Abstract
Rationale
Childbirth is associated with rapid neuroendocrine fluctuations, which are thought to contribute to the phatogenesis of postpartum major depression (PPD).
Objectives
The aim of this proton magnetic resonance spectroscopy (1H-MRS) study was two-fold; 1) to examine whether puerperium is associated with alterations in occipital cortex gamma-aminobutyric acid (GABA) concentrations and 2) to determine whether such alterations may be more prominent in women with PPD.
Materials and methods
Nine women with PPD, 14 postpartum healthy controls, and ten healthy follicular phase females underwent 1H-MRS at 2.1 Tesla to measure occipital cortex GABA concentrations. Postpartum women were scanned within 6 months of delivery and prior to resumption of menstruation. Healthy non-puerperal controls, drawn from a historical sample, were scanned during the early to mid-follicular phase when ovarian hormone levels would be similar to those found in the puerperium. GABA data were analyzed using analysis of covariance, and regression models were used to explore the relationship between cortical GABA concentrations and blood levels of estradiol, progesterone, and neurosteroids.
Results
Cortical GABA and plasma allopregnanolone (ALLO) concentrations were reduced in both groups of postpartum women, regardless of PPD diagnosis, compared to healthy follicular phase women. There was no correlation between cortical GABA concentrations and estradiol, progesterone, ALLO, or pregnenolone (PREG).
Conclusions
This study is the first to describe reductions in occipital cortex GABA levels in the postpartum period, a time of increased vulnerability to mood disturbances in women. The concomitant reduction in peripheral ALLO levels provides further evidence of alterations in the balance between cortical excitation and inhibition during the puerperium. Women with PPD may represent a subgroup of women who fail to adequately adapt to this alteration in the neuroendocrine milieu.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postpartum depression (PPD), with a prevalence of 10–13%, is one of the most common complications of childbirth (Epperson 1999; O’Hara et al. 1984). While the pathogenesis of PPD is most likely multifactorial, the temporal association between the onset of depression during the puerperium and the rapid shift in the neuroendocrine milieu has led investigators to seek a causal association. Unfortunately, with few exceptions, studies relying on peripheral measures of ovarian hormones and neurosteroids such as allopregnanolone during pregnancy and the puerperium have been disappointingly inconsistent. However, findings from Bloch and colleagues (2000) demonstrating that administration and withdrawal of supraphysiologic doses of estradiol and progesterone sufficient to mimic pregnancy and the puerperium, respectively, provide clear evidence that PPD can be triggered by hormonal changes but only in certain subgroups of vulnerable women. These findings are consistent with those from the same group showing that sensitivity to hormonal perturbations characterize women with premenstrual dysphoric disorder (PMDD; Schmidt et al. 1998). The mechanism for this vulnerability to mood disorders during times of hormonal change is not yet known but could include genetic, psychosocial and developmental factors.
Our group has found that menstrual-cycle-related changes in sex steroids and the progesterone derivative allopregnanolone (ALLO) are associated with changes in cortical gamma-aminobutyric acid (GABA) levels as measured using proton magnetic resonance spectroscopy (1H-MRS; Epperson et al. 2002). In that study, women with PMDD demonstrated evidence of an abnormal relationship between ALLO and GABAergic function.
That pregnancy is associated with prolonged exposure to these neuroactive steroids and the puerperium is characterized by follicular-phase levels of estradiol, progesterone and ALLO; we sought to investigate the impact of pregnancy and childbirth on central GABAergic function and to examine the role GABA may play in the pathogenesis of PPD. Several preclinical studies (Smolen et al. 1993; Jobe and Laird 1981) as well as a recent report (Altemus et al. 2004) of reduced cerebrospinal fluid GABA levels in healthy women undergoing a scheduled caesarian section suggested that we could anticipate finding a reduction in cortical GABA concentrations in postpartum women when compared to a non-puerperal control group.
Materials and methods
Participants
The majority of women in the PPD group were referred by their obstetrician or midwife to the Yale Behavioral Gynecology Program for consultation and treatment. All other study participants were self-referred in response to fliers or paid advertising. Healthy non-depressed postpartum and non-puerperal women were recruited by public advertisements. Subjects gave written informed consent for participation in this study, which was approved by the Yale University School of Medicine’s Human Investigation Committee (New Haven, CT, USA). All subjects were healthy, as determined by medical history and routine laboratory tests. Urine toxicology screens were also negative. The presence of a metallic implant or history of claustrophobia was a ground for exclusion.
To be included, all postpartum women had to be within 6 months of delivery and could not have resumed menstruating. Women with PPD had onset of major depressive disorder (MDD) per clinical interview between delivery and 4 months postpartum, and had a 19-item Hamilton Depression Rating Scale (HAM-D; Hamilton 1960) score of ≥18. Postpartum depressed women had no comorbid axis I disorders or history of a previous psychotic disorder. All subjects were psychotropic-medication-free for at least 9 months prior to undergoing 1H-MRS, with the exception of one woman who took lorazepam twice 6 days prior to presentation but not within 2 weeks of her 1H-MRS scan. Four of the nine postpartum depressed women reported a previous psychiatric history for which they received antidepressant treatment; dysthymia (n=1), MDD (n=3), PPD (n=1), and severe premenstrual syndrome (per retrospective report; n=1). Postpartum non-depressed healthy controls (postpartum HC) could not meet criteria for past or present Axis 1 psychiatric or substance-dependence disorder according to SCID DSM-III-R non-patient edition (SCID-NP; Spitzer et al. 1990) and could not have a HAM-D score of >4.
The ten follicular-phase non-depressed healthy controls (follicular HC) included in this present study are derived from a historical sample of 14 healthy women who participated in our investigation of the impact of menstrual-cycle phase on occipital cortex GABA concentrations (Epperson et al. 2002). Four who had been included in the previous report were excluded, for purposes of this study, as they had estradiol levels which were greater than 257 nmol/l (70 pg/ml) and, thus, not clearly consistent with the hypogonadism of the early follicular phase when non-puerperal women are mostly like postpartum women with respect to their endocrine status. Per study methods, all menstruating women were prospectively evaluated over 2 months to determine the length of their menstrual cycle and to rule out the presence of premenstrual syndrome or PMDD using the Daily Record of Severity of Problems (DRSP; Endicott & Harrison 1990). SCID-non-patient interviews were conducted to screen out individuals with a history of any axis I psychiatric or substance-dependence disorder. Subject report of a first-degree family member with an axis I psychiatric disorder resulted in exclusion from the study. Ovulation was confirmed during the screening using urine ovulation test kits (ANSWER Ovulation Tests, Church & Dwight Co., Princeton, NJ, USA). Women using hormonal contraception within the previous 6 months or pregnant within the previous year were not eligible to participate. Follicular-phase non-puerperal healthy controls (follicular HC) were also psychotropic-medication-free for at least 3 months and did not drink alcohol during the 2 days prior to their scans.
Timing of 1H-MRS scans
Postpartum women underwent 1H-MRS scans within 6 months of delivery of a healthy full-term baby. Special effort was made to scan women with PPD within 7 days of their presentation to the YBG Program so that appropriate treatment was not unduly delayed. Follicular HCs underwent 1H-MRS scanning twice; once during the early to mid-follicular phase and once during the mid-luteal phase of the menstrual cycle. Blood was taken on each scan day for ovarian hormone and neurosteroid determination. To provide an appropriate comparison group for our puerperal women, only data from those follicular HCs scanned early enough in the follicular phase to have estradiol levels <257 pmol/l were included in this present study.
Magnetic resonance spectroscopy of GABA
MR measurements were performed with a 2.1-Tesla spectrometer (Bruker Instruments, Billerica, MA, USA). A 7-cm surface coil was placed against the occipital surface of the head. Scout images were acquired for voxel placement, and non-iterative shimming was performed over a 2.2-cm diameter spherical volume (Shen et al. 1997). A rectangular volume was selected across the midline of the brain, centered 2 cm from the dura. A J-editing sequence (Behar and Boehm 1994; Rothman et al. 1993) was used for GABA detection. Twenty pairs of sub-spectra were acquired, with and without an inversion pulse applied to the GABA C4 proton. The difference of the pairs yielded GABA without contamination of the overlying creatine and choline. The resonance contained both GABA and the related metabolite homocarnosine (Petroff et al. 2000). Thus, the GABA in this paper reflects the sum of these metabolites. Spectra were acquired with 8K data points with a 510-ms acquisition and a 2-s repetition time. Unsuppressed water measurements were acquired to compensate for eddy currents and adjust for a small phase difference induced by the editing pulse. After beginning the study, an upgrade in the manufacturer’s software rendered the acquisition procedure ineffective, so the method was revised. The original measurement used a TE of 68 ms and a volume of 3×1.5×3 cm3. For the new measurement, technical requirements allowed a TE of no less than 80 ms for GABA, and a volume of 3.5×1.5×3.9 cm3 was used for improved signal-to-noise ratios. Subjects in all three groups, with the exception of six women in the postpartum HC group, were scanned with the original method. Measured concentrations of GABA observed with the old and new methods were similar.
Using software written in MATLAB (The Mathworks), each FID was line-broadened by 3 Hz, zero-filled to 32K points, and Fourier-transformed. The sub-spectra were phased based on the spectrum with the inversion pulse applied, and the area of the creatine resonance was measured. The area of the GABA resonances was measured in the difference of the paired sub-spectra. If patients moved during any of the pairs of GABA editing scans, the large, sharp creatine and choline resonances caused well-defined subtraction errors that obscured the GABA, and such pairs of sub-spectra were discarded. GABA was measured with the average of the remaining scans. For the first acquisition method, the concentration of GABA was determined from the ratio of GABA and total creatine resonances (Rothman et al. 1993) according to
where 0.07 was subtracted to account for contributions of co-edited macromolecules (Behar and Ogino 1993) to the GABA resonance, 0.93 is the integral correction factor for the 0.03-ppm difference in the chemical shift of Cr and GABA, 1.01 corrects for the editing efficiency, 3/2 adjusts for the difference of 2 protons detected in GABA vs 3 in Cr, and [Cr] was 9 mmol/kg (Petroff et al. 1989). For the second acquisition method, an in-house version of LCModel (Provencher 1993) was applied to fit the peaks in the GABA-edited spectrum and compare the GABA peak area to that of Cr in the unedited subspectrum without the additional correction factors.
Quantification of voxel gray matter (GM), white matter (WM), and cerebrospinal fluid (CSF)
Quantitative images of T 1 were obtained using inversion-recovery images and radiofrequency inhomogeneity maps (Mason and Rothman 2002). Seven 3-mm thick coronal image slices with 64×64 pixels were acquired with a 240×240 mm2 field of view, spanning the 1.5-cm thick MRS volume. The maps of the radio frequency excitation angle were acquired and used to analyze inversion-recovery time series to generate maps of T 1. T 1 was compared to calibration curves to determine the percentage of GM, WM, and CSF in each image pixel. The values of the image pixels within the MRS voxel were totaled and used to determine the percentage of the voxel that was GM, WM, and solid tissue (i.e., non-CSF tissue) (Mason and Rothman 2002).
Gonadal hormone and neurosteroid determination
Serum estradiol and progesterone levels were determined in a commercial laboratory using heterogeneous competitive magnetic separation assay with a lower limit of detection (LOD) of 30.7 pmol/l and immunoassay techniques with a within-run coefficient of variation (CV) of 8.1% at the LOD for estradiol and a LOD of 0.32 nmol/l and CV of 9.3% for progesterone. Plasma was assayed for neurosteroids including pregnenolone (PREG), 5α-dihydroprogesterone (5αDHP), ALLO and epiallopregnanolone (epiALLO), and pregnanolone were determined using gas chromatographic mass spectroscopic (GC-MS) methods.
GC-MS conditions
The mass spectrometer was a Perkin-Elmer Turbomass (NCI mode). The GC was an Autosystem XL equipped with 150.25 mm (i.d.) methylsilicone column with a 0.05-mm film thickness (Quadrex Corp., New Haven, CT, USA). The initial GC temperature was 150°C, followed by 230°C at 30°C /min, then to 250°C at 10°C/min, and finally to 320°C at 30°C/min. The injection port flow was 1.0 ml/min. Methane was used as the reagent gas for NCI. The injector and transfer-line temperatures were maintained at 300 and 310°C, respectively. Selected ions of m/z 460, m/z 462, and m/z 466 were monitored.
Steroid extraction and separation
Steroids in plasma were extracted by solid-phase extraction using C18 columns. Steroids were derivatized according to the method of Hubbard et al. 1994. All neurosteroids were batch-run under the same laboratory conditions. The range of between-day coefficient of variation for duplicate repeats of samples done over several months were 13.7, 15.9, 16.0, 17.9, and 10.0% for ALLO, pregnanolone, pregnenolone, epiallopregnanolone (epiALLO), and 5 alpha dihydroprogesterone (5DHP), respectively.
Data analysis
All outcome measures were checked for normality using normal probability plots and Kolmogorov–Smirnov statistics prior to analysis. Cortical GABA concentrations from the three groups, our primary outcome measures, were analyzed using analysis of covariance (ANCOVA), with the use of SAS PROC GLM (Littell et al. 1996). To assess whether GABA varies with the number of weeks postpartum, a mixed-effects model, with GABA as the response, group as a between-subject factor, and number of weeks postpartum as a within-subject factor, was fitted. Correlation analyses between serum estradiol and progesterone and plasma neurosteroids and cortical GABA concentrations were conducted with Bonferroni adjustment for multiple analyses. For each hormone, a linear model was fitted with GABA as the response and hormone levels, group, and their interaction as predictors.
Results
Participants
Demographic characteristics and subject mood ratings on scan days are shown in Table 1 for the women included in the data analysis. Mean age in years for the nine women with PPD (30+/−5.6), the 14 postpartum HCs (31+/−4.9), and the ten follicular HCs (29+/−3.8) were similar. Likewise, there were no group differences in years of education or parity. Postpartum depressed and healthy postpartum women were 10.6+/−7.6 weeks and 12.4+/−6.2 weeks postpartum, respectively, at the time of study enrollment. Women with PPD reported onset of symptoms within the first 6 weeks of delivery, with the exception of one subject who experienced onset 16 weeks post delivery. Thus, mean duration of illness prior to study participation was 7.1+/−6.8 weeks. Four of the nine postpartum depressed women reported a confirmed mood and/or substance use/dependence disorder in a first-degree relative, while two others reported suspected diagnoses of depression. All but two women with PPD and 1 postpartum HC were breast-feeding during the study and none had resumed menstruating.
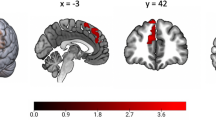
1H-MRS measurements of occipital cortex GABA Levels
Results of data analysis for neuroendocrine measures are depicted in Table 2 and Fig. 1. The first analysis was ANCOVA and compared occipital cortex GABA concentrations (in mmol/kg brain) among the three groups (PPD, postpartum HC, and follicular-phase HC) using SAS PROC GLM (Cary, NC, USA). Age by group interaction and age were considered for inclusion in the model, but were not-significant and were dropped from the final model for parsimony. The overall group effect was significant: F(2,29)=11.98, p=0.002. Multiple comparisons with Tukey adjustment were then performed among the three groups. Both postpartum groups had significantly lower cortical GABA concentrations than the follicular HC group. While the comparison between postpartum groups did not reach statistical significance (p=0.1), there was a trend for the women in the PPD group to have higher (1.39±0.29) cortical GABA levels than those in the healthy postpartum control group (1.11±0.27). ANOVA revealed no significant between group differences in % tissue [F(2,29)=1.12, p=0.34], %GM [F(2,27)=1.03, p=0.37] or %WM [F(2,27)=0.90, p=0.42] in the voxel. Likewise, there was no significant difference (p=0.81) in cortical GABA concentrations in the eight healthy postpartum controls (1.10±0.23) who were scanned after the upgrade compared to those six who were scanned before the upgrade (1.13±0.34).
To assess whether GABA varies with number of weeks postpartum in the postpartum depressed and postpartum HC groups, a mixed model with GABA as response and group and number of weeks postpartum as predictors was fitted. The relationship between the number of weeks postpartum and GABA was not statistically significant at 0.05 level, although it could be considered a trend if not adjusted for multiple tests [F(1,28.8)=3.98, p=0.056]. Note that the group main effect [F(1,29.9)=0.28, p=0.6] and the interaction between weeks postpartum and group [F(1,28.8)=0.68, p=0.42] were not significant.
Analysis of ovarian hormones and neurosteroids
The same approach used for GABA was also used for serum estradiol and progesterone and plasma ALLO, pregnenolone (PREG), the ratio of pregnenolone to progesterone, and the ratio of progesterone to ALLO. Only postpartum women were used for the comparison of the levels of epiALLO and pregnanolone. There were very few subjects in all three groups with values for 5αDHP and, thus, it was excluded from this analysis.
The age by group interaction was never significant and was dropped from the models. The age main effect was significant only for ALLO (although it did not survive multiple correction) and was kept in the model for analysis of group effects. Progesterone [F(2,29)=0.69, p=0.51], pregnenolone [F(2,26)=1.59, p=0.22], epiALLO [F(1,17)=1.6, p=0.22], the ratio of pregnenolone to progesterone [F(2,26)=1.50, p=0.24], and the ratio of progesterone to ALLO [F(2,26)=1.24, p=0.24] were not significant. Significant group differences were observed for estradiol [F(2,29)=12.65, p<0.0001] and ALLO [F(2,25)=7.29, p=0.001]. The results for estradiol and ALLO remained significant after Bonferroni correction. Tukey adjusted p values for the multiple group comparisons for estradiol and ALLO are shown in Table 2. Postpartum HC had significantly lower estradiol levels than both the PPD and follicular HC groups. However, plasma ALLO levels were significantly reduced in both postpartum populations when compared to follicular HCs.
Relationship between neuroendocrine measures
For each hormone, a linear model was fitted with GABA as the response, hormone levels, group, and their interaction as predictors. The results show that the interactions between each hormone (estradiol, progesterone, pregnenolone, and ALLO) and group are not significant. The hormone effects are also insignificant. Because epiALLO was almost completely missing for the follicular HC group, it could not be included in this analysis.
Discussion
The principal finding of this study was that the postpartum period, compared to the follicular phase of the menstrual cycle, is characterized by a reduction in occipital cortex GABA concentrations, regardless of the affective state of the individual. At first glance, it may appear that this finding is driven by unusually high GABA concentrations in our healthy follicular phase women (mean 1.69 mmol/kg brain). Published findings from our colleagues using similar 1H-MRS techniques (Sanacora et al. 1999) have suggested that cortical GABA concentrations are relatively lower in healthy subjects (1.48 mmol/kg brain). However, previous studies included both males and females and did not control for menstrual cycle phase or reproductive status (pre- or postmenopause) in female subjects. As healthy menstruating women have higher cortical GABA concentrations in the follicular compared to the luteal phase of the menstrual cycle (Epperson et al. 2002), and both healthy and depressed women have significantly higher GABA levels than their male counterparts (Sanacora et al. 1999), it is not surprising that occipital cortex GABA concentrations were found to be somewhat lower in healthy controls in previous studies.
In light of the observation that transient depressive symptoms occur in 26–85% (Epperson 1999) and major depression is experienced in up to 13% of postpartum women (O’Hara and Swain 1996), these data suggest that reductions in cortical GABA concentrations in the puerperium may be permissive for the expression of a vulnerability to depression. Preclinical (Smolen et al. 1993) and clinical (Altemus et al. 2004) studies indicate that GABA deficits may emerge during pregnancy. While parturition resulted in the normalization of GABA levels in the cortex and cerebellum of rodents, other brain areas continued to show GABAergic deficiencies into the puerperium (Smolen et al. 1993). Likewise, cerebral spinal fluid levels of GABA were reduced at the time of parturition in women undergoing elective caesarian section (Altemus et al. 2004).
That our women were up to 6 months postpartum when scanned indicates that GABA reductions may be relatively protracted even in healthy women. We found a trend towards increasing GABA levels as women moved further away from childbirth; however, our sample size and choice to scan women who were no more than 6 months postpartum may have limited our ability to determine whether there is a true correlation between cortical GABA levels and time after delivery. Presumably, all postpartum women would begin at some point in the puerperium to have cortical GABA concentrations, which are similar to those seen in follicular phase women. Whether this occurs before or after resumption of menses cannot be determined by this study. In addition, selection of postpartum women who had not yet resumed menstruation biased this sample to include primarily breast-feeding women, limiting the ability to generalize these data to those who choose not to breast-feed.
Another important finding from this first human study examining the role of GABA in the pathogenesis of PPD is that, in contrast to non-puerperal depressed males and females (Sanacora et al. 1999), women with PPD are similar to postpartum HCs with respect to cortical GABA concentrations. This observation raises the question whether PPD, as a potential subtype of MDD, which, like the atypical depression subtype, is associated with “normal” GABA levels (Sanacora et al. 2004). However, a post hoc review of depressive symptoms as recorded by the HAM-D and patient progress notes by the principal author, while blind to individual GABA concentrations, revealed that none of our PPD women met the criteria for the atypical subtype of MDD. Comparing our findings in PPD to those from Sanacora et al. 2004, which indicate that individuals meeting the melancholic criteria or no subtype criteria for MDD have reduced cortical GABA concentrations, suggests that alterations in GABAergic function may contribute to PPD in a manner that is distinct from other subtypes of MDD. Perhaps the reduction in GABA concentrations seen in postpartum women plays a permissive role for PPD in women with a vulnerability to affective disorders such as MDD and PMDD. At least half of the women in our postpartum depressed group had already demonstrated such vulnerability prior to the index pregnancy by having a previous history of dysthymia, MDD/PPD, or PMS.
Psychosocial factors and stressful life events are noted to increase the risk of PPD, but assessment of their relative contribution to the onset of depression would require a larger number of women than are typically included in neuroimaging studies. In addition, genotypic variations in populations of postpartum women may render some at greater risk of depressive symptoms when faced with reductions in GABA concentrations. Recent work has identified an A-to-G single nucleotide polymorphism (SNP) in the −243 position of the gene encoding glutamic acid decarboxylase-65 (GAD65). The G allele has been associated with increased transcriptional activity in vitro (Boutin et al. 2003) and G/A heterozygotes in a group of males and females with MDD have been found to have lower cortical GABA concentration as measured with 1H-MRS than A/A homozygotes with MDD (Sancora et al. 2005).
Several mechanisms may mediate pregnancy and the puerperium-associated reductions in brain GABA. Evidence suggests that normal pregnancy-related reductions in the coenzyme form of vitamin B6, pyridoxal 5’-phosphate (PLP; Furth-Walker et al. 1989; Brophy and Siiteri 1975), may contribute to reductions in brain GABA and lowering of seizure susceptibility during eclamptic pregnancies (Klieger et al. 1969; Jobe and Laird 1981), as PLP is an important coenzyme in the conversion of glutamate to GABA. In addition to pregnancy-related reductions in PLP, another mechanism mediating GABA reductions in postpartum women may involve ALLO modulation of GABAA receptor function. Preclinical findings indicate that pregnancy-related increases in ALLO result in reductions in mRNA encoding for the γ2L GABAA receptor subunit and decreases in the stimulatory effects of muscimol on Cl− uptake by cerebrocortical membrane vesicles (Concas et al. 1998). This pregnancy-induced plasticity in GABAA receptor subunit configuration can be blocked by administration of the 5α reductase inhibitor, finasteride. During withdrawal from ALLO, a decrease in GABAA receptor sensitivity to benzodiazepine administration corresponding to an increase in mRNA encoding for the α4 subunit of the GABAA receptor has been noted (Smith et al. 1998). Certainly, the human pregnancy and puerperium, particularly in nursing women, can be considered a lengthy period of ALLO exposure and withdrawal, respectively.
ALLO is thought to play an important role in the timing of parturition as high levels of ALLO inihibit oxytocin (OT) release from magnocellular neurons of the supraoptic nucleus (Koksma et al. 2003). However, to insure the appropriate secretion of OT around parturition, the peripartum decline in ALLO renders GABAA receptors on OT neurons less sensitive to its inhibitory effects, presumably by decreasing the ratio of α1 to α2 subunits (Brussaard et al. 1997). Thus, plasticity of the GABAA receptor to chronic ALLO modulation followed by acute ALLO withdrawal is likely to contribute to overall fluctuations in GABAergic tone and, thus, inhibitory neurotransmission in the puerperium. That exposure to neurosteroids during pregnancy is considerably longer than that seen in the luteal phase of the menstrual cycle may explain, in part, the relative reduction in cortical GABA concentrations in postpartum women, compared to follicular women, despite both groups having hormone levels consistent with the follicular phase.
Finally, pregnancy is a hyperprolactinemic state, which extends into the postnatal period in women who choose to breast-feed. While secretion of prolactin from anterior pituitary cells is under inhibitory control of both dopamine and GABA (Melis et al. 1984; Apud et al. 1989), hyperprolactinemia disrupts the diurnal rhythm of GABA synthesis and, thus, concentration in various hypothalamic regions (Duvilanski et al. 2003). In addition, prolactin inhibits 5 alpha-reductase activity, thus leading to decreased conversion of progesterone to steroids (such as ALLO) in the rat ovary (Takada et al. 1984). Whether prolactin has an impact on 5 alpha-reductase activity in the brain is not yet known. That the majority of women in our study were breast-feeding and, therefore, considered to be relatively hyperprolactinemic compared to follicular-phase controls may explain the finding of significant reductions in ALLO in the postpartum groups.
It is tempting to interpret the finding of reduced estradiol in the group with the lowest GABA concentration (postpartum HC) as suggesting that estradiol has a stimulatory effect on GABA synthesis. Estradiol is known to have stimulatory effects on NMDA receptor function (Gureviciene et al. 2003; Zamani et al. 2004) and inhibitory effects at the GABAA receptor. Its role in modulating GAD activity and, thus, GABA synthesis throughout the brain is also not clear (Nakamura et al. 2004; Weiland 1992).
While there was no correlation between any ovarian hormone, neurosteroid, or neurosteroid ratio and cortical GABA concentrations, simultaneous reductions in endogenous GABAA receptor agonist ALLO with reductions in GABA concentrations could conceivably lead to further imbalance between cortical excitation and inhibition during the puerperium. Of note, this study was not designed to address the potential differences between central and peripheral levels of ALLO known to exist under certain states (Purdy et al. 1991); nor did we obtain a physiologic measure of cortical excitation/inhibition.
Potential shortcomings of this study include our reliance on a historical follicular-phase healthy control group and restriction of GABA measurement to the occipital cortex. However, the majority of puerperal and non-puerperal subjects were accessioned during the same period and scanned using identical MR techniques. Those postpartum healthy controls scanned before and after the magnet upgrade had similar mean GABA levels. Although it is not usually considered in the pathogenesis of mood disorders, the occipital cortex has been shown to be affected by depression (Kumar et al. 1993), cocaine abuse (Hetherington et al. 1999), and nicotine administration (Domino et al. 2000). Nevertheless, as 1H-MRS techniques are advanced to allow for sequential measurement of GABA levels, they should be applied to other brain areas thought to be involved in mood disorders and/or modulated by sex hormones and their neurosteroid derivatives.
In summary, this is the first neuroimaging study to examine the role of GABA and neurosteroids in the pathogenesis of PPD. While women with PPD had similar occipital cortex GABA concentrations as non-depressed postpartum women, these data indicate that the puerperium is a period of relative reduction in central GABA and peripheral ALLO levels which may lead to an imbalance in cortical excitation and inhibition. Future investigations should include physiologic measures of cortical inhibition as well as determination of genetic polymorphisms, which may render individuals at risk for depression during periods which are normally characterized by GABA reductions.
References
Altemus M, Fong J, Yang R, Damast S, Luine V, Ferguson D (2004) Changes in cerebrospinal fluid neurochemistry during pregnancy. Biol Psychiatry 56(6):386–392
Apud JA, Cocchi D, Locatelli V, Masotto C, Muller EE, Racagni G (1989) Biochemical and functional aspects on the control of prolactin release by the hypothalamo-pituitary GABAergic system. Psychoneuroendocrinology 14:3–17
Behar KL, Boehm D (1994) Measurement of GABA following GABA-transaminase inhibition by gabaculine: a 1H and 31P NMR spectroscopic study of rat brain in vivo. Magn Reson Med 31:660–667
Behar KL, Ogino T (1993) Characterization of macromolecule resonances in the 1H NMR spectrum of rat brain. Magn Reson Med 30:38–44
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR (2000) Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry 157(6):924–930
Boutin P, Dina C, Vasseur F, Dubois S, Corset L, Seron K, Bekris L, Cabellon J, Neve B, Vasseur-Delannoy V, Chikri M, Charles MA, Clement K, Lernmark A, Froguel P (2003) GAD2 on chromosome 10p12 is a candidate gene for human obesity. PLoS Biol 1(3):E68
Brophy MH, Siiteri PK (1975) Pyridoxal phosphate and hypertensive disorders of pregnancy. Am J Obstet Gynecol 121(8):1075–1079
Brussaard AB, Kitts KS, Baker RE, Willems WP, Leyting-Vermeulen JL, Voorn P, Smit AB, Bicknell RJ, Herbison AE (1997) Plasticity in fast synaptic inhibition of adult oxytocin neurons caused by switch in GABAA receptor subunit expression. Neuron 19:1103–1114
Concas A, Mostallino MC, Porcu P, Follesa P, Barbaccia ML, Trabucchi M, Purdy RH, Grisenti P, Biggio G (1998) Role of brain allopregnanolone in the plasticity of gamma-aminobutyric acid type A receptor in rat brain during pregnancy and after delivery. Proc Natl Acad Sci U S A 95(22):13284–13289
Domino EF, Minoshima S, Guthrie SK, Ohl L, Ni L, Koeppe RA et al (2000) Effects of nicotine on regional cerebral glucose metabolism in awake resting tobacco smokers. Neuroscience 101:277–282
Duvilanski BH, Alvarez MP, Castrillon PO, Cano P, Esquifino AI (2003) Daily changes of GABA and taurine concentrations in various hypothalamic areas are affected by chronic hyperprolactinemia. Chronobiol Int 20(2):271–284
Endicott J, Harrison W (1990) Daily rating of severity of problems form. Department of Research Assessment and Training, New York State Psychiatric Institute, New York, NY
Epperson CN (1999) Postpartum major depression: detection and treatment. AFP Fam Pract Ann 59(8):2247–54, 2259–2260
Epperson CN, Haga KK, Mason GF, Sellers E, Gueorguieva R, Zhang W et al (2002) Cortical gamma-aminobutyric acid levels across the menstrual cycle in healthy women and those with premenstrual dysphoric disorder: A proton magnetic resonance spectroscopy study. Arch Gen Psychiatry 59:851–858
Furth-Walker D, Leibman D, Smolen A (1989) Changes in pyridoxal phosphate and pyridoxamine phosphate in blood, liver and brain in the pregnant mouse. J Nutr 119(5):750–756
Gureviciene I, Puolivali J, Pussinen R, Wang J, Tanila H, Ylinen A (2003) Estrogen treatment alleviates NMDA-antagonist induced hippocampal LTP blockade and cognitive deficits in ovariectomized mice. Neurobiol Learn Mem 79(1):72–80
Hamilton, M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Hetherington HP, Telang F, Pan JW, Sammi M, Schuhlein D, Molina P, Volkow ND (1999) Evaluation of cerebral gray white matter metabolite differences by spectroscopic imaging at 4.1T. Magn Reson Med 32:565–571
Hubbard WC, Bickel C, Schleimer RP (1994) Simultaneous quantitation of endogenous levels of cortisone and cortisol in human nasal and bronchoalveolar lavage fluids and plasma via gas chromatography-negative Ion Chemical Ionization Mass Spectrometry. Anal Biochem 221:109–117
Jobe PC, Laird HE (1981) Neurotransmitter abnormalities as determinants of seizure susceptibility and intensity in the genetic models of epilepsy. Biochem Pharmacol 30(23):3137–3144
Klieger JA, Altshuler CH, Krakow G, Hollister C (1969) Abnormal pyridoxine metabolism in toxemia of pregnancy. Ann NY Acad Sci 166(1):288–296
Koksma JJ, van Kesteren RE, Rosahl TW, Zwart R, Smit AB, Luddens H, Brussaard AB (2003) Oxytocin regulates neurosteroid modulation of GABAA receptors in the supraoptic nucleus around parturition. J Neurosci 23:788–797
Kumar A, Newberg A, Alavi A, Berlin J, Smith R, Relvich M (1993) Regional cerebral glucose metabolism in late-life depression and Alzheimer disease: a preliminary positron emission tomography study. Proc Natl Acad Sci U S A 90:7019–7023
Littell RC, Milliken GA, Stroup WW, Wolfinger RD (1996) SAS system for mixed models. SAS Institute, Cary, NC
Mason GF, Rothman DL (2002) Graded image segmentation of brain tissue in the presence of inhomogeneous radio frequency fields. Magn Reson Imaging 20:431–436
Melis GB, Fruzzetti F, Paoletti AM, Mais V, Kemeny A, Strigni F, Boldrini A, Fioretti P (1984) J Clin Endocrinol Metab 58(1):201–205
Nakamura NH, Rosell DR, Akama KT, McEwen BS (2004) Estrogen and ovariectomy regulate mRNA and protein of glutamic acid decarboxylases and cation-chloride cotransporters in the adult rat hippocampus. Neuroendocrinology 80(5):308–323
O’Hara MW, Neunaber DJ, Zekoski EM (1984) Prospective study of postpartum depression: prevalence, course, and predictive factors. J Abnorm Psychology 93(2):158–171
O’Hara MW, Swain A (1996) Rates and risk of postpartum depression—a meta analysis. Int Rev Psychiatry 8:37–54
Petroff OA, Spencer DD, Alger JR, Prichard JW (1989) High-field proton magnetic resonance spectroscopy of human cerebrum obtained during surgery for epilepsy. Neurology 39:1197–1202
Petroff OA, Hyder F, Rothman DL, Mattson RH (2000) Effects of gabapentin on brain GABA, homocarnosine, and pyrrolidinone in epilepsy patients. Epilepsia 41:675–680
Provencher SW (1993) Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn Reson Med 30:672–679
Purdy RH, Morrow AL, Moore PH Jr, Paul SM (1991) Stress-induced elevations of gamma-aminobutyric acid type A receptor-active steroids in the rat brain. Proc Natl Acad Sci U S A 88:4553–4557
Rothman DL, Petroff OA, Behar KL, Mattson RH (1993) Localized 1H NMR measurements of gamma-aminobutyric acid in human brain in vivo. Proc Natl Acad Sci U S A 90:5662–5666
Sanacora G, Mason GF, Rothman DL, Behar KL, Hyder F, Petroff OA et al (1999) Reduced cortical gamma-aminobutyric acid levels in depressed patients determined by proton magnetic resonance spectroscopy. AMA Arch Gen Psychiatry 56:1043–1047
Sanacora G, Gueorguieva R, Epperson CN, Wu YT, Appel M, Rothman DL, Krystal JH, Mason GF (2004) Subtype-specific alterations of gamma-aminobutyric acid and glutamate in patients with major depression. AMA Arch Gen Psychiatry 61(7):705–713
Schmidt PJ, Nieman LK, Danaceau MA, Adams LF, Rubinow DR (1998) Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. N Engl J Med 338(4):209–216
Shen J, Rycyna RE, Rothman DL (1997) Improvements on an in vivo automatic shimming method [FASTERMAP]. Magn Reson Med 38:834–839
Smith SS, Gong QH, Li X, Moran MH, Bitran D, Frye CA, Hsu FC (1998) Withdrawal from 3alpha-OH-5alpha-pregnan-20-One using a pseudopregnancy model alters the kinetics of hippocampal GABAA-gated current and increases the GABA A receptor alpha4 subunit in association with increased anxiety. J Neurosci 18(14):5275–5284
Smolen A, Smolen TN, Han PC (1993) Alterations in regional brain GABA concentrations and turnover during pregnancy. Pharmacol Biochem Behav 44:63–69
Spitzer RL, Williams JBW, Gibbon M, First MB (1990) Structured clinical interview for DSM-III-R-non-patient edition (SCID-NP, Version 1.0). American Psychiatric, Washington, District of Columbia
Takada M, Terakawa N, Aono T, Kurachi K, Tsuji M, Matsumoto K (1984) Divergent effects of prolactin on 4-ene-5 alpha reductase activity and the production of C19-steroids from progesterone in immature rat ovary. J Steroid Biochem 20(2):657–661
Weiland NG (1992) Glutamic acid decarboxylase messenger ribonucleic acid is regulated by estradiol and progesterone in the hippocampus. Endocrinology 131(6):2697–2702
Zamani MR, Levy WB, Desmond NL (2004) Estradiol increases delayed, N-methyl-d-aspartate receptor-mediated excitation in the hippocampal CA1 region. Neuroscience 129(1):243–254
Acknowledgements
The authors gratefully acknowledge the Ethel F. Donaghue Foundation for Medical Research for its generous support of this study. Additional support was provided by a Mentored Patient-Oriented Career Development Award (K23-MH1830; CNE), Independent Investigator Career Award (K02-MH73090; CNE), Investigator Award (RO1-MH64845; CNE) and the Dana Foundation (CNE); K05 AA014715-01 (JHK), P50 AA-12870-05 (JHK), Yale General Clinical Research Center (M01RR06022), and the Support from the State of Connecticut for the Abraham Ribicoff Research Facilities.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Epperson, C.N., Gueorguieva, R., Czarkowski, K.A. et al. Preliminary evidence of reduced occipital GABA concentrations in puerperal women: a 1H-MRS study. Psychopharmacology 186, 425–433 (2006). https://doi.org/10.1007/s00213-006-0313-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-006-0313-7