Abstract
Purpose of Review
Intercostal nerve blocks are indicated for multiple chronic pain and acute pain conditions including rib fractures, herpes zoster, post-thoracotomy pain syndrome, and intercostal neuralgia. Intercostal neuralgia is a type of neuropathic pain that is in the distribution of intercostal nerves. The purpose of this review is to evaluate the different techniques used to perform intercostal nerve blocks and review their efficacy and safety including blind technique using anatomical landmarks, and fluoroscopically guided and ultrasound-guided intercostal nerve blocks.
Recent Findings
Literature search was performed with the keywords including intercostal neuralgia, treatment, intercostal nerve blocks, and radiofrequency ablation on PubMed and Google Scholar. Three studies and one case report were identified. Literature review revealed that ultrasound-guided techniques and fluoroscopically guided techniques are superior to landmark-based technique in terms of efficacy. There was no difference in efficacy and complication rates between ultrasound and fluoroscopic guidance.
Summary
Ultrasound-guided techniques and fluoroscopically guided techniques can both be performed safely and effectively for various chronic pain conditions. Ultrasound guidance has its advantages of direct visualization of nerves, vessels, muscles, and the lung. It is potentially a superior technique in terms of improving accuracy and decreasing complications. Further large population randomized control studies should be conducted to compare the efficacy of intercostal nerve blocks performed under ultrasound and fluoroscopy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intercostal nerve blocks can be used to treat a various number of conditions that include acute and chronic pain conditions including intercostal neuralgia, Tietze’s syndrome, post-thoracotomy pain syndrome, acute herpes zoster, intercostal neuromas, malignancy, and post-mastectomy syndrome [1–3]. Intercostal neuralgia is a painful neuropathic condition that is in the distribution of the intercostal nerves [4].
For chronic pain conditions, intercostal nerve blocks are typically performed for diagnostic and therapeutic purposes [5]. If source of the pain is confirmed related to the intercostal nerve, radiofrequency ablation of intercostal nerves can be performed for long-term pain control [6]. Intercostal nerve blocks have also been used to treat cancer pain, such as liver metastatic lesions [7].
These blocks can be used in the acute pain setting and as part of the anesthetic for management of thoracic surgery, breast surgery, and upper abdominal surgeries including appendectomy [8, 9]. Intercostal nerve blocks have been combined with celiac plexus blocks, and light anesthesia can be administered for surgical procedures including thoracotomy, mastectomy, and cholecystectomy surgeries [10]. Patients with multiple rib fractures are also candidates for intercostal nerve blocks, paravertebral blocks, and epidural techniques [11]. Intercostal nerve blocks can also be used for analgesia prior to chest tube and nephrostomy tube insertion [10, 12].
Anatomy
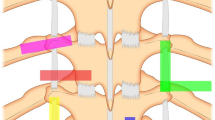
Intercostal nerves are the ventral rami of the thoracic spinal nerves from T1 to T11. The anterior division of the twelfth thoracic nerve is referred to as the subcostal nerve as it enters the abdominal wall. There are 3 intercostal muscles which are the external, internal, and innermost intercostal muscles [13]. The intercostal nerves enter the intercostal space in between the posterior intercostal membrane and the parietal pleura, and lie inferior to its associated rib between the innermost intercostal muscle and the internal intercostal muscle [2, 13]. The intercostal nerve has four branches—the gray rami communicantes, the posterior communicating branch, the lateral cutaneous branch, and the anterior cutaneous branch [14].
The anterior and posterior intercostal arteries travel along with the intercostal nerves. The intercostal vein is the most superior, with the intercostal artery inferior to it and the intercostal nerve more inferior to the artery [13, 14]. The anatomical position of the intercostal vein, intercostal artery, and intercostal nerve are arranged from superior to inferior position [4].
Complications
Complications of intercostal nerve blockade mostly are due to the proximity of the nerve to the lung and intercostal vessels. These include infection, bleeding leading to hemothorax, and local anesthetic systemic toxicity (LAST). There is also a risk of spinal blockade, and there have been multiple case reports of inadvertent spinal blockade including direct intrathoracic intercostal nerve blockade during lung resection surgery [15]. Inadvertent injection could also lead to subdural or epidural injections. Due to the proximity of the intercostal nerves to the lung, there is a risk of pneumothorax, which has been reported to range from 0.073 to 19% [16]. A retrospective chart review by [16] found that the incidence of pneumothorax per individual intercostal nerve blocked was 1.4% [16]. Also, due to the proximity of intercostal vessels, there is an increased risk of vascular uptake which can result in LAST [17]. The most feared complication is paraplegia which has been described in case reports after neurolysis of intercostal nerves with phenol were performed under fluoroscopic guidance [18, 19].
Techniques
In recent years, more chronic pain procedures have been performed under ultrasound guidance due to its ability to visualize soft tissue structures, vessels, and nerves [20]. Intercostal nerve blockade was first described in 1907 by Braun. In 1988, the use of Doppler ultrasound for intercostal nerve blockade was described [21]. The three techniques used for performing intercostal nerve blocks are the landmark-based technique, ultrasound-guided technique, and fluoroscopically guided technique. For the landmark-based technique, the patient is positioned either in the prone position with the arms hanging off the table or in the lateral decubitus position; both positions rotate the scapula upward and outward and allow for easier palpation of the upper ribs [10]. The index finger of the left hand pulls the skin which overlies the inferior border of the rib up and over the rib, and the needle is introduced at that point and advanced until it rests on the lower border of the rib [4].
Ultrasound-guided intercostal nerve block can be performed with an in-plane technique with the tip of the needle positioned between the internal and innermost intercostal muscles [2, 12]. The advantages of using ultrasound technique include visualization of vascular structures as well as real time visualization of the pleura, and the use of low volumes of local anesthetics [2, 22]. The disadvantage of ultrasound-guided procedures is that the procedures are operator dependent [20, 23]. The expertise of the operator obtaining ultrasound images can affect the quality of images obtained. Other limitations include the poor resolution of narrow-gauge needles and the loss of resolution with increasing tissue depth as well as the possible interference from overlying structures [24]. In the case of intercostal nerve blocks, rib shadows can sometimes interfere with the ability to view the neuromuscular bundle [12, 25].
Fluoroscopically guided intercostal nerve blocks are performed by identifying the inferior and superior ribs on anterior-posterior view. The target is then reached by walking off the inferior border of the corresponding rib. The disadvantages to fluoroscopic technique include radiation exposure, higher cost, use of contrast dye, and the lack of portability of fluoroscope [22].
We reviewed the current literature excluding review articles and found two studies that compared ultrasound- and fluoroscopically guided intercostal nerve blocks.
Methods and Results
A PubMed and Google Scholar search with the keywords intercostal neuralgia, intercostal nerve block, and treatment was performed until September 2019. Studies of patients aged 18 or older with intercostal nerve blocks performed were selected. Review articles on treatment options including intercostal blocks and non-English articles were excluded. Articles including continuous intercostal nerve blocks performed in the acute care setting or for perioperative analgesia were excluded. Three studies and one case report are identified and summarized in Table 1.
Discussion
Lee et al. reviewed thirty-eight patients and compared fluoroscopy-guided epidural nerve blocks compared to ultrasound-guided intercostal nerve block [23]. These patients had thoracic herpes zoster and chest wall herpetic eruption. Eighteen patients underwent fluoroscopically guided epidural nerve blocks, and twenty patients underwent ultrasound-guided intercostal nerve block which was performed at the midaxillary line, posterior to the lateral cutaneous branch of the intercostal nerve. The primary outcome was the numeric rating scale (NRS) score reduction for pain. Results showed that all patients showed significant pain relief on NRS at final follow-up point (p >0.05), and there was no significant difference in mean value of NRS based on intervention type, or difference in the duration of the treatment [23]. There were no complications reported with either technique [23].
Shankar et al. reviewed thirty-nine intercostal nerve blocks performed under ultrasound guidance and fluoroscopy guidance using similar 25 G hypodermic needles with the same injectates of 5% tetracaine and 10 mg of medroxyprogesterone acetate in 1 mL [22]. Fluoroscopically guided needle placement was confirmed with contrast prior to medication injection, and ultrasound-guided injection of medication was visualized in real time. The patients had a variety of pathologies ranging from blunt traumas, chemical exposures, and lung cancer. The primary outcomes include the difference between pre-procedure visual analog scale (VAS) score and the post-procedure VAS score and the duration of pain relief. Results showed that there was no difference in duration of pain relief nor differences in pre-post VAS scores between groups. Also, the complication rate was similar, and there were no complications of pneumothorax in either group.
Bhatia et al. performed a two-phase cadaveric experiment to evaluate between ultrasound-guided(USG) and anatomic-guided intercostal nerve blocks [26]. The first phase of the study consisted of 12 injections of dye (6 USG and 6 anatomic guided) on a single cadaver to evaluate spread of dye through dissection. The second phase consisted of 74 intercostal nerve injections of contrast dye (37 USG and 37 using anatomic landmarks) in 6 cadavers followed by fluoroscopy to evaluate contrast spread. It was noted in the first phase of the study that 5 out of 6 ultrasound-guided injections showed sufficient dye spread while only 2 out of 6 injections via anatomic guidance showed complete staining. It was noted that there were no intravascular injections in either guidance groups. In the second phase of the study, ultrasound-guided injections were associated with higher rates of intercostal spread compared with anatomic landmark guidance (97% vs 70%). It should be noted that fluoroscopy was used as the gold standard to evaluate correct anatomical spread.
Abd-Elsayed et al. published a case report on two patients who had intercostal neuralgia successfully treated with radiofrequency ablation (RFA) of the intercostal nerves. The first patient had chronic chest pain after a lumpectomy for breast cancer and had failed conservative therapy (physical therapy, medications including nonsteroidal anti-inflammatory drugs (NSAIDs), and anti-depressants). She had two positive diagnostic intercostal nerve blocks followed by RFA and had more than 1 year pain relief. The second case was a female who developed chronic chest pain after right upper lobe (RUL) resection. The patient failed conservative therapy with opioids, NSAIDs, and physical therapy. The patient underwent two successful intercostal nerve blocks prior to radiofrequency ablation of intercostal nerves. The second patient only had a 2-month follow-up but at the time reported complete pain relief. Both procedures were fluoroscopically guided, and the needles were positioned at the lower border of the rib and confirmed with contrast dye [5].
There are many indications for performing intercostal nerve blocks including intercostal neuralgia and chronic post thoracotomy pain syndrome. Intercostal nerve blocks have been found to be effective methods of analgesia in acute pain conditions as well as chronic pain conditions [6, 10]. For pain that does not respond to conservative therapy including physical therapy, anti-neuropathic agents, and antidepressants, intercostal nerve blocks can be considered. Recently, more chronic pain procedures have been performed under ultrasound guidance due to the benefit of decreased radiation and portability of machine. A review article by Bhatia et al. in 2013 found that there was insufficient data to support improved outcomes to relieve short-term and long-term chronic pain with ultrasound over traditional anatomic landmark and fluoroscopic-guided procedures [27]. However, in cases of resistant post-thoracotomy pain syndrome, intercostal surgical neurolysis was found to be effective [1, 28], which suggests that more accurate neurolysis performed under ultrasound guidance is potentially more effective in these chronic pain conditions.
Conclusion
Intercostal nerve blocks are indicated for multiple acute and chronic pain conditions. Based on this review, ultrasound-guided techniques and fluoroscopically guided techniques are superior to landmark-based technique in terms of efficacy. Ultrasound-guided techniques and fluoroscopically guided techniques can both be performed safely and effectively for various chronic pain conditions. This review of literature revealed no difference in efficacy and complication rates between ultrasound and fluoroscopic guidance. However, ultrasound, with its advantages of direct visualization of nerves, vessels, muscles, and the lung, is potentially a superior technique in terms of improving accuracy and decreasing complications, which suggests that more studies with larger number of patients need to be performed to compare the efficacy and complication rates between the two techniques.
Change history
27 November 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11916-021-00997-6
References
Williams EH, Williams CG, Rosson GD, Heitmiller RF, Dellon AL. Neurectomy for treatment of intercostal neuralgia. Ann Thorac Surg. 2008;85:1766–70.
Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of interventional techniques in managing chronic pain: Springer International Publishing; 2018.
Koehler RP, Keenan RJ. Management of postthoracotomy pain: acute and chronic. Thorac Surg Clin. 2006;16:287–97.
Intercostal nerve block – landmarks and nerve stimulator technique. 2019 at Intercostal Nerve Block – Landmarks and Nerve Stimulator Technique. 2019
Abd-Elsayed A, Lee S, Jackson M. Radiofrequency ablation for treating resistant intercostal neuralgia. Ochsner J. 2018;18:91–3.
Stolker RJ, Vervest AC, Groen GJ. The treatment of chronic thoracic segmental pain by radiofrequency percutaneous partial rhizotomy. J Neurosurg. 1994;80:986–92.
Waldman SD, Feldstein GS, Donohoe CD, Waldman KA. The relief of body wall pain secondary to malignant hepatic metastases by intercostal nerve block with bupivacaine and methylprednisolone. J Pain Symptom Manag. 1988;3:39–43.
Kopacz DJ, Thompson GE. Intercostal blocks for thoracic and abdominal surgery. Tech Reg Anesth Pain Manage. 1998;2:25–9
Bunting P, McGeachie JF. Intercostal nerve blockade producing analgesia after appendicectomy. Br J Anaesth. 1988;61:169–72.
Moore DC, Bridenbaugh LD. Intercostal nerve block in 4333 patients: indications, technique, and complications. Anesth Analg. 1962;41:1–11.
Ho AM, Karmakar MK, Critchley LA. Acute pain management of patients with multiple fractured ribs: a focus on regional techniques. Curr Opin Crit Care. 2011;17:323–7.
Ozkan D, Akkaya T, Karakoyunlu N, Arık E, Ergil J, Koc Z, et al. Effect of ultrasound-guided intercostal nerve block on postoperative pain after percutaneous nephrolithotomy: prospective randomized controlled study. Anaesthesist. 2013;62:988–94.
Baxter CS, Fitzgerald BM. Intercostal nerve block. Treasure Island (FL): StatPearls; 2019.
Hardy PA. Anatomical variation in the position of the proximal intercostal nerve. Br J Anaesth. 1988;61:338–9.
Chaudhri BB, Macfie A, Kirk AJ. Inadvertent total spinal anesthesia after intercostal nerve block placement during lung resection. Ann Thorac Surg. 2009;88:283–4.
Shanti CM, Carlin AM, Tyburski JG. Incidence of pneumothorax from intercostal nerve block for analgesia in rib fractures. J Trauma. 2001;51:536–9.
Gauntlett IS. Total spinal anesthesia following intercostal nerve block. Anesthesiology. 1986;65:82–4.
Gollapalli L, Muppuri R. Paraplegia after intercostal neurolysis with phenol. J Pain Res. 2014;7:665–8.
Kissoon NR, Graff-Radford J, Watson JC, Laughin RS. Spinal cord injury from fluoroscopically guided intercostal blocks with phenol. Pain Physician. 2014;17:E219–24.
Wang D. Image guidance technologies for interventional pain procedures: ultrasound, fluoroscopy, and CT. Curr Pain Headache Rep. 2018;22:6.
Vaghadia H, Jenkins LC. Use of a Doppler ultrasound stethoscope for intercostal nerve block. Can J Anaesth. 1988;35:86–9.
Shankar H, Eastwood D. Retrospective comparison of ultrasound and fluoroscopic image guidance for intercostal steroid injections. Pain Pract. 2010;10:312–7.
Lee HJ, Park HS, Moon HI, Yoon SY. Effect of ultrasound-guided intercostal nerve block versus fluoroscopy-guided epidural nerve block in patients with thoracic herpes zoster: a comparative study. J Ultrasound Med. 2019;38:725–31
Korbe S, Udoji EN, Ness TJ, Udoji MA. Ultrasound-guided interventional procedures for chronic pain management. Pain Manag. 2015;5:465–82.
Curatolo M, Eichenberger U. Ultrasound in interventional pain management. European J Pain Supplements. 2008;2:78–83.
Bhatia A, Gofeld M, Ganapathy S, Hanlon J, Johnson M. Comparison of anatomic landmarks and ultrasound guidance for intercostal nerve injections in cadavers. Reg Anesth Pain Med. 2013;38:503–7
Bhatia A, Brull R. Review article: is ultrasound guidance advantageous for interventional pain management? A systematic review of chronic pain outcomes. Anesth Analg. 2013;117:236–51.
Cappellari AM, Tiberio F, Alicandro G, Spagnoli D, Grimoldi N. Intercostal neurolysis for the treatment of postsurgical thoracic pain: a case series. Muscle Nerve. 2018;58:671–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Anesthetic Techniques in Pain Management
The original online version of this article was revised: The “Methods and Results” section heading contains added data.
Rights and permissions
About this article
Cite this article
Elkhashab, Y., Wang, D. A Review of Techniques of Intercostal Nerve Blocks. Curr Pain Headache Rep 25, 67 (2021). https://doi.org/10.1007/s11916-021-00975-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s11916-021-00975-y