Abstract
Takayasu arteritis (TAK) is a less common large-vessel vasculitis which can occur in either children or adults. However, differences between pediatric-onset and adult-onset TAK have not been systematically analyzed. We undertook a systematic review (pre-registered on PROSPERO, identifier CRD42022300238) to analyze differences in clinical presentation, angiographic involvement, treatments, and outcomes between pediatric-onset and adult-onset TAK. We searched PubMed (MEDLINE and PubMed Central), Scopus, major recent international rheumatology conference abstracts, Cochrane database, and clinicaltrials.gov, and identified seven studies of moderate to high quality comparing pediatric-onset and adult-onset TAK. Meta-analysis of 263 pediatric-onset and 981 adult-onset TAK suggested that constitutional features (fever, and in subgroup analyses, weight loss), hypertension, headache, and sinister features of cardiomyopathy, elevated serum creatinine, and abdominal pain were more frequent in pediatric-onset TAK, whereas pulse loss/pulse deficit and claudication (particularly upper limb claudication) were more frequent in adult-onset TAK. Hata’s type IV TAK was more common in pediatric-onset TAK, and Hata’s type I TAK in adult-onset TAK. Children with TAK also appeared to require more intense immunosuppression with more frequent use of cyclophosphamide, biologic DMARDs, tumor necrosis factor alpha inhibitors, and, in subgroup analyses, tocilizumab in pediatric-onset TAK than in adult-onset TAK. Surgical or endovascular procedures, remission, and risk of mortality were similar in both children and adults with TAK. No studies had compared patient-reported outcome measures between pediatric-onset and adult-onset TAK. Distinct clinical features and angiographic extent prevail between pediatric-onset and adult-onset TAK. Clinical outcomes in these subgroups require further study in multicentric cohorts.
Key Points • Pediatric-onset TAK more commonly presents with constitutional features, hypertension, cardiomyopathy, elevated serum creatinine, and abdominal pain. • Adult-onset TAK more commonly presents with pulse loss/pulse deficit or claudication (particularly of the upper limbs). • Angiographic type IV is more common in children, and type I in adults. • Remission and mortality are similar in pediatric-onset and adult-onset TAK. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Takayasu arteritis (TAK) is a rare form of large-vessel vasculitis (LVV) that predominantly affects younger individuals [1]. Large-vessel inflammation associated with or without systemic features drive the pathogenesis of TAK [2,3,4]. While the onset of TAK is often insidious and might progress to pulse loss without prominent symptoms, in rarer instances, the onset can be devastating with rapid-onset critical vascular occlusion resulting in stroke or myocardial infarction [1, 5]. The entities of pediatric-onset and adult-onset TAK are both well recognized. Separate classification criteria have been proposed for pediatric-onset TAK [6], distinct from the criteria commonly used for adult-onset TAK [7,8,9]. It is believed that pediatric-onset TAK has more prominent systemic symptoms and that the disease course might be more severe [10,11,12]. Until recently, few studies had compared pediatric-onset and adult-onset TAK [11]. Differences between the clinical presentation, angiographic involvement, treatment patterns, and outcomes between pediatric-onset and adult-onset TAK have not yet been systematically evaluated by pooling data across individual studies in the form of a systematic review with meta-analysis. Therefore, we undertook this systematic review to understand differences in the clinical presentation, angiographic extent, prevalent treatment practices, and outcomes between pediatric-onset and adult-onset TAK.
Methods
Protocol
The systematic review protocol was registered with the prospective international register of systematic reviews (PROSPERO identifier CRD42022300238). The systematic review was conducted in line with recommendations provided by the Cochrane collaboration [13]. The systematic review was reported to conform with Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA 2020, Supplementary Table S1) [14] and Meta-analysis of Observational Studies in Epidemiology (Supplementary Table S2) [15] reporting guidelines.
Literature searches
PubMed (both MEDLINE and PubMed Central) and Scopus, the Cochrane database of clinical trials (CENTRAL), the website of clinicaltrials.gov, conference abstracts of major international Rheumatology societies, viz., European Alliance of Associations for Rheumatology (EULAR, from 2018 to 2022), American College of Rheumatology (ACR, from 2018 to 2021), and Asia Pacific League of Associations for Rheumatology (from 2018 to 2021) were searched to identify articles related to pediatric-onset TAK. The search strategy is presented in Supplementary Table S3. Studies hitherto identified were screened to identify those comparing patients with pediatric-onset and adult-onset TAK. Literature searches were conducted on 10 January 2022 and updated on 23 May 2022. The updated search results are presented in the manuscript.
Inclusion criteria
Participants
Patients with pediatric-onset TAK either fulfilled the 2010 EULAR/Pediatric Rheumatology European Society (PRES)/Pediatric Rheumatology International Trials Organization (PRINTO) criteria for TAK [6], 2012 Chapel Hill Consensus Conference definition of TAK [5], or had a clinician diagnosis of TAK. Patients with adult-onset TAK either fulfilled the 1990 ACR classification criteria for TAK [7], the Ishikawa criteria [8], or Sharma’s modification of Ishikawa criteria [9], 2012 Chapel Hill Consensus Conference definition of TAK [5], or had a clinician diagnosis of TAK.
Intervention and comparator groups
Patients with pediatric-onset TAK were compared with those with adult-onset TAK.
Outcomes
Clinical features at presentation, angiographic involvement (individual vessels involved as well as using any of the angiographic classification systems), treatments used at any time or at the last visit (corticosteroids, conventional disease-modifying antirheumatic drugs (DMARDs), biologic DMARDs, targeted synthetic DMARDs), surgical or endovascular procedures (with complications, if any), and outcomes (remission as defined by the clinician at any visit or at last follow-up, angiographic stabilization, damage scores, mortality) were all primary outcomes.
Types of studies
Since TAK is a rare disease and there are few clinical trials in TAK [16], both observational and interventional studies were considered for inclusion, provided they had included at least 5 patients with TAK.
Exclusion criteria
Original articles which presented information about pediatric-onset TAK without a comparator group of adult-onset TAK were excluded. Review articles, case reports, letters to the editor not describing original data, or editorials were excluded.
Screening and data extraction
Titles and abstracts of studies derived from the search results were screened by two investigators independently (DPM, PP) and studies identified for full-text screening were further evaluated for eligibility, noting reasons for exclusion at each step. Results from PubMed and Scopus searches were exported using Endnote X9.3 and duplicates were removed. Searches conducted on conference abstracts, clinicaltrials.gov, and CENTRAL were done manually.
For the identified studies, data was extracted onto paper proformas by three investigators independently (DPM, UR, CRK). Any discrepancies were resolved by discussion with a fourth colleague (AS).
Quality assessment of individual studies
The quality of observational studies published as full text (but not conference abstracts) was assessed using the Newcastle–Ottawa scale. Selection of participants (out of 4), comparability of groups (out of 2), and outcome assessment (out of 3) were rated by two investigators (DPM and VA) independently. Discrepancies were resolved by discussion between investigators. Publication bias was ascertained only if there were at least ten studies available for a particular comparison [17].
Analysis of data
Detailed summary of findings tables were generated to detail demographic characteristics of participants in the identified studies, separately for pediatric-onset and adult-onset TAK. Wherever means with standard deviations were not available in the papers, these were imputed from the median and quartiles 1 and 3 [18] or from the median with lower and upper limits of range [19] using formulae available in the published literature. Risk ratios for various categorical outcomes and effect size for continuous variables (using Hedges’ g) for pediatric-onset vs adult-onset TAK were pooled using inverse variance restricted maximum likelihood method with random effects using meta command on STATA 16.1 I/C. This technique automatically adjusted for zeros if any in the numerator of the risk ratios. Random effects model was chosen a priori due to the expected heterogeneity among studies resulting from inter-study differences such as those in inclusion criteria for patient selection, study design (prospective or retrospective), and different care settings. Pooled log risk ratios (with 95% confidence intervals) were calculated using this technique. Statistical heterogeneity of the pooled estimates was calculated using the I2 statistic, with values > 50% indicative of significant heterogeneity. Wherever data could not be pooled across studies, standalone risk ratios with 95% confidence intervals were calculated using online calculators [20]. Subgroup analyses were pre-planned based on study design (prospective, retrospective, or both prospective and retrospective).
Results
Search results
Search results are detailed in Fig. 1 derived from the PRISMA flowchart. After screening and eligibility assessment as per criteria detailed previously, six full papers [21,22,23,24,25,26] and one conference abstract [27] were selected for qualitative and quantitative analysis.
Search strategy derived from the PRISMA 2020 flowchart [14]
Characteristics of included studies
Table 1 summarizes the characteristics of included studies. Overall, there were 263 patients with pediatric-onset TAK and 981 with adult-onset TAK. Six out of the seven identified studies were single-center studies, five were retrospective, whereas one each was prospective or both prospective and retrospective. Three studies defined pediatric-onset TAK as onset ≤ 18 years, three others as onset < 18 years, whereas another defined it as onset ≤ 16 years. Both pediatric-onset and adult-onset TAK had a predominance of female patients. Delay to diagnosis was similar in both groups. Delay to diagnosis could be pooled from three studies (Jales-Neto 2010, Aeschlimann 2019 and Karabacak 2021). Pooled delay to diagnosis was not significantly different between pediatric-onset and adult-onset TAK (effect size − 0.36, 95% confidence interval − 0.75 to + 0.03) without significant heterogeneity (Supplementary Fig. 1). Seven studies each had reported clinical presentation or angiographic extent of disease, whereas six studies each had reported treatments or outcomes comparatively between pediatric-onset and adult-onset TAK.
Quality assessment of individual studies
Two studies were of high quality (Newcastle–Ottawa scale score 7–9) and four others were of moderate quality (Newcastle–Ottawa scale score 4–6) [28]. Quality assessment could not be performed for the study published as a conference abstract alone (Cocchiara 2020) (Supplementary Table S4). Publication bias could not be evaluated due to a paucity of studies.
Comparisons between pediatric-onset and adult-onset TAK
Clinical features at presentation
Among vascular features, hypertension (with considerable statistical heterogeneity) was more frequent in pediatric-onset TAK, whereas pulse loss/pulse deficit and claudication were more frequent in adult-onset TAK. Cardiomyopathy was more frequent in pediatric-onset TAK. Among constitutional features, fever was more frequent in pediatric-onset TAK. Among neurological features, headache was more frequent in pediatric-onset TAK. Elevated serum creatinine and abdominal pain were also more frequent in pediatric-onset TAK (Fig. 2).
Angiographic extent of disease
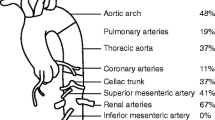
As per Hata’s angiographic classification [29], type IV disease was more frequent in pediatric-onset TAK, whereas type I disease was more frequent in adult-onset TAK (Fig. 3). As per a recently proposed novel angiographic classification [30], there was no difference observed between pediatric-onset and adult-onset TAK (Supplementary Fig. 2). Considering individual vessels, aorta, splanchnic vessels overall, superior mesenteric artery, and renal arteries were more commonly involved in pediatric-onset TAK, whereas subclavian arteries were more commonly involved in adult-onset TAK (Supplementary Figures S3a, S3b, S3c).
Drug treatments received
Cyclophosphamide, overall biologic DMARDs, and tumor necrosis factor inhibitors were more frequently used in pediatric-onset than in adult-onset TAK. The use of corticosteroids and other conventional DMARDs was similar between pediatric-onset and adult-onset TAK (Fig. 4a).
Surgical or endovascular procedures
The overall use of surgical or endovascular procedures was similar between pediatric-onset and adult-onset TAK (Fig. 4b).
Outcomes
The proportion of patients attaining remission (Fig. 4c) and mortality (Fig. 4d) were similar between pediatric-onset and adult-onset TAK. Outcomes that could not be pooled across studies are presented in Table 2. Aeschlimann et al. [23] reported remission at 6 months in a significantly lesser proportion of pediatric-onset than in adult-onset TAK. Karabacak et al. [25] reported greater damage assessed using the Vasculitis Damage Index in patients with adult-onset TAK than in pediatric-onset TAK.
Subgroup analyses
Excluding studies that were retrospective (Jales-Neto 2010) or both prospective and retrospective (Danda 2021), subgroup analyses were conducted for retrospective studies alone. Comparing with associations observed during primary analyses, claudication and elevated serum creatinine were no more different between pediatric-onset and adult-onset TAK, carotidodynia was more frequent in adult-onset TAK, and weight loss was more frequent in pediatric-onset TAK (Supplementary Figure S4a, S4b, S4c, S4d). These secondary analyses could not be performed for neurological features since the data did not permit meta-analysis. Hata’s type I disease continued to be more frequent in adults and type IV disease in children (Supplementary Figure S5). Comparing the involvement of individual vessels, aorta, splanchnic vessels overall and renal arteries (as on primary analyses) and celiac artery involvement (from a single study) were more frequently involved in pediatric-onset TAK. Subclavian artery involvement continued to be more frequent in adult-onset TAK (Supplementary Figure S6). Cyclophosphamide, overall biologic DMARDs, tumor necrosis factor inhibitors (as noted before), and additionally tocilizumab were more frequently used in pediatric-onset than in adult-onset TAK (Supplementary Figure S7a). Unlike in the primary analysis, remission was more frequently noted in adult-onset TAK than in pediatric-onset TAK (Supplementary Figure S7c). Other outcomes did not differ (Supplementary Figure S7b, S7d).
Discussion
Overall, few studies of moderate to high quality had compared pediatric-onset with adult-onset TAK. Both pediatric-onset and adult-onset TAK were more common in females. Similar delay to diagnosis was observed in both groups. All the parameters for which meta-analyses were undertaken were not available from all the identified studies. Meta-analysis suggested that constitutional features (fever, and in subgroup analyses, weight loss), hypertension, headache, and sinister features of cardiomyopathy, elevated serum creatinine, and abdominal pain were more frequent in pediatric-onset TAK, corresponding with predominant vascular involvement of Hata’s type IV TAK and greater frequency of splanchnic and renal artery involvement, whereas, pulse loss/pulse deficit and claudication (particularly upper limb claudication) were more frequent in adult-onset TAK, corresponding with predominant Hata’s type I TAK and more frequent subclavian artery involvement. Most clinical features and vascular involvement lacked considerable heterogeneity in pooled estimates. Children with TAK also appeared to require more intense immunosuppression with more frequent use of cyclophosphamide, biologic DMARDs, tumor necrosis factor alpha inhibitors, and, in subgroup analyses, tocilizumab than in adults. Surgical or endovascular procedures, remission, and risk of dying were similar in children and adults with TAK. Considerable statistical heterogeneity was observed in the pooled drug treatments, vascular interventions, and remission.
The present systematic review included more than a thousand patients with TAK, a significantly large number for a rare LVV [31]. The epidemiology of TAK suggests that, for reasons yet to be fully understood, TAK is more common in females [1, 32]. While previously suggested that children with TAK have greater delay to diagnosis than adults with TAK [33], the delay to diagnosis in studies identified in our systematic review was similar for both groups in a meta-analysis. Heterogenous definitions had been used for pediatric-onset TAK (≤ 18 years, < 18 years, ≤ 16 years). Future studies evaluating pediatric-onset TAK should consider using the standardized definition provided by EULAR/PRES/PRINTO criteria as onset ≤ 18 years [6].
Distinct syndromes of presentation and different patterns of vascular involvement were observed between pediatric-onset and adult-onset TAK. Children had more sinister vascular involvement such as splanchnic and renal vessels, as well as more severe manifestations of cardiomyopathy and renal dysfunction. Adult-onset TAK, on the other hand, had dominant upper limb vascular occlusive manifestations. These differences were confirmed by the dominant angiographic types (Hata’s) of type IV in children and type I in adults. It must be noted that meta-analysis was undertaken for clinical features and vascular involvement at presentation. Vascular involvement in TAK progresses with time in a subset of patients despite immunosuppressive therapy [16]. Angiographic subtypes might also evolve with time [33], although temporal changes in angiographic classification have not been systematically studied. Future cohort studies in both pediatric-onset and adult-onset TAK should systematically report angiographic progression to enable its comparative assessment in both subgroups.
Cardiomyopathy was more frequent in pediatric-onset TAK. Cardiac involvement in TAK could occur due to coronary artery involvement or cardiac inflammation resulting in myocarditis or cardiomyopathy [34]. Our meta-analysis suggested that coronary arterial involvement was similar in both pediatric-onset and adult-onset TAK. Cardiac involvement portends greater mortality risk in TAK [34]. Rarely, cardiac involvement in TAK might be sub-clinical, detectable only on cardiac imaging [35]. Renovascular hypertension was also more frequent in pediatric-onset TAK, possibly responsible for more common renal failure among pediatric-onset TAK than adult-onset TAK. Also, uncontrolled hypertension associates with myocardial dysfunction and heart failure in TAK [36]. A recent study reported that among TAK with coronary arterial involvement, pediatric-onset TAK (n = 9) had earlier onset of coronary artery involvement, higher disease activity, and greater risk of coronary artery dilatation then adult-onset TAK (n = 29) [37].
TAK is corticosteroid-responsive, albeit often relapses following corticosteroid taper [38]. Most patients with pediatric-onset and adult-onset TAK were treated with corticosteroids in studies identified in our systematic review, and in similar proportions between groups. Cyclophosphamide is generally reserved for more severe, aggressive vascular manifestations in TAK. Biologic DMARDs are used in refractory TAK when other DMARDs have failed. Treatment with cyclophosphamide or biologic DMARDs in more patients with pediatric-onset TAK possibly reflects an aggressive or treatment-refractory course in this sub-group of TAK. It also might reflect the need for faster corticosteroid taper in children due to complications such as growth stunting and cataract [39]. In this context, it is important to reiterate that drug therapies in TAK are mostly based on observational studies. Few clinical trials have been conducted in TAK, none exclusively focused on pediatric-onset TAK. The trial of tocilizumab in TAK included some pediatric-onset TAK (inclusion criteria ≥ 12 years) [40], whereas that of abatacept included only adults [41]. Janus kinase inhibitors are being increasingly used in different inflammatory rheumatic diseases [42], including in the pediatric population [43]. Recent studies have evaluated the use of Janus kinase inhibitors in TAK as well [44,45,46]. None of the studies analyzed in our systematic review had reported the use of Janus kinase inhibitors in pediatric-onset TAK. This shall form an interesting agenda for future research.
Despite more severe presentation, outcomes of remission and mortality were similar in pediatric-onset and adult-onset TAK in our meta-analysis. Sub-group analyses of retrospective studies (but not the overall analyses) alone suggested a greater chance of remission in adult-onset TAK than in pediatric-onset TAK. A standardized definition of remission in TAK is lacking; this is often patient-reported. Adults might better report improvement during routine clinical visits, which might explain why retrospective reviews of medical records identified higher proportions of remission in adults. The two studies that reported angiographic outcomes at different time points (6 months, at last visit) noted similar angiographic stabilization in pediatric-onset and adult-onset TAK. While similar proportions of pediatric-onset and adult-onset TAK experienced mortality, these were estimates of risk ratios without accounting for event rates. Future studies on pediatric-onset TAK should consider reporting hazard ratios of outcomes (including mortality).
There were limitations to our systematic review. Most identified studies were retrospective and, therefore, have inherent limitations imposed by such a study design. None presented patient-reported outcome measures (PROMs). A previous systematic review had also identified that few studies on childhood-onset TAK had reported PROMs [47]. A paucity of identified studies did not permit the assessment of publication bias. We have compared phenotypes and outcomes between pediatric-onset and adult-onset at an aggregated level rather than as an individual patient-data meta-analysis [48]. Risk ratios (rather than rate ratios, which account for follow-up duration and, therefore, are more robust) could be reported based on the available data. We could not contact individual authors to seek primary data of their studies due to limitations of resources available for this study. To the best of our knowledge, this is the first systematic review with meta-analysis comparing pediatric-onset and adult-onset TAK. Our findings were based on searches of multiple databases and also included gray literature searches. The findings of the present study enable a better understanding of differences in TAK based on age group of onset. When large-vessel vasculitis was recognized in the last century, TAK and its counterpart giant cell arteritis (GCA) were considered different simply based on the age of presentation. However, it is now recognized that TAK and GCA are distinct diseases with distinct genetic predisposition [49] and differing patterns of vascular involvement, based on information gathered from global, multicentric studies [50,51,52,53]. It is possible that future studies might similarly delineate distinctions between pediatric-onset and adult-onset TAK. The rarity of pediatric-onset TAK when compared with adult-onset TAK makes it difficult to envisage future clinical trials in this area, unless backed by multi-centric multi-national efforts. Multicentric cohorts with a standardized data collection and standardized outcome measures (including PROMs), possibly with concurrent adult-onset TAK cohorts, might enable better understanding of the natural history of pediatric-onset TAK.
Conclusion
Systematic differences could be identified between the clinical presentation and angiographic involvement of pediatric-onset and adult-onset TAK. Outcomes (including remission, relapses, and mortality) appeared to be similar between pediatric-onset and adult-onset TAK. Future multicentric cohort studies with common case record forms for data collection should help to better understand the differences between these two subsets of TAK.
Data availability
All the analyses performed for this systematic review have been reported in the main text or in the supplementary files. Data pertaining to the systematic review shall be shared on reasonable request to the corresponding author (Durga Prasanna Misra, durgapmisra@gmail.com).
References
Misra DP, Wakhlu A, Agarwal V, Danda D (2019) Recent advances in the management of Takayasu arteritis. Int J Rheum Dis 22(Suppl 1):60–68. https://doi.org/10.1111/1756-185x.13285
Singh K, Rathore U, Rai MK et al (2022) Novel Th17 lymphocyte populations, Th17.1 and PD1+Th17, are increased in Takayasu arteritis, and both Th17 and Th17.1 sub-populations associate with active disease. J Inflamm Res 15:1521–1541. https://doi.org/10.2147/jir.S355881
Arnaud L, Haroche J, Mathian A, Gorochov G, Amoura Z (2011) Pathogenesis of Takayasu’s arteritis: a 2011 update. Autoimmun Rev 11:61–67. https://doi.org/10.1016/j.autrev.2011.08.001
Pugh D, Karabayas M, Basu N et al (2022) Large-vessel vasculitis Nat Rev Dis Primers 7:93. https://doi.org/10.1038/s41572-021-00327-5
Jennette JC, Falk RJ, Bacon PA et al (2013) 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 65:1–11. https://doi.org/10.1002/art.37715
Ozen S, Pistorio A, Iusan SM et al (2010) EULAR/PRINTO/PRES criteria for Henoch-Schönlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: Final classification criteria. Ann Rheum Dis 69:798–806. https://doi.org/10.1136/ard.2009.116657
Arend WP, Michel BA, Bloch DA et al (1990) The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 33:1129–1134. https://doi.org/10.1002/art.1780330811
Ishikawa K (1988) Diagnostic approach and proposed criteria for the clinical diagnosis of Takayasu’s arteriopathy. J Am Coll Cardiol 12:964–972. https://doi.org/10.1016/0735-1097(88)90462-7
Sharma BK, Jain S, Suri S, Numano F (1996) Diagnostic criteria for Takayasu arteritis. Int J Cardiol 54(Suppl):S141-147. https://doi.org/10.1016/s0167-5273(96)88783-3
Brunner J, Feldman BM, Tyrrell PN et al (2010) Takayasu arteritis in children and adolescents. Rheumatology (Oxford) 49:1806–1814. https://doi.org/10.1093/rheumatology/keq167
Mathew AJ, Goel R, Kumar S, Danda D (2016) Childhood-onset Takayasu arteritis: an update. Int J Rheum Dis 19:116–126. https://doi.org/10.1111/1756-185x.12718
Goel R, Sathish Kumar T, Danda D (2019) Childhood-onset Takayasu arteritis (c-TA): current and future drug therapy. Paediatr Drugs 21:81–93. https://doi.org/10.1007/s40272-019-00327-9
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2019) Cochrane Handbook for Systematic Reviews of Interventions, 2nd edn. John Wiley & Sons, Chichester (UK)
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 134:178–189. https://doi.org/10.1016/j.jclinepi.2021.03.001
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Misra DP, Rathore U, Patro P, Agarwal V, Sharma A (2021) Disease-modifying anti-rheumatic drugs for the management of Takayasu arteritis-a systematic review and meta-analysis. Clin Rheumatol 40:4391–4416. https://doi.org/10.1007/s10067-021-05743-2
Misra DP, Agarwal V (2018) Systematic reviews: challenges for their justification, related comprehensive searches, and implications. J Korean Med Sci 33:9. https://doi.org/10.3346/jkms.2018.33.e92
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Practical Meta-analysis effect size calculator. Available at https://campbellcollaboration.org/escalc/html/EffectSizeCalculator-SMD1.php. Accessed 25 June 2022
Cong XL, Dai SM, Feng X et al (2010) Takayasu’s arteritis: clinical features and outcomes of 125 patients in China. Clin Rheumatol 29:973–981. https://doi.org/10.1007/s10067-010-1496-1
Jales-Neto LH, Levy-Neto M, Bonfa E, de Carvalho JF, Pereira RM (2010) Juvenile-onset Takayasu arteritis: peculiar vascular involvement and more refractory disease. Scand J Rheumatol 39:506–510. https://doi.org/10.3109/03009741003742730
Aeschlimann FA, Barra L, Alsolaimani R et al (2019) Presentation and disease course of childhood-onset versus adult-onset Takayasu arteritis. Arthritis Rheumatol 71:315–323. https://doi.org/10.1002/art.40690
Bolek EC, Kaya Akca U, Sari A et al (2021) Is Takayasu’s arteritis more severe in children? Clin Exp Rheumatol 39(Suppl 129):32–38. https://doi.org/10.55563/clinexprheumatol/kr357t
Karabacak M, Kaymaz-Tahra S, Şahin S et al (2021) Childhood-onset versus adult-onset Takayasu arteritis: a study of 141 patients from Turkey. Semin Arthritis Rheum 51:192–197. https://doi.org/10.1016/j.semarthrit.2020.10.013
Danda D, Goel R, Joseph G et al (2021) Clinical course of 602 patients with Takayasu’s arteritis: comparison between childhood-onset versus adult onset disease. Rheumatology (Oxford) 60:2246–2255. https://doi.org/10.1093/rheumatology/keaa569
Cocchiara E, Galli E, De Fanti A, Malattia C, Ravelli A, Salvarani C (2020) SAT0489 clinical course and therapy response in Takayasu arteritis: comparision between childhood and adult onset. Ann Rheum Dis 79:1201. https://doi.org/10.1136/annrheumdis-2020-eular.2491
Li L, Liu C, Cheng L, Yan S, Chen H, Li Y (2021) Assessment of diagnostic utility, clinical phenotypic associations, and prognostic significance of anti-NXP2 autoantibody in patients with idiopathic inflammatory myopathies: a systematic review and meta-analysis. Clin Rheumatol 40:819–832. https://doi.org/10.1007/s10067-020-05291-1
Hata A, Noda M, Moriwaki R, Numano F (1996) Angiographic findings of Takayasu arteritis: new classification. Int J Cardiol 54(Suppl):S155-163
Goel R, Gribbons KB, Carette S et al (2020) Derivation of an angiographically based classification system in Takayasu’s arteritis: an observational study from India and North America. Rheumatology (Oxford) 59:1118–1127. https://doi.org/10.1093/rheumatology/kez421
Watts RA, Hatemi G, Burns JC, Mohammad AJ (2022) Global epidemiology of vasculitis. Nat Rev Rheumatol 18:22–34. https://doi.org/10.1038/s41584-021-00718-8
Sun Y, Yin MM, Ma LL et al (2021) Epidemiology of Takayasu arteritis in Shanghai: a hospital-based study and systematic review. Int J Rheum Dis 24:1247–1256. https://doi.org/10.1111/1756-185x.14183
Misra DP, Aggarwal A, Lawrence A, Agarwal V, Misra R (2015) Pediatric-onset Takayasu’s arteritis: clinical features and short-term outcome. Rheumatol Int 35:1701–1706. https://doi.org/10.1007/s00296-015-3272-7
Misra DP, Shenoy SN (2017) Cardiac involvement in primary systemic vasculitis and potential drug therapies to reduce cardiovascular risk. Rheumatol Int 37:151–167. https://doi.org/10.1007/s00296-016-3435-1
Porter A, Youngstein T, Babar S, Mason JC (2021) A rare life-threatening presentation of Takayasu arteritis. Rheumatology (Oxford) 60:iii6-iii8. https://doi.org/10.1093/rheumatology/keab036
Guha Sarkar P, Bansal A, Tyagi S, Gupta MD (2022) Predictors of left ventricular dysfunction in patients with Takayasu’s arteritis: a single centre experience. Clin Exp Rheumatol 40:714–719. https://doi.org/10.55563/clinexprheumatol/53koap
Lei C, Huang Y, Yuan S et al (2020) Takayasu arteritis with coronary artery involvement: differences between pediatric and adult patients. Can J Cardiol 36:535–542. https://doi.org/10.1016/j.cjca.2019.08.039
Misra DP, Rathore U, Patro P, Agarwal V, Sharma A (2021) Corticosteroid monotherapy for the management of Takayasu arteritis-a systematic review and meta-analysis. Rheumatol Int 41:1729–1742. https://doi.org/10.1007/s00296-021-04958-5
Deshmukh CT (2007) Minimizing side effects of systemic corticosteroids in children. Indian J Dermatol Venereol Leprol 73:218–221. https://doi.org/10.4103/0378-6323.33633
Nakaoka Y, Isobe M, Takei S et al (2018) Efficacy and safety of tocilizumab in patients with refractory Takayasu arteritis: results from a randomised, double-blind, placebo-controlled, phase 3 trial in Japan (the TAKT study). Ann Rheum Dis 77:348–354. https://doi.org/10.1136/annrheumdis-2017-211878
Langford CA, Cuthbertson D, Ytterberg SR et al (2017) A randomized, double-blind trial of abatacept (CTLA-4Ig) for the treatment of Takayasu arteritis. Arthritis Rheumatol 69:846–853. https://doi.org/10.1002/art.40037
Choy EH (2018) Clinical significance of Janus kinase inhibitor selectivity. Rheumatology (Oxford) 58:953–962. https://doi.org/10.1093/rheumatology/key339
Ruperto N, Brunner HI, Synoverska O et al (2021) Tofacitinib in juvenile idiopathic arthritis: a double-blind, placebo-controlled, withdrawal phase 3 randomised trial. Lancet 398:1984–1996. https://doi.org/10.1016/s0140-6736(21)01255-1
Rathore U, Thakare DR, Patro P, Agarwal V, Sharma A, Misra DP (2022) A systematic review of clinical and preclinical evidences for Janus kinase inhibitors in large vessel vasculitis. Clin Rheumatol 41:33–44. https://doi.org/10.1007/s10067-021-05973-4
Kong X, Sun Y, Dai X et al (2022) Treatment efficacy and safety of tofacitinib versus methotrexate in Takayasu arteritis: a prospective observational study. Ann Rheum Dis 81:117–123. https://doi.org/10.1136/annrheumdis-2021-220832
Wang J, Dai X, Ma L et al (2022) Efficacy and safety of tofacitinib versus leflunomide with glucocorticoids treatment in Takayasu arteritis: a prospective study. Semin Arthritis Rheum 55:152018. https://doi.org/10.1016/j.semarthrit.2022.152018
Misra DP, Rathore U, Patro P, Agarwal V, Sharma A (2021) Patient-reported outcome measures in Takayasu arteritis: a systematic review and meta-analysis. Rheumatol Ther 8:1073–1093. https://doi.org/10.1007/s40744-021-00355-3
Riley RD, Lambert PC, Abo-Zaid G (2010) Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ 340:c221. https://doi.org/10.1136/bmj.c221
Carmona FD, Coit P, Saruhan-Direskeneli G et al (2017) Analysis of the common genetic component of large-vessel vasculitides through a meta-Immunochip strategy. Sci Rep 7:43953. https://doi.org/10.1038/srep43953
Gribbons KB, Ponte C, Carette S et al (2020) Patterns of arterial disease in Takayasu arteritis and giant cell arteritis. Arthritis Care Res (Hoboken) 72:1615–1624. https://doi.org/10.1002/acr.24055
Grayson PC, Maksimowicz-McKinnon K, Clark TM et al (2012) Distribution of arterial lesions in Takayasu’s arteritis and giant cell arteritis. Ann Rheum Dis 71:1329–1334. https://doi.org/10.1136/annrheumdis-2011-200795
Stamatis P (2020) Giant cell arteritis versus Takayasu arteritis: an update. Mediterr J Rheumatol 31:174–182. https://doi.org/10.31138/mjr.31.2.174
Kermani TA (2019) Takayasu arteritis and giant cell arteritis: are they a spectrum of the same disease? Int J Rheum Dis 22(Suppl 1):41–48. https://doi.org/10.1111/1756-185x.13288
Acknowledgements
Durga Prasanna Misra acknowledges support from Indian Council of Medical Research (Grant No 5/4/1-2/2019-NCD-II) for his research on Takayasu arteritis.
Author information
Authors and Affiliations
Contributions
The conception and design of the study—DPM, VA, AS; acquisition of data, analysis and interpretation of data—DPM, UR, CRK, PP, VA, AS; drafting the article—DPM, UR, CRK, PP; revising it critically for important intellectual content—VA, AS; final approval of the version to be submitted—DPM, UR, CRK, PP, VA, AS; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved—DPM, UR, CRK, PP, VA, AS.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Disclosures
None.
Disclaimer
The funding agency had no role in the actual conduct or reporting of this systematic review.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Misra, D.P., Rathore, U., Kopp, C.R. et al. Presentation and clinical course of pediatric-onset versus adult-onset Takayasu arteritis—a systematic review and meta-analysis. Clin Rheumatol 41, 3601–3613 (2022). https://doi.org/10.1007/s10067-022-06318-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06318-5