Abstract
Purpose of Review
The purpose of this review is to discuss the most recent evidence on the treatment innovations and future prospective in the management of anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitides (AAVs).
Recent Findings
In AAV, a growing body of research is available on novel treatment options for remission induction and to clarify some uncertainties concerning the optimal use of available drugs. Efforts are being made to reduce the toxicity associated with high-dose, prolonged glucocorticoids (GC) regimens. Despite major advances in the prognosis of AAV, relapses are still common and the intensity and duration of remission treatment constitute a great challenge in the management of these chronic conditions.
Summary
A paradigm shift in practice in the management of AAV is being supported by recent evidence suggesting the comparable efficacy and improved safety profile of schemes with a reduced dose of GC for the induction and maintenance of remission in patients with severe granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA). Moreover, recent appraisal of pathogenetic mechanisms, including complement activation pathways, has introduced the revolutionary concept of an alternative to GC, such as avacopan. Plasma exchange failed to prevent end-stage renal disease and mortality in patients with severe renal involvement or pulmonary haemorrhage according to a large multicentre randomised trial. Intensified immunosuppressive strategies for patients with life-threatening manifestations, including the combination of rituximab (RTX) with cyclophosphamide (CYC) have revealed promising preliminary data. New evidence for the use of alternative immunosuppressive agents (e.g. mycophenolate mofetil or abatacept) for the induction of remission in patients with non-severe disease is emerging. Several studies have been recently published, or are ongoing, to assess the optimal strategy and duration of maintenance of remission with the available treatment options (GC, azathioprine, and RTX). Preliminary evidence supports the superiority of a more prolonged course of maintenance treatment. The management of refractory or relapsing eosinophilic granulomatosis with polyangiitis (EGPA) has been improved by the recent demonstration of efficacy and safety of an interleukin-5 inhibitor, mepolizumab. Ongoing randomised studies will clarify the role of RTX in patients with severe manifestations of EGPA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitides (AAVs) has gone through paradigmatic changes over the past years. The prognosis of AAV radically changed since the introduction of glucocorticoids (GC) in the 1950s and the adjunction of cyclophosphamide (CYC) in the 1970s [1] with survival rates now approaching 80% at 10 years of diagnosis [2]. GC and CYC have been the only available options for severe cases of AAV until the first anecdotal reports on the effectiveness of rituximab (RTX) became available in the early 2000s. Only in 2010 the non-inferiority of RTX to CYC was formally demonstrated by two randomised controlled trials (RCT) expanding the therapeutic options for patients with life- or organ-threatening manifestations [3, 4].
Nevertheless, several critical issues remain in the management of AAV: the side effects associated with high-dose GC requirements for remission induction and subsequently the long-term GC regimens needed for the maintenance treatment are still relevant. CYC is associated with an increased risk of cancer development and exposes young patients to the risk of gonadal toxicity leading to infertility. Furthermore, the risk of infections is considerable with all the immunosuppressive drugs available to treat AAV [5]. Moreover, safety needs to be balanced against the need to control disease activity. This has introduced new uncertainty on the optimal frequency and duration of remission maintenance treatments [6, 7].
Novel induction strategies and optimization of maintenance regimens are being investigated by several studies. Evidence to support the use of reduced-dose GC is accumulating. Moreover, pioneer studies to find alternatives (e.g. avacopan) to the long-term use of GC have been recently proposed opening a whole new perspective on the future of AAV treatment and unrevealing innovative pathogenetic mechanisms.
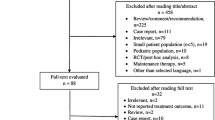
In this review, we will summarise the most recent evidence regarding advances in treatment strategies in AAV (Fig. 1).
Flowchart for the management of ANCA-associated vasculitis based on the available evidence and future perspectives. BVAS, Birmingham Vasculitis Activity Score; SOC, standard of care; GPA, granulomatosis with polyangiitis; MPA, microscopic polyangiitis; EGPA, eosinophilic granulomatosis with polyangiitis; AZA, azathioprine; MTX, methotrexate; RTX, rituximab; MMF, mycophenolate mofetil; LEF, leflunomide; MEPO, mepolizumab; GC, glucocorticoids; ABA, abatacept; TCZ, tocilizumab; BEL, belimumab; CYC, cyclophosphamide; IVIg, intravenous immunoglobulins. #, supported by lower level of evidence; (?), controversial evidence; *, being tested in ongoing trials
Innovations in Induction of Remission Strategies for Granulomatosis with Polyangiitis and Microscopic Polyangiitis
New Insights on the Optimal Dose of Glucocorticoids for Induction of Remission
GC remain the cornerstone of treatment for AAV. To date, the optimal dosing of GC to treat this condition has not been systematically assessed, with significant variability in clinical practice [8, 9••].
In 2019, a retrospective study assessed the use of GC in 114 patients with a newly diagnosed severe AAV. All patients were treated with standard of care for remission induction [CYC, plasma exchange (PLEX), high-dose oral GC], showing no difference in survival rate, risk of relapse or renal outcome, irrespective of whether high-dose intravenous pulses of GC (methylprednisolone 1–3 g) were administered or not. Rather, patients treated with GC pulses more often had infections and steroid-induced diabetes [10•]. An open-label single-arm clinical trial is currently evaluating the safety and efficacy of pulsed GC (methylprednisolone between 1 and 3 g) combined with RTX for remission induction, followed by a tapering dose of oral prednisolone (ClinicalTrials.gov Identifier: NCT02115997).
The LoVAS study is a multicentre RCT aimed at testing the non-inferiority of 0.5 mg/kg versus 1 mg/kg prednisone in combination with RTX for remission induction in AAV (ClinicalTrials.gov Identifier: NCT02198248). Similarly, the SCOUT trial (ClinicalTRials.gov Identifier: NCT02169219) is evaluating whether an 8-week course of GC in combination with RTX is sufficient to induce disease remission which should subsequently be maintained for up to 6 months.
The highest-quality evidence supporting the use of reduced-dose oral GC regimens derives from the PEXIVAS trial (discussed in further detail below) which demonstrated the non-inferiority of lower GC doses compared to standard-dose, while significantly reducing the risk of severe infections.
Revisiting the Role of Plasma Exchange in Severe Cases of AAV
PLEX has traditionally been used as an adjunctive treatment for the management of patients with aggressive, rapidly progressive glomerulonephritis (GN) and/or diffuse alveolar haemorrhage (DAH). The rationale for PLEX is the removal of circulating ANCA in the attempt to reduce their pathogenetic effects; however, other mechanisms may contribute to the therapeutic effect [11]. Previous evidence suggested a role for PLEX in reducing the risk of developing end-stage renal disease (ESRD), but not mortality [12]. Recently, a large, international, RCT (PEXIVAS) has evaluated the role of PLEX and two GC regimens (standard and reduced dose) in patients with severe AAV [estimated glomerular filtration rate (GFR) < 50 ml/min/1.73 m2 of body-surface area, or DAH]. The median creatinine level at study entry was 3.7 mg/dl, with 18.8% of patients requiring dialysis. Pulmonary haemorrhage was found in 27% of enrolled patients; however, the proportion of patients with severe DAH (oxygen saturation ≤ 85% or need for mechanical ventilation) occurred in < 10% in all study participants [13]. Patients were randomly assigned to receive seven PLEX over 14 days or no PLEX, in addition to standard remission induction with CYC or RTX (85% and 15% of patients, respectively). All patients received up to 3 g intravenous GC in the first 3 days, followed by 1 mg/kg of GC for 1-week duration. Subsequently patients were randomised to a standard oral GC regimen (starting with 1 mg/kg prednisone) or a reduced-dose (starting with 0.5mg) tapering regimen. The primary composite outcome of death from any cause or ESRD occurred in 100 of 352 patients (28.4%) in the PLEX group and in 109 of 352 patients (31.0%) in the control group [HR 0.86; 95% confidence interval (0.65, 1.13); p = 0.27]. The reduced-dose oral GC regimen was non-inferior to a standard-dose concerning death and ESRD outcomes, while it significantly reduced the risk of serious infections within the first year of treatment. Among the subgroup analyses that still need to be performed, a stratification of the response to PLEX according to the degree of chronicity of renal disease or the severity of DAH would be of major clinical interest [14]. Nevertheless, PEXIVAS opens new horizons in the management of patients with AAV by supporting the use of reduced-dose GC and discouraging the unconditional use of PLEX in all severe AAV patients.
Exploring New Therapeutic Options to Replace Glucocorticoids: Redefining the Role of Complement
The role of the complement system in the pathogenesis and, subsequently, as a potential therapeutic target, has only recently received increasing attention in the field of AAV. For several decades, the complement system has not been considered relevant in this group of diseases, given the pauci-immune hallmark of histologic findings with absence of complement deposition in affected tissues and the rare detection of hypocomplementemia. Preliminary evidence for a critical role of the alternative complement pathway in the development of glomerulonephritis induced by anti-myeloperoxidase antibody came from animal models demonstrating that genetic absence or pharmacological inhibition of C5a receptor1 (C5aR1) significantly reduced antibody production and intra-renal neutrophil activation and damage [15, 16]. Moreover, C5a has been implicated in the priming and activation of neutrophils and interference with their activity, especially in the presence of ANCA, and with endothelial activation. Subsequently, the presence of complement activation products has been confirmed on renal biopsies of AAV patients and on urinary and serum samples, demonstrating an association of complement activation with disease severity [17]. Finally, hypocomplementemia has been linked to a worse renal prognosis in observational studies of AAV [18, 19].
The first clinical trial testing the role complement-targeted therapies has introduced the revolutionary concept of replacing GC by complement inhibitors to treat patients with severe forms of AAV. CCX168 (avacopan), an oral small molecule inhibiting the complement C5a receptor, has been evaluated in the CLEAR study, a RCT on 67 patients with newly diagnosed or relapsing AAV. The study investigated whether different regimens of GC (standard dose, reduced dose, and no prednisone), added to a standard induction with CYC or RTX, could be replaced by CCX168 without compromising the efficacy of remission induction [20••]. Avacopan was non-inferior to standard therapy in achieving a treatment response [defined as a Birmingham Vasculitis Activity Score (BVAS) decrease of at least 50% and no worsening of any-body system between baseline and 12 weeks]. Treatment response occurred in 86.4% of patients treated with avacopan and reduced-dose GC, 81% of the patients receiving avacopan with no GC, and 70% in the high-dose GC control group. Albuminuria and levels of a renal inflammation marker [urinary creatinine-corrected monocyte chemoattractant protein-1 (MCP-1)] improved to a greater extent in the avacopan than in control groups, while eGFR and hematuria improved similarly in all treatment group. Health-related quality of life also significantly improved with avacopan. No safety concerns were reported [20••].
Another phase 2 randomised 12-week study (CLASSIC trial) evaluated two different doses of avacopan (10 or 30 mg twice daily) in adjunction to standard of care (induction with GC and CYC or RTX), compared to standard of care alone in newly diagnosed or relapsing AAV patients (n=42). Adverse events rates were similar across the three treatment groups. Early achievement of remission within the first month of treatment was numerically superior with avacopan 30 mg (20% of patients) compared to avacopan 10 mg (8% of patients) and standard of care (15%). Renal response was highest in the avacopan 30 mg compared to the other groups (63% with avacopan 30 mg, 40% with avacopan 10 mg, 17% with standard of care; p = 0.03). A variety of patient-reported outcomes including health-related quality of life significantly improved in the avacopan group compared to standard of care only [21].
A phase III trial is ongoing (ClinicalTrials.gov Identifier: NCT02994927) [22] to evaluate if avacopan can replace the need for chronic GC in the treatment of AAV. Other C5a inhibitors are under development (ClinicalTrials.gov Identifier: NCT03895801 and NCT03712345).
Unresolved Issues and Combination Strategies with Rituximab
B-cell depletion by RTX has proved its efficacy in the management of severe granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA). Nevertheless, some questions remain open concerning the efficacy of this drug in certain subpopulations such as DAH requiring mechanical ventilation or patients with severe renal involvement. These patients were either excluded from RTX trials or were concomitantly treated with a short-course of i.v. CYC [3, 4]. A recent observational study reported a comparable response-rate in patients with severe renal function impairment (GFR < 30 ml/min) when comparing RTX with CYC [23].
The role of combined therapy with RTX and CYC for remission induction in patients with life-threatening manifestations is elusive so far. A retrospective study concluded that the combination of RTX and low-dose oral CYC (2.5 mg/kg/day for one week, followed by 1.5 mg/kg/day for 7 weeks) was effective for induction of remission in severe manifestations of AAV. Neutropenia occurred in 8.5% of patients leading to an increased risk of serious infections [24].
A single-centre cohort study including 66 patients with renal involvement in AAV investigated a combination of oral GC, RTX, and low-dose pulsed intravenous CYC (10 mg/kg) followed by maintenance with azathioprine (AZA) and GC. The 66 included patients were assessed with a case-control analysis with propensity-matched patients included in the EUVAS trials and treated with either RTX or CYC to compare outcomes (relapse-free-, renal- and patient-survival). The group of patients treated with combined RTX + CYC had a significant reduced risk of death, ESRD, and relapse compared to the control group treated with either agent alone from the EUVAS trials cohort [25].
ENDURRANCE-1 trial is an ongoing RCT with the aim of comparing RTX plus CYC with RTX alone for remission induction in patients with severe AAV (ClinicalTrials.gov Identifier: NCT03942887).
Belimumab is a human monoclonal antibody inhibiting BLyS that has been approved for treatment of patients with systemic lupus erythematosus, which could potentially be effective also in AAV based on the hypothesised benefit of targeting B-cell cytokines such as BLyS known to be present at high concentrations in patients with AAV [26]. A randomised, double blind, controlled trial is currently evaluating whether in patients with proteinase 3 (PR3)-AAV, dual B-cell immunotherapy by co-administration of RTX and belimumab will improve remission induction as compared to RTX with placebo (COMBIVAS study, ClinicalTrials.gov Identifier: NCT03967925).
Evidence for New Induction of Remission Strategies
A non-inferiority RCT (MYCYC) compared mycophenolate mofetil (MMF) to intravenous CYC as an induction therapy in 140 patients with new-onset GPA or MPA. Patients with impending life-threatening disease, rapidly declining renal function or GFR <15 ml/min were excluded [27•]. MMF was non-inferior to CYC to induce remission, despite higher relapse rates in the PR3-ANCA subgroup treated with MMF.
Another non-inferiority RCT trial including 84 patients with non-life-threatening relapses of GPA/MPA compared MMF with intravenous CYC for remission induction [28]. Most patients were PR3-ANCA positive (89%) and had kidney involvement (75%). All participants were switched to maintenance therapy with AZA. MMF was non-inferior to CYC to induce remission at 6 months. At 4 years, relapse rate was similar in both groups, and there were no relevant safety issues. Therefore, remission induction with MMF in patients without severe renal involvement might be a viable option, especially in MPA/MPO-ANCA patients.
A small open-label trial with abatacept (intravenous infusions, 10 mg/kg) was conducted for non-severe relapsing GPA (n = 20 patients), with encouraging results in terms of disease remission (80% of patients achieving BVAS/WG = 0 at a median of 1.9 months) and steroid sparing effect, with 73% of patients being able to discontinue GC [29]. The efficacy of this therapeutic approach for non-severe relapsing GPA is being evaluated in an ongoing RCT (ABROGATE study, ClinicalTrials.gov Identifier: NCT02108860).
There is growing evidence resulting from uncontrolled observational studies that IL-6 pathway blockade could be an effective therapeutic option for patients with AAV. Recently, serum IL-6 concentrations have been correlated with PR3-ANCA titres and clinical manifestations of AAV [30, 31]. The role of tocilizumab (TCZ) has been investigated in a small pilot study in six MPA patients without concomitant GC treatment [32]. Two and three patients were able to achieve complete remission at 6 and 12 months, respectively. A Japanese randomised trial comparing TCZ with CYC for remission induction in GPA and MPA patients is still ongoing [33].
The effect of hydroxychloroquine or placebo, in addition to maintenance treatment is currently tested in patients with GPA, MPA, and eosinophilic granulomatosis with polyangiitis (EGPA) without organ-threatening relapses in the HAVEN trial (ClinicalTrials.gov Identifier: NCT04316494).
A recent meta-analysis explored the role of intravenous immunoglobulins (IVIG) in active AAV. To assess the specific efficacy of IVIG, avoiding the confounding effect of concomitant immunosuppressants, a subgroup analysis including a small number of patients with stable concomitant treatment in the weeks preceding the administration of IVIG was performed. BVAS, but not ANCA titres, nor C-reactive protein (CRP), significantly decreased after the administration of IVIG [34]. Further RCTs are necessary to investigate the possible role of IVIG in patients with AAV. An overview of published studies supporting novel evidence for induction strategies in AAV is presented in Table 1.
Innovations in Maintenance of Remission Strategies for Granulomatosis with Polyangiitis and Microscopic Polyangiitis
After successful achievement of remission, maintenance immunosuppressive treatment should be initiated with the aim of reducing relapse risk, tapering GC treatment, and minimising the burden of damage during follow-up. Several open questions remain on the optimal duration and intensity of maintenance therapeutic schemes. An overview of published evidence on maintenance of remission strategies is presented in Table 2.
Novel Evidence on the Optimal Duration of Maintenance Immunosuppressive Treatment
The ideal length of maintenance therapy is unknown. According to EULAR/EDTA recommendations, immunosuppressive treatment should be continued for at least 24 months after induction of sustained remission [43]. According to recent studies, a longer maintenance strategy might be more efficacious and safe than a shorter treatment duration. In a retrospective study including 157 remitted patients with GPA for example, prolonged maintenance treatment with AZA or methotrexate (MTX) lasting ≥ 36 months led to a 66% reduction of a relapse (HR, 0.59; 95% CI 0.42–0.83; p = 0.003) [35]. Notably, more than 50% of relapses occurred after treatment withdrawal and a significant proportion of relapsing patients were taking MTX dose < 15 mg/week or an AZA dose ≤ 50 mg/day. Recently, the REMAIN trial reported a lower relapse rate at 48 months following complete remission induction with CYC and GC in patients with GPA, MPA and renal-limited vasculitis treated with a longer course of AZA and GC (48 months), as compared to patients who stopped maintenance therapy after 18–24 months (22.0% vs 62.7%, respectively, p < 0.001). Persistent ANCA-positivity at 2 years correlated with a higher relapse risk [36••].
The continuation of immunosuppressive treatment in AAV patients with ESRD represents a matter of debate, as the risk of severe infections needs to be balanced against the risk of potentially severe relapse. MASTER-ANCA (ClinicalTrials.gov Identifier: NCT03323476) is a RCT with the aim of demonstrating the superiority of immunosuppressive treatment discontinuation compared with standard maintenance therapy in AAV patients reaching ESRD in terms of severe prejudicial events, defined as both severe infections and major relapses.
Ongoing Evolving Evidence Supporting the Duration and Timing for Rituximab Maintenance Treatment
In the MAINRITSAN trial, RTX demonstrated its superiority over AZA in maintaining remission at 28 months in patients affected with GPA and MPA, following remission induction with CYC [37]. In the long-term analysis of this cohort, RTX confirmed its higher efficacy at 60 months, although the risk for major relapses was similar in both groups between months 28 and 60 (17% for the AZA arm vs 23% for the RTX arm) [38••]. Treatment with RTX correlated with a higher survival rate, while persistent ANCA-positivity was a predictor of subsequent relapse. Relapse rate rapidly increased in the 12 months following AZA withdrawal, whereas most relapses in RTX-treated patients developed 18–24 months after the last administration, highlighting a more sustained effect of RTX on disease activity. RITAZAREM trial (ClinicalTrials.gov Identifier: NCT01697267) compared RTX with AZA in remission maintenance of relapsing GPA and MPA. However, this trial included 170 relapsing patients requiring remission re-induction treatment with RTX, followed by a different treatment schedule than that of the MAINRITSAN trial: RTX 1000 mg every 4 months for five doses [44••]. Despite these successful results, a standardised duration and timing of RTX administration is not yet available.
The MAINRITSAN 2 trial evaluated the role of two different RTX regimens in the prevention of relapses in 162 GPA and MPA remitted patients [39]: 500 mg infusions according to ANCA increase/return and/or circulating CD19 B-cell repopulation, versus regular 500 mg infusions at fixed intervals of 6 months. Although relapse rate did not differ between the two groups (17% in the experimental group vs 9.9% in the control group, p = 0.2), patients in the experimental arm received fewer infusions and lower total RTX doses. The maintenance of remission strategy with RTX to ensure the best relapse-free survival is being evaluated in the MAINTANCAVAS (ClinicalTrials.gov Identifier: NCT02749292), an open-label, RCT comparing the re-administration of RTX based on B-cell reconstitution versus serologic ANCA flare.
Furthermore, a 4-year maintenance treatment with fixed RTX infusions (every 6 months) has been compared with a 2-year treatment schedule in the MAINRITSAN 3 trial [40]. The results of this trial, which included 97 patients with GPA and MPA, demonstrated a higher relapse-free survival rate in patients who underwent a longer maintenance treatment with RTX, compared with standard maintenance therapy (96% vs 74%, HR 7.5, p = 0.008).
New Insights on the Optimal Dose of Glucocorticoids for Maintenance of Remission
As the prognosis of AAV significantly improved in the last decades, long-term management of AAV should focus on minimising treatment-related morbidity, including chronic GC toxicity. The optimal duration of GC treatment and its effect on disease relapses, however, remain to be elucidated. A meta-analysis including 983 patients reported a lower relapse rate in patients undergoing longer courses of GC (≥12 months) than patients who stopped GC treatment prior to 12 months [45].
The optimal duration of GC therapy in AAV is being addressed by two ongoing studies. The TAPIR trial (ClinicalTrials.gov Identifier: NCT01933724) is an open-label study comparing the continuation of low dose GC (5 mg/day) for 6 months with the discontinuation of GC in remitted GPA patients who required in the previous 12 months a GC dose ≥ 20 mg/day. The MAINEPSAN trial (ClinicalTrials.gov Identifier: NCT03290456) aims at assessing in patients with GPA and MPA the effect of low dose GC treatment (5 mg/day) for the 12 months following diagnosis on the relapse rate as compared to GC cessation after 1 month.
Novel Therapeutic Options for the Maintenance of Remission
The role of belimumab has been tested against placebo in the BREVAS trial, a RCT including 105 GPA and MPA patients receiving maintenance treatment with AZA (2 mg/kg/day) and low dose GC (≤10 mg/day) following successful remission induction with RTX or CYC [42]. In this study, patient enrollment was prematurely interrupted, in part due to changes in treatment practice. Nevertheless, preliminary evidence suggested that the addition of belimumab (10 mg/kg/month intravenously) to AZA and GC did not result in a reduction of the relapse risk (18.9% in the belimumab group vs 21.2% in the placebo group, HR 0.88, 95% CI 0.29–2.65; p = 0.821).
Reconsidering the Role of Trimethoprim-sulphametoxazole
Trimethoprim-sulphametoxazole (TMP-SMX) is an antibiotic that is recommended in the prophylaxis of Pneumocystis jirovecii pneumonia in patients undergoing remission induction treatment with CYC or RTX [43]. A rationale for the anti-microbial and/or anti-inflammatory role of TMP-SMX in GPA arises from the assumption that the nasal carriage of Staphylococcus aureus (SA) is associated with the risk of relapses exists [46,47,48]. Previous evidence, including data from a RCT, supported the concept that the administration of TMP-SMX could lead to a reduction of relapses in patients with GPA [49,50,51,52,53]. In a recent study from the French Vasculitis Study Group, no differences were observed between AAV patients with or without nasal carriage of SA concerning relapse rate even if SA was more prevalent among vasculitis patients than controls. TMP-SMX decreased the occurrence of nasal carriage but this did not affect the relapse rate [54]. Based on these contradictory results, there is insufficient evidence to recommend TMP-SMX monotherapy to maintain remission in AAV. A systematic literature review and meta-analysis of the available evidence on the efficacy of TMP-SMX on relapse occurrence and infectious risk is ongoing and will inform clinical practice (Prospero Identifier: CRD42019118983). The effect of a 4-week course of TMP-SMX on the nasal microbiome and host immunity of GPA patients will be investigated in the TEMPO trial (ClinicalTrials.gov Identifier: NCT03919435).
Novel Evidence for the Treatment of Eosinophilic Granulomatosis with Polyangiitis
Over the last decade, research on EGPA treatment has been focused on the role of eosinophils in its pathogenesis, as well as on refractory manifestations such as asthma and ear-nose-throat (ENT) involvement [55]. As IL-5 is the most powerful eosinophil activator, anti-IL-5 inhibitors, already successfully used for the treatment of severe asthma, have shown efficacy in the management of refractory/relapsing patients with EGPA, leading to the approval of the first drug for treatment of EGPA, mepolizumab (MEPO).
Mepolizumab
A 52-week randomised placebo-controlled trial (MIRRA) investigating the efficacy and safety of MEPO (300 mg subcutaneously every 4 weeks) in addition to standard of care treatment in relapsing or refractory EGPA showed a lower relapse rate and a higher GC-sparing effect of MEPO as compared to placebo [56••]. Longer accrued weeks of remission were significantly associated with the former treatment (OR 5.91; 95% CI 2.68, 13.03; p < 0.001). Nevertheless, remission (defined as BVAS = 0 and GC ≤ 4 mg/day over a 52-week period) still did not occur in 47% of participants in the MEPO group and in 81% in the placebo group. A post-hoc analysis of the clinical benefit of MEPO using a different comprehensive definition of benefit including remission [two definitions: (1) BVAS = 0 with GC ≤ 4 mg/day; (2) BVAS = 0 with GC ≤ 7.5 mg/day], ≥ 50% GC dose reduction, and no relapses, led to significantly higher frequencies of clinical benefit obtained with MEPO (ranging 78–87% of patients included in the trial) [57]. An extension of the MIRRA trial is ongoing to investigate the long-term effect of MEPO (ClinicalTrials.gov Identifier: NCT03298061). The majority of patients included in the MIRRA trial had asthma, pulmonary, and sinonasal involvement, while more severe manifestations (e.g. cardiomyopathy, glomerulonephritis, DAH) were rare. Hence, the efficacy of MEPO in severe cases of EGPA requires further studies [58, 59]. An ongoing European collaborative real-life observational project (the European EGPA Study Group) has confirmed in 142 patients positive effects of MEPO on systemic disease manifestations including neurological symptoms, pulmonary and ENT involvement [60].
Other Interleukin-5 Inhibitors
There are two ongoing RCTs assessing the role of reslizumab (an anti-IL5 humanised monoclonal antibody) and benralizumab (an anti-IL5-receptor humanised monoclonal antibody) in the treatment of patients with EGPA (ClinicalTrials.gov Identifier: NCT02947945 and NCT03010436, respectively). Moreover, a randomised double-blind active-controlled 52-week study (ClinicalTrials.gov Identifier: NCT04157348) with an open-label extension is being conducted with the aim of evaluating the efficacy and safety of benralizumab compared to MEPO as add-on therapy to the standard of care in EGPA patients.
Preliminary Observational Evidence on Omalizumab
Omalizumab, an anti-IgE humanised monoclonal antibody, is currently used in patients with IgE-mediated asthma. However, no RCTs have investigated its role in EGPA. Detoraki et al. evaluated the efficacy and safety of omalizumab in a 36-month observational study including 5 EGPA patients, demonstrating an improvement of pulmonary function, a diminished eosinophil count and successful GC tapering [61]. Similar results were reported in two other small case series [62, 63]. Nevertheless, in a case series of 17 EGPA patients, omalizumab was discontinued in 4 patients due to disease relapses and in 2 due to refractory disease [62]. Indeed, omalizumab has been linked to the potential occurrence of EGPA in patients with severe asthma, although this observation might have been confounded by a prompt discontinuation of GC in these patients [64, 65].
Rituximab for the Management of Severe Manifestations of Eosinophilic Granulomatosis with Polyangiitis
In retrospective cohort studies, RTX has shown effectiveness in controlling disease manifestations and revealed GC-sparing effects in patients with EGPA with refractory or relapsing course, especially in patients with ANCA positivity [66, 67]. Nevertheless, data from a retrospective cohort of 69 patients (35% ANCA positive) treated with RTX for refractory/frequently relapsing EGPA or contraindication to CYC showed high rates of asthma/ENT relapses even if RTX resulted in overall improvement of the disease in over 90% of patients by 24 months [67].
Patients with EGPA were excluded from RAVE and RITUXVAS trials leading to the approval of RTX only for severe cases of GPA and MPA [3, 4]. According to the EULAR/EDTA recommendations for the management of AAV, the use of RTX as a remission-induction therapy for EGPA is supported by a lower level of evidence derived from observational data only [68]. In 2016 and 2017, the French Vasculitis Study Group proposed two RCTs to assess the efficacy of RTX as compared to CYC in the induction of remission in newly diagnosed or relapsing patients with EGPA (REOVAS, ClinicalTrials.gov Identifier: NCT02807103) and as a maintenance of remission treatment (MAINRITSEG, ClinicalTrials.gov Identifier: NCT03164473) in comparison to AZA.
Conclusions
The management of patients with AAV has gone through remarkable advances over the past few years. Novel strategies for induction of remission are now available, and a number of ongoing RCT will likely expand the treatment options in the near future. The optimal length of maintenance immunosuppressive treatment to prevent relapses, as well as the intensity of specific target therapies administration is still debated and will be further clarified by the results of ongoing studies. Finally, new therapeutic strategies are being investigated in order to induce and maintain remission over time and provide a viable alternative to traditional immunosuppressants and even to GC.
GPA, granulomatosis with polyangiitis; MPA, microscopic polyangiitis; EGPA, eosinophilic granulomatosis with polyangiitis; MMF, mycophenolate mofetil; CYC, cyclophosphamide; AZA, azathioprine; MTX, methotrexate; RTX, rituximab; RCT, randomised controlled trial; IVIG, intravenous immunoglobulins; NA, not available; TCZ, tocilizumab
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fauci AS, Katz P, Haynes BF, Wolff SM. Cyclophosphamide therapy of severe systemic necrotizing vasculitis. N Engl J Med. 1979;301:235–8.
Flossmann O, Berden A, de Groot K, Hagen C, Harper L, Heijl C, et al. Long-term patient survival in ANCA-associated vasculitis. Ann Rheum Dis. 2011;70:488–94.
Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363:221–32.
Jones RB, Tervaert JWC, Hauser T, Luqmani R, Morgan MD, Peh CA, et al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med. 2010;363:211–20.
Lafarge A, Joseph A, Pagnoux C, Puéchal X, Cohen P, Samson M, et al. Predictive factors of severe infections in patients with systemic necrotizing vasculitides: data from 733 patients enrolled in five randomized controlled trials of the French Vasculitis Study Group. Rheumatol Oxf Engl. 2020;59:2250–7.
Cornec D, Cornec-Le Gall E, Specks U. Clinical trials in antineutrophil cytoplasmic antibody-associated vasculitis: what we have learnt so far, and what we still have to learn. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc. 2017;32:i37–47.
Monti S, Quinn KA, Christensen R, Jayne D, Langford C, Lanier GE, et al. Use and reporting of outcome measures in randomized trials for anti-neutrophil cytoplasmic antibody-associated vasculitis: a systematic literature review of randomized trials. Semin Arthritis Rheum. 2020;50:1314–25.
Furuta S, Sugiyama T, Umibe T, Kaneko Y, Amano K, Kurasawa K, et al. Low-dose glucocorticoids plus rituximab versus high-dose glucocorticoids plus rituximab for remission induction in ANCA-associated vasculitis (LoVAS): protocol for a multicentre, open-label, randomised controlled trial. BMJ Open [Internet]. 2017 [cited 2019 Oct 15];7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5778278/
•• Walsh M, Merkel PA, Peh C-A, Szpirt WM, Puéchal X, Fujimoto S, et al. Plasma exchange and glucocorticoids in severe ANCA-associated vasculitis. N Engl J Med. 2020;382:622–31 PEXIVAS opens new horizons on the management of patients with AAV by supporting the use of reduced-dose glucocorticoids and challenging the role of PLEX.
• Chanouzas D, McGregor JAG, Nightingale P, Salama AD, Szpirt WM, Basu N, et al. Intravenous pulse methylprednisolone for induction of remission in severe ANCA associated vasculitis: a multi-center retrospective cohort study. BMC Nephrol. 2019;20:–58 This study demonstrated that glucocorticoids pulses are not associated with better disease outcomes, but with a greater infections risk.
Casian A, Jayne D. Plasma exchange in the treatment of Wegener’s granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome and renal limited vasculitis. Curr Opin Rheumatol. 2011;23:12–7.
Jayne DRW, Gaskin G, Rasmussen N, Abramowicz D, Ferrario F, Guillevin L, et al. Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. J Am Soc Nephrol JASN. 2007;18:2180–8.
Cortazar FB, Niles JL. The fate of plasma exchange and glucocorticoid dosing in ANCA-associated vasculitis after PEXIVAS. Am J Kidney Dis Off J Natl Kidney Found. 2020;76:595–7.
Morris A, Geetha D. PEXIVAS challenges current ANCA-associated vasculitis therapy. Nat Rev Nephrol. 2020;16:373–4.
Dick J, Gan P-Y, Ford SL, Odobasic D, Alikhan MA, Loosen SH, et al. C5a receptor 1 promotes autoimmunity, neutrophil dysfunction and injury in experimental anti-myeloperoxidase glomerulonephritis. Kidney Int. 2018;93:615–25.
Kallenberg CGM, Heeringa P. Complement system activation in ANCA vasculitis: a translational success story? Mol Immunol. 2015;68:53–6.
Quintana LF, Kronbichler A, Blasco M, Zhao M-H, Jayne D. ANCA associated vasculitis: the journey to complement-targeted therapies. Mol Immunol. 2019;112:394–8.
Deshayes S, Aouba A, Khoy K, Mariotte D, Lobbedez T, Martin SN. Hypocomplementemia is associated with worse renal survival in ANCA-positive granulomatosis with polyangiitis and microscopic polyangiitis. PLoS One. 2018;13:e0195680.
Manenti L, Vaglio A, Gnappi E, Maggiore U, Allegri L, Allinovi M, et al. Association of serum C3 concentration and histologic signs of thrombotic microangiopathy with outcomes among patients with ANCA-associated renal vasculitis. Clin J Am Soc Nephrol CJASN. 2015;10:2143–51.
•• Jayne DRW, Bruchfeld AN, Harper L, Schaier M, Venning MC, Hamilton P, et al. Randomized trial of C5a receptor inhibitor avacopan in ANCA-associated vasculitis. J Am Soc Nephrol JASN. 2017;28:2756–67 First study to report the efficacy of avacopan and introducing the concept of an alternative to glucocorticoids in the management of AAV.
Merkel PA, Niles J, Jimenez R, Spiera RF, Rovin BH, Bomback A, et al. Adjunctive treatment with avacopan, an oral C5a receptor inhibitor, in patients with antineutrophil cytoplasmic antibody-associated vasculitis. ACR Open Rheumatol. 2020;2:662–71.
Merkel PA, Jayne DR, Wang C, Hillson J, Bekker P. Evaluation of the safety and efficacy of avacopan, a C5a receptor inhibitor, in patients with antineutrophil cytoplasmic antibody-associated vasculitis treated concomitantly with rituximab or cyclophosphamide/azathioprine: protocol for a randomized, double-blind, active-controlled, phase 3 trial. JMIR Res Protoc. 2020;9:e16664.
Moura MC, Irazabal MV, Eirin A, Zand L, Sethi S, Borah BJ, et al. Efficacy of rituximab and plasma exchange in antineutrophil cytoplasmic antibody–associated vasculitis with severe kidney disease. J Am Soc Nephrol. 2020;31:2688–704.
Cortazar FB, Muhsin SA, Pendergraft WF, Wallace ZS, Dunbar C, Laliberte K, et al. Combination therapy with rituximab and cyclophosphamide for remission induction in ANCA vasculitis. Kidney Int Rep. 2018;3:394–402.
McAdoo SP, Medjeral-Thomas N, Gopaluni S, Tanna A, Mansfield N, Galliford J, et al. Long-term follow-up of a combined rituximab and cyclophosphamide regimen in renal anti-neutrophil cytoplasm antibody-associated vasculitis. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc. 2019;34:63–73.
McClure M, Gopaluni S, Jayne D, Jones R. B cell therapy in ANCA-associated vasculitis: current and emerging treatment options. Nat Rev Rheumatol. 2018;14:580–91.
• Jones RB, Hiemstra TF, Ballarin J, Blockmans DE, Brogan P, Bruchfeld A, et al. Mycophenolate mofetil versus cyclophosphamide for remission induction in ANCA-associated vasculitis: a randomised, non-inferiority trial. Ann Rheum Dis. 2019;78:399–405 Supports the role of mycophenolate as induction of remission strategy for AAV.
Tuin J, Stassen PM, Bogdan DI, Broekroelofs J, van Paassen P, Cohen Tervaert JW, et al. Mycophenolate mofetil versus cyclophosphamide for the induction of remission in nonlife-threatening relapses of antineutrophil cytoplasmic antibody-associated vasculitis: randomized, controlled trial. Clin J Am Soc Nephrol CJASN. 2019;14:1021–8.
Langford CA, Monach PA, Specks U, Seo P, Cuthbertson D, McAlear CA, et al. An open-label trial of abatacept (CTLA4-IG) in non-severe relapsing granulomatosis with polyangiitis (Wegener’s). Ann Rheum Dis. 2014;73:1376–9.
Berti A, Cavalli G, Campochiaro C, Guglielmi B, Baldissera E, Cappio S, et al. Interleukin-6 in ANCA-associated vasculitis: rationale for successful treatment with tocilizumab. Semin Arthritis Rheum. 2015;45:48–54.
Sakai R, Ito M, Yoshimoto K, Chikuma S, Kurasawa T, Kondo T, et al. Tocilizumab monotherapy uncovered the role of the CCL22/17-CCR4+ Treg axis during remission of crescentic glomerulonephritis. Clin Transl Immunol. 2020;9:e1203.
Sakai R, Kondo T, Kikuchi J, Shibata A, Chino K, Okuyama A, et al. Corticosteroid-free treatment of tocilizumab monotherapy for microscopic polyangiitis: a single-arm, single-center, clinical trial. Mod Rheumatol. 2016;26:900–7.
JPRN-JMA-IIA00325. Clinical trial of tocilizumab versus cyclophosphamide for microscopic polyangiitis and granulomatosis with polyangiitis. Httpwwwwhointtrialsearchtrial2aspx Trialidjprn-Jma-Iia00325 [Internet]. 2019 [cited 2019 Jun 8]; Available from: https://www.cochranelibrary.com/central/doi/10.1002/central/CN-01901006/full
Shimizu T, Morita T, Kumanogoh A. The therapeutic efficacy of intravenous immunoglobulin in anti-neutrophilic cytoplasmic antibody-associated vasculitis: a meta-analysis. Rheumatol Oxf Engl. 2020;59:959–67.
Springer J, Nutter B, Langford CA, Hoffman GS, Villa-Forte A. Granulomatosis with polyangiitis (Wegener’s): impact of maintenance therapy duration. Medicine (Baltimore). 2014;93:82–90.
•• Karras A, Pagnoux C, Haubitz M, Groot K, de Puechal X, Tervaert JWC, et al. Randomised controlled trial of prolonged treatment in the remission phase of ANCA-associated vasculitis. Ann Rheum Dis. 2017;76:1662–8 Supports the efficacy and safety of a more prolonged remission maintenance treatment with azathioprine.
Guillevin L, Pagnoux C, Karras A, Khouatra C, Aumaître O, Cohen P, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014;371:1771–80.
•• Terrier B, Pagnoux C, Perrodeau É, Karras A, Khouatra C, Aumaître O, et al. Long-term efficacy of remission-maintenance regimens for ANCA-associated vasculitides. Ann Rheum Dis. 2018;77:1150–6 Supports the efficacy and safety of a more prolonged remission maintenance treatment with rituximab.
Charles P, Terrier B, Perrodeau É, Cohen P, Faguer S, Huart A, et al. Comparison of individually tailored versus fixed-schedule rituximab regimen to maintain ANCA-associated vasculitis remission: results of a multicentre, randomised controlled, phase III trial (MAINRITSAN2). Ann Rheum Dis. 2018;77:1143–9.
Charles P, Perrodeau É, Samson M, Bonnotte B, Néel A, Agard C, et al. Long-term rituximab use to maintain remission of antineutrophil cytoplasmic antibody-associated vasculitis: a randomized trial. Ann Intern Med. 2020;173:179–87.
Smith R, Jayne D, Merkel PA, on behalf of RITAZAREM Investigators. OP0026 a randomized, controlled trial of rituximab versus azathioprine after induction of remission with rituximab for patients with ANCA-associated vasculitis and relapsing disease. Ann Rheum Dis. 2020;79:19–20.
Jayne D, Blockmans D, Luqmani R, Moiseev S, Ji B, Green Y, et al. Efficacy and safety of belimumab and azathioprine for maintenance of remission in antineutrophil cytoplasmic antibody-associated vasculitis: a randomized controlled study. Arthritis Rheumatol Hoboken NJ. 2019;71:952–63.
Yates M, Watts RA, Bajema IM, Cid MC, Crestani B, Hauser T, et al. EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis. 2016;75:1583–94.
•• Gopaluni S, Smith RM, Lewin M, McAlear CA, Mynard K, Jones RB, et al. Rituximab versus azathioprine as therapy for maintenance of remission for anti-neutrophil cytoplasm antibody-associated vasculitis (RITAZAREM): study protocol for a randomized controlled trial. Trials. 2017;18:112 Supports the efficacy and safety of rituximab for the induction and maintenance of remission in AAV.
Walsh M, Merkel PA, Mahr A, Jayne D. Effects of duration of glucocorticoid therapy on relapse rate in antineutrophil cytoplasmic antibody-associated vasculitis: a meta-analysis. Arthritis Care Res. 2010;62:1166–73.
Pinching AJ, Rees AJ, Pussell BA, Lockwood CM, Mitchison RS, Peters DK. Relapses in Wegener’s granulomatosis: the role of infection. Br Med J. 1980;281:836–8.
Stegeman CA, Tervaert JW, Sluiter WJ, Manson WL, de Jong PE, Kallenberg CG. Association of chronic nasal carriage of Staphylococcus aureus and higher relapse rates in Wegener granulomatosis. Ann Intern Med. 1994;120:12–7.
Salmela A, Rasmussen N, Tervaert JWC, Jayne DRW, Ekstrand A, European Vasculitis Study Group. Chronic nasal Staphylococcus aureus carriage identifies a subset of newly diagnosed granulomatosis with polyangiitis patients with high relapse rate. Rheumatol Oxf Engl. 2017;56:965–72.
DeRemee RA. The treatment of Wegener’s granulomatosis with trimethoprim/sulfamethoxazole: illusion or vision? Arthritis Rheum. 1988;31:1068–74.
Fukuda K, Yuasa K, Uchizono A, Matsuyama H, Shimada K, Ohyama M. Three cases of Wegener’s granulomatosis treated with an antimicrobial agent. Arch Otolaryngol Head Neck Surg. 1989;115:515–8.
Reinhold-Keller E, De Groot K, Rudert H, Nölle B, Heller M, Gross WL. Response to trimethoprim/sulfamethoxazole in Wegener’s granulomatosis depends on the phase of disease. QJM Mon J Assoc Physicians. 1996;89:15–23.
Zycinska K, Wardyn KA, Zielonka TM, Krupa R, Lukas W. Co-trimoxazole and prevention of relapses of PR3-ANCA positive vasculitis with pulmonary involvement. Eur J Med Res. 2009;14(Suppl 4):265–7.
Stegeman CA, Tervaert JW, de Jong PE, Kallenberg CG. Trimethoprim-sulfamethoxazole (co-trimoxazole) for the prevention of relapses of Wegener’s granulomatosis. Dutch Co-Trimoxazole Wegener Study Group. N Engl J Med. 1996;335:16–20.
Tan BK, Crabol Y, Tasse J, Laurent F, Nekkab N, Vinter C, et al. No evident association of nasal carriage of Staphylococcus aureus or its small-colony variants with cotrimoxazole use or ANCA-associated vasculitis relapses. Rheumatol Oxf Engl. 2020;59:77–83.
Berti A, Specks U, Keogh K, Cornec D. Current and future treatment options for eosinophilic granulomatosis with polyangiitis. Curr Treat Options Rheumatol. 2017;3:1–14.
•• Wechsler ME, Akuthota P, Jayne D, Khoury P, Klion A, Langford CA, et al. Mepolizumab or placebo for eosinophilic granulomatosis with polyangiitis. N Engl J Med. 2017;376:1921–32 First trial to demonstrate the efficacy of mepolizumab in EGPA leading to the first targeted-treatment for EGPA.
Steinfeld J, Bradford ES, Brown J, Mallett S, Yancey SW, Akuthota P, et al. Evaluation of clinical benefit from treatment with mepolizumab for patients with eosinophilic granulomatosis with polyangiitis. J Allergy Clin Immunol. 2019;143:2170–7.
Guillevin L. Mepolizumab for eosinophilic granulomatosis with polyangiitis. Nat Rev Rheumatol Nature Publishing Group. 2017;13:518–9.
Ennis D, Lee JK, Pagnoux C. Mepolizumab for the treatment of eosinophilic granulomatosis with polyangiitis. Expert Opin Biol Ther. 2019;19:617–30.
Bettiol A, Urban ML, Alberici F, Agostini C, Baldini C, Bozzolo E, et al. Op0148 Mepolizumab for eosinophilic granulomatosis with polyangiitis (egpa): a retrospective real-world European study on 142 patients. Ann Rheum Dis BMJ Publishing Group Ltd. 2020;79:94–5.
Detoraki A, Di Capua L, Varricchi G, Genovese A, Marone G, Spadaro G. Omalizumab in patients with eosinophilic granulomatosis with polyangiitis: a 36-month follow-up study. J Asthma Off J Assoc Care Asthma. 2016;53:201–6.
Jachiet M, Samson M, Cottin V, Kahn J-E, Le Guenno G, Bonniaud P, et al. Anti-IgE monoclonal antibody (omalizumab) in refractory and relapsing eosinophilic granulomatosis with polyangiitis (Churg-Strauss): data on seventeen patients. Arthritis Rheum Hoboken NJ. 2016;68:2274–82.
Celebi Sozener Z, Gorgulu B, Mungan D, Sin BA, Misirligil Z, Aydin O, et al. Omalizumab in the treatment of eosinophilic granulomatosis with polyangiitis (EGPA): single-center experience in 18 cases. World Allergy Organ J. 2018;11:39.
Nazir S, Tachamo N, Fareedy SB, Khan MS, Lohani S. Omalizumab-associated eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome). Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol. 2017;118:372–374.e1.
Basta F, Mazzuca C, Nucera E, Schiavino D, Afeltra A, Antonelli IR. Omalizumab in eosinophilic granulomatosis with polyangiitis: friend or foe? A systematic literature review. Clin Exp Rheumatol. 2020;38(Suppl 124):214–20.
Mohammad AJ, Hot A, Arndt F, Moosig F, Guerry M-J, Amudala N, et al. Rituximab for the treatment of eosinophilic granulomatosis with polyangiitis (Churg-Strauss). Ann Rheum Dis. 2016;75:396–401.
Teixeira V, Mohammad AJ, Jones RB, Smith R, Jayne D. Efficacy and safety of rituximab in the treatment of eosinophilic granulomatosis with polyangiitis. RMD Open. 2019;5:e000905.
Yates M, Watts RA, Bajema IM, Cid MC, Crestani B, Hauser T, et al. EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis. BMJ Publishing Group Ltd. 2016;75:1583–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vasculitis
Rights and permissions
About this article
Cite this article
Monti, S., Brandolino, F., Milanesi, A. et al. Novel Therapies for ANCA-associated Vasculitis. Curr Rheumatol Rep 23, 38 (2021). https://doi.org/10.1007/s11926-021-01010-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s11926-021-01010-0