Abstract
Rituximab (RTX) is becoming a standard treatment for patients with anti-neutrophil cytoplasmic antibodies (ANCA)-associated vasculitis (AAV) but heterogeneity exists regarding its use. We present our uncontrolled experience with RTX in patients with refractory AAV and also the results of a systematic review of non-randomized studies on RTX in AAV patients. We retrospectively reviewed the records of AAV patients treated with RTX following an inadequate response to immunosuppressives between 2011 and 2015. The systematic review covered all English articles listed in PubMed until June 2017. There were 25 AAV patients (21 GPA, four unclassified) treated with RTX (median 2, IQR 1–3 courses; median follow-up 24, IQR 17–50 months). The kidney and the lung were the most commonly affected organs, observed in 14 and 16 patients, respectively. Complete remission rate was 72% at month 6 and 88% at month 12. Two patients had died and three serious adverse events occurred. The systematic review included 56 studies on 1422 patients with the majority being on refractory or relapsing disease. There was wide variability regarding disease characteristics, endpoints, concomitant immunosuppressives and RTX schedule. Most studies reported > 80% complete or partial remission rates with the lowest response (37.5%) for granulomatous lesions. The relapse rate was 30%. Infections and infusion reactions were the main adverse events. Our experience with RTX in refractory AAV is in line with the literature in terms of efficacy and safety. The systematic review underlines many uncertainties on its optimal use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
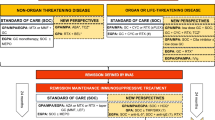
Cyclophosphamide (CYC) and glucocorticoids have been the standard therapy for remission induction for anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) for many years. Before this treatment, patients with granulomatosis with polyangiitis (GPA) had a median survival of 5 months, with a 1-year mortality of 82% and a 2-year mortality of 90% [1, 2]. With the use of CYC and glucocorticoids along with adjunctive treatments such as anti-hypertensive drugs, and renal replacement therapy, the outcome of AAV has improved dramatically with survival rates of approximately 90% at 1 year [3, 4]. However, not all patients respond to these drugs and disease flares necessitating intensification of treatment even among responders are not rare. Furthermore, serious adverse effects of CYC, such as cytopenia, infertility, infections, bladder injury and cancer are major obstacles for the long-term use of this regimen [1]. Among these adverse effects, infections are responsible for approximately half of the mortality [5, 6]. Thus, attention has focused on alternative treatment modalities with better efficacy and less toxicity.
Rituximab (RTX), an anti-CD20 monoclonal antibody, has emerged as a valuable treatment modality for AAV. The results of two randomized control studies (RCTs) [Rituximab versus Cyclophosphamide for ANCA-Associated Vasculitis (RAVE) and Rituximab versus Cyclophosphamide in ANCA-Associated Renal Vasculitis (RITUXVAS)] showed that RTX was not inferior to CYC for remission induction in newly diagnosed patients [7] or in patients with a severe disease relapse with a similar safety profile [8]. Moreover, RTX seemed to be superior to CYC in patients with severe relapsing disease [8]. However, these studies have some limitations to extrapolate the results to all AAV patients. First, newly diagnosed patients constituted the entire population of RITUXVAS trial and 48% of RAVE trial and both studies excluded refractory patients. Second, RITUXVAS has evaluated the efficacy of RTX only in patients with severe renal disease and RAVE has excluded patients with severe alveolar hemorrhage and renal disease. Third, in RCTs exclusion criteria are used to exclude high-risk patients such as those with comorbidities and poorer prognosis which makes the findings of RCTs difficult to generalize to wide patient populations [9]. Several reports on real life data obtained from observational studies have shed light on the efficacy of RTX in AAV patients with different types of involvement and especially those refractory to conventional treatment modalities [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33].
In this study, we report our experience with RTX in the management of patients with AAV refractory to conventional treatment. Furthermore, to more clearly understand the real life experience with RTX, we conducted a systematic literature review of non-randomized studies with RTX for remission induction in patients with AAV.
Methods
Observational study
We searched our biologic database and selected AAV patients who were treated with RTX in our clinic between June 2011 and October 2015. Among our 49 AAV patients treated with RTX, 24 had received RTX as first line therapy. Thus, we surveyed the remaining 25 AAV patients who were prescribed RTX due to inadequate response to conventional immunosuppressives. We used a standard form to recover all data on demographic and clinical characteristics of the patients, ANCA status, previous immunosuppressive treatment, concomitant immunosuppressive agents during remission induction and maintenance, corticosteroid dose, adverse events and response to RTX treatment from the charts.
The primary outcome was the proportion of patients achieving complete remission at month 6 which was defined as no disease activity with a daily corticosteroid dose of ≤ 10 mg. Secondary outcomes were corticosteroid dose reduction, improvement of individual organ manifestations and relapse rates during follow-up. Treatment response was also assessed with Birmingham Vasculitis Activity score (BVAS version 3) at the final visit [34]. Relapse was defined as the emergence of new disease activity during remission and requirement of an increase of corticosteroid dose (minor relapse) or addition of another immunosuppressive therapy (major relapse). Improvement of the renal function was assessed with the decrease of creatinine and decrease of proteinuria measured by spot urine or 24-h urine collection method. Additionally, infusion reactions, severe adverse events requiring hospitalization or intravenous antibiotic treatment, occurrence of cancer and minor adverse events were noted.
Systematic literature review
We searched PubMed with the keyword combination “(granulomatosis with polyangiitis OR Wegener OR microscopic polyangiitis OR eosinophilic granulomatosis with polyangiitis OR Churg Strauss OR ANCA-associated vasculitis) AND rituximab” from inception up to June 2017. Observational studies evaluating the efficacy of RTX treatment for remission induction in AAV patients were eligible. RCTs, articles reporting the outcome of RTX treatment for maintenance of remission, articles including pediatric age population, studies reporting on less than five patients and articles in languages other than English were excluded. Two independent reviewers (SNE and GA) screened titles and abstracts. The full text of articles that potentially met eligibility criteria at the first screening stage were assessed for inclusion criteria. Disagreements were solved by a senior author (GH). Data extraction was also done by two reviewers. The quality of the included studies was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach [35].
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki. The ethics committee of Cerrahpasa Medical Faculty approved the study (174711/2017).
Statistics
Statistical analysis was done using SPSS v.22.0. We used normality tests such as visual (histograms, probability plots) and analytical (Kolmogorov–Smirnov/Shapiro–Wilk’s test) methods to determine whether the data were normally distributed. Descriptive statistics were presented using median (interquartile range) for the non-normally distributed variables. The Wilcoxon signed rank test was used to compare the change in prednisolone dose, creatinine level and the amount of proteinuria between baseline and the end of the follow-up. A p value of less than 0.05 was considered statistically significant.
For the systematic literature review, we retrieved the data that the authors presented in their articles. We did not pool the data for an efficacy analysis due to heterogeneity of the included studies regarding the characteristics of patient populations, concomitant immunosuppressive therapies, RTX protocols, outcome measures, length of the follow-up time, and remission and relapse definitions.
Results
Clinical characteristics of patients
Twenty-five patients (21 GPA, four unclassified AAV) received RTX after an inadequate response to conventional immunosuppressives and comprised the study cohort. All patients met the 2012 Revised Chapel Hill Consensus nomenclature for AAV [36]. The baseline demographic and clinical characteristics of the patients are shown in Table 1.
Treatment protocol
RTX was given either intravenously in two weekly doses of 1000 mg (rheumatologic protocol; n = 21) or 375 mg/m2/week for 4 weeks (oncologic protocol; n = 4). The same cycles were repeated at fixed intervals every 6 months thereafter. All patients received premedication with intravenous methylprednisolone 100 mg, oral acetaminophen 1 g, and intravenous pheniramine maleate 45.5 mg before RTX infusions. Additionally, 19 patients (76%) received high-dose steroids concurrently with RTX. This was in the form of iv methylprednisolone 1 gm for 3 days in 5 patients and oral prednisolone 1 mg/kg/day in 14 patients. The remaining six patients received oral prednisolone between 10 and 20 mg daily.
Thirteen patients (52%) were given trimethoprim–sulfamethoxazole for pneumocystis jiroveci pneumonia prophylaxis. Three patients (12%) were vaccinated against pneumococcal bacteria and influenza virus. All patients were screened for hepatitis serology before the initiation of RTX. Two of them had positive anti-HBc IgG but they did not receive further investigation or intervention for this.
RTX was given for a median of two courses (IQR 1–3) during a median follow-up of 13 months (IQR 9–22). The concomitant drugs during remission induction and maintenance of remission are given in Table 1.
Outcome
At month 6, 18 (72%) patients had achieved complete remission, 6 had ongoing disease activity and 1 had died at month 4 due to respiratory failure. Four of the six patients with ongoing disease activity gradually achieved remission at month 12. Thus, there were 22 (88%) patients achieving remission at month 12. The remaining two patients were considered refractory to RTX and received high-dose corticosteroids with cyclophosphamide. One of them died with acute renal failure 14 months later and the second developed end-stage renal disease. Three patients experienced minor relapses after a median follow-up of 15 months (range 14–16) from baseline.
Final visit
After a median duration of 24 months (IQR 17–50), 23 patients were under follow-up, 2 patients had died, 1 due to renal failure and the other due to respiratory failure, as described above. BVAS score was 0 in 18 patients, whereas the median BVAS score was four (IQR 3–6) in the remaining five patients. The median prednisolone dose was 40 mg/day (IQR 25–60) at the beginning and 5 mg/day (IQR 0–25) at the final assessment (p = 0.004). Among the patents with BVAS score of 0, 7 were free of corticosteroids and 11 patients were using less than 10 mg/day.
Renal involvement was found to be stable in six patients, improved in six patients and worse in two patients. The median creatinine level remained stable at the initiation of RTX treatment and at the end of follow-up [1.98 mg/dL (IQR 1.22–3.35) vs 1.47 mg/dL (IQR 0.91–2.65); p = 0.35]. The amount of proteinuria was significantly lower at the end of follow-up [1333 mg/day (IQR 537–2300) vs 611 mg/day (150–1321); p = 0.016). One of the two patients who had been undergoing hemodialysis at RTX initiation had no need for this after RTX.
The last evaluation of patients with other types of organ involvement showed good clinical response in 11 of the 16 patients with lung involvement, 9 of the 10 patients with upper respiratory system involvement, all 2 patients with eye involvement, all 2 patients with peripheral nervous system involvement, 1 of the 2 patients with ear involvement, and both of the patients with cutaneous involvement and central nervous system involvement, respectively. One patient with lung involvement had persistent wheezing and another patient with upper respiratory system involvement had tenderness over paranasal sinuses. One patient had persistent sensorineural hearing loss and four patients with lung involvement showed signs of progression on CT scans.
Safety
RTX was terminated in two patients due to infusion reactions on first and fifth courses, respectively. Four patients were hospitalized while being on RTX, one due to pneumonia and the other three due to disease worsening. The pneumonia occurred after 15 days of RTX and the patient recovered with antibiotics.
Systematic literature review
The systematic literature search yielded 546 articles of which 458 were excluded after reading the titles and abstracts. Fifty-six articles were included after full text review [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33, 37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] (Fig. 1). Two articles reported the long-term followup of two previous studies [23, 37]. Data obtained from these 56 studies regarding the demographic characteristics, baseline vasculitis activity score, definition of remission and remission rates with induction, concomitant immunosuppressive therapies other than glucocorticoids and adverse events during follow-up are shown in Table 2.
We also retrieved the data on the definition of AAV, the disease status (newly diagnosed, relapsing and refractory), type of RTX regimen, RTX treatment for maintaining remission, definition of relapse, relapse rates, outcome after remission induction and follow-up time in each study and provided the quality of the included studies (see online supplementary Table S).
Overall, 56 studies (46 retrospective and 10 prospective) reported 1422 AAV patients (1098 GPA, 70 EGPA, 191 MPA, 11 renal-limited vasculitis, four unclassified, 48 type of AAV not provided) treated with RTX [10,11,12,13,14,15,16,17,18,19,20,21,22, 24,25,26,27,28,29,30,31,32,33, 37, 39,40,41,42, 44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68]. The majority of the patients (86%) had refractory or relapsing disease whereas 195 patients (14%) had new diagnosis. In 15 studies, RTX was prescribed for a specific manifestation such as diffuse alveolar hemorrhage (n = 1) [43]. ocular involvement (n = 8) [10,11,12, 15, 21, 27, 48, 64], severe renal disease (n = 2) [42, 45], pulmonary nodules (n = 1) [13], orbital mass (n = 1) [19], head and neck involvement (n = 1) [26], or granulomatous lesions (n = 1) [30]. Patients with renal transplantation [59] and elderly [44] patients are evaluated in two retrospective studies. The most common vasculitis assessment tools were BVAS.V.3.0 (18 studies), followed by BVAS/WG (11 studies) and BVAS (8 studies). Remission was defined as a BVAS score of 0 in most of the studies (n = 33) or as no disease activity (n = 15) with variable doses of glucocorticoids. Overall, 753 (53%) patients received immunosuppressive therapy in addition to RTX. Among the studies reporting the details of concomitant therapy, CYC (35%) was the most frequently used drug followed by mycophenolate mofetil (MMF) (16%), azathioprine (AZA) (12.5%), and methotrexate (MTX) (6%). RTX was given alone in 10 studies (147 patients). Among the 1283 patients with available data on RTX regimen, 640 (50%) patients received rheumatologic and 593 (46%) patients received oncologic protocol. Two studies on eye involvement used Foster regimen (eight doses of 375 mg/m2 weekly) in three patients [10, 11] and one study used 4 + 2 regimen (a dose of 375 mg/m2 on days 1, 8, 15 and 22 and two more doses 1 and 2 months after the last administration) in 11 patients [65]. The efficacy of low dose (13 patients) and a single dose of RTX (23 patients) was evaluated in one [50] and two [37, 52] studies, respectively.
The initial remission rates ranged between 7 and 100% but the definition of remission was not uniform across studies. When only complete or partial remission was considered, the remission rates were > 80% in most of the studies with the lowest rate being 37.5%. Regarding specific manifestations or conditions, remission rates were between 87.5–100% in scleritis, 86.5–100% in severe renal disease, 60% in pulmonary nodules, 94% in diffuse alveolar hemorrhage, 88% in head and neck involvement, 37.5% in granulomatous lesions. Remission rates were 97% in the elderly population, 80% in patients with renal transplantation and a study on orbital masses (ten patients) reported 100% improvement in visual acuity and 80% size reduction in mass [19]. However, it should be noted that remission rates were derived from one study each. After remission induction, 395 patients continued to receive maintenance therapy with RTX either according to a fixed schedule (11 studies) or when needed (10 studies). The mean follow-up time was longer than 12 months in 43 studies. Overall, 428 (30%) relapses occurred during the follow-up. Among 1216 adverse events, infections (69%) were the most frequent followed by infusion reactions (5%), cytopenias (4%) and malignancies (3%). There were 57 (4%) deaths with the main reasons being infections (n = 25), cardiovascular complications (n = 5), and refractory disease (n = 4).
Discussion
In the observational study, 72% of our 25 patients with refractory AAV achieved complete remission with RTX at month 6. At month 12, the remission rate reached 88% after a second course of RTX. Two patients died due to refractory disease. One infection requiring hospitalization and two infusion reactions occurred. During a median follow-up of 24 months, only three patients experienced minor relapses. These results are similar to the beneficial results reported in most of the studies summarized in the systematic review.
One unresolved issue is the additional benefit of immunosuppressive therapy such as CYC, AZA, MTX and MMF added to RTX during remission induction. Concomitant immunosuppressives were used in 50% of patients in the studies underlining the uncertainty of this issue. Another uncertainty is the optimal protocol for RTX. The systematic review showed that oncologic and rheumatologic regimens are preferred nearly equally. A retrospective study comparing these two RTX regimens did not find a difference regarding the duration of B-cell depletion and treatment response [67]. A single dose of RTX was evaluated in two small-sized studies, reporting beneficial result in one [37, 52]. Data on the Foster regimen is insufficient since there were only three patients with ocular involvement treated with this protocol [10, 11]. Finally, one single study with low-dose RTX reported 92% complete remission in 12 patients during a median of 7.5-month follow-up [50].
Early case series have suggested that granulomatous manifestations of AAV are less likely to respond to RTX [30, 69, 70]. A recent study also reported nearly double remission rates for vasculitis manifestations compared to granulomatous manifestations [20]. The authors have speculated that the lower response for granulomatous lesions may be due to the predominance of CD4 + T cell-mediated inflammation. On the other hand, there are also other studies reporting beneficial results with RTX in treating retro-orbital masses, head and neck involvement, and pulmonary manifestations [13, 27, 29]. Moreover, Joshi and colleagues compared the response rates between patients with orbital granulomatous disease and those with scleritis, and reported similar results among the groups [48]. These conflicting results indicate the need for further studies to better understand the value of RTX in treating granulomatous lesions especially in refractory patients.
Infections were the most common adverse events in our study and in the systematic review. Although RTX was thought to be safer than CYC, the RAVE trial reported similar safety profiles among CYC and RTX groups [8]. Similarly, severe adverse events were one of the primary outcomes in the RITUXVAS trial and safety profiles were similar between RTX versus CYC-based regimens [7]. However, both studies included complications that were also attributable to the disease, glucocorticoid exposure and study medications [7, 8]. Furthermore, both studies had insufficient duration of follow-up to show a difference regarding malignancy and infertility two well-known long-term adverse events of CYC. A retrospective study including 323 AAV patients with a mean follow-up of 5.6 years looked at whether RTX is a safer option with regard to malignancy. The malignancy risk was 3.10-fold higher in CYC-treated patients compared to the general population whereas RTX therapy was not associated with malignancy [71]. Longer follow-up results of the RAVE and RITUXVAS will throw more light on this subject. On the other hand, there is no doubt about the safety of RTX over CYC in preserving fertility.
The main limitations of our study are its retrospective design and small patient numbers. The limitations of the SLR are the heterogeneity of the included studies regarding the characteristics of patient populations, concomitant immunosuppressive therapies, RTX protocols, outcome measures, and remission definitions.
In conclusion, our experience and data coming from observational studies suggest that RTX may be a good option in patients with refractory disease. We still have few data on the long-term outcome of this treatment and on its efficacy on individual organ manifestations. In addition, more data on different patient populations are needed that would lead to the development of consensus on endpoints, outcome measures and treatment strategies.
References
Tesar V, Hruskova Z (2014) Limitations of standard immunosuppressive treatment in ANCA-associated vasculitis and lupus nephritis. Nephron Clin Pract 128(3–4):205–215. https://doi.org/10.1159/000368569
Fauci AS, Wolff SM (1973) Wegener’s granulomatosis: studies in 18 patients and a review of the literature. Medicine (Baltimore) 52(6):535–561
Smith RM (2015) Update on the treatment of ANCA associated vasculitis. Presse Med (Paris France 1983) 44(6 Pt 2):e241–e249. https://doi.org/10.1016/j.lpm.2015.04.008
Flossmann O, Berden A, de Groot K, Hagen C, Harper L, Heijl C, Hoglund P, Jayne D, Luqmani R, Mahr A, Mukhtyar C, Pusey C, Rasmussen N, Stegeman C, Walsh M, Westman K, European Vasculitis Study G (2011) Long-term patient survival in ANCA-associated vasculitis. Ann Rheum Dis 70 (3):488–494. https://doi.org/10.1136/ard.2010.137778
Little MA, Nightingale P, Verburgh CA, Hauser T, De Groot K, Savage C, Jayne D, Harper L (2010) Early mortality in systemic vasculitis: relative contribution of adverse events and active vasculitis. Ann Rheum Dis 69(6):1036–1043. https://doi.org/10.1136/ard.2009.109389
Solans-Laque R, Fraile G, Rodriguez-Carballeira M, Caminal L, Castillo MJ, Martinez-Valle F, Saez L, Rios JJ, Solanich X, Oristrell J, Pasquau F, Fonseca E, Zamora M, Callejas JL, Frutos B, Abdilla M, Fanlo P, Garcia-Sanchez I, Lopez-Dupla M, Sopena B, Perez-Iglesias A, Bosch JA (2017) Clinical characteristics and outcome of Spanish patients with ANCA-associated vasculitides: Impact of the vasculitis type, ANCA specificity, and treatment on mortality and morbidity. Medicine (Baltimore) 96(8):e6083. https://doi.org/10.1097/md.0000000000006083
Jones RB, Cohen Tervaert JW, Hauser T, Luqmani R, Morgan MD, Peh CA, Savage CO, Segelmark M, Tesar V, van Paassen P, Walsh D, Walsh M, Westman K, Jayne DRW (2010) Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med 363(3):211–220. https://doi.org/10.1056/NEJMoa0909169
Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, Kallenberg CGM, St. Clair EW, Turkiewicz A, Tchao NK, Webber L, Ding L, Sejismundo LP, Mieras K, Weitzenkamp D, Ikle D, Seyfert-Margolis V, Mueller M, Brunetta P, Allen NB, Fervenza FC, Geetha D, Keogh KA, Kissin EY, Monach PA, Peikert T, Stegeman C, Ytterberg SR, Specks U (2010) Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med 363(3):221–232. https://doi.org/10.1056/NEJMoa0909905
Sibinga EM, Jennings JM (2010) Strengths and limitations of randomized, controlled trials. Pediatr Rev 31(7):296–297. https://doi.org/10.1542/pir.31-7-296
You C, Ma L, Lasave AF, Foster CS (2017) Rituximab induction and maintenance treatment in patients with scleritis and granulomatosis with polyangiitis (Wegener’s). Ocul Immunol Inflamm:1–8. https://doi.org/10.1080/09273948.2017.1327602
Ebrahimiadib N, Modjtahedi BS, Roohipoor R, Anesi SD, Foster CS (2016) Successful treatment strategies in granulomatosis with polyangiitis-associated peripheral ulcerative keratitis. Cornea 35(11):1459–1465. https://doi.org/10.1097/ico.0000000000000919
Recillas-Gispert C, Serna-Ojeda JC, Flores-Suarez LF (2015) Rituximab in the treatment of refractory scleritis in patients with granulomatosis with polyangiitis (Wegener’s). Graefes Arch Clin Exp Ophthalmol 253(12):2279–2284. https://doi.org/10.1007/s00417-015-3198-5
Henderson SR, Copley SJ, Pusey CD, Ind PW, Salama AD (2014) Prolonged B cell depletion with rituximab is effective in treating refractory pulmonary granulomatous inflammation in granulomatosis with polyangiitis (GPA). Medicine (Baltimore) 93(27):e229. https://doi.org/10.1097/md.0000000000000229
Nagafuchi H, Atsumi T, Hatta K, Muso E, Takeno M, Yamada H, Ozaki S (2015) Long-term safety and efficacy of rituximab in 7 Japanese patients with ANCA-associated vasculitis. Mod Rheumatol 25(4):603–608. https://doi.org/10.3109/14397595.2014.981945
Pelegrin L, Jakob E, Schmidt-Bacher A, Schwenger V, Becker M, Max R, Lorenz HM, Mackensen F (2014) Experiences with rituximab for the treatment of autoimmune diseases with ocular involvement. J Rheumatol 41(1):84–90. https://doi.org/10.3899/jrheum.130206
Cartin-Ceba R, Diaz-Caballero L, Al-Qadi MO, Tryfon S, Fervenza FC, Ytterberg SR, Specks U (2016) Diffuse alveolar hemorrhage secondary to antineutrophil cytoplasmic antibody-associated vasculitis: predictors of respiratory failure and clinical outcomes. Arthritis Rheum 68(6):1467–1476. https://doi.org/10.1002/art.39562
Roll P, Ostermeier E, Haubitz M, Lovric S, Unger L, Holle J, Kotter I, Henes JC, Bergner R, Rubbert-Roth A, Specker C, Schulze-Koops H, Muller-Ladner U, Fleck M, Burmester GR, Hiepe F, Heitmann S, Aringer M, Fischer-Betz R, Dorner T, Tony HP (2012) Efficacy and safety of rituximab treatment in patients with antineutrophil cytoplasmic antibody-associated vasculitides: results from a German registry (GRAID). J Rheumatol 39(11):2153–2156. https://doi.org/10.3899/jrheum.120482
Pullerits R, Ljevak M, Vikgren J, Bokarewa M (2012) Off-trial evaluation of the B cell-targeting treatment in the refractory cases of antineutrophil cytoplasmic antibodies (ANCA)-associated vasculitis: long-term follow-up from a single centre. Scand J Immunol 76(4):411–420. https://doi.org/10.1111/j.1365-3083.2012.02747.x
Baslund B, Wiencke AK, Rasmussen N, Faurschou M, Toft PB (2012) Treatment of orbital inflammation with rituximab in Wegener’s granulomatosis. Clin Exp Rheumato 30(1 Suppl 70):S7–S10
Holle JU, Dubrau C, Herlyn K, Heller M, Ambrosch P, Noelle B, Reinhold-Keller E, Gross WL (2012) Rituximab for refractory granulomatosis with polyangiitis (Wegener’s granulomatosis): comparison of efficacy in granulomatous versus vasculitic manifestations. Ann Rheum Dis 71(3):327–333. https://doi.org/10.1136/ard.2011.153601
Joshi L, Lightman SL, Salama AD, Shirodkar AL, Pusey CD, Taylor SR (2011) Rituximab in refractory ophthalmic Wegener’s granulomatosis: PR3 titers may predict relapse, but repeat treatment can be effective. Ophthalmology 118(12):2498–2503. https://doi.org/10.1016/j.ophtha.2011.06.009
Rees F, Yazdani R, Lanyon P (2011) Long-term follow-up of different refractory systemic vasculitides treated with rituximab. Clin Rheumatol 30(9):1241–1245. https://doi.org/10.1007/s10067-011-1756-8
Henes JC, Kanz L, Koetter I (2011) Rituximab and leflunomide for Wegener’s granulomatosis: a long-term follow-up. Rheumatol Int 31(3):425–426. https://doi.org/10.1007/s00296-010-1462-x
Henes JC, Fritz J, Koch S, Klein R, Horger M, Risler T, Kanz L, Koetter I (2007) Rituximab for treatment-resistant extensive Wegener’s granulomatosis-additive effects of a maintenance treatment with leflunomide. Clin Rheumatol 26(10):1711–1715. https://doi.org/10.1007/s10067-007-0643-9
Ramos-Casals M, Garcia-Hernandez FJ, de Ramon E, Callejas JL, Martinez-Berriotxoa A, Pallares L, Caminal-Montero L, Selva-O’Callaghan A, Oristrell J, Hidalgo C, Perez-Alvarez R, Mico ML, Medrano F, Gomez de la Torre R, Diaz-Lagares C, Camps M, Ortego N, Sanchez-Roman J (2010) Off-label use of rituximab in 196 patients with severe, refractory systemic autoimmune diseases. Clin Exp Rheumatol 28(4):468–476
Martinez Del Pero M, Chaudhry A, Jones RB, Sivasothy P, Jani P, Jayne D (2009) B-cell depletion with rituximab for refractory head and neck Wegener’s granulomatosis: a cohort study. Clin Otolaryngol 34(4):328–335. https://doi.org/10.1111/j.1749-4486.2009.01968.x
Taylor SR, Salama AD, Joshi L, Pusey CD, Lightman SL (2009) Rituximab is effective in the treatment of refractory ophthalmic Wegener’s granulomatosis. Arthritis Rheum 60(5):1540–1547. https://doi.org/10.1002/art.24454
Lovric S, Erdbruegger U, Kumpers P, Woywodt A, Koenecke C, Wedemeyer H, Haller H, Haubitz M (2009) Rituximab as rescue therapy in anti-neutrophil cytoplasmic antibody-associated vasculitis: a single-centre experience with 15 patients. Nephrol Dial Transpl 24(1):179–185. https://doi.org/10.1093/ndt/gfn430
Seo P, Specks U, Keogh KA (2008) Efficacy of rituximab in limited Wegener’s granulomatosis with refractory granulomatous manifestations. J Rheumatol 35(10):2017–2023
Aries PM, Hellmich B, Voswinkel J, Both M, Nolle B, Holl-Ulrich K, Lamprecht P, Gross WL (2006) Lack of efficacy of rituximab in Wegener’s granulomatosis with refractory granulomatous manifestations. Ann Rheum Dis 65(7):853–858. https://doi.org/10.1136/ard.2005.044420
Keogh KA, Wylam ME, Stone JH, Specks U (2005) Induction of remission by B lymphocyte depletion in eleven patients with refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 52(1):262–268. https://doi.org/10.1002/art.20718
Keogh KA, Ytterberg SR, Fervenza FC, Carlson KA, Schroeder DR, Specks U (2006) Rituximab for refractory Wegener’s granulomatosis: report of a prospective, open-label pilot trial. Am J Respir Crit Care Med 173(2):180–187. https://doi.org/10.1164/rccm.200507-1144OC
Eriksson P (2005) Nine patients with anti-neutrophil cytoplasmic antibody-positive vasculitis successfully treated with rituximab. J Intern Med 257(6):540–548. https://doi.org/10.1111/j.1365-2796.2005.01494.x
Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, Flossmann O, Hall C, Hollywood J, Jayne D, Jones R, Lanyon P, Muir A, Scott D, Young L, Luqmani RA (2009) Modification and validation of the Birmingham vasculitis activity score (version 3). Ann Rheum Dis 68(12):1827–1832. https://doi.org/10.1136/ard.2008.101279
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schunemann HJ, GRADE Working Group (2008) What is “quality of evidence” and why is it important to clinicians?. BMJ 336(7651):995–998. https://doi.org/10.1136/bmj.39490.551019
Jennette JC (2013) Overview of the 2012 revised international Chapel Hill consensus conference nomenclature of vasculitides. Clin Exp Nephrol 17(5):603–606. https://doi.org/10.1007/s10157-013-0869-
Saito A, Takeuchi Y, Kagaya S, Ojima Y, Fukami H, Sato H, Matsuda K, Nagasawa T (2017) Remission induction therapy with rituximab for microscopic polyangiitis: a feasibility study. Tohoku J Exp Med 242(1):53–62. https://doi.org/10.1620/tjem.242.53
Roccatello D, Sciascia S, Rossi D, Alpa M, Naretto C, Radin M, Fenoglio R, Baldovino S, Menegatti E (2017) The “4 plus 2” rituximab protocol makes maintenance treatment unneeded in patients with refractory ANCA-associated vasculitis: a 10 years observation study. Oncotarget. https://doi.org/10.18632/oncotarget.18120
Lionaki S, Fragoulis GE, Venetsanopoulou A, Vlachoyiannopoulos P, Boletis JN, Tzioufas AG (2017) Cyclophosphamide followed by rituximab for aggressive multiple-relapsing antineutrophil cytoplasmic antibody-associated vasculitis. Clin Exp Rheumatol 35(Suppl 103 (1)):155–164
Novikov P, Moiseev S, Smitienko I, Zagvozdkina E (2016) Rituximab as induction therapy in relapsing eosinophilic granulomatosis with polyangiitis: a report of 6 cases. Jt B Spine 83(1):81–84. https://doi.org/10.1016/j.jbspin.2015.04.016
Mohammad AJ, Hot A, Arndt F, Moosig F, Guerry MJ, Amudala N, Smith R, Sivasothy P, Guillevin L, Merkel PA, Jayne DR (2016) Rituximab for the treatment of eosinophilic granulomatosis with polyangiitis (Churg-Strauss). Ann Rheum Dis 75(2):396–401. https://doi.org/10.1136/annrheumdis-2014-206095
Geetha D, Hruskova Z, Segelmark M, Hogan J, Morgan MD, Cavero T, Eriksson P, Seo P, Manno RL, Dale J, Harper L, Tesar V, Jayne DR (2016) Rituximab for treatment of severe renal disease in ANCA associated vasculitis. J Nephrol 29(2):195–201. https://doi.org/10.1007/s40620-015-0208-y
Cartin-Ceba R, Golbin JM, Keogh KA, Peikert T, Sanchez-Menendez M, Ytterberg SR, Fervenza FC, Specks U (2012) Rituximab for remission induction and maintenance in refractory granulomatosis with polyangiitis (Wegener’s): 10-year experience at a single center. Arthritis Rheum 64(11):3770–3778. https://doi.org/10.1002/art.34584
Timlin H, Lee SM, Manno RL, Seo P, Geetha D (2015) Rituximab for remission induction in elderly patients with ANCA-associated vasculitis. Semin Arthritis Rheum 45(1):67–69. https://doi.org/10.1016/j.semarthrit.2015.02
Shah S, Hruskova Z, Segelmark M, Morgan MD, Hogan J, Lee SK, Dale J, Harper L, Tesar V, Jayne DR, Geetha D (2015) Treatment of severe renal disease in ANCA positive and negative small vessel vasculitis with rituximab. Am J Nephrol 41(4–5):296–301. https://doi.org/10.1159/000431336
Md Yusof MY, Vital EM, Das S, Dass S, Arumugakani G, Savic S, Rawstron AC, Emery P (2015) Repeat cycles of rituximab on clinical relapse in ANCA-associated vasculitis: identifying B cell biomarkers for relapse to guide retreatment decisions. Ann Rheum Dis 74(9):1734–1738. https://doi.org/10.1136/annrheumdis-2014-206496
McGregor JG, Hogan SL, Kotzen ES, Poulton CJ, Hu Y, Negrete-Lopez R, Kidd JM, Katsanos SL, Bunch DO, Nachman PH, Falk RJ (2015) Rituximab as an immunosuppressant in antineutrophil cytoplasmic antibody-associated vasculitis. Nephrol Dial Transpl 30(Suppl 1):i123–i131. https://doi.org/10.1093/ndt/gfv076
Joshi L, Tanna A, McAdoo SP, Medjeral-Thomas N, Taylor SR, Sandhu G, Tarzi RM, Pusey CD, Lightman S (2015) Long-term outcomes of Rituximab therapy in ocular granulomatosis with polyangiitis: impact on localized and nonlocalized disease. Ophthalmology 122(6):1262–1268. https://doi.org/10.1016/j.ophtha.2015.01.016
Chocova Z, Hruskova Z, Mareckova H, Svobodova B, Duskova D, Bednarova V, Jancova E, Rysava R, Tesar V (2015) Rituximab use in patients with ANCA-associated vasculitis: clinical efficacy and impact on immunological parameters. Clin Rheumatol 34(1):107–115. https://doi.org/10.1007/s10067-014-2816-7
Wawrzycka-Adamczyk K, Zugaj A, Wludarczyk A, Kosalka J, Sznajd J, Bazan-Socha S, Musial J (2014) Lower doses of rituximab in remission induction for refractory granulomatosis with polyangiitis. Przegl Lek 71(12):663–665
Venhoff N, Niessen L, Kreuzaler M, Rolink AG, Hassler F, Rizzi M, Voll RE, Thiel J (2014) Reconstitution of the peripheral B lymphocyte compartment in patients with ANCA-associated vasculitides treated with rituximab for relapsing or refractory disease. Autoimmunity 47(6):401–408. https://doi.org/10.3109/08916934.2014.914174
Moog P, Probst M, Kuechle C, Hauser C, Heemann U, Thuermel K (2014) Single-dose rituximab for remission induction and maintenance therapy in ANCA-associated vasculitis: a retrospective analysis of 17 patients. Scand J Rheumatol 43(6):519–523. https://doi.org/10.3109/03009742.2014
Miloslavsky EM, Specks U, Merkel PA, Seo P, Spiera R, Langford CA, Hoffman GS, Kallenberg CG, St Clair EW, Tchao NK, Viviano L, Ding L, Ikle D, Villarreal M, Jepson B, Brunetta P, Allen NB, Fervenza FC, Geetha D, Keogh K, Kissin EY, Monach PA, Peikert T, Stegeman C, Ytterberg SR, Stone JH (2014) Rituximab for the treatment of relapses in antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheumatol 66(11):3151–3159. https://doi.org/10.1002/art.38788
Knight A, Hallenberg H, Baecklund E (2014) Efficacy and safety of rituximab as maintenance therapy for relapsing granulomatosis with polyangiitis-a case series. Clin Rheumatol 33(6):841–848. https://doi.org/10.1007/s10067-013-2351-y
Charles P, Neel A, Tieulie N, Hot A, Pugnet G, Decaux O, Marie I, Khellaf M, Kahn JE, Karras A, Ziza JM, Deligny C, Tcherakian C, Guillevin L (2014) Rituximab for induction and maintenance treatment of ANCA-associated vasculitides: a multicentre retrospective study on 80 patients. Rheumatology 53(3):532–539. https://doi.org/10.1093/rheumatology/ket381
Calich AL, Puechal X, Pugnet G, London J, Terrier B, Charles P, Mouthon L, Guillevin L (2014) Rituximab for induction and maintenance therapy in granulomatosis with polyangiitis (Wegener’s). Results of a single-center cohort study on 66 patients. J Autoimmun 50:135–141. https://doi.org/10.1016/j.jaut.2014.03.002
Azar L, Springer J, Langford CA, Hoffman GS (2014) Rituximab with or without a conventional maintenance agent in the treatment of relapsing granulomatosis with polyangiitis (Wegener’s): a retrospective single-center study. Arthritis Rheumatol 66(10):2862–2870. https://doi.org/10.1002/art.38744
Thiel J, Hassler F, Salzer U, Voll RE, Venhoff N (2013) Rituximab in the treatment of refractory or relapsing eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome). Arthritis Res Ther 15(5):R133. https://doi.org/10.1186/ar4313
Murakami C, Manoharan P, Carter-Monroe N, Geetha D (2013) Rituximab for remission induction in recurrent ANCA-associated glomerulonephritis postkidney transplant. Transpl Int 26(12):1225–1231. https://doi.org/10.1111/tri.12203
Gregersen JW, Chaudhry A, Jayne DR (2013) Rituximab for ANCA-associated vasculitis in the setting of severe infection. Scand J Rheumatol 42(3):207–210. https://doi.org/10.3109/03009742.2012.739638
Besada E, Koldingsnes W, Nossent JC (2013) Long-term efficacy and safety of pre-emptive maintenance therapy with rituximab in granulomatosis with polyangiitis: results from a single centre. Rheumatology 52(11):2041–2047. https://doi.org/10.1093/rheumatology/ket257
Wendt M, Gunnarsson I, Bratt J, Bruchfeld A (2012) Rituximab in relapsing or refractory ANCA-associated vasculitis: a case series of 16 patients Scand. J Rheumatol 41(2):116–119. https://doi.org/10.3109/03009742.2011.620573
Smith RM, Jones RB, Guerry MJ, Laurino S, Catapano F, Chaudhry A, Smith KG, Jayne DR (2012) Rituximab for remission maintenance in relapsing antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 64(11):3760–3769. https://doi.org/10.1002/art.34583
Lower EE, Baughman RP, Kaufman AH (2012) Rituximab for refractory granulomatous eye disease. Clin Ophthalmol 6:1613–1618. https://doi.org/10.2147/opth.s35521
Roccatello D, Sciascia S, Rossi D, Alpa M, Naretto C, Russo A, Menegatti E, Baldovino S (2011) Long-term effects of rituximab added to cyclophosphamide in refractory patients with vasculitis. Am J Nephrol 34(2):175–180. https://doi.org/10.1159/000329535
Mansfield N, Hamour S, Habib AM, Tarzi R, Levy J, Griffith M, Cairns T, Cook HT, Pusey CD, Salama AD (2011) Prolonged disease-free remission following rituximab and low-dose cyclophosphamide therapy for renal ANCA-associated vasculitis. Nephrol Dial Transplant 26(10):3280–3286. https://doi.org/10.1093/ndt/gfr127
Jones RB, Ferraro AJ, Chaudhry AN, Brogan P, Salama AD, Smith KG, Savage CO, Jayne DR (2009) A multicenter survey of rituximab therapy for refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 60(7):2156–2168. https://doi.org/10.1002/art.24637
Stasi R, Stipa E, Del Poeta G, Amadori S, Newland AC, Provan D (2006) Long-term observation of patients with anti-neutrophil cytoplasmic antibody-associated vasculitis treated with rituximab. Rheumatology 45(11):1432–1436. https://doi.org/10.1093/rheumatology/kel098
Omdal R, Wildhagen K, Hansen T, Gunnarsson R, Kristoffersen G (2005) Anti-CD20 therapy of treatment-resistant Wegener’s granulomatosis: favourable but temporary response. Scand J Rheumatol 34(3):229–232
Brihaye B, Aouba A, Pagnoux C, Cohen P, Lacassin F, Guillevin L (2007) Adjunction of rituximab to steroids and immunosuppressants for refractory/relapsing Wegener’s granulomatosis: a study on 8 patients. Clin Exp Rheumatol 25(1 Suppl 44):S23–S27
van Daalen EE, Rizzo R, Kronbichler A, Wolterbeek R, Bruijn JA, Jayne DR, Bajema IM, Rahmattulla C (2017) Effect of rituximab on malignancy risk in patients with ANCA-associated vasculitis. Ann Rheum Dis 76(6):1064–1069. https://doi.org/10.1136/annrheumdis-2016-209925
Acknowledgements
All authors contributed to writing this study and have approved the final version.
Funding
We did not receive any funding support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The ethics committee of Istanbul University, Cerrahpasa Medical Faculty approved the study (174711/2017).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ayan, G., Esatoglu, S.N., Hatemi, G. et al. Rituximab for anti-neutrophil cytoplasmic antibodies-associated vasculitis: experience of a single center and systematic review of non-randomized studies. Rheumatol Int 38, 607–622 (2018). https://doi.org/10.1007/s00296-018-3928-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-018-3928-1