Abstract
Summary
This study from southern India showed that the trabecular microarchitecture and proximal hip geometry were significantly impaired in postmenopausal women with diabetes as compared to age and BMI matched non-diabetic controls. This is despite there being no significant difference in bone mineral density at the femoral neck and hip not between both groups. One-third of the study subjects with type 2 diabetes had prevalent vertebral fractures. Bone mineral density assessment as a standalone tool may not adequately reflect bone health in subjects with diabetes.
Introduction
There is limited information with regard to bone health in Indian postmenopausal women with type 2 diabetes. We studied the bone mineral density (BMD), trabecular bone score (TBS), prevalent vertebral fractures (VF), proximal hip geometry, and bone mineral biochemistry in ambulatory postmenopausal women with and without type 2 diabetes mellitus (T2DM).
Methods
This was a cross-sectional study conducted at a tertiary care center. BMD, TBS, prevalent vertebral fractures, and hip structural analysis (HSA) were assessed using a dual-energy X-ray absorptiometry (DXA) scanner. Bone mineral biochemical profiles were also studied.
Results
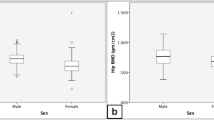
A total of 202 ambulatory postmenopausal women known to have type 2 diabetes mellitus with mean (SD) age of 65.6 (5.2) years and 200 age and BMI matched non-diabetic controls with mean (SD) age of 64.9 (4.7) years were recruited from the local community. Although the prevalence of lumbar spine osteoporosis was significantly lower among cases (30.7%) as compared to controls (42.9%), the prevalence of degraded bone microarchitecture (TBS < 1.200) was significantly higher among cases (51%) than in controls (23.5%); P < 0.001. Prevalent vertebral fractures were not significantly different in cases and controls. The various geometric indices of the proximal hip were significantly impaired in subjects with diabetes as compared to controls.
Conclusion
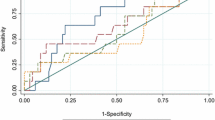
This study may highlight the utility of the trabecular bone score and hip structural analysis in subjects with diabetes, where the bone mineral density tends to be paradoxically high, and may not adequately predict fracture risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of diabetes mellitus (DM) in India is increasing at a rapid pace, and with improved longevity, a significant proportion of people living with diabetes are in their seventh decade of life [1]. The number of patients with diabetes mellitus in India has progressively increased from 26 million in 1990 to 64 million in 2016 and is projected to reach a figure of 134 million by 2045. In India, recent epidemiological studies have shown evidence of the emerging epidemic of DM across all classes, affecting both the affluent and poor alike. In 2016, the prevalence of diabetes was highest in Tamil Nadu, Kerala, and Delhi [2]. Poorly controlled diabetes mellitus is associated with neuropathy, retinopathy, and nephropathy leading to end-stage renal disease. Besides these micro-vascular complications, the non-communicable diseases that occur more commonly with diabetes include cardiovascular disease, cancer, osteoporosis, and fractures resulting from trivial trauma and increased skeletal fragility [3].
In India, about 30–50% of the ambulatory postmenopausal women are affected with osteoporosis [4]. The mortality after a hip fracture is estimated to be about 20% in the first year following the fracture. Several epidemiological studies have shown an increased fracture risk in individuals with diabetes. In the recently published INDIAB study, which is a community-based survey to estimate the prevalence of diabetes across India, it was found that the prevalence of self-reported fractures was significantly higher in subjects with diabetes (4%) as compared to those without (2.5%). Moreover, after gender stratification, diabetes emerged as an important risk factor for fractures only in women [5].
The presence of peripheral neuropathy, poor vision, and hypoglycemia further predispose subjects with diabetes to an increased risk of falls. Oral glucose-lowering medications such as thiazolidinediones may have an adverse effect on skeletal integrity. However, bone mineral density (BMD) which is a surrogate measure of bone strength is found to be elevated in patients with type 2 diabetes mellitus and is not necessarily reflective of the increased bone fragility inherent to diabetes. Some of the mechanisms postulated to cause an increase in BMD in individuals with diabetes include reduced bone turnover due to osteocyte dysfunction, accumulation of advanced glycation end products, impaired incretin response, and elevated sclerostin levels. Hyperinsulinemia and presence of obesity are also factors that contribute to an increase in BMD. Thus, measurement of BMD as a standalone test may not be a true indicator of bone strength in subjects with diabetes [6].
Despite a higher BMD, the increased fracture risk in subjects with diabetes has been attributed to deteriorated proximal hip geometry, increased cortical porosity, and degraded trabecular microarchitecture resulting in poor bone quality. Poor hip geometry in subjects with diabetes has previously been shown in the Baltimore Longitudinal Study, the Canadian Multicentre osteoporosis Study, and the Women’s Health Initiative observational study [7]. In healthy individuals, both physical activity and mechanical properties of the proximal hip are significant players determining bone strength. Although few studies have shown better BMD and hip geometric parameters in insulin-treated subjects, when corrected for lean mass, geometric indices of bone resistance to axial (cross-sectional area) and bending (section modulus) forces were significantly lower than in non-diabetic women. The exact mechanism underlying the poor hip geometry in subjects with diabetes is unclear although it appears that the presence of hyperglycemia tends to diminish the response of bone to mechanical stimuli [8].
The inherent limitations with regard to mere assessment of BMD in subjects with diabetes mellitus may result in poor capture of microarchitectural alterations and geometric changes, both of which contribute significantly to fracture risk. Trabecular bone score (TBS) is a novel densitometric tool that evaluates pixel gray-level variations in the lumbar spine DXA image, providing an indirect measure of bone microarchitecture [9].
TBS improves fracture-risk prediction beyond that provided by BMD and clinical risk factors, and can be incorporated to the Fracture Risk Assessment tool (FRAX) to enhance fracture prediction [10]. In patients with diabetes mellitus with paradoxically higher BMD, trabecular bone score may be a better predictor of fracture risk. Hip structural analysis (HSA) is also performed by the DXA and evaluates different variables pertaining to proximal hip geometry such as the cross-sectional area (CSA), cross-sectional moment of inertia (CSMI), section modulus (Z), and buckling ratio (BR) [11, 12]. These geometric indices are measured at each of three sites namely the narrow neck (NN), the inter-trochanteric area (IT), and the femoral shaft (FS). There is limited literature on the utility of HSA and TBS in assessing skeletal integrity in postmenopausal women with diabetes mellitus.
In this study, we aimed to assess DXA-derived parameters including TBS, BMD, HSA, and vertebral fractures as well as bone biochemistry in ambulatory South Indian postmenopausal women with type 2 diabetes mellitus and compare them with age- and BMI-matched non-diabetic controls recruited from the community.
Material and methods
This was a cross-sectional study conducted over 1 year in which ambulatory postmenopausal women with type 2 diabetes mellitus, aged 60 years and more, were recruited from the Endocrinology out-patient clinic. Age- and BMI-matched healthy control subjects without diabetes (HbA1C < 5.7%) were recruited from the community.
A simple random sampling method was utilized to recruit these subjects. This study was approved by the Institutional Review Board (IRB Min no. 12525). All subjects provided a written informed consent at the time of recruitment in the study. Postmenopausal women who were on treatment for osteoporosis, those with chronic kidney disease stages 4 and 5, those with secondary osteoporosis, and those taking medications known to affect bone health were excluded from the study. Among subjects with type 2 diabetes mellitus, those with Charcot’s osteoarthropathy were excluded. Diabetic nephropathy was diagnosed based on an elevated urinary albumin:creatinine ratio on a first-morning urine sample at two separate time points. Peripheral neuropathy was assessed using a 10-g monofilament testing on the dorsal aspect of the great toe bilaterally. Vibration perception threshold (VPT) was also examined by a single observer on the great toe of both feet using a biothesiometer. Neuropathy was diagnosed if the mean VPT as measured by the biotheosiometer was ≥ 25 V or if the pressure sensation from a 10-g monofilament was not perceived [13]. A subject was considered having retinopathy if any grade of retinopathy, including maculopathy, was detected by direct and/or indirect ophthalmoscopy in one or both eyes and/or on a more detailed assessment by an ophthalmologist.
The sample size was calculated from a previous study by Ho-Pham et al., which compared the mean TBS between postmenopausal diabetic women and age-matched controls. Based on this study, to obtain an estimated mean difference in TBS of 0.019 between both groups, with a 95% CI, and an alpha error of 5%, the sample size was calculated to be 172 in each of the cases and control groups [14].
Clinical assessment
All study participants were subjected to a detailed clinical evaluation that included duration and treatment of diabetes, assessment of anthropometric parameters such as height and weight by standard measures, and evaluation of complications of diabetes.
Biochemical parameters
Glycemic control was assessed by glycated hemoglobin (HbA1c), and the presence of diabetic nephropathy was diagnosed with serum creatinine and urine microalbumin. Fasting (overnight for 8 h) venous blood samples were collected for the measurement of serum calcium (N 8.3–10.4 mg/dL), phosphate (N 2.5–4.5 mg/dL), alkaline phosphatase (N 40–125 U/L), albumin (N 3.5–5.0 g/dL), creatinine (N 0.6–1.4 mg/dl), 25-hydroxy vitamin D (N 30–75 ng/mL), and intact parathormone (N 8–50 pg/mL). Serum calcium, phosphate, albumin, creatinine, and alkaline phosphatase were measured using colorimetric method with Beckman Coulter (Beckman Coulter AU 5800). An iced sample for intact parathormone (iPTH) was collected and estimated by chemiluminescence assay (Advia Centaur XPT immunoassay system), and 25-hydroxyvitamin D (vitamin D) was measured using electrochemiluminescence assay (Roche Cobas 6000 - Immunoassay system). Bone turnover markers - Plasma CTX (N: 226-1088 pg/mL in postmenopausal women) and P1NP (N: 16-73.9 ng/mL in postmenopausal women) were measured using electrochemiluminescence immunoassay (ECLIA) on a Roche Elecsys Modular E170 analyzer. Urine microalbumin was estimated by immuno-turbidimetry (N: < 30 mg/g of creatinine), and HbA1C was estimated by high-performance liquid chromatography (HPLC).
Dual-energy X-ray absorptiometry scan parameters
Bone mineral density
Areal BMD (g/cm2) at the femoral neck, total hip, and lumbar spine (L1-L4) were assessed using DXA scanner Hologic machine Discovery A series. The categorization of BMD into osteoporosis, osteopenia, and normal was done based on T-scores, as defined by the ISCD (International Society for Clinical Densitometry) guidelines [15].
Vertebral fracture assessment
Lateral spine images by fan-beam DXA for the assessment of vertebral fractures were used to evaluate for the presence of vertebral fractures. Images were obtained at the same time as that of BMD measurement. Prevalent vertebral fractures were classified as mild, moderate, and severe as follows [16].
-
Grade 0—normal
-
Grade 1—mildly deformed, approximately 20-25% reduction in anterior, middle, and/or posterior height
-
Grade 2—moderately deformed, approximately 25-40% reduction in anterior, middle, and/or posterior height
-
Grade 3—severely deformed, approximately 40% or greater reduction in anterior, middle, and/or posterior height
As there is less consistency in the diagnosis of mild (grade 1) fractures as compared to moderate (grade 2) and severe (grade 3) fractures [17], in this study, a subject was classified as having prevalent vertebral fractures if she was diagnosed to have either moderate or severe vertebral fractures or both.
Trabecular bone score (TBS)
TBS is a novel non-invasive method that evaluates pixel gray-level variations in the spine DXA image and helps in assessing the microarchitecture of the bone [18]. A TBS value of more than 1.350 indicates normal microarchitecture, 1.200–1.350 indicates partially degraded microarchitecture, and a TBS < 1.200 indicates degraded bone microarchitecture [19].
Hip structural analysis
Hip structural analysis (HSA) is a simple tool to determine bone strength at the proximal femur by geometric assessment [20]. The HSA program performs its analysis at 3 femoral sites using averages from 5 parallel lines 1 pixel apart across the cross-section of three sites [8, 20].
-
(1)
Narrow neck (NN), which is the narrowest point of the femoral neck
-
(2)
Inter-trochanteric region (IT), along the bisector of the angle of the axes of the neck and femoral shaft
-
(3)
Femoral shaft (FS), a site across the shaft at a distance of 2 cm distal to the midpoint of the lesser trochanter
The following four parameters of HSA were assessed in all the three sites:
-
a.
Cross-sectional area (CSA) excluding soft spaces in the marrow and pores—an index of resistance to axial forces (cm2).
-
b.
Cross-sectional moment of inertia (CSMI)—estimate of resistance to bending forces in a cross-section (cm4).
-
c.
Section modulus(Z)—an index of strength calculated as the CSMI ÷ the distance from the bone edge to the centroid (assumed here to be half the subperiosteal width) (cm3).
-
d.
Buckling ratio (BR)—index of susceptibility to local cortical buckling under compressive loads [21].
Statistical methods
Data were analyzed using SPSS v 24.0 (SPSS IBM Corp, USA). Continuous variables were expressed as mean and SD, and categorical variables were expressed as frequencies and percentages. The differences in means of continuous variables in the two groups were compared using Student’s t test for normally distributed parameters, and the Mann-Whitney test was used to compare the parameters that were not normally distributed. The differences in proportions were compared using the Pearson’s chi-square test or the Fisher exact test as appropriate. The relationship between two quantitative variables was assessed using the Pearson’s correlation coefficient. For all comparisons, a two-tailed P value of < 0.05 was considered statistically significant.
Results
Our study sample comprised a total of 202 ambulatory postmenopausal women with type 2 diabetes mellitus and 200 age- and BMI-matched non-diabetic controls recruited from the local community. The mean (SD) ages of cases and controls were 65.6 (5.2) years and 64.9 (4.7) years respectively. Among cases, the mean duration of diabetes was 11.0 (5.8) years. At baseline, the mean (SD) HbA1C of the cases was 7.5 (1.6) % and 60/202 (29.7%) of the subjects were on insulin therapy. The proportions of subjects with diabetic peripheral neuropathy, nephropathy, and retinopathy were 15%, 11%, and 10%, respectively.
The prevalence of vitamin D deficiency (< 20 ng/mL) was not significantly different in cases and controls (34.2% vs 35%; P=NS). The prevalence of osteoporosis at the hip (10.4% vs 14.3%) and the femoral neck (23.8% vs 32.7%) trended lower in cases as compared to controls. Although the prevalence of lumbar spine osteoporosis was significantly lower among cases (30.7%) as compared to controls (42.9%), the prevalence of degraded bone microarchitecture (TBS < 1.200) was significantly higher (P < 0.001) among cases (51%) as compared to controls (23.5%). Prevalent vertebral fractures (moderate and severe) were seen in 67/202 (33.2%) of the subjects and were not significantly different when compared to controls 52/200 (26%); P = 0.15. The markers of bone resorption (CTX—432.5 (197.9) vs 621.4 (284.5) pg/mL; P < 0.001) and bone formation (P1NP—30.1 (9.9) vs 68.3 (36.9) ng/mL; P < 0.001) were significantly lower among postmenopausal women with diabetes as compared to age- and BMI-matched non-diabetic controls. Other clinical and biochemical parameters, bone mineral density, trabecular bone score, and prevalent vertebral fractures were compared between cases and controls and are shown in Tables 1 and 2.
The various geometric indices of the proximal hip were measured using the hip structural analysis program and are shown in Table 3. It was found that most parameters of proximal hip geometry were significantly impaired in subjects with diabetes as compared to controls.
Further, bone biochemical parameters and the densitometric variables were compared between diabetic subjects with vertebral fractures and controls with vertebral fractures. It was found that markers of bone turnover were significantly lower in diabetic subjects with vertebral fracture as compared to non-diabetic subjects with vertebral fracture (CTX—414.6 (156.4) vs 626.0 (324.5) pg/mL; P < 0.001 and P1NP—30.3 (9.2) vs 69.4 (40.7); P < 0.001) (Table 4). Among the DXA-derived parameters, it was observed that the BMD at the femoral neck, hip, and lumbar spine were not significantly different between these groups of subjects (P = NS). However, the trabecular bone score and most parameters of proximal hip geometry were significantly impaired among diabetic subjects with vertebral fractures as compared to controls with vertebral fractures (P < 0.05) (Table 5).
In a sub-group analysis among cases, it was noted that the buckling ratio trended higher in subjects with an HbA1C ≥ 7.5% as compared to subjects with an HbA1C < 7.5% (11.6 (3.4) vs 10.7 (2.4) P = 0.05).
Discussion
This is the first study from India assessing comprehensive bone health including trabecular bone score (TBS), hip structural analysis (HSA), and prevalent vertebral fractures in ambulatory postmenopausal women with type 2 diabetes mellitus compared with age- and BMI-matched non-diabetic controls. In this study, it was found that the prevalence of osteoporosis at the femoral neck and hip trended lower among cases. The prevalence of degraded bone microarchitecture was significantly higher among cases as compared to controls, as opposed to the prevalence of lumbar spine osteoporosis which was significantly higher among non-diabetic controls. Moreover, the indices of proximal hip geometry were significantly impaired among subjects with diabetes as compared to controls. The prevalence of vitamin D deficiency and vertebral fractures were not significantly different between cases and controls. Among the bone biochemical parameters, it was found that both the CTX and the P1NP were significantly lower among postmenopausal women with diabetes than in non-diabetic controls. Moreover, in a sub-group analysis among subjects with vertebral fractures, it was found that most indices of hip geometry and the trabecular microarchitecture were significantly worse among postmenopausal women with diabetes as compared to non-diabetic controls.
In this study, the prevalence of osteoporosis at the femoral neck and hip was lower among subjects with diabetes as compared to those without diabetes. In a previous study done from the authors’ center, the prevalence of osteoporosis in postmenopausal women without diabetes was as high as 50% at any site [22]. Although the prevalence of osteoporosis at the lumbar spine was significantly lower among subjects with diabetes, the presence of degraded bone micro-architecture (TBS < 1.200) was more frequently encountered among subjects with diabetes as compared to non-diabetic controls. Schwartz et al. assessed BMD among postmenopausal women and showed that after adjustment for age and body mass index (BMI), there was a 2.9% higher BMD at femoral neck in subjects with diabetes mellitus as compared to those without diabetes mellitus [23]. In the abovementioned study, despite having a higher BMD, over 30% of subjects with diabetes mellitus sustained fragility fractures during a mean follow-up of 9.4 years. In a study done in a Korean population by Kim et al., similar findings were noted [24]. This implies that BMD may be a sub-optimal indicator for predicting fractures in subjects with diabetes mellitus. Hyperinsulinemia, obesity, and reduced bone turnover are the postulated mechanisms for a higher BMD observed in patients with type 2 diabetes mellitus. A meta-analysis confirmed the presence of discrepancy in BMD in subjects with type 1 and type 2 diabetes mellitus with the former showing a lower BMD than the latter [25].
A study assessing the correlation of bone quantity (BMD) and quality (TBS) with various insulin resistance–related parameters such as visceral adipose tissue, intrahepatic lipids, and homeostatic model assessment of insulin resistance (HOMA-IR) showed negative correlation between TBS and all these parameters, which was not observed with BMD [26]. Thus, in patients with type 2 diabetes mellitus where insulin resistance is a major player, TBS may be a better predictor of bone health [17, 27]. Previous studies by Leslie et al. and Ebrahimpur et al. have also shown a significantly low mean TBS in patients with diabetes mellitus [28, 29].
Prevalent vertebral fractures (moderate and severe) were seen in about one-third of the study subjects and were not significantly different when compared to non-diabetic controls, despite a significantly higher BMD among the postmenopausal women with diabetes. The prevalence of vertebral fractures in this cohort was high as compared to European and Brazilian studies which documented a prevalence of 23 to 25% vertebral fractures in postmenopausal women with diabetes mellitus [30, 31]. In a population-based study from southern India, among postmenopausal women after excluding those with self-reported diabetes mellitus, 36.7% had prevalent vertebral fractures (moderate and severe) [32]. The possible explanations for the high prevalence of vertebral fractures in south Indian postmenopausal women include a large proportion of individuals with undiagnosed osteoporosis and the lack of awareness among physicians and patients in identifying and treating osteoporosis [33]
Hip structural analysis (HSA) refers to the methodology used to assess bone strength based on the measurement of geometric characteristics in the proximal femur [34]. Low values of CSA, CSMI, and Z and a high BR denote poor hip strength and a higher tendency to fracture [35]. In the present study, it was observed that most indices of proximal hip geometry were significantly worse in subjects with diabetes as compared to non-diabetic controls. In a study by Lee et al., a buckling ratio of more than 10 was considered to have an adverse outcome [21]. Furthermore, in a sub-group analyses among subjects with vertebral fracture, it was found that the trabecular bone score and hip geometric parameters showed greater impairment despite similar BMD in subjects with diabetes as compared to controls.
In the current study, the bone turnover markers were significantly lower among cases as compared to controls. This is also in keeping with previous studies which have demonstrated that the bone turnover is suppressed in subjects with diabetes [36]. Pentosidine is an advanced glycosylation end product (AGE) that has been shown to have a negative association with the mechanical properties of femoral cortex and vertebra [37]. A study done by Yamamoto et al. showed that plasma pentosidine levels were significantly higher in postmenopausal women who had sustained vertebral fractures [38]. In our study however, assessment of pentosidine levels was not undertaken.
The key strength of this research work is that it is the first study from the Indian subcontinent comparing bone mineral parameters, bone mineral density, trabecular bone score, prevalent vertebral fractures, and hip structural analysis in postmenopausal women with and without diabetes. This study highlights the utility of the trabecular bone score and hip structural analysis in subjects with diabetes, where the bone mineral density tends to be paradoxically high, thus not adequately predicting fracture risk. This study, however, is limited by its inherent cross-sectional design and prospective studies may be undertaken to further validate these findings.
References
Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, Adhikari P, Rao PV, Saboo B, Kumar A, Bhansali A, John M, Luaia R, Reang T, Ningombam S, Jampa L, Budnah RO, Elangovan N, Subashini R, Venkatesan U, Unnikrishnan R, Das AK, Madhu SV, Ali MK, Pandey A, Dhaliwal RS, Kaur T, Swaminathan S, Mohan V, Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, Adhikari P, Rao PV, Saboo B, Kumar A, Bhansali A, John M, Luaia R, Reang T, Ningombam S, Jampa L, Budnah RO, Elangovan N, Subashini R, Venkatesan U, Unnikrishnan R, Das AK, Madhu SV, Ali MK, Pandey A, Dhaliwal RS, Kaur T, Swaminathan S, Mohan V, Sudha V, Parvathi SJ, Jayashri R, Velmurugan K, Borah PK, Rao SB, Padhiyar JM, Sharma S, Lalramenga P, Das SK, Singh TB, Kaki T, Basaiawmoit MR, Shukla DK, Rao MN, Joshi PP, Dhandania VK, Joshi SR, Yajnik CS (2017) Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR–INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol 5(8):585–596
Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, Mukhopadhyay S, Thomas N, Bhatia E, Krishnan A, Mathur P, Dhaliwal RS, Shukla DK, Bhansali A, Prabhakaran D, Rao PV, Yajnik CS, Kumar GA, Varghese CM, Furtado M, Agarwal SK, Arora M, Bhardwaj D, Chakma JK, Cornaby L, Dutta E, Glenn S, Gopalakrishnan N, Gupta R, Jeemon P, Johnson SC, Khanna T, Kinra S, Kutz M, Muraleedharan P, Naik N, Odell CM, Oommen AM, Pandian JD, Parameswaran S, Pati S, Prasad N, Raju DS, Roy A, Sharma M, Shekhar C, Shukla SR, Singh NP, Thakur JS, Unnikrishnan R, Varughese S, Xavier D, Zachariah G, Lim SS, Naghavi M, Dandona R, Vos T, Murray CJL, Reddy KS, Swaminathan S, Dandona L (2018) The increasing burden of diabetes and variations among the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health 6(12):e1352–e1362
Ferrari SL, Abrahamsen B, Napoli N, Akesson K, Chandran M, Eastell R et al (2018) Diagnosis and management of bone fragility in diabetes: an emerging challenge. Osteoporos Int 29(12):2585–2596
Paul TV, Thomas N, Seshadri MS, Oommen R, Jose A, Mahendri NV (2008) Prevalence of osteoporosis in ambulatory postmenopausal women from a semiurban region in Southern India: relationship to calcium nutrition and vitamin D status. Endocr Pract 14(6):665–671
Kaur P, Anjana RM, Tandon N, Singh MK, Mohan V, Mithal A (2020) Increased prevalence of self-reported fractures in Asian Indians with diabetes: results from the ICMR-INDIAB population based cross-sectional study. Bone. 135:115323
Starup-Linde J, Hygum K, Langdahl BL (2018) Skeletal Fragility in Type 2 Diabetes Mellitus. Endocrinol Metab (Seoul) 33(3):339–351
Choi YJ, Chung Y-S (2016) Type 2 diabetes mellitus and bone fragility: special focus on bone imaging. Osteoporos Sarcopenia 2(1):20–24
Garg R, Chen Z, Beck T, Cauley JA, Wu G, Nelson D, Lewis B, LaCroix A, LeBoff MS (2012) Hip geometry in diabetic women: implications for fracture risk. Metabolism. 61(12):1756–1762
Rajan R, Cherian KE, Kapoor N, Paul TV (2020) Trabecular bone score-an emerging tool in the management of osteoporosis. Indian J Endocrinol Metab 24(3):237–243
Hans D, Šteňová E, Lamy O (2017) The Trabecular Bone Score (TBS) complements DXA and the FRAX as a Fracture Risk Assessment Tool in routine clinical practice. Curr Osteoporos Rep 15(6):521–531
Beck TJ, Broy SB (2015) Measurement of hip geometry-technical background. J Clin Densitom 18(3):331–337
Ohnaru K, Sone T, Tanaka K, Akagi K, Ju Y-I, Choi H-J, Tomomitsu T, Fukunaga M (2013) Hip structural analysis: a comparison of DXA with CT in postmenopausal Japanese women. Springerplus. 2:331
Pop-Busui R, Boulton AJM, Feldman EL, Bril V, Freeman R, Malik RA, Sosenko JM, Ziegler D (2017) Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care 40(1):136–154
Ho-Pham LT, Nguyen TV (2019) Association between trabecular bone score and type 2 diabetes: a quantitative update of evidence. Osteoporos Int 30(10):2079–2085
Lewiecki EM, Binkley N, Morgan SL, Shuhart CR, Camargos BM, Carey JJ, Gordon CM, Jankowski LG, Lee JK, Leslie WD (2016) Best practices for dual-energy X-ray absorptiometry measurement and reporting: International Society for Clinical Densitometry Guidance. J Clin Densitom 19(2):127–140
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11(7):984–996
Rajan R, Paul J, Cherian KE, Asha HS, Kapoor N, Paul TV (2020) FRAX® with or without BMD and TBS predicts fragility fractures in community-dwelling rural southern Indian postmenopausal women. Arch Osteoporos 15(1):82
Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD Official Positions Part 2: Trabecular Bone Score. J Clin Densitom 18(3):309–330
Mirzaei A, Jahed SA, Nojomi M, Rajaei A, Zabihiyeganeh M (2018) A study of the value of trabecular bone score in fracture risk assessment of postmenopausal women. Taiwan J Obstet Gynecol 57(3):389–393
Broy SB, Cauley JA, Lewiecki ME, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA Measures: the 2015 ISCD Official Positions Part 1: Hip Geometry. J Clin Densitom 18(3):287–308
Lee T, Choi JB, Schafer BW, Segars WP, Eckstein F, Kuhn V, Beck TJ (2009) Assessing the susceptibility to local buckling at the femoral neck cortex to age-related bone loss. Ann Biomed Eng 37(9):1910–1920
Binu AJ, Cherian KE, Kapoor N, Jebasingh FK, Asha HS, Paul TV (2019) Bone health after fifth decade in rural ambulatory South Indian postmenopausal women. Indian J Community Med 44(3):205–208
Schwartz AV, Sellmeyer DE, Ensrud KE, Cauley JA, Tabor HK, Schreiner PJ, Jamal SA, Black DM, Cummings SR, Study of Osteoporotic Features Research Group (2001) Older women with diabetes have an increased risk of fracture: a prospective study. J Clin Endocrinol Metab 86(1):32–38
Kim JH, Choi HJ, Ku EJ, Kim KM, Kim SW, Cho NH, Shin CS (2015) Trabecular bone score as an indicator for skeletal deterioration in diabetes. J Clin Endocrinol Metab 100(2):475–482
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes--a meta-analysis. Osteoporos Int 18(4):427–444
de Araújo IM, Parreiras-e-Silva LT, Carvalho AL, Elias J, Salmon CEG, de Paula FJA (2020) Insulin resistance negatively affects bone quality not quantity: the relationship between bone and adipose tissue. Osteoporos Int 31(6):1125–1133
Harvey NC, Glüer CC, Binkley N, McCloskey EV, Brandi M-L, Cooper C et al (2015) Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone. 78:216–224
Ebrahimpur M, Sharifi F, Nezhad FA, Bagherzadeh M, Ostovar A, Shafiee G, Heshmat R, Mehrdad N, Razi F, Khashayar P, Nabipour I, Larijani B (2019) Effect of diabetes on BMD and TBS values as determinants of bone health in the elderly: Bushehr Elderly Health program. J Diabetes Metab Disord 18(1):99–106
Leslie WD, Aubry-Rozier B, Lamy O, Hans D (2013) TBS (Trabecular Bone Score) and diabetes-related fracture risk. J Clin Endocrinol Metab 98(2):602–609
Viégas M, Costa C, Lopes A, Griz L, Medeiro MA, Bandeira F (2011) Prevalence of osteoporosis and vertebral fractures in postmenopausal women with type 2 diabetes mellitus and their relationship with duration of the disease and chronic complications. J Diabetes Complicat 25(4):216–221
Raška I, Rašková M, Zikán V, Škrha J (2017) Prevalence and risk factors of osteoporosis in postmenopausal women with type 2 diabetes mellitus. Cent Eur J Public Health 25(1):3–10
Shetty S, John B, Mohan S, Paul TV (2020) Vertebral fracture assessment by dual-energy X-ray absorptiometry along with bone mineral density in the evaluation of postmenopausal osteoporosis. Arch Osteoporos 15(1):25
Thakur P, Kuriakose C, Cherian KE, Asha HS, Kapoor N, Paul TV (2020) Knowledge gap regarding osteoporosis among medical professionals in Southern India. J Eval Clin Pract 26(1):272–280
Beck T (2003) Measuring the structural strength of bones with dual-energy X-ray absorptiometry: principles, technical limitations, and future possibilities. Osteoporos Int 14(Suppl 5):S81–S88
LaCroix AZ, Beck TJ, Cauley JA, Lewis CE, Bassford T, Jackson R et al (2010) Hip structural geometry and incidence of hip fracture in postmenopausal women: what does it add to conventional bone mineral density? Osteoporos Int 21(6):919–929
Starup-Linde J, Vestergaard P (2016) Biochemical bone turnover markers in diabetes mellitus - a systematic review. Bone. 82:69–78
Saito M, Fujii K, Soshi S, Tanaka T (2006) Reductions in degree of mineralization and enzymatic collagen cross-links and increases in glycation-induced pentosidine in the femoral neck cortex in cases of femoral neck fracture. Osteoporos Int 17(7):986–995
Yamamoto M, Yamaguchi T, Yamauchi M, Yano S, Sugimoto T (2008) Serum pentosidine levels are positively associated with the presence of vertebral fractures in postmenopausal women with type 2 diabetes. J Clin Endocrinol Metab 93(3):1013–1019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Paul, J., Devarapalli, V., Johnson, J.T. et al. Do proximal hip geometry, trabecular microarchitecture, and prevalent vertebral fractures differ in postmenopausal women with type 2 diabetes mellitus? A cross-sectional study from a teaching hospital in southern India. Osteoporos Int 32, 1585–1593 (2021). https://doi.org/10.1007/s00198-021-05855-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-05855-0