase with methotrexate [26,27,28]. These findings have resulted in FDA approval for this combination [54]. Additional trials studying co-administration of azathioprine, leflunomide, and mycophenolate mofetil have also yielded promising findings [55,56,57]. SEL-212 combines ImmTOR nanoparticles with a recombinant uricase to decrease its immunogenicity and avoid the need for a separate immunosuppressive [30].
A novel oral uricase inhibitor, ALLN-346, acts only in the gastrointestinal tract and could be useful if proven to avoid the limitations of immunogenicity and IV formulation characteristic of pegloticase. For the management of acute gout, there is a definite interest in the NLRP3 inflammasome inhibitor, dapansutrile, which offers both a novel target and an oral formulation.
Future Research Directions
Additional novel gout treatment approaches have recently been proposed, largely on the basis of known inflammatory cascade responses in gout. There has been an implication for the role of transforming growth factor (TGF)-beta in the inflammatory pathway triggered by soluble urate, as described previously (Fig. 2), resulting in an increase in IL-1 beta and a decrease in IL-1 receptor antagonist. One such study examines levels of TGF-beta mRNA in normal subjects, those with hyperuricemia without gout, and patients with gout [58]. Elevated levels of TGF-beta mRNA were noted in monocytes of patients with gout compared with those of healthy controls. Significantly higher serum concentrations of TGF-beta mRNA were found in patients with hyperuricemia compared with healthy controls. These provocative results raise the question of whether future studies might demonstrate that blocking of TGF-beta might have a future role in gout management.
Additional potential targets along the inflammasome pathway currently show promise. Recent work on monosodium urate (MSU) crystal-induced NLRP3 activation suggests a role for microRNA-mediated negative regulation of IL-1β production and macrophage migration in both in vitro human cells and murine models [59]. Mouse model and in vitro human monocyte-derived cell data have demonstrated the role of TFNR-associated factor 1 (TRAF1) in negatively regulating inflammasome activity via limitation of adaptor protein ubiquitination [60]. A detailed genetic, RNA sequencing, and proteomic study of a premenopausal woman with normouricemic erosive gout identified variants in the NLRP3 gene and deficiency in the protein lubricin; in subsequent experimental models, lubricin was found to attenuate MSU crystal precipitation and xanthine oxidase induction by IL-1β [61]. While still in the bench phases of investigation, these targets suggest future directions for proximal modulation of IL-1β release and activity.
Conclusion
Current treatments for gout are very successful, if considering only the patients who receive them, tolerate them, are dosed appropriately, and comply with their regimens. Unfortunately, the international record for getting patients onto urate-lowering agents, and getting them to goal urate, is poor [62, 63]. The pipeline agents described here, and others developed in the future, may allow more patients to reach goal urate and control their gout, by offering an alternative to medications not tolerated, being easier to take, less expensive, and/or more effective than currently approved agents. While effective patient education, close patient follow-up, and nurse management can markedly improve medication adherence and achievement of urate target goals [64, 65], improvements in our medications to manage gout could lead to significantly better outcomes for our gout patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Li L, Yang C, Zhao Y, Zeng X, Liu F, Fu P. Is hyperuricemia an independent risk factor for new-onset chronic kidney disease?: A systematic review and meta-analysis based on observational cohort studies. BMC Nephrology. 2014;15:122. https://doi.org/10.1186/1471-2369-15-122.
Cicero AF, Salvi P, D’Addato S, Rosticci M, Borghi C. Association between serum uric acid, hypertension, vascular stiffness and subclinical atherosclerosis: data from the Brisighella Heart Study. J Hyper. 2014;32(1):57–64. https://doi.org/10.1097/HJH.0b013e328365b916.
Choi HK, McCormick N, Yokose C. Excess comorbidities in gout: the causal paradigm and pleiotropic approaches to care. Nature Rev Rheuma. 2022;18(2):97–111. https://doi.org/10.1038/s41584-021-00725-9.
Lv Q, Meng XF, He FF, Chen S, Su H, Xiong J, et al. High serum uric acid and increased risk of type 2 diabetes: a systemic review and meta-analysis of prospective cohort studies. PloS One. 2013;8(2):e56864. https://doi.org/10.1371/journal.pone.0056864.
Cipolletta E, Tata LJ, Nakafero G, Avery AJ, Mamas MA, Abhishek A. Risk of venous thromboembolism with gout flares. Arthritis & rheumatology (Hoboken, NJ). 2023. https://doi.org/10.1002/art.42480.
Edwards NL, Sundy JS, Forsythe A, Blume S, Pan F, Becker MA. Work productivity loss due to flares in patients with chronic gout refractory to conventional therapy. J Med Eco. 2011;14(1):10–5. https://doi.org/10.3111/13696998.2010.540874.
Flores NM, Nuevo J, Klein AB, Baumgartner S, Morlock R. The economic burden of uncontrolled gout: how controlling gout reduces cost. J Med Eco. 2019;22(1):1–6. https://doi.org/10.1080/13696998.2018.1532904.
Blake KEG, Saag JL, Saag KG. What’s new on the front-line of gout pharmacotherapy? Exp Opinion Pharma. 2022;23(4):453–64. https://doi.org/10.1080/14656566.2021.2020249.
Saag KG, Fitz-Patrick D, Kopicko J, Fung M, Bhakta N, Adler S, et al. Lesinurad Combined with allopurinol: a randomized, double-blind, placebo-controlled study in gout patients with an inadequate response to standard-of-care allopurinol (a US-based study). Arthritis Rheuma (Hoboken, NJ). 2017;69(1):203–12. https://doi.org/10.1002/art.39840.
Bardin T, Keenan RT, Khanna PP, Kopicko J, Fung M, Bhakta N, et al. Lesinurad in combination with allopurinol: a randomised, double-blind, placebo-controlled study in patients with gout with inadequate response to standard of care (the multinational CLEAR 2 study). Annals Rheumatic Dis. 2017;76(5):811–20. https://doi.org/10.1136/annrheumdis-2016-209213.
Hosoya T, Sano T, Sasaki T, Fushimi M, Ohashi T. Clinical efficacy and safety of dotinurad, a novel selective urate reabsorption inhibitor, in Japanese hyperuricemic patients with or without gout: randomized, multicenter, double-blind, placebo-controlled, parallel-group, confirmatory phase 2 study. Clin Exp Nephrology. 2020;24(Suppl 1):53–61. https://doi.org/10.1007/s10157-019-01818-2.
Hosoya T, Sano T, Sasaki T, Fushimi M, Ohashi T. Dotinurad versus benzbromarone in Japanese hyperuricemic patient with or without gout: a randomized, double-blind, parallel-group, phase 3 study. Clinical and experimental nephrology. 2020;24(Suppl 1):62–70. https://doi.org/10.1007/s10157-020-01849-0.
Hosoya T, Furuno K, Kanda S. A non-inferiority study of the novel selective urate reabsorption inhibitor dotinurad versus febuxostat in hyperuricemic patients with or without gout. Clinical and experimental nephrology. 2020;24(Suppl 1):71–9. https://doi.org/10.1007/s10157-020-01851-6.Arandomizeddouble-blindedstudycomparingdotinuradtofebuxostatonceagainshowednon-inferiorityintheabilitytoloweruricacid.
Hosoya T, Fushimi M, Okui D, Sasaki T, Ohashi T. Open-label study of long-term administration of dotinurad in Japanese hyperuricemic patients with or without gout. Clinical and experimental nephrology. 2020;24(Suppl 1):80–91. https://doi.org/10.1007/s10157-019-01831-5.
Yanai H, Katsuyama H, Hakoshima M, Adachi H. Urate transporter 1 can be a therapeutic target molecule for chronic kidney disease and diabetic kidney disease: a retrospective longitudinal study. Biomedicines. 2023;11(2). https://doi.org/10.3390/biomedicines11020567.
Fitz-Patrick D, Roberson K, Niwa K, Fujimura T, Mori K, Hall J, et al. Safety and efficacy of verinurad, a selective URAT1 inhibitor, for the treatment of patients with gout and/or asymptomatic hyperuricemia in the United States and Japan: findings from two phase II trials. Modern rheumatology. 2019;29(6):1042–52. https://doi.org/10.1080/14397595.2018.1538003.
Stack AG, Dronamraju N, Parkinson J, Johansson S, Johnsson E, Erlandsson F, et al. Effect of intensive urate lowering with combined verinurad and febuxostat on albuminuria in patients with type 2 diabetes: a randomized trial. Ame J Kidney Diseases: official J National Kidney Foundation. 2021;77(4):481–9. https://doi.org/10.1053/j.ajkd.2020.09.009.
Heerspink HJL, Stack AG, Terkeltaub R, Greene TA, Inker LA, Bjursell M, et al. Rationale, design, demographics and baseline characteristics of the randomized, controlled, phase 2b SAPPHIRE study of verinurad plus allopurinol in patients with chronic kidney disease and hyperuricaemia. Nephrology, Dialysis, Transplantation: official Publ Eur Dialysis Transplant Assoc - European Renal Assoc. 2022;37(8):1461–71. https://doi.org/10.1093/ndt/gfab237.
McWherter C, Choi YJ, Serrano RL, Mahata SK, Terkeltaub R, Liu-Bryan R. Arhalofenate acid inhibits monosodium urate crystal-induced inflammatory responses through activation of AMP-activated protein kinase (AMPK) signaling. Arthritis Res Therapy. 2018;20(1):204. https://doi.org/10.1186/s13075-018-1699-4.
• Poiley J, Steinberg AS, Choi YJ, Davis CS, Martin RL, McWherter CA, et al. A randomized, double-blind, active- and placebo-controlled efficacy and safety study of arhalofenate for reducing flare in patients with gout. Arthritis & rheumatology (Hoboken, NJ). 2016;68(8):2027-34. https://doi.org/10.1002/art.39684. Arhalofenate 12-week phase IIb double-blinded RCT comparing arhalofenate to allopurinol and colchicine finding a modest reduction in uric acid and incident flare rates without renal issues.
3.Terkeltaub R LJ, Min J, Shin S, Saag KG. Serum urate-lowering efficacy and safety of tigulixostat in gout patients with hyperuricemia: a randomized, double-blind, placebo-controlled, dose-finding trial (CLUE). Arthritis & Rheumatology. 2023. https://doi.org/10.1002/art.42447. Latest data on tigulixostat findings demonstrated the capability of moderate to high-dose drug to reach a serum urate goal early in the trial and maintain control.
ClinicalTrials.gov. 2022. https://clinicaltrials.gov/ct2/show/NCT05586958. Accessed 19 Apr 2023.
ClinicalTrials.gov. 2022. https://clinicaltrials.gov/ct2/show/NCT05586971. Accessed 19 Apr 2023.
Padda IS BR, Parmar M. Pegloticase. In: StatPearls. 2023 January ed. Treasure Island (FL): StatPearls Publishing. 2023. https://www.ncbi.nlm.nih.gov/books/NBK572054/Pegloticase. Accessed 19 Apr 2023.
Schlesinger NLP. Pegloticase treatment of chronic refractory gout: update on efficacy and safety. Seminars Arthritis Rheumatism. 2020;50(3S):S31–8. https://doi.org/10.1016/j.semarthrit.2020.04.011.
Albert JHT, LaMoreaux B. Increased efficacy and tolerability of pegloticase in patients with uncontrolled gout co-treated with methotrexate: a retrospective study. Rheumatol Therapy. 2020;7(3):639–48. https://doi.org/10.1007/s40744-020-00222-7.
Botson JKPJ. Pretreatment and coadministration with methotrexate improved durability of pegloticase response: an observational, proof-of-concept case series. Journal of Clinical Rheumatology. 2022;28(1):e129–34. https://doi.org/10.1097/RHU.0000000000001639.
Botson JK OK, LaMoreaux B, Zhao L, Weinblatt ME, Peterson J. Improved joint and patient-reported health assessments with pegloticase plus methotrexate co-therapy in patients with uncontrolled gout: 12-month exploratory outcomes of the MIRROR open-label trial. Arthritis research & therapy. 2022;24(1). https://doi.org/10.1186/s13075-022-02979-4.
Sands EKA, Johnston L, Kishimoto TK. THU0422 SEL-212: enhanced serum uric acid control in hyperuricemic patients through selective mitigation of anti-drug antibodies against pegsiticase. Annals of the rheumatic diseases. 2017;76 367.
TK K. Development of ImmTOR tolerogenic nanoparticles for the mitigation of anti-drug antibodies. Frontiers in Immunology. 2020;11. https://doi.org/10.3389/fimmu.2020.00969.
ClinicalTrials.gov. 2016. https://clinicaltrials.gov/ct2/show/NCT02648269. Accessed 2016 January 7.
ClinicalTrials.gov. 2016. https://clinicaltrials.gov/ct2/show/NCT02959918. Accessed 2016 November 9.
Sands EKA, Johnston L, DeHaan W, Kishimoto TK. FRI0234 SEL-212: Selective mitigation of anti-drug antibodies against pegsiticase to control serum uric acid in hyperuricemic subjects. Annals Rheumatic Dis. 2018;77:658. https://doi.org/10.1136/annrheumdis-2018-eular.7396.
Smolinski S KA, Dehaan W, Johnston L, Azeem R, Kishimoto TK. SAT0402 SEL-212 Phase 2 clinical study in symptomatic gout patients: ImmTOR tolerogenic nanoparticles combined with pegadricase mitigates immunogenicity and enables sustained reduction of serum uric acid levels, low rate of gout flares and monthly dosing. Annals of the rheumatic diseases. 2019:1288-9. https://doi.org/10.1136/annrheumdis-2019-eular.7769.
ClinicalTrials.gov. 2019. https://clinicaltrials.gov/ct2/show/NCT03905512. Accessed 2019 April 5.
ClinicalTrials.gov. 2020 https://clinicaltrials.gov/ct2/show/NCT04596540. Accessed 19 Apr 2023.
Pierzynowska K DA, Mosiichuk N, Terkeltaub R, Szczurek P, Salido E, Pierzynowski S, Grujic D. Oral treatment with an engineered uricase, ALLN-346, reduces hyperuricemia, and uricosuria in urate oxidase-deficient mice. Frontiers in Medicine. 2020;7. https://doi.org/10.3389/fmed.2020.569215.
Clark DGD, Tosone C, Dahl N, Terkeltaub R. Phase 1 trials of novel oral enzyme therapy (ALLN-346) for hyperuricemia & gout: safety, pharmacodynamics, and lack of systemic absorption of single and multiple ascending doses in healthy volunteers. Annals of the rheumatic diseases. 2022;81:906–7. https://doi.org/10.1136/annrheumdis-2022-eular.843.
Terkeltaub RCD, Tosone C, Kandinov B, Zhang P, Dahl N, Grujic D, Goldfarb D. POS1157 Safety and efficacy of ALLN-346 oral enzyme therapy in patients with hyperuricemia and chronic kidney disease (CKD): results of the phase 2A study 201. Annals Rheumatic Dis. 2022;81:907. https://doi.org/10.1136/annrheumdis-2022-eular.1662.
Garlanda C, Dinarello CA, Mantovani A. The interleukin-1 family: back to the future. Immunity. 2013;39(6):1003–18. https://doi.org/10.1016/j.immuni.2013.11.010.
Martinon F, Pétrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440(7081):237–41. https://doi.org/10.1038/nature04516.
Schlesinger N, Alten RE, Bardin T, Schumacher HR, Bloch M, Gimona A, et al. Canakinumab for acute gouty arthritis in patients with limited treatment options: results from two randomised, multicentre, active-controlled, double-blind trials and their initial extensions. Annals of the rheumatic diseases. 2012;71(11):1839–48. https://doi.org/10.1136/annrheumdis-2011-200908.
Janssen CA, Oude Voshaar MAH, Vonkeman HE, Jansen T, Janssen M, Kok MR, et al. Anakinra for the treatment of acute gout flares: a randomized, double-blind, placebo-controlled, active-comparator, non-inferiority trial. Rheumatology (Oxford). 2019. https://doi.org/10.1093/rheumatology/key402. This is a double-blind, double-dummy, non-inferiority RCT comparing anakinra to naproxen, colchicine, or prednisone for management of acute gout flare demonstrating non-inferiority of anakinra to usual care.
Saag KG, Khanna PP, Keenan RT, Ohlman S, Osterling Koskinen L, Sparve E, et al. A randomized, phase II study evaluating the efficacy and safety of anakinra in the treatment of gout flares. Arthritis Rheuma (Hoboken, NJ). 2021;73(8):1533–42. https://doi.org/10.1002/art.41699. This double-blind, double-dummy superiority RCT comparing anakinra to triamcinolone for the management of acute gout flare found no statistically significant difference between study arms in pain reduction or time to resolution of pain.
van de Laar CJ, Janssen CA, Janssen M, Oude Voshaar MAH, Al MJ, van de Laar M. Model-based cost-effectiveness analyses comparing combinations of urate lowering therapy and anti-inflammatory treatment in gout patients. PloS one. 2022;17(1):e0261940. https://doi.org/10.1371/journal.pone.0261940.
Richette P, Doherty M, Pascual E, Barskova V, Becce F, Castañeda-Sanabria J, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Annals Rheumatic Dis. 2017;76(1):29–42. https://doi.org/10.1136/annrheumdis-2016-209707.
FitzGerald JD, Dalbeth N, Mikuls T, Brignardello-Petersen R, Guyatt G, Abeles AM, et al. 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis Care Res. 2020;72(6):744–60. https://doi.org/10.1002/acr.24180.
Guttmann A, Krasnokutsky S, Pillinger MH, Berhanu A. Pegloticase in gout treatment-safety issues, latest evidence and clinical considerations. Therapeutic Adv Drug Safety. 2017;8(12):379–88. https://doi.org/10.1177/2042098617727714.
Assistance Publique - Hôpitaux de P: Anakinra vs prednisone to treat gout flare in patients with chronic kidney disease stage 4/5 or renal transplantation. https://ClinicalTrials.gov/show/NCT04844814 (2025). Accessed.
Twi Biotechnology I: a proof-of-concept study of AC-201 to prevent gout flares. https://ClinicalTrials.gov/show/NCT01712204 (2013). Accessed.
Pharm R, Covance, Laboratories ZAOU, Data Matrix S, Pharmaceutical Analytics Center LLC, Ltd OCTR: safety, tolerability, pharmacokinetics and pharmacodynamics evaluation of RPH-104 administered at different doses to patients with acute gout attack. https://ClinicalTrials.gov/show/NCT04067492 (2020). Accessed.
Alten R, Krüger K, Rellecke J, Schiffner-Rohe J, Behmer O, Schiffhorst G, et al. Examining patient preferences in the treatment of rheumatoid arthritis using a discrete-choice approach. Patient Prefer Adherence. 2016;10:2217–28. https://doi.org/10.2147/ppa.S117774.
Klück V, Jansen T, Janssen M, Comarniceanu A, Efdé M, Tengesdal IW, et al. Dapansutrile, an oral selective NLRP3 inflammasome inhibitor, for treatment of gout flares: an open-label, dose-adaptive, proof-of-concept, phase 2a trial. Lancet Rheumatol. 2020;2(5):e270-e80. https://doi.org/10.1016/s2665-9913(20)30065-5. This is an upcoming phase II/III randomized, double-blind, placebo-controlled safety and efficacy study of dapansutrile (OLT1177), an oral small molecule that selectively binds and inhibits the NLRP3 inflammasome and is expected to be completed in October 2023.
Therapeutics H. Krystexxa (pegloticase) [prescribing information].
Rainey HBH, Yeo A, Lipsky P. THU0410 Companion immunosuppression with azathioprine increases the frequency of persistent responsiveness to pegloticase in patients with chronic refractory gout. Annals of the rheumatic diseases. 2020;79:442–3. https://doi.org/10.1136/annrheumdis-2020-eular.4642.
Masri KRP-SL, Winterling K, LaMoreaux B. Effect of leflunomide on pegloticase response rate in patients with uncontrolled gout: a retrospective study. Rheuma Therapy. 2022;9(2):555–63. https://doi.org/10.1007/s40744-021-00421-w.
Khanna PPKD, Cutter G, Foster J, Melnick J, Jaafar S, Biggers S, Rahman AKMF, Kuo HC, Feese M, Kivitz A, King C, Shergy W, Kent J, Peloso PM, Danila MI, Saag KG. Reducing immunogenicity of pegloticase with concomitant use of mycophenolate mofetil in patients with refractory gout: a phase II, randomized, double-blind, placebo-controlled trial. Arthritis & Rheumatology. 2021;73(8):1523–32. https://doi.org/10.1002/art.41731.
Klück V CG, Mies L, Bukkems F, van Emst L, Bakker R, van Caam A; HINT consortium; Crişan TO, Joosten LAB. TGF-β is elevated in hyperuricemic individuals and mediates urate-induced hyperinflammatory phenotype in human mononuclear cells. Arthritis research & therapy. 2023;25(1). https://doi.org/10.1186/s13075-023-03001-1.
Ma T, Liu X, Cen Z, Xin C, Guo M, Zou C, et al. MicroRNA-302b negatively regulates IL-1β production in response to MSU crystals by targeting IRAK4 and EphA2. Arthritis research & therapy. 2018;20(1):34. https://doi.org/10.1186/s13075-018-1528-9.
Mirzaesmaeili A, Zangiabadi S, Raspanti J, Akram A, Inman RD, Abdul-Sater AA. Cutting edge: negative regulation of inflammasome activation by TRAF1 can limit gout. J Immunol. 2023. https://doi.org/10.4049/jimmunol.2200465.
Elsaid K, Merriman TR, Rossitto LA, Liu-Bryan R, Karsh J, Phipps-Green A, et al. Amplification of inflammation by lubricin deficiency implicated in incident, erosive gout independent of hyperuricemia. Arthritis & rheumatology (Hoboken, NJ). 2022. https://doi.org/10.1002/art.42413.
Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy. 2008;28(4):437–43. https://doi.org/10.1592/phco.28.4.437.
Harrold LR, Andrade SE. Medication adherence of patients with selected rheumatic conditions: a systematic review of the literature. Seminars in arthritis and rheumatism. 2009;38(5):396–402. https://doi.org/10.1016/j.semarthrit.2008.01.011.
Doherty M, Jenkins W, Richardson H, Sarmanova A, Abhishek A, Ashton D, et al. Efficacy and cost-effectiveness of nurse-led care involving education and engagement of patients and a treat-to-target urate-lowering strategy versus usual care for gout: a randomised controlled trial. Lancet (London, England). 2018;392(10156):1403–12. https://doi.org/10.1016/s0140-6736(18)32158-5.
Fields TR, Batterman A. How can we improve disease education in people with gout? Current Rheumatol Rep. 2018;20(3):12. https://doi.org/10.1007/s11926-018-0720-x.
Fields JK, Günther S, Sundberg EJ. Structural basis of IL-1 family cytokine signaling. Front Immunol. 2019;10:1412. https://doi.org/10.3389/fimmu.2019.01412.
Lopez-Castejon G, Brough D. Understanding the mechanism of IL-1β secretion. Cytokine Growth Factor Rev. 2011;22(4):189–95. https://doi.org/10.1016/j.cytogfr.2011.10.001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
TF disclosures are as follows: Horizon Pharmaceuticals (payment for consulting on gout exhibit), Avion Pharmaceuticals (Advisory Board), and Novartis Pharmaceuticals (payment for consultation). Authors KY, LY, and GB declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Summary Points
• Current and future investigations into oral formulations and more proximal inflammasome pathway modulation for acute gout flares are of great research interest, as are further studies into IL-1β blocking agents.
• The combination uricase/immunosuppressive SEL-212 avoids the need for co-administration with methotrexate or other immunosuppressants to reduce the formation of neutralizing ADAs and maintain urate-lowering efficacy. Monthly infusion dosing is another potential advantage.
• Bioengineered uricase ALLN-346 is positioned to take advantage of the intestinal uric acid excretion pathway and may prove especially useful in patients with CKD. Oral administration is an advantage, and early studies showed a lack of adverse reactions.
• Tigulixostat is a selective xanthine oxidase inhibitor with effective sUA lowering capabilities at even moderate dose which may be easier to titrate than existing agents.
• The URAT1 agent dotinurad has promise as a monotherapy, possibly without significant renal problems, and could be effective even in mild CKD.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yip, K., Braverman, G., Yue, L. et al. Pipeline Therapies for Gout. Curr Rheumatol Rep 26, 69–80 (2024). https://doi.org/10.1007/s11926-023-01128-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-023-01128-3