Abstract
Purpose of Review
We review 2016–2019 peer-reviewed literature which summarizes the factors contributing to high expense of treating depression among adults in the USA, and interventions that have been conducted to decrease depression treatment expenditures.
Recent Findings
Treatment expenditures associated with depression are high and growing, driven in part by increased health care utilization and a shift toward increased insurance coverage of medications and therapies. The majority of identified articles describe the elevated financial burden associated with treating individuals with chronic medical conditions who also have a depression diagnosis. The few available studies documenting health care system-level interventions identify that multi-target treatment for comorbid illness, collaborative care management, and integration of psychiatric treatment into primary care show promise for reducing depression treatment expenditures.
Summary
Additional research is needed to identify innovative, cost-effective state, and federal payer-initiated depression treatment models, and evaluation of collaborative care and integrated care models implemented to scale across multiple health care systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression is a common and often debilitating mood disorder associated with impairments in cognitive, emotional, and physical functioning [1]. A major depressive episode—the key diagnostic feature of the disorder—is a period of at least 2 weeks during which, more days than not, individuals experience low mood, loss of interest or pleasure in daily activities, and a significant disturbance in sleep, appetite, energy, concentration, or self-worth [1]. Onset may occur at any age, and risk factors range from temperament, environment, and genetic/physiological traits to minority stressors and social determinants of mental health [2]. While symptom-related burdens are well documented at the patient level [3], recent studies have begun to document disproportionate and rising financial burdens unique to this disease [4, 5].
With a lifetime prevalence of 20.6% in the United States (US) population [6], annual estimated expenditures to treat depression in the USA range widely: from $71.1 to $238.3 billion [7]. By one estimate, depression is the most expensive mental health disorder and the 6th costliest condition to treat nationwide [8]. Patients with depression incur greater health care costs and have higher health care utilization [9,10,11,12,13], the majority of which is associated with the treatment of frequently comorbid medical conditions [14, 15]. Depression is also associated with a number of negative health-related (e.g., decreased treatment compliance, increased smoking, biological dysregulations) and non-health-related (e.g., termination of education, interpersonal difficulties, loss of employment) burdens. In a recent national survey, for example, adults diagnosed with major depressive disorder (MDD) reported functioning at a full standard deviation below the national average [6]. The significant health care expenditures required to treat depression pose a major burden to the US health care system and for patients that face high out-of-pocket expenses. Therefore, reducing depression treatment expenditures is a timely and urgent issue.
The objective of this systematic review is twofold: (1) to examine factors underlying depression treatment expenditures in the USA and (2) to review interventions aimed to reduce expense for health care systems and patients. The scope of the review is limited to exploring the health care expenditures of depression treatment in the USA. There are myriad studies documenting the societal costs of depression, which include or are exacerbated by issues such as absenteeism from work and school, overall decrease in productivity, reduced interpersonal and social support, and public health concerns such as increased rates of teen pregnancy [5]. We update older reviews of depression treatment expenditures [4, 16], providing a focus on health care expenditures among those with and without comorbid chronic conditions, to review health system-specific factors that may contribute to rising expense, to highlight interventions that reduce depression treatment expenditures, and to summarize and provide suggestions to offer guidance for possible directions for future intervention and research.
Methods
In order to characterize depression treatment expenditures for adults in the USA and review interventions to reduce the financial burden of depression treatment, the research team conducted a systematic review of peer-reviewed articles published between 2016 and 2019. The review followed the Preferred Reporting Items for Systematic review and Meta-Analyses for Protocols (PRISMA-P) [17].
Identification, Screening, and Eligibility of Studies
Inclusion of articles was the result of a three-stage process: identification, screening, and eligibility. In the identification stage, the research team searched the PubMed online database for entries published between January 1, 2016, and April 26, 2019. Search criteria included abstracts containing the following terms: (1) depression or depressive disorders and (2) expenditure, expense, or payment. The term “cost,” although perhaps an obvious inclusion criteria, was not included due to the frequent use of the term to describe non-financial (i.e., societal, relational, vocational) burdens of depression in the USA [5]. The search was limited to peer-reviewed journal articles published in English with an adult (18 years or older) sample drawn from the USA estimating expenditures for depression care. Identification procedures yielded 245 studies after duplicates were deleted.
In the screening stage, abstracts of the 245 records were reviewed by two authors for inclusion. In the case an author determined a record did not meet inclusion criteria, the relevant exclusion criterion was recorded. After independent review, the same authors met to discuss discrepancies and reach consensus regarding whether articles satisfied inclusion criteria. Of the initial 245 records, 219 were excluded for the following reasons: (1) not about depression, n = 71, 32.4%; (2) sample not drawn from USA, n = 53, 24.2%; (3) not about health care expenditures, n = 88, 40.2%; (4) not empirical, n = 2, 0.9%; (5) not adult human focused, n = 5, 2.3%. The remaining 26 articles were screened in more depth for inclusion.
In the eligibility stage, three authors subsequently reviewed the full text of the remaining 26 articles for eligibility with the same exclusion criteria. An additional six articles were excluded for the following reasons: (1) not about depression, n = 2, 33.3%; (2) not about health care expenditures, n = 2, 33.3%; and (3) not adult human focused, n = 2, 33.3%. At the end of the eligibility phase, 20 articles met inclusion criteria (See Fig. 1).
Data Extraction
Three authors extracted and coded variables and themes from the full text of the 20 included articles. Authors met to reach consensus regarding coding discrepancies. Variables of interest included study characteristics (i.e., corresponding author, publication year, sample characteristics), results (i.e., unique expense of treating depression, factors contributing to expense, and guidelines for reducing expense), implications for research, and study biases and limitations (See Table 1). Three major categories were determined by the study team after review of the articles, with some reporting data in multiple categories: (1) factors contributing to the high expense of treating depression alone (n = 6); (2) incremental expense of treating depression in the presence of comorbid illness (n = 14); and (3) interventions showing promise to reduce the expense of depression treatment.
Results
Factors Contributing to the High Expense of Treating Depression
Across studies, depression was shown to confer significant increases in expenditures for payers (e.g., commercial insurance, Medicaid, Medicare) and out-of-pocket expenses. The majority of studies identified factors contributing to the high expense of treating depression by measuring either total expenditures (defined as expenditures aggregated across all individuals over a range of years), or annual per patient expenditures.
Studies show that depression has a significant impact on health care expenditures due to prolonged treatment, frequent outpatient visits, increased post-acute care, and recurrent hospitalization for preventable concerns, in part due to noncompliance with behavioral treatments. In a retroactive observational study using 2006–2013 Medicare Current Beneficiary Survey (MCBS) data, depression was associated with an increase of $5259 annual per member expenditures above mean annual member expenditures (i.e., depression treatment expenditures were $14,436 compared with the mean of $9177), after controlling for comorbidities and adjusting for risk [28].
From 1998 to 2007 to 2015, total overall expenditures for depression treatment in the USA increased from $12.4 billion to $15.6 billion to $17.4 billion, respectively, after adjustment for inflation to 2015 US dollars. This is a 40% overall increase in expenditures; however, there has been slowing growth in outpatient expenditures in the most recent years [27••]. Between 1998 and 2015, the percentage of total depression treatment expenditures paid for by the uninsured decreased from 32 to 20%, while the percentage of total depression treatment expenditures paid for by Medicaid increased from 19% in 1998 to 36% in 2015. Among those in depression treatment, the proportion of respondents receiving psychotherapy (53.7% in 1998 to 50.4% in 2015) and prescription medications (81.9% in 1998 to 80.8% in 2015) remained relatively stable over time. Total expenditures on medications for depression increased by 22.6% between 2008 and 2015, but per capita prescription expenditures for individuals receiving outpatient depression care decreased from $848 in 1998 to $603 in 2015, suggesting increased access to (greater number of individuals taking) psychotropic medications and an increased use of lower-cost generic psychotropic medications.
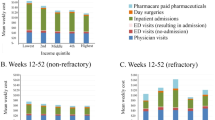
Other studies identified depression treatment expenditures among specific subgroups. One study identified that higher health care expenditures of treating depression are moderated by absenteeism at work. In a 2011–2014 analysis of the Medical Expenditure Panel Study (MEPS), depressed patients with work absences were found to have significantly higher rates of hospitalization and other health care visits than depressed patients who do not have work absences [37], suggesting that work absences may be a proxy for severity of illness and need for treatment. In another study, among Medicaid beneficiaries with severe mental illness, including depression, enrollment in medical home care coordination programs were associated with improved outcomes (i.e., increased access to specialty programming) but higher Medicaid expenditures [24]. A third study examined MEPS data from 1996 to 2011 to determine health care expenditures among a cohort of high-risk mothers facing marked social adversity (i.e., unmarried women aged 18–35 with ≥ 1 child and either unmarried or low income) [18•]. Among this subgroup, having a diagnosis of depression was associated with significantly greater payer and out-of-pocket expense. Depression increased total direct health care expenditures (i.e., expenditures for physicians, hospital services, medication, diagnostic testing) by $1.89 billion and indirect costs (i.e., labor productivity losses) by $523 million annually, suggesting income and gender-based adversity can compound the severity of depression, health care expenditures, and social costs.
Incremental Expense of Treating Depression in the Presence of Comorbid Illness
The majority of identified articles (n = 14) measured the incremental expense of treating depression in the context of comorbid illness: medical conditions that may exacerbate and/or be exacerbated by psychiatric illness [1]. Many of these studies examined medical claims for Medicare beneficiaries, a group with rates of comorbidities above the national average. Comorbidities in the current sample of papers include: diabetes (n = 3), rheumatoid arthritis (n = 1), back problems (n = 1), irritable bowel disease (n = 1), joint arthroplasty (n = 2), lupus (n = 1), hypertension (n = 3), migraine (n = 1), cognitive impairment (n = 1), and comorbidities generally (n = 1).
In a 2010–2012 MEPS sample of adult patients with spondylosis, intervertebral disc, and other back problems, patients with depression (a subsample of 20.2%) had significantly higher expenditures (overall and for inpatient, outpatient, prescription drug, and home health agency expenditures) compared with non-depressed patients [20]. Similarly, in a study with 2078 adults with irritable bowel disease, patients in the “high expenditure” category had significantly higher rates of psychiatric illness, including depression, than the median patient with irritable bowel disease (35.9% compared with 19.9%, p = 0.002), again demonstrating a positive association between comorbid depression and medical expenditures [21]. Patients with rheumatoid arthritis and comorbid depression (n = 647, 25.8% of the sample) had significantly higher annual health care expenditures than patients without comorbid depression ($14,752 versus $10,541, p < .001) as well as a greater out-of-pocket spending burden [23]. Other social costs of depression among such patients included increased unemployment and higher missed work days annually and lost annual wages.
Similar findings were demonstrated among patients with diabetes [7, 25]. In a large (n = 147,095), 8-year MEPS study, average annual health care expenditures were compared among patients with depression only, diabetes only, and comorbid depression and diabetes to a control group of patients who had neither disease. Per patient expenditures increased incrementally for all groups compared with those with no diagnoses: by $2654 (95% CI 2343–2966) for patients with depression only; by $2692, (95% CI 2338–3046) for patients with diabetes only; and by $6037 (CI 95% 5243–6830) for patients with comorbid depression and diabetes [7]. The adjusted total incremental expense per diagnostic group was $77.3 billion, $38.8 billion, and $26.6 billion per year, respectively. In another study with 15,548 diabetes patients, adjusted total incremental expense increased by $4.0 billion for unrecognized depression ($2872 per patient), $9.2 billion for asymptomatic depression ($3347 per patient), and $7.8 billion for symptomatic depression ($5170 per patient), as compared with non-depressed diabetes patients [25].
Similar results were found among patients with lupus, hypertension, and migraine headache. Patients with lupus and depression had higher average annual per-patient expenditures ($19,854 vs. $9735) compared with their non-depressed counterparts [30]. Comorbid hypertension and depression contributed similarly to elevated expense. In a 2011–2014 survey of patients with hypertension, depression was found to be the fourth most common comorbidity and increased annual total medical expenditures by $4296 per patient per year [31] compared with patients with hypertension but no depression diagnosis. Another hypertension study found that patients with depression had significantly higher inpatient ($4689.18 vs. $2712.74, p < .01) and pharmacy expenditures ($4301.38 vs. $2377.73, p < 0.01) than their non-depressed counterparts [33]. A 2006–2012 study assessing data from 2400 migraine patients (804 of whom had depression) found that comorbid depression was associated with higher all-cause medical ($6900 vs $3683, p < .001), prescription drug ($3112 vs $1057, p < .001), and overall ($10,012 vs $4740, p < .001) expenses per patient per year.
Interventions Showing Promise to Reduce the Expense of Depression Treatment
In line with previous reviews on cost-effective depression treatments [38], articles identified in this review highlight the importance of coordination of care among people with depression. Domino and colleagues [24], for example, estimated the expense of enrolling people with severe mental illness (including major depression) in primary care-based medical homes, in which an interdisciplinary team maintains responsibility for patients’ health care and coordinate care with specialty providers. Although these programs were found to improve access to care, overall and payer health care expenditures were not reduced, largely because of increased specialty mental health care utilization. These findings highlight that increased access to treatment may not reduce overall expenditures because reductions in inpatient treatment expenditures may not be realized, or may be offset by increased specialty mental health utilization.
A 2017 study by Ammerman and colleagues [19] found that in-home cognitive behavioral therapy, an adapted version of CBT tested among 93 depressed mothers facing social adversity, reduced health care expenditures significantly below those associated with standard of care. Reductions in expenditures were in part driven by decreased number of days per year experiencing depression symptoms. Another study assessed the merits of integrating depression treatment into primary care settings through an evaluation of 32 New York clinics implementing collaborative care programming [29•]. At the end of the implementation phase, 24 clinics sustained the collaborative care model and 7 opted out, with clinics terminating the program citing time/resource/personnel requirements, patient engagement, and staff engagement as key barriers. Clinics that sustained the collaborative care programming, however, reported greater clinical improvement rates (i.e., retention in outpatient care for depressed patients) than clinics that opted out, as well as steady rates of depression screening, staffing and treatment rates, and a greater number of contacts with patients. Although the study did not compare cost-saving merits of integrating coordinated care programming, representatives at sustaining clinics reported the program was financially secure and had robust patient and departmental support.
A second theme across studies is the need for further systematic evaluation of disease-modifying drugs to treat comorbid depressive and medical symptoms. Among rheumatoid arthritis patients, for example, Deb and colleagues [23] highlight improvements in depression symptoms following commencement and continuity of the rheumatoid arthritis-targeting medication rituximab [39].Well managed outpatient-psychiatric drug therapies may thus present an opportunity to reduce psychopharmaceutic expenditures among patients with depression and chronic medical conditions.
Other studies provide suggestions for interventions based on their own analyses of the pathways underlying high depression treatment expenditures. Collaborative care, multi-target psychotherapies, and disease-modifying drug treatments were mentioned often as showing promise in reducing depression symptoms and medical expenditures simultaneously [20, 23, 24, 29•]. Specific suggestions include the integration of cognitive behavioral therapy modalities with pain management to address corollary depressive symptoms among patients with back pain and depression [20]. Suggestions also include the development and further study of treatment outside the hospital setting, including in-home treatments to reduce hospital expenditures such as in-home cognitive behavioral therapy for low-income, depressed mothers [19]. In the context of comorbid depression and diabetes, Egede and colleagues argue for additional preventative screening, diagnosis, and treatment of depression among diabetes patients treated in primary care settings [7].
Similarly, among a sample of patients with rheumatoid arthritis (for whom the rate of depression was 25.8%), Deb and colleagues [23] recommend co-management of depression and rheumatoid arthritis through concurrent, collaborative depression care. Such an approach has been shown not only to reduce expenditures for health systems and out-of-pocket expenses for patients, but also to improve both psychiatric and medical outcomes given the complex interplay between mental and physical health [40]. Similarly, another study highlights the importance of incorporating disease-informed psychotherapeutic modalities, such as a dual pain management/depression cognitive behavioral therapy deliverable by a combination of psychiatrists and psychotherapists [20]. Similarly, medical providers (e.g., rheumatologists) are encouraged to train in strategies to integrate mental health services within primary care and specialty clinics [23]. Studies focused on comorbid depression and diabetes also touted the importance of collaborative depression care in primary care settings and within medical specialty clinics [7, 24].
Conclusions
We reviewed 20 articles related to depression treatment expenditures for adults published between January 2016 and April 2019. These articles represent a broad body of research outlining the factors contributing to the high expense of treating depression, the incremental expense of having a depression diagnosis in the presence of comorbid chronic illnesses, and evaluations and recommendations for interventions to reduce associated depression treatment expenditures.
In multiple adjusted analyses, individuals with a depression diagnosis had greater health care expenditures than their non-depressed counterparts, including among Medicare beneficiaries and among subgroups of individuals with varying chronic physical health conditions. These incremental costs are attributable to prolonged treatment, frequent hospitalizations, readmissions, post-acute care, and other potentially avoidable costly treatments received by this population [28].
Depression treatment continues to be a major factor in the US health care budget both in terms of level and growth. Total depression treatment expenditures increased by 40% after inflation adjustment between 1998 and 2015 from $12 to $17 billion [27••]. Much of this increase was driven by the 22.6% increase in expenditures for medications for depression treatment. An important development in expenditures is that the total amount spent in the USA on depression treatment by the uninsured has declined over time and increased for Medicaid, reflecting expanded insurance coverage of depression treatment in the USA, and decreasing the financial burden for some of the most vulnerable patients living with depression.
Given the high expense associated with depression care, we expect more health systems to move toward more cost-effective and financially sustainable payment and service delivery models such as value-based payment structures and collaborative care models (CCM). CCM integrates physical and mental health care using a team led by a primary care provider and may include a psychiatrist, care coordinator, and clinical psychologist/psychotherapist; long-term analyses suggest that for $1 spent on CCM, there is a $6.50 savings in health care expenditures [41]. CCM teams are often characterized by interdisciplinary teams, high levels of patient engagement, routine evidence-based follow-up, and value-based payment structures tying reimbursement to the quality of care and patient outcomes. While CCM may be best suited to address chronic comorbidities in primary care settings [7, 31, 34••, 35], several articles suggested approaches that co-manage chronic physical illnesses in specialty mental health care settings [20,21,23, 30].
In one study, payment reform away from fee for service to global payment or value-based payment models was found to be a strong incentive for clinics to transition to formal CCM; however, sustaining CCM also required buy-in from staff, administration, and time [29•]. Early research on health system and state-backed implementation of CCM has yielded mixed results and has identified obstacles to implementation. One major obstacle is that it takes time for clinics to realize the cost-saving benefits of CCM and integrated service delivery models. To overcome CCM implementation obstacles, Chung and colleagues outline a continuum-based framework for behavioral health integration, encouraging sites to make progress in some, if not all, domains depending on their administrative capacity [42]. Successful integrated care initiatives will facilitate provider and staff buy-in and will be resource-flexible permitting integration in lower-resource settings such as non-academic and rural health systems. As others note [7, 31], additional preventative screening and monitoring of depression in primary care settings is essential as depression synergistically aggravates other comorbidities. Developing collaborative medical-psychiatric treatment programs by integrating psychiatric care into community, primary, and specialty clinics may also help decrease depression-related stigma and improve retention and treatment outcomes [43].
Results and implications of the current review need to be considered within the study’s limitations. Sample sizes were at times small for studies for analyzing expenditures for comorbid patients. Future studies can identify broader, national samples of treatment expense for patients with depression within the context of large, diagnostically homogenous samples. Additionally, results estimating the systemic/health system-related factors contributing to treatment expenditures were limited given the majority of papers focused on the incremental expense of depression for those with chronic medical comorbid conditions. As such, more studies are needed to assess strategies to estimate and/or reduce the expense of treating depression at a health system level.
Given the critical importance of reducing expenditures to treat this highly prevalent, complex illness, health systems and patients will benefit from rigorous research evaluating the success and limitations of specific interventions [44]. Future research is needed to evaluate multiple types of intervention, ranging from innovative, peer-led models of care to large, multisite studies aimed to reduce the increasing impact of depression and comorbid illness on health care expenditures, patients, and society.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, D.C: American Psychiatric Pub; 2013.
Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26(4):392–407.
Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D depression symptoms index. J Aging Health. 1993;5(2):179–93.
Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155–62.
Kessler RC. The costs of depression. Psychiatr Clin N Am. 2012;35(1):1–14.
Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, et al. Epidemiology of adult dsm-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–46.
Egede LE, Bishu KG, Walker RJ, Dismuke CE. Impact of diagnosed depression on healthcare costs in adults with and without diabetes: United States, 2004-2011. J Affect Disord. 2016;195:119–26.
Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, et al. US spending on personal health care and public health, 1996-2013. JAMA. 2016;316(24):2627–46.
Beiser DG. et al., Depression in emergency department patients and association with health care utilization. Acad Emerg Med. 2019;0(0).
Dennehy EB, Robinson RL, Stephenson JJ, Faries D, Grabner M, Palli SR, et al. Impact of non-remission of depression on costs and resource utilization: from the COmorbidities and symptoms of DEpression (CODE) study. Curr Med Res Opin. 2015;31(6):1165–77.
Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care. 2004;42(6):512–21.
Robinson RL, Grabner M, Palli SR, Faries D, Stephenson JJ. Covariates of depression and high utilizers of healthcare: impact on resource use and costs. J Psychosom Res. 2016;85:35–43.
Yoon J, M. Yano E, Altman L, Cordasco KM, E. Stockdale S, Chow A, et al. Reducing costs of acute care for ambulatory care-sensitive medical conditions: the central roles of comorbid mental illness. Med Care. 2012;50(8):705–13.
Croghan TW, Obenchain RL, Crown WE. What does treatment of depression really cost? Health Aff. 1998;17(4):198–208.
Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Arch Intern Med. 2002;162(16):1860–6.
Birnbaum HG, Kessler RC, Kelley D, Ben-Hamadi R, Joish VN, Greenberg PE. Employer burden of mild, moderate, and severe major depressive disorder: mental health services utilization and costs, and work performance. Depress Anxiety. 2010;27(1):78–89.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
• Ammerman RT, et al. Annual direct health care expenditures and employee absenteeism costs in high-risk, low-income mothers with major depression. J Affect Disord. 2016;190:386–94. This article reviews the high costs associated with depression treatment among high-risk, low-income mothers facing social adversity. Using a longitudinal, large, and nationally representative sample, this is the sole study in the current review highlighting the impact of social determinants of health on treatment outcomes and expenditures.
Ammerman RT, Mallow PJ, Rizzo JA, Putnam FW, van Ginkel JB. Cost-effectiveness of in-home cognitive behavioral therapy for low-income depressed mothers participating in early childhood prevention programs. J Affect Disord. 2017;208:475–82.
Bilal J, et al. The influence of depression on health care expenditures among adults with spondylosis, intervertebral disc disorders, and other Back problems in the United States. Pain Med. 2018;0(0):1–9.
Click B, Ramos Rivers C, Koutroubakis IE, Babichenko D, Anderson AM, Hashash JG, et al. Demographic and clinical predictors of high healthcare use in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(6):1442–9.
Courtney PM, Bohl DD, Lau EC, Ong KL, Jacobs JJ & Della Valle CJ. Risk adjustment is necessary in Medicare bundled payment models for total hip and knee arthroplasty. J. Arthroplast. 2018;33(8):2368–2375. https://doi.org/10.1016/j.arth.2018.02.095.
Deb A, et al. Burden of depression among working-age adults with rheumatoid arthritis. Arthritis. 2018;2018:1–11.
Domino ME, Kilany M, Wells R, Morrissey JP. Through the looking glass: estimating effects of medical homes for people with severe mental illness. Health Serv Res. 2017;52(5):1858–80.
Egede LE, Walker RJ, Bishu K, Dismuke CE. Trends in costs of depression in adults with diabetes in the United States: medical expenditure panel survey, 2004-2011. J Gen Intern Med. 2016;31(6):615–22.
Gangan N & Yang Y. The impact of work absences on health services utilization and costs among employed individuals with depression. J. Occup. Environ. Med. 2018;60(3):e139–e145. https://doi.org/10.1097/jom.0000000000001259.
•• Hockenberry JM, et al. Trends in treatment and spending for patients receiving outpatient treatment of depression in the United States, 1998–2015. JAMA Psychiatry. 2019;Online:E1–8. This review of national trends in outpatient depression treatment and associated costs documents significant shifts in expenditures from 1998 to 2007, then again from 2007 to 2015 due to changes in health policy.
Johnston KJ, et al. Association between patient cognitive and functional status and Medicare Total annual cost of care: implications for value-based PaymentAssociation between patient cognitive and functional status and Medicare cost of CareAssociation between patient cognitive and functional status and Medicare cost of care. JAMA Intern Med. 2018;178(11):1489–97.
• Moise N, et al. Sustainability of collaborative care management for depression in primary care settings with academic affiliations across New York State. Implement Sci : IS. 2018;13(1):128–128. This New York State study reviews barriers and facilitators affecting whether 32 primary care clinics sustain a care management model for outpatient depression treatment.
Ogunsanya ME, Nduaguba SO, Brown CM. Incremental health care services and expenditures associated with depression among individuals with cutaneous lupus erythematosus (CLE). Lupus. 2018;27(7):1107–15.
Park C, Fang J, Hawkins NA, Wang G. Comorbidity status and annual total medical expenditures in U.S. hypertensive adults. Am J Prev Med. 2017;53(6, Supplement 2):S172–81.
Penna S, Bell KL, Kuo FC, Henderson RA, Foltz C & Chen AF. Impact of co-morbidities on the cost of care in primary elective joint arthroplasty. J. Arthroplast. 2019;34(5):834–838. https://doi.org/10.1016/j.arth.2019.01.038.
Shao H, Mohammed MU, Thomas N, Babazadeh S, Yang S, Shi Q, et al. Evaluating excessive burden of depression on health status and health care utilization among patients with hypertension in a nationally representative sample from the Medial Expenditure Panel Survey (MEPS 2012). J Nerv Ment Dis. 2017;205(5):397–404.
•• Thorpe K, Jain S, Joski P. Prevalence and spending associated with patients who have a behavioral health disorder and other conditions. Health Affairs. 2017;36(1):124–32. This review examines factors contributing to the high costs associated with comorbid medical and psychiatric illness and demonstrates a need for evidence-based, whole person-oriented collaborative models of care.
Wallace K, Zhao X, Misra R, Sambamoorthi U. The humanistic and economic burden associated with anxiety and depression among adults with comorbid diabetes and hypertension. Journal of diabetes research. 2018;2018:1–9.
Wu J, Davis‐Ajami ML & Kevin Lu Z. Impact of depression on health and medical care utilization and expenses in US adults with migraine: a retrospective cross sectional study. Headache: The Journal of Head and Face Pain. 2017;56(7):1147–1160. https://doi.org/10.1111/head.12871.
Gangan, N. and Y. Yang, The impact of work absences on health services utilization and costs among employed individuals with depression. 2018. 60(3): p. e139-e145.
Barrett B, Byford S, Knapp M. Evidence of cost-effective treatments for depression: a systematic review. J Affect Disord. 2005;84(1):1–13.
Gaisin I, Ivanova L. FRI0239 decreased prevalence of anxiety and depression in rheumatoid arthritis patients following b cell-targeted biologic therapy. Ann Rheum Dis. 2013;72(Suppl 3):A454-A454.
Centers for Disease Control and Prevention. Current depression among adults---United States, 2006 and 2008. MMWR. Morb Mortal Wkly Rep. 2010;59(38):1229.
Unutzer J, et al. The collaborative care model: an approach for integrating physical and mental health care in medicaid health homes, in health home: Information Resource Center. Baltimore: Centers for Medicare & Medicaid Services; 2013.
Chung H, et al. Advancing integration of behavioral health into primary care: A continuum-based framework. New York: United Hospital Fund; 2016.
Shim R, Rust G. Primary care, behavioral health, and public health: partners in reducing mental health stigma (editorial). Am J Prev Med. 2013;(May 2013).
Berwick D, Nolan T, Whittington J. The triple aim: care, health, And Cost. Health Aff. 2008;27(1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Aaron Samuel Breslow, Nathaniel M. Tran, Frederick Q. Lu, and Benjamin Lê Cook declare that they have no conflicts of interest.
Jonathan Alpert is a consultant for GLG consulting; grant funding from Otsuka Pharmaceuticals, Axome Therapeutics, and the Patient Centered Research Outcomes Institute (PCORI); payment for manuscript from Belvior Publications through Editorial Fees; and is the Chair of American Psychiatric Association Council on Research.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mood Disorders
Rights and permissions
About this article
Cite this article
Breslow, A.S., Tran, N.M., Lu, F.Q. et al. Depression Treatment Expenditures for Adults in the USA: a Systematic Review. Curr Psychiatry Rep 21, 105 (2019). https://doi.org/10.1007/s11920-019-1083-3
Published:
DOI: https://doi.org/10.1007/s11920-019-1083-3