Abstract
Purpose of Review
Mindfulness therapy is a widely used treatment for many diseases and has been shown to improve pain-related functions. There is growing support for the use of psychotherapy in the treatment of chronic pain. While studies have shown a positive effect of mindfulness therapy, it is important to consider psychosocial factors as there are still a small number of studies that question its effectiveness.
Recent Findings
Based on current studies, mindfulness therapy involves cognitive factors related to chronic pain, both in terms of cognitive production and its impact on cognitive control. Psychological and neurobasic studies were reviewed to provide a deeper understanding of these components, which include thought inhibition, attention deficit, pain catastrophizing, and self-efficacy. Mindfulness therapy has the potential to normalize psychology and nerves, and increase internal and external connectivity to work networks related to stress perception, cognition, and emotion. However, further research is needed to fully understand its effects. By exploring the relationship between mindfulness therapy and chronic pain.
Summary
This review provides a new avenue for future research in psychotherapy for patients with chronic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic Pain (CP) is defined by the International Assoiciation for the Study of Pain as pain that lasts more than three months and is associated with actual or potential soft-tissue injury. It is considered the fifth vital sign after body temperature, breathing, pulse, and blood pressure [1,2,3]. Reports indicated a global incidence of CP as high as 31%, with women being affected more than men, which can seriously impact their quality of life [4]. Medication is currently the primary treatment for CP [5]. However, they are insufficient in restoring normal physical and mental functions and may cause neurological dysfunction as well as other side effects. Therefore, social and psychological factors should be considered in the treatment of CP, and corresponding psychotherapy should be administered based on individual psychological conditions.
Mindfulness therapy (MT) is represented in psychotherapy and has sufficient randomized controlled trial evidence [6]. As research on MT deepens, it is increasingly being used to treat a range of deseases, including depression, acromegaly, and even CP(7–8). The efficacy of MT in published studies remains controversial due to the neglect of cognitive differences. This review analyses the cognitive structure and its influencing factors to find out the reasons for the disparities. It also examines the mechanism of MT treatment of CP and analyses the relationship between the two to provide new ideas for the clinical treatment of CP from a psychological perspective.
Relationship Between Mindfulness Therapy and Cognition
It has been shown that MT contributes to the sense of well-being and quality of life. To achieve high levels of mindfulness, it is important to maintain a general orientation towards objective information and avoid subjective evaluations. Mindfulness is the ability of individual to focus their attention on their thoughts, emotions, and experiences while remaining fully aware and conscious of them. MT is primarily based on mindfulness-based stress reduction(MBSR). MBSR requires individuals to be self-aware, accept and focus on the present moment, refrain from making judgments based on their experiences, and maintain a compassionate attitude in their daily practice. To cater to specific population, MBSR has been modified into various forms such as mindfulness-based cognitive therapy, mindfulness-based relapse prevention, and mindfulness-based stress reduction [9]. These adaptations aim to address the unique needs of different population. The main forms of MT are cognitive therapy, relapse prevention, and relationship enhancement, including exercises in sensory, emotional, and respiratory mindfulness, which can help individuals cultivate and enhance positive thoughts [10,11,12]. We will analyze the causes of cognitive differences among individuals in terms of the order of thinking, way of attentional focus, and levels of negative emotions and experiences [13].
Variances in the Order of Thinking Produce Cognitive Differences
The use of language and words is central to the coalescence of complex information into a succinct foundation of thought. Different combinations of language can result in cognitive differences. The thought-language hypothesis has been proposed by Folder that the mind constructs complex ideas and expresses them by recombining the internal language of symbols [14]. Even simple ideas require the activation of various brain networks working together. Research by Frankland et al [15] has revealed the important role of the Default Mode Network (DMN) of the brain in idea generation and comprehension. DMN is a brain network structure comprised of the prefrontal cortex (PFC), posterior cingulate cortex (PCC) and angular gyrus. It is activated when an individual attempts to comprehend a thought and collaborates with the brain to gather and articulate the necessary information for the thought. This information is then conveyed between individuals through natural language [16]. Natural language is the input and output system for information. When information is input, the brain constructs a mental model for the individual to identify the input information and stimulate mental activities and thoughts(17–18). Simultaneously, the brain processes information and produces output, which subsequently impacts the development of behavior and cognitive system of individuals. However, the sequencing of thoughts can differ among individuals, leading to variations in behavior and cognition [19].
Variances in Attentional Focus Produce Cognitive Differences
Attention is a crucial element of cognitive structure(20). It is divided into selective, sustained, and dispersed types. Its essence lies in concentration, which enables individuals to selectively process information and exclude irrelevant information in various environments. This improves the efficiency of individual behaviors and gradually forms a fixed pattern that is retained in memory [20,21,22]. Shomstein et al [23] states that attention is achieved through a top-down signal transmission process. This process is realized by projecting information through the posterior parietal cortex (PPC) and activating cortical or subcortical regions such as the superior frontal and inferior parietal lobes to generate attention. Under high pressure, the regions mentioned above will be activated, causing the brain to overemphasize the target and increase attention, thereby enhancing the ability of the DMN to encode information and improve memory efficiency(24–25). Two studies on the attentional blink have shown that individuals report different orders of stimuli in memory when presented with the same visual stimuli frequently. This is due to the different cognitive and emotional stimuli given to them, indicating that attention is equally influenced by cognition and emotion(26–27).
Varying Levels of Negativity Produce Cognitive Differences
Emotions can affect both peripheral and neurological modes of perception and interpretation [28]. The mechanisms behind their generation are often explained through emotional filtering process, which involves the processing of natural language after the initial filtering of emotional information through attention and storing the processed information is ultimately stored in memory(29–28). Memory of Humans and animals store six basic emotions: happiness, sadness, anger, disgust, surprise, and fear. These emotions are expressed consistently across cultures and races, and individuals can discern them through various information, such as facial expressions, language, and body movements(30–31). The Inner Canon of Huangdi recorded that emotional stability is crucial for promoting mental health and quality of life. Negative emotions, which may be due to stress and illness, can affect mental health, as well as judgment and decision-making [32].
The activation of anterolateral regions, including the prefrontal lobes in the brain, is associated with positive emotions and personality. Due to the neuroplastic nature of these regions, they can be trained to improve functionality. Mindfulness-based meditation can have a positive effect on left anterior activation and long-term meditation can enhance the positive effects as well as reduce negative effects such as anxiety brought about from this region. The study found that the effect spilled over into immune function, with activation of the left anterior part of the brain leading to a faster rise in antibody titres in individuals [33]. Enhanced memory training mitigates negative emotions in depressed individuals, and highly cognitive individuals experiencing stressful events are less affected by negative emotions and decision making [34].
Variances in Experience Produce Differences in Perception
Experiences are patterns of cognitive behavior developed during social participation that can influence mental health [35]. Social participation includes events in which individuals engage with family, friends, peers, and other members of society [36]. Individuals may experience various negative events, such as illness, failure, property crises, and other experiences that can impact their levels of anxiety, depression, and overall life satisfaction [37]. Simultaneously, these experiences form memories and influence cognitive abilities. Surveys indicate that cultural and experiential disparities lead to seniors in the United States and Japan reporting greater disparities in recalling significant events throughout their lives, and exhibiting diverse personality traits and cognitive levels [38]. According to a study [39], exposure to adverse experiences and chronic stressful events may reduce the life goals and cognitive flexibility of children.
Cognitive flexibility develops gradually during childhood and adolescence, determining ability of individuals to adapt to environmental contingencies. Therefore, researching intracerebral networks has become a breakthrough point in modulating cognitive flexibility [40]. Research has shown that the joint participation of the distribution network of frontal-parietal regions, such as PFC, anterior cingulate cortex (ACC), PPC, and insula, regulates cognitive flexibility. This network also supports the attention generation and persistence. Thus, experiencing CP not only affects cognitive flexibility but also impacts attention [41, 42].
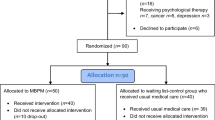
Although it has been shown that MT can improve cognition and mindfulness, the controversy surrounding the effectiveness of clinical studies on MT is due to differences in various population. Individuals disparities can affectt the way DMN processes information, which can influence the development of individual thought and cognitive behavioral systems, ultimately affect attentional focus patterns. Therefore, it is significant for MT studies need to use similar population to avoid biased results caused by significant disparities. Figure 1 illustrates the interdependence of attention, emotion, and experience in determining cognitive ability of individuals. Cognitive flexibility develops gradually during childhood and can be enhanced through specific training. In addition to attention, cognitive flexibility is also influenced by the level of cognitive processing and positive thoughts.
Mechanisms of mindfulness therapy for chronic pain. The management of chronic pain encompasses various components that specifically target pain symptoms, including the adjustment of cognitive patterns, perception of stress, secretion of cortisol, and enhancement of connectivity within relevant neural networks. Each of these mechanisms independently regulates the experience of pain. Therefore, mindfulness therapy possesses the capability to engage multiple regulatory systems for direct alleviation of chronic pain
Relationship between Chronic Pain and Cognition
CP is typically evaluated through self-perception of patient and related questionnaires, as it cannot be directly detected. Zhu et al [43] discovered that individuals with CP experienced more fatigue, higher stress levels, and lower levels of mindfulness. The statement suggests that the brain will automatically adjusts to ‘low energy consumption’ modes of response when receiving pain information. The negative stress and emotions induced in these modes will increase pain catastrophizing, decrease self-efficacy, and heighten perception of CP.
Strategies to Cope with Chronic Pain
Thought Suppression
When the CP information is inputted into the DMN to eliminate subjective pain perception, the DMN produces the thought ‘do not want the pain’. This phenomenon can lead to an increase in ‘unwanted’ thought, the cognition then continues to emphasize the thought and blindly retrieve it from memory, and the cognition continues to emphasize the thought and blindly retrieve it from memory. However, the suppression eventually seases, leading to a ‘rebound effect’, this effect provides the foundation for the development of phobic support [44].
The sensation of fear is regulated by the connections between the amygdala and key areas of PFC, specifically the ACC and orbitofrontal cortex. These areas are associated with thought inhibition. The networks of brain passively engage in thought suppression after receiving information about pain, resulting in effects that contradict their initial purpose. This phenomenon is explained by the environmental cues hypothesis. Based on this hypothesis, the brain automatically emphazies the ‘unwanted’ thought and searches for distracting information in memory and the environment. This can cause the thought to reappear in the mind and become linked with distractions, thereby increasing the risk of stress and disease recurrence [45]. In addition, individuals with higher levels of mindfulness tend to suppress their thoughts less. It is inmportant to note that the theories of yhought suppression and attentional bias have similarities [46].
Attentional Bias
Maladaptive attentional bias is a passive process, similar to thought suppression, where the focus is on the CP, resulting in a response that reduces the perceived threat of pain. The focus on the pain is intrusive, leading to cognitive interference that increases fear and avoidance [47]. Research indicates that individuals with a higher cognitive load and attentional bias experience lower pain perception compared to those with a lower cognitive load. This is because attentional processing influences pain-related brain nerves [48]. Thus, the brain receives information about pain at the expense of other stimuli and allocates attention preferentially to pain-related stimuli. This prompts individuals with chronic pain to focus more on their pain, as it increases cognitive conformity and enhances individual pain perception.
Unlike thought suppression, attentional bias can be used to reduce pain perception. Braithwaite et al [49] found that attentional bias and reframing of positive memories reduced the intensity of pain and fear reported by participants. Previous research has shown that deficient attentional processing and negative physical threat-related interpretations have a significant cumulative impact on self-reported pain and pain-related worries/disasters. On the other hand, enhanced attention is the basis for improved cognitive functioning, and inadequate attentional allocation results in cognitive bias [50]. Cognitive biases may trigger catastrophic thoughts and emotions, which can exacerbate the experience of pain and lead to further catastrophic thoughts [49].
Effect of Chronic Pain on Cognition
Pain Catastrophizing
CP research often describes an individual’s psychological response to pain in terms of three constructs related to cognitive appraisal of pain: self-efficacy, catastrophizing, and fear avoidance [51]. Most studies suggest that pain catastrophizing is a form of extreme worry that exacerbates the negative effects of pathologizing concerns. It is characterized by a tendency to magnify the threat value of the painful stimulus, a feeling of helplessness and apprehension in the context of pain, and an inability to inhibit pain-related thoughts during the painful event [52]. Episodes of pain catastrophizing can lead to an increase in pain perception, which is unrelated to negative emotions. Furthermore, the induction of negative emotions can lead to a dysfunction in pain perception, resulting in an increase in the perceived intensity of pain [53]. Therefore, an increase in catastrophizing may lead to more intense pain, higher levels of fear avoidance, and stronger cognitive interference.
Pain catastrophizing and pain-related fear are partially overlapping constructs. The fear component of catastrophizing may cause individuals to prioritize information about pain-related stimuli, resulting in attentional bias. For instance, if an individual believes that thinking about and analyzing their pain or emotions will help to resolve, cope with, or prevent the pain, they may engage in overthinking that exacerbates pain catastrophizing [54]. Rabinowitz et al [55] observed that PFC is the brain region associated with catastrophizing. This region is involved in executive control aspects related to emotional and cognitive pain processing. A reduced ability to distract from pain or hypervigilance to painful stimuli may also interfere directly with cognitive performance by taking away attentional resources needed for effective cognitive processing. The PPC in the brain has a wider role in attentional focusing. It regulates the dynamic interactions between the DMN and the hetero-modal cognitive control and attention networks [56]. Pain catastrophizing can lead to negative attitudes such as fear, avoidance, anxiety, and depression. This is often caused by experiences of psychological injury, worsening pain, and social harm, which can interfere with cognition [57].
Self-Efficacy for Pain
Both pain self-efficacy and pain catastrophizing are significant factors in the experience of individuals coping with common pain conditions such as arthritis and cancer [58]. Self-efficacy refers to confidence of an individual in their ability to manage pain. CP can reduce self-efficacy over time due to coping mechanisms such as thought suppression and attentional bias. These mechanisms can promote higher levels of catastrophizing, undermine confidence of individuals in their ability to manage pain, and lead to lower levels of cognition as well as maladaptive behaviors. Research has shown that self-efficacy is negatively correlated with fear of pain and exercise avoidance. Combining educational and exercise interventions can improve self-efficacy in athletes, and reduce fear and avoidance beliefs, and enhance cognitive abilities. Early cognitive training involves multiple cognitive domains can also enhance self-efficacy, cognitive abilities, and positive emotions in seniors(59–60).
Pain Intensity is Influenced by Emotions
Individuals with CP exhibit reduced cognitive abilities compared to those without condition, these changes are influenced by emotional factors related to CP rather than the pain itself [61]. Individuals with chronic pain often experience a significant emotional burden, including feelings of self-blame, guilt, and anxiety. This can make it difficult for them to focus on learning about their condition and effectively managing their rehabilitation [62].
The relationship between emotions and pain is reciprocal. Pain can guide emotions, while emotions can also guide pain perception. According to Christiansen et al., emotions can be beneficial when they appropriately guide sensory processing, enhance decision-making abilities, or provide information about the best course of action. However, they can be potentially harmful when the intensity, duration, frequency, or type of emotion is inappropriate for a given situation [63]. The brain encodes input information and triggers emotions through the decision-making ability, sensory processing, and situational factors. In the case of painful stimuli, the brain determines the intensity and duration of the pain and triggers associated emotions, leading to varying levels of anxiety and depression. It is important to maintain objectivity and avoid subjective evaluations.
Pain Perception is Influenced by Stress
Not only emotions, but also stress and pain are closely related. Healthy individuals exposed to acute stress tend to show a decrease in pain perception and an increase in pain tolerance. This phenomenon is known as stress-induced analgesia. However, in patients with chronic pain, stress directly increases pain perception. Previous studies have suggested a positive correlation between stress perception and pressure receptor activation. However, recent research has contradicted this [64].
Pressure receptors are mechanosensitive elements of the peripheral nervous system that help maintain homeostasis in the body. They coordinate the physiological responses of the internal and external nervous systems. The transmission of signals through the vagus nerve and the glossopharyngeal nerve by pressure receptor afferent nerves has an inhibitory effect on pain perception [65]. However, pressure can directly affect the transmission rate of signaling substances and inhibit the activation of pressure receptors, making it difficult for them to exert their homeostatic effect [66]. When an individual experiences pain, pressure receptors are activated, which in turn affect their heart rate, respiration, and blood pressure. The pressure receptors also transmit signals to areas such as the ACC, PFC, and amygdala. These areas work together to integrate the individual’s perception of injury, awareness, and cognition [67]. CP can impact pressure perception and disrupt the balancing effect of pressure receptors. Therefore, restoring signaling is an important mechanism to reduce stress perception and improve an individual’s level of mindfulness.
Mechanisms of Mindfulness Therapy for Chronic Pain
Psychological Mechanisms of Mindfulness Therapy for the Treatment of Chronic Pain
Mindfulness Therapy Reduces Stress Perception to Treat Chronic Pain
Research has shown that pain resulting from trauma, musculoskeletal disorders, or other illnesses can be distressing to individuals. Conversely, exercise that results in muscle soreness can enhance individual well-being [68]. The higher incidence of CP in women may be due to gender disparities in how individuals react to stressful events. Men are usually more sensitive to work-related stress, while women are more susceptible to life-related stress(69–70). Furthermore, stress is a known factor in the development of CP [71].
A study has shown that MT intervention can decrease subjective stress perception and enhance well-being [72]. MT is characterized by two features: grounding attention and perception in the present moment, and openness and acceptance of experience of their own [73]. The former is a behavioral approach that trains skills to reduce an individual’s primary threatening and negative emotional responses to everyday stressors. The latter is a cognitive approach that improves attitudes towards the self to reduce evaluative and judgmental narratives about the individual’s experiences, i.e. judgemental behavior/thinking. After completing mindfulness training, an individual’s non-judgmental behaviors, thoughts, and cognitions are likely to increase, leading to a reduction in stress caused by judgment and overthinking [74]. This hugh level of cognitive function not only reduces the perception of stress but also restores the balancing effect of stress receptors.
Positive Thought Therapy Adjusts Cognitive Patterns to Treat Chronic Pain
Individuals with CP typically exhibit stimulus-dependent pain responses. However, individuals who engage in long-term meditation do not display such responses. Wielgosz et al [75] hypothesized that during orthostatic training involves a gradual shift from sensory to cognitive pain modulation. They suggest that this transition may be related to changes in pain catastrophizing of individuals, and that this gradual transition from a sensory to a cognitive modulation pattern may be related to changes in pain catastrophizing of individuals. The change in the pattern could be attributed to the fact that MT improves control over pain perception of individuals. MT requires individuals to confront and accept the sensations brought about by pain and to restructure their cognitive processes and content of pain catastrophizing [76].
During the transition period, the shift to cognitive conditioning causes an attentional shift that disrupts the normal cognitive structure. According to Day et al., observing brain waves showed that MT reduces the beta band of deteriorating cognition and behavior, making the individual’s attention more focused and flexible [77]. Another study shown that emotion, as a cognitive factor, can significantly impact pain perception [78]. Positive beliefs and expectations conveyed by MT can improve pain threshold and tolerance of individuals. MT interventions, such as positive thought meditation, provide individuals with complete attentional control, enhancing cognitive control and thoughts. Anxiety states and negative affect are linked to attentional control. MT increases theta-wave power, which has direct benefits not only for anxiety states but also for negative states such as anger and depression that trigger thought suppression [79]. Therefore, MT can alter pain perception of individuals by communicating positive beliefs and expectations, modulating attention, and reducing catastrophizing and related emotions.
Cellular Molecular Mechanisms of Mindfulness Therapy for the Treatment of Chronic Pain
Mindfulness Therapy Reduces Cortisol Secretion to Treat Pain
A study indicates that MT may decrease the perception of stress by effectively reducing cortisol secretion [80]. Pain amplifies stress perception in individuals experiencing chronic pain, making it challenging to maintain a positive emotional state [81]. This amplification not only originates from the body, but CP also affects the pituitary gland and hypothalamus with abnormal signaling, generating more mental stress [82].
Excessive stress leads to increased in cortisol production in the brain. Cortisol has an anti-inflammatory effect by binding to the glucocorticoid receptor. Abnormal cortisol secretion decreases the compensatory properties of the receptor, rendering it unable to bind to cortisol properly. This disruption leads to prolonged pain persistence(83–84). CP can cause stress, which may lead to an abnormal physiological stress response and the persistence of pain.
The amygdala in the brain processes stressors by rapidly assigning emotional significance to events in the environment. It is beliThus, MT has a psychological impact on individuals by reducing the amount of cortisol secreted to alleviate the effects of perceived stress and achieve pain relief.eved to be involved in coordinating behavioral changes induced by stressors, particularly in unfavorable environmental conditions and stressors that negatively impact health [85].
Mindfulness Therapy Reduces Expression of Inflammatory Factors in the Treatment of Chronic Pain
In indivuduals with CP, MT not only affects cortisol secretion but also reduces the expression levels of IL-1β, IL-6, and TNF-α [86,87,88]. The increase of inflammatory factors by pain may be due to the activation of the amygdala in the brain when individuals are afraid of CP, which leads to the release of catecholamines from the brainstem, which in turn leads to the proliferation of inflammatory factors [89], whereas IL-1β and IL-6 are representative inflammatory factors that are widely used to detect inflammatory changes and to predict major depressive disorder [86, 90].
In individuals with depression, proliferation of inflammatory factor affects neurotransmitter synthesis, signaling, metabolism, and function. It also has a severe impact on the morphology of PFC and hippocampal regions of the brain and can influence mood circuits in the central nervous system [91]. In individuals with chronic pain, inflammatory factor proliferation also increases pain sensitivity, which accelerates the vicious cycle between stress, inflammation, and pain [92]. CP has been found to have a close association with depression and anxiety. This association leads to higher levels of inflammatory factors expression and lower cognitive performance among individuals with CP(93–94). Furthermore, inflammatory factor expression levels are closely associated with sarcopenia, which may explain the reparative effects of MT on skeletal muscle [84].
Mindfulness Therapy Repairs Soft Tissue for Chronic Pain
Musculoskeletal pain can have various causes, including injury, receptor sensitization, trigger point formation, and musculoskeletal transmission signals. Chronic stress can also contribute to the development of pain by increasing muscle tension and sensitivity, resulting in a startle reflex that perpetuates pain. These causal connections have been established in previous research(95–86). Cervical spondylosis is a musculoskeletal disorder that causes chronic neck pain. It has been reported to be associated with increased apoptosis in neck muscles and nerve cells [95]. Psychological studies have shown that individuals with CP may avoid exercise due to excessive attention paid to pain, which can lead to neglecting exercises aimed at improving muscle function, resulting in a vicious cycle of decreasing muscle function, stress, and anxiety(96–97). Thus, prioritising muscle exercises is a crucial component in the treatment of chronic pain. Yoga is a mind-body practice that promotes positive emotional, mental, and muscular functioning, and can improve muscle function in patients with CP [98]. Furthermore, Herbert et al [99] have shown that yoga can modulate respiratory rate, heart rate, and muscular exercises, which can help reduce stress perception.
Neurological Mechanisms in the Brain of Mindfulness Therapy for Chronic Pain
The Triple Network of the Brain Regulates Cognitive Levels
The brain’s Central Executive Network (CEN), DMN, and Salience Network (SN) work together to generate and regulate emotions, attention, and cognitive processes. These networks can be modified through training [6]. The DMN is thought to reflect various cognitive processes, such as situational memory retrieval, autobiographical memory, internal thinking, self-relevant and social cognitive processes, value-based decision-making, and emotion regulation. Its significant connections are with the hippocampus and the amygdala. SN is a brain system responsible for detecting, integrating, and filtering relevant internal perceptual, autonomic, and emotional information. Its pivotal nodes are located in the insulae of the ACC. The SN is centered on the dorsolateral prefrontal cortex (dlPFC) and the PPC. It modifies and monitors the state of CEN and DMN, and receives an allocation of attentional resources to support cognitive control and processes mentally demanding activities and working memory [100].
Mindfulness Therapy Regulates Nerves
Individuals with CP exhibit increased activity in several brain regions, including the dlPFC, vlPFC, orbitofrontal cortex, somatosensory cortex, amygdala, thalamus, and hippocampus. In contrast, healthy individuals show increased activation of the anterior cingulate cortex and anterior insular cortex, and decreased activation of the thalamus [101]. Pain is believed to be caused by injury receptors that transmit signals from the peripheral tissue to the dorsal horn of the spinal cord. This injurious information then travels to the brain on the opposite side of the pain site through the spinal thalamic pathway, with feedback connections between lower sensory regions playing a crucial role. The feedback connections involve brain regions such as the thalamus. Subsequently, harmful information is transmitted to the posterior insular cortex and the anterior insular cortex. These regions are further refined to activate the PFC, ACC, and other higher-order brain regions [102]. The PCC, ACC, PFC, and subcortical regions are all central sites for controlling attention, regulating emotion, and enhancing self-awareness.
MT modifies the central site, which includes the brain regions mentioned above. Changes in these brain regions and the amygdala are accompanied by functional and structural alterations in the brain. Ong et al [103] discovered that the PFC has a dual role in pain. On the one hand, it can mediate resistance to painful feelings through connections with other cortical areas. On the other hand, it participates in inducing chronic pain by suppressing impaired thoughts, behaviors, and emotions. Additionally, ACC is believed to be involved in both pain and emotional processing, becoming active when an individual directs their attention towards the site of the pain. The ACC and frontal insular cortex are also part of SN, which facilitates cognitive processes by linking brain regions that are far apart(104–105).
Research has shown that mindfulness-based art therapy (MBAT) can increase blood flow to specific areas of the brain, such as the insular cortex, amygdala, hippocampus, and striatum. Additionally, undergoing MBAT can lead to a decrease in activation of the ACC in response to stressors, indicating that MBAT may help regulate the stress response and anxiety levels [106]. MT improves functional connectivity and activates areas of the PFC, enhancing vigilance, visuospatial processing, working memory, and cognitive flexibility. The PCC and PFC are key regions of the DMN, which is overactivated in a negative state. The DMN can invade the CEN, affecting attentional control [107]. A study has shown that mindfulness-based cognitive therapy can alter connectivity and somato-motor networks in the dACC, alPFC, and anterior insula regions during depressive rumination. Furthermore, these brain regions can predict the response to psychotherapy for depression. Moreover, during the intervention, MT enhances the functional connectivity of the triadic network. It is important to note that the internal connectivity of the DMN is strongly correlated with the level of positive thoughts. Additionally, MT decreases the activation caused by noxious heat in the supplementary motor area, bilateral secondary somatosensory cortex/parietal lid, and posterior insula [108].
Therefore, it is suggested that MT may enhance ability of individuals to control pain perception by increasing the internal and external connectivity of the triple network model. It may also modulate the involvement of mental states such as stress, anxiety, depression, environmental CP and co-symptoms caused by CP. Furthermore, MT may help to train more efficient brain states with higher regulation of energy expenditure in the human brain, while also improving limited attention, cognitive control, and conscious processing.
Conclusion
This review describes the relationship between MT and CP and the mechanism study (Fig. 1). The impact of CP on cognition has been established, and while the use of MT as a therapy has gained widespread acceptance, there is still some controversy surrounding its effectiveness. This may be due to cognitive differences between different populations, and therefore, more high-quality clinical trials are needed to validate its efficacy in the future.
Cognitive testing and pain assessment both use questionnaires to evaluate cognitive levels. However, neurological studies rely on observing changes in brain area networks through techniques such as MR and EEG. Unfortunately, the use of different observation methods often leads to discrepancies in data between studies. Thus, it is necessary to establish a uniform method for validation and to reduce discrepancies when detecting pain and cognitive levels.
One advantage of MT is that operators can choose different forms based on the occurrence and causes of CP. However, MT should only be implemented by professional operators to avoid discrepancies caused by human factors. Therefore, researchers need to ensure uniform training and testing of MT operators.
Current research on the mechanisms of MT focuses on the neurological, psychological, and hormonal aspects of the brain that can impact cognition and behaviour. However, few studies have have considered cognitive differences when selecting experimental population. Future studies should aim to avoid population with significant cognitive disparities between individuals. At the same time, studies can compare the mechanism of medical treatment in different population to identify disparities and reasons for such variations. This can lead to the development of a rich, standardized, and unified theory. As the mechanism of medical treatment for diseases is still not completely understood, it is necessary to continue to strengthen relevant basic research.
Data Availability
The paper is a review, so no data availability is required.
References
Lv N, Lv ZF. Research progress of m ~ 6A modification in chronic pain[J]. Chin J Pain Med. 2023;29:528–34.
Dou XY, Liang C, Zhu B, et al. Progress of intrathecal drug delivery for chronic pain[J]. Chin J Pain Med. 2023;29:645–53.
Liao JB, Liu Miao, Wang WX, et al. Exploring ideas of chronic pain of traditional Chinese medicine about disease, pathogenesis, syndrome and treatment[J]. China J Traditional Chin Medine Pharm. 2018;33:1441–4.
Xu H, Zhou H, Zhou YF, et al. Research progress on brain center remodeling mechanism of Tuina based on fMRI technology in chronic pain[J]. China J Traditional Chin Medine Pharm. 2023;38:2762–5.
Wang F, Mao XH, Li CY, et al. Mediating effect of mental flexibility on health perception and quality of life in elderly patients with chronic pain[J]. Chin Nurs Res. 2021;28:51–5.
Bremer B, Wu Q, Mora Álvarez MG, et al. Mindfulness meditation increases default mode, salience, and central executive network connectivity. Sci Rep. 2022;12:13219.
Santos A, Nalin C, Bortolotti G, et al. The effect of mindfulness therapy in acromegaly, a pilot study. Clin Endocrinol (Oxf). 2023;98:363–74.
Hsu T, Forestell CA. Mindfulness, mood, and food: the mediating role of positive affect. Appetite. 2021;158:105001.
Valderrama Rodríguez MF, Sánchez-Sánchez LC, García-Montes JM, Petisco-Rodríguez C. A scoping review of the influence of mindfulness on men’s sexual activity. Int J Environ Res Public Health. 2023;20:3739.
Tsur N, Defrin R, Haller CS, Bercovitz K, Langer EJ. The effect of mindful attention training for pain modulation capacity: exploring the mindfulness-pain link. J Clin Psychol. 2021;77:896–909.
Murphy S, Donma AJ, Kohut SA, et al. Mindfulness practices for children and adolescents receiving Cancer therapies. J Pediatr Hematol Oncol Nurs. 2022;39:40–8.
Ameli R, Sinaii N, West CP, et al. Effect of a Brief Mindfulness-Based Program on Stress in Health Care Professionals at a US Biomedical Research Hospital: A Randomized Clinical Trial. JAMA Netw Open. 2020;3(8):e2013424.
Wells RE, O’Connell N, Pierce CR, et al. Effectiveness of Mindfulness Meditation vs Headache Education for adults with migraine: a Randomized Clinical Trial. JAMA Intern Med. 2021;181:317–28.
Romano S, Salles A, Amalric M, et al. Bayesian validation of grammar productions for the language of thought. PLoS ONE. 2018;13:e0200420.
Frankland SM, Greene JD. Concepts and compositionality: in search of the Brain’s Language of Thought. Annu Rev Psychol. 2020;71:273–303.
Tillas A. Language as grist to the mill of cognition. Cogn Process. 2015;16:219–43.
Jon-And A, Jonsson M, Lind J, Ghirlanda S, Enquist M. Sequence representation as an early step in the evolution of language. PLoS Comput Biol. 2023;19:e1011702.
Borghi AM, Fernyhough C. Concepts, abstractness and inner speech. Philos Trans R Soc Lond B Biol Sci. 2023;378:20210371.
Carruthers P. The cognitive functions of language. Behav Brain Sci. 2002;25:657–725.
Ben Azouz O, Dellagi L, Kebir O, et al. Le concept d’attention [The concept of attention]. Tunis Med. 2009;87:680–4.
McDowd JM. An overview of attention: behavior and brain. J Neurol Phys Ther. 2007;31:98–103.
Carlisle NB. Negative and positive templates: two forms of cued attentional control. Atten Percept Psychophys. 2023;85:585–95.
Shomstein S, Gottlieb J. Spatial and non-spatial aspects of visual attention: interactive cognitive mechanisms and neural underpinnings. Neuropsychologia. 2016;92:9–19.
Prull MW, Liu Y, Adhikari N, et al. Can divided attention at retrieval improve memory? Effects of target detection during recognition. Memory. 2023;31:573–87.
Beaudette DM, Gold JM, Waltz J, et al. Predicting attention-shaping response in people with Schizophrenia. J Nerv Ment Dis. 2021;209:203–7.
Snir G, Yeshurun Y. Perceptual episodes, temporal attention, and the role of cognitive control: lessons from the attentional blink. Prog Brain Res. 2017;236:53–73.
Ray SB, Mishra MV, Srinivasan N. Attentional blink with emotional faces depends on emotional expressions: a relative positive valence advantage. Cogn Emot. 2020;34:1226–45.
Kozubal M, Szuster A, Wielgopolan A. Emotional regulation strategies in daily life: the intensity of emotions and regulation choice. Front Psychol. 2023;14:1218694.
Morie KP, Crowley MJ, Mayes LC, et al. The process of emotion identification: considerations for psychiatric disorders. J Psychiatr Res. 2022;148:264–74.
Ruan K, Problems. The problems, risks and regulations of emotion Recognition Technology[J]. J Dialectics Nat. 2023;45:82–90.
Huang Ying L, Wei L, Jinquan, et al. Individual emotion recognition in open space based on multi-modal fusion[J]. J Comput Appl. 2022;42:36–41.
Chen XF, Zhang WJ, Li MM, et al. Correlation analysis of negative emotions and quality of life in patients with superficial bladder cancer after pirarubicin infusion[J]. Chin Nurs Res. 2023;37:3786–9.
Davidson RJ, Kabat-Zinn J, Schumacher J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65:564–70.
Liu F, Huo R, Han C, et al. The effects of executive function on individuals’ tendency to use emotion regulation strategies and regulation effects[J]. Stud Psychol Behav. 2022;20:382–9.
Konieczny P, Cierpiałkowska L. Positive and negative life experiences and changes in internal working models of attachment - a comparative study. Psychiatr Pol. 2022;56:551–70.
Zhao ZX, Mei YX, Wang XX et al. Cognition and experience of Social Participation in Stroke survivors: a Meta-synthesis based on qualitative Studies[J]. Chin Gen Pract:1–9.
Marum G, Clench-Aas J, Nes RB, et al. The relationship between negative life events, psychological distress and life satisfaction: a population-based study. Qual Life Res. 2014;23:601–11.
da Rosa G, Martin P, Gondo Y, et al. Examination of important life experiences of the oldest-old: cross-cultural comparisons of U.S. and Japanese centenarians. J Cross Cult Gerontol. 2014;29:109–30.
Bashir M, Majeed S. Childhood adverse experiences, cognitive flexibility and goal orientation in adolescents. J Pak Med Assoc. 2023;73:1884–6.
Cantwell A, Buckholtz JW, Atencia R, et al. The origins of cognitive flexibility in chimpanzees. Dev Sci. 2022;25:e13266.
Dajani DR, Uddin LQ. Demystifying cognitive flexibility: implications for clinical and developmental neuroscience. Trends Neurosci. 2015;38:571–8.
Spellman T, Svei M, Kaminsky J, Manzano-Nieves G, Liston C. Prefrontal deep projection neurons enable cognitive flexibility via persistent feedback monitoring. Cell. 2021;184(10):2750-2766.e17. *This study highlights the relationship between prefrontal cortex and cognitive flexibility and identifies a key role for prefrontal cortical projection neurons in monitoring shifted attentional sets through behavioural feedback.
Zhu Y, Sun F, Li C, Chow DHK. Acute effects of brief mindfulness intervention coupled with carbohydrate ingestion to Re-energize Soccer players: a randomized crossover trial. Int J Environ Res Public Health. 2020;17:9037.
Hooper N, Davies N, Davies L, McHugh L. Comparing thought suppression and mindfulness as coping techniques for spider fear. Conscious Cogn. 2011;20:1824–30.
Hooper N, Sandoz EK, Ashton J, Clarke A, McHugh L. Comparing thought suppression and acceptance as coping techniques for food cravings. Eat Behav. 2012;13:62–4.
Smith-Russell D, Bowen S. Mediating effects of Thought suppression in the relationship between mindfulness and substance use craving. Subst Use Misuse. 2023;58:1196–201.
Kreddig N, Hasenbring MI, Keogh E. Comparing the effects of Thought suppression and focused distraction on Pain-related attentional biases in men and women. J Pain. 2022;23:1958–72.
Wang K, Chen Y, Huang S, Liu H, Wu W. Attention Bias to Pain Words Comes Early and Cognitive Load Matters: Evidence from an ERP Study on Experimental Pain. Neural Plast. 2021:9940889.
Braithwaite FA, Noel M, Jones HG, et al. Reframe the pain: divided attention and positive memory reframing to reduce needle pain and distress in children-A feasibility randomized controlled trial. Eur J Pain. 2022;26:1702–22.
Kavallari D, Lau JYF. Testing a combined cognitive Bias Hypothesis of Pain and Pain-related worry in Young people. J Pain. 2022;23:1082–91.
Marshall A, Joyce CT, Tseng B, et al. Changes in Pain Self-Efficacy, coping skills, and fear-avoidance beliefs in a Randomized Controlled Trial of yoga, physical therapy, and Education for Chronic Low Back Pain. Pain Med. 2022;23:834–43.
Petrini L, Arendt-Nielsen L. Understanding Pain Catastrophizing: putting Pieces together. Front Psychol. 2020;11:603420.
Goli Z, Asghari A, Moradi A. Effects of Mood induction on the Pain responses in patients with migraine and the role of Pain Catastrophizing. Clin Psychol Psychother. 2016;23:66–76.
Schütze R, Rees C, Smith A, Slater H, O’Sullivan P. Metacognition, perseverative thinking, and pain catastrophizing: a moderated-mediation analysis. Eur J Pain. 2020;24:223–33.
Rabinowitz EP, Sayer MA, Delahanty DL. The role of catastrophizing in chronic cyclical pelvic pain: a systematic review and meta-analysis. Womens Health (Lond). 2023;19:17455057231199949.
ark E, Park JW, Kim E, et al. Effects of alterations in resting-state neural networks on the Severity of Neuropathic Pain after spinal cord Injury. Bioeng (Basel). 2023;10:860.
Fonseca das Neves J, Kornacka M, Serra E, et al. The impact of rumination on fibromyalgia pain after physical activity: an experimental study. Sci Rep. 2023;13:20523.
Fisher HM, Stalls J, Winger JG, et al. Role of self-efficacy for pain management and pain catastrophizing in the relationship between pain severity and depressive symptoms in women with breast cancer and pain. J Psychosoc Oncol. 2023;41:87–103.
Moraes ÉB, Martins Junior FF, Silva LBD, et al. Self-efficacy and fear of pain to movement in chronic low back pain: an intervention developed by nurses. Rev Gaucha Enferm. 2021;42:e20200180.
Lee J, Cho E, Kim H, Lee KH, Kim E, Ye BS. The development and evaluation of a self-efficacy enhancement program for older adults with mild cognitive impairment. Appl Nurs Res. 2023;73:151726.
Javdaneh N, Saeterbakken AH, Shams A, Barati AH. Pain Neuroscience Education Combined with Therapeutic exercises provides added benefit in the treatment of chronic Neck Pain. Int J Environ Res Public Health. 2021;18:8848.
Li N, Ni CC,Ni G. Investigation on KAP current status in elderly patients with cervical spondylosis and its correlation with social support and self-perceived burden[J]. J Cervicodynia Lumbodynia. 2023;44:726–30.
Christiansen H, Hirsch O, Albrecht B, et al. Attention-Deficit/Hyperactivity disorder (ADHD) and emotion regulation over the Life Span. Curr Psychiatry Rep. 2019;21:17.
al’Absi M, Nakajima M, Bruehl S. Stress and pain: modality-specific opioid mediation of stress-induced analgesia. J Neural Transm (Vienna). 2021;128:1397–407.
Keller M, Pelz H, Müller G, et al. Autonomic nervous system responses in the intermediate band to cranial cutaneous stimulation. Physiol Rep. 2024;12:e15891.
Dabbagh A, Horn U, Kaptan M et al. Reliability of task-based fMRI in the dorsal horn of the human spinal cord. Preprint bioRxiv, 2023; 572825.
Suarez-Roca H, Mamoun N, Sigurdson MI, Maixner W. Baroreceptor Modulation of the Cardiovascular System, Pain, consciousness, and Cognition. Compr Physiol. 2021;11:1373–423.
Lera-López F, Ollo-López A, Sánchez-Santos JM. Is Passive Sport Engagement positively Associated with Happiness? Appl Psychol Health Well Being. 2021;13:195–218.
Shields GS, Trainor BC, Lam JC, et al. Acute stress impairs cognitive flexibility in men, not women. Stress. 2016;19:542–6.
Dadomo H, Gioiosa L, Cigalotti J, et al. What is stressful for females? Differential effects of unpredictable environmental or social stress in CD1 female mice. Horm Behav. 2018;98:22–32.
Miró J, Sánchez-Rodríguez E, Nolla MC, et al. The Role of Resilience, Happiness, and Social Support in the Psychological Function during the Late Stages of the Lockdown in Individuals with and without Chronic Pain. Int J Environ Res Public Health. 2022;19(11):6708. *This study highlights significant differences in psychosocial factors in patients with chronic pain.
Łoś K, Chmielewski J, Cebula G, et al. Relationship between mindfulness, stress, and performance in medical students in pediatric emergency simulations. GMS J Med Educ. 2021;38:Doc78.
Majeed MH, Ali AA, Sudak DM. Mindfulness-based interventions for chronic pain: evidence and applications. Asian J Psychiatr. 2018;32:79–83.
Chin B, Lindsay EK, Greco CM, et al. Psychological mechanisms driving stress resilience in mindfulness training: a randomized controlled trial. Health Psychol. 2019;38:759–68.
Wielgosz J, Kral TRA, Perlman DM, et al. Neural signatures of pain modulation in short-term and long-term mindfulness training: a randomized active-control trial. Am J Psychiatry. 2022;179(10):767.
Day MA, Ward LC, Thorn BE, et al. Mechanisms of Mindfulness Meditation, cognitive therapy, and mindfulness-based Cognitive Therapy for Chronic Low Back Pain. Clin J Pain. 2020;36:740–9.
Day MA, Matthews N, Mattingley JB, et al. Change in Brain oscillations as a mechanism of Mindfulness-Meditation, cognitive therapy, and mindfulness-based cognitive therapy for chronic low back Pain. Pain Med. 2021;22:1804–13.
Davies JN, Sharpe L, Day MA, Colagiuri B. How do placebo effects contribute to mindfulness-based analgesia? Probing acute pain effects and interactions using a randomized balanced placebo design. Pain. 2022;163:1967–77.
Nien JT, Gill DL, Chou TY, et al. Effect of brief mindfulness and relaxation inductions on anxiety, affect and brain activation in athletes. Psychol Sport Exerc. 2023;67:102422.
Gherardi-Donato ECDS, Gimenez LBH, Fernandes MNF, et al. Mindfulness practice reduces hair cortisol, anxiety and perceived stress in University workers: Randomized Clinical Trial. Healthc (Basel). 2023;11:2875.
Pinto AM, Geenen R, Wager TD, et al. Emotion regulation and the salience network: a hypothetical integrative model of fibromyalgia. Nat Rev Rheumatol. 2023;19:44–60.
Wippert PM, Wiebking C. Stress and alterations in the Pain Matrix: a Biopsychosocial Perspective on Back Pain and its Prevention and Treatment. Int J Environ Res Public Health. 2018;15:785.
Yang N, Ray DW, Matthews LC. Current concepts in glucocorticoid resistance. Steroids. 2012;77:1041–9.
Hannibal KE, Bishop MD. Chronic stress, cortisol dysfunction, and pain: a psychoneuroendocrine rationale for stress management in pain rehabilitation. Phys Ther. 2014;94:1816–25.
González-Palau F, Medrano LA. A mini-review of work stress and mindfulness: a neuropsychological point of View. Front Psychol. 2022;13:854204.
Marinovic DA, Hunter RL. Examining the interrelationships between mindfulness-based interventions, depression, inflammation, and cancer survival. CA Cancer J Clin. 2022;72:490–502.
Diez GG, Anitua E, Castellanos N, Vázquez C, et al. The effect of mindfulness on the inflammatory, psychological and biomechanical domains of adult patients with low back pain: a randomized controlled clinical trial. PLoS ONE. 2022;17:e0276734. This study highlights evidence from randomised controlled trial that mindfulness therapy for the treatment of chronic pain has benign effects on the body and mind.
Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: systematic review and meta-analysis. J Psychiatr Res. 2017;95:156–78.
Beckers T, Krypotos AM, Boddez Y, Effting M, Kindt M. What’s wrong with fear conditioning? Biol Psychol. 2013;92:90–6.
Rostami S, Alyasin A, Saedi M, et al. Astaxanthin ameliorates inflammation, oxidative stress, and reproductive outcomes in endometriosis patients undergoing assisted reproduction: a randomized, triple-blind placebo-controlled clinical trial. Front Endocrinol (Lausanne). 2023;14:1144323.
Roohi E, Jaafari N, Hashemian F. On inflammatory hypothesis of depression: what is the role of IL-6 in the middle of the chaos? J Neuroinflammation. 2021;18:45.
Dupont J, Vercauteren L, Amini N, et al. Are inflammatory markers associated with sarcopenia-related traits in older adults with Sarcopenia? - a cross-sectional analysis of the ENHANce study. Exp Gerontol. 2023;178:112196.
Liu F, Fang T, Zhou F, et al. Association of depression/anxiety symptoms with neck pain: a systematic review and meta-analysis of literature in China. Pain Res Manag. 2018;2018:3259431.
Nowak KL, Hung A, Ikizler TA, et al. Interleukin-1 inhibition, chronic kidney disease-mineral and bone disorder, and physical function. Clin Nephrol. 2017;88:132–43.
Zhu, Meiling, Liu Hongchen. Peripheral mechanisms of chronic pain in temporomandibular joint and related muscles. Chin J Stomatol 2001:80–1.
Liu FFTH, Tao, et al. Effects of acupotomy therapy on PI3K/Akt signaling pathway of posterior cervical extensor muscles cells in cervical spondylosis rabbits[J]. China J Traditional Chin Medine Pharm. 2020;35:918–22.
Crombez G, Veirman E, Van Ryckeghem D, Scott W, De Paepe A. The effect of psychological factors on pain outcomes: lessons learned for the next generation of research. Pain Rep. 2023;8(6):e1112.
Neumark-Sztainer D, Wall MM, Levine A, et al. Yoga practice among ethnically/racially diverse emerging adults: associations with body image, mindful and disordered eating, and muscle-enhancing behaviors. Int J Eat Disord. 2021;54:376–87.
Herbert C. Can yoga Boost Access to the Bodily and Emotional Self? Changes in Heart Rate Variability and in affective evaluation before, during and after a single Session of yoga Exercise with and without instructions of controlled breathing and mindful body awareness in Young Healthy women. Front Psychol. 2021;12:731645.
Raffone A, Marzetti L, Del Gratta C, et al. Toward a brain theory of meditation. Prog Brain Res. 2019;244:207–32.
Nascimento SS, Oliveira LR, DeSantana JM. Correlations between brain changes and pain management after cognitive and meditative therapies: a systematic review of neuroimaging studies. Complement Ther Med. 2018;39:137–45.
Jinich-Diamant A, Garland E, Baumgartner J, et al. Neurophysiological mechanisms supporting mindfulness meditation-based Pain Relief: an updated review. Curr Pain Headache Rep. 2020;24:56.
Ong WY, Stohler CS, Herr DR. Role of the Prefrontal Cortex in Pain Processing. Mol Neurobiol. 2019;56:1137–66.
Zhang S, Li T, Kobinata H, et al. Attenuation of offset analgesia is associated with suppression of descending pain modulatory and reward systems in patients with chronic pain. Mol Pain. 2018;14:1744806918767512.
Tang YY, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16:213–25.
Beerse ME, Van Lith T, Pickett SM, et al. Biobehavioral utility of mindfulness-based art therapy: neurobiological underpinnings and mental health impacts. Exp Biol Med (Maywood). 2020;245:122–30.
Rathore M, Verma M, Nirwan M, Trivedi S, Pai V. Functional Connectivity of Prefrontal Cortex in various meditation techniques - a Mini-review. Int J Yoga. 2022;15:187–94.
van der Velden AM, Scholl J, Elmholdt EM, et al. Mindfulness training changes Brain Dynamics during Depressive Rumination: a Randomized Controlled Trial. Biol Psychiatry. 2023;93:233–42.
Acknowledgements
We thank the research participants for their contributions to this review.
Funding
National Natural Science Foundation of China (82360940); Natural Science Foundation of Jiangxi Province of China (20224ACB206041); Educational Commission of Jiangxi Province of China (GJJ211206, GJJ22000984, GJJ2200990).
Author information
Authors and Affiliations
Contributions
B and K contributed to the writing and examination of the manuscript, T, C and W jointly organized and drew Fig. 1, J and Y organized the retrieved data and classified it, F proposed the topic, and all authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Consent for Publication
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Biao, D., Umoh, K., Qiguang, C. et al. The Role of Mindfulness Therapy in the Treatment of Chronic Pain. Curr Pain Headache Rep (2024). https://doi.org/10.1007/s11916-024-01284-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s11916-024-01284-w