Abstract
Purpose of Review
The present review will cover most recent and important studies on acute treatment of intracerebral hemorrhage (ICH).
Recent Findings
Overly pessimistic prognostication in ICH may deny meaningful recovery achieved by specialized neurocritical care. Hematoma enlargement represents the most important target of acute ICH care, which is reduced by aggressive blood pressure management (targeting a systolic blood pressure of 140 mmHg) and appropriate hemostatic treatment especially in anticoagulation-associated ICH (INR reversal using prothrombin complex concentrates, eventually idarucizumab, andexanet, or tranexamic acid). Surgical treatment strategies involving fibrinolytics either used for direct hematoma lysis or used for intraventricular clot removal with/without additional lumbar drainage show great promise. Further novel treatment strategies are underway and need validation or evaluation strongly warranting well-designed future ICH research.
Summary
Several randomized and large-sized observational studies have considerably expanded the field and the evidence on how to treat acute ICH patients. Yet, the one breakthrough intervention to improve functional outcome is still missing, though various treatment concepts possibly interacting with one another have been evaluated and such treatment bundle may improve patients’ outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
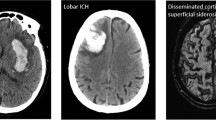
Spontaneous intracerebral hemorrhage (ICH) accounts for 10–15% of all strokes [1] and the worldwide incidence is expected to increase [2, 3]. Patients with ICH are severely affected as one-half dies within 30 days and only 12–39% reach long-term independency [4, 5]. The most important risk factor to develop primary ICH is arterial hypertension, which may lead to vasculopathy of small penetrating arteries located in the basal ganglia and thalamus or brain stem predisposing these regions for hemorrhagic complications [1]. Etiologically different may be lobar ICH, which is more frequently found in the elderly associated with cerebral amyloid angiopathy, characterized by deposition of amyloid-β, micro-hemorrhages, and vascular fragility leading to a greater risk for ICH and recurrence [1]. Anticoagulation-associated ICH has gained importance as the incidence is increasing in conjunction with patients requiring anticoagulation [1]. Important predictors of outcome—ICH volume, neurological status, and age—are non-modifiable; therefore, acute ICH management focusses on prevention and treatment of possibly modifiable factors such as hematoma enlargement (HE), peri-hemorrhagic edema development, acute hydrocephalus with intraventricular hemorrhage, and elevevated intracranial pressure (ICP) to avoid secondary brain injury [6]. Over the last years, several large clinical trials and observational studies provided new evidence, enhancing acute ICH care and improving our understanding of the underlying pathophysiology. In this review, we will outline, discuss, and interpret the latest advances and ongoing investigation.
Prognostication and Neurocritical Care
Full aggressive care over the first 48 h in all ICH patients is recommended according to the current AHA/ASA guideline, yet observational data suggests otherwise [6]. In up to 15% of patients, palliative care due to advanced directives or physicians judgment limits care before therapy is started [7•, 8]. Offering “full medical support” with avoidance of do not resuscitate (DNR) orders within the first 5 days resulted in a substantially lower mortality than predicted by the most commonly used prognostication model (absolute 30-day mortality difference of 29.8%) [9]. The problem is raised: do scores/scales limit treatment variability or do lead to a self-fulfilling prophecy by over-interpreting poor outcome? Early prognostication is difficult, always includes uncertainty, and may be confounded by physicians foreseeing a futile prognosis [7•, 10]. Lack of early improvement over 24 h predicts poor outcome [11] and early reassessments may be more accurate [12] but the optimal time point to validly prognosticate remains unclear. Therefore, efforts were made to design a potentially less biased and improved model to predict long-term outcome. The max-ICH Score was developed in a cohort of roughly 500 maximally treated ICH patients [7•] and was successfully validated in a prospective, multicenter cohort investigating over 2500 Chinese patients [13]. However, its clinical usefulness to reduce false poor outcome attribution has to be further evaluated [7•, 14]. Physicians should be aware that early care limitations may deny a meaningful recovery [6, 7•, 10], especially as dedicated neurocritical care was shown to significantly reduce death and dependency in ICH patients [15, 16]. The influence of a bundle of interventions including management of fever, hyperglycemia, and swallowing dysfunction improved patient outcomes in a cluster randomized trial (n = 1696) that investigated a mixed cohort of ischemic and hemorrhagic stroke patients and showed that 6.4 patients needed to be treated to gain functional independence for one more patient [17]. Furthermore, awareness should be heightened that functional improvements in ICH survivors may take place even up to 12 months, highlighting the importance and potential benefits of continued therapy [18].
Treatment of Hematoma Enlargement
Clinically significant HE, mostly defined as ICH volume increase of 33%, occurs in about one fourth of spontaneous ICH [19] and in 30–40% in anticoagulation-associated ICH [20••]. HE is one of the most important outcome parameters as it exemplifies a potential therapeutic target [19]. Patients at higher risk for HE may be identified by using contrast-enhanced computed tomography (CT) to depict the so-called spot sign; spot sign-positive patients showed a HE rate of 54.1% compared to 18.6% (spot sign negative) resulting in a negative predictive value of 78% (71–84) [21]. Recently, various other non-contrast CT parameters have been assessed for HE prediction, i.e., blend sign, fluid level, intrahematoma hypodensities, black hole sign, swirl sign, heterogeneous hematoma density, or irregular shape of ICH [22] (please see Fig. 1). Easily assessable parameters have been condensed to calculate a 5-point prediction score (BAT score: 1 point for blend sign, 2 points for any intrahematoma hypodensity, and 2 points for timing of CT scan < 2.5 h) which identified subjects at high risk of HE with good accuracy (AUC 0.65–0.70) and a BAT score ≥ 3 showed almost 90% specificity [23]. Another HE prediction model, the so-called BRAIN-Score, was developed from trial data (INTERACT-1 and INTERACT-2) also integrating clinical information (prior anticoagulation) and notably weighing time from symptom onset to diagnosis [24]. HE is caused by active bleeding during the hyper-acute phase; hence, knowledge of the time window is important as HE-limiting treatment shows greater potential the earlier applied [6]. Nevertheless, HE may occur protractedly up to 24 h or even longer (24–48 h) especially in patients with disturbed hemostasis, largely due to anticoagulation [25, 26]. Therefore, the two main therapeutic interventions to minimize HE constitute aggressive blood pressure and hemostatic management, which will be discussed in the following.
Contrast-enhanced (a) and non-contrast-enhanced (b–f) computed tomography signs predicting high risk of hematoma enlargement. a Spot sign—unifocal or multifocal contrast enhancement within the hematoma. b Blend sign—blending of hypoattenuating area next to hyperattenuating region within the hematoma, separated by a well-defined margin. c Swirl sign—any region of iso- or hypoattenuation (compared to brain parenchyma) within the hemorrhage. d black hole sign—Hypodense region with clear margins, encapsulated within the hemorrhage. e Fluid level—fluid blood level within the hemorrhage. f Irregular shape—no round or ellipsoid shape of hematoma, multicentric or separated hematomas; and Intrahematoma hypodensities—any hypodense region (compared to surrounding hemorrhage) encapsulated within the hematoma [22]. With kind approval by Prof. A. Dörfler, Department of Neuroradiology, University Hospital Erlangen, Germany.
Blood Pressure Management
Elevated blood pressure (BP) levels on hospital arrival are common in stroke patients (75%) and have been associated with HE, neurological deterioration, and poor outcome [27, 28]. Former beliefs that lowering BP may lead to peri-hemorrhagic ischemia due to the reduction of cerebral perfusion could be refuted by the ICH-ADAPT study (The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial). The study documented similar levels of perihematomal cerebral blood flow measured by CT perfusion imaging in patients randomized to targeting systolic BP of either < 150 mmHg (n = 39) or < 180 mmHg (n = 36) [29]. Large randomized controlled trials—INTERACT-1 [30] and ATACH-1 [31]—contributed to a certain safety profile for intensive BP control not leading to ischemic events but attenuated HE over 72 h [32]. Investigating 2839 patients, the INTERACT-2 (Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial 2) published in 2013 showed that intensive BP lowering (targeting systolic level of < 140 mmHg within 6 h after symptom onset) was not statistically effective in reducing the primary outcome (death or severe disability; odds ratio 0.87; 95% confidence interval [CI] [0.75–1.01]; p = 0.06) [33••]. Though, investigating outcome over the full range of the modified Rankin Scale (mRS) by ordinal regression analysis provided results in favor of the intervention (odds ratio 0.87; 95% CI [0.77–1.00]; p = 0.04) [33••]. This finding was not confirmed in the ATACH-2 (Antihypertensive Treatment of Acute Cerebral Hemorrhage 2) trial which was stopped prematurely for futility after an interim analysis of 1000 enrolled patients [34••]. Intensive blood pressure lowering through intravenous administration of nicardipine did not lead to improved outcome compared to standard care (mRS 4–6 after 3 months: intensive blood pressure lowering 38.7% vs standard care 37.7%; RR 1.04 [0.85–1.27]) and was associated with a greater number of serious adverse events, especially renal complications (serious complications, 25.6% vs 20.0%; RR 1.30 95% CI [1.00–1.69]; p = 0.05). In line, a recent prospective cohort study investigating 448 patient provided associations of pronounced systolic BP reduction (> 90 mmHg) with acute kidney injury in patients with normal renal function (OR 2.1; 95% CI [1.19–3.62], p = 0.010) and chronic kidney disease (OR 3.91; 95% CI [1.26–12.15], p = 0.019) [35]. However, ATACH-2 documented a statistical trend towards less HE (18.9% vs 24.4%, p = 0.09), but provided no evidence that patients with ICH and a spot sign, cerebral microbleeds, or other parameters associated with HE specifically benefited from intensive BP reduction in post hoc analyses [22, 36, 37]. Further, a recent post hoc analyses of the ATACH-2 trial showed that patients with reduction and maintenance of systolic BP levels below 140 mmHg over 24 h resulted in more patients exhibiting neurological deterioration within 24 h (10.4% vs 5.6%; relative risk, 1.98; 95% CI [1.08–3.62]) and showed higher rates of cardiac-related adverse events within 7 days (11.2% vs 6.4%; adjusted relative risk, 1.84; 95% CI [1.04–3.27]) [38]. Possible explanations of these divergent findings between the ATACH-2 and INTERACT-2 trials are that the control group of ATACH-2 was treated earlier and more aggressively per se, attaining systolic BP levels actually similar to the intervention arm of the INTERACT-2 trial (see Table 1 for further comparison of both trials). Another hyopothetical aspect may be related to class effects of medications used for BP control, as in ATACH-2 nicardipine was used first line per protocol versus only 16% in INTERACT-2. Dating back to the 1990s, available randomized data for the use of potent vasodilators such as calcium channel blockers (nimodipine) showed negative effects on outcome in stroke patients.
Nevertheless, meta-analyses of the five available randomized controlled trials provide strong reasoning for intensive BP lowering being associated with less ICH expansion (OR 0.82; 95% CI [0.68–1.00], p = 0.056), and possibly influencing clinical endpoints (3-month death or dependency risk: OR 0.91; 95% CI [0.80–1.02], p = 0.106) [39••]. Altogether, rapid BP lowering targeting a systolic pressure of 140 mmHg seems safe and should be recommended, but further lowering may increase adverse events and choice of medications used for BP control needs future evaluation.
Hemostasis
The main aim is to stop the ongoing bleed by hemostatic therapies and to identify patients who received antithrombotic medications to specifically tailor hemostatic treatment. Treatment in spontaneous ICH should promote hemostasis by increasing blood clot formation whereas treatment in anticoagulation or antiplatelet-associated ICH targets reversal of antithrombotic effects. The use of oral anticoagulation as well as its most feared complication is increasing, and for several of the new oral anticoagulants, specific reversal agents are no longer missing, though widespread available agents such as prothrombin complex concentrates may not be effective in restoring normal coagulation. In general, the coagulation cascade needs to be optimized by restoring missing factors or possibly improving function by essential electrolytes (magnesium and calcium), which have been inversely correlated with increased hematoma volumes suggesting potential associations [40•, 41, 42].
-
Spontaneous ICH
Mainly two hemostatic agents—recombinant factor VIIa and tranexamic acid (TXA)—have been investigated in spontaneous ICH. Recombinant factor VIIa (rFVIIa; NovoSeven) activates factors IX and X, promoting thrombin generation on the surface of activated platelets [43]. After promising phase 2 results [44], hope was dampened by the subsequent Factor Seven for Acute Hemorrhagic Stroke (FAST) trial [45]. This phase 3 trial confirmed a reduction of HE by rFVIIa, yet the intervention failed to improve survival or functional outcome [45]. The missing clinical benefit may partially be explained by an increased frequency of arterial thromboembolic events by 5%. The hypothesis that patients at high risk for HE (spot sign positive) might benefit from rFVIIa administration was also refuted by preliminary results from two parallel multicenter randomized controlled trials in Canada (SPOTLIGHT) and the USA (STOP-IT); preplanned pooled analysis presented at the International Stroke Conference 2017. According to data presented, rFVIIa treatment within 6 h of onset did not significantly alter final ICH volume or clinical outcomes compared to placebo among 69 spot sign-positive ICH patients.
TXA is an anti-fibrinolytic agent investigated mostly in trauma patients. The randomized controlled (CRASH-2) trial included over 20,000 trauma patients in 274 hospitals in 40 countries and documented a reduction of mortality (1463 [14.5%] vs 1613 [16.0%]; p < 0.01) among patients receiving TXA (loading dose 1 g over 10 min followed by infusion of 1 g over 8 h) within 8 h after injury [46]. The ongoing CRASH-3 trial will enroll 13,000 patients with isolated traumatic brain injury and will provide evidence regarding the influence of TXA on HE (ClinicalTrials.gov Identifier: NCT01402882). Most recently, robust data for treatment with TXA after spontaneous ICH was generated from the randomized placebo-controlled phase III TICH-2 trial [47••]. Investigating 1161 patients who received TXA versus 1164 who received placebo provided no significant benefit on the primary outcome defined as functional outcome measured by shift analyses of the modified Rankin Scale (ordinal OR 0.88, 95% CI [0.76–1.03], p = 0.11) [47••]. Though, fewer patients developed HE in the TXA group compared to the placebo group (265 [25%]) vs 304 [29%]; aOR 0.80, 95% CI [0.66–0.98], p = 0.03) [47••]. Pre-specified subgroup analyses categorized according to baseline systolic BP ≤ 170 mmHg versus >170 mmHg suggest a favorable outcome shift in patients with controlled BP receiving the intervention (OR 0.73, 95% CI [0.59–0.90], p = 0.02) [47••]. As there were no safety concerns, TXA still seems very promising for the reduction of HE, but the effect size seems smaller than anticipated. Several ongoing clinical trials [the Spot sign and TXA on Preventing ICH growth--Australasia Trial (STOP-AUST) [48]; the Tranexamic Acid for Spontaneous Acute Cerebral Hemorrhage Trial (TRANSACT); tranexamic acid for acute intracerebral hemorrhage growth predicted by spot sign trial (TRAIGE) [49]] will provide further details regarding TXA treatment in ICH patients.
-
Vitamin K antagonist-associated ICH
Vitamin K antagonists (VKA) inhibit the hepatic synthesis of vitamin K-dependent coagulation factors II, VII, IX, and X, as well as proteins C and S. HE in VKA-related ICH is more frequent than in primary ICH and occurs protractedly for up to 72 h after the initial event [25, 50]. Over the last years, large observational data and one clinical trial provided evidence on how to reverse anticoagulation in patients with VKA-related ICH.
The randomized, controlled INCH trial demonstrated superiority of prothrombin complex concentrate (PCC, 30 IU/kg) compared to fresh frozen plasma (FFP, 20 mL/kg)—both combined with vitamin K (10 mg i. v.)—with respect to normalizing the INR (INR ≤ 1.2 within 3 h: PCC 67% vs FFP 9%; OR 30.6 [4.7–197.9]; p = 0.0003) in patients with VKA ICH (INR ≥ 2 on admission; inclusion within 12 h after symptom onset) [51•]. The trial was prematurely stopped after inclusion of 50 of the 74 initially planned patients related to safety concerns in FFP-treated patients [51•] as hematoma volume increased significantly (ICH volume difference 16.4 mL, 95% CI [2.9–29.9]; p = 0.018) and the risk for HE or death was almost five times greater with FFP treatment. Rates of thromboembolic complications were comparable between both groups [51•]. A German-wide retrospective cohort study RETRACE (n = 1176) investigated reversal management targets to minimize HE. Patients achieving an INR< 1.3—regardless of chosen hemostatic treatment (almost 90% with PCC alone or in combination)—had significantly reduced rates of HE (INR< 1.3, 26.9% vs INR≥ 1.3, 45.4%; p < 0.001) [20••]. The positive effect of anticoagulation reversal was observed up to approximately 4 h after hospital admission (INR< 1.3 within 4 h, 22.4% vs 42.2%; p = 0.02), but was more pronounced the earlier achieved [20••]. The most potent reduction of HE with beneficial effects on in-hospital mortality (OR 0.60, 95% CI [0.37–0.95]; p = 0.03) was achieved by the combination of optimal reversal management and BP control. These results were also reproduced for patients with implanted mechanical heart valves and VKA-related ICH without showing a feared increase in thromboembolic complications with full reversal (RETRACE study-program) [52]. Given the limited half-life of coagulation factors compared to VKA, serial INR monitoring, simultaneous administration of vitamin K, and if necessary repeated replacement of coagulation factors are recommended [6]. As the thromboembolic risk in patients with mechanical heart valves is reported to be high (up to 1% per day), uncertainty exists regarding the optimal timing of resuming systemic anticoagulation after ICH. The authors of this German-wide multicenter study showed that restarting therapeutic anticoagulation after 2 weeks after ICH may be safe and after weighing between least risks for thromboembolic and hemorrhagic complications an earliest starting point for anticoagulation after 1 week may be considered, which should only be reserved for patients with highest thromboembolic risk (two valves, old valve types, concomitant atrial fibrillation, etc.) [52].
Altogether, effective (INR< 1.3) reversal of anticoagulation is mandatory in VKA ICH and should take place as quick as possible (at least within 4 h) using intravenous prothrombin concentrates (PCC) with additional substitution of vitamin K.
-
Non-vitamin k antagonist oral anticoagulant-associated ICH
Non-vitamin K antagonist oral anticoagulants (NOACs) inhibit either thrombin (dabigatran) or factor Xa (rivaroxaban, apixaban, edoxaban). The risk of intracranial hemorrhage in patients using NOACs is reduced compared to VKA; however, ICH severity, rates of HE, and functional outcome are likely to be comparable [53•, 54,55,56]. However, two recent larger observational studies reported that NOAK patients had smaller hematoma volumes and were less severely affected possibly resulting in lower mortality rates [57, 58]. In line large registry data from the Get With The Guidelines program reported lower risk of in-hospital mortality (adjusted risk difference, − 5.7% [97.5% CI − 7.3% to − 4.2%]) in patients with prior use of NOACs compared to prior warfarin use [59]. Although the half-life of NOACs is relatively short (5–17 h), waiting is not an option and aggressive hemostatic treatment should be executed, especially as patients with effective NOAC intake can reliably be identified using point-of-care testing methods [60].
Reversal of dabigatran using the licensed monoclonal antibody fragment idarucizumab (Praxbind) was investigated by the multicenter, prospective, single-arm open-label study RE-VERSE AD. Intravenous idarucizumab (5 g) was effective in reversing anticoagulation effects, i.e., normalizing coagulation test results (dilute thrombin time and ecarin clotting time), which was achieved in every included patient with serious bleeding (group A, n = 285; including 98 patients with intracranial hemorrhage) or requiring an urgent surgical procedure (group B, n = 196) [61••]. There were low rates of thrombotic events (6.3% in group A and 7.4% in group B) reported, but no controlled group for comparison [61••]. Effect of Praxbind treatment on imaging or clinical endpoints remains unclear as no detailed analyses are available for patients with intracranial hemorrhages. Yet, theoretically comparing 30 day mortality rates of patients experiencing intracranial hemorrhages under dabigatran from the RE-LY trial (no Praxbind treatment; mortality rate 37.5%, n = 24/64) with patients from the REVERSE-AD study (treated with Praxbind, mortality rate 16.4%) suggests potential benefits for idarucizumab with a reduced mortality rate.
Reversal management of factor Xa inhibitors may change in the very near future. The recombinant modified human factor Xa decoy protein andexanet (andexanet alfa), administered as a bolus followed by a 2-h infusion, showed reduction of anti-factor Xa activity in patients with acute major bleeding in the multicenter, prospective, open-label, single-group ANNEXA-4 study including 67 patients [62]. Most recently, the FDA granted approval of andexanet in the USA for treatment of life-threatening or uncontrolled bleeding under rivaroxaban and apixaban, supported by a newly supplied interim analyses of the ongoing ANNEXA-4 trial and data from two phase 3 studies (ANNEXA-R and ANNEXA-A) [63]. Approval in Europe is pending but anticipated, given the limited alternatives to reverse factor Xa inhibitors. Recently, a large multicenter investigation (n = 1328) documented that PCC administration was not associated with reduced HE rates, neither in overall NOAC-related ICH nor in patients using factor Xa inhibitors [53•]. The potential of other agents such as TXA is currently under investigation (Swiss TICH-NOAC trial; NCT02866838).
Therefore, patients with NOAC-associated ICH should receive reversal agents as quickly as possible. Patients using dabigatran should receive bolus injections of idarucizumab (2 × 2.5 g). Patients with ICH under factor Xa inhibitors should receive andexanet (if available); otherwise, given the lack of alternatives, PCC administration in high dosing (≥ 50 IU/kg) can be considered.
-
Antiplatelet-associated ICH
Latest evidence derives from the multicenter, randomized PATCH (platelet transfusion vs standard care after acute stroke due to spontaneous cerebral hemorrhage associated with antiplatelet therapy) trial conducted at 60 hospitals in the Netherlands, the UK, and France investigating 190 spontaneous primary ICH patients taking antiplatelet medication. Platelet transfusion was inferior to standard care and increased the odds of death or dependence at 3 months (odds ratio 2.05, 95% CI [1.18–3.56]; p = 0.01) [64•]. Poor outcome was likely driven by higher rates of serious adverse events (40 [42%] vs 28 [29%]), albeit the clear mechanism explaining this finding remains unclear [64•]. Thus, platelet transfusion cannot be recommended for treatment of antiplatelet-associated ICH.
Hematoma Evacuation Surgery
The rationale behind hematoma evacuation in ICH comprises immediate reduction of the space-occupying effect due to hematoma removal, prevention of acute herniation, amelioration of edema development, and reduction of toxic blood components potentiating inflammation and local ischemia. However, the role of hematoma evacuation surgery in ICH remains controversial.
Supratentorial ICH
Two multicenter randomized controlled trials showed, neither in patients with spontaneous supratentorial ICH patients with a minimum hematoma diameter of at least 2 cm and a Glasgow Coma Score of 5 or more (STICH-I) [65] nor in conscious patients with superficial lobar intracerebral hemorrhage of 10–100 mL without intraventricular hemorrhage (STICH-II) [66], that functional outcome was significantly improved after hematoma evacuation surgery via open craniotomy. Less invasive methods are currently under investigation. The MISTIE (Minimally Invasive Surgery Plus rt-PA for Intracerebral Hemorrhage Evacuation) program evaluated minimally invasive catheter evacuation followed by thrombolysis with rtPA. Results of this phase 2 randomized study including 96 subjects showed no difference in primary safety outcomes, i.e., mortality, symptomatic bleeding, brain infections, and withdrawal of care, in patients receiving the intervention. Beneficial associations were less peri-hemorrhagic edema development and a statistical trend for improved functional outcome after 6 months [67••]. However, increased asymptomatic bleeding was a major cautionary finding (3 [7%] vs 12 [22%]; p = 0.05) [67••]. The ongoing phase 3 MISTIE-III trial (NCT01827046) will investigate the efficacy to improve functional outcome in 500 ICH patients. Another minimally invasive method using an endoscopically guided suction device is also currently under investigation in a single-arm feasibility study (INVEST; NCT02654015) enrolling 50 patients in the USA. Another concept is oriented towards decompressive craniectomy similar to patients with malignant middle cerebral artery infarction (SWITCH; NCT02258919).
Infratentorial ICH
Larger infratentorial ICH may quickly lead to brainstem compression and acute obstructive hydrocephalus. Therefore, guidelines suggest that patients with cerebellar hemorrhages > 3 cm in diameter or with brainstem compression or hydrocephalus should undergo surgical hematoma evacuation [6]. This suggestion is mainly based on small observational, non-randomized studies and the benefit of hematoma evacuation surgery on clinical endpoints is not established [68, 69]. A randomized controlled trial comparing surgery versus conservative treatment seems unlikely to be conducted [6]. There was one small randomized trial which compared large suboccipital craniectomy to paramedian suboccipital mini-craniectomy without showing significant difference in postoperative outcomes between both groups [70]. One recent retrospective study including 85 patients documented that surgical removal of the spontaneous cerebellar hematoma by a large craniectomy, dura enlargement, and removal of the posterior arch of C1 leads to lower mortality and showed a trend towards superior neurological recovery and functional outcome compared to evacuations via craniotomy alone [71]. The management of an acute hydrocephalus with an external ventricular drainage (EVD) alone is considered insufficient by ICH guidelines due to the possible risk of upward herniation, but this recommendation is not sufficiently backed by robust data and seems somewhat contradictory to the management approach recommended for large infratentorial infarctions [6, 72].
Altogether, hematoma evacuation surgery after ICH cannot be recommended on a general basis in supratentorial ICH, but promising strategies (minimally invasive or decompressive procedures) are currently under investigation. Surgery in space-occupying infratentorial ICH seems logical to save lives, yet data quality is limited.
Peri-hemorrhagic Edema
The development of peri-hemorrhagic edema after ICH is common and related to early neurological deterioration and unfavorable functional outcome [73]. The acute phase of edema development is characterized by extravasation of osmotic factors from the blood clot leading to vasogenic edema [74]. Consecutively, edema may be aggravated by release of inflammatory mediators due to hemolysis and activation of the coagulation cascade, leading to a mixed cytotoxic and vasogenic edema [74]. This delayed phase may be a treatment target as progressive edema formation may lead to direct peri-lesional damage, and raised ICP resulting in decreased cerebral perfusion aggravating secondary brain damage [74]. Potential treatment approaches consist of osmotic substances such as mannitol, hypertonic saline infusion, deferoxamine or anti-inflammatory drugs, and interventions such as mild hypothermia or above-mentioned decompressive surgery. Until now, evidence is scant regarding effect and safety of any of the above-mentioned treatments.
A sub-analysis of the INTERACT-2 study documented an association between mannitol treatment and reduced rates of poor outcome in patients with larger (≥ 15 mL) hematomas (OR, 0.52, 95% CI [0.35–0.78] vs OR, 0.91, 95% CI [0.72–1.15]; p homogeneity 0.02) [75]. However, matching 304 hyperosmolar-treated cases to 304 untreated cases from a large prospective observational study showed more frequent poor outcome (73.0% vs 65.8%) and higher mean mRS at 3 months among patients treated with hyperosmolar therapy compared to untreated cases (Wilcoxon, p = 0.0174) [76]. Yet, it seems possible that selection bias may not have been fully accounted for [76].
Therapeutic hypothermia was assessed in a retrospective, single-center, case-control study investigating 70 patients in which early hypothermia (target temperature 35 °C) led to a decrease of peri-hemorrhagic edema if started within 3 days after hospital admission [77]. Potential benefits on clinical outcome were documented in a small prospective study which included 25 patients with an ICH volume > 25 mL showing a decreased mortality compared to historical controls (mortality after 1 year, 28% vs 44%) [78]. Treatment of fever is strongly recommended, but therapeutic hypothermia using cooling devices is still under investigation, TTM-ICH [79, 80].
Deferoxamine is an iron-chelating agent with limited data in ICH patients. Two small prospective studies—one observational, one randomized—showed no differences for functional outcomes but a potential effect on edema size [81]. The use of oral fingolimod—a sphingosine 1-phosphate receptor modulator—within 72 h of disease onset to modulate inflammatory processes after small- to moderate-sized ICH showed promising results in a proof-of-concept study including 23 patients [82]. Administration of fingolimod appeared to be safe and reduced peri-hemorrhagic edema resulting in more frequent full neurologic recovery (modified Barthel Index score range, 95–100; 63% vs 0%; p < 0.01; mRS range, 0–1; 63% vs 0%; p < 0.01) [82]. The efficacy and safety of fingolimod for acute ischemic and hemorrhagic stroke are currently under investigation in an ongoing phase 2 trial (NCT02002390).
Currently, for the treatment of peri-hemorrhagic edema, valid results from randomized controlled trials are missing and treatment approaches routinely used consist mostly of hyperosmolar strategies, yet formally evaluated these options to prevent peri-hemorrhagic edema should be considered experimental.
Intraventricular Hemorrhage
Intraventricular hemorrhage (IVH) is a frequent complication of ICH (~ 45%) and validated as independent predictor of poor outcome [6]. Especially, obstruction of the third and fourth ventricles leads to acute hydrocephalus representing a life-threatening situation with need for urgent treatment to prevent death from herniation. In this situation, placement of an EVD is required to allow for compensatory diversion of cerebrospinal fluid. Over the last years, several studies were conducted to assess efficacy and safety of intraventricular administration of fibrinolytic agents such as recombinant tissue-type plasminogen activator (rtPA). The aim of this strategy is to accelerate clot lysis especially of the third and fourth ventricles leading to re-communication between the inner and outer cerebral spinal fluid systems possibly minimizing hypoperfusion and inflammation. After promising data from the CLEAR-IVH trial [83], the recent phase 3 CLEAR III trial did not reach its primary endpoint [84]. Investigating 500 patients, randomly assigned to receive either up to 12 doses, 8 h apart, of 1 mg of alteplase or 0.9% saline via EVD showed no difference in the primary efficacy outcome defined as good functional outcome (mRS≤ 3 at 180 days: alteplase group 48% vs saline 45%; risk ratio [RR] 1.06, 95% CI [0.88–1.28]; p = 0.55) [84]. However, there was a 50% decrease in the odds of being dead for alteplase versus saline (adjusted OR 0.50 [95% CI 0.31–0.80], p = 0.004) [84]. A planned adjusted secondary analysis relating mRS score to the amount and timing of clot removal showed a significant relation between clot removal (per clot remaining [mL]) and both good outcome (adjusted OR 0.96, 95% CI [0.94–0.97], p < 0.01) and case fatality (adjusted HR of death per mL of time-weighted clot volume remaining 1.03 95% CI [1.02–1.04], p < 0.01) [84]. Overall, there were no safety concerns in respect to ventriculitis, symptomatic bleeding, or other serious adverse events [84].
Performing an overlapping lumbar drainage in patients with confirmed communication between the internal and external cerebral spinal fluid systems represents a valuable treatment strategy [6]. Due to normalization of physiological circulation and removal of inflammatory blood components, the rate of permanent shunt dependency may be reduced. Some smaller pilot and observational studies [85, 86] and more recently a small randomized trial including an individual patient data meta-analysis provided evidence that a combined approach of intraventricular fibrinolysis plus lumbar drain treatment is feasible and safe and significantly reduced rates of permanent shunt dependency as compared to treatment with intraventricular fibrinolysis alone (intervention group, 0% (0/14) vs control group, 43% (7/16), p < 0.01) [87•]. To avoid shunt dependency post IVH represents an important goal as this was shown to double the odds for disability (mRS 4–5) at 6 months (OR 2.14; 95% CI [1.13–4.08]) in the CLEAR III trial [88].
In summary, IVH associated with obstructive hydrocephalus should be treated with EVD placement to prevent herniation, control ICP, and possibly install lytic medications. Intraventricular fibrinolysis with an overlapping lumbar drainage may likely further reduce permanent shunt dependency with potential benefits on outcome.
Conclusions
Over recent years, several randomized and large-sized observational studies have considerably expanded the field of acute ICH care (see Table 2 for overview of data and recommendations). Yet, the one breakthrough intervention to improve functional outcome is still missing, though various treatment concepts and approaches possibly interacting with one another have been evaluated and such treatment bundle may improve patients’ outcome.
Abbreviations
- BP:
-
Blood pressure
- CI:
-
Confidence interval
- DNR:
-
Do not resuscitate
- EVD:
-
External ventricular drain
- FFP:
-
Fresh frozen plasma
- HE:
-
Hematoma enlargement
- ICH:
-
Intracerebral hemorrhage
- ICP:
-
Intracranial pressure
- INR:
-
International normalized ratio
- IQR:
-
Interquartile range
- IVH:
-
Intraventricular hemorrhage
- mRS:
-
Modified Rankin Scale
- NOAC:
-
Non-vitamin k antagonist oral anticoagulant
- OR:
-
Odds ratio
- PCC:
-
Prothrombin complex concentrate
- RR:
-
Risk ratio
- rtPA:
-
Recombinant tissue-type plasminogen activator
- TXA:
-
Tranexamic acid
- VKA:
-
Vitamin K antagonist
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373(9675):1632–44. https://doi.org/10.1016/s0140-6736(09)60371-8.
Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001;344(19):1450–60. https://doi.org/10.1056/nejm200105103441907.
Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016;15(9):913–24. https://doi.org/10.1016/S1474-4422(16)30073-4.
Sacco S, Marini C, Toni D, Olivieri L, Carolei A. Incidence and 10-year survival of intracerebral hemorrhage in a population-based registry. Stroke. 2009;40(2):394–9. https://doi.org/10.1161/STROKEAHA.108.523209.
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9(2):167–76. https://doi.org/10.1016/s1474-4422(09)70340-0.
Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(7):2032–60. https://doi.org/10.1161/str.0000000000000069.
• Sembill JA, Gerner ST, Volbers B, Bobinger T, Lucking H, Kloska SP, et al. Severity assessment in maximally treated ICH patients: the max-ICH score. Neurology. 2017;89(5):423–31. https://doi.org/10.1212/WNL.0000000000004174. Authors report that overly pessimisitc prognostication may deny a meanignfull recovery and provide a novel prognostic tool.
Zahuranec DB, Brown DL, Lisabeth LD, Gonzales NR, Longwell PJ, Smith MA, et al. Early care limitations independently predict mortality after intracerebral hemorrhage. Neurology. 2007;68(20):1651–7. https://doi.org/10.1212/01.wnl.0000261906.93238.72.
Morgenstern LB, Zahuranec DB, Sanchez BN, Becker KJ, Geraghty M, Hughes R, et al. Full medical support for intracerebral hemorrhage. Neurology. 2015;84(17):1739–44. https://doi.org/10.1212/WNL.0000000000001525.
Becker KJ, Baxter AB, Cohen WA, Bybee HM, Tirschwell DL, Newell DW, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56(6):766–72.
Yogendrakumar V, Smith EE, Demchuk AM, Aviv RI, Rodriguez-Luna D, Molina CA, et al. Lack of early improvement predicts poor outcome following acute intracerebral hemorrhage. Crit Care Med. 2018;46(4):e310–e7. https://doi.org/10.1097/CCM.0000000000002962.
Maas MB, Francis BA, Sangha RS, Lizza BD, Liotta EM, Naidech AM. Refining prognosis for intracerebral hemorrhage by early reassessment. Cerebrovasc Dis. 2017;43(3–4):110–6. https://doi.org/10.1159/000452679000452679.
Suo Y, Chen WQ, Pan YS, Peng YJ, Yan HY, Zhao XQ, Liu LP, Wang YL, Liu GF, Wang YJ The max-intracerebral hemorrhage score predicts long-term outcome of intracerebral hemorrhage. CNS Neurosci Ther. 2018. https://doi.org/10.1111/cns.12846.
Jacobs BS, Poggesi A, Terry JB. Max-ICH score: can it prevent self-fulfilling prophecy in ICH? Neurology. 2017;89(5):417–8. https://doi.org/10.1212/WNL.0000000000004195.
Langhorne P, Fearon P, Ronning OM, Kaste M, Palomaki H, Vemmos K, Kalra L, Indredavik B, Blomstrand C, Rodgers H, Dennis MS, Salman RAS, on behalf of the Stroke Unit Trialists’ Collaboration, The following collaborators provided new data, advice and comment, and assisted with the redrafting of the report:, Blomstrand C, Indredavik B, Kalra L, Kaste M, Palomaki H, Rodgers H, Ronning MO, Vemmos K, The Stroke Unit Trialists’ Collaboration supported and provided for the main stroke unit review:, Asplund K, Berman P, Blomstrand C, Britton M, Cabral NL, Cavallini A, Dey P, Hamrin E, Hankey G, Indredavik B, Kalra L, Kaste M, Laursen SO, Ma RH, Patel N, Rodgers H, Ronning MO, Sivenius J, Stevens R, Sulter G, Svensson A, Vemmos K, Wood-Dauphinee S, Yagura H Stroke unit care benefits patients with intracerebral hemorrhage: systematic review and meta-analysis. Stroke 2013;44(11):3044–3049. https://doi.org/10.1161/STROKEAHA.113.001564
Damian MS, Ben-Shlomo Y, Howard R, Bellotti T, Harrison D, Griggs K, et al. The effect of secular trends and specialist neurocritical care on mortality for patients with intracerebral haemorrhage, myasthenia gravis and Guillain-Barre syndrome admitted to critical care : an analysis of the Intensive Care National Audit & Research Centre (ICNARC) national United Kingdom database. Intensive Care Med. 2013;39(8):1405–12. https://doi.org/10.1007/s00134-013-2960-6.
Middleton S, McElduff P, Ward J, Grimshaw JM, Dale S, D’Este C, et al. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): a cluster randomised controlled trial. Lancet. 2011;378(9804):1699–706. https://doi.org/10.1016/S0140-6736(11)61485-2.
Sreekrishnan A, Leasure AC, Shi FD, Hwang DY, Schindler JL, Petersen NH, et al. Functional improvement among intracerebral hemorrhage (ICH) survivors up to 12 months post-injury. Neurocrit Care. 2017;27(3):326–33. https://doi.org/10.1007/s12028-017-0425-4.
Delcourt C, Huang Y, Arima H, Chalmers J, Davis SM, Heeley EL, et al. Hematoma growth and outcomes in intracerebral hemorrhage: the INTERACT1 study. Neurology. 2012;79(4):314–9. https://doi.org/10.1212/WNL.0b013e318260cbba.
•• Kuramatsu JB, Gerner ST, Schellinger PD, Glahn J, Endres M, Sobesky J, et al. Anticoagulant reversal, blood pressure levels, and anticoagulant resumption in patients with anticoagulation-related intracerebral hemorrhage. JAMA. 2015;313(8):824–36. https://doi.org/10.1001/jama.2015.0846. Large cohort study reporting on both acute and long-term management in anticoaugulation-associated ICH. For the first time provides INR targets to minimize hematoma expansion.
Demchuk AM, Dowlatshahi D, Rodriguez-Luna D, Molina CA, Blas YS, Dzialowski I, et al. Prediction of haematoma growth and outcome in patients with intracerebral haemorrhage using the CT-angiography spot sign (PREDICT): a prospective observational study. Lancet Neurol. 2012;11(4):307–14. https://doi.org/10.1016/S1474-4422(12)70038-8.
Morotti A, Boulouis G, Romero JM, Brouwers HB, Jessel MJ, Vashkevich A, et al. Blood pressure reduction and noncontrast CT markers of intracerebral hemorrhage expansion. Neurology. 2017;89(6):548–54. https://doi.org/10.1212/WNL.0000000000004210.
Morotti A, Dowlatshahi D, Boulouis G, Al-Ajlan F, Demchuk AM, Aviv RI, et al. Predicting intracerebral hemorrhage expansion with noncontrast computed tomography: the BAT score. Stroke. 2018;49(5):1163–9. https://doi.org/10.1161/STROKEAHA.117.020138.
Wang X, Arima H, Al-Shahi Salman R, Woodward M, Heeley E, Stapf C, et al. Clinical prediction algorithm (BRAIN) to determine risk of hematoma growth in acute intracerebral hemorrhage. Stroke. 2015;46(2):376–81. https://doi.org/10.1161/STROKEAHA.114.006910.
Flibotte JJ, Hagan N, O’Donnell J, Greenberg SM, Rosand J. Warfarin, hematoma expansion, and outcome of intracerebral hemorrhage. Neurology. 2004;63(6):1059–64.
Biffi A, Battey TW, Ayres AM, Cortellini L, Schwab K, Gilson AJ, et al. Warfarin-related intraventricular hemorrhage: imaging and outcome. Neurology. 2011;77(20):1840–6. https://doi.org/10.1212/WNL.0b013e3182377e12.
Kobayashi J, Koga M, Tanaka E, Okada Y, Kimura K, Yamagami H, et al. Continuous antihypertensive therapy throughout the initial 24 hours of intracerebral hemorrhage: the stroke acute management with urgent risk-factor assessment and improvement-intracerebral hemorrhage study. Stroke. 2014;45(3):868–70. https://doi.org/10.1161/STROKEAHA.113.004319.
Tsivgoulis G, Katsanos AH, Butcher KS, Boviatsis E, Triantafyllou N, Rizos I, et al. Intensive blood pressure reduction in acute intracerebral hemorrhage: a meta-analysis. Neurology. 2014;83(17):1523–9. https://doi.org/10.1212/WNL.0000000000000917.
Butcher KS, Jeerakathil T, Hill M, Demchuk AM, Dowlatshahi D, Coutts SB, et al. The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial. Stroke. 2013;44(3):620–6. https://doi.org/10.1161/strokeaha.111.000188.
Anderson CS, Huang Y, Wang JG, Arima H, Neal B, Peng B, et al. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomised pilot trial. Lancet Neurol. 2008;7(5):391–9. https://doi.org/10.1016/S1474-4422(08)70069-3.
Qureshi AI, Palesch YY, Martin R, Novitzke J, Cruz-Flores S, Ehtisham A, et al. Effect of systolic blood pressure reduction on hematoma expansion, perihematomal edema, and 3-month outcome among patients with intracerebral hemorrhage: results from the antihypertensive treatment of acute cerebral hemorrhage study. Arch Neurol. 2010;67(5):570–6. https://doi.org/10.1001/archneurol.2010.61.
Anderson CS, Huang Y, Arima H, Heeley E, Skulina C, Parsons MW, et al. Effects of early intensive blood pressure-lowering treatment on the growth of hematoma and perihematomal edema in acute intracerebral hemorrhage: the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial (INTERACT). Stroke. 2010;41(2):307–12. https://doi.org/10.1161/strokeaha.109.561795.
•• Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368(25):2355–65. https://doi.org/10.1056/NEJMoa1214609. Randomized controlled trial showing improved functional outcomes with intensive lowering of blood pressure among ordinal analysis of the modified Rankin scale.
•• Qureshi AI, Palesch YY, Barsan WG, Hanley DF, Hsu CY, Martin RL, et al. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. N Engl J Med. 2016;375(11):1033–43. https://doi.org/10.1056/NEJMoa1603460. Most recent randomized controlled trial documenting no significant benefit of intensive blood pressure lowering.
Burgess LG, Goyal N, Jones GM, Khorchid Y, Kerro A, Chapple K et al. Evaluation of acute kidney injury and mortality after intensive blood pressure control in patients with intracerebral hemorrhage. J Am Heart Assoc. 2018;7(8). https://doi.org/10.1161/JAHA.117.008439.
Morotti A, Brouwers HB, Romero JM, Jessel MJ, Vashkevich A, Schwab K, et al. Intensive blood pressure reduction and spot sign in intracerebral hemorrhage: a secondary analysis of a randomized clinical trial. JAMA Neurol. 2017;74(8):950–60. https://doi.org/10.1001/jamaneurol.2017.1014.
Shoamanesh A, Morotti A, Romero JM, Oliveira-Filho J, Schlunk F, Jessel MJ, et al. Cerebral microbleeds and the effect of intensive blood pressure reduction on hematoma expansion and functional outcomes: a secondary analysis of the ATACH-2 randomized clinical trial. JAMA Neurol. 2018;75:850–9. https://doi.org/10.1001/jamaneurol.2018.0454.
Qureshi AI, Palesch YY, Foster LD, Barsan WG, Goldstein JN, Hanley DF, et al. Blood pressure-attained analysis of ATACH 2 trial. Stroke. 2018;49(6):1412–8. https://doi.org/10.1161/STROKEAHA.117.019845.
•• Boulouis G, Morotti A, Goldstein JN, Charidimou A. Intensive blood pressure lowering in patients with acute intracerebral haemorrhage: clinical outcomes and haemorrhage expansion. Systematic review and meta-analysis of randomised trials. J Neurol Neurosurg Psychiatry. 2017;88(4):339–45. https://doi.org/10.1136/jnnp-2016-315346. Meta-analysis of randomized data ( n = 4360) investigating the effect of intensive blood pressure reductions on outcomes.
• Morotti A, Charidimou A, Phuah CL, Jessel MJ, Schwab K, Ayres AM, et al. Association between serum calcium level and extent of bleeding in patients with intracerebral hemorrhage. JAMA Neurol. 2016;73(11):1285–90. https://doi.org/10.1001/jamaneurol.2016.22522546924. Authors report on a novel parameter associated with ICH volumes.
Liotta EM, Prabhakaran S, Sangha RS, Bush RA, Long AE, Trevick SA, et al. Magnesium, hemostasis, and outcomes in patients with intracerebral hemorrhage. Neurology. 2017;89(8):813–9. https://doi.org/10.1212/WNL.0000000000004249.
Goyal N, Tsivgoulis G, Malhotra K, Houck AL, Khorchid YM, Pandhi A et al. Serum magnesium levels and outcomes in patients with acute spontaneous intracerebral hemorrhage. J Am Heart Assoc. 2018;7(8). https://doi.org/10.1161/JAHA.118.008698
Hoffman M, Monroe DM 3rd, Roberts HR. Activated factor VII activates factors IX and X on the surface of activated platelets: thoughts on the mechanism of action of high-dose activated factor VII. Blood Coagul Fibrinolysis. 1998;9(Suppl 1):S61–5.
Mayer SA, Brun NC, Begtrup K, Broderick J, Davis S, Diringer MN, et al. Recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2005;352(8):777–85. https://doi.org/10.1056/NEJMoa042991.
Mayer SA, Brun NC, Begtrup K, Broderick J, Davis S, Diringer MN, et al. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008;358(20):2127–37. https://doi.org/10.1056/NEJMoa0707534.
Roberts I, Shakur H, Coats T, Hunt B, Balogun E, Barnetson L, et al. The CRASH-2 trial: a randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol Assess. 2013;17(10):1–79. https://doi.org/10.3310/hta17100.
•• Sprigg N, Flaherty K, Appleton JP, Salman RA, Bereczki D, Beridze M, et al. Tranexamic acid for hyperacute primary IntraCerebral Haemorrhage (TICH-2): an international randomised, placebo-controlled, phase 3 superiority trial. Lancet. 2018;391:2107–15. https://doi.org/10.1016/S0140-6736(18)31033-X. Randomized controlled trial on effects of tranexamic acid in ICH patients showing a decreased early (7 days) mortality, reduced hematoma enlargement, and a favorable safety profile for tranexamic acid. Sub-group analyses favored treatment in patients with systolic blood pressures below 170 mmHg, lobar ICH location, and ICH volumes between 30 and 60 mL.
Meretoja A, Churilov L, Campbell BC, Aviv RI, Yassi N, Barras C, et al. The spot sign and tranexamic acid on preventing ICH growth--AUStralasia Trial (STOP-AUST): protocol of a phase II randomized, placebo-controlled, double-blind, multicenter trial. Int J Stroke. 2014;9(4):519–24. https://doi.org/10.1111/ijs.12132.
Liu L, Wang Y, Meng X, Li N, Tan Y, Nie X, et al. Tranexamic acid for acute intracerebral hemorrhage growth predicted by spot sign trial: rationale and design. Int J Stroke. 2017;12(3):326–31. https://doi.org/10.1177/1747493017694394.
Brouwers HB, Chang Y, Falcone GJ, Cai X, Ayres AM, Battey TW, et al. Predicting hematoma expansion after primary intracerebral hemorrhage. JAMA Neurol. 2014;71(2):158–64. https://doi.org/10.1001/jamaneurol.2013.5433.
• Steiner T, Poli S, Griebe M, Husing J, Hajda J, Freiberger A, et al. Fresh frozen plasma versus prothrombin complex concentrate in patients with intracranial haemorrhage related to vitamin K antagonists (INCH): a randomised trial. Lancet Neurol. 2016;15(6):566–73. https://doi.org/10.1016/S1474-4422(16)00110-1. Randomized controlled trial comparing PCC versus FFP in VKA ICH patients providing evidence in favor of PCC for reversal of anticoagulation.
Kuramatsu JB, Sembill JA, Gerner ST, Sprugel MI, Hagen M, Roeder SS, et al. Management of therapeutic anticoagulation in patients with intracerebral haemorrhage and mechanical heart valves. Eur Heart J. 2018;39:1709–23. https://doi.org/10.1093/eurheartj/ehy056.
• Gerner ST, Kuramatsu JB, Sembill JA, Sprugel MI, Endres M, Haeusler KG, et al. Association of prothrombin complex concentrate administration and hematoma enlargement in non-vitamin K antagonist oral anticoagulant-related intracerebral hemorrhage. Ann Neurol. 2018;83(1):186–96. https://doi.org/10.1002/ana.25134. Large cohort study reporting on reversal strategies in non-vitamin K anticoaugulation-associated ICH.
Purrucker JC, Haas K, Rizos T, Khan S, Wolf M, Hennerici MG, et al. Early clinical and radiological course, management, and outcome of intracerebral hemorrhage related to new oral anticoagulants. JAMA Neurol. 2016;73(2):169–77. https://doi.org/10.1001/jamaneurol.2015.3682.
Boulouis G, Morotti A, Pasi M, Goldstein JN, Gurol ME, Charidimou A. Outcome of intracerebral haemorrhage related to non-vitamin K antagonists oral anticoagulants versus vitamin K antagonists: a comprehensive systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2018;89(3):263–70. https://doi.org/10.1136/jnnp-2017-316631.
Wilson D, Seiffge DJ, Traenka C, Basir G, Purrucker JC, Rizos T, et al. Outcome of intracerebral hemorrhage associated with different oral anticoagulants. Neurology. 2017;88(18):1693–700. https://doi.org/10.1212/WNL.0000000000003886.
Kurogi R, Nishimura K, Nakai M, Kada A, Kamitani S, Nakagawara J, et al. Comparing intracerebral hemorrhages associated with direct oral anticoagulants or warfarin. Neurology. 2018;90(13):e1143–e9. https://doi.org/10.1212/WNL.0000000000005207.
Tsivgoulis G, Lioutas VA, Varelas P, Katsanos AH, Goyal N, Mikulik R, et al. Direct oral anticoagulant- vs vitamin K antagonist-related nontraumatic intracerebral hemorrhage. Neurology. 2017;89(11):1142–51. https://doi.org/10.1212/WNL.0000000000004362.
Inohara T, Xian Y, Liang L, Matsouaka RA, Saver JL, Smith EE, et al. Association of intracerebral hemorrhage among patients taking non-vitamin K antagonist vs vitamin K antagonist oral anticoagulants with in-hospital mortality. JAMA. 2018;319(5):463–73. https://doi.org/10.1001/jama.2017.21917.
Ebner M, Birschmann I, Peter A, Spencer C, Hartig F, Kuhn J, et al. Point-of-care testing for emergency assessment of coagulation in patients treated with direct oral anticoagulants. Crit Care. 2017;21(1):32. https://doi.org/10.1186/s13054-017-1619-z.
•• Pollack CV Jr, Reilly PA, van Ryn J, Eikelboom JW, Glund S, Bernstein RA, et al. Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 2017;377(5):431–41. https://doi.org/10.1056/NEJMoa1707278. Full cohort analysis of idarucizumab for dabigatran reversal.
Connolly SJ, Milling TJ Jr, Eikelboom JW, Gibson CM, Curnutte JT, Gold A, et al. Andexanet alfa for acute major bleeding associated with factor Xa inhibitors. N Engl J Med. 2016;375:1131–41. https://doi.org/10.1056/NEJMoa1607887.
Siegal DM, Curnutte JT, Connolly SJ, Lu G, Conley PB, Wiens BL, et al. Andexanet alfa for the reversal of factor Xa inhibitor activity. N Engl J Med. 2015;373(25):2413–24. https://doi.org/10.1056/NEJMoa1510991.
• Baharoglu MI, Cordonnier C, Salman RA, de Gans K, Koopman MM, Brand A, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016;387(10038):2605–13. https://doi.org/10.1016/S0140-6736(16)30392-0. Randomized controlled trial investigating platelet transfusions in ICH patients using platelet inhibitors, showing evidence in disfavor of platelet transfusions.
Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet. 2005;365(9457):387–97. https://doi.org/10.1016/s0140-6736(05)17826-x.
Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013;382(9890):397–408. https://doi.org/10.1016/s0140-6736(13)60986-1.
•• Hanley DF, Thompson RE, Muschelli J, Rosenblum M, McBee N, Lane K, et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol. 2016;15(12):1228–37. https://doi.org/10.1016/s1474-4422(16)30234-4. Randomized controlled trial investigating intraventricular thrombolysis, showing a reduced mortality at 180 days, a safe profile, and faster clot removal which was associated with favorable functional outcome.
van Loon J, Van Calenbergh F, Goffin J, Plets C. Controversies in the management of spontaneous cerebellar haemorrhage. A consecutive series of 49 cases and review of the literature. Acta Neurochir. 1993;122(3–4):187–93.
Firsching R, Huber M, Frowein RA. Cerebellar haemorrhage: management and prognosis. Neurosurg Rev. 1991;14(3):191–4.
Tamaki T, Kitamura T, Node Y, Teramoto A. Paramedian suboccipital mini-craniectomy for evacuation of spontaneous cerebellar hemorrhage. Neurol Med Chir (Tokyo). 2004;44(11):578–82. discussion 83
Hackenberg KA, Unterberg AW, Jung CS, Bosel J, Schonenberger S, Zweckberger K. Does suboccipital decompression and evacuation of intraparenchymal hematoma improve neurological outcome in patients with spontaneous cerebellar hemorrhage? Clin Neurol Neurosurg. 2017;155:22–9. https://doi.org/10.1016/j.clineuro.2017.01.019.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–e110. https://doi.org/10.1161/STR.0000000000000158.
Volbers B, Giede-Jeppe A, Gerner ST, Sembill JA, Kuramatsu JB, Lang S, et al. Peak perihemorrhagic edema correlates with functional outcome in intracerebral hemorrhage. Neurology. 2018;90(12):e1005–e12. https://doi.org/10.1212/WNL.0000000000005167.
Xi G, Keep RF, Hoff JT. Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol. 2006;5(1):53–63. https://doi.org/10.1016/s1474-4422(05)70283-0.
Wang X, Arima H, Yang J, Zhang S, Wu G, Woodward M, et al. Mannitol and outcome in intracerebral hemorrhage: propensity score and multivariable intensive blood pressure reduction in acute cerebral hemorrhage trial 2 results. Stroke. 2015;46(10):2762–7. https://doi.org/10.1161/STROKEAHA.115.009357.
Shah M, Birnbaum L, Rasmussen J, Sekar P, Moomaw CJ, Osborne J, et al. Effect of hyperosmolar therapy on outcome following spontaneous intracerebral hemorrhage: Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study. J Stroke Cerebrovasc Dis. 2018;27(4):1061–7. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.11.013.
Volbers B, Herrmann S, Willfarth W, Lucking H, Kloska SP, Doerfler A, et al. Impact of hypothermia initiation and duration on perihemorrhagic edema evolution after intracerebral hemorrhage. Stroke. 2016;47(9):2249–55. https://doi.org/10.1161/STROKEAHA.116.013486.
Staykov D, Wagner I, Volbers B, Doerfler A, Schwab S, Kollmar R. Mild prolonged hypothermia for large intracerebral hemorrhage. Neurocrit Care. 2013;18(2):178–83. https://doi.org/10.1007/s12028-012-9762-5.
Rincon F, Friedman DP, Bell R, Mayer SA, Bray PF. Targeted temperature management after intracerebral hemorrhage (TTM-ICH): methodology of a prospective randomized clinical trial. Int J Stroke. 2014;9(5):646–51. https://doi.org/10.1111/ijs.12220.
Fischer M, Schiefecker A, Lackner P, Frank F, Helbok R, Beer R, et al. Targeted temperature management in spontaneous intracerebral hemorrhage: a systematic review. Curr Drug Targets. 2017;18(12):1430–40. https://doi.org/10.2174/1389450117666160703161511.
Zeng L, Tan L, Li H, Zhang Q, Li Y, Guo J. Deferoxamine therapy for intracerebral hemorrhage: a systematic review. PLoS One. 2018;13(3):e0193615. https://doi.org/10.1371/journal.pone.0193615.
Fu Y, Hao J, Zhang N, Ren L, Sun N, Li YJ, et al. Fingolimod for the treatment of intracerebral hemorrhage: a 2-arm proof-of-concept study. JAMA Neurol. 2014;71(9):1092–101. https://doi.org/10.1001/jamaneurol.2014.1065.
Morgan T, Awad I, Keyl P, Lane K, Hanley D. Preliminary report of the clot lysis evaluating accelerated resolution of intraventricular hemorrhage (CLEAR-IVH) clinical trial. Acta Neurochir Suppl. 2008;105:217–20.
Hanley DF, Lane K, McBee N, Ziai W, Tuhrim S, Lees KR, et al. Thrombolytic removal of intraventricular haemorrhage in treatment of severe stroke: results of the randomised, multicentre, multiregion, placebo-controlled CLEAR III trial. Lancet. 2017;389(10069):603–11. https://doi.org/10.1016/S0140-6736(16)32410-2.
Staykov D, Huttner HB, Struffert T, Ganslandt O, Doerfler A, Schwab S, et al. Intraventricular fibrinolysis and lumbar drainage for ventricular hemorrhage. Stroke. 2009;40(10):3275–80. https://doi.org/10.1161/strokeaha.109.551945.
Huttner HB, Nagel S, Tognoni E, Kohrmann M, Juttler E, Orakcioglu B, et al. Intracerebral hemorrhage with severe ventricular involvement: lumbar drainage for communicating hydrocephalus. Stroke. 2007;38(1):183–7. https://doi.org/10.1161/01.str.0000251795.02560.62.
• Staykov D, Kuramatsu JB, Bardutzky J, Volbers B, Gerner ST, Kloska SP, et al. Efficacy and safety of combined intraventricular fibrinolysis with lumbar drainage for prevention of permanent shunt dependency after intracerebral hemorrhage with severe ventricular involvement: a randomized trial and individual patient data meta-analysis. Ann Neurol. 2017;81(1):93–103. https://doi.org/10.1002/ana.24834. Small randomized controlled trial and meta-analyses investigating the influence of lumbar drains on permanent shunt dependency.
Murthy SB, Awad I, Harnof S, Aldrich F, Harrigan M, Jallo J, et al. Permanent CSF shunting after intraventricular hemorrhage in the CLEAR III trial. Neurology. 2017;89(4):355–62. https://doi.org/10.1212/WNL.0000000000004155.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jochen A. Sembill, Hagen B. Huttner, and Joji B. Kuramatsu declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Stroke
Rights and permissions
About this article
Cite this article
Sembill, J.A., Huttner, H.B. & Kuramatsu, J.B. Impact of Recent Studies for the Treatment of Intracerebral Hemorrhage. Curr Neurol Neurosci Rep 18, 71 (2018). https://doi.org/10.1007/s11910-018-0872-0
Published:
DOI: https://doi.org/10.1007/s11910-018-0872-0