Abstract
Purpose of Review
Imaging research has sought to uncover brain structure, function, and metabolism in women with postpartum depression (PPD) as little is known about its underlying pathophysiology. This review discusses the imaging modalities used to date to evaluate postpartum depression and highlights recent findings.
Recent Findings
Altered functional connectivity and activity changes in brain areas implicated in executive functioning and emotion and reward processing have been identified in PPD. Metabolism changes involving monoamine oxidase A, gamma-aminobutyric acid, glutamate, serotonin, and dopamine have additionally been reported. To date, no studies have evaluated gray matter morphometry, voxel-based morphometry, surface area, cortical thickness, or white matter tract integrity in PPD.
Summary
Recent imaging studies report changes in functional connectivity and metabolism in women with PPD vs. healthy comparison women. Future research is needed to extend these findings as they have important implications for the prevention and treatment of postpartum mood disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The peripartum period is a complex period in a woman’s life that is marked by normal changes in psychological functioning and physiology. It is also a period of heightened vulnerability, with lifetime prevalence of psychiatric disorders in women reaching its zenith in the first 3 postpartum months [1,2,3]. Up to 85% of primiparous mothers experience postpartum mood symptoms such as mood swings, anxiety, and poor concentration [4]. Approximately 10–20% of pregnant and postpartum women worldwide meet the criteria for a peripartum mental health disorder [5, 6], with depression and anxiety the most common [7].
Peripartum mental health disorders are a major public health concern with significant consequences for mothers, their children, and their families [8]. Mothers with peripartum mental disorders are more stigmatized, less likely to participate in the healthcare system [9, 10], at increased risk of complications such as preeclampsia and operative delivery [11], and have higher rates of psychiatric hospitalization, self-harm, and suicide [12]. Infants with mothers affected by perinatal mental disorders are more likely to be born prematurely with intrauterine growth restriction and low birth weight [13]. In developing countries, infants have lower immunization rates [14, 15] and higher rates of malnutrition [16], infectious diseases [16, 17], and hospitalization [15]. Peripartum depression has a negative impact on the cognitive, emotional, and behavioral development of children [18,19,20,21].
While the devastating sequelae of peripartum mental health disorders have been well studied, diagnosis and pathophysiology of even the most common disorder, depression, is not well defined. The Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) defines major depression with peripartum onset as occurring during pregnancy or within 4 weeks of delivery [22]. Other organizations such as the World Health Organization (WHO) define the onset within 12 months postpartum [23]. While there are similarities between the diagnostic criteria of non-peripartum and peripartum depressive disorders, peripartum depression is a heterogeneous disorder with several distinct phenotypes [24] that warrant further study.
The peripartum period is associated with profound changes in physiology. Across the cardiovascular, digestive, integumentary, and immune systems for example, many of these normal changes in physiology are driven by changes in the endocrine system. Increasing research into peripartum endocrine [25, 26, 27•, 28,29,30,31,32,33] and immune function [34, 35] and chronobiology [36, 37] in women with peripartum depression is increasing; however, studies examining the effects of pregnancy on the central nervous system (CNS), particularly the human brain, are limited. Understanding the normal peripartum-related physiological changes in brain structure, function, and metabolism, using non-invasive brain imaging techniques, will allow us to understand how peripartum mood disorders develop. The primary aim of this review is to provide a concise background for imaging modalities used in peripartum depression research and second, to review and synthesize recent findings.
Methods
Papers were searched on MEDLINE, PsychINFO, Web of Science, Scopus, Embase, and PubMed with the following key words: (“diffusion imaging” or “brain mapping” or “brain morphology” or “connectome” or “dti” or “fmri” or “functional mri” or “functional neuroimaging” or “diffusion imaging” or “diffusion tensor imaging” or “functional neuroimaging” or “magnetic resonance imaging (MRI)” or “magnetic resonance spectroscopy (MRS)” or “mri” or “neuroimaging” or “PET” or “structural mri” or “tomography” or “volumetric based morphometry” or “volume positron emission” or “volume based morphometry”) AND (“pregnancy” or “antepartum” or “perinatal” or “motherhood” or “postpartum” or “maternal” or “antenatal” or “postnatal” or “prepartum” or “peripartum” or “mothers”) AND (“depression” or “depressive”). This review is limited to papers published in English on subjects up to 6 months postpartum, with a focus on papers published in the last 5 years. In this review, studies of healthy non-depressed mothers were included, whereas preclinical research was excluded. Additional articles were identified by reviewing bibliographies of review articles identified within the literature search.
Structural MRI: Volumetric and Diffusion Tensor Imaging Investigations
Structural MRI methods are used to examine gray matter (GM) and white matter (WM) morphometry. Common methods for examining GM volume include manual measurement of specific brain regions or regions of interest (ROI), voxel-based morphometry (VBM) which is a hypothesis-free approach to examine GM differences among groups across the entire brain [38], and surface-based measures which measure the thickness of the GM of the cortical sheet as a way of estimating the number of neuronal cell bodies in a given area. Diffusion tensor imaging (DTI) is an MRI-based method that determines the location, orientation, and anisotropy of the brain’s WM tracts [38].
Recent research suggests that normal pregnancy is associated with structural changes in the maternal brain. Using VBM, Kim et al. reported GM volume increases across the postpartum period in the superior, middle, and inferior prefrontal cortex, precentral and postcentral gyrus, superior and inferior parietal lobe, and the insula, as well as the thalamus [39]. Measured volume changes were localized in areas implicated to play a role in maternal behavior and maternal-infant interactions [40]. A more recent study, which measured GM volume pre-pregnancy, in the early postpartum period and at 2 years postpartum in first-time mothers, reported GM volume reductions in the anterior and posterior midline (extending from the medial frontal cortex to the anterior cingulate cortex (ACC)), bilateral lateral prefrontal cortex (PFC), and bilateral temporal cortex. The GM reductions were stable at the 2-year postpartum time point with the exception of the left hippocampal cluster whose volume recovered. Areas of GM volume reduction were active during tests of parental attachment and implicated in social interaction and cognition. Reductions in surface area and cortical thickness were also reported across prepartum and early postpartum time points [41••].
No imaging studies to date have examined GM ROI morphometry, VBM, surface area, or cortical thickness differences between euthymic peripartum women and those with peripartum mood disorders nor have any studies to date examined WM tract integrity.
Functional MRI: Activation-Based and Resting-State Investigations
Functional magnetic resonance imaging (fMRI) is a class of imaging techniques that detects cerebral blood-oxygenation-level dependent (BOLD) changes that occur in response to changes in neural activity [42] either with activation or at rest. fMRI is used to assess activation patterns in separate and distinct brain regions which imply communication and thus “connectivity” between regions at a given time [43, 44]. Functional connectivity can be examined while a patient completes a task in the scanner or “at rest”. The latter, resting-state functional connectivity (rs-fc), is used to observe changes in discrete brain networks implicated in physiological and disease states, including the default mode network (DMN) [43, 44].
Functional connectivity research [45, 46] has identified a series of groups of brain regions which are active together either at rest or during performance of a task. Networks important in non-peripartum major depression include the default mode network (DMN), the central executive network (CEN), the salience network (SN), dorsal attention network (DAN), and frontoparietal network (FN) [45, 47], though additional networks exist, and full delineation of the networks, and the areas they include, is an area of ongoing research. Overlapping brain areas within each network allow cross-communication. Briefly, the DMN is believed to be a diffuse, discrete network of connected brain regions most active at rest and involved in monitoring of the external environment and internal mentation. Although studies differ, this network often includes the medial prefrontal cortex (MPFC), posterior cingulate cortex (PCC), precuneus, and inferior parietal lobule (IPL) [46]. The CEN is involved in emotional-processing tasks and during attention, working memory, and response-inhibition tasks. The CEN most often includes the LPFC, posterior parietal cortex, frontal eye fields, and part of dorsomedial prefrontal cortex (DMPFC). The SN, in concert with other interconnected brain networks, integrates sensory, emotional, and cognitive information to contribute to a variety of complex functions including social behavior and self-awareness [48]. The SN is a paralimbic-limbic network and often includes the dorsal ACC, anterior insula, amygdala, ventral striatum, dorsomedial thalamus, hypothalamus, and the substantia nigra/ventral tegmental area [49]. The FN includes portions of the lateral PFC and posterior parietal cortex and is involved in dynamic cognitive control [50]. And finally, the DAN is involved with attention to events within the current focus of attention and includes the intraparietal sulcus and the frontal eye fields of each hemisphere [51].
Among functional studies in PPD, a total of ten papers were identified with eight task-based and two resting-state functional connectivity imaging studies. Table 1 summarizes findings from the functional studies reviewed here. Several postpartum neuroimaging studies have examined the neurocircuitry underlying mother-infant interactions in healthy women and are reviewed elsewhere [40, 66].
To examine executive functioning across the early postpartum period, healthy postpartum and non-postpartum women underwent fMRI while performing a response inhibition Go/NoGo task at 48 h and 4–7 weeks postpartum. Responses in postpartum women were compared to healthy non-postpartum women participating in the same task at two points during the menstrual cycle. Overall, postpartum women had a decrease in prefrontal activity during response inhibition tasks when compared to non-postpartum women. Late postpartum women had even greater decreases in prefrontal activity during response inhibition than early postpartum women [52].
Gingnell et al. examined longitudinal changes in emotional processing using two postpartum time points (i.e., within 48 h and 4–6 weeks) in 13 healthy postpartum women and 15 naturally cycling non-pregnant controls [53•]. Early postpartum women had lower reactivity in the right insula, left middle frontal gyrus, and bilateral inferior frontal gyrus when compared to late postpartum women. Postpartum women had greater reactivity in the insula and inferior frontal gyrus when compared to non-pregnant controls. Although study participants did not have a diagnosis of PPD or anxiety, inferior frontal gyrus and insular reactivity was positively correlated with self-reported symptoms of anxiety in the early postpartum and with depression in the late postpartum. It is possible that these changes may allow expression of postpartum mood or anxiety disorders in susceptible women.
The first neuroimaging study to explore differences in neural activation among women with PPD was published in 2007 [54]. In that pilot study, four mothers with PPD and four healthy mothers were tasked with distinguishing emotionally valenced words from non-words while undergoing BOLD fMRI. Silverman et al. expanded the study in 2011 [55]. Both studies report decreased right amygdala activation with threatening words in PPD. This result is contrary to several studies in non-peripartum depression [67] which have reported an association of increased amygdala activation with threatening and sad stimuli [68,69,70]. The authors hypothesized that increased sensitivity to threat may be evolutionarily advantageous in the postpartum period as the mother protects the newborn. Hence, attenuated threat sensitivity may be a disadvantage in PPD.
The results by Silverman et al. were supported by another fMRI study in which 14 mothers with PPD and 16 healthy mothers were asked to match negative adult faces and geometrical shapes [56]. This study found significantly decreased activity in the left DMPFC and left amygdala with negative emotional faces in depressed and anxious mothers. Decreased right amygdala activity was associated with increased infant-related hostility in depressed mothers. Finally, depressed mothers had reduced functional connectivity between DMPFC and amygdala, which could account for hyposensitivity to salient infant cues in PPD. In a different study, Moses-Kolko et al. assessed neural activity during positive emotions using fMRI [57]. Both depressed and healthy mothers had similar initial positive activity peaks in the left ventral striatum in response to the reward task. However, depressed mothers’ responses rapidly attenuated to baseline while healthy mothers had a sustained response to the reward. The rapid attenuation could contribute to decreased motivation and goal-directed behavior in PPD.
Though tasks based on negative adult faces and positive emotions elicited functional differences between depressed and healthy mothers, Barrett et al. hypothesized that infant faces—especially those of their own infant—are particularly salient to mothers [71••]. In their 2012 study, they studied 22 healthy mothers in an affect rating task for infant images—own negative (ON), own positive (OP), unfamiliar negative (UN), and unfamiliar positive (UP). They found that poor quality of maternal experience, which included anxiety and depressed mood, was significantly correlated with reduced amygdala, thalamus, and temporal cortex response to OP compared to UP faces. For all mothers, ON faces were associated with greater response in subgenual ACC, putamen, superior temporal gyrus, and parietal cortex—regions implicated in maternal response to infant cries [72].
With anhedonia as a prominent depressive symptom and prior studies showing decreased amygdala response with negative stimuli in PPD, Wonch et al. focused on amygdala response to positive stimuli [58••]. fMRI results from 28 mothers with PPD were compared to those from 17 healthy mothers when they were engaged in affect rating task for positive stimuli—own infant, other infant, and non-infant. There was an overall increase in right amygdala response to all positive stimuli in PPD, contrary to prior MDD study results [73], and decreased amygdala-right insular cortex connectivity in mothers with PPD when viewing own vs. other infants, when compared to healthy mothers. The insular cortex has been associated with emotional awareness [74] and has been proposed to play a role in anxiety disorders [75]. As anxiety is a common symptom in the postpartum period and is often experienced by women with PPD [24, 76, 77], these results suggest that decreased bilateral amygdalae and right insular cortex connectivity may be related to anxiety experienced in the postpartum period in those with PPD.
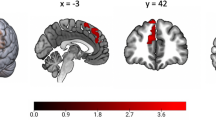
Deligiannnidis et al. examined changes in rs-fc in unmedicated women with unipolar PPD compared to healthy postpartum women. This prospective preliminary study evaluated women across the peripartum period for mood symptoms and then completed cross-sectional neuroimaging within 9 weeks of delivery. ROIs were selected based on results of published activation fMRI studies in PPD [55,56,57, 71••] and included the ACC, and bilateral amygdalae, hippocampi, and DLPFC [27•]. Healthy postpartum women had stronger connectivity between the ACC and the left DLPFC and bilateral amygdalae. Stronger connections in healthy controls were also found between the bilateral amygdalae, ACC and bilateral DLPFC and between the left DLPFC and right amygdalae, and between the right hippocampus and right DLPFC [27•]. These findings are in line with rs-fc studies in non-peripartum depression which have shown decreased functional connectivity between cortical and limbic structures [78,79,80] and suggest a possible commonality between the two disease states.
While the DMN is not completely understood, it is believed to be a diffuse, discrete network of connected brain regions most active at rest and involved in monitoring of the external environment and internal mentation [46, 81]. Research indicates that the DMN is altered in Alzheimer’s disease, schizophrenia [46], and non-peripartum depression [82]. Chase et al. [76] used rs-fc to evaluate alterations in the DMN in 14 women with PPD and 23 healthy postpartum women, focusing mainly on the PCC in addition to the ACC given their hypothesized importance in the DMN [46] and the implication of the PCC in non-peripartum depressive disorders [79]. Postpartum scans performed within 12 weeks of delivery revealed disrupted PCC to right amygdala connectivity in PPD patients compared to healthy postpartum controls. Across all subjects, disrupted PCC-right amygdala connectivity was correlated with PCC-parahippocampus gyrus/subiculum connectivity but not PCC-ACC connectivity. As the ACC is believed to play a significant role in the DMN [46], these findings may suggest that the disrupted connectivity observed for the PCC is not due to a generalized fault in the DMN and may in fact involve parahippocampal areas. While the PCC is suggested to be an important component of the DMN [46], it has also been implicated to have a role in future-planning and attention [83], while the amygdala plays an integral role in emotional regulation and emotional processing [84]. The authors speculated that the disrupted PCC to amygdala connectivity may be related to how attentive the mother is to her responsibilities with the newborn and may even be related to the deficits in mother-infant bonding seen in PPD. The role of parahippocampal areas are currently unclear and further research will be required to determine how these areas contribute to changes in brain connectivity in PPD.
MR Molecular Imaging: Positron Emission Tomography and Magnetic Resonance Spectroscopy
Table 1 summarizes findings from the molecular imaging studies reviewed here.
Positron Emission Tomography Imaging of Brain Metabolism
Positron emission tomography (PET) methods are used to examine cerebral metabolism; protein expression and changes in expression (e.g., density of receptors, ligand transporters, enzymes); drug occupancy and radiotracer competition; and endogenous neurotransmitter release [85]. Tracers of interest labeled with positron-emitting radioisotopes are injected into the bloodstream. Radioactivity from the labeled tracers is detected by the PET scanner as the tracer traverses the cerebral vasculature and interacts with the brain parenchyma.
To date, PET studies of postpartum mood have focused on biochemical systems implicated in non-peripartum depression. Monoamine oxidase A (MAO-A) metabolizes a variety of neurotransmitters such as serotonin and norepinephrine, both of which are implicated in depressive disorders outside of the peripartum period [86, 87]. Moreover, alterations in MAO-A enzyme density have been reported in non-peripartum depressive disorders [88], and preclinical studies report a relationship between estrogen and MAO-A [89]. Carbon-11 (11C)-harmine has high selectivity and affinity for MAO-A and is highly reversible [90]. In a study comparing healthy women 4–6 days postpartum to healthy non-postpartum controls [60••], Sacher et al. used 11C-harmine PET to measure MAO-A total volume distribution (VT), an index of MAO-A levels, in several brain areas. MAO-A VT in the PFC, ACC, anterior temporal cortex, thalamus, dorsal putamen, hippocampus, and midbrain were significantly elevated (43%) in healthy postpartum women compared with healthy non-postpartum controls at a time of estrogen decline. Elevated early postpartum MAO-A (VT) may indicate a monoamine-lowering process important to the development of postpartum blues or mood disorders. In a follow-up study [61], MAO-A levels were examined using 11C–harmine PET in the PFC and ACC of women with PPD, healthy postpartum women who cry due to sad mood, healthy postpartum women, and healthy non-postpartum controls. MAO-A density was increased by 22% in PPD in the PFC and by 19% in the ACC compared to healthy postpartum women and by 15% in healthy women who cry in the PFC and by 13% in the ACC compared with healthy postpartum women. Together, these findings suggest a role of MAO-A in PPD.
PET has also been used to evaluate changes in the dopaminergic system in postpartum women. As decreases in dopamine transmission and dopamine metabolites have been noted in non-peripartum depression [91], Moses-Kolko et al. used carbon-11(11C) labeled raclopride to evaluate alterations in dopamine receptor binding in depressed women (postpartum and non-postpartum) compared to healthy controls (postpartum and non-postpartum) [62••]. The tracer 11C–raclopride is a D2 and D3 receptor antagonist and is a measure of the availability and density of dopamine receptors [92, 93]. Unipolar depression and postpartum status were associated with lower D2/3 receptor binding in the whole striatum; however, there were no differences in D2/3 receptor binding between postpartum depressed and healthy postpartum women. The observed lower binding could be due to either increased competitive binding of intrasynaptic dopamine or reduced D2/3 receptor expression. The postpartum-associated decrease in D2/3 binding may indicate vulnerability toward developing depression in the postpartum period.
11C-WAY100635, a serotonin-1A receptor radioligand [94], has been used to examine serotonin receptor binding in PPD. Statistically significant differences in serotonin receptor binding were reported in the mesiotemporal cortex, subgenual ACC, and left lateral OFC by a magnitude of 17–27% in women with PPD compared with healthy postpartum women [63]. These results suggest that the alterations in the serotonergic system implicated in non-peripartum depression [95] may additionally be an important factor in the pathogenesis of PPD.
Magnetic Resonance Spectroscopy
Magnetic resonance spectroscopy (MRS) is a non-invasive, non-radiating technique which is used frequently in the evaluation of biochemical changes in non-peripartum depression [96] among many other psychiatric [97, 98] and neurological disorders [99, 100]. MRS is similar to magnetic resonance imaging in that it uses signals from hydrogen ions, though while MRI creates an image of the brain, the MRS technique gives information about the concentration of biochemicals in selected brain regions. Initial MRS studies have focused on the main CNS inhibitory and excitatory neurotransmitters, gamma-aminobutyric acid (GABA), and glutamate.
Very little is known about how neurochemistry and metabolism changes across the peripartum period [101]. The first MRS study in PPD measured potential differences in cortical GABA concentration between healthy postpartum, postpartum depressed, and healthy-follicular-phase women [64]. Occipital cortex GABA concentrations were reduced in all postpartum vs. healthy-follicular-phase women, and no differences were identified between depressed or healthy postpartum women [64]. Women who develop postpartum mood disorders may not be able to adapt to this transient period of reduced cortical GABA concentration in comparison to women who do not develop postpartum mood disturbances.
More recently, MRS has been used to assess cortical glutamate concentrations in PPD given increasing evidence suggesting glutamate as a key biochemical in non-peripartum depression through effects on both neuroplasticity and regulation of neurotransmitter release [102]. To evaluate whether the glutaminergic changes seen in non-peripartum depression [103] are evident in PPD, McEwen et al. used MRS to measure medial prefrontal cortex (MPFC) glutamate concentrations in 12 women with PPD and 12 healthy postpartum women [65]. Study participants from both groups were matched based on the time of their scan following delivery, between 3 weeks and 3 months postpartum. MPFC glutamate concentration was significantly increased in PPD. As studies using MRS in non-peripartum depression have reported reduced levels of glutamate in the MPFC [103], this study shows a possible difference between non-peripartum depression and PPD. Most recently, a late postpartum MRS study of 36 women with PPD and 25 healthy postpartum controls reported lower combined glutamate plus glutamine and combined N-acetylaspartate (NAA) plus N-acetylaspartylglutamate in the left DLPFC in PPD with no between-group difference in the ACC [104]. Authors reported that these findings were in alignment with those reported in non-peripartum depression and that PPD may be a subtype of MDD.
Conclusions
Depression is increasingly understood as a disorder of communication among large-scale “functional” brain networks. To date, much more research has been reported in non-peripartum depression than PPD. Understanding the main networks implicated in non-peripartum depression will aid our understanding in how imaging findings are similar to or specific to PPD. As summarized in a recent meta-analysis (of 27 resting-state data sets) of network dysfunction in depression [45], reduced connectivity within regions of the FN may give rise to deficits in cognitive control of attention and emotion regulation, whereas ruminative thoughts may arise due to increased connectivity between the FN and the DMN and reduced connectivity between the FN and the DAN. Abnormalities in emotion/arousal control may stem from reduced connectivity between the AN and top-down regulation by MPFC areas. This meta-analysis concluded that altered connectivity between the VAN and posterior regions may additionally contribute to abnormalities in salience monitoring.
While there are only two resting-state studies in PPD compared to dozens in non-peripartum depression, there is a growing evidence base for changes in functional connectivity in PPD compared to healthy postpartum women. Bringing together the resting-state and task-based functional connectivity data reviewed here, PPD appears to be associated with changes in connectivity involving the DMN, the SN, and CEN. For example, studies point to reduced connectivity between the DMN and the SN, particularly between the PCC and right AMYG and reduced connectivity between regions of the PFC and amygdala. In PPD, several studies indicate less engagement of neurocircuitry involved in emotional salience and fear processing of negative stimuli including the amygdala, with a couple of studies indicating increased amygdala engagement with positive stimuli. This response pattern appears to differ from that reported in non-peripartum depression [73]. A few PPD studies lend additional evidence of changes in the SN including those demonstrating attenuation of ventral striatal activity after receipt of a reward and reduced ventral striatal activation with positive stimuli. Fewer studies have specifically examined the CEN in PPD; however, bringing together the findings from this review, there is evidence of altered connectivity in the posterior OFC related to a task involving emotion-influenced decision-making and in connections between bilateral DLPFC (regions involved in memory encoding) and between the DLPFC and amygdala. More detailed studies are needed to better examine the executive and attentional networks in PPD and their connectivity with other networks.
Imaging studies in PPD utilizing MRS and PET to evaluate changes in biochemical systems throughout the postpartum brain are in their infancy. Metabolism changes involving monoamine oxidase A, GABA, glutamate, serotonin, and dopamine have been reported. While we still do not have a full understanding of the effects of biochemical changes on PPD, these imaging studies have laid a foundation for future research and will have important implications for the treatment and prevention of postpartum mood disorders.
Initial studies reviewed here indicate that the peripartum period itself is associated with localized changes in GM volume, but there are no structural MRI studies published in PPD. As imaging studies have reported structural brain changes in non-puerperal depression [105,106,107], future research is needed to examine potential structural changes associated with peripartum mood disorders.
A challenge to interpreting the current imaging data in PPD includes the lack of studies which fully characterize the normal structural, functional, and metabolic changes occurring due to pregnancy and then in early and late postpartum. This gap of knowledge is an opportunity for understanding the longitudinal changes which occur throughout this period that will help us put the current imaging findings into context. It would be surprising if we did not find natural changes in structural and functional connectivity and metabolism across the peripartum period. It might be that for women who are at risk to develop peripartum mood and anxiety disorders, the normal longitudinal changes take an alternate course, resulting in the differences we observe in cross-sectional imaging studies which are correlated with behavioral changes including maternal depressive and anxiety symptomatology and changes in attachment or mothering behaviors.
PPD is a heterogeneous disorder with regard to timing of onset and symptomatology [24]. Imaging studies to date have included a variety of PPD putative subtypes which could make it challenging to fully examine functional brain networks without significant numbers of participants within each subtype to make adequately powered comparisons. While the impact of peripartum change in reproductive hormones on the CNS is not fully appreciated, studies have suggested that rapid physiological shifts in neuroactive hormones may play a role in the development of PPD [26]. Further research is needed to understand how these physiological shifts elicit changes at the structural, functional, and molecular neural levels [27•, 108,109,110] and may contribute to the development of peripartum depressive and anxiety disorders.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662–73.
Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New parents and mental disorders: a population-based register study. JAMA. 2006;296(21):2582–9.
Valdimarsdottir U, Hultman CM, Harlow B, Cnattingius S, Sparen P. Psychotic illness in first-time mothers with no previous psychiatric hospitalizations: a population-based study. PLoS Med. 2009;6(2):e13.
O'Hara MW, Schlechte JA, Lewis DA, Wright EJ. Prospective study of postpartum blues. Biologic and psychosocial factors. Arch Gen Psychiatry. 1991;48(9):801–6.
Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139G–49G.
Tebeka S, Le Strat Y, Dubertret C. Developmental trajectories of pregnant and postpartum depression in an epidemiologic survey. J Affect Disord. 2016;203:62–8.
O'Hara MW, Swain A. Rates and risk of postpartum depression—a meta-analysis. Int Rev Psychiatry. 1996;8(1):37–54.
Wisner KL, Chambers C, Sit DK. Postpartum depression: a major public health problem. JAMA. 2006;296(21):2616–8.
Fisher J, Tran T, La BT, Kriitmaa K, Rosenthal D, Tran T. Common perinatal mental disorders in northern Viet Nam: community prevalence and health care use. Bull World Health Organ. 2010;88(10):737–45.
Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet (London, England). 2007;370(9590):859–77.
Hu R, Li Y, Zhang Z, Yan W. Antenatal depressive symptoms and the risk of preeclampsia or operative deliveries: a meta-analysis. PLoS One. 2015;10(3):e0119018.
Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77–87.
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–24.
Turner C, Boyle F, O'Rourke P. Mothers’ health post-partum and their patterns of seeking vaccination for their infants. Int J Nurs Pract. 2003;9(2):120–6.
Minkovitz CS, Strobino D, Scharfstein D, Hou W, Miller T, Mistry KB, et al. Maternal depressive symptoms and children’s receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–14.
Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: a cohort study. Arch Gen Psychiatry. 2004;61(9):946–52.
Rahman A, Bunn J, Lovel H, Creed F. Maternal depression increases infant risk of diarrhoeal illness: a cohort study. Arch Dis Child. 2007;92(1):24–8.
Wisner KL, Parry BL, Piontek CM. Clinical practice. Postpartum depression. N Engl J Med. 2002;347(3):194–9.
Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of the literature. Arch Womens Ment Health. 2003;6(4):263–74.
Murray L. The impact of postnatal depression on infant development. J Child Psychol Psychiatry. 1992;33(3):543–61.
Halligan SL, Murray L, Martins C, Cooper PJ. Maternal depression and psychiatric outcomes in adolescent offspring: a 13-year longitudinal study. J Affect Disord. 2007;97(1–3):145–54.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, DSM-5. 5th ed. Washington, D.C.: American Psychiatric Publishing; 2013.
Robertson E, Celasun N, Stewart DE. Risk factors for postpartum depression. In: Stewart DE, Robertson E, Dennis C-L, Grace SL, Wallington T, editors. Postpartum depression: literature review of risk factors and interventions. Toronto: World Health Organization; 2003.
Postpartum Depression: Action Towards Causes and Treatment (PACT) Consortium. Heterogeneity of postpartum depression: a latent class analysis. Lancet Psychiatry. 2015;2(1):59–67.
Bloch M, Rubinow DR, Schmidt PJ, Lotsikas A, Chrousos GP, Cizza G. Cortisol response to ovine corticotropin-releasing hormone in a model of pregnancy and parturition in euthymic women with and without a history of postpartum depression. J Clin Endocrinol Metab. 2005;90(2):695–9.
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry. 2000;157(6):924–30.
• Deligiannidis KM, Sikoglu EM, Shaffer SA, Frederick B, Svenson AE, Kopoyan A, et al. GABAergic neuroactive steroids and resting-state functional connectivity in postpartum depression: a preliminary study. J Psychiatr Res. 2013;47(6):816–28. This study evaluated resting-state connectivity in women with PPD and healthy postpartum women and demonstrated decreased functional connectivity in brain areas previously implicated in non-puerperal depression.
Harris B, Lovett L, Newcombe RG, Read GF, Walker R, Riad-Fahmy D. Maternity blues and major endocrine changes: Cardiff puerperal mood and hormone study II. BMJ. 1994;308(6934):949–53.
Magiakou MA, Mastorakos G, Rabin D, Dubbert B, Gold PW, Chrousos GP. Hypothalamic corticotropin-releasing hormone suppression during the postpartum period: implications for the increase in psychiatric manifestations at this time. J Clin Endocrinol Metab. 1996;81(5):1912–7.
Stuebe AM, Grewen K, Pedersen CA, Propper C, Meltzer-Brody S. Failed lactation and perinatal depression: common problems with shared neuroendocrine mechanisms? J Women's Health (Larchmt). 2012;21(3):264–72.
Hellgren C, Akerud H, Skalkidou A, Sundstrom-Poromaa I. Cortisol awakening response in late pregnancy in women with previous or ongoing depression. Psychoneuroendocrinology. 2013;38(12):3150–4.
Meinlschmidt G, Martin C, Neumann ID, Heinrichs M. Maternal cortisol in late pregnancy and hypothalamic-pituitary-adrenal reactivity to psychosocial stress postpartum in women. Stress. 2010;13(2):163–71.
Nierop A, Bratsikas A, Zimmermann R, Ehlert U. Are stress-induced cortisol changes during pregnancy associated with postpartum depressive symptoms? Psychosom Med. 2006;68(6):931–7.
Corwin EJ, Pajer K, Paul S, Lowe N, Weber M, McCarthy DO. Bidirectional psychoneuroimmune interactions in the early postpartum period influence risk of postpartum depression. Brain Behav Immun. 2015;49:86–93.
Boufidou F, Lambrinoudaki I, Argeitis J, Zervas IM, Pliatsika P, Leonardou AA, et al. CSF and plasma cytokines at delivery and postpartum mood disturbances. J Affect Disord. 2009;115(1–2):287–92.
Sharkey KM, Pearlstein TB, Carskadon MA. Circadian phase shifts and mood across the perinatal period in women with a history of major depressive disorder: a preliminary communication. J Affect Disord. 2013;150(3):1103–8.
Parry BL, Meliska CJ, Sorenson DL, Lopez AM, Martinez LF, Nowakowski S, et al. Plasma melatonin circadian rhythm disturbances during pregnancy and postpartum in depressed women and women with personal or family histories of depression. Am J Psychiatry. 2008;165(12):1551–8.
Bandettini PA. What’s new in neuroimaging methods? Ann N Y Acad Sci. 2009;1156:260–93.
Kim P, Leckman JF, Mayes LC, Feldman R, Wang X, Swain JE. The plasticity of human maternal brain: longitudinal changes in brain anatomy during the early postpartum period. Behav Neurosci. 2010;124(5):695–700.
Swain JE, Lorberbaum JP, Kose S, Strathearn L. Brain basis of early parent-infant interactions: psychology, physiology, and in vivo functional neuroimaging studies. J Child Psychol Psychiatry. 2007;48(3–4):262–87.
•• Hoekzema E, Barba-Muller E, Pozzobon C, Picado M, Lucco F, Garcia-Garcia D, et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci. 2017;20(2):287–96. This prospective fMRI study identified gray matter volume reductions that occurred exclusively as a product of pregnancy and additionally demonstrated that majority of these reductions persist at 2 years postpartum.
Logothetis NK, Pauls J, Augath M, Trinath T, Oeltermann A. Neurophysiological investigation of the basis of the fMRI signal. Nature. 2001;412(6843):150–7.
van den Heuvel MP, Hulshoff Pol HE. Exploring the brain network: a review on resting-state fMRI functional connectivity. Eur Neuropsychopharmacol. 2010;20(8):519–34.
Glover GH. Overview of functional magnetic resonance imaging. Neurosurg Clin N Am. 2011;22(2):133–9. vii
Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA. Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiat. 2015;72(6):603–11.
Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1–38.
Mulders PC, van Eijndhoven PF, Schene AH, Beckmann CF, Tendolkar I. Resting-state functional connectivity in major depressive disorder: a review. Neurosci Biobehav Rev. 2015;56:330–44.
Menon V. Salience network. In: Toga AW, editor. Brain mapping: an encyclopedic reference. vol 2. Elsevier: Academic Press; 2015. p. 597–611.
Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27(9):2349–56.
Zanto TP, Gazzaley A. Fronto-parietal network: flexible hub of cognitive control. Trends Cogn Sci. 2013;17(12):602–3.
Vossel S, Geng JJ, Fink GR. Dorsal and ventral attention systems: distinct neural circuits but collaborative roles. Neuroscientist. 2014;20(2):150–9.
Bannbers E, Gingnell M, Engman J, Morell A, Sylven S, Skalkidou A, et al. Prefrontal activity during response inhibition decreases over time in the postpartum period. Behav Brain Res. 2013;241:132–8.
• Gingnell M, Bannbers E, Moes H, Engman J, Sylven S, Skalkidou A, et al. Emotion reactivity is increased 4–6 weeks postpartum in healthy women: a longitudinal fMRI study. PLoS One. 2015;10(6):e0128964. This study was the first to address longitudinal changes in emotion-induced brain reactivity in healthy women during the postpartum period using fMRI and found that women had lower reactivity in the right insula, left middle frontal gyrus, and bilateral inferior frontal gyrus in early postpartum when compared to late postpartum.
Silverman ME, Loudon H, Safier M, Protopopescu X, Leiter G, Liu X, et al. Neural dysfunction in postpartum depression: an fMRI pilot study. CNS Spectr. 2007;12(11):853–62.
Silverman ME, Loudon H, Liu X, Mauro C, Leiter G, Goldstein MA. The neural processing of negative emotion postpartum: a preliminary study of amygdala function in postpartum depression. Arch Womens Ment Health. 2011;14(4):355–9.
Moses-Kolko EL, Perlman SB, Wisner KL, James J, Saul AT, Phillips ML. Abnormally reduced dorsomedial prefrontal cortical activity and effective connectivity with amygdala in response to negative emotional faces in postpartum depression. Am J Psychiatry. 2010;167(11):1373–80.
Moses-Kolko EL, Fraser D, Wisner KL, James JA, Saul AT, Fiez JA, et al. Rapid habituation of ventral striatal response to reward receipt in postpartum depression. Biol Psychiatry. 2011;70(4):395–9.
•• Wonch KE, de Medeiros CB, Barrett JA, Dudin A, Cunningham WA, Hall GB, et al. Postpartum depression and brain response to infants: differential amygdala response and connectivity. Soc Neurosci. 2016;11(6):600–17. This study used fMRI to evaluate amygdala response to positive stimuli and demonstrated that there is overall increased right amygdala response and decreased amygdala-right insular cortex connectivity in PPD women compared to healthy postpartum women. This is also the first report of altered response and functional connectivity in mothers by parity status.
•• Chase HW, Moses-Kolko EL, Zevallos C, Wisner KL, Phillips ML. Disrupted posterior cingulate-amygdala connectivity in postpartum depressed women as measured with resting BOLD fMRI. Soc Cogn Affect Neurosci. 2014;9(8):1069–75. This study examined resting-state functional connectivity in postpartum women and found that posterior cingulate cortex-right amygdala connectivity was significantly disrupted in depressed compared to healthy mothers.
•• Sacher J, Wilson AA, Houle S, Rusjan P, Hassan S, Bloomfield PM, et al. Elevated brain monoamine oxidase A binding in the early postpartum period. Arch Gen Psychiatry. 2010;67(5):468–74. This study examined brain MAO-A total distribution volume in the early postpartum period and reported that mean distribution volume was significantly elevated throughout several areas analyzed.
Sacher J, Rekkas PV, Wilson AA, Houle S, Romano L, Hamidi J, et al. Relationship of monoamine oxidase-A distribution volume to postpartum depression and postpartum crying. Neuropsychopharmacology. 2015;40(2):429–35.
•• Moses-Kolko EL, Price JC, Wisner KL, Hanusa BH, Meltzer CC, Berga SL, et al. Postpartum and depression status are associated with lower [[(1)(1)C]raclopride BP(ND) in reproductive-age women. Neuropsychopharmacology. 2012;37(6):1422–32. This study used PET scans with carbon-11 raclopride to demonstrate that D2/3 receptor binding is decreased in both unipolar depressed patients and postpartum patients regardless of depressive status with no difference in D2/3 receptor binding between PPD women and healthy postpartum women.
Moses-Kolko EL, Wisner KL, Price JC, Berga SL, Drevets WC, Hanusa BH, et al. Serotonin 1A receptor reductions in postpartum depression: a positron emission tomography study. Fertil Steril. 2008;89(3):685–92.
Epperson CN, Gueorguieva R, Czarkowski KA, Stiklus S, Sellers E, Krystal JH, et al. Preliminary evidence of reduced occipital GABA concentrations in puerperal women: a 1H-MRS study. Psychopharmacology. 2006;186(3):425–33.
McEwen AM, Burgess DT, Hanstock CC, Seres P, Khalili P, Newman SC, et al. Increased glutamate levels in the medial prefrontal cortex in patients with postpartum depression. Neuropsychopharmacology. 2012;37(11):2428–35.
Kim P, Strathearn L, Swain JE. The maternal brain and its plasticity in humans. Horm Behav. 2016;77:113–23.
Drevets WC, Price JL, Furey ML. Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct. 2008;213(1–2):93–118.
Fu CH, Williams SC, Cleare AJ, Brammer MJ, Walsh ND, Kim J, et al. Attenuation of the neural response to sad faces in major depression by antidepressant treatment: a prospective, event-related functional magnetic resonance imaging study. Arch Gen Psychiatry. 2004;61(9):877–89.
Siegle GJ, Steinhauer SR, Thase ME, Stenger VA, Carter CS. Can’t shake that feeling: event-related fMRI assessment of sustained amygdala activity in response to emotional information in depressed individuals. Biol Psychiatry. 2002;51(9):693–707.
Sheline YI, Barch DM, Donnelly JM, Ollinger JM, Snyder AZ, Mintun MA. Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: an fMRI study. Biol Psychiatry. 2001;50(9):651–8.
•• Barrett J, Wonch KE, Gonzalez A, Ali N, Steiner M, Hall GB, et al. Maternal affect and quality of parenting experiences are related to amygdala response to infant faces. Soc Neurosci. 2012;7(3):252–68. This is the first study to use fMRI activation patterns as a function of the affect of an infant face and found that poor quality of maternal experience is significantly correlated to reduced amygdala response to own compared to other positive infant faces.
Swain JE, Lorberbaum JP. Imaging the human parental brain. Burlington: Academic Press; 2008. p. 584.
Stuhrmann A, Dohm K, Kugel H, Zwanzger P, Redlich R, Grotegerd D, et al. Mood-congruent amygdala responses to subliminally presented facial expressions in major depression: associations with anhedonia. J Psychiatry Neurosci. 2013;38(4):249–58.
Gu X, Hof PR, Friston KJ, Fan J. Anterior insular cortex and emotional awareness. J Comp Neurol. 2013;521(15):3371–88.
Paulus MP, Stein MB. An insular view of anxiety. Biol Psychiatry. 2006;60(4):383–7.
Wenzel A, Haugen EN, Jackson LC, Brendle JR. Anxiety symptoms and disorders at eight weeks postpartum. J Anxiety Disord. 2005;19(3):295–311.
Britton JR. Maternal anxiety: course and antecedents during the early postpartum period. Depress Anxiety. 2008;25(9):793–800.
Anand A, Li Y, Wang Y, Wu J, Gao S, Bukhari L, et al. Activity and connectivity of brain mood regulating circuit in depression: a functional magnetic resonance study. Biol Psychiatry. 2005;57(10):1079–88.
Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry. 2007;62(5):429–37.
Veer IM, Beckmann CF, Baerends E, van Tol MJ, Ferrarini L, Milles JR, et al. Reduced functional connectivity in major depression: a whole brain study of multiple resting-state networks. NeuroImage. 2009;47(Supplement 1):S70.
Andrews-Hanna JR. The brain’s default network and its adaptive role in internal mentation. Neuroscientist. 2012;18(3):251–70.
Sheline YI, Price JL, Yan Z, Mintun MA. Resting-state functional MRI in depression unmasks increased connectivity between networks via the dorsal nexus. Proc Natl Acad Sci U S A. 2010;107(24):11020–5.
Leech R, Sharp DJ. The role of the posterior cingulate cortex in cognition and disease. Brain. 2014;137(Pt 1):12–32.
Phelps EA, LeDoux JE. Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron. 2005;48(2):175–87.
Placzek MS, Zhao W, Wey HY, Morin TM, Hooker JM. PET neurochemical imaging modes. Semin Nucl Med. 2016;46(1):20–7.
Gaweska H, Fitzpatrick PF. Structures and mechanism of the monoamine oxidase family. Biomol Concepts. 2011;2(5):365–77.
Harmer CJ, Duman RS, Cowen PJ. How do antidepressants work? New perspectives for refining future treatment approaches. Lancet Psychiatry. 2017.
Meyer JH, Ginovart N, Boovariwala A, Sagrati S, Hussey D, Garcia A, et al. Elevated monoamine oxidase a levels in the brain: an explanation for the monoamine imbalance of major depression. Arch Gen Psychiatry. 2006;63(11):1209–16.
Chevillard C, Barden N, Saavedra JM. Estradiol treatment decreases type A and increases type B monoamine oxidase in specific brain stem areas and cerebellum of ovariectomized rats. Brain Res. 1981;222(1):177–81.
Bergstrom M, Westerberg G, Langstrom B. 11C-harmine as a tracer for monoamine oxidase A (MAO-A): in vitro and in vivo studies. Nucl Med Biol. 1997;24(4):287–93.
Dunlop BW, Nemeroff CB. The role of dopamine in the pathophysiology of depression. Arch Gen Psychiatry. 2007;64(3):327–37.
Hall H, Kohler C, Gawell L, Farde L, Sedvall G. Raclopride, a new selective ligand for the dopamine-D2 receptors. Prog Neuro-Psychopharmacol Biol Psychiatry. 1988;12(5):559–68.
Gurevich EV, Joyce JN. Distribution of dopamine D3 receptor expressing neurons in the human forebrain: comparison with D2 receptor expressing neurons. Neuropsychopharmacology. 1999;20(1):60–80.
Fornal CA, Metzler CW, Gallegos RA, Veasey SC, McCreary AC, Jacobs BL. WAY-100635, a potent and selective 5-hydroxytryptamine1A antagonist, increases serotonergic neuronal activity in behaving cats: comparison with (S)-WAY-100135. J Pharmacol Exp Ther. 1996;278(2):752–62.
Wang L, Zhou C, Zhu D, Wang X, Fang L, Zhong J, et al. Serotonin-1A receptor alterations in depression: a meta-analysis of molecular imaging studies. BMC Psychiat. 2016;16(1):319.
Rao NP, Venkatasubramanian G, Gangadhar BN. Proton magnetic resonance spectroscopy in depression. Indian J Psychiatry. 2011;53(4):307–11.
Merritt K, Egerton A, Kempton MJ, Taylor MJ, McGuire PK. Nature of glutamate alterations in schizophrenia: a meta-analysis of proton magnetic resonance spectroscopy studies. JAMA psychiat. 2016;73(7):665–74.
Schur RR, Draisma LW, Wijnen JP, Boks MP, Koevoets MG, Joels M, et al. Brain GABA levels across psychiatric disorders: a systematic literature review and meta-analysis of (1) H-MRS studies. Hum Brain Mapp. 2016;37(9):3337–52.
Wang W, Hu Y, Lu P, Li Y, Chen Y, Tian M, et al. Evaluation of the diagnostic performance of magnetic resonance spectroscopy in brain tumors: a systematic review and meta-analysis. PLoS One. 2014;9(11):e112577.
Oz G, Alger JR, Barker PB, Bartha R, Bizzi A, Boesch C, et al. Clinical proton MR spectroscopy in central nervous system disorders. Radiology. 2014;270(3):658–79.
Holdcroft A, Hall L, Hamilton G, Counsell SJ, Bydder GM, Bell JD. Phosphorus-31 brain MR spectroscopy in women during and after pregnancy compared with nonpregnant control subjects. AJNR Am J Neuroradiol. 2005;26(2):352–6.
Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62(1):63–77.
Hasler G, van der Veen JW, Tumonis T, Meyers N, Shen J, Drevets WC. Reduced prefrontal glutamate/glutamine and gamma-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2007;64(2):193–200.
Rosa C, Soares J, Figueiredo F, Cavalli R, Barbieri M, Spanghero M, et al. Glutamatergic and neural dysfunction in postpartum depression using magnetic resonance spectroscopy. Psychiatry Res. Neuroimaging. 2017;265:18–25.
Wise T, Radua J, Nortje G, Cleare AJ, Young AH, Arnone D. Voxel-based meta-analytical evidence of structural disconnectivity in major depression and bipolar disorder. Biol Psychiatry. 2016;79(4):293–302.
Redlich R, Almeida JJ, Grotegerd D, Opel N, Kugel H, Heindel W, et al. Brain morphometric biomarkers distinguishing unipolar and bipolar depression. A voxel-based morphometry-pattern classification approach. JAMA Psychiat. 2014;71(11):1222–30.
Videbech P, Ravnkilde B. Hippocampal volume and depression: a meta-analysis of MRI studies. Am J Psychiatry. 2004;161(11):1957–66.
Schiller CE, Meltzer-Brody S, Rubinow DR. The role of reproductive hormones in postpartum depression. CNS Spectr. 2015;20(1):48–59.
Altemus M, Fong J, Yang R, Damast S, Luine V, Ferguson D. Changes in cerebrospinal fluid neurochemistry during pregnancy. Biol Psychiatry. 2004;56(6):386–92.
Deligiannidis KM, Kroll-Desrosiers AR, Mo S, Nguyen HP, Svenson A, Jaitly N, et al. Peripartum neuroactive steroid and gamma-aminobutyric acid profiles in women at-risk for postpartum depression. Psychoneuroendocrinology. 2016;70:98–107.
Acknowledgements
The authors would like to thank the following: Janice Lester, MLS; Reference and Education Librarian; Health Science Library; Long Island Jewish Medical Center; Northwell Health.
Role of the Funding Source
This manuscript was supported by the National Institutes of Health Grant (5K23MH097794). Dr. Deligiannidis currently receives funding from the National Institutes of Health and SAGE Therapeutics and receives royalties from an NIH Employee Invention. The views expressed in this article are those of the authors and do not necessarily reflect the position of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Christy Duan and Jessica Cosgrove each declare no potential conflicts of interest.
Kristina M. Deligiannidis reports a research grant from the National Institutes of Health.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Reproductive Psychiatry and Women’s Health
Rights and permissions
About this article
Cite this article
Duan, C., Cosgrove, J. & Deligiannidis, K.M. Understanding Peripartum Depression Through Neuroimaging: a Review of Structural and Functional Connectivity and Molecular Imaging Research. Curr Psychiatry Rep 19, 70 (2017). https://doi.org/10.1007/s11920-017-0824-4
Published:
DOI: https://doi.org/10.1007/s11920-017-0824-4