Abstract
Objectives
Arthritis is a common clinical manifestation of hereditary hemochromatosis (HH), and HH is one of a handful of conditions linked to calcium pyrophosphate deposition (CPPD) in joints. The connection between these two types of arthritis has not yet been fully elucidated. In light of new pathogenic pathways recently implicated in CPPD involving bone, we reviewed the literature on the etiology of hemochromatosis arthropathy (HHA) seeking shared pathogenic mechanisms.
Results
Clinical observations reinforce striking similarities between HHA and CPPD even in the absence of CPP crystals. They share a similar joint distribution, low grade synovial inflammation, and generalized bone loss. Excess iron damages chondrocytes and bone cells in vitro. While direct effects of iron on cartilage are not consistently seen in animal models of HH, there is decreased osteoblast alkaline phosphatase activity, and increased osteoclastogenesis. These abnormalities are also seen in CPPD. Joint repair processes may also be impaired in both CPPD and HHA.
Conclusions
Possible shared pathogenic pathways relate more to bone and abnormal damage/repair mechanisms than direct damage to articular cartilage. While additional work is necessary to fully understand the pathogenesis of arthritis in HH and to firmly establish causal links with CPPD, this review provides some plausible hypotheses explaining the overlap of these two forms of arthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hereditary hemochromatosis (HH) is a relatively common genetic disorder of iron metabolism with variable penetrance. End-organ damage in HH is typically attributed to increased intestinal iron absorption and decreased hepcidin levels resulting in iron deposition in tissues. The liver, pancreas, heart, and pituitary gland are common sites of damage. Risk factors for clinically important manifestations of HH include advanced age, male sex, high dietary iron intake, and pre-existing or concurrent tissue damage. The most common genetic mutation causing HH is the C282Y mutation in the HFE gene. HH is one of the strongest known associations with calcium pyrophosphate crystal deposition (CPPD). CPPD occurs in 20–30% of patients with HH [1, 2]. After several decades of observation and experimental attempts to clarify the process, the link between these two diseases remains unexplained. Here, we will discuss the shared clinical features of hemochromatosis arthropathy (HHA) and CPPD, describe the existing theories of CPPD pathogenesis, and review the current understanding of HHA pathogenesis. The purpose of this review is to delineate potential pathogenic pathways common to both types of arthritis.
Shared Clinical Overlap Between HHA and CPPD
HHA shares important clinical features with CPPD even without evidence of CPP crystal deposition, and both of these types of arthritis have features which distinguish them from the most common type of degenerative arthritis, osteoarthritis (OA) (Table 1). The patterns of joint involvement in HHA and CPPD are nearly identical and involve sites that are not commonly affected by primary OA, such as the 2nd and 3rd metacarpophalangeal (MCP) joints. Larger joints such as wrists and shoulders are also involved. Increased but mild inflammation in the synovium distinguishes HHA synovial tissue from that of OA [3], and low-grade inflammation is also present in CPPD, with higher blood cell counts in synovial fluids of joints with CPPD compared to OA even in the absence of acute CPP crystal arthritis [4, 5]. Most CPPD occurs sporadically in patients over the age of 60 but is also associated with a handful of seemingly unrelated conditions including hypophosphatasia, hyperparathyroidism, and hypomagnesemia. Reversal of these secondary causes in CPPD and iron removal in HHA does not ameliorate the disease. In fact, reduction of iron has been shown to have no beneficial effects on symptoms and may actually worsen joint pain [6, 7]. Treatment of both these forms of arthritis currently focuses on controlling symptoms.
Interestingly, both diseases share a similar bone phenotype. Patients demonstrate osteopenia and osteoporosis more commonly than age and sex matched controls. Guggenbuhl in 2005 reported that of 38 men with HH and confirmed iron overload by liver biopsy, 79% had osteopenia and 34% had osteoporosis as measured by DXA [8]. Similar results were shown by Valenti et al. in 2009, although Nguyen [2] reported lower frequency of osteoporosis [2, 9]. In CPPD, increased rates of osteopenia and osteoporosis were noted in two large cross-sectional studies of CPPD patients [10, 11]
Current Theories of CPPD Pathogenesis
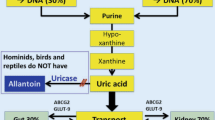
While the pathogenesis of CPPD is not fully understood, current data support the existence of two overarching and intertwined theories. The first and best experimentally supported theory is that CPPD begins in articular cartilage due to the overproduction of inorganic pyrophosphate (PPi) by chondrocytes. Excess PPi complexes with extracellular calcium from synovial fluid form CPP crystals in the pericellular matrix. CPP crystals then induce synovial inflammation, damage the surrounding cartilage, and alter joint biomechanics to produce arthritis. The best clinical examples of such a mechanism are gain-of-function mutations in the ANKH protein seen in some cases of familial CPPD. ANKH is present in normal chondrocytes, and ANKH gain of function increases levels of the PPi precursor, ATP in cartilage [12].
The second theory is based on the recent discovery that a loss of function mutation in the gene that codes for osteoprotegerin (OPG) accounts for multiple kindred with familial CPPD [13]. However, a neither mutant or wild-type OPG nor its cognate ligands affected CPP crystal formation or cartilage PPi production [14]. This shifted attention to the role of mutant OPG in bone homeostasis. This OPG mutation permits excess RANKL-mediated osteoclast formation in bone [13]. Excess osteoclasts in subchondral bone may release factors into cartilage, such as TGFβ, which mediate joint destruction [15]. TGFβ is also a potent inducer of increased PPi production in cartilage [16], and this results in CPP crystal formation and further exacerbates joint damage. Bone abnormalities in CPPD are further supported by the observations that (1) there is increased risk of osteoporosis in sporadic CPPD; (2) there are abnormal bone phenotypes associated with other risk factors for CPPD such as hypophosphatasia and hyperparathyroidism; and (3) there is abundant evidence for a critical role of bone in other forms of degenerative arthritis [17,18,19]. Aging and injury, which are common risk factors for sporadic CPPD, likely affect both cartilage and bone. For example, ANKH levels increase with age in cartilage, as does osteoclast activity and aggressive bone resorption [20, 21].
Work Directly Exploring the Link Between HHA and CPPD
To date, relatively few studies address the causal links between HH and CPPD. Most of this early work sought to implicate iron in processes important for CPPD. Two groups postulated a direct role for iron in CPP mineral formation. The presence of ferric or ferrous ions in solution or in gel models of CPP crystal formation demonstrated a complex effect. Iron both interfered with [22] and enhanced crystal formation [23]. Early papers speculated that iron might decrease CPP crystal dissolution, but there is little evidence for this experimentally [1, 24], nor is it easily supported clinically as removal of iron does not ameliorate CPPD in HHA. Ryan et al. found no effects of either ferrous or ferric salts on levels of chondrocyte extracellular pyrophosphate (PPi) although significant cell toxicity was observed [25].
Current Theories of HHA Pathogenesis that Share Features with Those of CPPD Pathogenesis
For many years, all types of degenerative arthritis were attributed to primary articular cartilage damage. It follows logically that HHA was felt to occur due to iron detrimental actions on chondrocyte/cartilage homeostasis, and that aging produces parallel processes in cartilage promoting CPPD. Indeed, much of the work in HHA investigated the direct cellular toxicity of iron on cartilage. In studies of HHA patients, there is little consistent evidence that iron deposits in cells or extracellular matrix of articular cartilage [26, 27], and CPP crystals are not physically associated with iron deposits [28]. Murine models of HH based on HFE deficiency show iron deposition in subchondral bone and synovium, but iron is often absent from articular cartilage [29, 30]. Fe has well known toxic effects on cells and increases ROS through the Fenton reaction. Not surprisingly, in vitro exposure of chondrocytes, osteoblasts, and osteocytes to high level of iron decreases cell viability [31,32,33,34]. In CPPD, chondrocyte senescence associated with advanced age may play a similar role to iron [35].
Both CPPD and HHA share moderately increased synovial inflammation compared to OA. Synovial inflammation can certainly contribute to joint damage, impede repair after injury, and contribute to degenerative arthritis [36]. In HHA, human and murine studies confirm the presence of iron deposits in synovial tissue with iron overload. Direct effects of iron on synovial tissues have not been well studied in HHA. In one study of synovial tissue from a hemophilia patient with iron deposition, ex vivo cultures showed increased production of Il-6, TNFα, and other inflammatory cytokines compared to normal synovial tissue [37]. CPPD synovium also shows more inflammation in certain settings [38]. Certainly ATP, a critical precursor of extracellular PPi which is increased in joints affected by CPPD [39] can induce IL-1β production by macrophages through the P2X7 receptor activation [40] and also induces inflammation in other cell types through its action as a DAMP [41].
Joint damage and/or deficient repair processes may contribute to both HHA and CPPD. A longstanding theory of many types of degenerative arthritis is that arthritis stems from a lifetime of minor and major injuries followed by ineffective repair. Injury is a major risk factor for CPPD as illustrated by the dramatic increase in CPPD in damaged menisci compared to undamaged menisci [42]. In a murine joint injury model, Camacho et al. showed that HFE-deficient mice developed more severe injury-induced OA than wild type mice [30]. A critical role for defective repair processes is further supported in HHA by studies of HFE deficient mice which show no spontaneous arthritis up to 12 months of age [29]. Iron may also impede joint repair [43]. Ample evidence exists for deficiencies in joint repair processes with advanced age that may explain the association of age with CPPD [44].
There is increasing attention to the role of bone in joint injury and repair which may be important in both CPPD and HHA. The mechanisms through which HH produces bone loss remain unclear. There is literature supporting the notion that HH bone disease results from a direct effect of iron on osteoclastogenesis [45,46,47,48] and subsequent excess bone resorption [46]. A slightly smaller number of studies fail to show enhanced osteoclast differentiation with iron exposure [49, 50] or genetic manipulation [51, 52]. Two seminal studies examining bone in HFE deficient mice showed progressive osteopenia with age [53, 54]. One study attributed this to enhanced osteoclastogenesis while the second attributed it to defective osteoblast function and thus reduced mineral formation. Another recent study by Yang (34) suggested that iron-induced osteocyte apoptosis provided a rich source of RANKL for osteoclast formation and subsequent bone resorption [34].
Increased osteoclast activity can worsen joint injury and impede repair. Multiple studies demonstrate that one of the earliest findings in degenerative arthritis, for example, is an increase in the number of subchondral osteoclasts [18, 44]. It is logical that subchondral bone instability resulting from aggressive destruction of the cartilage/bone interface may contribute to cartilage microcracks and accelerate joint damage. Osteoblasts and osteocytes may also contribute to arthritis either through their ability to regulate osteoclast-mediated bone resorption or through other actions [17]. A loss of function mutation in osteoprotegerin, resulting in increased OC activity, has recently been identified as a cause of familial CPPD as described above [13]. The delicate balance between bone formation and bone resorption in both HHA and CPPD is clearly a shared mechanism that warrants further study.
A key regulator of PPi levels in bone and cartilage is tissue non-specific alkaline phosphatase (TNAP). TNAP hydrolyzes PPi and hypophosphatasia, which results from a congenital deficiency of TNAP, increases the risk of CPPD by raising PPi levels in bone and cartilage. Bone levels of TNAP are dysregulated in both HHA and CPPD. Osteoblasts account for a large percentage of bone TNAP which is essential to normal bone matrix mineralization. Interestingly, multiple studies of osteoblasts show decreased TNAP activity resulting from treatment with iron [55,56,57,58,59]. Iron may also affect osteoblast-mediated bone mineral formation. Human bone marrow stromal cells treated with ferrous sulfate demonstrated attenuation of bone mineralization and osteoblastogenesis in one study [60], while other studies found no such affect [47]. The effects of iron on osteocyte alkaline phosphatase remain unclear.
Other Theories
HFE may have additional functions independent of its iron-regulating properties that produce or are shared with CPPD. HFE is a membrane protein with similarities to major histocompatibility complex (MHC)-class I proteins. Studies of patients carrying HFE mutations but without clinical evidence of iron overload show a propensity for hand OA patterns that mimic HHA and CPPD, such as predominant involvement of the MCPs. This observation has raised questions about whether iron mediates joint damage or whether some other function of HFE may be involved. The best of these studies positively correlates MCP-predominant hand OA with the C282Y HFE mutation [61], but there are limitations in the study design. In another study, patients with idiopathic CPPD were screened for C282Y [62, 63], but no differences in gene frequencies were found in the CPPD group compared to random controls.
HFE binds β2-microglobulin [64], which is present in musculoskeletal tissues and has important effects on bone [65] and anti-anabolic effects on chondrocytes [66]. It is not known whether loss of function mutations in HFE alter β2 microglobulin levels in musculoskeletal tissues. Interestingly, β2-microglobulin is the protein involved in dialysis-related amyloid deposits, and amyloid has been noted around CPP crystals in cartilage [67, 68]. In addition, factors such as FGF23, which can be regulated along with iron and regulate pathologic calcification in many tissues [69], may also play a role in both conditions.
Summary
In summary, current evidence supports the existence of certain shared pathogenic pathways in HHA and CPPD which may explain their clinical overlap. There may be a role for synovial inflammation in both diseases. There is some experimental evidence for abnormal joint damage/repair processes in HHA and good clinical support for similar processes in CPPD. While there is a paucity of evidence for a direct effect of iron exposure on cartilage in HHA, altered bone metabolism particularly related to increased osteoclastogenesis is supported clinically and experimentally in both diseases. Further work in this area is clearly needed, but elucidation of these pathogenic mechanisms may eventually identify potential therapeutic targets for both types of arthritis.
References
Dymock IW, Hamilton EB, Laws JW, Williams R. Arthropathy of haemochromatosis. Clinical and radiological analysis of 63 patients with iron overload. Ann Rheum Dis. 1970;29(5):469–476.
Nguyen CD, Morel V, Pierache A, Lion G, Cortet B, Flipo RM, et al. Bone and joint complications in patients with hereditary hemochromatosis: a cross-sectional study of 93 patients. Ther Adv Musculoskelet Dis. 2020;12:1759720x20939405.
Schumacher HR Jr. Hemochromatosis and arthritis. Arthritis Rheum. 1964;7:41–50.
Frischknecht J, Steigerwald JC. High synovial fluid white blood cell counts in pseudogout: possible confusion with septic arthritis. Arch Intern Med. 1975;135(2):298–9.
Martínez Sanchis A, Pascual E. Intracellular and extracellular CPPD crystals are a regular feature in synovial fluid from uninflamed joints of patients with CPPD related arthropathy. Ann Rheum Dis. 2005;64(12):1769–72.
Richette P, Eymard C, Deberg M, Vidaud D, de Kerguenec C, Valla D, et al. Increase in type II collagen turnover after iron depletion in patients with hereditary haemochromatosis. Rheumatology (Oxford, England). 2010;49(4):760–6.
Sandhu K, Flintoff K, Chatfield MD, Dixon JL, Ramm LE, Ramm GA, et al. Phenotypic analysis of hemochromatosis subtypes reveals variations in severity of iron overload and clinical disease. Blood. 2018;132(1):101–10.
Guggenbuhl P, Deugnier Y, Boisdet JF, Rolland Y, Perdriger A, Pawlotsky Y, et al. Bone mineral density in men with genetic hemochromatosis and HFE gene mutation. Osteoporos Int. 2005;16(12):1809–14.
Valenti L, Varenna M, Fracanzani AL, Rossi V, Fargion S, Sinigaglia L. Association between iron overload and osteoporosis in patients with hereditary hemochromatosis. Osteoporos Int. 2009;20(4):549–55.
KleiberBalderrama C, Rosenthal AK, Lans D, Singh JA, Bartels CM. Calcium pyrophosphate deposition disease and associated medical comorbidities: a national cross-sectional study of US Veterans. Arthritis Care Res. 2017;69(9):1400–6.
Abhishek A, Doherty M. Update on calcium pyrophosphate deposition. Clin Exp Rheumatol. 2016;34(4 Suppl 98):32–8.
Pendleton A, Johnson MD, Hughes A, Gurley KA, Ho AM, Doherty M, et al. Mutations in ANKH cause chondrocalcinosis. Am J Hum Genet. 2002;71(4):933–40.
Mitton-Fitzgerald E, Gohr CM, Williams CJ, Ortiz A, Mbalaviele G, Rosenthal AK. Effects of the TNFRSF11B mutation associated with calcium pyrophosphate deposition disease in osteoclastogenesis in a murine model. Arthritis Rheumatol (Hoboken, NJ). 2021;73(8):1543–9.
Williams CJ, Qazi U, Bernstein M, Charniak A, Gohr C, Mitton-Fitzgerald E, et al. Mutations in osteoprotegerin account for the CCAL1 locus in calcium pyrophosphate deposition disease. Osteoarthr Cartil. 2018;26(6):797–806.
Zhen G, Wen C, Jia X, Li Y, Crane JL, Mears SC, et al. Inhibition of TGF-β signaling in mesenchymal stem cells of subchondral bone attenuates osteoarthritis. Nat Med. 2013;19(6):704–12.
Rosenthal AK, Cheung HS, Ryan LM. Transforming growth factor beta 1 stimulates inorganic pyrophosphate elaboration by porcine cartilage. Arthritis Rheum. 1991;34(7):904–11.
Hu W, Chen Y, Dou C, Dong S. Microenvironment in subchondral bone: predominant regulator for the treatment of osteoarthritis. Ann Rheum Dis. 2020;80(4):413–22.
Bertuglia A, Lacourt M, Girard C, Beauchamp G, Richard H, Laverty S. Osteoclasts are recruited to the subchondral bone in naturally occurring post-traumatic equine carpal osteoarthritis and may contribute to cartilage degradation. Osteoarthr Cartil. 2016;24(3):555–66.
Löfvall H, Newbould H, Karsdal MA, Dziegiel MH, Richter J, Henriksen K, et al. Osteoclasts degrade bone and cartilage knee joint compartments through different resorption processes. Arthritis Res Ther. 2018;20(1):67.
Johnson K, Terkeltaub R. Upregulated ank expression in osteoarthritis can promote both chondrocyte MMP-13 expression and calcification via chondrocyte extracellular PPi excess. Osteoarthr Cartil. 2004;12(4):321–35.
Møller AMJ, Delaissé J-M, Olesen JB, Madsen JS, Canto LM, Bechmann T, et al. Aging and menopause reprogram osteoclast precursors for aggressive bone resorption. Bone Res. 2020;8(1):27.
Cheng PT, Pritzker KP. Ferrous [Fe++] but not ferric [Fe] ions inhibit de novo formation of calcium pyrophosphate dihydrate crystals: possible relationships to chondrocalcinosis and hemochromatosis. J Rheumatol. 1988;15(2):321–4.
Mandel GS, Halverson PB, Mandel NS. Calcium pyrophosphate crystal deposition: the effect of soluble iron in a kinetic study using a gelatin matrix model. Scan Microsc. 1988;2(2):1177–88.
Brighton CT, Bigley EC Jr, Smolenski BI. Iron-induced arthritis in immature rabbits. Arthritis Rheum. 1970;13(6):849–57.
Ryan LM, Kurup I, Rosenthal AK, McCarty DJ. Stimulation of inorganic pyrophosphate elaboration by cultured cartilage and chondrocytes. Arch Biochem Biophys. 1989;272(2):393–9.
Axford JS, Bomford A, Revell P, Watt I, Williams R, Hamilton EB. Hip arthropathy in genetic hemochromatosis. Radiographic and histologic features. Arthritis Rheum. 1991;34(3):357–361.
Walker RJ, Dymock IW, Ansell ID, Hamilton EB, Williams R. Synovial biopsy in haemochromatosis arthropathy. Histological findings and iron deposition in relation to total body iron overload. Ann Rheum Dis. 1972;31(2):98–102.
Faraawi R, Harth M, Kertesz A, Bell D. Arthritis in hemochromatosis. J Rheumatol. 1993;20(3):448–52.
Simão M, Gavaia PJ, Camacho A, Porto G, Pinto IJ, Ea HK, et al. Intracellular iron uptake is favored in Hfe-KO mouse primary chondrocytes mimicking an osteoarthritis-related phenotype. BioFactors (Oxford, England). 2019;45(4):583–97.
Camacho A, Simão M, Ea HK, Cohen-Solal M, Richette P, Branco J, et al. Iron overload in a murine model of hereditary hemochromatosis is associated with accelerated progression of osteoarthritis under mechanical stress. Osteoarthr Cartil / OARS, Osteoarthritis Research Society. 2016;24(3):494–502.
Yao X, Sun K, Yu S, Luo J, Guo J, Lin J, et al. Chondrocyte ferroptosis contribute to the progression of osteoarthritis. J Orthop Transl. 2021;27:33–43.
Ferreira AV, Duarte TL, Marques S, Costa P, Neves SC, dos Santos T, et al. Iron triggers the early stages of cartilage degeneration in vitro: the role of articular chondrocytes. Osteoarthr Cartil Open. 2021;3(2):100145.
Lertsuwan K, Nammultriputtar K, Nanthawuttiphan S, Tannop N, Teerapornpuntakit J, Thongbunchoo J, et al. Differential effects of Fe2+ and Fe3+ on osteoblasts and the effects of 1,25(OH)2D3, deferiprone and extracellular calcium on osteoblast viability under iron-overloaded conditions. PLoS One. 2020;15(5):e0234009.
Yang J, Dong D, Luo X, Zhou J, Shang P, Zhang H. Iron overload-induced osteocyte apoptosis stimulates osteoclast differentiation through increasing osteocytic RANKL production in vitro. Calcif Tissue Int. 2020;107(5):499–509.
Meyer F, Dittmann A, Kornak U, Herbster M, Pap T, Lohmann CH, et al. Chondrocytes from osteoarthritic and chondrocalcinosis cartilage represent different phenotypes. Front Cell Dev Biol. 2021;9:622287.
Griffin TM, Scanzello CR. Innate inflammation and synovial macrophages in osteoarthritis pathophysiology. Clin Exp Rheumatol. 2019;37 Suppl 120(5):57–63.
Roosendaal G, Vianen ME, Wenting MJ, van Rinsum AC, van den Berg HM, Lafeber FP, et al. Iron deposits and catabolic properties of synovial tissue from patients with haemophilia. J Bone Joint Surg Br Vol. 1998;80(3):540–5.
Pang L, Hayes CP, Buac K, Yoo DG, Rada B. Pseudogout-associated inflammatory calcium pyrophosphate dihydrate microcrystals induce formation of neutrophil extracellular traps. J Immunol (Baltimore, Md: 1950). 2013;190(12):6488–6500.
Ryan LM, Rachow JW, McCarty DJ. Synovial fluid ATP: a potential substrate for the production of inorganic pyrophosphate. J Rheumat. 1991;18(5):716–20.
Mortaz E, Adcock IM, Shafei H, Masjedi MR, Folkerts G. Role of P2X7 receptors in release of IL-1β: a possible mediator of pulmonary inflammation. Tanaffos. 2012;11(2):6–11.
Rosenthal AK, Gohr CM, Mitton-Fitzgerald E, Lutz MK, Dubyak GR, Ryan LM. The progressive ankylosis gene product ANK regulates extracellular ATP levels in primary articular chondrocytes. Arthritis Res Ther. 2013;15(5):R154.
Doherty M, Watt I, Dieppe PA. Localised chondrocalcinosis in post-meniscectomy knees. Lancet (London, England). 1982;1(8283):1207–10.
Wright JA, Richards T, Srai SK. The role of iron in the skin and cutaneous wound healing. Front Pharmacol. 2014;5:156.
Geurts J, Nasi S, Distel P, Müller-Gerbl M, Prolla TA, Kujoth GC, et al. Prematurely aging mitochondrial DNA mutator mice display subchondral osteopenia and chondrocyte hypertrophy without further osteoarthritis features. Sci Rep. 2020;10:1296
Zhang P, Wang S, Wang L, Shan BC, Zhang H, Yang F, et al. Hepcidin is an endogenous protective factor for osteoporosis by reducing iron levels. J Mol Endocrinol. 2018;60(4):297–306.
Jia P, Xu YJ, Zhang ZL, Li K, Li B, Zhang W, et al. Ferric ion could facilitate osteoclast differentiation and bone resorption through the production of reactive oxygen species. J Orthop Res. 2012;30(11):1843–52.
Li J, Hou Y, Zhang S, Ji H, Rong H, Qu G, et al. Excess iron undermined bone load-bearing capacity through tumor necrosis factor-α-dependent osteoclastic activation in mice. Biomed Rep. 2013;1(1):85–8.
Wang X, Chen B, Sun J, Jiang Y, Zhang H, Zhang P, et al. Iron-induced oxidative stress stimulates osteoclast differentiation via NF-κB signaling pathway in mouse model. Metabolism. 2018;83:167–76.
Li Y, Bai B, Zhang Y. Expression of iron-regulators in the bone tissue of rats with and without iron overload. Biometals. 2018;31(5):749–57.
Xie W, Lorenz S, Dolder S, Hofstetter W. Extracellular iron is a modulator of the differentiation of osteoclast lineage cells. Calcif Tissue Int. 2016;98(3):275–83.
Ledesma-Colunga MG, Baschant U, Fiedler IAK, Busse B, Hofbauer LC, Muckenthaler MU, et al. Disruption of the hepcidin/ferroportin regulatory circuitry causes low axial bone mass in mice. Bone. 2020;137:115400.
Yang Q, Jian J, Abramson SB, Huang X. Inhibitory effects of iron on bone morphogenetic protein 2-induced osteoblastogenesis. J Bone Miner Res. 2011;26(6):1188–96.
Guggenbuhl P, Fergelot P, Doyard M, Libouban H, Roth MP, Gallois Y, et al. Bone status in a mouse model of genetic hemochromatosis. Osteoporos Int. 2011;22(8):2313–9.
Doyard M, Chappard D, Leroyer P, Roth MP, Loréal O, Guggenbuhl P. Decreased bone formation explains osteoporosis in a genetic mouse model of hemochromatosiss. PLoS One. 2016;11(2):e0148292.
Zhao GY, Zhao LP, He YF, Li GF, Gao C, Li K, et al. A comparison of the biological activities of human osteoblast hFOB1.19 between iron excess and iron deficiency. Biol Trace Elem Res. 2012;150(1-3):487–495.
Yamasaki K, Hagiwara H. Excess iron inhibits osteoblast metabolism. Toxicol Lett. 2009;191(2–3):211–5.
Zarjou A, Jeney V, Arosio P, Poli M, Zavaczki E, Balla G, et al. Ferritin ferroxidase activity: a potent inhibitor of osteogenesis. J Bone Miner Res. 2010;25(1):164–72.
Jiang Y, Yan Y, Wang X, Zhu G, Xu YJ. Hepcidin inhibition on the effect of osteogenesis in zebrafish. Biochem Biophys Res Commun. 2016;476(1):1–6.
Morais S, Carvalho GS, Faria JL, Gomes HT, Sousa JP. In vitro biomineralization by osteoblast-like cells. II. Characterization of cellular culture supernatants. Biomaterials. 1998;19(1-3):23–29.
Balogh E, Tolnai E, Nagy B, Nagy B, Balla G, Balla J, et al. Iron overload inhibits osteogenic commitment and differentiation of mesenchymal stem cells via the induction of ferritin. Biochim Biophys Acta (BBA) Mol Basis Dis. 2016;1862(9):1640–1649.
Ross JM, Kowalchuk RM, Shaulinsky J, Ross L, Ryan D, Phatak PD. Association of heterozygous hemochromatosis C282Y gene mutation with hand osteoarthritis. J Rheumatol. 2003;30(1):121–5.
Timms AE, Sathananthan R, Bradbury L, Athanasou NA, Wordsworth BP, Brown MA. Genetic testing for haemochromatosis in patients with chondrocalcinosis. Ann Rheum Dis. 2002;61(8):745–7.
Jordan JM. Arthritis in hemochromatosis or iron storage disease. Curr Opin Rheumatol. 2004;16(1):62-6.
Barton JC, Edwards CQ, Acton RT. HFE gene: structure, function, mutations, and associated iron abnormalities. Gene. 2015;574(2):179–92.
Menaa C, Esser E, Sprague SM. Beta2-microglobulin stimulates osteoclast formation. Kidney Int. 2008;73(11):1275–81.
Zhang H, Liew CC, Marshall KW. Microarray analysis reveals the involvement of beta-2 microglobulin (B2M) in human osteoarthritis. Osteoarthr Cartil / OARS, Osteoarthritis Research Society. 2002;10(12):950–60.
Egan MS, Goldenberg DL, Cohen AS, Segal D. The association of amyloid deposits and osteoarthritis. Arthritis Rheum. 1982;25(2):204–8.
Doherty M. Pyrophosphate arthropathy--recent clinical advances. Ann Rheum Dis. 1983;42 Suppl 1(Suppl 1):38–44.
Edmonston D, Wolf M. FGF23 at the crossroads of phosphate, iron economy and erythropoiesis. Nat Rev Nephrol. 2020;16(1):7–19.
Funding
This work was partially supported by a VA Merit Review Grant I01BX004454 (AKR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Crystal Arthritis
Rights and permissions
About this article
Cite this article
Mitton-Fitzgerald, E., Gohr, C.M., Williams, C.M. et al. Identification of Common Pathogenic Pathways Involved in Hemochromatosis Arthritis and Calcium Pyrophosphate Deposition Disease: a Review. Curr Rheumatol Rep 24, 40–45 (2022). https://doi.org/10.1007/s11926-022-01054-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-022-01054-w