Abstract
Purpose of Review
The purpose is to review current literature on pain management strategies from initial presentation to postoperative care on common fracture types.
Recent Findings
- Hip fractures benefit from use of multimodal pain control for early mobility and decreased narcotic requirement.
- Distal radius fracture pain during reduction can be managed with hematoma block. Postoperatively, a soft dressing is adequate, and use of a compression glove may improve pain control and edema.
- Ankle fractures can be reduced with hematoma block, though use of procedural sedation may reduce reduction attempts for fracture dislocations.
- Long bone fracture pain management is trending toward multimodal pain control. Though there is no high-quality evidence, concern that regional anesthesia may mask compartment syndrome has limited its use in high-risk fractures.
- The effect of NSAIDs on bone healing has not been conclusively demonstrated.
Summary
The literature is still inconclusive regarding superiority of either spinal or general anesthesia during operative treatment. Fracture pain control is complex and multifactorial, requiring nuanced clinical judgment in the face of mixed clinical findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
This article provides an overview of the management of pain associated with fractures, with an emphasis on updates to the literature within the past 3 years. It is broken down into sections based on fracture type: hip, distal radius, ankle, and long bone fractures. For each fracture type, pain management is addressed at the various stages of care, from initial presentation, through operative management, and discharge. The article is followed by a list of annotated references.
Hip Fractures
Hip fractures represent a major source of morbidity, mortality, disability, pain, and hospitalization in the geriatric population. Traditional pain management in this patient population is challenging due to physiologic changes associated with aging and increased number of comorbidities. Management of hip fracture pain has been the focus of much recent research. The most notable advances that have positively impacted clinical practice are demonstration of the efficacy of hip fracture protocols and utilization of blocks for multimodal pain control. Though tremendous advances have been made in understanding and optimizing geriatric hip fracture pain management, there is more work to be done in every stage of care.
This section will give an overview of hip fracture pain management from a patient’s initial presentation in the emergency room, to the peri-operative period, and finally through postoperative recovery and hospital discharge.
Rapid effective pain control upon presentation to the emergency room has been recognized as an important component of hip fracture management. Dementia and opioid-related side effects pose challenges to traditional systemic modes of acute pain control. Healthcare personnel have identified cognitive impairment as a significant barrier for effective pain management and patients with dementia have been shown to receive less pain medication than those who are unimpaired [1]. Optimizing pain control while reducing the adverse effects of systemic analgesics has been the focus of much research. Numerous studies have shown utilization of regional blocks to be superior to systemic analgesia alone for management of acute hip fracture pain.
A recent randomized controlled trial (RCT) demonstrated that use of femoral nerve block decreased preoperative pain and reduced opiate use in elderly hip fracture patients, including those with dementia [2•]. Fascia-iliaca compartment blocks (FICB) administered preoperatively decrease and delay analgesic consumption, reduce the amount of time required to administer preoperative spinal anesthesia, and provide superior pain control during movement compared with opioids [3]. Another RCT mirrored these findings and additionally showed that continuous FICB improved pain not only with movement but also at rest, increased patient satisfaction, and decreased nausea and vomiting, a common opioid side effect [4]. A majority of recent studies have utilized FICB for regional block in hip fractures; however, a blinded RCT of intra-capsular hip fractures demonstrated superior pain control with intra-articular hip injection (IAHI) as compared with FICB [5•]. In addition to femoral, fascia-iliaca, and intra-articular injection sites for regional blockade, a technique paper describes ultrasound-guided blockade of pericapsular nerve group (PENG) as a feasible alternative [6]. Implementation of an institution-wide geriatric hip fracture protocol that includes regional block in the emergency room has been shown to decrease time to first analgesia and reduce the quantity of morphine equivalents administered in geriatric hip fracture patients [7]. Other non-pharmacologic interventions that can help to improve patients preoperative comfort include initiation of bed rest and placement of a foley to minimize movement of the fractured extremity immediately upon diagnosis.
Though standard of care dictates that hip fractures should receive expedient operative fixation or arthroplasty to achieve pain control and reduce morbidity and mortality, there are circumstances in which comorbid conditions, overall prognosis, and patient/family preference may lead to a need for longer-term pain control in elderly non-surgical candidates. A case report describes pericapsular alcohol neurolysis of the articular branches of the femoral and obturator nerves providing excellent pain control in the terminal 2 months of an elderly non-surgical hip fracture patient’s life [8]. Though this has by no means been established as standard of care, it may represent an area of continued exploration for an otherwise very challenging clinical scenario.
There are numerous pain management considerations to be made during the operative management of hip fractures. Some of these considerations include use of spinal versus general anesthesia, addition of supplemental local or regional anesthesia, and type of operative intervention. Spinal anesthesia has gained popularity in recent years, though there is no consistent evidence to support its superiority over general anesthesia [9•]. Many elderly patients take anticoagulation or antiplatelet medications, which are often a contraindication to spinal anesthesia, thus the urgency of operative treatment necessitates use of general anesthesia for this group of patients. Risks of bleeding need to be weighed against the benefits of spinal or regional anesthesia. There is a multicenter RCT currently evaluating efficacy of spinal versus general anesthesia for operative treatment of hip fractures in patients over age 65 [10]. Results have yet to be published. Another multicenter RCT is currently underway comparing regional with general anesthesia on postoperative delirium (RAGA-delerium) in elderly patients undergoing hip fracture surgery [11]. The complex decision between spinal and general anesthesia for hip fracture repair is multifactorial and still under investigation.
Supplementation of either spinal or general anesthesia with local or regional anesthesia has also been explored as a component of multimodal pain control. As discussed earlier, peripheral nerve blocks placed in the preoperative period have been investigated extensively and consistently improve pain and reduce opioid usage. A Cochrane review of RCTs provides strong evidence that use of peripheral nerve blocks for hip fracture surgery reduces pain on movement, with an effect size proportional to the concentration of the local anesthetic used and it provides moderate evidence of decreased risk of pneumonia and reduced time to first postoperative mobilization [12]. Evidence supporting use of intraoperative local anesthesia is less robust, though a consensus paper outlining technique recommendations for the intra- and extra-capsular infiltration of local liposomal bupivacaine in hip fracture surgery has recently been published [13].
With respect to type of operative intervention, few decision-making discussions focus primarily on postoperative pain, but instead are geared toward the related issue of early mobilization. Non-displaced femoral neck fractures can be managed with either screw fixation or arthroplasty. A multicenter randomized controlled trial showed improved early mobility with hemiarthroplasty as compared with screw fixation but no difference in Harris Hip Score (HHS) or postoperative pain [14]. Intertrochanteric femur fractures require fixation with either sliding hip screw or intramedullary nail constructs. The goal in elderly patients is closed anatomic reduction and rapid stable fixation to minimize the stress of prolonged operative time and allow for early mobilization. A retrospective case-control study demonstrated increased postoperative pain in patients with lesser trochanter displacement > 1 cm post operatively [15]. Although lesser trochanter reduction is associated with increased operative time, it may be a worthwhile endeavor to minimize patient’s postoperative pain. The topic warrants further investigation. Finally, a retrospective review of hip fractures fixed with dynamic hip screw versus cemented hemiarthroplasty found increased pain and opiate consumption in patients receiving fixation as opposed to arthroplasty [16]. The conclusions of this study are limited by the significant confounding factor of fracture type influencing operative procedure. While intracapsular fractures, amenable to arthroplasty, are inherently more stable and less painful, extra-capsular fractures, which require fixation rather than arthroplasty, are less stable and therefore often more painful. The results of this paper, though potentially useful in anticipating postoperative pain management needs, cannot be directly applied to a discussion of fixation versus arthroplasty for purposes of pain control alone.
In the acute postoperative period, the goals of hip fracture pain management include adequate pain control to allow for early mobilization as well as minimizing the common complication of postoperative cognitive dysfunction. Inadequate postoperative pain control and cognitive dysfunction are problems that go hand in hand for elderly hip fracture patients. A 2019 prospective RCT demonstrated that elderly hip fracture patients with postoperative cognitive dysfunction (POCD) had higher VAS pain scores and cortisol levels 12 h after surgery than patients without POCD [17]. Though the association is not necessarily causal, this study highlights one of the complexities of pain control in this challenging population as both narcotic use and uncontrolled pain have been associated with postoperative cognitive dysfunction.
Multimodal pain control in the postoperative period helps to control pain and reduce narcotic use. As discussed above, the use of regional blocks has demonstrated efficacy in the immediate postoperative period. A 2018 meta-analysis of fascia iliaca compartment block for hip fracture included 11 studies and 937 patients, and found reduced total morphine consumption and reduction of pain intensity in the immediate postoperative period (1-8 h) but not at 72 h [18]. An RCT published that same year showed that immediate continuous femoral nerve block resulted in improved postoperative pain at rest but no improvement in pain with movement relative to traditional systemic pain control [19]. Postoperative administration of local anesthetic is rarely utilized and has not demonstrated similar effectiveness. A double-blind RCT showed no statistically significant reduction in pain or opioid consumption with use of long-acting local anesthetic administered for 6 doses in the 48 h following fracture fixation with sliding hip screw [20].
The association between pain and inflammation suggests the potential for non-pharmacologic adjuvant therapies targeting inflammation to be incorporated into postoperative multimodal pain control regimens for hip fracture patients; however, at this point in time little evidence supports their use. A cross-sectional study showed that levels of the inflammatory mediators IL-18 and TNF-alpha were positively associated with pain on postoperative day 3 in elderly patients with acute hip fractures [21]. Continuous-flow cryocompression, often used after elective arthroplasty, was investigated in a RCT of hip fracture patients and was found to have only mild analgesic effects 72 h after operative intervention. This study concluded that overall, continuous-flow cryocompression provided no added value in the acute recovery period for hip fracture patients [22]. Low-risk non-pharmacologic adjuvant therapies to reduce inflammation may warrant further investigation and can be relatively safely incorporated into postoperative hip fracture care; however, their efficacy has not yet been demonstrated.
For the hospitalized hip fracture patient, pain control can influence discharge status. Many hip fracture patients require discharge to a subacute rehabilitation facility or nursing home rather than discharge home. This final phase of care is less studied than the immediate perioperative period but is important to patients and their families as well as healthcare systems as a whole. Regional block with femoral nerve catheter has been shown to increase hip fracture patients’ chances of being discharged home rather than to a rehabilitation facility. Two studies published in 2017 demonstrated increased discharge home and decreased pain, narcotic consumption, and opioid-related side effects in hip fracture patients with continuous femoral nerve catheter as compared with those receiving standard analgesia [23, 24]. A retrospective study of hip fractures treated with hemiarthroplasty showed that the addition of intraoperative periarticular liposomal bupivacaine decreased patients’ length of stay and increased their likelihood of being ambulatory at discharge [25]. In spite of these benefits, however, these patients did not report decreased pain relative to those without intraoperative local anesthesia.
When hip fracture patients cannot be safely discharged home, continuity of pain management strategy from hospital to nursing home or subacute rehabilitation facility can be challenging. This is especially true, and of more significant concern when patients have cognitive dysfunction. A retrospective study of hospitalized patients with dementia demonstrated that > 50% experienced abrupt changes to analgesic regimens upon discharge to skilled nursing facilities [26]. Such abrupt changes can result in both uncontrolled pain and increased cognitive dysfunction upon discharge.
In conclusion, the vast majority of the recent research in fracture pain management has focused on geriatric hip fractures. By improving pain control and minimizing narcotic use in this population, the use of regional blocks in addition to systemic analgesia has been shown to improve mobility, reduce postoperative cognitive dysfunction, and optimize discharge disposition. In contrast to the strong evidence supporting the use of regional blocks, the evidence for use of local anesthesia for hip fractures is mixed. The decision between spinal and general anesthesia in the operating room is complex and still under investigation. With many institutions implementing standardized hip fracture protocols, it is of great importance that the advances in hip fracture analgesia be understood and incorporated into practice in order to facilitate safe, early, effective pain control and optimize outcomes for hip fracture patients.
Distal Radius Fractures
Distal radius fractures represent a common injury in adults. In patients over 65, these fractures often occur after a ground-level fall and the majority do not require operative treatment. Similar results are found at 1 year of follow-up no matter what treatment option was chosen [27]. In patients under 65, operative treatment is often considered for displaced, comminuted fractures; high-energy injuries and trauma patients with multiple injuries. The AAOS AUC (American Academy of Orthopaedic Surgeons Appropriate Use Criteria) can be applied in the decision making process (https://www.aaos.org/uploadedFiles/auc-treatment-distal-radius-fractures.pdf).
No matter what the treatment, pain with fractures is to be acknowledged and recognized. This article will cover the pain management of distal radius fractures in the emergency room and with surgical fixation with a volar locking plate.
Displaced distal radius fractures require a reduction. There are two main methods of pain control for the reduction. This includes a hematoma block or sedation. There are provider preferences, institutional and regional variances which may dictate one alternative over another. In addition, sedation carries additional risks of respiratory compromise which may influence the decision. Reducing a displaced fracture can result in improvement of pain and discomfort. The patient should be comfortable during the procedure and this should be a treatment goal.
Chen et al. completed an analysis of the literature on this topic. There were three studies on adult subjects included. During the reduction, there was no difference in the pain. However, post procedure, the adults receiving hematoma block had better reduction of pain [28•]. As mentioned, sedation carries more inherent risks and this paper found that the adverse events after reduction including nausea, vomiting, and respiratory distress were greater in those treated with procedural sedation anesthesia (PSA). The hematoma block was found to be an acceptable form of anesthesia in the reduction of distal radius fractures. Since this was a literature review, it is difficult to discern the reason. If a hematoma block is used, in many instances the inclusion of bupivacaine in the block can prolong the effect of the pain control. However, even a hematoma block can have risks. DeSilva et al. reported on seizures in a patient with a therapeutic dose [29]. Their patient was an elderly female, 88 years of age, and it is difficult to ascertain the contribution of additional comorbidities and advanced age is a known risk factor for lidocaine toxicity. The risk versus benefit decision-making tree most likely favored the hematoma block.
Once the fracture is reduced and decision made toward open reduction internal fixation (ORIF), postoperative pain control needs to be considered. These cases are most often outpatient procedures. We acknowledged earlier, each state has laws regarding postoperative opioid prescription and each state’s laws are foremost in consideration. The use of narcotics after multiple types of orthopedic procedures is under review. There are certain factors under surgeon control that may contribute overall to the use of narcotics post operatively.
Immobilization after ORIF of distal radius fractures varies from splinting to removable wrist splint to soft dressing. Surgeon preference is often the rationale in the decision-making. There is no evidence of untoward outcomes based on postoperative immobilization so if decisions can be made based on objective evidence regarding immobilization and pain control, another option to minimize pain can be considered.
Silva et al. evaluated use of opioids post operatively whether or not postoperative splint immobilization was used in a prospective randomized trial. This study was completed in Brazil, and there was a hospital stay after surgery. Those in the No Splint group had greater use of tramadol during the hospital stay and after, but this was not significant. The pain scores were similar at all time points assessed. There was no difference in functional results and complication rates [30•].
In a similar study conducted at the Rothman institute, use of a soft dressing resulted in improvements in ROM (range of motion), VAS (visual analogue scale) and functional outcomes fixed at final follow up with no differences in radiographic outcomes [31•]. Thus, it appears that use of a plaster splint after surgery does not result in improved outcomes and/or decreased narcotic use.
Another variable after distal radius fractures is the use of compression gloves post-operative. Milmam et al. evaluated their use during twice weekly physical therapy. Those who used the compression glove had decreased pain, swelling and analgesic use and were more active in normal activities of daily living [31•]. These results indicate a compression/edema glove could be helpful after surgery in reducing swelling, which then reduces pain and medication use.
To summarize, when treating distal radius fractures, in the emergency room a hematoma block is effective in reducing pain during reduction, and post operatively a soft dressing is adequate and a compression glove can be effective in decreasing swelling and pain.
Ankle Fractures
Ankle fractures occur from a variety of causes, including sports and trauma. There is a spectrum of severity. Most fractures can be treated in the outpatient setting. Often, a patient is seen in the emergency room, reduced and splinted as appropriate and scheduled for elective fixation. The use of a hematoma block (IAHB) versus procedural sedation (PS) was evaluated retrospectively by Lafferty et al., and multiple variables were evaluated. When there was an ankle fracture/dislocation, the use of PS resulted in a successful reduction with one attempt more often. However, the time to closed reduction was faster in patients with IAHB. Orthopedic surgeons were more successful on first reduction attempts compared with ED (emergency department) providers. Overall, both methods were successful, demonstrating that IAHB represents a viable option in ankle fracture reduction [32•]. This often was not considered a first-line treatment.
When the soft tissue swelling has subsided, surgery can be completed. Variables affecting time to surgery include the energy of injury, patient compliance with elevation and medical comorbidities to name a few. Many surgery centers and facilities offer peripheral nerve blocks as a mode of anesthesia and also as an adjunct to general anesthesia. There are concerns regarding rebound pain and if the nerve blocks actually reduce opioid consumption. Herling et al. completed a study in which they interviewed patients who received a nerve block after ankle fracture surgery who had peripheral nerve blocks as primary anesthesia. Patient understanding of a block and what to do as the block wore off were obstacles. Some patients reported rebound pain for up to 2 h, but most reported no or little pain. The benefits of peripheral nerve block as primary anesthesia provided mental alertness, ability to ambulate and had efficient pain relief. Education of patients was felt to be crucial for a good result [33•]. Currently, a Danish group is completing a randomized trial of peripheral nerve block versus spinal anesthesia for ankle fracture surgery [34]. The study is not completed yet.
The contributing factors to postoperative pain should be considered. Lee et al. completed an evaluation of factors contributing to postoperative pain by evaluating patient controlled anesthesia (PCA) use. The maximum pain was noted to be 8 h after fracture surgery, and the only factor significant in contributing to postoperative pain was the severity of the fracture [35]. With this knowledge, educating the patients regarding realistic pain expectations can be useful.
The use of non-steroidal anti-inflammatory medications (NSAIDS) after fracture surgery raises concerns for fracture healing. Potter et al. completed a meta-analysis of studies using NSAIDS after fracture surgery, both in adults and pediatric patients. They found there still is warranted concern for NSAID use after long bone fracture surgery and the occurrence of nonunion. However, short-term or low-dose exposure to NSAIDS after fracture surgery did not compromise fracture healing [36•].
Two recent studies evaluated use of perioperative and postoperative Ketorolac. A prospective study evaluated use of opioids (control) and use of Ketorolac and opioid’s (treatment group) perioperatively after ankle fracture surgery. The use of Ketorolac decreased opioid usage after ORIF of ankle fractures with mixed and minor effects on pain reduction. Fracture healing was not affected [37].
Daniel et al. evaluated perioperative Ketorolac administration in fracture healing. Patients received 20 tablets of 10 mg Ketorolac every 6 h after ankle fracture fixation. The results were promising demonstrating no cases of non-union and no significant differences in time to healing [38•]. Further studies on Ketorolac should be centered on pain scores and reducing opioid consumption.
To summarize, a hematoma block can be effectively used in reduction of ankle fractures. There are inadequate studies to determine the best anesthesia type, though peripheral nerve blocks can be a useful adjunct. With a fracture/dislocation, procedural sedation may result in decreased reduction attempts. Ketorlac may be used at least in the short term after fracture surgery without negative effects on fracture healing. Further studies are warranted.
Long Bone Fractures
The topic of pain management in long bone fracture care is broad and diverse. Long bone fractures occur from a variety of causes, impact a diverse patient population, and can be treated with a broad spectrum of management approaches. Whether low velocity fragility fractures in the elderly or high velocity blunt trauma in young healthy patients, long bone fractures are painful and can be associated with a diverse array of complications. Certain aspects of long bone fracture pain control have been implicated in some of these complications and must be taken into account when treating long bone fracture pain.
This section aims to provide the reader with a brief overview of the pain management considerations taken in treating long bone fractures of the upper and lower extremities, with a focus on associated complications.
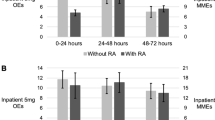
Following the trend in fracture care overall, there has been a focus on multimodal pain control and utilization of local and regional anesthesia as a means of achieving more effective pain management and minimizing narcotic use in patients with long bone fractures. The concern in many of these patients, especially high velocity tibia fractures, has been the potential for delayed diagnosis of compartment syndrome. Though numerous case reports of compartment syndrome in patients with regional anesthesia have been published, clinical studies are lacking. A systematic review of compartment syndrome following orthopedic surgical procedures with regional anesthesia and PCA showed that 75% of the case reports in the literature found no delay in diagnosis [39•]. Due to the low incidence and catastrophic implications of missed or delayed diagnosis, prospective studies of acute compartment syndrome in fractures with regional anesthesia would be challenging to obtain. Likewise, high-quality retrospective reviews are similarly challenging as illustrated by a large retrospective cohort study comparing regional/neuraxial anesthesia (RA/NA) and general anesthesia (GA) for low-velocity orthopedic lower extremity trauma surgeries. This study found that less than 10% of patients were given RA/NA and though they reported no difference in postoperative complication rates, compartment syndrome was not a variable included in the database and was thus not included in the analysis [40•]. There is a need for high-quality evidence to guide clinical practice regarding the use of regional anesthesia in patients at risk of compartment syndrome. In the absence of such evidence it is important to provide at-risk patients with adequate analgesia without masking the symptoms of an acute compartment syndrome and to monitor closely for increasing analgesia requirement.
NSAIDs are often used as an adjunct or alternative to narcotics for acute pain control. In the treatment of fracture pain, there is a much-debated risk of impaired bone healing with the use of NSAIDs. This has been demonstrated in animal studies, but the results of clinical trials have been mixed. A 2019 meta-analysis evaluating the effects of NSAIDs on bone healing in long bone and spine fractures found predominantly fair and moderate-quality retrospective studies, which limits the clinical application of findings and highlights the need for further research [41]. Another recent meta-analysis concluded that NSAID exposure correlates with delayed union or nonunion in long bone and other fractures. However, this effect was not present in low dose/short duration of exposure [36•]. Similarly, a single institution retrospective comparative study demonstrated that Ketorolac given in the first 24 h after fracture repair did not have a statistically significant impact on time to healing or incidence of nonunion for femoral or tibial shaft fractures [42••].
Pain management for fractures is complex and definitive conclusions from the literature cannot yet be made with respect to use of regional anesthesia in patients at risk for compartment syndrome or for the use of NSAIDs in fractures. There is no high-quality evidence of regional anesthesia placing patients at increased risk of delayed diagnosis of compartment syndrome; however, the physician must use his or her best judgment to appropriately dose and closely monitor all forms of analgesia in this patient population. The potentially detrimental effects of NSAIDs on bone healing has not been conclusively demonstrated in clinical studies; thus, their use in the immediate postoperative period as a means of improving pain control and reducing narcotic requirement is at the discretion of the physician.
Conclusion
Though systemic analgesia is the mainstay of fracture pain management, evidence is trending toward multimodal pain control, supplementation with regional anesthesia, and minimizing narcotic use. Evidence is lacking regarding superiority of either spinal or general anesthesia for lower extremity operative intervention. Fracture pain control is complex and multifactorial, requiring nuanced clinical judgment in the face of mixed clinical findings.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Moschinski K, Kuske S, Andrich S, Stephan A, Gnass I, Sirsch E, Icks A. Drug-based pain management for people with dementia after hip or pelvic.
• Unneby A, Svensson O, Gustafson Y, Olofsson B. Femoral nerve block in a representative sample of elderly people with hip fracture: A randomized controlled trial. Injury. 2017;48(7):1542–9 This randomized controlled trial showed that use of femoral nerve block led to lower preoperative pain scores and decreased opiate use in elderly hip fracture patients, including those previously diagnosed with dementia, who accounted for 45% of the study population.
Steenberg J, Møller AM. Systematic review of the effects of fascia iliaca compartment block on hip fracture patients before operation. Br J Anaesth. 2018 Jun;120(6):1368–80.
Ma YH, Wu J, Jia B, Xue JX, Wang TL. Continuous fascia iliaca compartment block combined with oral analgesics for preoperative pain control in elderly hip fracture patients. Zhonghua Yi Xue Za Zhi. 2018;98(10):723–7.
• Aprato A, Audisio A, Santoro A, Grosso E, Devivo S, Berardino M, et al. Fascia-iliaca compartment block vs intra-articular hip injection for preoperative pain management in intracapsular hip fractures: A blind, randomized, controlled trial. Injury. 2018;49(12):2203–8 This blind randomized controlled trial demonstrated that, as compared with facia-iliaca compartment block (FICB), intra-articular hip injection (IAHI) provided superior pain control during movement and decreased opiate use during the preoperative period for intra-capsular hip fractures.
Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular Nerve Group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43(8):859–63.
Casey SD, Stevenson DE, Mumma BE, Slee C, Wolinsky PR, Hirsch CH, et al. Emergency department pain management following implementation of a geriatric hip. Fracture Program. West J Emerg Med. 2017;18(4):585–91.
Sasaki S, Chan WS, Ng TK, Sham P. Ultrasound-guided pericapsular hip joint alcohol neurolysis for the treatment of hip pain: A case report of a novel approach. A A Pract. 2018;11(3):60–2.
• Cowan R, Lim JH, Ong T, Kumar A, Sahota O. The challenges of anaesthesia and pain relief in hip fracture care. Drugs Aging. 2017;34(1):1–11 This review article highlights the persistent inadequacy of pain relief in patients with hip fracture, reliance on systemic analgesia, and benefits of supplementation with regional analgesia. The decision regarding the appropriate choice of general versus spinal anaesthesia for hip fracture repair is multifactorial and complex, without consistent evidence in support one over the other.
Kowark A, Adam C, Ahrens J, Bajbouj M, Bollheimer C, Borowski M, et al. Improve hip fracture outcome in the elderly patient (iHOPE): a study protocol for a pragmatic, multicentre randomised controlled trial to test the efficacy of spinal versus general anaesthesia. BMJ Open. 2018;8(10):e023609.
Li T, Yeung J, Li J, Zhang Y, Melody T, Gao Y, et al. RAGA-Delirium Investigators. Comparison of regional with general anaesthesia on postoperative delirium (RAGA-delirium) in the older patients undergoing hip fracture surgery: study protocol for a multicentre randomised controlled trial. BMJ Open. 2017;7(10):e016937.
Guay J, Parker MJ, Griffiths R, Kopp SL. Peripheral nerve blocks for hip fractures: A cochrane review. Anesth Analg. 2018;126(5):1695–704.
Amin NH, Hutchinson HL, Sanzone AG. Infiltration techniques for local infiltration analgesia with liposomal bupivacaine in extracapsular and intracapsular hip fracture surgery: Expert panel opinion. J Orthop Trauma. 2018;32(Suppl 2):S5–S10.
Dolatowski FC, Frihagen F, Bartels S, Opland V, Šaltytė Benth J, Talsnes O, et al. Screw fixation versus hemiarthroplasty for nondisplaced femoral neck fractures in elderly patients: A multicenter randomized controlled trial. J Bone Joint Surg Am. 2019;101(2):136–44.
Sun Q, Ge W, Hu H, Li G, Wu J, Lu G, et al. The influence of position of the displaced lesser trochanter on clinical outcome of unstable trochanteric femur fractures in the elderly. Biomed Res Int. 2018;2018:5013646.
A’court J, Lees D, Harrison W, Ankers T, Reed MR. Pain and analgesia requirements with hip fracture surgery. Orthop Nurs. 2017;36(3):224–8.
Wang LW, Zhu MJ, Li Y, Wang ST, Zhou MY, Yu YJ, et al. FKBP51 is associated with early postoperative cognitive dysfunction in elderly patients undergoing hip fracture surgery. Medicine (Baltimore). 2019;98(5):e14037.
Hong HK, Ma Y. The efficacy of fascia iliaca compartment block for pain control after hip fracture: A meta-analysis. Medicine (Baltimore). 2019;98(28):e16157.
Rowlands M, Walt GV, Bradley J, Mannings A, Armstrong S, Bedforth N, et al. Femoral Nerve Block Intervention in Neck of Femur Fracture (FINOF): a randomised controlled trial. BMJ Open. 2018;8(4):e019650.
Bech RD, Ovesen O, Lauritsen J, Emmeluth C, Lindholm P, Overgaard S. Local anesthetic wound infiltration after osteosynthesis of extracapsular hip fracture does not reduce pain or opioid requirements: A randomized, Placebo-Controlled, Double-Blind Clinical Trial in 49 Patients. Pain Res Manag. 2018;2018:6398424.
Ko FC, Rubenstein WJ, Lee EJ, Siu AL, Sean MR. TNF-α and sTNF-RII are associated with pain following hip fracture surgery in older adults. Pain Med. 2018;19(1):169–77.
Leegwater NC, Bloemers FW, de Korte N, Heetveld MJ, Kalisvaart KJ, Schönhuth CP, et al. Postoperative continuous-flow cryocompression therapy in the acute recovery phase of hip fracture surgery-A randomized controlled clinical trial. Injury. 2017;48(12):2754–61.
Arsoy D, Huddleston JI 3rd, Amanatullah DF, Giori NJ, Maloney WJ, Goodman SB. Femoral nerve catheters improve home disposition and pain in hip fracture patients treated with total hip arthroplasty. J Arthroplasty. 2017;32(11):3434–7.
Arsoy D, Gardner MJ, Amanatullah DF, Huddleston JI 3rd, Goodman SB, Maloney WJ, et al. Continuous femoral nerve catheters decrease opioid-related side effects and increase home disposition rates among geriatric hip fracture patients. J Orthop Trauma. 2017;31(6):e186–9.
Hutchinson HL, Jaekel DJ, Lovald ST, Watson HN, Ong KL. Multimodal pain management of femoral neck fractures treated with hemiarthroplasty. J Surg Orthop Adv. 2019;28(1):58–62.
Gilmore-Bykovskyi AL, Block L, Hovanes M, Mirr J, Kolanowski A. Analgesic use patterns among patients with dementia during transitions from hospitals to skilled nursing facilities. Res Gerontol Nurs. 2019;12(2):61–9.
Bruyere A, Vernet P, Botero SS, Igeta Y, Hidalgo Diaz JJ, Liverneaux P. Conservative treatment of distal fractures after the age of 65: a review of literature. Eur J Orthop Surg Traumatol. 2018;28(8):1469–75. https://doi.org/10.1007/s00590-018-2150-x.
• Tseng PT, Leu TH, Chen YW, Chen YP. Hematoma block or procedural sedation and analgesia, which is the most effective method of anesthesia in reduction of displaced distal radius fracture? J Orthop Surg Res. 2018;13(1):62. https://doi.org/10.1186/s13018-018-0772-7The use of a hematoma block in reduction of adult distal radius fractures was shown to be safe and effective. There was adequate relief of pain when compared with PSA.
Dezfuli B, Edwards CJ, DeSilva GL. Distal radius fracture hematoma block with combined lidocaine and bupivacaine can induce seizures while within therapeutic window: a case report. J Orthop Case Rep. 2012;2(4):10–3.
• O’Neil JT, Wang ML, Kim N, Maltenfort M, Ilyas AM. Prospective evaluation of opioid consumption after distal radius fracture repair surgery. Am J Orthop (Belle Mead NJ). 2017;46(1):E35–40 This was a prospective study on consecutive adult patients who underwent ORIF of distal radius fractures to determine if fracture and patient characteristics affected opioid consumption. There was an inverse relationship between age and opioid consumption. There was more consumption in self pay and Medicaid patients, along with worse fracture classifications. These factors should be considered in prescribing practices.
• Miller-Shahabar I, Schreuer N, Katsevman H, Bernfeld B, Cons A, Raisman Y, et al. Efficacy of compression gloves in the rehabilitation of distal radius. Fractures: Randomized controlled study. Am J Phys Med Rehabil. 2018;97(12):904–10. https://doi.org/10.1097/PHM.0000000000000998This was a non-blinded, randomized clinical trial in which patients received standard physical therapy twice a week, and one group used compression gloves. The compression glove group demonstrated improved daily functioning and decreased adverse symptom occurrence.
• MacCormick LM, Baynard T, Williams BR, Vang S, Xi M, Lafferty P. Intra-articular hematoma block compared to procedural sedation for closed reduction of ankle fractures. Foot Ankle Int. 2018;39(10):1162–8. https://doi.org/10.1177/1071100718780693This was a retrospective review over an 11 year period. Both methods were viable options. The use of PS resulted in less attempts at reduction of ankle fracture dislocations.
• Henningsen MJ, Sort R, Møller AM, Herling SF. Peripheral nerve block in ankle fracture surgery: a qualitative study of patients’ experiences. Anaesthesia. 2018;73(1):49–58. https://doi.org/10.1111/anae.14088This study interviewed patients who received peripheral nerve blocks for ankle fracture surgery. The purpose was to evaluate the usefulness. Patients had a positive experience, but false expectations and understanding of the nerve block.
Sort R, Brorson S, Gögenur I, Møller AM. BMJ Open. 2017;7(5):e016001. https://doi.org/10.1136/bmjopen-2017-016001.
Won SH, Chung CY, Park MS, Lee SY, Suh YS, Lee KM. Characteristics of and factors contributing to immediate postoperative pain after ankle fracture surgery. J Foot Ankle Surg. 2018;57(5):890–3. https://doi.org/10.1053/j.jfas.2018.03.008.
• Wheatley BM, Nappo KE, Christensen DL, Holman AM, Brooks DI, Potter BK. Effect of NSAIDs on bone healing rates: A meta-analysis. J Am Acad Orthop Surg. 2019;27(7):e330–6. https://doi.org/10.5435/JAAOS-D-17-00727This meta-analysis evaluated NSAIDS on bone healing rates.,both in adults and pediatric patients. They found there still is warranted concern for NSAID use after long bone fracture surgery and the occurrence of nonunion. However, short term or low dose exposure to NSAIDS after fracture surgery did not compromise fracture healing.
McDonald EL, Daniel JN, Rogero RG, Shakked RJ, Nicholson K, Pedowitz DI, et al. How does perioperative ketorolac affect opioid consumption and pain management after ankle fracture surgery? Clin Orthop Relat Res. 2020;478(1):144–51. https://doi.org/10.1097/CORR.0000000000000978.
• McDonald E, Winters B, Nicholson K, Shakked R, Raikin S, Pedowitz DI, et al. Effect of postoperative ketorolac administration on bone healing in ankle fracture surgery. Foot Ankle Int. 2018;39(10):1135–40. https://doi.org/10.1177/1071100718782489This study found perioperative use of Ketorolac had a high rate of fracture union at 12 weeks (94%). It was a retrospective review.
• Driscoll EB, Maleki AH, Jahromi L, Hermecz BN, Nelson LE, Vetter IL, et al. Regional anesthesia or patient-controlled analgesia and compartment syndrome in orthopedic surgical procedures: a systematic review. Local Reg Anesth. 2016;9:65 This systematic review evaluates whether the use of regional anesthesia (RA) or patient-controlled analgesia (PCA) in orthopedic extremity procedures contributes to a delayed diagnosis of compartment syndrome (CS). Of the 28 case reports published after 2009, 75% concluded that RA does not increase risk of a delayed diagnosis of CS.
• Brovman EY, Wallace FC, Weaver MJ, Beutler SS, Urman RD. Anesthesia type is not associated with postoperative complications in the care of patients with lower extremity traumatic fractures. Anesth Analg. 2019;129(4):1034–42 This retrospective cohort study of >18,000 low velocity orthopedic lower extremity trauma patients found no significant differences in 30-day mortality and postoperative complications between regional/neuraxial anesthesia (RA/NA) and general anesthesia (GA), though only < 10% of these patients received RA/NA, with the majority receiving spinal anesthesia.
Ali MU, Usman M, Patel K. Effects of NSAID use on bone healing: A meta-analysis of retrospective case–control and cohort studies within clinical settings. Trauma. 2019:1460408619886211.
•• Donohue D, Sanders D, Serrano-Riera R, Jordan C, Gaskins R, Sanders R, et al. Ketorolac administered in the recovery room for acute pain management does not affect healing rates of femoral and tibial fractures. J Orthop Trauma. 2016;30(9):479–82 This single institution retrospective comparative study demonstrated that Ketorolac given in the first 24 h after fracture repair does not seem to have a negative impact on time to healing or incidence of nonunion for femoral or tibial shaft fractures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Cannada and Dr. Elsevier have no known conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Orthopedic Management of Fractures
Rights and permissions
About this article
Cite this article
Elsevier, H., Cannada, L.K. Management of Pain Associated with Fractures. Curr Osteoporos Rep 18, 130–137 (2020). https://doi.org/10.1007/s11914-020-00578-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-020-00578-3