Abstract
Purpose of Review
Nerve blocks constitute an integral portion in the management of chronic pain. The widespread use of ultrasound imaging opened the door to a flood of newer blocks especially truncal plane nerve blocks. We reviewed the current medical literature for studies and case reports utilizing the two most common truncal plane nerve blocks, transversus abdominis plane and erector spinae plane blocks, to manage chronic pain.
Recent Findings
We found some evidence, mostly in case reports and retrospective observational studies, that supports the use of transversus abdominis plane and erector spinae plane nerve blocks, usually with steroids, as a safe and valuable part of interdisciplinary management of chronic abdominal and chest walls pain.
Summary
Ultrasound-guided truncal fascial plane nerve blocks are safe, easy to learn, and proven to help with post-operative acute pain management. Although limited, our current review provides evidence from the current medical literature regarding the utility of these blocks to manage some of the challenging chronic and cancer-related pain conditions of the trunk region.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of nerve blocks is an integral part of the multidisciplinary management of chronic pain. These blocks are usually performed as diagnostic and/or therapeutic with local anesthetics (with or without steroids). They are frequently followed by a denervation procedure, such as radiofrequency ablation, to achieve a longer period of pain relief. The advancement and the widespread use of ultrasound imaging for regional anesthesia have led to a massive increase in the use of truncal plane blocks such as transversus abdominis plane (TAP) and erector spine plane (ESP) blocks. The utilization of these blocks to treat chronic pain has been expanding with some good outcomes; however, it is still controversial among pain physicians, and many are skeptical regarding the use of these blocks for chronic pain management. Fascial plane nerve blocks usually target more than one nerve traveling at the same plane; therefore, the use of denervation techniques targeting specific nerve(s) to prolong the duration of the pain relief is not an option. However, clinical experience and some studies have shown that even nerve blocks with local anesthetics may provide a long-lasting pain relief for chronic pain patients. In this narrative review, we evaluated the available evidence in the current medical literature regarding the use of TAP and ESP blocks to treat chronic and cancer-related pain conditions.
Truncal Fascial Plane Nerve Blocks
History, Anatomy, and Techniques
Carl Schleich described what became the rectus sheath block with the use of local anesthetic infiltration to relax the abdominal wall in 1899 [1, 2]. In 2001, Rafi et al. [3] described a new technique that utilizes a single “pop” or loss of resistance over the lumbar triangle of Petit to anesthetize one side of the abdominal wall. Later on, McDonnel et al. [4] advanced upon that technique to describe a two “pop” technique and named the technique transversus abdominis plane block. Hebbard et al. [5] later applied that technique with the use of ultrasound, and it became the TAP block we have today. Foreo et al. [6] first described the ultrasound-guided ESP block in 2016 to control neuropathic pain in a patient with presumed postherpetic neuralgia that was later found to have metastatic cancer seeded to the ribs.
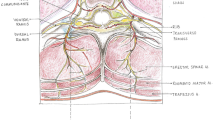
The ventral rami of T6-L1 that traverses between the plane of the internal oblique muscle and the transversus abdominis muscle form the cutaneous nerves that provide innervation to the abdominal wall from the xiphoid process to the iliac crest [7] (Fig. 1). There are three approaches to the TAP block: lateral, posterior, and subcostal [7, 8]. The lateral approach places the linear ultrasound probe transverse on the mid axillary line between the costal margin and iliac crest. The 3 layers of the abdominal wall (external oblique muscle, internal oblique muscle, and transversus abdominis muscle) are then well visualized. The needle is then advanced in plane until it reaches the layer between the internal oblique and transversus abdominis and deposits about 15–20 mL of local anesthetic. The subcostal and posterior approach is very similar in concept. Subcostal technique places the probe oblique to the transversus position right below the subcostal margin while depositing the local anesthetic in between the rectus abdominis muscle and transversus abdominis muscle. The posterior approach starts off from the lateral TAP to more posterior and lateral position with the three layers of muscle ending and coming together. The local anesthetic is deposited below the internal oblique right before the aponeurosis of all three layers [7, 8].
While the TAP block is the most used block for the abdomen, the ESP block is quickly becoming the block to use for the thoracic region due to its ease of performance and minimal risk of complications. The ESP block can be done under ultrasound and fluoroscopy guidance in either sitting, prone, or lateral position. The erector spinae muscle (ESM) is a group of 3 muscle spindles that runs longitudinally along the back from the base of the skull to the sacrum. This muscle helps link one bony component of the back to another. It is postulated that with the injection deep to the ESM plane the local anesthetic can reach both the dorsal and ventral rami of the thoracic spine, thereby being able to anesthetize both dorsal and ventral chest wall. There is some evidence that the local anesthetic can reach the thoracic paravertebral space; however, cadaveric studies have been inconsistent in this. When performing the ESP block, the linear ultrasound probe is positioned in the parasagittal to the thoracic spinous processes until the transversus processes are visualized. The needle is advanced in plane as it passes the trapezius, the rhomboid major, and the ESM before it stops right on top of the transversus process (Fig. 1). About 20 mL of local anesthetic is deposited along the fascial plane relying on passive spread of local anesthetic to target nerves within the plane or in adjacent tissue compartments where it produces analgesia for both the anterior and posterior chest wall [9, 10].
Transversus Abdominis Plane Block
Chronic Abdominal Pain
Chronic abdominal pain (CAP) is a common complaint and frequently is difficult to manage. Most of these patients undergo extensive work-up including procedures such as esophagogastroduodenoscopy (EGD) and colonoscopy. Unfortunately, CAP management options are limited and in many cases are not effective and may cause side effects more bothersome than the pain itself. One of the commonly overlooked causes of CAP is chronic abdominal wall pain, also referred to as anterior cutaneous nerve entrapment syndrome (ACNES). This type of pain accounts for almost 10% of CAP cases [11]. ACNES pain is predominantly somatic pain and in theory may respond better for TAP block. ACNES is often underdiagnosed and mistaken for visceral abdominal pain. ACNES is more common in females (4 times more than males) and most commonly in the fifth and the sixth decade of life [12]. Possible risks factors for ACNES include prior abdominal surgery, pregnancy, and oral contraceptive (nerve entrapment by edema or scaring) [12]. ACNES diagnosis is usually made through medical history and physical examination. Carnett’s sign helps in making the diagnosis of ACNES and distinguishes between abdominal wall pain and intra-abdominal pain as shown in Fig. 2.
The use of TAP block to treat CAP has gained some momentum in the last few years. Abd-Elsayed et al. [13] described the use of TAP block to manage patients with CAP who have failed other treatment options. They reviewed retrospectively the charts and analyzed collected data of 30 CAP patients who failed other pain management options and were treated with TAP blocks with bupivacaine and triamcinolone. This study showed that TAP block improved pain scores (an average of 54.7%) in 79.5% of the performed blocks. The average duration of improvement for the patients who have completed data was 84 days. In another retrospective chart review and data analysis, Abd-Elsayed et al. [14] analyzed the charts of 92 patients. The authors noted that 56% of their study patients had prior abdominal surgery as the likely triggering factor of their chronic abdominal pain. Almost 82% of the patients had improvement in their pain scores during follow-up visits. Patients reported an average of 50% improvement (50.3% ± 39.0%). The average duration of the improvement was 108 days. Furthermore, the intervention led to a significant decrease in emergency room visits related to CAP.
Several case reports and case series have been published supporting the use of TAP block to manage CAP and more specifically ACNES pain. Baciarello et al. [15] reported five consecutive cases with abdominal wall pain. Patient received TAP blocks of an admixture of bupivacaine and triamcinolone. Two of their patients maintained low pain intensities at 6- and 12-month follow-up calls. Nizamuddin et al. [16] described three case reports of teenagers who received one-sided targeted TAP blocks for suspected ACNES causing CAP, two patients with right upper quadrant abdominal pain, and one with left upper quadrant abdominal pain, utilizing lidocaine mixed with triamcinolone. The blocks were repeated 1–3 times. All patients reported significant pain relief and improvement in function for months. Simpson et al. [17] reported a case 15-year-old girl of CAP with suspected ACNES who received subcostal TAP block of an admixture of bupivacaine and triamcinolone with good pain relief and functional improvement for 1 month. Guirguis et al. [18] utilized a local anesthetic TAP catheter infusion to manage CAP for an 18-year-old girl who developed CAP after a routine laparoscopic cholecystectomy. After failed management with medical and interventional therapies, including epidural and celiac plexus blocks, a TAP block was performed with significant improvement of pain for about 24 h. Later, an indwelling TAP catheter for continuous infusion of a local anesthetic was placed. The patient was sent home with a continuous infusion for 2 weeks. She reported marked improvement of her pain level as well as her functional status up to 9 months of follow-up. Takimoto [19] reported a case showing the benefit of single-shot TAP block and then a continuous infusion of local anesthetic through a TAP catheter to manage intractable severe abdominal causalgia in a critically ill patient in the intensive care unit after failed multimodal pain medical therapies including fentanyl, dexmedetomidine, and ketamine. The TAP block and catheter helped the patient’s pain significantly without the need for fentanyl, dexmedetomidine, or ketamine. They kept the TAP catheter after discharge for several days (total of 31 days).
Erector Spinae Plane Block
Chronic Thoracic Neuropathic Pain
Chronic thoracic neuropathic pain may be present due to infections, cancer, surgery, or trauma. The pain is often debilitating and can be refractory to conventional analgesia. Comparable to the use of TAP block to manage CAP, the utilization of ESP block to treat thoracic pain has expanded in the last few years. In this review, we shed light on several case reports, case series, and studies published recently supporting the use of the ESP block to treat chronic or cancer-related pain as a component of multidisciplinary management.
Forero et al. [6] published two case reports. In the first case, a 67-year-old male presented with a 4-month history of burning neuropathic pain radiating from the spine into the anterior chest wall. They inserted an epidural catheter in the erector spinae plane and used intermittent injections of 20 mL of bupivacaine 0.25% (each injection provided an average of 12 h of complete analgesia). Their second case was a 48-year-old man with a 3-year history of chronic neuropathic pain secondary to rib fractures. ESP block was performed using 20 mL 0.5% ropivacaine. During a 30-day follow-up visit, the patient reported that pain had been reduced to 25% of its original severity and complete cessation of allodynia. His pain did not require more medications for management, and the patient was reportedly satisfied with his improved quality of life.
In 2017, Forero et al. [20] presented a case series of seven patients with post-thoracotomy pain syndrome (PTPS) managed with ESP blocks:
-
1.
A 58-year-old man with history of PTPS following a right upper lobectomy. An ESP block was performed with 30 mL of 0.5% ropivacaine with good pain control for 4–6 weeks. The block was repeated a few times after that with significant continued analgesia.
-
2.
An 81-year-old woman with PTPS who received one ESP block with 25 mL of 0.5% ropivacaine with good analgesia for more than 4 weeks.
-
3.
A 64-year-old man presented with PTPS 6 months after undergoing right pneumonectomy. He continued to experience pain and significant limitation of daily activities despite medical management with opioids. An ESP block with 25 mL of 0.5% ropivacaine and 40 mg of methylprednisolone was performed with good pain relief lasting 2 weeks, allowing improved sleep and reduction in the use of breakthrough opioid. The injection was repeated with ropivacaine only and produced significant analgesia for another 2 weeks.
-
4.
A 77-year-old man with PTPS 5 months after a robotic left lower lung lobectomy. An ESP block was performed with 30 mL of 0.5% ropivacaine. The block was repeated twice in a few weeks later. Good pain relief lasted only for hours (2–24 h) with some change in the quality of his pain after the 2-week follow-up assessment (decrease in the pressure-like and sharp pain).
-
5.
A 66-year-old woman presented with PTPS 1 year following a robotic left lung upper lobe segmentectomy. An ESP block was performed with 20 mL of 0.5% ropivacaine. Thirty minutes later, she reported almost complete resolution of her pain and hyperalgesia. At a telephone follow-up 1 week later, she reported that analgesia had lasted 2 days before returning to its original intensity. However, there was subsequent improvement to tolerable levels with pregabalin therapy and she declined further intervention and follow-up.
-
6.
A 67-year-old woman presented with PTPS 2 months following left pneumonectomy. An ESP block was performed with 20 mL of 0.5% ropivacaine. Thirty minutes later, she reported that her pain intensity had significantly declined. At a telephone follow-up 1 week later, she reported that the effects of the block lasted for 4 h before recurring at its original intensity.
-
7.
A 55-year-old man presented with PTPS 8 months after right thoracotomy for upper lung lobectomy. An ESP block with 35 mL of 0.375% ropivacaine and 80 mg methylprednisolone was done. He reported a 50% reduction in pain intensity during his 1-week follow-up visit. The block was repeated with 25 mL of 0.375% ropivacaine (helped for few weeks) and then with 20 mL of 0.25% ropivacaine and 80 mg methylprednisolone, which helped his pain and improved his function for more than 4 weeks, and furthermore, reduced his use of opioids.
Fusco et al. [21] presented a case of a 75-year-old man affected by parotid carcinoma with multiple metastasis to the ribs and vertebral bodies. The patient reported neuropathic pain in the T7 to T12 dermatomal distribution. An ESP block was performed at the T9 transverse process level with 20 mL 0.2% ropivacaine and 8 mg of dexamethasone producing significant decrease in his pain level for hours after the block. At the 7-day follow-up visit, the patient reported recurrence of the pain but lower in intensity. The same treatment was carried out twice, and the pain became gradually mitigated.
Hasoon et al. [22] also described the use of the ESP block for the treatment of two patients with refractory thoracic neuropathic pain after surgery. The first patient was an 83-year-old male who underwent a video-assisted thoracoscopic surgery (VATS). He experienced severe chronic burning neuropathic pain after recovery. The second patient was a 48-year-old male with severe chronic chest wall neuropathic pain after undergoing thoracotomy for trauma. Each patient underwent an ESP block with 9 mL of 0.25% bupivacaine mixed with 40 mg of methylprednisolone. The first patient reported almost immediate resolution of his pain with pain relief lasting through his 1-month follow-up appointment. The second patient reported 90% relief shortly after the injection. At his 1-month follow-up appointment, he continued to endorse 50% pain relief and had weaned his opioid use by 50% as well.
Hasoon et al. [23] also used ESP block in a case of post-mastectomy pain syndrome, a common complication after breast cancer surgery. The reported case was a 63-year-old female who complained of severe allodynia and constant burning pain in her left breast for 6 years after mastectomy. She failed pain medical and non-invasive pain therapies. She underwent an ESP block with 9 mL of 0.25% bupivacaine and 40 mg of methylprednisolone with immediate complete pain relief. At her 1-month follow-up appointment, she reported a 70% improvement of her pain and 50% decrease in her opioid usage. She continued to have pain relief for 3 months following the procedure and reported significant improvement in her quality of life.
Sirohiya et al. [24] published a case series of cancer associated pain managed by ESP blocks. The first patient was a 42-year-old male with right Pancoast tumor causing severe pain in the dermatomal distribution from C5 to T3 for 5 months. His pain was incompletely relieved on medical treatment. After an ESP block was given at T2 level with 20 ml of 0.375% ropivacaine and 40 mg of triamcinolone, pain was relieved dramatically in few minutes associated with sensory blockade from C3 to T5. The patient was still pain-free without consumption of any other oral analgesics at the 2-month follow-up visit. Their second case was a 64-year-old male with PTPS 1 year after right bilobectomy. Patient experienced significant pain despite the high dosage of oral analgesics. An ESP block with 20 mL of 0.375% ropivacaine and 40 mg of triamcinolone produced immediate pain relief. The patient remained pain-free for 1.5 months without consumption of any other oral analgesic. A second ESP block was performed with similar admixture of ropivacaine and triamcinolone which again produced significant analgesia lasting for 2 weeks.
Postherpetic Neuralgia
Postherpetic neuralgia (PHN) is the most common chronic complication following the onset of herpes zoster. ESP block has been reported to relieve PHN in multiple case reports and studies. Audyn et al. [25] designed a multicenter retrospective observational study evaluating the efficacy of ESP block for the management of pain in herpes zoster. The medical records of 34 patients with acute or chronic herpetic neuralgia between May 2017 and June 2018 were investigated. The patients received ultrasound-guided ESP blocks, a single injection for the patients with the acute pain (23 patients), and a continuous infusion with an ESP catheter for the patients with the chronic pain (11 patients). Their study concluded that the median value of analgesia time was 18 h. The median pain numeric rating scale (NRS) score before the block was 9, the median NRS score was 1.5 after the block, and the difference was found to be statistically significant with p < 0.0001. The median NRS score after the third month was 1 with p = 0.002.
Lin et al. [26] designed a randomized double-blind placebo-controlled trial in patients diagnosed with acute or subacute herpes zoster. The primary end point was the incidence of PHN at 12 weeks. The patients were randomized to receive either ultrasound-guided ESP block or placebo subcutaneous injection every 24 h for 3 days. A total of 50 patients completed 12 weeks of follow-up. The incidence of PHN at 12 weeks was significantly lower in the ESP block group (15.4%) compared to the control group (41.7%) with p value = 0.039. At 12 weeks, the pain visual analogue scale (VAS) scores at rest and the total scores from the Short-Form McGill Pain Questionnaire-2 were significantly decreased in the ESP block group (p values were 0.046 and 0.001, respectively). The incidence of neuropathic pain, sleep disturbance, and anxiety/depression was significantly reduced in the ESP block group (p values were 0.002, 0.002, and 0.025, respectively).
Kumar et al. [27] described a case of a 52-year-old male who developed PHN after herpes zoster infection. The patient complained of severe debilitating burning pain associated with allodynia on the right side of his lower back. A right-sided ESP block was performed at the L3 level with 30 ml of 0.25% bupivacaine and 40 mg of triamcinolone with good immediate pain relief. The block was repeated twice afterwards. The patient reported a decline in his pain score and analgesics consumption in follow-up clinic visits.
Chronic Lumbar Pain
Takahashi et al. [28] presented a case of a 72-year-old woman with failed back surgery syndrome after two back surgeries. She underwent extensive medical therapies and epidural steroid injections without much improvement in her pain. After a bilateral ultrasound-guided ESP blocks at the L2 level using 20 mL of 0.1875% ropivacaine on each side, she reported almost complete resolution of her pain for several hours. The procedure was repeated twice within a month providing an overall reduction of baseline pain to almost 40% of its original severity.
Sirohiya et al. [24] published a case series of ESP block used in the management of cancer associated pain in three patients in the palliative care unit. One of the patients (a 19-year-old female) had severe burning pain in the right flank area 2 years after desmoid tumor resection. After failing conservative medical treatment, an ESP block was performed at the level of L2 with 20 ml of 0.375% ropivacaine and 40 mg of triamcinolone. The patient had an adequate immediate pain relief after the block and an extensive sensory blockade from dermatome T10 to L5. The patient was still pain-free without consumption of any oral analgesics at follow-up visit after 8 weeks.
Chronic Shoulder Pain
Forero et al. [29] published a case report of ESP block at the T2/T3 level performed in a patient with long-standing bilateral shoulder pain secondary to a combination of rotator cuff tear, subacromial bursitis, bicipital tendinopathy, and acromioclavicular joint arthritis in both shoulders. His right shoulder pain improved with other therapies; however, he continued to have significant left shoulder pain. He underwent a left-sided ESP block at the T3 level injecting 20 mL of 0.375% bupivacaine and 40 mg of methylprednisolone. Within minutes, the patient reported complete resolution of pain and had regained full active range of motion in his shoulder, including abduction overhead to 180°. No clinically apparent motor blockade of the left upper limb was noted. At the follow-up visit 12 weeks later, the patient reported that his left shoulder remained pain-free at rest with only mild pain on movement.
Controversies and Challenges
One of the main challenges for using these blocks for chronic pain is the correct diagnosis for chest wall neuropathic pain or abdominal wall pain in the first place. It is uncommon in clinical practice to see an isolated abdominal wall pain. Furthermore, many pain medicine providers are skeptical about the effectiveness of these blocks to treat chronic pain for a reasonable duration, especially with the inability to use the denervation techniques such as radiofrequency ablation to prolong the duration of the pain relief.
Conclusion
The use of single peripheral nerve blocks (such as occipital, spinal medial branch, and genicular nerves) to manage chronic or cancer pain is well-established as a part of the multidisciplinary management of chronic and cancer-related pain. ESP and TAP blocks target a group of nerves run in a truncal fascial plane. In this report, we presented some evidence supporting the effectiveness of these blocks in the management of chronic and cancer-related pain. This evidence includes case reports, case series, retrospective observational, and one prospective randomized controlled trial.
The indications for the ESP block, as presented in this review, included post-thoracotomy pain syndrome, postherpetic neuralgia, post-mastectomy pain syndrome, chronic shoulder pain, chronic lumbar pain, and other types of neuropathic pain involving mainly the thoracic dermatomes. On the other hand, TAP block indications were more limited to the abdominal wall pain, specifically the anterior cutaneous nerve entrapment syndrome. Even though the effectiveness of those two blocks in managing the above pain condition is not yet well-established, our review showed surprisingly months of pain relief and functional improvement after single-shot blocks in numerous cases.
Both blocks are very safe when performed by experienced hands and with the use of a skillful imaging technique, usually ultrasound and occasionally fluoroscopy in the case of ESP block. Other than the rare risks of any other regional anesthesia procedure such as infection, bleeding, nerve injury, and local anesthetic toxicity, ESP block has the potential to cause pneumothorax. Furthermore, the injected admixture of local anesthetic (with or without steroid) after ESP block may spread significantly into the adjacent spinal structures.
The majority of these blocks were performed with the use of bupivacaine or ropivacaine and a steroid (methylprednisolone, triamcinolone, or dexamethasone). Because of the lack of strong evidence from controlled clinical studies, we suggest using these blocks when other established methods to treat this pain fail or are not adequate such as physical therapy, pharmacological agents, or other interventional procedures.
References
Chakraborty A, Khemka R, Datta T. Ultrasound-guided truncal blocks: a new frontier in regional anaesthesia. Indian J Anaesth. 2016;60(10):703–11.
Manassero A, Bossolasco M, Meineri M, Ugues S, Liarou C, Bertolaccini L. Spread patterns and effectiveness for surgery after ultrasound-guided rectus sheath block in adult day-case patients scheduled for umbilical hernia repair. J Anaesthesiol Clin Pharmacol. 2015;31(3):349–53.
Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56(10):1024–6.
McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104(1):193–7.
Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35(4):616–7.
Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–7.
Tran DQ, Bravo D, Leurcharusmee P, Neal JM. Transversus abdominis plane block: a narrative review. Anesthesiology. 2019;131(5):1166–90.
Abrahams MS, Horn JL, Noles LM, Aziz MF. Evidence-based medicine: ultrasound guidance for truncal blocks. Reg Anesth Pain Med. 2010;35(2 Suppl):S36–42.
De Cassai A, Bonvicini D, Correale C, Sandei L, Tulgar S, Tonetti T. Erector spinae plane block: a systematic qualitative review. Minerva Anestesiol. 2019;85(3):308–19.
Kot P, Rodriguez P, Granell M, Cano B, Rovira L, Morales J, Broseta A, Andrés J. The erector spinae plane block: a narrative review. Korean J Anesthesiol. 2019;72(3):209–20.
Kamboj AK, Hoversten P, Oxentenko AS. Chronic abdominal wall pain: a common yet overlooked etiology of chronic abdominal pain. Mayo Clin Proc. 2019;94(1):139–44.
Costanza CD, Longstreth GF, Liu AL. Chronic abdominal wall pain: clinical features, health care costs, and long-term outcome. Clin Gastroenterol Hepatol. 2004;2(5):395–9.
Abd-Elsayed A, Malyuk D. Efficacy of transversus abdominis plane steroid injection for treating chronic abdominal pain. Pain Pract. 2018;18(1):48–52.
Abd-Elsayed A, Luo S, Falls C. Transversus abdominis plane block as a treatment modality for chronic abdominal pain. Pain Physician. 2020;23(4):405–12.
Baciarello M, Migliavacca G, Marchesini M, Valente A, Allegri M, Fanelli G. Transversus abdominis plane block for the diagnosis and treatment of chronic abdominal wall pain following surgery: a case series. Pain Pract. 2018;18(1):109–17.
Nizamuddin SL, Koury KM, Lau ME, Watt LD, Gulur P. Use of targeted transversus abdominus plane blocks in pediatric patients with anterior cutaneous nerve entrapment syndrome. Pain Physician. 2014;17(5):E623–7.
Simpson DM, Tyrrell J, De Ruiter J, Campbell FA. Use of ultrasound-guided subcostal transversus abdominis plane blocks in a pediatric patient with chronic abdominal wall pain. Paediatr Anaesth. 2011;21(1):88–90.
Guirguis MN, Abd-Elsayed AA, Girgis G, Soliman LM. Ultrasound-guided transversus abdominis plane catheter for chronic abdominal pain. Pain Pract. 2013;13(3):235–8.
Takimoto K. Transversus abdominis plane block for chronic abdominal pain in a critically ill patient. Anaesth Intensive Care. 2014;42(6):809–10.
Forero M, Rajarathinam M, Adhikary S, Chin KJ. Erector spinae plane (ESP) block in the management of post thoracotomy pain syndrome: a case series. Scand J Pain. 2017;17:325–9.
Fusco P, Maggiani C, Volpe D, Petroni GM, Bagaphou CT, Marinangeli F. Erector spinae plane block for the management of chronic cancer pain in the era of COVID-19. Minerva Anestesiol. 2021;87(7):836–7.
Hasoon J, Urits I, Viswanath O, Aner M. Utilization of erector spinae plane block in the chronic pain clinic for two patients with post-thoracotomy pain. Cureus. 2020;12(7): e8988.
Hasoon J, Urits I, Viswanath O, Dar B, Kaye AD. Erector spinae plane block for the treatment of post mastectomy pain syndrome. Cureus. 2021;13(1): e12656.
Sirohiya P, Yadav P, Bharati SJ, Sushma B. Unfolding role of erector spinae plane block for the management of chronic cancer pain in the palliative care unit. Indian J Palliat Care. 2020;26(1):142–4.
Aydın T, Balaban O, Ahiskalioglu A, Alici HA, Acar A. Ultrasound-guided erector spinae plane block for the management of herpes zoster pain: observational study. Cureus. 2019;11(10): e5891.
Lin ZM, Wang HF, Zhang F, Ma JH, Yan N, Liu XF. The effect of erector spinae plane blockade on prevention of postherpetic neuralgia in elderly patients: a randomized double-blind placebo-controlled trial. Pain Physician. 2021;24(7):E1109–18.
Kumar A, Mistry T, Gupta N, Kumar V, Bhatnagar S. Lumbar erector spine plane block for pain management in postherpetic neuralgia in a patient with chronic lymphocytic leukemia. Indian J Palliat Care. 2020;26(1):134–6.
Takahashi H, Suzuki T. Erector spinae plane block for low back pain in failed back surgery syndrome: a case report. JA Clin Rep. 2018;4(1):60.
Forero M, Rajarathinam M, Adhikary SD, Chin KJ. Erector spinae plane block for the management of chronic shoulder pain: a case report. Can J Anaesth. 2018;65(3):288–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elsharydah, A., De La Cruz, R., Horani, S.M. et al. Utilization of Truncal Fascial Plane Nerve Blocks for Chronic Pain Management: A Narrative Review. Curr Pain Headache Rep 27, 149–155 (2023). https://doi.org/10.1007/s11916-023-01112-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-023-01112-7