Abstract
Purpose of Review
This review highlights some of the important changes in the immune system that occur in the process of normal aging. Immunosenescence as a concept is directly relevant to the world of neuro-inflammation, as it may be a contributing factor to the risks associated with some of the current immunosuppressive and immunomodulatory therapies used in treating multiple sclerosis (MS) and other inflammatory disorders.
Recent Findings
Profound qualitative and quantitative changes occur in the adaptive and innate immunity compartments during aging. These changes may explain why patients of older age are at an increased risk of infections and infection-associated mortality.
Summary
Immunosenescence-associated changes may be additive or synergistic with the effects produced by immunomodulatory and immunosuppressive medications. Clinicians should exercise a high level of vigilance in monitoring the risk of infections in older patients on these treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
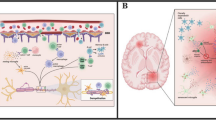
Immunosenescence is a concept that describes the quantitative and functional changes that occur in the innate and adaptive compartments of the immune system during the course of normal human aging. A functional decline and remodeling in cellular subsets have significant impacts on the course of neuro-inflammatory conditions, risk of infections, tumor surveillance, and response to vaccines [1••]. These changes may be particularly relevant in patients whose immune systems are iatrogenically altered by immunosuppressive and immunomodulatory medications used to treat inflammatory conditions, such as MS, neuromyelitis optica (NMO), connective tissue disorders, or sarcoidosis. Over the past decade, the emergence of several novel immunotherapeutic agents and their association with infections highlighted the relevance of immunosenescence to the risk of infection in older patients.
This review will focus on the changes that occur in the CD4, CD8 T lymphocytes, B lymphocytes, and the innate compartment of the immune system during aging, in an attempt to explain how these alterations can be additive to or synergistic with the changes induced by the disease-modifying therapies in regard to the risk of infections.
Immunosenescence: a Risk Factor for Opportunistic Infections Associated with Disease-Modifying Therapies
Several MS therapies (natalizumab, fingolimod, and dimethyl fumarate) have been increasingly associated with a risk of infections, including progressive multifocal leukoencephalopathy (PML). Some epidemiologic trends suggest that older age may be an important risk factor in PML development and outcomes.
In one study of natalizumab-associated PML, the infection occurred significantly earlier (before 24 infusions) in patients who were older at the time of natalizumab’s initiation as compared to those who were diagnosed at a later time during therapy (43.5 ± 9.7 vs. 36.9 ± 8.3 years, p = 0.03) [2]. In addition, older age is considered to be a predictive factor of poorer outcome in PML: a concept that is ubiquitously true in the context of age and infection-associated mortality. The age of the U.S. PML patients was found to be mean 47 years (median 47 years) in survivors and 52 (median 55) in those who did not survive [3]. However, one must note that the average age of patients with PML with natalizumab was 45 (22–73), not significantly different from the average age of the patients on natalizumab without PML [4]. A development of PML case in a 70-year-old patient treated with natalizumab for MS whose JCV antibody seroconverted to positive only 2 weeks prior to the onset of the disease [5] suggests the possibility that age-associated changes in humoral immunity reduce the ability to mount an effective antibody response, thus, possibly diminishing the reliability of the interval-based JCV antibody surveillance in that age group. Likewise, in the rare instance in which PML occurs in the absence of an identifiable predisposing cause, the immunological changes associated with aging may be a substantial contributing factor. In the literature, PML cases in apparently non-immunocompromised non-MS patients occurred in patients of more advanced age than the average population (mean age 59.4, median 62) [6,7,8,9,10,11,12].
Fingolimod, another disease-modifying drug, recently associated with PML cases, appears to demonstrate a similar age-dependent trend for both PML and cryptococcal meningitis. For fingolimod-associated PML, the mean age was 54 and median 58 (range 34–63) [13]. For cryptococcal meningitis cases, average age reported in the literature cases was 56 [14]. These patients are substantially older than the average age of the patients with relapsing remitting MS. In one large cohort of MS patients, the median age of onset was 28.7 years with an average duration before the onset of secondary progressive MS of 8.7 years ± 8.6 years [15]. In patients on long-term fingolimod, absolute counts of peripheral circulating CD4 and CD8 T cells were remarkably low as expected, but there was also a striking CD4:CD8 ratio reversal of 1:2 [16], mimicking the immunosenescent changes observed in cohorts of octa- and nonagenarians with increased risk of mortality [17]. In addition, a slightly higher rate of Varicella zoster virus (VZV) reactivation in patients on fingolimod was observed in the clinical trials and in the post-marketing surveillance. One study showed that the frequency of VZV-specific and EBV-specific IFN-γ producing T lymphocytes was reduced in patients on fingolimod. In this cohort, 20% developed a subclinical VZV or EBV reactivation. In addition, upon stimulation with VZV, the absolute number of cells proliferating in response to the virus was reduced [18]. This effect may be particularly important, as VZV predominantly reactivates in those of older age [19, 20, and 21]. In the USA, annual incidence of VZV reactivation nearly doubles from 5 to 6.5 per 1000 in those of 60 years of age to about 8–11 patients per 1000 in those 70 years of age or older [22].
Dimethyl fumarate (DMF)-associated PML cases occurred in patients who were 54, 59, 61, 64, and 66 years of age (mean 60.8/median 61) [23]. The risk of PML with dimethyl fumarate in most (though not all) cases has been associated with absolute lymphocyte counts of <500 cells/cu mm and, similarly, PML with the use of monomethyl fumarate in the treatment of psoriasis has also been linked to lower lymphocyte counts. Older age may increase susceptibility to lymphopenia in patients on fumarates. A recent retrospective study of patients on DMF showed that among patients who were 60 years old or older, 24 (71%) developed lymphopenia, while only 62 (36%) of the 172 younger than 60 years of age developed lymphopenia (P = .0005). The study concluded that patient age of 60 or older and baseline absolute lymphocyte counts <2.0 were an independent risk factor for developing lymphopenia [24]. Another retrospective study of 221 patients on DMF showed that people of older age (>55) had an increased risk of developing moderate to severe lymphopenia [25]. Foley et al. compared absolute lymphocyte counts (ALC) in 30 multiple sclerosis patients younger than 30 and 30 patients older than 65 and showed that the mean baseline ALC was 2543 in the younger patient versus 2189 in the older; after DMF exposure, the ALC declined to 1844 (27% decrease) in the younger cohort and to 1279 (41% decrease) in the older cohort. Moreover, 67% of patients in the lowest quartile for lymphocyte count at baseline were those older than 65 [26]. CD8 T cells, critically important for viral control and clearance, are preferentially lowered by DMF [27]. CD4/CD8 ratio alterations, such as those occurring with DMF [28], long-term fingolimod [16], and in the CSF of natalizumab patients in the first 6 months [29], may impair the immune surveillance to various degrees and increase the risk of infections, such as PML. These alterations may be additive to the many changes in the CD4 and CD8 compartments in those of older age.
In non-MS non-transplant patients treated with rituximab, a similar trend for advanced age and PML was noted [30]. These immune-modulating therapies affect various subsets of the immune system in many complex ways beyond their basic mechanism of action, thus adding to or potentiating the subtle deleterious effects of immunosenescence.
West Nile virus (WNV) epidemiology offers another unique example of the relationship between age and infection. WNV meningoencephalitis is more common among people over the age of 50 and, in fact, is 40 to 50 times more common in people over 70 as compared to those younger than 40 [31].
Those of older age have a higher magnitude and frequency of cytomegalovirus (CMV) and Epstein-Barr virus (EBV) reactivation [32].
This review will highlight age-related changes in the immune system that may be both additive and synergistic in the context of disease-modifying therapies’ quantitative and qualitative effects on the immune system.
Thymus and Aging
The thymus is a primary lymphoid organ that provides an environment for T cell differentiation, maturation, and education, resulting in a positive (functional) and negative (deletion of autoreactive T cells) selection of naive T cells and their output into the circulation. Studies suggest that beginning in the 1st year of life, the thymus begins to involute at a rate of approximately 3% per year [33]. As the thymus atrophies, thymic output of naïve T cells falls [34, 35]. This age-related difference in thymic output is best highlighted by the studies of immune reconstitution in HIV-infected adolescents versus older adults, showing a significantly more robust naïve T cell reconstitution in adolescents, when treated with HAART [36]. Murray et al. found that at the age of 25, 20% of naïve T cells emerge directly from the thymus, whereas by the age of 55, only 5% of naïve T cells arise from thymic output [34]. Other studies also confirmed that some level of thymopoiesis continues well into the 5th decade [37].
As thymic output of naïve T cells falls, homeostatic peripheral T cell proliferation acts as a compensatory mechanism to maintain normal peripheral T cell counts [38, 39]. This peripheral naïve T cell pool is aged and may have accumulated senescence-associated defects, passing it onto the newly derived naïve T cells. In addition, this peripheral T cell pool is limited in its diversity, which leads to a more restricted T cell receptor repertoire, eventually undermining immune systems’ ability to respond to novel antigens. Initially peripheral proliferative responses may be sufficient to maintain a diverse naïve T cell repertoire well into the 50s; however, after the age 65, the diversity of the T cell repertoire drops precipitously [40].
Reduced thymic output is of particular interest in patients with MS, with some studies showing that in patients with MS, thymic involution occurs earlier. Duszczyszyn et al. showed that recent thymic emigrants (RTE) were reduced in patients with RRMS and PPMS as compared to the age-matched healthy controls. When compared to healthy controls, patients with RRMS showed an age-associated thymic output of progressively immature CD4 RTEs. Further analysis of Ki-67 (cell proliferation marker) showed important changes in the T cell proliferative responses, leading to failure to maintain naïve CD4 T cell numbers [41].
Effects on T Cell-Mediated Immunity
Both CD4 and CD8 T lymphocyte subsets are affected by aging, with the changes being most profound in the CD8+ compartment [42••]. In the elderly, there is a decrease in the naive CD8+ T cells, with a predominance of terminally differentiated late effector memory CD8+ T cells. These cells exhibit features of replicative immunosenescence such as reduced ability to proliferate, shortened telomeres, and reduced telomerase activity. Some studies report that an increase in cell negative regulatory cell receptors such as PD1 (programmed death 1), TIM-3 (T cell immunoglobulin and mucin-domain containing-3), and KIRs (killer inhibitory receptors) is responsible for the reduced activation and proliferation that occur with age [43, 44]. However, whether these receptors represent markers of immunosenescence or simply terminal differentiation remains a matter of debate [45]. Aged CD8 T cells have a decrease in their primary response to infections and vaccinations [46, 47] as well as reduced quality of target cell lysis [48, 49]. Thus, in the course of aging, T cell repertoire is profoundly affected by the shifts in the ratios of naïve T cells to memory T cells [50] with some suggesting a two- to fivefold decrease in the size of the naïve T cell subset [51]. Van Epps et al. showed that people of older age (median age 80) had markedly lower frequencies of CD8+ naïve T cells (11 vs 47%) as compared to those of younger age (median age 27). The same age-related trend was observed for CD4+ naïve T cells (33 vs 45%) [52] (Table 1). In addition, virus-specific CD8+ T lymphocytes from the aged individuals produce less antigen-specific IFN-γ [53].
While naive CD8+ T cells decrease in numbers and accumulate age-associated defects in their ability to proliferate in response to antigen stimulation [54•], some argue that naïve CD4+ T lymphocytes may be affected to a lesser extent [55••]. Shulz et al. showed that after a vaccination with a yellow fever virus, those of older age had a decrease in peak frequencies of CD8+ T lymphocytes, while CD4 peak response frequency was not affected [56].
However, other studies suggest that the CD4 compartment likewise undergoes many important changes (Table 1). CD4 cells have critical helper functions in activating B cells, promoting germinal center formation and high affinity antibody production [57]. An adoptive transfer model comparing antigen-specific antibody responses between CD4 deficient mice who were inoculated with naïve TCR transgenic CD4 from aged mice donors versus young donors showed a 3 log decrease in the antigen-specific antibody response and a reduced germinal center expansion in the setting of CD4 cells from aged mice [58]. In addition, CD4 T cells from aged individuals (both human and mice) have a lower proliferative capacity and IL-2 production [59], essential for T cell differentiation into effector and memory subsets after antigen stimulation. Some studies report an increase in CD4 FOXp3 regulatory subset that can make the immune response to pathogens less robust [60, 61]. With age, CD4+ T cells are more susceptible to apoptosis and have a weakened T cell receptor response [62].
Another important change that occurs in the T cell compartment is a loss of CD28, an important co-stimulatory molecule necessary for the effector functions of CD4 and CD8 T cells. Loss of CD28 and expansion of CD28 negative cell subset is associated with a decrease in antigen receptor diversity, reduced antigen-induced proliferation, and shorter life span [63, 64]. Expansion of CD28 T cell subset appears to be proportional to aging and is seen widely in polyclonal expansion associated with CMV infection. At birth, almost all CD8+ T cells contain CD28; by the age of 20–30, CD28 expression is reduced by about 20% and in people over 80, the expression is reduced by 50–60% [65]. This reduction is thought to occur due to prior burden of repetitive antigen exposure and is associated with chronic infections, such as CMV and EBV. Life-long repeated bouts of CMV reactivation within the host result in a repeated CMV antigen presentation and memory cell boosting, leading to a clonal expansion of CMV-specific CD8 T memory T cells, now comprising a larger part of the T cell compartment at the expense of the smaller numbers of naïve T cells. These CMV-specific T memory cells have phenotypic and replicative features characteristic of the immunosenescent cells [66]. Some studies report that with age, naïve T cells are less likely to become effector cells and when they do, the response is preferentially Th2 and not Th1 (due to a shift towards type II cytokine responses) [67]. Th1 is necessary for cellular immunity response to pathogens such as viruses and fungi. As T cell compartment becomes increasingly clonal, some studies suggest a propensity for auto-reactivity [68].
A recent study showed a defect in the interferon type I signaling pathway in T cells in the aged individuals [69]. Type I interferons (IFN-I) (interferon-α and interferon-β) are critical in T cell responses to bacterial and viral infections, allowing for T cell survival and differentiation. In activated T cells, interferon-α upregulates expression of IL-2Rα, c-myc, and pim-1, a set of genes responsible for cellular proliferation [70]. Using gene expression arrays, older individuals were shown to have a decreased IFN-I-induced gene expression in naïve CD4 cells. This reduced responsiveness to IFN-I may represent yet another mechanism of immune impairment in those of older age [69].
Longitudinal studies of healthy octagenarians and nonagenarians reported specific immunologic changes associated with increased morbidity and mortality, constituting an immune risk phenotype, characterized by CD4:CD8 ratio reversal (less than 1), increased terminally differentiated CD28- CD8 T cells, CMV seropositivity, decreased proliferation of T cells to mitogens, clonal expansion of CMV and EBV CD8 T cells, and increased frequency of CD28-KLRG-1+ dysfunctional cells among CMV-specific CD8 T cells that have low ability to proliferate and produce IFN [17, 100].
Most studies of immunosenescence have focused on the mechanisms of T cells in circulation, which represent only 2% of the total lymphocytes. Several recent studies illustrated that a large number of T cells consist of T resident memory cells that reside in the epithelial barriers and do not recirculate [71, 72]. These cells travel through the extracellular matrix (ECM) of the non-lymphoid organs. The T cell’s ability to mobilize and navigate in these tissues is critical for the successful immune surveillance and response in tissues and organs [73]. Changes that occur in the ECM in the process of aging may be important, as ECM proteins and proteoglycans contribute to the cell behavior via interacting with secreted ligands and, importantly, transmembrane receptors, such as integrins. This study led to a novel hypothesis that with age, increased stiffness and cross-linking of ECM leads to a decreased mobility of T resident memory cells and thus may be in part responsible for the reduced immune competency we observe in aged individuals [74]. T cell passage through a stiff matrix may damage its membrane and/or nucleus, potentially resulting in cellular death [75, 76] or sending danger signals that trigger the inflammasome. This leads to increased levels of pro-inflammatory cytokines such as IL 1, IL 18, and upregulation of NF kB (nuclear factor kappa-light-chain-enhancer of activated B cells) [77••], a transcription factor that regulates genes associated with chronic inflammation and leads to cellular phenotypes associated with aging in the brain, skin, and spine [78, 79] termed senescence-associated secretory phenotype (SASP) [80].
Effects on B Cell-Mediated Immunity
The humoral compartment of the immune system also undergoes important changes in the process of aging (Table 2). This is best illustrated by the reduced ability of the elderly to mount an adequate antibody response to novel antigens and vaccines [81]. A decreased ability to mount a specific antibody response to various vaccines (influenza, tetanus, Salmonella, S. pneumoniae) has been demonstrated in multiple studies [82, 83]. Several studies report that the total numbers of peripheral B cells are reduced in the course of aging [83, 84•]. B cell subsets also undergo many important changes such as a loss of naïve follicular B cells, increasing number of antigen-experienced B cells and changes in the antibody production, both functionally and qualitatively [85].
In adults, B cells are continuously repopulated from the pool of the hematopoietic stem cells (HSC) that reside in the bone marrow. With age, the frequencies of B cell progenitors decrease [86], likely reflecting HSC’s decreased propensity for lymphoid differentiation secondary to downregulation of the genes responsible for lymphoid specification [87]. Younger adults have a higher proportion of HSC committed to lymphoid lineage, whereas the elderly have a balance shift towards myeloid lineage [87]. McKenna et al. evaluated bone marrow B cell precursors in several hundred patients and showed a decrease associated with age [88]. With aging, B cells accumulate defects that result in the reduced efficiency of somatic hypermutation (SHM) (responsible for generating high avidity antibodies) and class switch recombination (CSR) (changing effector functions of the specific antibody) as well as AID (activation-induced cytidine deaminase), critical for CSR and SHM [83, 89]. Decrease in somatic hypermutation of IgG genes reduces the specific affinity of the antibody to the antigen [90]. In addition, Gibson et al. studied peripheral blood B cells from adults between the age of 19 and 85 and showed that in some elderly adults, there was a significant reduction in the antibody repertoire, a finding that was associated with frailty [89]. There is a decrease in B cell responses to novel antigenic stimulation, which in part may be due to the changes in CD4 helper T cells [58].
Effects on the Innate Immunity
Aging also leads to variable changes to the NK cell [91], monocyte, and neutrophil compartments, resulting in the impairment of their phagocytic and chemotactic functions [92, 93]. NK cells are critical as a first-line defense against intracellular pathogens as well as tumor surveillance and control. Low function of NK cells in elderly people was found to be associated with an increased risk of infection [94], while those 85 and older with decreased numbers of NK cells were found to have an increased rate of mortality at 2-year follow-up [95]. NK cell compartment undergoes changes quantitatively, phenotypically, and functionally [96]. Immature NK bright cells decrease in numbers, while NK dim cells prevail, with a predominance of CD57+ phenotype, a marker of terminal differentiation, that are highly cytotoxic but have a decreased ability to respond to cytokines and proliferate [97]. NK cells from healthy elderly people have lower rates of proliferation and production (by 50%) [98] compared to healthy young people, yet the overall numbers are similar, likely reflecting a proportionally expanded NK dim subset [99]. Cytotoxicity may be reduced at the cellular level, but due to the expansion of the NK dim subset, overall cytotoxicity is preserved [100]. NKp30 activating receptor expression decreases with age [101]. This receptor is critical in the cross talk between NK and dendritic cells presenting a foreign ligand. Engagement of this receptor leads to production of TNFα, IFN-γ, and dendritic cell activation or to direct killing of the dendritic cell by the NK cell [96]. When activated, dendritic cells produce Th1 cytokines further activating NK cells and recruiting cytotoxic arm of the adaptive immunity [102]. Other activating receptors such as NKp46 and DNAM-1 are also reduced in the elderly donors [96].
To summarize, aging is associated with an overall increase in NK cells, perhaps as a compensatory mechanism for their reduced function (reduced cytotoxicity at a single cell level, decreased cytokine production, and decreased ability to respond to cytokines) and subset redistribution (decreased NK brights) and phenotype changes (decreased activating receptors) [1•]. Blood sample analysis from middle-aged and elderly groups showed an increase in neutrophil counts and C-reactive protein (CRP) in the elderly. Some studies suggest that the former reflect low-grade inflammation and are associated with frailty [103].
Inflammaging
In addition to the many changes that occur in the immune system cellular compartments and function, aging is associated with a low-grade pro-inflammatory state, termed inflammaging [104]. This important theory of aging first began with an observation that peripheral mononuclear cells from the elderly patients expressed higher levels of pro-inflammatory cytokines (IL-6, TNFα, and IL-1β) than the cells from their younger counterparts [105]. A series of further experiments led to a better characterization of the cytokines involved. TNFα levels were found to be increased in the elderly populations and positively correlated with IL-6 and CRP levels and were associated with general atherosclerosis and Alzheimer’s disease [106]; in another study, IL-6 was found to be elevated in the elderly and associated with increased morbidity and mortality [107].
Over the past several years, many studies looked into the mechanisms that comprise inflammaging. As tissues age, cellular and organelle damage results in the accumulation of cellular debris. This cellular debris (for example, damaged DNA) contains damage-associated molecular patterns (DAMP) that are sensed by the pattern recognition molecules, such as the Nod-like receptor family and toll-like receptors [108], capable of activating the innate immune system as well as the inflammasome and NF-κB [109]). Free radicals from oxidative stress, components of the damaged cells and organelles, and metabolic by-products such as fatty acids, urate crystals, cardiolipin, peroxidized lipids, amyloid, advanced glycation end products, and altered N-glycans can be recognized by a series of sensors as “danger” signals that activate immune responses [110].
One of these sensors is a Nlrp3 inflammasome, a multi-protein complex, which upon sensing a danger signal, leads to the activation of pro-caspase, resulting in an increase of the pro-inflammatory cytokines such as IL-1β and IL-18. IL-1β is a potent activator of IL-6 and IL-8, important players in SASP (senescence-associated secretory phenotype) [111]. Rodier et al. showed that persistent DNA damage leads to senescence-associated inflammatory cytokine secretion [112].
As cellular damage accumulates with aging, this pro-inflammatory state becomes chronic [104].
Most of the signals that activate the inflammasome result in the generation of reactive oxygen species in the mitochondria. When mitochondria are damaged, they release damage-associated molecular patterns (mitochondrial DNA and formyl peptides), some of which are phylogenetically similar to bacteria-associated molecular patterns, which are powerful activators of the innate immune system [113] as well as Nlrp3 inflammasome. Both mitochondrial cardiolipin and fragments of mitochondrial DNA (due to its evolutionary similarity to bacteria) represent an endogenous pathogen-associated molecular pattern capable of activating the inflammasome and leading to chronic inflammation [114, 115]. Wikby et al. found that IL-6 levels were associated with an immune risk phenotype (described above) [107]. Another group showed that two inflammatory marker (IL-6 and TNFα soluble receptor 1) levels could be used to predict the 10-year mortality in the elderly [116]. Erschler et al. showed that elevated IL-6 levels in the elderly are associated with the increased frailty and chronic inflammation [117].
Cumulative cellular damage and stress lead to cellular senescence via a cell cycle arrest, a mechanism that is set to protect the organism from accumulating damaged, aberrant machinery that can potentially result in cancer. These senescent cells comprise a senescence-associated secretory phenotype (SASP), producing various inflammatory cytokines (Il-1, IL-6, IL-8, IL-7, IL-13, IL-15) [118, 119]. With age, senescent cells accumulate in many tissues, particularly in the adipose tissue, known to be responsible for a large source of pro-inflammatory cytokines [120], such as IL-6 [121].
Conclusion
The concept of immunosenescence has an important implication for how we view inflammatory diseases, risk of infections, and safety of immunomodulatory and immune suppressive treatments in the aging population. Immune system changes in the elderly impart a higher susceptibility to infection and are associated with mortality, as well as a poor response to vaccines. The use of disease-modifying treatments, which are either immunomodulatory or overtly immunosuppressive, may have a more profound impact on patients whose immune system is already compromised and, thus, their risk of infection, for example, PML, may be higher. A similar concern stands for the increased risk of cancers associated with the use of some disease-modifying agents (fingolimod: lymphoma, basal cell carcinoma; natalizumab: melanoma), as the risk may be higher in the aging population due to the immunosenescent changes impairing tumor surveillance and control. Additionally, the qualitative and quantitative changes that occur with aging may be responsible for the nature of expression of multiple sclerosis, perhaps explaining the higher incidence of primary progressive MS in the older population [122].
Clinicians should exercise a high level of vigilance in monitoring the risk of infections in patients of older age on immunomodulatory treatments. The effects of immunosenescence should be strongly considered in the individual risk stratification of infection and cancer.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Pera A, Campos C, López N, Hassouneh F, Alonso C, Tarazona R, et al. Immunosenescence: implications for response to infection and vaccination in older people. Maturitas. 2015;82(Issue 1):50–55, ISSN 0378–5122. This paper discusses T cell and NK changes associated with immunosenescence, and how these affect risk of infection and response to vaccination in those of older age
Prosperini L, de Rossi N, Scarpazza C, et al. Natalizumab-related progressive multifocal leukoencephalopathy in multiple sclerosis: findings from an Italian Independent Registry. Aktas O PLoS One. 2016;11(12):e0168376. doi:10.1371/journal.pone.0168376
Dong-Si T, Gheuens S, Gangadharan A, et al. Predictors of survival and functional outcomes in natalizumab-associated progressive multifocal leukoencephalopathy. J Neurovirol. 2015;21(6):637–44. doi:10.1007/s13365-015-0316-4.
Biogen, 2016. Internal data on file.
Gagne Brosseau MS, Stobbe G, Wundes A. Natalizumab-related PML 2 weeks after negative anti-JCV antibody assay. Neurology. 2016;86(5):484–6. doi:10.1212/WNL.0000000000002330.
Nanda T. Progressive multifocal leukoencephalopathy in a HIV negative, Immunocompetent Patient. Case Reports in Neurological Medicine 2016;2016:7050613. doi:10.1155/2016/7050613.
Grewal J, Dalal P, Bowman M, Kaya B, Otero JJ, Imitola J. Progressive multifocal leukoencephalopathy in a patient without apparent immunosuppression. J Neurovirology. 2016 Oct;22(5):683–7.
Gourineni VC, Juvet T, Kumar Y, Bordea D, Sena KN. Progressive multifocal leukoencephalopathy in a 62-year-old immunocompetent woman. Case Reports in Neurological Medicine. 2014;2014:549271. doi:10.1155/2014/549271.
Johansen KK, Torp SH, Rydland J, Aasly JO. Progressive multifocal leukoencephalopathy in an immunocompetent patient? Case Rep Neurol. 2013;5(3):149–54. doi:10.1159/000354828. eCollection 2013
Christakis PG, Okin D, Huttner AJ, Baehring JM. Progressive multifocal leukoencephalopathy in an immunocompetent patient. J Neurol Sci. 2013;326(1–2):107–10. doi:10.1016/j.jns.2013.01.010.
Chang YY, Lan MY, Peng CH, Wu HS, Chang D, Liu JS. Progressive multifocal leukoencephalopathy in an immunocompetent Taiwanese patient. J Formos Med Assoc. 2007;106(2 Suppl):S60–4.
Naess H, Glad S, Storstein A, Rinaldo CH, Mørk SJ, Myhr KM, et al. Progressive multifocal leucoencephalopathy in an immunocompetent patient with favourable outcome. A case report BMC Neurol. 2010;10:32. doi:10.1186/1471-2377-10-32.
Novartis, 2016. Internal data on file.
Grebenciucova E, Reder AT, Bernard JT. Immunologic mechanisms of fingolimod and the role of immunosenescence in the risk of cryptococcal infection: a case report and review of literature. Mult Scler Relat Disord. 2016;9:158–62. doi:10.1016/j.msard.2016.07.015. Review
Confavreux C, Vukusic S. Natural history of multiple sclerosis: a unifying concept. Brain. 2006;129(Pt 3):606–16.
Schwanitz N, Boldt A, Stoppe M, Orthgiess J, Borte S, Sack U, and Bergh FT. Treatment, safety, and tolerance: longterm fingolimod treatment of multiple sclerosis Induces Phenotypical Immunsenescence (P2.082). April 5, 2016, 86: 16 Supplement P2.082; published ahead of print April 8, 2015, 1526-632X.
Wikby A, Ferguson F, Forsey R, et al. An immune risk phenotype, cognitive impairment, and survival in very late life: impact of allostatic load in Swedish octogenarian and nonagenarian humans. J Gerontol A Biol Sci Med Sci. 2005;60(5):556–65.
Ricklin ME, Lorscheider J, Waschbisch A, Paroz C, Mehta SK, Pierson DL, et al. T-cell response against varicella-zoster virus in fingolimod-treated MS patients. Neurology. 2013;81(2):174–81. doi:10.1212/WNL.0b013e31829a3311.
Mitchell BM, Bloom DC, Cohrs RJ, Gilden DH, Kennedy PG. Herpes simplex virus-1 and varicella-zoster virus latency in ganglia. J Neurovirology. 2003;9(2):194–204.
Fleming DM, Cross KW, Cobb WA, Chapman RS. Gender difference in the incidence of shingles. Epidemiol Infect. 2004;132:1–5.
Kennedy PG, Cohrs RJ. Varicella-zoster virus human ganglionic latency: a current summary. J Neurovirology. 2010;16(6):411–8. doi:10.3109/13550284.2010.515652.
Donahue JG, Choo PW, Manson JE, Platt R. The incidence of herpes zoster. Arch Intern Med. 1995;155:1605–9.
Biogen, 2017 Jan. Internal data on file.
Robb J, Hyland M, Samkoff L. Dimethyl fumarate-associated lymphopenia in clinical practice: implications for disease modifying therapy selection. Session 231- MS and CNS Inflammatory Disease: Switching and Comparator Studies II. P6.192. April 21, 2016 AAN.
Longbrake EE, Naismith RT, Parks BJ, Wu GF, Cross AH. Dimethyl fumarate-associated lymphopenia: risk factors and clinical significance. Mult Scler J Exp Transl Clin. 2015;
Foley J, Christensen A, Hoyt T, Foley A, Metzger R. Is aging and immunosenescence a risk factor for dimethyl fumarate induced PML? Neurology. 2016;86:P2.088.
Khatri BO, Garland J, Berger J, Kramer J, Sershon L, Olapo T, et al. The effect of dimethyl fumarate (Tecfidera™) on lymphocyte counts: a potential contributor to progressive multifocal leukoencephalopathy risk. Mult Scler Relat Disord. 2015;4(4):377–9. doi:10.1016/j.msard.2015.05.003.
Spencer CM, Crabtree-Hartman EC, Lehmann-Horn K, Cree BA, Zamvil SS. Reduction of CD8(+) T lymphocytes in multiple sclerosis patients treated with dimethyl fumarate. Neurol Neuroimmunol Neuroinflamm. 2015;2(3):e76. doi:10.1212/NXI.0000000000000076.
Stüve O, Marra CM, Bar-Or A, Niino M, Cravens PD, Cepok S, et al. Altered CD4+/CD8+ T-cell ratios in cerebrospinal fluid of natalizumab-treated patients with multiple sclerosis. Arch Neurol. 2006;63(10):1383–7.
Carson KR, Evens AM, Richey EA, et al. Progressive multifocal leukoencephalopathy after rituximab therapy in HIV-negative patients: a report of 57 cases from the research on adverse drug events and reports project. Blood. 2009;113(20):4834–40.
Brien JD, Uhrlaub JL, Hirsch A, Wiley CA, Nikolich-Žugich J. Key role of T cell defects in age-related vulnerability to West Nile virus. J Exp Med. 2009;206(12):2735–45. doi:10.1084/jem.20090222.
Stowe RP, Kozlova EV, Yetman DL, Walling DM, Goodwin JS, Glaser R. Chronic herpesvirus reactivation occurs in aging. Exp Gerontol. 2007;42(6):563–70. doi:10.1016/j.exger.2007.01.005.
Steinmann GG, Klaus B, Müller-Hermelink HK. The involution of the ageing human thymic epithelium is independent of puberty. A morphometric study. Scand J Immunol. 1985 Nov;22(5):563–75.
Murray JM, Kaufmann GR, Hodgkin PD, Lewin SR, Kelleher AD, Davenport MP, et al. Naive T cells are maintained by thymic output in early ages but by proliferation without phenotypic change after age twenty. Immunol Cell Biol. 2003;81(6):487–95.
Ferrando-Martínez S, Ruiz-Mateos E, Hernández A, Gutiérrez E, Rodríguez-Méndez Mdel M, Ordoñez A, et al. Age-related deregulation of naive T cell homeostasis in elderly humans. Age (Dordr). 2011;33(2):197–207. doi:10.1007/s11357-010-9170-8.
Franco JM, León-Leal JA, Leal M, Cano-Rodriguez A, Pineda JA, Macías J, et al. CD4+ and CD8+ T lymphocyte regeneration after anti-retroviral therapy in HIV-1-infected children and adult patients. Clin Exp Immunol. 2000 Mar;119(3):493–8.
Jamieson BD, Douek DC, Killian S, Hultin LE, Scripture-Adams DD, Giorgi JV, et al. Generation of functional thymocytes in the human adult. Immunity. 1999;10(5):569–75.
Den Braber I, Mugwagwa T, Vrisekoop N, Westera L, Mögling R, de Boer AB, et al. Maintenance of peripheral naive T cells is sustained by thymus output in mice but not humans. Immunity. 2012;36(2):288–97. doi:10.1016/j.immuni.2012.02.006.
Palmer DB. The effect of age on thymic function. Front Immunol. 2013;4:316.
Naylor K, Li G, Vallejo AN, Lee WW, Koetz K, Bryl E, et al. The influence of age on T cell generation and TCR diversity. J Immunol. 2005;174(11):7446–52.
Duszczyszyn DA, Williams JL, Mason H, Lapierre Y, Antel J, Haegert DG. Thymic involution and proliferative T-cell responses in multiple sclerosis. J Neuroimmunol. 2010;221(1–2):73–80. doi:10.1016/j.jneuroim.2010.02.005.
•• Nikolich-Zugich J, Li G, Uhrlaub JL, Renkema KR, Smithey MJ. Age-related changes in CD8 T cell homeostasis and immunity to infection. Semin Immunol. 2012;24:356–64. This paper discusses age-associated defects in T cell response to vaccines
Cavanagh MM, Qi Q, Weyand CM, Goronzy JJ. Finding balance: T cell regulatory receptor expression during aging. Aging Dis. 2011;2:398–413.
Wherry EJ. T cell exhaustion. Nat Immunol. 2011;12:492–9.
Akbar AN, Henson SM. Are senescence and exhaustion intertwined or unrelated processes that compromise immunity? Nat Rev Immunol. 2011;11:289–95.
Deng Y, Jing Y, Campbell AE, Gravenstein S. Age-related impaired type 1 T cell responses to influenza: reduced activation ex vivo, decreased expansion in CTL culture in vitro, and blunted response to influenza vaccination in vivo in the elderly. J Immunol. 2004;172:3437–46.
McElhaney JE, Xie D, Hager WD, Barry MB, Wang Y, Kleppinger A, et al. T cell responses are better correlates of vaccine protection in the elderly. J Immunol. 2006;176:6333–9.
Messaoudi I, LeMaoult J, Guevara-Patino JA, Metzner BM, Nikolich-Žugich J. Age-related CD8 T cell clonal expansions constrict CD8 T cell repertoire and have the potential to impair immune defense. J Exp Med. 2004;200(10):1347–58. doi:10.1084/jem.20040437.
Smithey MJ, Renkema KR, Rudd BD, Nikolich-Zugich J. Increased apoptosis, curtailed expansion and incomplete differentiation of CD8+ T cells combine to decrease clearance of L. monocytogenes in old mice. Eur J Immunol. 2011;41:1352–64.
Britanova OV, Putintseva EV, Shugay M, et al. Age-related decrease in TCR repertoire diversity measured with deep and normalized sequence profiling. J Immunol. 2014;192:2689–98.
Qi Q, Liu Y, Cheng Y, et al. Diversity and clonal selection in the human T-cell repertoire. Proc Natl Acad Sci U S A. 2014;111
Van Epps P, Banks R, Aung H, Betts MR, Canaday DH. Age-related differences in polyfunctional T cell responses. Immun Ageing. 2014;11:14. doi:10.1186/1742-4933-11-14. eCollection 2014
Effros RB, Dagarag M, Spaulding C, Man J. The role of CD8+ T-cell replicative senescence in human aging. Immunol Rev. 2005;205:147–57. Review
• Briceno O, Lissina A, Wanke K, et al. Reduced naive CD8(1) T cell priming efficacy in elderly adults. Aging Cell. 2016;15:14–21. This paper describes functional deficits of CD8 T cells in those of older age
•• Goronzy JJ, Weyand CM. Understanding immunosenescence to improve responses to vaccines. Nat Immunol. 2013;14:428–36. These author reviews age-associated immune changes and how they impact one’s response to vaccines
Schulz AR, Malzer JN, Domingo C, et al. Low thymic activity and dendritic cell numbers are associated with the immune response to primary viral infection in elderly humans. J Immunol. 2015;195:4699–711.
Foy TM, Aruffo A, Bajorath J, Buhlmann JE, Noelle RJ. Immune regulation by CD40 and its ligand GP39. Annu Rev Immunol. 1996;14:591–617.
Eaton SM, Burns EM, Kusser K, Randall TD, Haynes L. Age-related defects in CD4 T cell cognate helper function lead to reductions in humoral responses. J Exp Med. 2004;200(12):1613–22.
Rea IM, Stewart M, Campbell P, Alexander HD, Crockard AD, Morris TC. Changes in lymphocyte subsets, interleukin 2, and soluble interleukin 2 receptor in old and very old age. Gerontology. 1996;42:69–78.
Lages CS, Suffia I, Velilla PA, Huang B, Warshaw G, Hildeman DA, et al. Functional regulatory T cells accumulate in aged hosts and promote chronic infectious disease reactivation. J Immunol. 2008;181(3):1835–48.
Rosenkranz D, Weyer S, Tolosa E, Gaenslen A, Berg D, Leyhe T, et al. Higher frequency of regulatory T cells in the elderly and increased suppressive activity in neurodegeneration. J Neuroimmunol. 2007;188:117–27.
Lefebvre JS, Haynes L. Aging of the CD4 T cell compartment. Open Longev Sci. 2012;6:83–91.
Weinberger B, Welzl K, Herndler-Brandstetter D, Parson W, Grubeck-Loebenstein B. CD28(−)CD8(+) T cells do not contain unique clonotypes and are therefore dispensable. Immunol Lett. 2009;1:27–32.
Weng N, Akbar AN, Goronzy J. CD28− T cells: their role in the age-associated decline of immune function. Trends Immunol. 2009;30(7):306–12. doi:10.1016/j.it.2009.03.013.
Fagnoni FF, Vescovini R, Mazzola M, Bologna G, Nigro E, Lavagetto G, et al. Expansion of cytotoxic CD8+ CD28- T cells in healthy ageing people, including centenarians. Immunology. 1996;4:501–7.
Kim J, Kim A-R, Shin E-C. Cytomegalovirus infection and memory T cell inflation. Immune Network. 2015;15(4):186–90. doi:10.4110/in.2015.15.4.186.
Stacy S, Krolick KA, Infante AJ, Kraig E. Immunological memory and late onset autoimmunity. Mech Ageing Dev. 2002;123(8):975–85.
Quinn KM, Zaloumis SG, Cukalac T, et al. Heightened self-reactivity associated with selective survival, but not expansion, of naive virus-specific CD8 T cells in aged mice. Proc Natl Acad Sci USA. 2016;113:1333–8. 13139–44
Li G, Ju J, Weyand CM, Goronzy JJ. Age-associated failure to adjust type I interferon receptor signaling thresholds after T-cell activation. Journal of immunology (Baltimore, Md : 1950). 2015;195(3):865–74. doi:10.4049/jimmunol.1402389.
Matikainen S, Sareneva T, Ronni T, Lehtonen A, Koskinen PJ, Julkunen I. Interferon-alpha activates multiple STAT proteins and upregulates proliferation-associated IL-2Ralpha, c-myc, and pim-1 genes in human T cells. Blood. 1999;93:1980–199.
Fan X, Rudensky AY. Hallmarks of tissue-resident lymphocytes. Cell. 2016;164:1198–211.
Thome JJC, Farber DL. Emerging concepts in tissue-resident T cells: lessons from humans. Trends Immunol. 2015;36:428–35.
Ariotti S, Beltman JB, Chodaczek G, Hoekstra ME, van Beek AE, Gomez-Eerland R, et al. Tissue-resident memory CD8+ T cells continuously patrol skin epithelia to quickly recognize local antigen. Proc Natl Acad Sci U S A. 2012;109(48):19739–44. doi:10.1073/pnas.1208927109.
Moreau JF, Pradeu T, Grignolio A, Nardini C, Castiglione F, Tieri P, et al. The emerging role of ECM crosslinking in T cell mobility as a hallmark of immunosenescence in humans. Ageing Res Rev. 2016; doi:10.1016/j.arr.2016.11.005.
Denais CM, Gilbert RM, Isermann P, McGregor AL, te Lindert M, Weigelin B, et al. Nuclear envelope rupture and repair during cancer cell migration. Science. 2016;352(6283):353–8. doi:10.1126/science.aad7297.
Raab M, Gentili M, de Belly H, Thiam HR, Vargas P, Jimenez AJ, et al. ESCRT III repairs nuclear envelope ruptures during cell migration to limit DNA damage and cell death. Science. 2016;352:359–62.
•• Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014;69(Suppl 1):S4–9. doi:10.1093/gerona/glu057. These authors discuss the concept of inflammaging and how it is relevant to those of older age
Zhang G, Li J, Purkayastha S, et al. Hypothalamic programming of systemic ageing involving IKK-β. NF-κB and GnRH Nature. 2013;497:211–6. doi:10.1038/nature12143.
Adler AS, Sinha S, Kawahara TL, Zhang JY, Segal E, Chang HY. Motif module map reveals enforcement of aging by continual NF-kappaB activity. Genes Dev. 2007;21:3244–57. doi:10.1101/gad.1588507.
Freund A, Patil CK, Campisi J. p38MAPK is a novel DNA damage response-independent regulator of the senescence-associated secretory phenotype. EMBO J. 2011;30:1536–48. doi:10.1038/emboj.2011.69.
Boraschi D, Del Giudice G, Dutel C, Ivanoff B, Rappuoli R, Grubeck-Loebenstein B. Ageing and immunity: addressing immune senescence to ensure healthy ageing. Vaccine. 2010;28:3627–31.
McElhaney JE, Effros RB. Immunosenescence: what does it mean to health outcomes in older adults? Curr Opin Immunol. 2009;21:418–24.
Frasca D, Diaz A, Romero M, et al. Intrinsic defects in B cell response to seasonal influenza vaccination in elderly humans. Vaccine. 2010;28(51):8077–84.
• Ademokun A, Wu YC, Dunn-Walters D. The ageing B cell population: composition and function. Biogerontology. 2010;11:125–37. The authors highlight age-related changes occurring in B cell subset
Guerrettaz LM, Johnson SA, Cambier JC. Acquired hematopoietic stem cell defects determine B-cell repertoire changes associated with aging. Proc Natl Acad Sci U S A. 2008;105(33):11898–902. doi:10.1073/pnas.0805498105.
Riley RL, et al. B cell precursors are decreased in senescent BALB/c mice, but retain normal mitotic activity in vivo and in vitro. Clin Immunol Immunopathol. 1991;59:301–13.
Rossi DJ, Bryder D, Zahn JM, Ahlenius H, Sonu R, Wagers AJ, et al. Cell intrinsic alterations underlie hematopoietic stem cell aging. Proc Natl Acad Sci U S A. 2005;102:9194–9.
McKenna RW, Washington LT, Aquino DB, Picker LJ, Kroft SH. Immunophenotypic analysis of hematogones (B-lymphocyte precursors) in 662 consecutive bone marrow specimens by 4-color flow cytometry. Blood. 2001;98(8):2498–507.
Gibson KL, Wu YC, Barnett Y, Duggan O, Vaughan R, Kondeatis E, et al. B-cell diversity decreases in old age and is correlated with poor health status. Aging Cell. 2009;8:18–25.
Frasca D, Blomberg BB. Aging affects human B cell responses. J Clin Immunol. 2011;31:430–5.
Abbatecola AM, Ferrucci L, Grella R, Bandinelli S, Bonafè M, Barbieri M, et al. Diverse effect of inflammatory markers on insulin resistance and insulin resistance syndrome in the elderly. J Am Geriatr Soc. 2004;52:399–404. doi:10.1111/j.1532-5415.2004.52112.x.
Joehanes R, Johnson AD, Barb JJ, Raghavachari N, Liu P, Woodhouse KA, et al. Gene expression analysis of whole blood, peripheral blood mononuclear cells, and lymphoblastoid cell lines from the Framingham Heart Study. Physiol Genomics. 2012;44:59–75. doi:10.1152/physiolgenomics.00130.2011.
De Martinis M, Franceschi C, Monti D, Ginaldi L. Inflamm-ageing and lifelong antigenic load as major determinants of ageing rate and longevity. FEBS Lett. 2005;579:2035–9. doi:10.1016/j.febslet.2005.02.055.
Ogata K, Yokose N, Tamura H, An E, Nakamura K, Dan K, et al. Natural killer cells in the late decades of human life. Clin Immunol Immunopathol. 1997;84:269–75.
Remarque E, Pawelec G. T cell immunosenescence and its clinical relevance in man. Rev Clin Gerontol. 1998;8:5–14.
Gayoso I, Sanchez-Correa B, Campos C, Alonso C, Pera A, Casado JG, et al. Immunosenescence of human Natural killer cells. J Innate Immun. 2011;3:337–43.
Lopez-Verges S, Milush JM, Pandey S, York VA, Rakawa-Hoyt J, Pircher H, et al. CD57 defines a functionally distinct population of mature NK cells in the human CD56dimCD16+ NK cell subset. Blood. 2010;116:3865–74.
Mariani E, Monaco MC, Cattini L, Sinoppi M, Facchini A. Distribution and lytic activity of NK cell subsets in the elderly. Mech Ageing Dev. 1994;76:177–87.
Borrego F, Alonso MC, Galiani MD, Carracedo J, Ramirez R, Ostos B, et al. NK phenotypic markers and IL2 response in NK cells from elderly people. Exp Gerontol. 1999;34:253–65.
DelaRosa O, Pawelec G, Peralbo E, Wikby A, Mariani E, Mocchegiani E, et al. Immunological biomarkers of ageing in man: changes in both innate and adaptive immunity are associated with health and longevity. Biogerontology. 2006 Oct-Dec;7(5–6):471–81.
Tarazona R, Gayoso I, Alonso C, Pita-Lopez ML, Peralbo E, Casado JG, et al. NK cells in human ageing. In: Fulop T, Franceschi C, Hirokawa K, Pawelec G, editors. Handbook on Immunosenescence. New York: Springer; 2009. p. 533–46.
Arnon TI, Achdout H, Levi O, Markel G, Saleh N, Katz G, et al. Inhibition of the NKp30 activating receptor by pp65 of human cytomegalovirus. Nat Immunol. 2005;6:515–23.
Fernández- Garrido J, Navarro- Martínez R, Buigues- González C, Martínez- Martínez M, Ruiz- Ros V, Cauli O. The value of neutrophil and lymphocyte count in frail older women. Exp Gerontol. 2014;54:35–41. doi:10.1016/j.exger.2013.11.019.
Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E, et al. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci. 2000;908:244–54.
Fagiolo U, Cossarizza A, Scala E, Fanales-Belasio E, Ortolani C, Cozzi E, et al. Increased cytokine production in mononuclear cells of healthy elderly people. Eur J Immunol. 1993;23(9):2375–8.
Bruunsgaard H, Andersen-Ranberg K, Jeune B, Pedersen AN, Skinhøj P, Pedersen BK. A high plasma concentration of TNF-alpha is associated with dementia in centenarians. J Gerontol A Biol Sci Med Sci. 1999;54(7):M357–64.
Wikby A, Nilsson BO, Forsey R, et al. The immune risk phenotype is associated with IL-6 in the terminal decline stage: findings from the Swedish NONA immune longitudinal study of very late life functioning. Mech Ageing Dev. 2006;127:695–704. doi:10.1016/j.mad.2006.04.003.
Fritz JH, Ferrero RL, Philpott DJ, Girardin SE. Nod-like proteins in immunity, inflammation and disease. Nat Immunol. 2006;7:1250–7.
Youm YH, Grant RW, McCabe LR, Albarado DC, Nguyen KY, Ravussin A, et al. Canonical Nlrp3 inflammasome links systemic low-grade inflammation to functional decline in aging. Cell Metab. 2013;18(4):519–32. doi:10.1016/j.cmet.2013.09.010.
Dall’Olio F, Vanhooren V, Chen CC, Slagboom PE, Wuhrer M, Franceschi C. N-glycomic biomarkers of biological aging and longevity: a link with inflammaging. Ageing Res Rev. 2013;12:685–98. doi:10.1016/j.arr.2012.02.002.
Acosta JC, Banito A, Wuestefeld T, Georgilis A, Janich P, Morton JP, et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat Cell Biol. 2013;15(8):978–90. doi:10.1038/ncb2784.
Rodier F, Coppé J-P, Patil CK, et al. Persistent DNA damage signaling triggers senescence-associated inflammatory cytokine secretion. Nat Cell Biol. 2009;11(8):973–9. doi:10.1038/ncb1909.
Zhang Q, Raoof M, Chen Y, et al. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010;464:104–7. doi:10.1038/nature08780.
Iyer SS, He Q, Janczy JR, et al. Mitochondrial cardiolipin is required for Nlrp3 inflammasome activation. Immunity. 2013;39(2):311–23. doi:10.1016/j.immuni.2013.08.001.
Pinti M, Cevenini E, Nasi M, De Biasi S, Salvioli S, Monti D, et al. Circulating mitochondrial DNA increases with age and is a familiar trait: implications for “inflamm-aging”. Eur J Immunol. 2014;44(5):1552–62. doi:10.1002/eji.201343921.
Varadhan R, Yao W, Matteini A, Beamer BA, Xue QL, Yang H, et al. Simple biologically informed inflammatory index of two serum cytokines predicts 10 year all-cause mortality in older adults. J Gerontol A Biol Sci Med Sci. 2014;69(2):165–73. doi:10.1093/gerona/glt023.
Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annu Rev Med. 2000;51:245–70.
Campisi J, d’Adda di Fagagna F. Cellular senescence: when bad things happen to good cells. Nat Rev Mol Cell Biol. 2007;8:729–40. doi:10.1038/nrm2233.
Coppé J-P, Desprez P-Y, Krtolica A, Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Annual Review of Pathology. 2010;5:99–118. doi:10.1146/annurevpathol-121808-102144.
Tchkonia T, Morbeck DE, Von Zglinicki T, et al. Fat tissue, aging, and cellular senescence. Aging Cell. 2010;9:667–84. doi:10.1111/j.1474-9726.2010.00608.
Khaodhiar L, Ling PR, Blackburn GL, Bistrian BR. Serum levels of interleukin-6 and C-reactive protein correlate with body mass index across the broad range of obesity. JPEN J Parenter Enteral Nutr. 2004;28(6):410–5.
Polliack ML, Barak Y, Achiron A. Late-onset multiple sclerosis. J Am Geriatr Soc. 2001;49(2):168–71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Elena Grebenciucova, M. D. received James T. Lubin Clinician Scientist Fellowship Award from The Transverse Myelitis Association dedicated to promising research and exceptional clinical care for rare neuro-immune disorders, such as transverse myelitis, including acute flaccid myelitis, acute disseminated encephalomyelitis, neuromyelitis optica, and optic Neuritis. Joseph R. Berger, M.D. has served as a consultant and/or on the PML adjudication committees of Amgen, AstraZeneca, Bristol Myers Squibb, Eisai, Janssen, Parexel, and Pfizer; serves on the Scientific Advisory Board of NeuVir and ExcisionBio; has received honoraria from Prime Education and the MS Foundation for lectures; serves as an Associate Editor for the Journal of Neurovirology, serves as an editorial board member of ISRN Education, Neuroscience, World Journal of Rheumatology, and MS and other related disorders; receives publishing royalties for Handbook of Clinical Neurology, Vol. 85 (Elsevier, 2007); has served as a consultant to Alcimed, Amgen, AstraZeneca, Bayer, Biogen, Eisai, EMD Serono, Forward Pharmaceuticals, Genentech/Roche, Genzyme, Inhibikase, Millenium/Takeda, Novartis, Johnson and Johnson, Pfizer, and Sanofi Aventis; receives research support from Biogen; and has participated in legal proceedings for Biogen.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Demyelinating Disorders
Rights and permissions
About this article
Cite this article
Grebenciucova, E., Berger, J.R. Immunosenescence: the Role of Aging in the Predisposition to Neuro-Infectious Complications Arising from the Treatment of Multiple Sclerosis. Curr Neurol Neurosci Rep 17, 61 (2017). https://doi.org/10.1007/s11910-017-0771-9
Published:
DOI: https://doi.org/10.1007/s11910-017-0771-9