Abstract
Purpose of Review
We lack evidence-based data for the treatment of childhood-onset Takayasu arteritis (c-TA) since it is a rare disease in children. In this systematic literature review, we aimed to evaluate the treatment choices in c-TA patients and integrate our experience for the treatment of our patients in the recent years/in the biologic era.
Recent Findings
We reviewed 24 articles addressing treatments of 413 c-TA patients. Steroids were given to 352 patients (85.2%) as the main immunosuppressive therapy. Other immunosuppressive agents included methotrexate (37.3%), cyclophosphamide (24.5%), azathioprine (16.9%), and mycophenolate mofetil (7.9%). Besides, various biological agents were used, including tumor necrosis factor-alpha inhibitors in 70 of 107 c-TA patients (65.4%) and interleukin-6 inhibitors in 33 of them (30.8%). Biologics are increasingly used in our center as well. Even in severe patients, CYC is switched to either anti-TNF or antiIL6 once disease control is achieved.
Summary
Recently, in addition to conventional immunosuppressants, biologics are increasingly used in c-TA. We have revised our treatment protocol to start with 1–3 doses of high-dose steroids and CYC, in a child with TA with types III–V involvement and high acute phase reactants; once clinical features subside and CRP normalizes, biologics should be started to replace CYC while decreasing the steroid dose.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
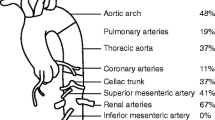
Takayasu arteritis (TA) is a chronic granulomatous, inflammatory disease of the aorta and its major branches at their origin [1]. TA is characterized by dilatation, occlusion, stenosis, or aneurysm formation of the affected arteries [2]. The childhood-onset TA (c-TA) subset affects any age group, from young infants to late adolescents [3, 4].
The findings range from systemic nonspecific symptoms, such as malaise, myalgia, weight loss, and fever, to vascular and ischemic manifestations, such as stroke, syncope, limb claudication, pulselessness, hypertension, and vascular bruit [5, 6]. Although hypertension is the most common form of presentation in children and adults, the overall clinical spectrum at the presentation of children with TA may differ from that in adults [3, 4, 7].
The Ankara 2008 criteria used in classification for pediatric patients were endorsed by the European League Against Rheumatism (EULAR), the International Trials of Pediatric Rheumatology (PRINTO), and the European Association of Pediatric Rheumatology (PRES) [1, 8•]. However, diagnostic delay in children is typical and almost certainly contributes to worse outcomes [9].
Although TA is suggested to be the third most common vasculitis in children, management is challenging because of the delay in diagnosis and difficulty assessing disease activity. Studies on the management of TA patients are rare and different approaches are available. Adequate therapy in c-TA is essential to prevent irreversible vessel damage with the resulting insufficiency of vital organs. Ongoing evidence reveals that biological therapies could be effectively used in refractory cases or even in first-line management. The aim of this paper is to systemically review the literature to evaluate the treatment options in c-TA patients. We also aimed to analyze our treatment approach in c-TA patients in the recent years, along with the relevant literature. As a secondary objective, we have compared the outcome (activity index) of the c-TA patients in our center before and after the use of biologics.
Methods
Protocol for Systematic Review
This systematic review was reported by the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [10].
Search Strategy
We reviewed the literature using Pubmed/MEDLINE and Scopus between January 1, 1990, to January 31, 2021, combining the following keywords: “Takayasu arteritis,” “Takayasu disease,” “large vessel arteritis,” “aortic arch syndromes,” “arteritis brachiocephalica,” “occlusive thromboaortopathy,” “pulseless disease,” “young female arteritis,” “brachiocephalic ischemia,” “idiopathic arteritis of Takayasu,” and “reverse coarctation.” We restricted our research to English articles. Case reports, original research articles, editorials, and review articles about TA were analyzed. The articles, which include data about the treatment of patients with c-TA, have been included in the final analysis. Two reviewers (OB, SS) performed the literature searches independently based on inclusion and exclusion criteria, deleting irrelevant literature, abandoning duplications, and screening titles and abstracts.
Inclusion and Exclusion Criteria
Inclusion criteria were set in the literature about c-TA patients’ treatment, including randomized controlled trials (RCTs), cohort study, case series, case report, review, and pilot study. Exclusion criteria were as follows: (1) no information on the treatment of patients with c-TA; (2) animal researches; (3) literature about epidemiology, mechanism, diagnosis (variable biomarkers, radiological techniques, etc.), and evaluation (disease activity, radiological assessment, etc.); and (4) case reports fewer than three cases.
Data Extraction
Two reviewers (OB, SS) independently extracted data from the included studies, including information such as genders, ages, previous and current treatments, relapses, and outcomes. Disagreements between the reviewers were resolved by consensus.
Patients from Our Center
We retrospectively evaluated the medical treatment records of 25 c-TA patients followed between August 2005 and January 2021 at the Pediatric Rheumatology Department of Hacettepe University Faculty of Medicine, Ankara, Turkey. All c-TA patients fulfilled the EULAR/PReS/PRINTO-endorsed Ankara 2008 criteria [8•]. Patients were evaluated in two groups as those who received treatment before and after the date that we started to use biologic drugs to treat TA. Treatment regimens in the disease course were compared between the two groups. Severe disease was defined as types III–V involvement according to the Numano classification of angiographic findings, and all had high acute phase reactants [9].
The activity of TA was assessed with the Indian Takayasu’s Clinical Activity Score (ITAS).
Statistical Analysis
Statistical analysis was performed using SPSS version 23.0 (IBM, Armonk, NY, USA). Quantitative variables are expressed as mean and standard deviation (SD). Student’s T-test was used to compare continuous variables. A p-value of less than 0.05 was considered statistically significant.
Results
Literature Search
The selection process for the studies included in this review is shown in Fig. 1. Electronic searches resulted in 339 articles that were potentially relevant to eliminating duplicates. After excluding studies that did not include case reports (<3 cases) or medical treatment information of c-TA patients, 24 articles meeting the research criteria remained were analyzed in detail.
Medical Treatments in Childhood-Onset Takayasu Arteritis
Clinical characteristics of c-TA patients in the literature are presented in Table 1. We identified 24 articles describing 413 c-TA patients (excluding case series with <3 patients) during our literature search [4, 6, 11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. Two hundred ninety-seven patients were female. The patients’ median age was 12.6 years (range 0.1–18). The median follow-up was of 2.4 years (range 0.1–16).
Detailed treatments for c-TA patients are summarized in Table 2 [4, 6, 11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. Steroids were given to 352 patients (85.2%) as the main immunosuppressive therapy. Other immunosuppressive agents included methotrexate (MTX) (n = 154, 37.3%), cyclophosphamide (CYC) (n = 101, 24.5%), azathioprine (AZA) (n = 70, 16.9%), mycophenolate mofetil (MMF) (n = 33, 7.9%), leflunomide (LEF) (n = 8, 1.9%), and cyclosporine A (CSA) (n = 2, 0.5%). One hundred seventy of 232 c-TA patients (73.3%) received 5-ASA as antiaggregant treatment. The pediatric centers tend to give more aggressive treatment for severe patients; however, severe patients are defined as those with involvement on both sides of the diaphragm and high acute phase reactants.
Biological agents were increasingly used in the treatment of 107 c-TA patients in the last 10 years [4, 6, 15,16,17, 20,21,22, 24,25,26, 27•, 30,31,32]. Seventy (65.4%) of 107 patients received anti-tumor necrosis factor-alpha (TNF-α) therapy [4, 6, 15,16,17, 22, 24,25,26, 30, 32]. Among the anti-TNF-α agents, infliximab (IFX) was often the first choice. Thirty-eight (54.3%) of 70 c-TA patients received IFX, 7 (10%) received adalimumab (ADA), and three patients (4.3%) were treated with etanercept (ETA). Another commonly used biological agent was tocilizumab (TCZ), an anti-interleukin (IL) 6 receptor antibody. Thirty-three c-TA patients (30.8%) were treated with TCZ [4, 20, 21, 25, 26, 27•, 30,31,32]. Three patients received anakinra, which is an anti-IL-1 agent [6], and one patient was treated with rituximab (RTX) [22].
In two studies, a striking feature was the switch between biological agents [4, 11]. In a study by Eleftheriou et al. with 11 c-TA patients, ADA was used in one patient because there was no response to IFX, and TCZ was used in another patient who was unresponsive to ADA [4]. In another study conducted by Filocamo et al., two patients were switched to ADA because there was no response to IFX, and complete remission was achieved with ADA treatment [17].
Eighty-five (28.3%) patients relapsed during follow-up. Two hundred thirty-seven of 357 (66.4%) patients achieved complete remission, and 99 (27.7%) of them were partial responders. Death was reported in 24 (5.8%) of all c-TA patients.
Assessment of Patients from Hacettepe University Department of Pediatric Rheumatology
Twenty-five c-TA patients have been followed up in our Department of Pediatric Rheumatology. Most of the patients were judged to have severe disease since they had types III–V involvement according to the Numano classification, and all had high acute phase reactants. Corticosteroid, the main therapeutic agent of TA treatment, was administered to all patients. MTX was given to 16 patients, CYC to 15, AZA to seven, MMF to one, and LEF to three of our patients.
In recent years, we have started to use biological agents in treating c-TA patients. Until today, we have used biological agents in 18 c-TA patients. These patients initially received two or rarely three doses of CYC and switched to biologics once no new clinical symptoms and inflammatory markers returned to normal. While 13 of our 25 patients received anti-TNF-α treatment, 10 received TCZ. Among the anti-TNF-α agents, we preferred ADA in 12 patients and ETA in one patient.
Due to the progression of MR angiography findings or the persistent elevation in acute phase reactants, biologic agent switch was made between ADA and TCZ in six patients. Four patients were switched from TCZ to ADA treatment, and ADA to TCZ switch was performed in two patients.
We used the Indian Takayasu’s Clinical Activity Score (ITAS-2010) to evaluate disease activity in our c-TA patients [33]. In treatment selection, we applied steroids only or steroids + CYC combination for those with severe disease at the beginning. When acute phase reactants decreased, and disease activity scores (ITAS-2010) returned to normal during follow-up, we switched to biological agent therapy. There was no statistically significant difference in post-treatment disease activity scores (ITAS-2010) between the patients treated with conventional immunosuppressive agents and those switched to biological agents (p = 0.876; mean ITAS-2010 for conventional immunosuppressants and biological agents was 0.5 ± 0.53 and 0.56 ± 0.92 respectively).
Discussion
This systematic literature review suggests that biologic agents are effective alternatives in treating c-TA patients. The primary goal of treatment in c-TA is to prevent complications and disease progression. However, delay in diagnosis due to nonspecific early symptoms continues to be a significant therapeutic challenge. TA leads to significant and sometimes irreversible damage even in the phase before diagnosis [4].
The mainstay of treatment is steroids, with the EULAR 2019 guidelines suggesting high-dose glucocorticoid therapy (40–60 mg/day prednisone-equivalent) for induction of remission in active TA. Adjunctive treatment using tocilizumab was recommended in selected patients (refractory or relapsing disease, presence of an increased risk for glucocorticoid-related adverse events or complications). Moreover, the recommendations suggest the use of non-biological glucocorticoid-sparing agents combined with glucocorticoids in all patients with TA and biological agents in refractory or relapsing patients [34••].
Due to the rarity of the disease in childhood and lack of solid evidence in children, we rely on the adult recommendations for treatment endorsed by EULAR [34••]. On the other hand, children tend to have a more inflammatory disease course. This was reflected in our study comparing pediatric and adult TA patients. A recent study showed that children had a more inflammatory disease, and the use of immunosuppressive drugs and the need for additional immunosuppressive on top of steroids were more common in c-TA compared to adult patients [32].
Although corticosteroids remain the mainstay for remission induction, relapse is frequent during dose tapering, and long-term use of high-dose corticosteroids needs to be avoided in children [35••, 36]. Pediatricians want to spare their growing children from the side effects of high-dose corticosteroids for long periods. Thus steroid-sparing immunosuppressives have been traditionally used in children, which is reflected in this literature review. The aim is to lower the steroid dose while preventing relapse when the steroid dose is reduced or stopped [13]. Therefore, it is recommended to add corticosteroid-sparing agents to the treatment [26, 35••, 36]. The use of immunosuppressant drugs, such as MTX, CYC, AZA, and MMF, has been suggested to be safe and effective, to achieve sustained remission, improve vascular lesions, and decrease steroid dose in c-TA therapy [25, 35••, 36]. CYC is traditionally used in children with extensive or life-threatening disease or critical organ perfusion, whereas MTX, AZA, and MMF are used in less severe cases [37].
After the year 2008, in addition to conventional immunosuppressants, biological agents have been increasingly used in the treatment of adult patients [36, 38]. Several studies have also reported beneficial effects of biological agents on clinical and laboratory responses in patients with c-TA [17, 38]. Their use was included in the recent European consensus-based recommendations [36]. Among biological agents, especially, TNF-α inhibitors (IFX, ADA, ETA) have been used in c-TA treatment, and very successful results have been obtained [4, 6, 15,16,17, 22, 24,25,26, 30, 32]. The largest series reporting on TNF inhibitors in c-TA to date studied 23 children in a combined American–Brazilian cohort [22]. In this study, 11 of 23 c-TA patients were given IFX treatment. Nine out of 16 c-TA patients who received CYC did not respond during follow-up; 6 of them were switched to IFX, and five (83%) subsequently experienced stabilization of disease activity. Seven of the 11 patients who received IFX, including those who switched from CYC (n = 6), responded, while four cases worsened [22]. In another study, Szugye et al. [6] treated two of 21 c-TA patients with only prednisone, 7 of them with MTX and prednisone alone. Biological agents were used in addition to conventional immunosuppressive agents in 10 patients. IFX, which was used in 9 c-TA patients (42.9%), was the most commonly used medication when disease activity was still present despite prednisone and methotrexate use. Besides, ETA was also used in the treatment of two c-TA patients. Complete remission was achieved in 19 patients, and there was partial remission in the other two patients [6].
Serum IL-6 levels of patients with TA have been significantly higher than those of controls and higher in the active disease group than in the stable disease group [39]. Besides its role as a biomarker in TA, IL-6 has profibrotic effects on aortic adventitial fibroblasts, and this stimulation has been demonstrated in TA patients [40]. TCZ has shown promising results as a treatment option for TA in numerous observational studies and subsequent systematic reviews of such studies [41]. In a study by Batu et al. [25] examining the short-term effectiveness of TCZ in c-TA, TCZ treatment was given to a total of 12 patients. TCZ effectively induced remission in all ten patients with refractory c-TA and the remaining two patients who received TCZ as first-line therapy. No recurrence was observed in the patients during the follow-up period, and imaging studies demonstrated vascular improvement in two of these patients and stable disease in four; these patients had been assessed among our patients. In one RCT, the safety and efficacy of TCZ in refractory TA were investigated. Although TCZ failed to meet the primary endpoint, the study results recommended that TCZ was favored over placebo in the per-protocol set. [42, 43••]. Kong et al. [44] evaluated response to treatment with TCZ and CYC in patients with TA and explored the mechanism by analyzing their impact on various cytokines. They found no significant improvement in the vascular stenosis, thickness, and enhancement scores in both groups. However, they showed decreased ESR, CRP level, significantly reduced matrix metalloproteinase (MMP)-9 level, and increased MMP-2 level in the TCZ group than in the CYC group [44]. It should be emphasized that biologic inflammation may be suppressed, and disease activity scores that include acute phase reactants may not be sensitive enough for accurate detection [45, 46]. Consequently, recent data support the use of biologic pathway–targeting agents, such as TNF-α or IL-6 inhibitors, for c-TA patients with critical organ perfusion or end-organ damage at diagnosis and those showing severe, refractory disease [37].
The reflection of the aforementioned literature is evident in our practice as well. Since we have obtained excellent results with our recent treatment strategy in severe patients (types III–V with involvement on both sides of the diaphragm), we now suggest switching CYC to biologic agents in the early phases of the disease and maintaining the remission with low-dose corticosteroids. Thus, in a child with TA with types III–V involvement and high acute phase reactants, which is often the case, two doses — maximum of three — of CYC should accompany the pulse steroid. Once clinical features subside and CRP normalizes, biologics should be started to replace CYC while decreasing the steroid dose.
Different biological agents such as RTX and anakinra have also been used in c-TA patients in a few studies [6, 22]. However, results regarding the post-treatment state of the patients were not reported, and therefore, the place of these agents in c-TA treatment remains unclear. Recent studies have shown that interferon-gamma expression (IFN-γ) is increased in aortic tissue from TA patients with active inflammation [47]. A study conducted on an animal model by Zhang et al. [48] has suggested the efficacy of JAK-STAT signaling inhibition with tofacitinib in suppressing tissue-resident memory T lymphocytes, inhibiting microvascular angiogenesis, and intima proliferation. These data support the notion that JAK inhibitors could be potentially effective in patients with LVV. After that, some clinicians used tofacitinib in refractory TA patients [49,50,51]. Kuwabara et al. [49] had a successful outcome with tofacitinib in an adult patient with TA who did not respond to anti-TNF and anti-IL-6 therapy. In another case report [51], complete remission was achieved with tofacitinib in an adult TA patient who did not respond to glucocorticoids, immunosuppressants, TNF-α blockers, and TCZ.
Therapies other than immunosuppressive drugs are commonly used in the management of TA. There is an increased risk of atherosclerosis and hypercoagulation due to increased platelet aggregation with excessive thromboxane A2 release in TA. Therefore, antiplatelet therapy such as 5-ASA or full anticoagulation might be indicated in c-TA patients [35••, 36, 52•, 53–54]. Hypertension is one of the most common symptoms, especially in c-TA, and antihypertensive agents may also be needed for the treatment [3, 55].
There are some limitations in this study. First of all, it is too difficult to manage RCTs in medical treatments of c-TA patients to obtain high-quality evidence. Second, existed evidence derived from retrospective, small-sample, and single-center cases with discrepancies in treatment alternatives are weak since standardized guidelines in c-TA are limited. Third, there is no consensus on evaluation and follow-up indicators to assess the therapeutic efficacy and safety, so that it is challenging to perform a valuable systematic review. Another limitation is that the included studies address mainly adult patient populations. We were unable to extract the pediatric cases for all the studies.
Conclusion
In conclusion, the use of biological agents in the treatment of c-TA is gradually increasing. Studies support the efficacy of biological agents such as TNF-α or IL-6 inhibitors, especially in cases of c-TA resistant to conventional therapies. On the other hand, multicenter studies are needed to judge the need for steroid pulses and limited doses of CYC at the induction phase of the severe disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ozen S, Ruperto N, Dillon MJ, Bagga A, Barron K, Davin JC, et al. EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides. Ann Rheum Dis. 2006;65(7):936–41.
Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, et al. Takayasu arteritis. Ann Intern Med. 1994;120(11):919–29. https://doi.org/10.7326/0003-4819-120-11-199406010-00004.
Brunner J, Feldman BM, Tyrrell PN, Kuemmerle-Deschner JB, Zimmerhackl LB, Gassner I, et al. Takayasu arteritis in children and adolescents. Rheumatology (Oxford). 2010;49(10):1806–14. https://doi.org/10.1093/rheumatology/keq167.
Eleftheriou D, Varnier G, Dolezalova P, McMahon AM, Al-Obaidi M, Brogan PA. Takayasu arteritis in childhood: retrospective experience from a tertiary referral centre in the United Kingdom. Arthritis Res Ther. 2015;17(1):36. https://doi.org/10.1186/s13075-015-0545-1.
Clemente G, Hilario MO, Lederman H, Silva CA, Sallum AM, Campos LM, et al. Takayasu arteritis in a Brazilian multicenter study: children with a longer diagnosis delay than adolescents. Clin Exp Rheumatol. 2014;32(3 Suppl 82):S128–33.
Szugye HS, Zeft AS, Spalding SJ. Takayasu Arteritis in the pediatric population: a contemporary United States-based single center cohort. Pediatr Rheumatol Online J. 2014;12:21. https://doi.org/10.1186/1546-0096-12-21.
Morales E, Pineda C, Martínez-Lavín M. Takayasu’s arteritis in children. J Rheumatol. 1991;18(7):1081–4.
• Ozen S, Pistorio A, Iusan SM, Bakkaloglu A, Herlin T, Brik R, et al. EULAR/PRINTO/PRES criteria for Henoch-Schönlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: final classification criteria. Ann Rheum Dis. 2010;69(5):798–806. https://doi.org/10.1136/ard.2009.116657. The Ankara 2008 criteria used in classification for pediatric vasculitis patients were endorsed by the European League Against Rheumatism (EULAR), the International Trials of Pediatric Rheumatology (PRINTO), and the European Association of Pediatric Rheumatology (PRES).
Hata A, Noda M, Moriwaki R, Numano F. Angiographic findings of Takayasu arteritis: new classification. Int J Cardiol. 1996;54(Suppl):S155–63. https://doi.org/10.1016/s0167-5273(96)02813-6.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1.
Singh S, Bali HK, Salaria M, Lal R, Pandav SS, Kumar L. Takayasu’s arteritis in young children: a potentially treatable condition. Indian Pediatr. 1999;36(3):291–6.
Aluquin VP, Albano SA, Chan F, Sandborg C, Pitlick PT. Magnetic resonance imaging in the diagnosis and follow up of Takayasu’s arteritis in children. Ann Rheum Dis. 2002;61(6):526–9. https://doi.org/10.1136/ard.61.6.526.
Ozen S, Duzova A, Bakkaloglu A, Bilginer Y, Cil BE, Demircin M, et al. Takayasu arteritis in children: preliminary experience with cyclophosphamide induction and corticosteroids followed by methotrexate. J Pediatr. 2007;150(1):72–6. https://doi.org/10.1016/j.jpeds.2006.10.059.
Al Abrawi S, Fouillet-Desjonqueres M, David L, Barral X, Cochat P, Cimaz R. Takayasu arteritis in children. Pediatr Rheumatol. 2008;6(1):17. https://doi.org/10.1186/1546-0096-6-17.
Cakar N, Ozçakar ZB, Soy D, Uçar Y, Fitöz S, Kara N, et al. Renal involvement in childhood vasculitis. Nephron Clin Pract. 2008;108(3):c202–6. https://doi.org/10.1159/000118943.
Cakar N, Yalcinkaya F, Duzova A, Caliskan S, Sirin A, Oner A, et al. Takayasu arteritis in children. J Rheumatol. 2008;35(5):913–9.
Filocamo G, Buoncompagni A, Viola S, Loy A, Malattia C, Ravelli A, et al. Treatment of Takayasu’s arteritis with tumor necrosis factor antagonists. J Pediatr. 2008;153(3):432–4. https://doi.org/10.1016/j.jpeds.2008.04.049.
Hijazi R, Chandar J, Nwobi O, Muneeruddin S, Zilleruelo G, Abitbol CL. Renal manifestations in toddlers with Takayasu’s arteritis and malignant hypertension. Pediatr Nephrol. 2009;24(6):1227–30. https://doi.org/10.1007/s00467-008-1088-3.
Jales-Neto LH, Levy-Neto M, Bonfa E, de Carvalho JF, Pereira RM. Juvenile-onset Takayasu arteritis: peculiar vascular involvement and more refractory disease. Scand J Rheumatol. 2010;39(6):506–10. https://doi.org/10.3109/03009741003742730.
Cañas CA, Cañas F, Izquierdo JH, Echeverri AF, Mejía M, Bonilla-Abadía F, et al. Efficacy and safety of anti-interleukin 6 receptor monoclonal antibody (tocilizumab) in Colombian patients with Takayasu arteritis. J Clin Rheumatol. 2014;20(3):125–9. https://doi.org/10.1097/rhu.0000000000000098.
Kumar S, Goel R, Danda D, Surin AK, Bacon PA. A103: Childhood onset Takayasu arteritis—experience from a tertiary care centre in South India. Arthritis Rheumatol. 2014;66(S3):S139-S. https://doi.org/10.1002/art.38524.
Stern S, Clemente G, Reiff A, Ramos MP, Marzan KA, Terreri MT. Treatment of pediatric Takayasu arteritis with infliximab and cyclophosphamide: experience from an American-Brazilian cohort study. J Clin Rheumatol. 2014;20(4):183–8. https://doi.org/10.1097/rhu.0000000000000106.
Misra DP, Aggarwal A, Lawrence A, Agarwal V, Misra R. Pediatric-onset Takayasu’s arteritis: clinical features and short-term outcome. Rheumatol Int. 2015;35(10):1701–6. https://doi.org/10.1007/s00296-015-3272-7.
Conkar S, Mir S, Sözeri B, Bulut İK, Çınar C. Evaluation and therapy in four patients with Takayasu’s arteritis. Saudi J Kidney Dis Transpl. 2016;27(1):164–9. https://doi.org/10.4103/1319-2442.174205.
Batu ED, Sönmez HE, Hazırolan T, Özaltın F, Bilginer Y, Özen S. Tocilizumab treatment in childhood Takayasu arteritis: case series of four patients and systematic review of the literature. Semin Arthritis Rheum. 2017;46(4):529–35. https://doi.org/10.1016/j.semarthrit.2016.07.012.
Aeschlimann FA, Eng SWM, Sheikh S, Laxer RM, Hebert D, Noone D, et al. Childhood Takayasu arteritis: disease course and response to therapy. Arthritis Res Ther. 2017;19(1):255. https://doi.org/10.1186/s13075-017-1452-4.
•• Sahin S, Hopurcuoglu D, Bektas S, Belhan E, Adrovic A, Barut K, et al. Childhood-onset Takayasu arteritis: A 15-year experience from a tertiary referral center. Int J Rheum Dis. 2019;22(1):132–9. https://doi.org/10.1111/1756-185x.13425. A study discussing the responses of 16 childhood Takayasu arteritis patients to high-dose immunosuppressive and biologic treatment.
Fan L, Zhang H, Cai J, Yang L, Liu B, Wei D, et al. Clinical course and prognostic factors of childhood Takayasu’s arteritis: over 15-year comprehensive analysis of 101 patients. Arthritis Res Ther. 2019;21(1):31. https://doi.org/10.1186/s13075-018-1790-x.
Vijayvergiya R, Jindal AK, Pilania RK, Suri D, Gupta A, Sharma A, et al. Complex interventions of abdominal aorta and its branches in children with Takayasu arteritis: clinical experience from a tertiary care center in north-west India. Int J Rheum Dis. 2019;22(1):140–51. https://doi.org/10.1111/1756-185x.13420.
Aeschlimann FA, Barra L, Alsolaimani R, Benseler SM, Hebert D, Khalidi N, et al. Presentation and disease course of childhood-onset versus adult-onset Takayasu arteritis. Arthritis Rheum. 2019;71(2):315–23. https://doi.org/10.1002/art.40690.
Lei C, Huang Y, Yuan S, Chen W, Liu H, Yang M, et al. Takayasu arteritis with coronary artery involvement: differences between pediatric and adult patients. Can J Cardiol. 2020;36(4):535–42. https://doi.org/10.1016/j.cjca.2019.08.039.
Bolek EC, Kaya Akca U, Sari A, Sag E, Demir S, Kilic L, et al. Is Takayasu’s arteritis more severe in children? Clin Exp Rheumatol. 2020.
Misra R, Danda D, Rajappa SM, Ghosh A, Gupta R, Mahendranath KM, et al. Development and initial validation of the Indian Takayasu Clinical Activity Score (ITAS2010). Rheumatology (Oxford). 2013;52(10):1795–801. https://doi.org/10.1093/rheumatology/ket128.
•• Hellmich B, Agueda A, Monti S, Buttgereit F, de Boysson H, Brouwer E, et al. 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2020;79(1):19–30. https://doi.org/10.1136/annrheumdis-2019-215672. Updated EULAR recommendations for the management of large vessel vasculitis.
•• de Graeff N, Groot N, Brogan P, Ozen S, Avcin T, Bader-Meunier B, et al. European consensus-based recommendations for the diagnosis and treatment of rare paediatric vasculitides -the SHARE initiative. Rheumatology (Oxford). 2019;58(4):656–71. https://doi.org/10.1093/rheumatology/key322. European consensus-based recommendations for diagnosing and treating rare pediatric vasculitis, including the Takayasu arteritis.
Kötter I, Henes JC, Wagner AD, Loock J, Gross WL. Does glucocorticosteroid-resistant large-vessel vasculitis (giant cell arteritis and Takayasu arteritis) exist and how can remission be achieved? A critical review of the literature. Clin Exp Rheumatol. 2012;30(1 Suppl 70):S114–29.
Aeschlimann FA, Twilt M, Yeung RSM. Childhood-onset Takayasu arteritis. Eur J Rheumatol. 2020;17:S58+.
Mekinian A, Comarmond C, Resche-Rigon M, Mirault T, Kahn JE, Lambert M, et al. Efficacy of biological-targeted treatments in Takayasu arteritis: multicenter, retrospective study of 49 patients. Circulation. 2015;132(18):1693–700. https://doi.org/10.1161/circulationaha.114.014321.
Park MC, Lee SW, Park YB, Lee SK. Serum cytokine profiles and their correlations with disease activity in Takayasu’s arteritis. Rheumatology (Oxford). 2006;45(5):545–8. https://doi.org/10.1093/rheumatology/kei266.
Kong X, Ma L, Ji Z, Dong Z, Zhang Z, Hou J, et al. Pro-fibrotic effect of IL-6 via aortic adventitial fibroblasts indicates IL-6 as a treatment target in Takayasu arteritis. Clin Exp Rheumatol. 2018;36(1):62–72.
Singh A, Danda D, Hussain S, Najmi AK, Mathew A, Goel R, et al. Efficacy and safety of tocilizumab in treatment of Takayasu arteritis: a systematic review of randomized controlled trials. Mod Rheumatol. 2021;31(1):197–204. https://doi.org/10.1080/14397595.2020.1724671.
Elefante E, Bond M, Monti S, Lepri G, Cavallaro E, Felicetti M, et al. One year in review 2018: systemic vasculitis. Clin Exp Rheumatol. 2018;36(Suppl 111(2)):12–32.
•• Nakaoka Y, Isobe M, Takei S, Tanaka Y, Ishii T, Yokota S, et al. Efficacy and safety of tocilizumab in patients with refractory Takayasu arteritis: results from a randomised, double-blind, placebo-controlled, phase 3 trial in Japan (the TAKT study). Ann Rheum Dis. 2018;77(3):348–54. https://doi.org/10.1136/annrheumdis-2017-211878. This is a randomized, double-blind, placebo-control phase 3 trial investigating the efficacy and safety of the interleukin-6receptor antibody tocilizumab in patients with Takayasu arteritis.
Kong X, Zhang X, Lv P, Cui X, Ma L, Chen H, et al. Treatment of Takayasu arteritis with the IL-6R antibody tocilizumab vs. cyclophosphamide. Int J Cardiol. 2018;266:222–8. https://doi.org/10.1016/j.ijcard.2017.12.066.
Pazzola G, Muratore F, Pipitone N, Crescentini F, Cacoub P, Boiardi L, et al. Rituximab therapy for Takayasu arteritis: a seven patients experience and a review of the literature. Rheumatology (Oxford). 2018;57(7):1151–5. https://doi.org/10.1093/rheumatology/kex249.
Xenitidis T, Horger M, Zeh G, Kanz L, Henes JC. Sustained inflammation of the aortic wall despite tocilizumab treatment in two cases of Takayasu arteritis. Rheumatology (Oxford). 2013;52(9):1729–31. https://doi.org/10.1093/rheumatology/ket107.
Savioli B, Abdulahad WH, Brouwer E, Kallenberg CGM, de Souza AWS. Are cytokines and chemokines suitable biomarkers for Takayasu arteritis? Autoimmun Rev. 2017;16(10):1071–8. https://doi.org/10.1016/j.autrev.2017.07.023.
Zhang H, Watanabe R, Berry GJ, Tian L, Goronzy JJ, Weyand CM. Inhibition of JAK-STAT signaling suppresses pathogenic immune responses in medium and large vessel vasculitis. Circulation. 2018;137(18):1934–48. https://doi.org/10.1161/circulationaha.117.030423.
Kuwabara S, Tanimura S, Matsumoto S, Nakamura H, Horita T. Successful remission with tofacitinib in a patient with refractory Takayasu arteritis complicated by ulcerative colitis. Ann Rheum Dis. 2020;79(8):1125–6. https://doi.org/10.1136/annrheumdis-2019-216606.
Li J, Li M, Tian X, Zeng X. Tofacitinib in patients with refractory Takayasu’s arteritis. Rheumatology (Oxford). 2020;59(11):e95–e8. https://doi.org/10.1093/rheumatology/keaa281.
Yamamura Y, Matsumoto Y, Asano Y, Katayama Y, Hayashi K, Ohashi K, et al. Refractory Takayasu arteritis responding to the oral Janus kinase inhibitor, tofacitinib. Rheumatol Adv Pract. 2020;4(1):rkz050. https://doi.org/10.1093/rap/rkz050.
• Keser G, Direskeneli H, Aksu K. Management of Takayasu arteritis: a systematic review. Rheumatology (Oxford). 2014;53(5):793–801. https://doi.org/10.1093/rheumatology/ket320. A systematic literature review discussing the management strategies of Takayasu arteritis.
Seyahi E, Ugurlu S, Cumali R, Balci H, Seyahi N, Yurdakul S, et al. Atherosclerosis in Takayasu arteritis. Ann Rheum Dis. 2006;65(9):1202–7. https://doi.org/10.1136/ard.2005.047498.
Wang X, Dang A, Lv N, Cheng N, Cheng X. Inflammation is associated with platelet coagulation function rather than enzymatic coagulation function in patients with Takayasu arteritis. Int Heart J. 2017;58(4):589–92. https://doi.org/10.1536/ihj.16-533.
Feng Y, Tang X, Liu M, Zhou J, Zhao X, Li Q. Clinical study of children with Takayasu arteritis: a retrospective study from a single center in China. Pediatr Rheumatol. 2017;15(1):29. https://doi.org/10.1186/s12969-017-0164-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Rheumatology
Rights and permissions
About this article
Cite this article
Sener, S., Basaran, O. & Ozen, S. Wind of Change in the Treatment of Childhood-Onset Takayasu Arteritis: a Systematic Review. Curr Rheumatol Rep 23, 68 (2021). https://doi.org/10.1007/s11926-021-01032-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s11926-021-01032-8