Abstract
Patients with rheumatoid arthritis (RA) often inquire about dietary interventions to improve RA symptoms. Although the majority of studies of diet and RA were published prior to the start of the twenty-first century, this review discusses the evidence for a relationship between diet, in particular omega-3 fatty acid supplements, vitamin D supplements, alcohol, and the Mediterranean diet and RA disease activity. We review possible mechanisms by which these dietary intakes may affect RA disease activity. Given the complexity of studying the relationship between diet and RA disease activity, we highlight areas deserving further study before specific recommendations can be made to RA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While effective pharmacologic treatments for rheumatoid arthritis (RA) now exist, patients frequently ask their rheumatologists whether dietary changes could improve their RA symptoms. Even with current medical therapies, many RA patients have persistent disease activity and/or acute exacerbations [1]. A variety of patient-focused medical resources and websites have responded to patient interest in this topic, by advocating either avoidance or increased consumption of particular foods that may affect RA symptoms [2–4]. When patients inquire whether diet influences disease activity, clinicians only have a handful of older small clinical trials for guidance.
This review proposes a framework for understanding the evidence supporting and possible mechanisms for dietary intakes as potential adjunctive therapy for RA. While most studies on this topic were conducted prior to the start of the twenty-first century, we have emphasized evidence from recent years. We direct interested readers to several reviews of older dietary studies in RA patients [5–7].
Proposed Basic Mechanisms for an Influence of Dietary Intake on RA Disease Activity
There is strong rationale from laboratory studies suggesting that dietary nutrients, patterns, and intakes could influence RA disease activity. Few of these proposed mechanisms have been specifically studied in RA, however. Here we have highlighted five different potential mechanisms by which diet may be related to pathways involved in inflammation and autoimmunity in RA, even though most have not been specifically evaluated in RA. The preponderance of the evidence for these proposed pathways comes from laboratory studies, either in vitro or in animal models. Human studies proving the links between dietary intakes and specific pathways of inflammatory and immune regulation in RA are still lacking.
Decreased Inflammatory Eicosanoids
Omega-3 and omega-6 fatty acids modulate the lipid content of phospholipid membranes, which are in turn metabolized to eicosanoids, lipid mediators of inflammation [8, 9]. These two types of fatty acids have opposing effects: omega-3 fatty acids decrease the production of pro-inflammatory cytokines, whereas omega-6 fatty acids stimulate the production of pro-inflammatory cytokines [10]. Omega-3 fatty acids are primarily obtained from fatty fish, but also poultry, nuts, and berries in the diet [11]. Fatty fish and fish oil supplements contain two types of long chain omega-3 fatty acids, both of which humans cannot synthesize and are thus nutritionally dependent on intake: eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Arachidonic acid, an omega-6 fatty acid in cell membranes, is primarily derived from animal fats in the diet. Plant-derived foods do not contain arachidonic acid. Eating plants exclusively (e.g., vegetarian diet) thus removes exogenous arachidonic acid from the diet, which is expected to decrease production of arachidonic acid-derived pro-inflammatory eicosanoids such as leukotriene B4 (LTB4) and prostaglandin E2 (PGE2).
The effect of increasing omega-3 intake relative to omega-6 intake on inflammation has been of interest in conditions including cardiovascular disease and cognition, as well as RA [12–14]. In vitro, human macrophages stimulated with EPA and DHA produced lower levels of pro-inflammatory eicosanoids [9]. Similarly, a study in seven healthy human subjects taking 3.2 g EPA and 2.2 g DHA supplements daily for 6 weeks reported complete inhibition of neutrophil adherence to endothelium in the setting of LTB4 [15]. Furthermore, neutrophil chemotaxis in response to LTB4 was reduced 70 % compared to pre-treatment chemotactic response levels.
Downregulation of the NLRP3 Inflammasome
Myeloid cells contain inflammasomes, large intracellular complexes that recognize harmful intracellular pathogens and trigger an inflammatory response [16•]. Activation of the nod-like receptor (NLRP3) inflammasome leads to production of inflammatory cytokines including interleukin-1 beta (IL-1β), involved in the pathological inflammatory response in RA [17, 18]. Genetic variation in components of the NLRP3 inflammasome has been reported to influence RA severity [19]. Inhibition of the inflammasome may be one of several mechanisms by which omega-3 fatty acids could affect RA symptoms, as omega-3 fatty acids were shown to inhibit the NLRP3 inflammasome in human macrophages in vitro [20].
In a starvation state, or in the setting of a low-carbohydrate ketogenic diet, the human body produces and utilizes ketone bodies—beta-hydroxybutyrate (BHB) and acetoacetate—as alternate energy sources in place of adenosine triphosphate. Recently, it was shown that BHB suppressed macrophage NLRP3 inflammasome activation in response to urate crystals in a murine model [21]. Additionally, in human monocytes, BHB reduced NLRP3 inflammasome-mediated IL-1β production [21]. These in vitro and animal studies support the idea that NLRP3 inflammasome inhibition may underlie the benefit of caloric restriction or a very low-carbohydrate ketogenic diet in RA.
Caloric restriction has been tested as a potential therapy for RA, generally with favorable results [22–24]. Caloric restriction involves consistent intake of a limited number of calories while maintaining essential nutrients [25]. In this setting, metabolic adaptation occurs. In a prospective study of ten obese Caucasian males with type 2 diabetes, caloric restriction and weight loss for 1 year led to a reduction in adipose tissue expression of the NLRP3 inflammasome and IL-1β [26]. Furthermore, in a study of 218 non-obese subjects randomized to caloric restriction vs. regular caloric intake for 2 years, tumor necrosis factor-alpha (TNF-α) was decreased in the caloric restriction group vs. control arm at 24 months [25]. We hypothesize that inhibition of the NLRP3 inflammasome in the setting of caloric restriction may explain part of the beneficial effect on RA symptoms observed in small trials of caloric restriction.
Microbiome-Derived Metabolites Affect Immune Cell Function
The commensal bacteria residing in the human gastrointestinal system are collectively referred to as the gut microbiome, a topic of growing interest in autoimmunity research. These bacteria are involved in digestion of dietary fiber and other foodstuffs into metabolites, and also play a role in vitamin synthesis. Commensal gut bacteria cleave ingested fiber into short-chain fatty acids (SCFA), which are among the predominant metabolites produced by the microbiome [27]. SCFA produced in the gut are then distributed through the circulation and have been shown to influence macrophage and dendritic cell function, with anti-inflammatory results [28]. SCFA have been shown to decrease production of inflammatory cytokines including TNF-α, interleukin-6 (IL-6), and interferon-gamma [29]. SCFA have also been demonstrated to increase the number and function of regulatory T cells (Tregs), which in turn promote self-tolerance [30•].
Additionally, dietary metabolites, including SCFA, omega-3 fatty acids, and medium-chain fatty acids, have been shown to act as ligands for G protein-coupled receptors (GPR) on the gut epithelium, as well as on innate immune cells (neutrophils and macrophages) and regulatory T lymphocytes [27]. When bound to their ligands, these GPRs are thought to stimulate anti-inflammatory pathways. In a murine model of inflammatory arthritis, mice lacking a SCFA-binding GPR had more active synovitis and more neutrophil activation compared to wild-type mice [31].
Decreased Expression of Cellular Adhesion Markers on Lymphocytes and Monocytes
Expression of vascular adhesion molecules and intracellular adhesion molecules on immune system cells contribute to the inflammatory response in RA [32]. Thus, it is posited that downregulation of these adhesion proteins may decrease inflammation. A study of fish oil supplements in 12 healthy adults reported changes in monocyte surface molecule expression [33]. In vitro studies of olive oil extract have also demonstrated downregulation of vascular cell adhesion molecule-1 (VCAM-1), intracellular adhesion molecule-1 (ICAM-1), and E-selectin expression in vascular endothelial cells [34, 35].
Dampening of Inflammatory Cytokine Production and the Promotion of Inflammation Resolution
Multiple in vitro studies have reported that omega-3 fatty acid-derived EPA and DHA can inhibit inflammatory cytokine production by human leukocytes [36–40]. A newly discovered genus of locally active, omega-3-derived molecules including resolvins, protectins, and maresins—collectively termed “specialized pro-resolving mediators” (SPM)—facilitate the cessation of inflammation [41••]. In vitro, omega-3-derived SPMs stimulate macrophage phagocytosis to clear cellular debris and deter local neutrophil invasion. They also dampen the production of many inflammatory cytokines and chemokines, leading to the resolution of inflammation [41••]. In 100 human volunteers, taking a capsule containing 500 mg EPA and 200 mg DHA resulted in measurable short-term (4 h) increases in circulating plasma levels of many SPM measured by liquid chromatography and mass spectroscopy (“lipidomics”) [42]. Lipidomic profiling of synovial fluid from five RA patients, obtained during knee arthroscopy, identified the presence of SPMs [43]. The influence of omega-3 fatty acid consumption and the production of pre-resolving mediators of inflammation in RA have not yet been evaluated.
Additionally, ingestion of raw olive oil—a component of the Mediterranean diet—has been shown to decrease plasma concentrations of IL-6 and C-reactive protein (CRP) in a randomized, placebo-controlled crossover trial of 28 subjects with stable coronary artery disease [44].
Nutrients and RA Disease Activity
Fish Oil and Omega-3 Fatty Acids
Several important trials of fish oil supplementation were performed in the 1990s, before widespread access to biologic disease-modifying anti-rheumatic drugs (DMARDs). Trials of fish oil (EPA + DHA) supplements in RA have tested doses from 2 to 9 g per day, and have generally shown positive results [12, 45, 46, 47••, 48]. As a point of comparison, one serving of fish generally provides less than 2 g of EPA + DHA [49]. (Comprehensive reviews of studies of marine omega-3 fatty acids in RA are provided in these references [7, 50–52].)
In 1995, a double-blind, 48-week trial randomized 66 RA patients with baseline use of non-steroidal anti-inflammatory drugs (NSAIDs) to fish oil (up to 9 g/day) vs. placebo following cessation of NSAID therapy [48]. Those randomized to fish oil had improvements in tender joint count and physician global assessment of RA activity. In 2000, another double-blind, randomized trial evaluated fish oil supplements (up to 2 g omega-3 fatty acid/day) vs. placebo for 15 weeks among 50 RA subjects whose baseline diet was low in omega-6 fatty acids (<10 g/day) [12]. The intervention arm had significant improvements from baseline to 15 weeks in swollen joint count, morning stiffness, pain visual analog scale (VAS), patient global, physician global, and health assessment questionnaire (HAQ). Compared to the placebo arm, the intervention arm had significantly greater improvement in morning stiffness and HAQ by week 15.
A more recent 12 month, double-blind, placebo-controlled trial of high-dose (5.5 g/day EPA + DHA) vs. low-dose (400 mg/day EPA + DHA) fish oil in 140 early RA (<12 months disease duration, DMARD naïve) patients was conducted in Australia [47••]. All subjects also started “triple therapy” with oral methotrexate, sulfasalazine, and hydroxychloroquine at study entry; the primary endpoint was failure of triple therapy to achieve low disease activity at 12 months. The high-dose fish oil group had less failure of triple therapy (10.5 %) compared to the low-dose group (32.1 %) at 12-month follow-up. The rate of triple therapy failure was significantly lower in the high-dose fish oil group (hazard ratio 0.28, 95 % CI [0.12–0.63]) compared to the low-dose group. Achievement of clinical remission occurred significantly earlier among the high-dose than the low-dose group, after adjustment for smoking, human leukocyte antigen (HLA)-shared epitope, and the presence of anti-cyclic citrullinate peptide (CCP) antibodies.
Another recent but shorter 16-week double-blind, randomized, placebo-controlled trial involved 109 RA patients in South Korea [53]. Subjects were randomized to 2.1 g EPA plus 1.2 g DHA daily or placebo. The intervention had no significant effects on RA symptoms or inflammatory cytokine concentrations (CRP, LTB4, PGE2, TNF-α, IL-6) among all subjects, but significantly decreased NSAID use and LTB4 levels among subjects weighing >55 kg.
While fish oil supplementation appears to have anti-inflammatory effects in most RA clinical trials, the potential benefit of eating whole foods, such as fatty fish and other foods with high omega-3 content, has not been evaluated to date.
Vitamin D
Vitamin D is a pleiotropic hormone with endocrine and paracrine effects, as well as multiple effects on immune function, at least in vitro. Lymphocytes express vitamin D receptors, and vitamin D has been shown to affect antigen presentation by dendritic cells and to alter of B and T lymphocyte function [54••]. Vitamin D is produced in the skin after sunlight exposure and circulating levels are also affected by oral intake [55, 56]. Vitamin D is found in fish, milk, cheese, egg yolks, meat, poultry, and fortified foods [57, 58]. The relationship between vitamin D intake and risk of developing RA is not clear from observational studies [59, 60].
Two prospective trials have evaluated the impact of vitamin D supplementation on disease activity in established RA patients. A 3-month, open-label trial of high-dose oral alphacalcidol, an active vitamin D3 analog (2 μg/day), enrolled 19 RA subjects with longstanding RA (3 to 13 years duration) on standard DMARD therapy [61]. After 3 months, 89 % reported a beneficial effect on disease activity, 100 % had decreased tender joint count compared to baseline; the swollen joint count decreased non-significantly. By contrast, a recent 12 week randomized, double-blind, placebo-controlled trial of 25-hydroxy vitamin D 50,000 IU weekly vs. placebo among 117 RA subjects found that vitamin D supplementation did not affect RA disease activity [62••]. At enrollment, subjects had active RA (disease activity score in 28 joints (DAS28) >3.2 and morning stiffness ≥45 min) and were taking a stable dose of methotrexate (7.5–20 mg/week) for at least 8 weeks; use of hydroxychloroquine and/or a stable dose of prednisone ≤10 mg daily was also permitted. At week 12, subjects in the intervention arm had significantly higher serum vitamin D levels compared to the placebo arm. However, there was no significant difference in achievement of DAS28 response, defined as improvement in DAS28 by 0.6 units, between the vitamin D arm (76 %) and placebo arm (65 %). There was also no significant difference in erythrocyte sedimentation rate (ESR) between the two arms at week 12.
While vitamin D does not appear to have disease-modifying effects in RA, it does have beneficial effects in the treatment and prevention of osteoporosis [63], for which RA patients are at increased risk, and, for that reason, we continue to recommend it to our RA patients.
Alcohol
In the general population, moderate alcohol intake has been associated with lower levels of inflammatory cytokines [64–66]. However, studying the effects of alcohol on RA disease activity is complicated. Methotrexate and leflunomide are potentially hepatotoxic, and the risk of cirrhosis may be synergistically elevated in the setting of alcohol intake. Glucocorticoids and NSAIDs both increase the risk of gastrointestinal ulceration and bleeding, as does alcohol. Thus, patients using these medications for RA are generally counseled to decrease or abstain from alcohol.
The first study to evaluate the relationship between alcohol intake and RA disease activity was a cross-sectional study in a UK-based cohort of 873 RA subjects with disease duration three or more years [67]. Alcohol consumption at cohort entry was assessed in relationship to clinical and radiographic severity at cohort entry. At cohort entry, 63 % reported alcohol use on one or more days per month, and 54 % were taking methotrexate. Increasing frequency of alcohol consumption (days per month) was inversely associated with all measures of RA severity (CRP, DAS28-CRP, pain VAS, modified HAQ, and radiographic damage by the Larsen score).
A prospective observational study of 615 RA patients followed at a US academic medical center evaluated the relationship between alcohol consumption and repeated measures of RA disease activity [68]. DAS28-CRP3 was assessed by the treating rheumatologist annually, for up to seven years. At cohort entry, mean disease duration was 15 years, mean DAS28-CRP3 was 4, 66 % reported current alcohol use, and 48 % of all subjects were taking methotrexate. Alcohol consumption had a weak J-shaped relationship with DAS28-CRP3 in seropositive RA (anti-CCP and/or RF positive) in models adjusted for baseline DAS28-CRP3, medication use, sex, age, race, education, disease duration, and body mass index. The minimum DAS28-CRP3 was detected in RA patients consuming 5.1–10.0 g of alcohol per day, which is less than one standard drink per day [69].
The relationship between alcohol consumption and RA disease activity was also studied in a cross-sectional analysis of a prospective cohort of early RA patients (≤2 years) in Sweden [70]. In 2010, 1238 subjects completed a one-time mailed survey assessing alcohol use, medications, patient global, pain VAS, HAQ, and self-reported swollen and tender joint counts. Of these, 89 % reported alcohol use, 21 % of the cohorts were classified as “hazardous drinkers,” and 60 % of the total was taking methotrexate. Self-reported tender joint count, patient global, pain VAS, and HAQ were each significantly lower in subjects who drank alcohol compared to non-drinkers, but the absolute magnitude of difference in these disease activity measures between groups was small. In multivariable-adjusted analyses, alcohol use had a non-significant inverse association with patient global and HAQ.
Given the aforementioned health risks associated with alcohol in combination with methotrexate and leflunomide in particular, we counsel RA patients to completely avoid or consume only very small quantities of alcohol (less than two to three drinks per week). The benefit and the safety of moderate alcohol intake in RA deserve further evaluation.
Dietary Patterns and RA Disease Activity
Mediterranean Diet
The diet of countries bordering the Mediterranean Sea includes high quantities of olive oil, fruits, vegetables, whole grain cereals, legumes, nuts, seeds; moderate amounts of fish, shellfish, white meat, eggs, and fermented dairy (cheese and yogurt); small amounts of red meat, processed meats, and sugars; and frequent, moderate red wine intake [71]. This diet has high total fat content (40–50 % of total daily calories), but low saturated fat (≤8 % of calories). Greater adherence to a Mediterranean diet pattern was associated with lower concentrations of inflammatory biomarkers among healthy female nurses in the USA [72] and among subjects with cardiovascular risk factors in Spain and Greece [73, 74]. Data on specific anti-inflammatory effects are scarce and mainly based on observational findings and short-term interventions [75, 76].
Two trials of the Mediterranean diet in RA have been published. A 12-week randomized, controlled trial among 51 RA patients in Sweden evaluated the impact of a Cretan Mediterranean diet (modified to include more fermented dairy [yogurt and cheese] to appeal to the Swedish patient population) versus regular diet [77]. Subjects had active disease (DAS28 > 2.0), disease duration greater than 2 years, and were taking stable doses of DMARDs for ≥3 months, corticosteroids <12.5 mg prednisolone for ≥1 month, and/or NSAIDs for ≥10 days. The dietary intervention was monitored for the first 3 weeks, during which subjects were served lunch and dinner at an outpatient rehabilitation center. Subsequently, they were instructed to continue with the assigned diet at home for the duration of the trial. Eighty-six percent of subjects were taking at least one DMARD at study entry. At week 12, subjects in the Cretan diet arm had a significant improvement in DAS28, HAQ, and vitality scores compared to baseline, whereas subjects in the control arm had no significant change in these measures.
A real-world, non-randomized, Mediterranean-type dietary intervention was conducted in the UK among 130 female RA patients with mean disease duration of 9 years [78]. The intervention consisted of a weekly cooking class for 6 weeks with emphasis on a Mediterranean-type diet, while the control arm received written information on healthy eating. A significant increase in the number of daily fruit and vegetable servings between baseline and 3 months was seen in the intervention arm, but not in the control arm. At 3 months, pain VAS and HAQ were significantly better in the intervention arm than the control arm. At 6 months, patient global, pain VAS, and morning stiffness were significantly better in the intervention arm than the control arm.
Why Is There such a Dearth of Data About Diet as a Treatment for RA?: Challenges in the Study of Diet in Relationship to RA Disease Activity
Studying the relationship of diet to RA disease activity is challenging for many reasons. Most RA patients are now treated with DMARDs, which are often highly effective. Compared to these pharmacological treatments, the effect of diet on RA symptoms is likely to be small. Thus, studies of diet in RA patients receiving pharmacological treatment may require large sample sizes to detect small differences in disease activity associated with dietary intake and to be able to control for many other factors, including medications, that can influence RA disease activity. Most past studies of diet and RA disease activity were conducted before the widespread use of biologic DMARDs. The potential influence of diet in the setting of these potent therapies is not well-studied.
Designing and implementing studies to evaluate the relationship between diet and RA disease activity is challenging. Double-blind, randomized, placebo-controlled trials, the gold standard for prospective studies, are difficult to design and implement for studying dietary factors. Subjects cannot be blinded to what they are eating, unless formula feeding is provided for the intervention and control arms. Subject compliance with dietary interventions is often less than ideal, and secular trends in diet may inadvertently result in the control group adopting the dietary behavior assigned to the intervention group [79]. Additionally, interventions that result in weight loss could result in improved disease activity via weight loss itself, rather than due to changes in diet composition.
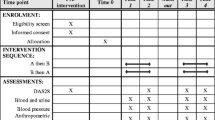
Confounders are particularly important in observational studies and small, non-randomized trials of diet and disease activity (Fig. 1). Some confounders of the relationship between diet and RA disease activity are measureable, for example, smoking, physical activity, socioeconomic status, and obesity. Measurement of and adjustment for these and other potential confounders are critical for the validity of study results. However, many unmeasured or difficult-to-measure potential confounders of the relationship between dietary intakes and patterns and RA disease activity likely exist (depression, sleep habits, health literacy) and may challenge the validity of results.
In addition to potential confounding, prospective observational studies are subject to other challenges. Among the multiple tools available for collecting dietary data, there is no consensus about which is ideal. Diet records, in which subjects measure and record their food intake in real-time, are often considered the gold standard for dietary assessment but may be difficult to implement. They require a large commitment of subject time and effort, are relatively expensive to process, and do not represent time-integrated data but rather reflect recent dietary intake, which varies by season [79]. Twenty-four hour dietary recall relies on a subject remembering what he or she has eaten in the past 24 hours; this method is subject to error due to memory, and only reflects recent intake rather than long-term intake. Food frequency questionnaires, which assess usual dietary intake in the past year, correlate well with diet records [79]; however, these are also subject to recall bias. Moreover, retrospective study designs generally are inappropriate for studying diet and RA disease activity, as affected subjects would be likely to have biased recall of dietary exposures.
The appropriate interval to study between dietary exposure and change in disease activity is also unclear. It is possible that chronic dietary exposures—for example, adherence to particular dietary patterns or frequent consumption of specific foods or nutrients—may impact a patient’s general state of disease activity over many months. While patients may report fluctuations in symptoms in relationship to recent dietary changes, existing literature on this topic is extremely limited.
Gaps in Knowledge and Areas for Future Investigations
Omega-3 fatty acids are the most thoroughly studied potential dietary therapy for RA; more sparse data exist for vitamin D, alcohol, and Mediterranean diet. Future studies should focus on dietary patterns that have been implicated in other inflammatory conditions, including cardiovascular disease. The “Western” dietary pattern involves higher intake of red and processed meats, sweets and desserts, French fries, and refined grains, and has been associated with elevated biomarkers of inflammation [80]. A recent study found that women in the U.S. Nurses’ Health Studies whose diets were characterized by a Western pattern had increased risk of developing RA [81]. By contrast, women whose diet was most aligned with a “prudent” dietary pattern, with higher intake of fruits, vegetables, legumes, fish, poultry, and whole grains, had decreased RA risk. Whether adherence to these dietary patterns affects RA symptoms in patients with an established RA diagnosis is unknown.
Nightshade vegetables (tomatoes, potatoes, peppers, eggplant) are often mentioned by patients and discussed in patient-oriented websites as exacerbating RA symptoms [82, 83]. To our knowledge, current published, peer-reviewed literature has never addressed potential associations between nightshade vegetables and RA disease activity. We do not counsel our patients to avoid these vegetables, which contain important vitamins and minerals. Data on gluten and RA symptoms is also scarce; trials of gluten-free diets in RA involved concurrent vegan diets, and thus the effect of the gluten elimination alone cannot be discerned [22, 84].
A review of all dietary supplements is beyond the scope of this review. A number of small trials in RA patients have investigated the effects of probiotics [85–87], glucosamine [88], and antioxidant supplements (selenium, zinc, vitamin A, vitamin C, vitamin E) [89, 90] on RA disease activity, oxidative stress, or inflammatory biomarkers in RA. In general, these supplements had marginal, non-significant beneficial effects in RA. As many RA patients believe that diet affects their symptoms and/or have altered their diets in attempt to alleviate RA symptoms [91], additional, well-designed studies of dietary patterns and nutrients are needed before RA-specific recommendations can be made.
Conclusions
The literature supports a beneficial effect of moderate-to-high doses of omega-3 fatty acids (EPA and DHA) on several parameters of RA disease activity [52]. However, these effects are not sufficient to replace standard-of-care pharmacotherapy with DMARDs. For patients who are interested in adjunctive dietary therapy in addition to DMARD therapy and who are able to afford the out-of-pocket cost of fish oil supplements, we advise that consuming approximately 3 g EPA plus DHA daily may improve some of their RA symptoms.
The most robust data on vitamin D supplementation do not support a beneficial effect on RA disease activity. However, this conclusion is based on a single randomized trial of high-dose weekly vitamin D supplementation; the impact of lower, daily doses of vitamin D supplementation on RA disease activity has not been evaluated. Moderate alcohol use appears to be associated with lower RA disease activity in observational studies, although causal effects cannot be established by the existing literature. Additionally, the relative risks and benefits of alcohol use among patients using DMARDs, corticosteroids, and NSAIDs remain to be studied. Strict adherence to a Mediterranean diet appeared to have modest benefit on RA disease activity and symptoms among a Scandinavian RA population. We advocate for repeating this study in other countries, to evaluate its effectiveness in the context of different baseline diets prior to the intervention. Although there are many challenges to studying diet as an adjunctive treatment in RA, further study of other dietary patterns and nutrients will be necessary before RA-specific recommendations can be made.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bykerk VP, Shadick N, Frits M, et al. Flares in rheumatoid arthritis: frequency and management. A report from the BRASS registry. J Rheumatol. 2014;41(2):227–34.
Arthritis Foundation. Nutrition guidelines for people with rheumatoid arthritis. Accessed May 29, 2015 http://www.arthritis.org/living-with-arthritis/arthritis-diet/anti-inflammatory/rheumatoid-arthritis-diet.php.
WebMD. Can your diet help ease rheumatoid arthritis? Accessed May 29, 2015 http://www.webmd.com/rheumatoid-arthritis/rheumatoid-arthritis-diet.
Arthritis Foundation. Anti-inflammatory diet. Accessed May 29, 2015 http://www.arthritis.org/living-with-arthritis/arthritis-diet/anti-inflammatory/anti-inflammatory-diet.php.
Smedslund G, Byfuglien MG, Olsen SU, et al. Effectiveness and safety of dietary interventions for rheumatoid arthritis: a systematic review of randomized controlled trials. J Am Diet Assoc. 2010;110(5):727–35.
Hagen KB, Byfuglien MG, Falzon L, et al. Dietary interventions for rheumatoid arthritis. Cochrane Database Syst Rev. 2009;1:CD006400.
Stamp LK, James MJ, Cleland LG. Diet and rheumatoid arthritis: a review of the literature. Semin Arthritis Rheum. 2005;35(2):77–94.
Dwyer JH, Allayee H, Dwyer KM, et al. Arachidonate 5-lipoxygenase promoter genotype, dietary arachidonic acid, and atherosclerosis. N Engl J Med. 2004;350(1):29–37.
Norris PC, Dennis EA. Omega-3 fatty acids cause dramatic changes in TLR4 and purinergic eicosanoid signaling. Proc Natl Acad Sci U S A. 2012;109(22):8517–22.
Whelan J. Antagonistic effects of dietary arachidonic acid and n-3 polyunsaturated fatty acids. J Nutr. 1996;126(4 Suppl):1086S–91S.
Raper NR, Cronin FJ, Exler J. Omega-3 fatty acid content of the US food supply. J Am Coll Nutr. 1992;11(3):304–8.
Volker D, Fitzgerald P, Major G, et al. Efficacy of fish oil concentrate in the treatment of rheumatoid arthritis. J Rheumatol. 2000;27(10):2343–6.
Tani S, Takahashi A, Nagao K, et al. Association of fish consumption-derived ratio of serum n-3 to n-6 polyunsaturated fatty acids and cardiovascular risk with the prevalence of coronary artery disease. Int Heart J. 2015;56(3):260–8.
Sakayori N, Kikkawa T, Tokuda H, et al. Maternal dietary imbalance between omega-6 and omega-3 polyunsaturated fatty acids impairs neocortical development via epoxy metabolites. Stem Cells. 2015.
Lee TH, Hoover RL, Williams JD, et al. Effect of dietary enrichment with eicosapentaenoic and docosahexaenoic acids on in vitro neutrophil and monocyte leukotriene generation and neutrophil function. N Engl J Med. 1985;312(19):1217–24.
Camell C, Goldberg E, Dixit VD. Regulation of Nlrp3 inflammasome by dietary metabolites. Semin Immunol. 2015. This review article provides an overview of activation of the NLRP3 inflammasome via dietary metabolites including fatty acids, glucose, and ketone bodies
Harrison P, Pointon JJ, Chapman K, et al. Interleukin-1 promoter region polymorphism role in rheumatoid arthritis: a meta-analysis of IL-1B-511A/G variant reveals association with rheumatoid arthritis. Rheumatology (Oxford). 2008;47(12):1768–70.
Gabay C, Lamacchia C, Palmer G. IL-1 pathways in inflammation and human diseases. Nat Rev Rheumatol. 2010;6(4):232–41.
Choulaki C, Papadaki G, Repa A, et al. Enhanced activity of NLRP3 inflammasome in peripheral blood cells of patients with active rheumatoid arthritis. Arthritis Res Ther. 2015;17:257.
L’Homme L, Esser N, Riva L, et al. Unsaturated fatty acids prevent activation of NLRP3 inflammasome in human monocytes/macrophages. J Lipid Res. 2013;54(11):2998–3008.
Youm YH, Nguyen KY, Grant RW, et al. The ketone metabolite beta-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat Med. 2015.
Kjeldsen-Kragh J, Haugen M, Borchgrevink CF, et al. Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. Lancet. 1991;338(8772):899–902.
Skoldstam L, Larsson L, Lindstrom FD. Effect of fasting and lactovegetarian diet on rheumatoid arthritis. Scand J Rheumatol. 1979;8(4):249–55.
Muller H, de Toledo FW, Resch KL. Fasting followed by vegetarian diet in patients with rheumatoid arthritis: a systematic review. Scand J Rheumatol. 2001;30(1):1–10.
Ravussin E, Redman LM, Rochon J, et al. A 2-year randomized controlled trial of human caloric restriction: feasibility and effects on predictors of health span and longevity. J Gerontol A Biol Sci Med Sci. 2015;70(9):1097–104.
Vandanmagsar B, Youm YH, Ravussin A, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17(2):179–88.
Thorburn AN, Macia L, Mackay CR. Diet, metabolites, and “western-lifestyle” inflammatory diseases. Immunity. 2014;40(6):833–42.
Trompette A, Gollwitzer ES, Yadava K, et al. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat Med. 2014;20(2):159–66.
Vinolo MA, Rodrigues HG, Nachbar RT, et al. Regulation of inflammation by short chain fatty acids. Nutrients. 2011;3(10):858–76.
Arpaia N, Campbell C, Fan X, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature. 2013;504(7480):451–5. This study demonstrated that in a murine model, commensal gut flora metabolized starch into short-chain fatty acids, which promoted regulatory T cell (Treg) differentiation.
Maslowski KM, Vieira AT, Ng A, et al. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature. 2009;461(7268):1282–6.
Sweeney SE, Firestein GS. Rheumatoid arthritis: regulation of synovial inflammation. Int J Biochem Cell Biol. 2004;36(3):372–8.
Hughes DA, Pinder AC, Piper Z, et al. Fish oil supplementation inhibits the expression of major histocompatibility complex class II molecules and adhesion molecules on human monocytes. Am J Clin Nutr. 1996;63(2):267–72.
Dell’Agli M, Fagnani R, Mitro N, et al. Minor components of olive oil modulate proatherogenic adhesion molecules involved in endothelial activation. J Agric Food Chem. 2006;54(9):3259–64.
Carluccio MA, Siculella L, Ancora MA, et al. Olive oil and red wine antioxidant polyphenols inhibit endothelial activation: antiatherogenic properties of Mediterranean diet phytochemicals. Arterioscler Thromb Vasc Biol. 2003;23(4):622–9.
Khalfoun B, Thibault F, Watier H, et al. Docosahexaenoic and eicosapentaenoic acids inhibit in vitro human endothelial cell production of interleukin-6. Adv Exp Med Biol. 1997;400B:589–97.
Trebble T, Arden NK, Stroud MA, et al. Inhibition of tumour necrosis factor-alpha and interleukin 6 production by mononuclear cells following dietary fish-oil supplementation in healthy men and response to antioxidant co-supplementation. Br J Nutr. 2003;90(2):405–12.
Babcock TA, Novak T, Ong E, et al. Modulation of lipopolysaccharide-stimulated macrophage tumor necrosis factor-alpha production by omega-3 fatty acid is associated with differential cyclooxygenase-2 protein expression and is independent of interleukin-10. J Surg Res. 2002;107(1):135–9.
Novak TE, Babcock TA, Jho DH, et al. NF-kappa B inhibition by omega-3 fatty acids modulates LPS-stimulated macrophage TNF-alpha transcription. Am J Physiol Lung Cell Mol Physiol. 2003;284(1):L84–9.
Lo CJ, Chiu KC, Fu M, et al. Fish oil decreases macrophage tumor necrosis factor gene transcription by altering the NF kappa B activity. J Surg Res. 1999;82(2):216–21.
Serhan CN, Chiang N, Dalli J. The resolution code of acute inflammation: novel pro-resolving lipid mediators in resolution. Semin Immunol. 2015;27(3):200–15. This review article describes the role of lipid mediators (specialized pro-resolving mediators) involved in the active process of inflammation resolution.
Colas RA, Shinohara M, Dalli J, et al. Identification and signature profiles for pro-resolving and inflammatory lipid mediators in human tissue. Am J Physiol Cell Physiol. 2014;307(1):C39–54.
Giera M, Ioan-Facsinay A, Toes R, et al. Lipid and lipid mediator profiling of human synovial fluid in rheumatoid arthritis patients by means of LC-MS/MS. Biochim Biophys Acta. 2012;1821(11):1415–24.
Fito M, Cladellas M, de la Torre R, et al. Anti-inflammatory effect of virgin olive oil in stable coronary disease patients: a randomized, crossover, controlled trial. Eur J Clin Nutr. 2008;62(4):570–4.
Adam O, Beringer C, Kless T, et al. Anti-inflammatory effects of a low arachidonic acid diet and fish oil in patients with rheumatoid arthritis. Rheumatol Int. 2003;23(1):27–36.
Berbert AA, Kondo CR, Almendra CL, et al. Supplementation of fish oil and olive oil in patients with rheumatoid arthritis. Nutrition. 2005;21(2):131–6.
Proudman SM, James MJ, Spargo LD, et al. Fish oil in recent onset rheumatoid arthritis: a randomised, double-blind controlled trial within algorithm-based drug use. Ann Rheum Dis. 2015;74(1):89–95. This randomized, double-blind, placebo-controlled trial evaluated the efficacy of high-dose versus low-dose fish oil supplements in preventing failure of triple DMARD therapy in early RA.
Kremer JM, Lawrence DA, Petrillo GF, et al. Effects of high-dose fish oil on rheumatoid arthritis after stopping nonsteroidal antiinflammatory drugs. Clinical and immune correlates. Arthritis Rheum. 1995;38(8):1107–14.
Health.gov Dietary Guidelines. EPA and DHA content of fish species (Data from NDB SR 16-1) Accessed June 8, 2015 http://www.health.gov/dietaryguidelines/dga2005/report/HTML/table_g2_adda2.htm.
Miles EA, Calder PC. Influence of marine n-3 polyunsaturated fatty acids on immune function and a systematic review of their effects on clinical outcomes in rheumatoid arthritis. Br J Nutr. 2012;107 Suppl 2:S171–84.
Proudman SM, Cleland LG, James MJ. Dietary omega-3 fats for treatment of inflammatory joint disease: efficacy and utility. Rheum Dis Clin North Am. 2008;34(2):469–79.
Goldberg RJ, Katz J. A meta-analysis of the analgesic effects of omega-3 polyunsaturated fatty acid supplementation for inflammatory joint pain. Pain. 2007;129(1-2):210–23.
Park Y, Lee A, Shim SC, et al. Effect of n-3 polyunsaturated fatty acid supplementation in patients with rheumatoid arthritis: a 16-week randomized, double-blind, placebo-controlled, parallel-design multicenter study in Korea. J Nutr Biochem. 2013;24(7):1367–72.
Jeffery LE, Raza K, Hewison M. Vitamin D in rheumatoid arthritis—towards clinical application. Nat Rev Rheumatol. 2015. This review article discusses mechanisms through which vitamin D could potentially affect RA pathogenesis and severity.
Heaney RP, Armas LA, French C. All-source basal vitamin D inputs are greater than previously thought and cutaneous inputs are smaller. J Nutr. 2013;143(5):571–5.
Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80(6 Suppl):1678S–88S.
Schmid A, Walther B. Natural vitamin D content in animal products. Adv Nutr. 2013;4(4):453–62.
Jakobsen J, Maribo H, Bysted A, et al. 25-Hydroxyvitamin D3 affects vitamin D status similar to vitamin D3 in pigs—but the meat produced has a lower content of vitamin D. Br J Nutr. 2007;98(5):908–13.
Costenbader KH, Feskanich D, Holmes M, et al. Vitamin D intake and risks of systemic lupus erythematosus and rheumatoid arthritis in women. Ann Rheum Dis. 2008;67(4):530–5.
Merlino LA, Curtis J, Mikuls TR, et al. Vitamin D intake is inversely associated with rheumatoid arthritis: results from the Iowa Women’s Health Study. Arthritis Rheum. 2004;50(1):72–7.
Andjelkovic Z, Vojinovic J, Pejnovic N, et al. Disease modifying and immunomodulatory effects of high dose 1 alpha (OH) D3 in rheumatoid arthritis patients. Clin Exp Rheumatol. 1999;17(4):453–6.
Salesi M, Farajzadegan Z. Efficacy of vitamin D in patients with active rheumatoid arthritis receiving methotrexate therapy. Rheumatol Int. 2012;32(7):2129–33. This is the only randomized, placebo-controlled trial of vitamin D supplementation in RA published as of January 2016, to our knowledge.
Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. 2011;364(3):248–54.
Imhof A, Froehlich M, Brenner H, et al. Effect of alcohol consumption on systemic markers of inflammation. Lancet. 2001;357(9258):763–7.
Sierksma A, Patel H, Ouchi N, et al. Effect of moderate alcohol consumption on adiponectin, tumor necrosis factor-alpha, and insulin sensitivity. Diabetes Care. 2004;27(1):184–9.
Brien SE, Ronksley PE, Turner BJ, et al. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636.
Maxwell JR, Gowers IR, Moore DJ, et al. Alcohol consumption is inversely associated with risk and severity of rheumatoid arthritis. Rheumatology (Oxford). 2010;49(11):2140–6.
Lu B, Rho YH, Cui J, et al. Associations of smoking and alcohol consumption with disease activity and functional status in rheumatoid arthritis. J Rheumatol. 2014;41(1):24–30.
Prevention CfDCa. Alcohol and public health. Accessed 4 Feb 2016 http://www.cdc.gov/alcohol/faqs.htm.
Bergman S, Symeonidou S, Andersson ML, et al. Alcohol consumption is associated with lower self-reported disease activity and better health-related quality of life in female rheumatoid arthritis patients in Sweden: data from BARFOT, a multicenter study on early RA. BMC Musculoskelet Disord. 2013;14:218.
Casas R, Sacanella E, Estruch R. The immune protective effect of the Mediterranean diet against chronic low-grade inflammatory diseases. Endocr Metab Immune Disord Drug Targets. 2014;14(4):245–54.
Fung TT, McCullough ML, Newby PK, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82(1):163–73.
Sanchez-Tainta A, Estruch R, Bullo M, et al. Adherence to a Mediterranean-type diet and reduced prevalence of clustered cardiovascular risk factors in a cohort of 3,204 high-risk patients. Eur J Cardiovasc Prev Rehabil. 2008;15(5):589–93.
Athyros VG, Kakafika AI, Papageorgiou AA, et al. Effect of a plant stanol ester-containing spread, placebo spread, or Mediterranean diet on estimated cardiovascular risk and lipid, inflammatory and haemostatic factors. Nutr Metab Cardiovasc Dis. 2011;21(3):213–21.
Mena MP, Sacanella E, Vazquez-Agell M, et al. Inhibition of circulating immune cell activation: a molecular antiinflammatory effect of the Mediterranean diet. Am J Clin Nutr. 2009;89(1):248–56.
Bendinelli B, Masala G, Saieva C, et al. Fruit, vegetables, and olive oil and risk of coronary heart disease in Italian women: the EPICOR Study. Am J Clin Nutr. 2011;93(2):275–83.
Skoldstam L, Hagfors L, Johansson G. An experimental study of a Mediterranean diet intervention for patients with rheumatoid arthritis. Ann Rheum Dis. 2003;62(3):208–14.
McKellar G, Morrison E, McEntegart A, et al. A pilot study of a Mediterranean-type diet intervention in female patients with rheumatoid arthritis living in areas of social deprivation in Glasgow. Ann Rheum Dis. 2007;66(9):1239–43.
Willett WC. Nutritional epidemiology. 3 ed: Oxford University Press, 2012.
Fung TT, Schulze M, Manson JE, et al. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Arch Intern Med. 2004;164(20):2235–40.
Lu B, Hu Y, Sparks JA, et al. Prospective study of dietary patterns and risk of rheumatoid arthritis in women. San Francisco, CA: American College of Rheumatology Annual Scientific Meeting; 2015.
Clinic C. How to ease your arthritis pain with simple food swaps. Accessed 2016 Feb 4 http://health.clevelandclinic.org/2014/07/simple-food-swaps-to-ease-arthritis-pain/.
Report UNSW. Is the autoimmune paleo diet legit? Accessed 4 February 2016 http://health.usnews.com/health-news/health-wellness/articles/2015/01/16/is-the-autoimmune-paleo-diet-legit.
Hafstrom I, Ringertz B, Spangberg A, et al. A vegan diet free of gluten improves the signs and symptoms of rheumatoid arthritis: the effects on arthritis correlate with a reduction in antibodies to food antigens. Rheumatology (Oxford). 2001;40(10):1175–9.
Hatakka K, Martio J, Korpela M, et al. Effects of probiotic therapy on the activity and activation of mild rheumatoid arthritis—a pilot study. Scand J Rheumatol. 2003;32(4):211–5.
Vaghef-Mehrabany E, Homayouni-Rad A, Alipour B, et al. Effects of probiotic supplementation on oxidative stress indices in women with rheumatoid arthritis: a randomized double-blind clinical trial. J Am Coll Nutr. 2015;1–9.
Alipour B, Homayouni-Rad A, Vaghef-Mehrabany E, et al. Effects of Lactobacillus casei supplementation on disease activity and inflammatory cytokines in rheumatoid arthritis patients: a randomized double-blind clinical trial. Int J Rheum Dis. 2014;17(5):519–27.
Nakamura H, Masuko K, Yudoh K, et al. Effects of glucosamine administration on patients with rheumatoid arthritis. Rheumatol Int. 2007;27(3):213–8.
Jalili M, Kolahi S, Aref-Hosseini SR, et al. Beneficial role of antioxidants on clinical outcomes and erythrocyte antioxidant parameters in rheumatoid arthritis patients. Int J Prev Med. 2014;5(7):835–40.
van Vugt RM, Rijken PJ, Rietveld AG, et al. Antioxidant intervention in rheumatoid arthritis: results of an open pilot study. Clin Rheumatol. 2008;27(6):771–5.
Tanner SB, Callahan LF, Panush RS, et al. Dietary and allergic associations with rheumatoid arthritis. Arthritis Rheum. 1990;3(4):189–95.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
KHC reports funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes of Health for research on diet and risk of developing rheumatoid arthritis: NIH R01 AR049880, R01 AR059086, and R01 AR061362.
Human and Animal Rights and Informed Consent
This article does not contain studies performed by either of the authors with human or animal subjects.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Complementary and Alternative Medicine
Rights and permissions
About this article
Cite this article
Tedeschi, S.K., Costenbader, K.H. Is There a Role for Diet in the Therapy of Rheumatoid Arthritis?. Curr Rheumatol Rep 18, 23 (2016). https://doi.org/10.1007/s11926-016-0575-y
Published:
DOI: https://doi.org/10.1007/s11926-016-0575-y