Abstract
Purpose of Review
This review aims to clarify the current role of minimally invasive surgery in the treatment of rectal cancer, highlighting short- and long-term outcomes from the latest trials and studies.
Recent Findings
Data from previous trials has been conflicting, with some failing to demonstrate non-inferiority of laparoscopic surgical resection of rectal cancer compared to an open approach and others demonstrating similar clinical outcomes. Robot-assisted surgery was thought to be a promising solution to the challenges faced by laparoscopic surgery, and even though the only randomized controlled trial to date comparing these two techniques did not show superiority of robot-assisted surgery over laparoscopy, more recent retrospective data suggests a statistically significant higher negative circumferential resection margin rate, decreased frequency of conversion to open, and less sexual and urinary complications.
Summary
Minimally invasive surgery techniques for resection of rectal cancer, particularly robot-assisted, offer clear short-term peri-operative benefits over an open approach; however, current data has yet to display non-inferiority in terms of oncological outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer remains the third most common cancer in the world and the second leading cause of cancer-associated deaths in the USA, accounting for approximately 8% of all cancer deaths. Rectal cancer accounts for 38% of the total colorectal cancer incidence with an estimated number of 43,030 new cases diagnosed in 2018 [1]. Rectal cancer, from an oncologic standpoint, is defined as a tumor located within the distal 12–15 cm of the large intestine (proximal to the anal canal). Surgical resection is paramount for optimal results and its different approaches have been heavily debated over recent decades. Minimally invasive approaches for resection of malignant rectal tumors appear to be the new norm, with laparoscopic surgery being accepted as an alternative method to open surgery in patients who can tolerate pneumoperitoneum and without extensive adhesions from prior instrumentation, given its comparable short and long-term outcomes [2,3,4]. However, laparoscopic surgery has several limitations, highlighted by results from two recent randomized controlled trials (RCTs), which revealed higher rates of positive circumferential resection margins in laparoscopic surgery for rectal cancer than in open surgery [5, 6]. These findings might be related to the high degree of technical difficulty associated with working with straight and inflexible instruments in the narrow pelvic space, in addition to the availability of surgical expertise, and learning curves for surgeons performing these operations.
Robotic-assisted surgery has been proposed as an alternative to overcome these challenges since its inception in the field of colorectal surgery in the early 2000s [7, 8]. The advantages of robotic-assisted surgery include providing an immersive three-dimensional view, better ergonomics and enhanced dexterity with tremor filtration and motion scaling, instrument articulation, and a stable endoscope platform. These advantages were initially expected to translate into superior clinical, oncological, and functional outcomes in rectal cancer. However, results from a recently published RCT suggest that robotic-assisted surgery, when performed by surgeons with varying experience with this technique, does not confer an advantage in rectal cancer resection over conventional laparoscopy [9]. In this review article, we state an overview of current data on minimally invasive techniques for rectal cancer resection, with emphasis on the rapidly evolving robot-assisted surgery field.
Outcomes
Short-term Outcomes and Oncologic Parameters
The use of minimally invasive techniques for rectal cancer, including laparoscopy and robot-assisted surgery, has been extensively investigated and compared to open surgery. Evaluating intraoperative and postoperative complications has been essential for discussing the safety and adequacy of these approaches, as well as the capability of achieving optimal short-term oncologic parameters, such as intact total mesorectal excision (TME), adequate circumferential resection margin (CRM), distal margin, and number of harvested lymph nodes (HLN).
Long established benefits of laparoscopic surgery over an open approach include less intraoperative blood loss, earlier return of bowel function, shorter hospital length of stay, and lower 28-day morbidity [5, 6, 10, 11]. Data evaluating oncologic parameters of the resected specimen is more conflicting. Three large RCTs (COLOR II, CLASSIC, and COREAN) described no statistical difference of oncologic parameters when laparoscopic-assisted surgery was compared to open surgery for rectal cancer [3, 4, 12]. Conversely, the American ACOSOG Z6051 multicenter trial, which randomized 446 patients with stage IIA, IIIA, or IIIB rectal cancer, demonstrated that laparoscopic resection did not meet non-inferiority criteria for pathologic outcomes when compared to open approach [5]. Its endpoint, comparing gross and pathologic evaluation of the resected specimen, used clear distal and radial margins, and completeness of TME specimen as a combined assessment for optimal surgery. Similarly, a randomized controlled trial comprising 475 patients with T1–T3 low-rectal cancer less than 15cm from the anal verge, distributed between 24 different sites throughout Australia and New Zealand, compared laparoscopic surgery to open approach for rectal cancer, and failed to establish non-inferiority of a laparoscopic approach (ALaCaRT trial) [6].
Prospective data investigating robot-assisted surgery for rectal cancer is scarce. However, the Robotic vs Laparoscopic Resection for Rectal Cancer (ROLARR) trial described no significant differences between the two approaches [9]. The ROLARR trial was the first international, multicenter, randomized, unblinded, parallel-group trial comparing robot-assisted vs conventional laparoscopic surgery for the curative treatment of rectal adenocarcinoma (distal extent <15cm of the anal margin) by high anterior resection, low anterior resection, or abdominoperineal resection. Randomization of 471 patients was performed (234 to conventional laparoscopy and 237 to robotic-assisted surgery) and participating surgeons had to have previously performed at least 30 minimally invasive rectal cancer resections before taking part in the trial. The only absolute requirement of the surgical procedure was that the robot had to be used for the mesorectal dissection.
The primary endpoint of the ROLARR trial was rate of conversion to open surgery, defined as the use of a laparotomy incision for any part of the mesorectal dissection. In the conventional laparoscopic group, 12.2% of patients required conversion to open surgery, compared with 8.1% of the patients in the robotic-assisted group; however, this result was not statistically significant. The mean operative time was 37.5 min longer in the robotic-assisted group compared to the conventional laparoscopic group (mean operative time [SD], 298.5 [88.7] vs. 261 [83.34] min, respectively). Patient self-reported assessment of bladder and sexual function between baseline and 6 months was carried out in 351 of 466 cases (75.3%) utilizing the I-PSS, IIEF, and FSFI scores. The adjusted analysis comparing 6-month scores yielded no statistically significant differences between conventional laparoscopic surgery and robotic-assisted groups, which differs from previous studies that suggest recovery is earlier with a robotic-assisted approach [13, 14]. Other secondary endpoints such as pathologic outcomes, quality of the plane of dissection for the mesorectal area, postoperative complications, and hospital length of stay revealed no statistically significant difference between the groups.
A recently published retrospective analysis compared patients diagnosed with stage II or III rectal adenocarcinoma, who underwent rectal resection by an open approach vs. a minimally invasive surgical (MIS) approach. This study evaluated 31,190 patients from the National Cancer Database (NCDB), of which 16,455 (52.8%) underwent an open approach and 14,735 (47.2%) underwent a MIS approach [15]. The conversion rate was 15.6% for laparoscopic operations, compared to 7.4% for robotic-assisted. Interestingly, conversion rates decreased over the study period, possibly accounting for improved surgical techniques of the same operators. Furthermore, on univariate analysis, the MIS approach was associated with decreased rates of positive CRM (6.1% MIS vs. 8.4% open, p<0.001) and increased likelihood of examining > 12 lymph nodes (71.5% vs. 67.8%, p<0.001). Additionally, on multivariable analysis, the MIS approach was found to be an independent predictor of negative CRM (OR 0.82, 95% CI 0.72–0.94, p=0.03) and increased likelihood of examining >12 lymph nodes (OR 1.12, 95% CI 1.04–1.21, p=0.04) [15].
A recent network meta-analysis was conducted by Simillis et al., which included 6237 patients who underwent TME for rectal cancer by different techniques: 2350 open, 3276 laparoscopic, 561 robot-assisted, and 50 transanal [16]. Results from this series found no significant differences in intraoperative morbidity between these approaches nor conversion to open rates between laparoscopic and robot-assisted techniques. Of note, the open technique showed to have a significantly longer time to first flatus compared with robotic approach and longer time to first bowel movement and oral diet when compared with both laparoscopic and robotic approaches. Patients undergoing laparoscopic TME had a significantly longer hospital stay compared with robotic surgery by 0.9 days. Finally, histopathological outcomes were notable for significantly more incomplete TMEs with the laparoscopic approach. The robot-assisted approach was found to have significantly longer distal margins compared with open (7.6mm), laparoscopic (6.8mm), and transanal (6.8mm) techniques.
Long-term Oncologic Outcomes
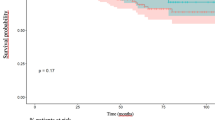
Laparoscopic surgery has comparable long-term outcomes to open surgery in the treatment of rectal cancer. The backbone of this conclusion results from data from 3 large randomized controlled trials, in which disease-free survival, overall survival, and quality of life, revealed no differences between the two groups [2,3,4, 17]. Although these results were very encouraging for supporters of minimally invasive surgery, no real superiority was ever demonstrated over an open technique (Table 1).
Well-described independent predictors of worse overall survival in patients undergoing rectal cancer resection, by any technique, include positive CRM, APR, age>65 years old, male sex, greater comorbidities, larger tumor size, poorly differentiated tumor grade, and advanced pathologic stage. The argument has been made that minimally invasive surgery can improve some of these parameters and results from the recently published ACOSOG Z6051 shed more light on the subject [18]. In this trial, the 2-year disease-free survival for patients who underwent laparoscopic resection was 79.5% and for open resection was 83.2%, with no statistical difference between groups. Similar rates were observed up to 4 years, with again no statistical difference. Additionally, disease-free survival was worse for patients with stage II/III rectal cancer who underwent APR, when compared with LAR. Local, regional, or distant recurrence was not significantly different between the laparoscopic approach and the open approach. Of note, unsuccessful surgery, influenced mostly by positive CRM, significantly increased the risk of recurrence. Results from the ACOSOG Z6051 trial, when interpreted in the setting of a novel technique such as robotic surgery that could decrease the rate of positive CRM significantly, helps to support the case of MIS approaches for the treatment of rectal cancer [18].
Long-term outcome data of patients undergoing rectal cancer resection through robot-assisted techniques are still limited. Recent data extracted from the National Cancer Database suggest that patients with stage II and stage III rectal adenocarcinoma, who underwent resection through an MIS approach, have improved 1-year and 5-year overall survival (OS) [15]. Rates of 1-year and 5-year OS were 95.0% and 69.8%, respectively, in patients who underwent an open approach, compared to 96.2% and 75.6%, respectively, in patients who underwent an MIS approach. Moreover, Cox proportional hazards analysis demonstrated that the MIS approach was independently associated with decreased risk of mortality (HR 0.90, 95% CI 0.83–0.98, p=0.01) compared to open surgery [19]. Other series describe no evidence of a significant difference between MIS and open approaches for 5-year overall survival, disease-free survival, or locoregional recurrence [16].
Sexual and Urinary Complications and Quality of Life
Due to the close proximity of the pelvic nerve bundles to the mesorectum and the difficulty in identifying anatomical structures such as the inferior hypogastric plexus in the narrow pelvis, sexual and urinary dysfunctions continue to be well-known complications of rectal cancer surgery. Open TME for rectal surgery has been associated with urinary dysfunction rates of 0–12% and sexual dysfunction rates of 10–35% [13, 20]. Laparoscopic surgery has resulted in similar, or even higher rates, of sexual dysfunction when compared to open surgery, with erectile dysfunction being consistently worse after a laparoscopic approach [21]. On the other hand, robotic surgery provides increased magnification and improved visualization when dissecting deep in the pelvis [22]. Kim et al. prospectively evaluated voiding and sexual function of 69 patients who underwent laparoscopic-assisted TME (n=39) or robot-assisted TME (n=30) over a 12-month period and reported that robot-assisted TME was associated with earlier recovery of normal voiding and sexual function, compared to laparoscopy [13]. In this series, patients who underwent laparoscopic surgery had 6 months of reduced urinary function compared to 3 months in the robotic group.
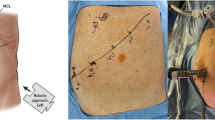
Challenges to Implementation
Several barriers have delayed the adoption of minimally invasive surgery as a standard of care for the management of rectal cancer. Technical difficulty, steep learning curves, and questionable cost-effectiveness are some of the key challenges. The pelvis is a narrow and deep space confined by osseous structures which make achieving an optimal oncologic TME, without injuring adjacent nerves, blood vessels, and ureters challenging. Non-articulating laparoscopic instruments and difficult stapler angulations add to the difficulty of the dissection, some of which are overcome by a robot-assisted approach. Nevertheless, adequate surgeon training is imperative. Most importantly, the need for more robust and decisive data showing clear benefits, or equivalence between the open and MIS techniques, is still lacking. Long-term survival data from the recent ACOSOG Z6051 and ALaCaRT trials might make it easier to adopt those techniques as the standard of care.
Learning Curve
Many of the aforementioned randomized controlled trials required surgeons to successfully perform 20–30 laparoscopic procedures prior to enrollment, as this was initially considered to be the learning curve required to become competent at a procedure [23]. SAGES suggests that proficiency in laparoscopic rectal surgery requires at least 50 cases [24,25,26,27], while several other studies report the learning curve for laparoscopic rectal surgery to be even greater, at between 50 and 90 cases [28,29,30]. Higher surgical volume has been shown to correlate with lower complication rates and reinterventions for early localized rectal cancer, suggesting that MIS rectal cancer operations should be performed, preferentially, in high-volume centers [31].
Interestingly, robotic surgery has been reported to have a shorter learning curve compared to the laparoscopic approach [10, 32]. Series using risk-adjusted cumulative sum analysis have demonstrated the learning curve for sphincter-preserving robotic rectal operation to reach a peak at the 52nd case [33]. Foo and colleagues described that the learning curve for robotic low-rectal resections of a novice surgeon with limited experience in open and laparoscopic rectal resection was 25 cases. [34] These results align with those previously published by Kim et al. whose group revealed that a surgeon with expertise in open colorectal surgery but lacking laparoscopic skills would achieve proficiency in robot-assisted rectal resection after 20 cases [35]. Additionally, it was shown that with increasing experience, over a 5-year study period, the rate of grade 3 mesorectal completeness increased from 61.4 to 90.7% (p=0.001). The rate of negative distal resection margin also increased significantly with time during the learning period (2.5 ± 1.7cm vs. 4.5cm ± 4.3cm, p=0.008) [33]. Interestingly and not surprisingly, different studies have repeatedly reported that surgeons experienced in laparoscopic colorectal surgery do not have a significant learning curve for robotic TME. Therefore, a robot-assisted approach might serve in achieving quicker proficiency during the teaching of this complex procedure to residents, more so if the dual console is utilized [36].
Costs
Another obstacle in the adoption of minimally invasive proctectomies is the cost of such procedures. Despite popular beliefs that laparoscopy costs more than open surgery, data actually suggest there is no difference in cost when comparing these different techniques [37]. On the other hand, numerous series have evaluated the dollars spent on robotic surgery and have largely concluded higher costs compared with an open or laparoscopic approach [38,39,40]. However, a more important measure should be valued, which can be defined as the ratio of health outcomes per dollar spent. Studies generally focus only on the cost of the index surgery and the index hospital admission, thereby failing to appreciate that the potential for robot-assisted surgery to generate benefit may extend beyond the index surgical admission. Justiniano and colleagues executed a population-based study to compare the 90-day cost and 90-day hospital utilization associated with 12,218 colorectal cancer resections by surgical approach [41]. After propensity adjustment, neither laparoscopic nor robotic surgery was significantly associated with decreased 90-day cost compared with open surgery for colorectal cancer in intention-to-treat analysis. In non-intention-to-treat analysis, robotic surgery, but not laparoscopic, was associated with significantly decreased 90-day cost (IRR 0.460, CI: 0.155, 0.775) compared with an open approach. Further prospective studies, evaluating its value in a more comprehensive manner, are in need to better assess the “costs” of implementing minimally invasive techniques for the treatment of rectal cancer.
Conclusion
In conclusion, the current evidence suggests that a minimally invasive approach for the treatment of rectal cancer has similar postoperative morbidity and short-term oncologic outcomes compared to open surgery. These results do not necessarily translate into long-term outcomes and more data is needed to assess long-term survival. In addition, exposure to MIS techniques during training is crucial to avoid long learning curves of this complex oncologic dissection. Finally, rectal cancer surgery should be individualized to each patient, preferably in a high-volume center, in the setting of multidisciplinary clinics.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. https://doi.org/10.3322/caac.21442.
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100:75–82. https://doi.org/10.1002/bjs.8945.
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014;15:767–74. https://doi.org/10.1016/S1470-2045(14)70205-0.
van der Pas MHGM, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WCJ, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013;14:210–8. https://doi.org/10.1016/S1470-2045(13)70016-0.
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, et al. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes the ACOSOG Z6051 randomized clinical trial. JAMA - J Am Med Assoc. 2015;314:1346–55. https://doi.org/10.1001/jama.2015.10529.
Stevenson ARL, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA - J Am Med Assoc. 2015;314:1356–63. https://doi.org/10.1001/jama.2015.12009.
Weber PA, Merola S, Wasielewski A, Ballantyne GH, Delaney CP. Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis Colon Rectum. 2002;45:1689–96. https://doi.org/10.1007/s10350-004-7261-2.
Hashizume M, Shimada M, Tomikawa M, Ikeda Y, Takahashi I, Abe R, et al. Early experiences of endoscopic procedures in general surgery assisted by a computer-enhanced surgical system. Surg Endosc Other Interv Tech. 2002;16:1187–91. https://doi.org/10.1007/s004640080154.
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer the rolarr randomized clinical trial. JAMA - J Am Med Assoc. 2017;318:1569–80. https://doi.org/10.1001/jama.2017.7219.
Liao G, Zhao Z, Lin S, Li R, Yuan Y, Du S, et al. Robotic-assisted versus laparoscopic colorectal surgery: a meta-analysis of four randomized controlled trials. World J Surg Oncol. 2014;12:122. https://doi.org/10.1186/1477-7819-12-122.
Li MZ, Bin XL, Wu WH, Bin YS, Li SZ. Meta-analysis of laparoscopic versus open colorectal surgery within fast-track perioperative care. Dis Colon Rectum. 2012. https://doi.org/10.1097/DCR.0b013e31824bd31e.
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AMH, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718–26. https://doi.org/10.1016/S0140-6736(05)66545-2.
Kim JY, Kim NK, Lee KY, Hur H, Min BS, Kim JH. A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol. 2012;19:2485–93. https://doi.org/10.1245/s10434-012-2262-1.
Park SY, Choi GS, Park JS, Kim HJ, Ryuk JP, Yun SH. Urinary and erectile function in men after total mesorectal excision by laparoscopic or robot-assisted methods for the treatment of rectal cancer: a case-matched comparison. World J Surg. 2014;38:1834–42. https://doi.org/10.1007/s00268-013-2419-5.
Lee GC, Bordeianou LG, Francone TD, Blaszkowsky LS, Goldstone RN, Ricciardi R, et al. Superior pathologic and clinical outcomes after minimally invasive rectal cancer resection, compared to open resection. Surg Endosc. 2020;34:3435–48. https://doi.org/10.1007/s00464-019-07120-2.
Simillis C, Lal N, Thoukididou SN, Kontovounisios C, Smith JJ, Hompes R, et al. Open versus laparoscopic versus robotic versus transanal mesorectal excision for rectal cancer: a systematic review and network meta-analysis. Ann Surg. 2019;270:59–68. https://doi.org/10.1097/SLA.0000000000003227.
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MHGM, de Lange-de Klerk ESM, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372:1324–32. https://doi.org/10.1056/nejmoa1414882.
Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA, et al. Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage ii to iii rectal cancer: follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg. 2019;269:589–95. https://doi.org/10.1097/SLA.0000000000003002.
Skancke M, Schoolfield C, Umapathi B, Amdur R, Brody F, Obias V. Minimally Invasive surgery for rectal adenocarcinoma shows promising outcomes compared to laparotomy, a National Cancer Database observational analysis. J Laparoendosc Adv Surg Tech. 2019;29:218–24. https://doi.org/10.1089/lap.2018.0471.
Kim NK, Aahn TW, Park JK, Lee KY, Lee WH, Sohn SK, et al. Assessment of sexual and voiding function after total mesorectal excision with pelvic autonomic nerve preservation in males with rectal cancer. Dis Colon Rectum. 2002;45:1178–85. https://doi.org/10.1007/s10350-004-6388-5.
Jayne DG, Brown JM, Thorpe H, Walker J, Quirke P, Guillou PJ. Bladder and sexual function following resection for rectal cancer in a randomized clinical trial of laparoscopic versus open technique. Br J Surg. 2005;92:1124–32. https://doi.org/10.1002/bjs.4989.
Luca F, Valvo M, Ghezzi TL, Zuccaro M, Cenciarelli S, Trovato C, et al. Impact of robotic surgery on sexual and urinary functions after fully robotic nerve-sparing total mesorectal excision for rectal cancer. Ann Surg. 2013;257:672–8. https://doi.org/10.1097/SLA.0b013e318269d03b.
A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004. doi:https://doi.org/10.1056/nejmoa032651.
Zerey M, Hawver LM, Awad Z, Stefanidis D, Richardson W, Fanelli RD. SAGES evidence-based guidelines for the laparoscopic resection of curable colon and rectal cancer. Surg Endosc. 2013;27:1–10. https://doi.org/10.1007/s00464-012-2592-x.
Park IJ, Choi GS, Lim KH, Kang BM, Jun SH. Multidimensional analysis of the learning curve for laparoscopic colorectal surgery: lessons from 1,000 cases of laparoscopic colorectal surgery. Surg Endosc Other Interv Tech. 2009;23:839–46. https://doi.org/10.1007/s00464-008-0259-4.
Li JCM, Hon SSF, Ng SSM, Lee JFY, Yiu RYC, Leung KL. The learning curve for laparoscopic colectomy: experience of a surgical fellow in an university colorectal unit. Surg Endosc. 2009;23:1603–8. https://doi.org/10.1007/s00464-009-0497-0.
Akiyoshi T, Kuroyanagi H, Ueno M, Oya M, Fujimoto Y, Konishi T, et al. Learning curve for standardized laparoscopic surgery for colorectal cancer under supervision: a single-center experience. Surg Endosc. 2011;25:1409–14. https://doi.org/10.1007/s00464-010-1404-4.
Son GM, Kim JG, Lee JC, Suh YJ, Cho HM, Lee YS, et al. Multidimensional analysis of the learning curve for laparoscopic rectal cancer surgery. J Laparoendosc Adv Surg Tech. 2010;20:609–17. https://doi.org/10.1089/lap.2010.0007.
Park IJ, Choi GS, Lim KH, Kang BM, Jun SH. Multidimensional analysis of the learning curve for laparoscopic resection in rectal cancer. J Gastrointest Surg. 2009;13:275–81. https://doi.org/10.1007/s11605-008-0722-5.
Kayano H, Okuda J, Tanaka K, Kondo K, Tanigawa N. Evaluation of the learning curve in laparoscopic low anterior resection for rectal cancer. Surg Endosc. 2011;25:2972–9. https://doi.org/10.1007/s00464-011-1655-8.
Jonker FHW, Hagemans JAW, Verhoef C, Burger JWA. The impact of hospital volume on perioperative outcomes of rectal cancer. Eur J Surg Oncol. 2017;43:1894–900. https://doi.org/10.1016/j.ejso.2017.07.009.
Yamaguchi T, Kinugasa Y, Shiomi A, Sato S, Yamakawa Y, Kagawa H, et al. Learning curve for robotic-assisted surgery for rectal cancer: use of the cumulative sum method. Surg Endosc. 2015;29:1679–85. https://doi.org/10.1007/s00464-014-3855-5.
Aghayeva A, Baca B. Robotic sphincter saving rectal cancer surgery: a learning curve analysis. Int J Med Robot Comput Assist Surg. 2020;16:e2112. https://doi.org/10.1002/rcs.2112.
Foo CC, Law WL. The learning curve of robotic-assisted low rectal resection of a novice rectal surgeon. World J Surg. 2016;40:456–62. https://doi.org/10.1007/s00268-015-3251-x.
Kim YW, Lee HM, Kim NK, Min BS, Lee KY. The learning curve for robot-assisted total mesorectal excision for rectal cancer. Surg Laparosc Endosc Percutaneous Tech. 2012;22:400–5. https://doi.org/10.1097/SLE.0b013e3182622c2d.
Bolger JC, Broe MP, Zarog MA, Looney A, McKevitt K, Walsh D, et al. Initial experience with a dual-console robotic-assisted platform for training in colorectal surgery. Tech Coloproctol. 2017;21:721–7. https://doi.org/10.1007/s10151-017-1687-8.
Ramji KM, Cleghorn MC, Josse JM, MacNeill A, O’Brien C, Urbach D, et al. Comparison of clinical and economic outcomes between robotic, laparoscopic, and open rectal cancer surgery: early experience at a tertiary care center. Surg Endosc. 2016;30:1337–43. https://doi.org/10.1007/s00464-015-4390-8.
Keller DS, Senagore AJ, Lawrence JK, Champagne BJ, Delaney CP. Comparative effectiveness of laparoscopic versus robot-assisted colorectal resection. Surg Endosc. 2014;28:212–21. https://doi.org/10.1007/s00464-013-3163-5.
Silva-Velazco J, Dietz DW, Stocchi L, Costedio M, Gorgun E, Kalady MF, et al. Considering value in rectal cancer surgery: an analysis of costs and outcomes based on the open, laparoscopic, and robotic approach for proctectomy. Ann Surg. 2017;265:960–8. https://doi.org/10.1097/SLA.0000000000001815.
Park JS, Choi GS, Park SY, Kim HJ, Ryuk JP. Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg. 2012;99:1219–26. https://doi.org/10.1002/bjs.8841.
Justiniano CF, Becerra AZ, Xu Z, Aquina CT, Boodry CI, Schymura MJ, et al. A population-based study of 90-day hospital cost and utilization associated with robotic surgery in colon and rectal cancer. J Surg Res. 2020;245:136–44. https://doi.org/10.1016/j.jss.2019.07.052.
Author information
Authors and Affiliations
Contributions
Leonardo E. Garcia: literature review, drafting article; James Taylor: literature review, revision of article; Chady Atallah: critical revision of the article, approval of article
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Gastrointestinal Cancers
Rights and permissions
About this article
Cite this article
Garcia, L.E., Taylor, J. & Atallah, C. Update on Minimally Invasive Surgical Approaches for Rectal Cancer. Curr Oncol Rep 23, 117 (2021). https://doi.org/10.1007/s11912-021-01110-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s11912-021-01110-1