Abstract
Purpose of Review
This paper summarizes key, recently published research examining longitudinal outcomes for preschoolers with high levels of inattention and/or hyperactivity/impulsivity.
Recent Findings
Symptom trajectories show that hyperactivity/impulsivity declines across childhood. At the group level, the course of inattention appears more variable. However, identification of subgroups of children showing stable, rising, and falling inattention over time is promising. Early ADHD-like symptoms portend risk for academic and social difficulties, as well as comorbid emotional and behavioral problems in childhood and adolescence. Several early risk factors appear to moderate these relations, including comorbid symptoms, parental psychopathology, socioeconomic disadvantage, and perhaps neuropsychological dysfunction. Furthermore, high levels of inattention and/or hyperactivity/impulsivity during the preschool period appear to compromise development of regulatory and neuropsychological functions, which in turn increases risk for negative outcomes later in childhood.
Summary
Identified risk factors are targets for novel interventions, which ideally would be delivered early to at-risk children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
ADHD is an early-emerging, chronic disorder characterized by inattention and hyperactivity/impulsivity that lead to marked impairment across multiple contexts [1]. Despite well-replicated group differences between individuals with and without the disorder, ADHD is highly heterogeneous. This has made it extremely challenging for researchers to identify the underlying pathophysiology, efficacious interventions that alter developmental trajectories, and the diversity of outcomes of ADHD, particularly at the level of the individual.
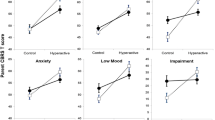
This review aims to summarize and evaluate key, recently published studies (i.e., 2014–March 2017) that examined longitudinal outcomes for preschoolers presenting with high levels of inattention and/or hyperactivity/impulsivity (see Table 1 for a summary of papers reviewed). At this early stage of development, levels of inattention and particularly hyperactivity/impulsivity are frequently high, but considerable variability in children’s trajectories is seen (see Fig. 1). Among preschool children with elevated levels of inattention and hyperactivity/impulsivity, many, but not all, go on to develop ADHD during the school-age years. Beginning in adolescence, symptom severity declines for a substantial portion of youth with ADHD. While “persisters” continue to present with high levels of symptoms and generally continue to meet diagnostic criteria for ADHD, symptom severity for many declines modestly (i.e., “partial remitters”) or even substantially (i.e., “remitters”). Notably, persisters, partial remitters, and remitters do not form discrete subgroups as depicted in the figure. These “groupings” represent artificial cuts in a dimension of symptom severity. Further, even most remitters remain symptomatic and impaired relative to their typically developing peers.
In light of it being unclear which preschoolers will and will not go on to develop an ADHD diagnosis, we included studies whose samples comprised children at high risk for ADHD (i.e., elevated levels of inattention and/or hyperactivity/impulsivity), but did not necessarily meet criteria for ADHD during the preschool period. Given our aim to shed light on longitudinal outcomes for children with early-emerging ADHD behaviors, we included studies with a minimum 2-year follow up period, thus following children into school age. This review highlights key advances in our knowledge of trajectories of ADHD-like behaviors and associated impairment from preschool, and discusses current issues in need of further study.
ADHD Symptom Trajectories
Research suggests both stability and variability of inattentive and hyperactive/impulsive behaviors in preschoolers over time. However, relatively few studies have followed preschool children over development to elucidate continuities and discontinuities in ADHD symptomatology and associated functional impairment.
Lahey and colleagues [10••] examined children’s symptom trajectories across 13 time-points from ages 4–6 to 18 years based on mother- and teacher-rated ADHD symptoms. Two cohorts of preschoolers were recruited, 125 with ADHD and 130 well-matched controls. Both inattention and hyperactivity/impulsivity declined with age, but a diagnosis by age interaction indicated a significantly greater decline in inattention, but not hyperactivity, in the group with ADHD.
Leopold et al. [11] also found that hyperactivity/impulsivity declined from preschool through ninth grade (mean (SD) age = 15.4 (0.30) years) in their community twin sample. In contrast to Lahey et al. [10••], they found inattention was relatively stable and sluggish cognitive tempo (SCT) ratings increased over the 10-year period. This study provides evidence for temporal stability of SCT and its discriminability from inattention and hyperactivity/impulsivity, perhaps suggesting that SCT should be evaluated alongside inattention and hyperactivity/impulsivity during clinical assessment.
An alternative approach to examining longitudinal course has identified subgroups of children who show different symptom trajectories. Sasser, Beekman, and Bierman [20] recruited children (N = 356) from low-income families and had teachers rate children’s inattention from kindergarten through third grade. Latent profile analysis of trajectories yielded four groups: Stable Low, Stable High, Rising, and Declining symptoms over time.
Finally, other researchers sought to identify specific symptoms holding greater predictive power for future outcomes. Harvey et al. [9] examined ADHD and ODD symptoms over 4 annual time-points in 126 children, 75 of who met criteria for ADHD both at preschool and 3 years later (mean age at fourth assessment = 80 months). Rates of hyperactive symptoms remained flat except for “fidgeting” and “blurting out answers,” which increased over time. Preschoolers initially had relatively low rates of individual inattentive symptoms, but significant increases were seen in “making careless mistakes,” and “forgetful,” with “making careless mistakes” highly indicative of ADHD because it so rarely occurred in typically developing children.
Curchack-Lichtin et al. [8] also examined individual symptoms among ADHD and typically developing preschoolers followed annually from 4 to 5 through 6–7 years. Diagnoses and symptom endorsement were determined by integrating parent, teacher, and clinician reports. Overall, hyperactive/impulsive symptoms were superior to inattentive symptoms in discriminating those with and without ADHD at 4–5 years. This reversed by 6–7 years, at which time inattention symptoms were increasingly endorsed and gained moderate discriminant value. Out of all symptoms, only the Hyperactive/Impulsive symptom “Fidgets” was of high discriminant value. The authors suggested that a reduced threshold of inattention symptoms before age 6, as was adopted for both symptom domains by DSM-5 [1] for adults, may prevent the shift from hyperactive/impulsive to combined presentation that often occurs during the transition from preschool to school-age.
Overall, hyperactivity/impulsivity declines over time from the high levels seen during preschool. With the exception of “fidgeting,” hyperactive/impulsive symptoms are less able to differentiate children with and without an ADHD diagnosis when children move from preschool to school-age. More variable findings have been observed regarding the course of inattention over time. Some show that, on average, inattention declines, while others show stable or rising inattention. Promisingly, Sasser et al. [20] identified subgroups of children who appear to show different symptom trajectories. As children get older, the discriminative ability of inattentive symptoms to distinguish between those with and without a diagnosis improves.
Mediators and Moderators of ADHD Symptom Trajectories
Beyond elucidating trajectories of inattention and hyperactivity/impulsivity across childhood, it is critical to determine risk factors or mechanisms by which they unfold. Recognizing these moderating and mediating variables can help with identification of at-risk children and provide clues for treatment development.
Psychosocial Moderators/Mediators
Recent work affirms that psychosocial factors both within and outside the home influence ADHD trajectories. Sasser et al. [20] found that among low-income American families, attending a school with higher levels of student achievement and living in two-parent households were associated with declining inattention between preschool and third grade. Conversely, living in a single-parent household was associated with stable high or rising inattention.
Similarly, Russell et al. [19] found that early adversity was associated with higher risk for ADHD. Children whose family experienced socioeconomic disadvantage (difficulty affording basic amenities) when they were 33 months old were more than twice as likely to be diagnosed with ADHD at age 7. This relation was mediated by greater family adversity (i.e., lack of partner affection, partner cruelty, maternal psychopathology, substance abuse or crime) at 2–4 years and less parental involvement at 6 years. These findings [19, 20] raise critical questions about how society addresses poverty and structural inequality, and how exposure to early adversity has ripple effects on children and their families.
In addition to socioeconomic indicators, parental characteristics can influence the course of ADHD symptoms. Breaux et al. [3] found that maternal ADHD symptoms predicted their child’s ADHD symptoms at age 6 after controlling for children’s symptoms at age 3 and other potential confounders. Although paternal ADHD symptoms did not predict worsening ADHD over early childhood, paternal psychopathology and extended family history of ADHD predicted more severe ADHD and ODD at age 6.
The above studies highlight potential psychosocial targets for intervention. In particular, newer research is examining whether comprehensive approaches that address children’s symptoms as well as known risk factors (such as parental ADHD) improves treatment outcomes for children [26]. These studies are essential to address the complex interactions among family and social factors that place children with ADHD at risk for poorer outcomes.
Temperament
Beyond external influences, child characteristics can influence the course of ADHD. Recent papers have focused on the interplay between children’s “bottom up” reactive and “top down” regulatory systems. Rabinovitz et al. [16] showed that preschoolers’ Anger/Frustration increased risk for ADHD at age 7, in part by compromising development of executive functioning. Sjowall and colleagues’ [23] showed the importance of also evaluating children’s capacity to regulate positive emotions. They found that dysregulated happiness, measured at 6.5 years-old was associated with greater inattention (but not hyperactivity/impulsivity) at 18 years, even after controlling for preschool symptoms, SES, and gender.
Neuropsychological Functioning
Over the past 30 years, neuropsychological dysfunction has been posited to be a core etiological factor for ADHD [27,28,29]. Several recent papers have examined whether early neuropsychological functioning is associated with later diagnosis/severity of ADHD. Lahey et al. [10••] found that 4–6 year olds’ scores on the Short Form of the Stanford-Binet Intelligence Scale were not predictive of future ADHD symptoms. Similarly, Rajendran et al. [18] examined whether neurocognitive groupings of hyperactive/inattentive preschool children were predictive of ADHD diagnosis at six annual follow-up evaluations. Latent profile analysis identified two classes of hyperactive/inattentive preschoolers: selective impairment in attention/executive functioning and more severe, broad-based neuropsychological dysfunction. Both groups were at greater risk of ADHD diagnosis relative to typically developing children at each follow-up, but there were no differences between the selective and broad deficit groups. Furthermore, when examined separately, none of the nine neuropsychological measures were predictive of later ADHD diagnosis. Thus, although neuropsychological deficits are associated with ADHD, they may not be good indicators of which “at-risk” children go on to develop a diagnosis.
Some theories of ADHD also highlight a role for motivational processes in ADHD etiology [30, 31]. Breaux, et al. [4] evaluated “hot” (e.g., delay aversion) and “cold” (e.g. response inhibition, working memory) neurocognitive functioning in an at-risk sample of 3- and 4-year-olds, and ADHD symptoms at age 6. They found little support for the notion that “hot” and “cool” measures differentially predict symptoms, but did report some significant associations between early neuropsychological functioning and later ADHD after controlling for early behavior problems. However, the measures had only poor to fair sensitivity, specificity, and positive and negative predictive power with regard to later ADHD, suggesting limited clinical utility.
Sasser et al. [20] had pre-kindergarteners complete three tasks that loaded on to a single executive functioning factor. Children who had initially low, but rising inattention trajectory from preschool to third grade were found to have had lower executive functioning skills and higher rates of oppositional-aggressive behavior in preschool relative to children who remained low on inattention.
Thus, findings are not fully consistent as to whether early neuropsychological measures are predictive of later ADHD. Some studies report significant group effects, which might have heuristic value, but on an individual level there is relatively little evidence of the prognostic value of early testing.
Brain Structure
The basal ganglia have been consistently implicated in the pathogenesis of ADHD. In the only study of its kind, Shaw et al. [22••] combined longitudinal and cross-sectional magnetic resonance imaging data to map basal ganglia developmental trajectories from age 4 through 19 years in 270 youth with ADHD and 270 well-matched controls. Two key findings emerged. First, the ventral striatum, a region closely associated with reward processing, showed progressive surface contraction in youth with ADHD but not in controls. This might contribute to motivational deficits in ADHD and the vulnerability to substance misuse in adolescents/adults with ADHD. Second, ADHD was linked to fixed, non-progressive surface area reductions in striatal regions supporting motor planning and executive functions, hallmark features of the disorder. These findings may provide clues about potential neural mediators of distinct ADHD phenotypes.
Non-pharmacological Interventions
Recent research is beginning to identify preschool factors associated with ADHD trajectories. A key follow-up question is whether we can design appropriate interventions for young children that can alter symptom trajectories. Non-pharmacological treatment options tend to be recommended as first-line treatment for preschoolers [32], given a somewhat poorer treatment response and greater incidence of medication side effects for preschoolers compared to older children [33]. However, we still have a long way to go in our design and implementation of efficacious treatments for ADHD [34].
In a randomized controlled trial (RCT), Abikoff et al. [2] compared three groups of preschoolers: (1) those whose parents participated in the New Forest Parenting Package (NFPP), which was designed specifically for ADHD; (2) those whose parents went through the “Helping the Noncompliant Child” (HNC) program, a more generic intervention for children with disruptive behavior disorders; and (3) a wait list control group. Compared to the wait list group, NFPP and HNC showed improvement of parent-rated symptoms of ADHD and oppositionality, but reports were not corroborated by either direct observations or teacher reports, consistent with findings showing that when the most proximal rater is used in the analyses, treatment effect sizes are large, but when more distal raters are used, significant treatment effects are severely diminished or vanish [34]. Also notable, the specific ADHD intervention (NFPP) was not superior to the more generic behavioral intervention [2].
Although blinded RCTs are the gold standard for evaluating intervention efficacy, many children receive services at school, where treatment effectiveness is rarely evaluated. Mlodnicka and colleagues [12] conducted a naturalistic study of the impact of speech therapy (ST) and occupational/physical therapy (OT/PT) delivered in schools to hyperactive/inattentive preschoolers. Preschoolers were assessed at baseline and two years later for behavior, language and motor development, and social skills. ST and OT/PT seemed to have no effect on hyperactive/inattentive children’s language or motor functioning, respectively. However, there was significant improvement in social skills in those children who received ST. Obviously, there are limitations to naturalistic follow-up studies. However, it raises several questions: when children receive services in school, what is being delivered? What outcomes should be measured? Importantly, without randomization to treatment, we cannot accurately gauge how children would function without service delivery. These are areas for further study.
Impairment
Understanding symptom trajectories is clearly important, but individuals with ADHD show functional impairment across multiple domains, even when symptoms remit [35]. Thus, examining impairment, as separate from symptoms, is not only important, but of great clinical significance.
Lahey and colleagues [10••] assessed global impairment from ages 4–18 years using parent and parent-interviewer ratings on the Children’s Global Assessment Scale, which reflects the lowest level of overall functioning in the past 6 months. Across the full sample, both informants rated functioning as significantly improving with age. However, across time, the ADHD group had significantly lower ratings by parents (16.87 points) and interviewers (17.46 points). Among children with ADHD in preschool, greater impairment from 7 to 18 years was associated with female sex, and more inattention, anxiety, oppositionality, and conduct symptoms. Consistent with findings showing that importance of psychosocial factors [19], higher family income predicted better functioning.
It is not surprising that, as a group, individuals with ADHD have lower global functioning than their non-ADHD peers. Identification of specific domains of impairment may be more informative and are discussed below.
Comorbidity
ADHD is associated with increased risk for comorbid psychopathology. Several studies have assessed links between early ADHD symptoms and risk for later comorbidity, and potential moderators of these relations.
Breaux, Harvey, and Lugo-Candelas [5] examined relations between parental psychopathology and internalizing, externalizing, and social problems in a sample of 3-year-olds (n = 132) who were rated as having high aggression and/or hyperactivity by their parents. Parental psychopathology was assessed dimensionally at baseline and children were re-evaluated at ages 4, 5, and 6 years. Mothers with greater psychopathology reported that their children had more externalizing and internalizing problems and weaker social skills. Fathers experiencing more psychopathology did not rate their children as having more difficulties but these children had higher maternal ratings of internalizing problems. Thus, parental psychopathology may moderate the emergence of comorbid difficulties in children.
Harvey and colleagues [36] examined development of comorbidity between ADHD and ODD from ages 3 to 6 years. ODD symptoms did not predict future hyperactivity/impulsivity or inattention when controlling for early ADHD. Consistent with a “developmental precursor” model, however, at every time point from ages 3 through 6, both inattention and hyperactivity/impulsivity predicted argumentativeness/defiance 1-year later; neither ADHD domain was associated with subsequent anger/irritability. In support of the correlated risk factors model, family history of hyperactivity/impulsivity and inattention significantly predicted age 3 hyperactivity/impulsivity and inattention, respectively, while family histories of ODD and CD were significantly associated with children’s anger/irritability at age 3.
Lahey et al. [10] investigated predictors of youth-reported depression and anxiety at 9–18 years among children who met criteria for ADHD in early childhood. Neither early inattention nor hyperactivity/impulsivity severity predicted anxiety or depression. Younger age, higher parent-rated anxiety during preschool, lower childhood IQ, and female sex predicted higher self-reported anxiety in late childhood/adolescence, while younger age and lower childhood IQ predicted depression. Similar risk factors predicted parent- and teacher-rated anxiety and depression from 7 to 18 years.
Social Problems
Considerable research shows that ADHD is associated with poorer social outcomes [37, 38]. Stenseng et al. [24] provided evidence for reciprocity between ADHD and peer rejection in early childhood. Teachers completed measures of peer rejection when children were aged 4, 6, and 8 years, and parents were interviewed about children’s ADHD symptoms. A cross-lagged model showed reciprocal relations between peer rejection and ADHD symptoms between ages 4 and 6 years, but not between 6 and 8.
Two studies examined the link between ADHD and a particularly severe social problem: bullying. Verlinden and colleagues [25] investigated the risk that early ADHD has for later perpetration of or victimization from bullying at age 7. After adjusting for ODD, age 3 ADHD (not ages 1.5 or 5) increased risk for teacher-reported bully-victim status at age 7. When risk was evaluated relative to symptom trajectory, children with high increasing ADHD symptoms were 2.18 times more likely to be a bully at age 7, and 2.86 times more likely to be a bully-victim. Those with high increasing ADHD and ODD symptoms (n = 51) had the greatest risk of being a bully or bully-victim.
Rajendran and colleagues [17] asked whether more optimal parenting was related to lower rates of bullying over time among children diagnosed with behavioral problems. Parenting was assessed via direct observations at 4–5 years of age and teachers evaluated bullying behaviors over the next 4 years. Children with comorbid ADHD/ODD were more likely to bully than children with ADHD alone or with neither diagnosis. Although bullying decreased over time for all, parent support for child autonomy was associated with a greater decline in bullying, especially among children who had both ADHD/ODD. Thus, ADHD symptoms during preschool pose a risk for both later bullying and being a bully-victim. When ADHD is coupled with ODD, risk may be amplified.
Academic Achievement
A robust literature shows a negative association between ADHD and academic outcomes [39, 40]. Most recent studies support earlier findings that inattention is more strongly related to achievement than hyperactivity/impulsivity [14, 15, 21]. Schmideler and Schneider [21] showed this irrespective of whether predicting reading or math, and even after controlling for pre-academic skills (e.g., phonological awareness, quantity-number competencies).
O’Neill et al. [14] and Plourde et al. [15] investigated potential mechanisms accounting for the association between ADHD and reading. O’Neill and colleagues [14] found that inattention at age 4 compromised children’s language development by age 5, which in turn was associated with poorer reading achievement, as measured using objective tests and teacher ratings, at age 8 years. Using a population-based twin sample, Plourde et al. [15] examined whether the association between ADHD and later reading comprehension occurred through shared genetic etiology. Regression analyses showed that inattention, measured during kindergarten and first grade, as well as nonverbal abilities, significantly predicted decoding and comprehension at age 8 years. In fact, inattention remained a predictor of reading comprehension even after decoding was included in the model, and the relation was largely due to shared genetic influences.
Claessens et al. [7] assessed the timing and direction of the association between changes in academic achievement and problems with attention and disruptive behavior to isolate meaningful intervention points. Children were assessed in the fall and spring of kindergarten, and the spring of the first, third, and fifth grades. Worsening attention problems were associated with decreased math and reading gains between kindergarten and first grade and between first and third grade; for reading only, worsening attention from first to third grade was associated with lower reading gains between third and fifth grade. In contrast, changes in disruptive behavior were not associated with either math or reading achievement. Less consistent findings were observed when looking at whether changes in academic achievement were associated with later changes in attention problems. In general, greater improvement in math achievement was associated with diminished growth in attention problems.
Sasser et al. [20] investigated academic outcomes for four inattention trajectory classes: Stable Low, Rising, Declining, and Stable High inattention. At grade 3, those with Rising symptoms had inattention levels that were the same as those with Declining symptoms. However, while those with Rising inattention had largely similar academic outcomes at grade 5 to children with Stable Low symptoms, those in the Declining inattention group performed more poorly on all academic measures than the Stable Low group.
Driving and Criminal Offending
Compared to non-ADHD peers, individuals with ADHD have poorer driving outcomes that cannot be fully accounted for by comorbid ODD/CD [41]. They are also at greater risk of arrest, conviction, and incarceration, although these latter relations appear to be mediated by antisocial personality disorder and substance use [42]. Consistent with these findings, Lahey and colleagues [10••] showed that when compared to the controls, adolescents (ages 15–18 years) who had received a diagnosis of ADHD as preschoolers were more likely to engage in risky driving behavior and were 4.31 times as likely to have been arrested. The presence of conduct symptoms at baseline was a risk factor for both arrest and driving without a license.
Clinical Applications and Methodological Considerations
The papers reviewed assessed the psychosocial, behavioral, and neuropsychological predictors of outcomes across several domains and show that risk factors present early in childhood exert a long-lasting influence on children’s functioning. Though certainly not a new recommendation, it bears repeating that prompt identification of youngsters at risk for ADHD and access to early intervention is essential [43]. This call to action is particularly meaningful given Sasser et al.’s work, reviewed above, showing that children with Declining inattention showed poorer academic outcomes than children with Stable Low symptoms, while children with Rising inattention and Stable Low inattention had largely similar academic outcomes [20]. Such findings may reflect a developmental cascade [44], where young children with low levels of inattention and/or hyperactivity/impulsivity develop greater regulatory skills and in-turn greater coping resources should symptom severity increase later in childhood. In contrast, high symptom levels early in development may restrict or reduce growth in critical areas of functioning, setting-up children for greater impairment, even if symptoms eventually remit.
Unfortunately, the sensitivity required to identify which child will attain what particular outcome continues to elude us [10••]. O’Neill et al. [13] found that at least two informants were needed from different settings to accurately predict which preschoolers would go on to meet criteria for ADHD during school-age; obtaining parent report alone is not sufficient. Thorough assessment, especially in the early years, is essential and although likely more expensive, may help to better allocate resources.
Ultimately, the difficult question of where to allocate limited resources is one faced by health, education, and justice departments, and families. The financial burden of ADHD is enormous [45] and appears to be particularly so for early-emerging ADHD. For instance, Chorozoglou et al. [6] followed a large sample of hyperactive preschoolers through ages 14 and then 24 years, and found them to have significantly greater mental health, education, criminal justice, and family costs than controls. Each unit increase in hyperactivity added a cost of £49.60 to average yearly costs, primarily via later mental health problems. Heckman [46] reported greater discounting of each dollar spent as individuals get older and, therefore, return on investment is greater when spent on young children, emphasizing (again) the importance of early intervention.
Beyond the application of recent research to clinical practice and policy, there are methodological issues to consider. First, most researchers test linear models, yet development generally progresses in a non-linear manner (e.g., brain growth, executive control, negative affect). Lahey et al. [10••] tested quadratic models and showed steeper declines in symptoms at older ages. More work of this nature is needed.
Further, for studies using neuropsychological measures, careful consideration needs to be given to what tests measure, particularly in younger age groups. Poor psychometric properties of neuropsychological measures administered to preschoolers [4] limits valid conclusions. Additionally, particularly for young children, the extent to which poor performance reflects true underlying deficits versus behavioral problems and non-compliance is difficult to disentangle.
Finally, in very young children, differences in assessment age affect conclusions drawn because of the developmental trajectory of neural circuitry that underlies behavior and neuropsychological functioning. Since the neural circuits underlying neuropsychological functions are thought to be fine-tuned with experience, it is possible that the same ability/test measured at different time points may have differential predictions due to developmental maturation.
Conclusion
ADHD is a chronic, impairing condition that commonly emerges at an early age. Longitudinal data sets spanning different developmental periods have enabled us to model long-term course of the disorder and associated impairment, and to identify risk factors for these paths.
For clinicians, despite the uptick in longitudinal studies over recent years, our measures and models are not sensitive enough to be able to tell parents what the outcome will be for their child, and ultimately this is what they want to know. So, as a field, we still have work to do. However, we are able to tell parents that many children will continue to show symptoms and/or impairment associated with early-emerging inattention and/or hyperactivity over time, although they may not necessarily meet criteria for an ADHD diagnosis. Overt hyperactivity, in particular, will likely lessen in severity, but the path of inattention symptoms is less clear. Early symptoms increase risk for poorer outcomes in multiple domains including social, emotional, and behavioral functioning, with risk amplified if early oppositional or conduct symptoms are present. Inattention specifically increases risk for poorer academic outcomes, especially in the domain of reading. Certain environmental factors increase the risk of later ADHD and possible comorbid diagnoses for youngsters. These include parental psychopathology and adverse environments, which may act directly or indirectly through their effects on parenting practices. Taken together, clinicians should be on the look out for youngsters with high levels of inattention and/or hyperactivity/impulsivity and routinely monitor their progress across the preschool period. Interventions likely need to be holistic, targeting child-, family-, and school-level factors, although further research is needed to lend empirical support to this assumption. Finally, with respect to assessment: (1) obtaining ratings from multiple informants is critical, and (2) neuropsychological assessment at such a young age can aid in distinguishing those with and without elevated inattention/hyperactivity, but do not appear to have great utility for distinguishing which children will follow what trajectory.
For researchers, advanced statistical modeling will enable us to analyze non-linear and heterogeneous trajectories, which currently, are not often analyzed. In addition, careful thought about which covariates to measure at which time points in longitudinal studies may help us to better understand the transactional nature of developmental psychopathology over time, which in turn, will help inform intervention.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington DC: American Psychiatric Publishing; 2013.
Abikoff HB, Thompson M, Laver-Bradbury C, Long N, Forehand RL, Miller Brotman L, et al. Parent training for preschool ADHD: a randomized controlled trial of specialized and generic programs. J Child Psychol Psychiatry. 2015;56:618–31. https://doi.org/10.1111/jcpp.12346.
Breaux RP, Brown HR, Harvey EA. Mediators and moderators of the relation between parental ADHD symptomatology and the early development of child ADHD and ODD symptoms. J Abnorm Child Psych. 2017;45:443–56. https://doi.org/10.1007/s10802-016-0213-1.
Breaux RP, Griffith SF, Harvey EA. Preschool neuropsychological measures as predictors of later attention deficit hyperactivity disorder. J Abnorm Child Psych. 2016;44:1455–71. https://doi.org/10.1007/s10802-016-0140-1.
Breaux RP, Harvey EA, Lugo-Candelas CI. The role of parent psychopathology in the development of preschool children with behavior problems. J Clin Child Adolesc Psychol. 2014;43(5):777–90. https://doi.org/10.1080/15374416.2013.836451.
Chorozoglou M, Smith E, Koerting J, Thompson MJ, Sayal K, Sonuga-Barke EJ. Preschool hyperactivity is associated with long-term economic burden: evidence from a longitudinal health economic analysis of costs incurred across childhood, adolescence and young adulthood. J Child Psychol Psychiatry. 2015;56:966–75. https://doi.org/10.1111/jcpp.12437.
Claessens A, Dowsett C. Growth and change in attention problems, disruptive behavior, and achievement from kindergarten to fifth grade. Psychol Sci. 2014;25(12):2241–51. https://doi.org/10.1177/0956797614554265.
Curchack-Lichtin JT, Chacko A, Halperin JM. Changes in ADHD symptom endorsement: preschool to school age. J Abnorm Child Psych. 2014;42:993–1004. https://doi.org/10.1007/s10802-013-9834-9.
Harvey EA, Lugo-Candelas CI, Breaux RP. Longitudinal changes in individual symptoms across the preschool years in children with ADHD. J Clin Child Adolesc Psychol. 2015;44:580–94. https://doi.org/10.1080/15374416.2014.886253.
•• Lahey BB, Lee SS, Sibley MH, Applegate B, Molina BS, Pelham WE. Predictors of adolescent outcomes among 4–6-year-old children with attention-deficit/hyperactivity disorder. J Abnorm Psychol. 2016;125:168. https://doi.org/10.1037/abn0000086. This longitudinal study across 13 points of time from age of 4-6 years to 18 years found that both inattention and hyperactivity declined with age and that children with ADHD exhibited greater numbers of symptoms of every dimension of psychopathology (i.e., inattention, hyperactivity-impulsivity, ODD, CD, anxiety, and depression) reported by parents and teachers or by the youth themselves
Leopold DR, Christopher ME, Burns GL, Becker SP, Olson RK, Willcutt EG. Attention-deficit/hyperactivity disorder and sluggish cognitive tempo throughout childhood: temporal invariance and stability from preschool through ninth grade. J Child Psychol Psych. 2016;57:1066–74. https://doi.org/10.1111/jcpp.12505.
Mlodnicka AE, O’Neill S, Marks DJ, Rajendran K, Bedard AC, Schneiderman RL, et al. Impact of occupational, physical, and speech and language therapy in preschoolers with hyperactive/inattentive symptoms: a naturalistic 2-year follow-up study. Children's Health Care. 2016;45:67–83. https://doi.org/10.1080/02739615.2014.979918.
O’Neill S, Schneiderman RL, Rajendran K, Marks DJ, Halperin JM. Reliable ratings or reading tea leaves: can parent, teacher, and clinician behavioral ratings of preschoolers predict ADHD at age six? J Abnorm Child Psychol. 2014;42(4):623–34. https://doi.org/10.1007/s10802-013-9802-4.
O’Neill S, Thornton V, Marks DJ, Rajendran K, Halperin JM. Early language mediates the relations between preschool inattention and school-age reading achievement. Neuropsychology. 2016;30(4):398–404. https://doi.org/10.1037/neu0000247.
Plourde V, Boivin M, Forget-Dubois N, Brendgen M, Vitaro D, Marino C, et al. Phenotypic and genetic associations between reading comprehension, decoding skills, and ADHD dimensions: evidence from two population-based studies. J Child Psychol Psychiatry. 2015;56(10):1074–82. https://doi.org/10.1111/jcpp.12394.
Rabinovitz BB, O’Neill S, Rajendran K, Halperin JM. Temperament, executive control, and attention-deficit/hyperactivity disorder across early development. J Abnorm Psychol. 2016;125(2):196. https://doi.org/10.1037/abn0000093.
Rajendran K, Kruszewski E, Halperin JM. Parenting style influences bullying: a longitudinal study comparing children with and without behavioral problems. J Child Psychol Psychiatry. 2016;57:188–95. https://doi.org/10.1111/jcpp.12433.
Rajendran K, O’Neill S, Marks DJ, Halperin JM. Latent profile analysis of neuropsychological measures to determine preschoolers’ risk for ADHD. J Child Psychol Psych. 2015;56:958–65. https://doi.org/10.1111/jcpp.12434.
Russell AE, Ford T, Russell G. Socioeconomic associations with ADHD: findings from a mediation analysis. PLoS One. 2015;10(6):e0128248. https://doi.org/10.1371/journal.pone.0128248.
Sasser TR, Beekman CR, Bierman KL. Preschool executive functions, single-parent status, and school quality predict diverging trajectories of classroom inattention in elementary school. Dev Psychopathol. 2015;27(3):681–93. https://doi.org/10.1017/S0954579414000947.
Schmiedeler S, Schneider W. Attention-deficit hyperactivity disorder (ADHD) in the early years: diagnostic issues and educational relevance. Clin Child Psychol Psychiatry. 2014;19(3):460–75. https://doi.org/10.1177/1359104513489979.
•• Shaw P, De Rossi P, Watson B, Wharton A, Greenstein D, Raznahan A, et al. Mapping the development of the basal ganglia in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2014;53(7):780–9. https://doi.org/10.1016/j.jaac.2014.05.003. This longitudinal study using advanced MRI techniques in 270 youth with ADHD and 270 sex-matched controls showed multiple group differences in the basal ganglia in individuals with ADHD, some that are fixed but others that are progressive over development
Sjöwall D, Bohlin G, Rydell AM, Thorell LB. Neuropsychological deficits in preschool as predictors of ADHD symptoms and academic achievement in late adolescence. Child Neuropsychology. 2017;23(1):111–28. https://doi.org/10.1080/09297049.2015.1063595.
Stenseng F, Belsky J, Skalicka V, Wichstrøm L. Peer rejection and attention deficit hyperactivity disorder symptoms: reciprocal relations through ages 4, 6, and 8. Child Dev. 2016;87:365–73. https://doi.org/10.1111/cdev.12471.
Verlinden M, Jansen PW, Veenstra R, Jaddoe VW, Hofman A, Verhulst FC, et al. Preschool attention-deficit/hyperactivity and oppositional defiant problems as antecedents of school bullying. J Am Acad Child Adolesc Psychiatry. 2015;54:571–9. https://doi.org/10.1016/j.jaac.2015.05.002.
Wang CH, Mazursky-Horowitz H, Chronis-Tuscano A. Delivering evidence-based treatments for child attention-deficit/hyperactivity disorder (ADHD) in the context of parental ADHD. Curr Psychiatry Rep. 2014;16(10):474. https://doi.org/10.1007/s11920-014-0474-8.
Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997 Jan;121(1):65–94.
Rapport MD, Alderson RM, Kofler MJ, Sarver DE, Bolden J, Sims V. Working memory deficits in boys with attention-deficit/hyperactivity disorder (ADHD): the contribution of central executive and subsystem processes. J Abnorm Child Psychol. 2008 Aug;36(6):825–37. https://doi.org/10.1007/s10802-008-9215-y.
Sergeant J. The cognitive-energetic model: an empirical approach to attention-deficit hyperactivity disorder. Neurosci Biobehav Rev. 2000;24(1):7–12.
Solanto MV, Abikoff H, Sonuga-Barke EJS, Schachar R, Logan GD, Wigal T, et al. The ecological validity of delay aversion and response inhibition as measures of impulsivity in AD/HD: a supplement to the NIMH multimodal treatment study of AD/HD. J Abnorm Child Psychol. 2001;29(3):215–28.
Sonuga-Barke EJS, Dalen L, Remington B. Do executive deficits and delay aversion make independent contributions to preschool attention-deficit/hyperactivity disorder symptoms? J Am Acad Child Adolesc Psychiatry. 2003;42(11):1335–42.
Fiks AG, Ross ME, Mayne SL, Song L, Liu W, Steffes J, et al. Preschool ADHD diagnosis and stimulant use before and after the 2011 AAP practice guideline. Pediatrics. 2016; 138(6).
Greenhill L, Kollins S, Abikoff H, McCracken J, Riddle M, Swanson J, et al. Efficacy and safety of immediate-release methylphenidate treatment for preschoolers with ADHD. J Am Acad Child Adolesc Psychiatry. 2006 Nov;45(11):1284–93.
Sonuga-Barke EJ, Brandeis D, Cortese S, Daley D, Ferrin M, Holtmann M, et al. Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. Am J Psychiatry. 2013 Mar;170(3):275–89. https://doi.org/10.1176/appi.ajp.2012.12070991.
Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry. 2000;157:816–8.
Harvey EA, Breaux RP, Lugo-Candelas CI. Early development of comorbidity between symptoms of attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD). J Abnorm Psychol. 2016;125:154. https://doi.org/10.1037/abn0000090.
Greene RW, Biederman J, Faraone SV, Monuteaux MC, Mick E, Dupre EP, et al. Social impairment in girls with ADHD: patterns, gender comparisons, and correlates. J Am Acad Child Adolesc Psychiatry. 2001;40(6):704–10.
Staikova E, Gomes H, Tartter V, McCabe A, Halperin JM. Pragmatic deficits and social impairment in children with ADHD. J Child Psychol Psychiatry. 2013;54(12):1275–83. https://doi.org/10.1111/jcpp.12082.
Hart SA, Petrill SA, Willcutt E, Thompson LA, Schatschneider C, Deater-Deckard K, et al. Exploring how symptoms of attention-deficit/hyperactivity disorder are related to reading and mathematics performance: general genes, general environments. Psychol Sci. 2010;21(11):1708–15. https://doi.org/10.1177/0956797610386617.
Langberg JM, Dvorsky MR, Molitor SJ, Bourchtein E, Eddy LD, Smith Z, et al. Longitudinal evaluation of the importance of homework assignment completion for the academic performance of middle school students with ADHD. J Sch Psychol. 2016;55:27–38. https://doi.org/10.1016/j.jsp.2015.12.004.
Barkley RA. Driving impairments in teens and adults with attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2004;27(2):233–60.
Mannuzza S, Klein RG, Moulton JL. Lifetime criminality among boys with attention deficit hyperactivity disorder: a prospective follow-up study into adulthood using official arrest records. Psychiatry Res. 2008;160(3):237–46. https://doi.org/10.1016/j.psychres.2007.11.003.
Sonuga-Barke EJ, Halperin JM. Developmental phenotypes and causal pathways in attention deficit/hyperactivity disorder: potential targets for early intervention? J Child Psychol Psychiatry. 2010;51(4):368–89. https://doi.org/10.1111/j.1469-7610.2009.02195.x.
Masten AS, Cicchetti D. Developmental cascades. Dev Psychopathol. 2010;22(3):491–5. https://doi.org/10.1017/S0954579410000222.
Marks DJ, Mlodnicka A, Bernstein M, Chacko A, Rose S, Halperin JM. Profiles of service utilization and the resultant economic impact in preschoolers with attention deficit/hyperactivity disorder. J Pediatr Psychol. 2009;34(6):681–9. https://doi.org/10.1093/jpepsy/jsn112.
Heckman JJ. Schools, skills, and synapses. Econ Inq. 2008;46(3):289–324. https://doi.org/10.1111/j.1465-7295.2008.00163.x.
Acknowledgments
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (S.O., grant number SC2 HD086868) of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sarah O’Neill, Khushmand Rajendran, Shelagh M. Mahbubani, and Jeffrey M. Halperin declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
This article is part of the Topical Collection on Attention-Deficit Disorder
Rights and permissions
About this article
Cite this article
O’Neill, S., Rajendran, K., Mahbubani, S.M. et al. Preschool Predictors of ADHD Symptoms and Impairment During Childhood and Adolescence. Curr Psychiatry Rep 19, 95 (2017). https://doi.org/10.1007/s11920-017-0853-z
Published:
DOI: https://doi.org/10.1007/s11920-017-0853-z