Abstract
Purpose of Review
Multiple sclerosis (MS) is a chronic, immune-mediated demyelinating disorder of the central nervous system. Age is one of the most important factors in determining MS phenotype. This review provides an overview of how age influences MS clinical characteristics, pathology, and treatment.
Recent findings
New methods for measuring aging have improved our understanding of the aging process in MS. New studies have characterized the molecular and cellular composition of chronic active or smoldering plaques in MS. These lesions are important contributors to disability progression in MS. These studies highlight the important role of immunosenescence and the innate immune system in sustaining chronic inflammation. Given these changes in immune function, several studies have assessed optimal treatment strategies in aging individuals with MS.
Summary
MS phenotype is intimately linked with chronologic age and immunosenescence. While there are many unanswered questions, there has been much progress in understanding this relationship which may lead to more effective treatments for progressive disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a chronic, immune-mediated demyelinating disorder of the central nervous system. Disease presentation and clinical course are variable and significantly influenced by an individual’s age. The average age of onset is between 20 and 40 years with over 80% of cases initially presenting with a relapsing and remitting phenotype [1]. Over time many of these patients go on to develop a progressive phenotype characterized by disability accumulation in the absence of relapses. As our population ages and improvements have been made in the diagnosis and management of MS, the prevalence of MS has increased from 58 per 100,000 in 1990 to 309 per 100,000 in 2010 [2]. With improved treatment, the average age of individuals with MS has also increased, peaking at 50–59 in 2008 [2]. Because older age is one of the main risk factors for progressive disease, the number of individuals living with progressive MS is expected to increase. Our current MS treatments are effective in preventing relapses but have been less effective in treating progressive disease, creating a large unmet need. There are numerous age-related changes in immune and neuronal function that affect MS phenotype, pathology, and treatment efficacy [3]. Understanding these changes is crucial for developing effective management strategies for patients aging with MS. This review provides an overview of how age influences MS clinical characteristics, pathology, and treatment.
The clinical effects of aging in multiple sclerosis
MS is typically diagnosed between the ages of 20 and 40 years, with a mean onset around 30 years [1]. However, age of onset can range from childhood to older adulthood, with age of onset affecting disease activity and clinical course. Younger individuals tend to have more frequent relapses, while older individuals have fewer relapses but more progressive disability [4,5,6]. Chronologic age is strongly associated with disability accumulation and conversion to a progressive phenotype [4].
Pediatric-onset multiple sclerosis (POMS) accounts for 3–10% of all MS cases [5]. Approximately 99% of POMS begins as relapsing–remitting MS, while primary progressive MS is virtually nonexistent in this population [7]. In comparison, primary progressive MS makes up approximately 10–15% of MS cases in the adult population with a mean age of onset of 45 years [6, 8]. Gorman et al. demonstrated nearly threefold higher relapse rates in POMS patients compared to adult MS patients [5]. POMS is also associated with a higher burden of T2 lesions on MRI and more extensive axonal injury compared to adults, suggesting more aggressive inflammatory relapses [9, 10]. Despite high relapse rates, POMS patients tend to recover well and take longer to reach ambulatory disability milestones compared to adults [7]. The time to develop secondary progressive MS is about 32 years in pediatric-onset disease compared to 18 years in adult-onset disease [7]. Despite this, individuals with POMS reach disability milestones 7 to 12 years younger than individuals with adult-onset MS [7].
In relapsing-onset MS, relapse rates decline with disease duration by approximately 17% every 5 years [11]. Individuals who are older at MS onset experience a more rapid decline in relapse rates compared to individuals who are younger at onset [11]. Tremlett et al. observed a 30.5% decline in relapse rates for every 5 years disease duration in individuals > 40 years, a 22.9% decline in individuals 30–40 years, and a 6.9% decline in individuals < 20 years [11]. In addition, chronologic age is the most consistent risk factor associated with progressive disease. Both primary and secondary progressive MS occur at a mean age of 45 years and follow similar clinical trajectories once established, regardless of preceding relapse history [6, 8]. Older age at time of relapsing–remitting diagnosis increases the probability of developing secondary progressive disease and shortens the interval in which individuals accumulate ambulatory disability [4, 6]. Scalfari et al. found the risk of converting to secondary progressive MS was doubled with MS onset at 40 years and tripled with onset at 50 years, compared to onset at 20 years [6]. This effect was independent of disease duration [6]. The precise mechanism by which age drives this phenotype shift is not fully elucidated but is likely driven by intrinsic aging-related changes to immune and nervous system function.
The effect of age on multiple sclerosis pathophysiology
Acute demyelination is the hallmark of relapsing remitting MS, but even early in disease course there is also evidence of neurodegeneration. With aging and longer disease duration, there are shifts in predominant pathophysiology, which is seen in both histology and imaging.
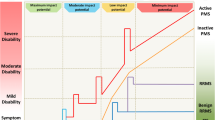
During the formation of an acute demyelinating lesion or plaque, peripheral leukocytes, primarily CD8 + T cells, monocytes, and macrophages, cross the blood brain barrier of leaky venules and attack myelin sheathes [1]. This is histologically characterized by perivenular infiltration of leukocytes with surrounding demyelination (Fig. 1). On MRI, these lesions acutely appear as T2 hyperintense with enhancement on T1 gadolinium sequences, the latter representing blood brain barrier breakdown [1]. Initially, neurons may be left intact, but even early in lesion evolution there is some degree of axonal loss and neuronal damage [1]. As acute lesions heal, they cease to enhance and either decrease in size or stabilize. More severe inflammatory lesions cause significant axonal loss, leaving behind hypointense T1 lesions, informally termed “black holes” [1]. Lucchinetti et al. described four distinct pathologic subtypes of MS lesions [12]. Type I and II were characterized by the above described perivenular inflammation with type II expressing more pronounced immunoglobulin deposition [12]. Type III and IV lesions were characterized by oligodendrocyte dystrophy with type IV lesions being seen exclusively in primary progressive MS and further characterized by extensive oligodendrocyte loss and lack of remyelination [12].
Early and Late Disease Stages in Multiple Sclerosis Lesion Phenotypes. Created with BioRender.com. Early disease stage in Relapsing/Remitting MS (RRMS) lesions (a) are primarily acute active inflammatory lesions caused by leakage of peripheral lymphocytes through the blood brain barrier (BBB) and secretion of pro-inflammatory markers activating inflammatory macrophages and resulting in demyelination and reduced remyelination. Late disease state in progressive MS lesions (b) are primarily characterized as chronic active or “smoldering” lesions caused by macrophage/microglia activation, leading to axonal loss and neurodegeneration. Activated microglia contribute to the chronic micro-inflammatory environment that leads to OPC dysfunction and reduced remyelination. Created by biorender.com/
With advancing chronologic age and disease duration, the number of actively demyelinating plaques declines [13]. Active plaques may be replaced by either inactive or slowly expanding lesions (SELs), also referred to as chronic active or smoldering plaques [13]. On histology, smoldering plaques are primarily characterized by a rim of activated microglia, macrophages and reactive astrocytes surrounding a hypocellular, gliotic core (Fig. 1) [1]. The microglia and macrophages at the lesion’s leading-edge express inflammation associated proteins such as nitric oxide synthase (iNOS), CD40, interleukins, complement, major histocompatibility complex (MHC) class II, and tumor necrosis factors (TNFs) [14]. Absinta et al. described a unique inflammatory microglial transcriptional profile, termed “microglia inflamed in MS” (MIMS), which overlaps with that of the disease-associated microglia (DAM) observed in other neurodegenerative diseases [15•]. Within the gliotic core, there is virtually no remyelination and remaining progenitor cells express senescence markers such as p16INK4a [14, 16]. Perivascular lymphocytic infiltrates are present, but to less of an extent than in active MS lesions, and the blood brain barrier remains largely intact [1, 13].
On neuroimaging, smoldering plaques rarely enhance and instead may appear as slowly expanding lesions (SELs) or paramagnetic rim lesions (PRLs) [17•]. SELs are characterized by gradual enlargement of preexisting T2 lesions on serial imaging [17•]. Paramagnetic rim lesions (PRL) are characterized by a rim of hypointensity on susceptibility weighted imaging, representing the accumulation of iron-laden activated microglia and macrophages at the leading-edge of these lesions [17•]. SELs and PRLs are present in all MS phenotypes but are more frequent and numerous in progressive MS [17•, 18]. PRLs correlate with increased levels of neurofilament light chain (NFL) as a marker of axonal injury and are histologically associated with persistent inflammation, impaired remyelination, axonal loss, and irreversible tissue degeneration [19].
With advancing chronologic age and disease duration there is a shift in the underlying histologic and radiographic characteristics of MS plaques. Frischer et al. found that after approximately 30 years of disease duration there were virtually no active plaques (0.002%), with most plaques consisting of inactive (50%), smoldering (23%), or partially remyelinated shadow plaques (20%) [13]. On average, smoldering plaques develop after a disease duration of 10 years and peak around 50 years of age [13]. These lesions are associated with greater relapse-independent disability accumulation and progressive MS [20]. Active MS plaques are more likely to become smoldering plaques when they are larger volume or occur in older individuals [17•]. For example, active MS plaques that form in individuals > 35 years are more likely to become smoldering plaques [21]. Overall, smoldering plaques appear to correlate with the clinical transition between relapsing and progressive MS.
Brain atrophy is accelerated in individuals with MS compared to healthy controls occurring at a rate of 0.7%-1% per year and 0.1%-0.3% per year respectively [22]. MS-specific atrophy accounts for a larger proportion of total brain atrophy earlier in the disease course but represents a diminishing proportion as normal age-related atrophy accumulates with advancing chronologic age [23]. Azevendo et al. demonstrated that at 30 years most atrophy observed was attributable to MS, while at 60 years most atrophy accumulation was attributable to normal aging with little excess atrophy attributable to MS [23]. The gray matter atrophy observed is not entirely explained by white matter lesion volume and likely represents local gray-matter demyelination and neurodegeneration [23, 24]. Gray matter atrophy is seen in all disease phenotypes, occurs early in the disease course, and becomes more prominent with advancing disease [25]. Cortical demyelination has been shown to follow a superficial to deep gradient, suggesting inflammation being driven from the meningeal-subpial border [26, 27]. Cortical demyelination is associated with meningeal inflammation and the development of meningeal lymphoid structures, which resemble tertiary lymphoid structures but lack important regulatory elements such as the FOXP3 + regulatory T cells [27]. These meningeal lymphoid follicles are primarily observed in progressive MS and are associated with more aggressive disease and disability [27]. Furthermore, meningeal inflammation has been shown to induce phenotypic changes in cortical microglia associated with neuronal loss and may represent a pathologic mechanism behind cortical neurodegeneration [28].
In summary, the clinical change from relapsing–remitting MS to progressive MS is associated with a shift from highly active inflammatory lesions driven by peripheral lymphocytes to chronic slowly expanding lesions characterized by activated microglia.
Measuring somatic biological age in multiple sclerosis
Chronologic age is defined by an individual’s birthdate, whereas biological age is defined by biomarkers of the overall aging process across different organ systems and tissues. Several studies have shown that biological age varies substantially in individuals with the same chronologic age [29, 30]. Measuring biological age in patients with MS may serve as a more precise measure of aging effects on the disease [31, 32].
Telomere length is one of the most well studied measures of biological age. Telomeres are complexes of repetitive nucleotide sequences and proteins at the end of chromosomes, which act to preserve genomic stability during replication [33]. With each cell division the telomere’s terminal end is shortened due to the inability of DNA polymerase to completely replicate the 5’ ends of DNA. Progressive telomere shortening ultimately leads to DNA damage and initiation of signal cascades involved in cellular senescence [34]. Telomere attrition is also influenced by environmental stressors that lead to oxidative stress [33]. Leukocyte telomere length (LTL) has been associated with several age-related diseases such as cardiovascular disease, diabetes, cancer, and dementia [35, 36]. LTL is associated with increased mortality in patients with coronary heart disease [35, 36]. Modifiable cardiovascular risk factors such as smoking, obesity, and alcohol consumption are associated with shorter telomere length while exercise and adherence to a mediterranean diet are associated longer telomere length [37,38,39,40,41]. Certain nonmodifiable risk factors such as sex, race, and socioeconomic factors also influence telomere length [42,43,44]. Shorter LTL has been associated with autoimmune disorders such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) which may be driven by increased oxidative damage from chronic inflammation and accelerated lymphocyte turn over [45].
Telomere attrition is associated with progressive MS phenotypes and disability progression. Krysko et al. found that shorter LTL is associated with disability accumulation and brain atrophy in MS patients, independent of chronological age, sex, and disease duration [31]. In this study of over five hundred participants, telomere attrition explained 15% of variance of the effect of chronological age on disability [31]. Hecker et al. showed that shorter baseline LTL is associated with a higher conversion rate to SPMS after 10 years [46]. Habib et al. observed shorter LTL in patients with MS compared to controls. In patients with MS, LTL was shorter in patients with progressive MS compared to RRMS [45]. Redondo et al. demonstrated accelerated telomere shortening in bone marrow mesenchymal stromal cells of MS patients relative to healthy controls [47]. These findings suggest biological aging contributes to disability progression, brain atrophy, and cellular aging in MS. Chronic inflammation in MS may lead to increased oxidative damage and lymphocyte turnover, causing premature cellular senescence in lymphocytes and other neighboring cells.
Other biomarkers of biological aging include epigenetic clocks based on DNA methylation (DNAm) patterns. These clocks have been shown to estimate accelerated biological aging in a variety of disease states [48]. Levine et al. demonstrated an association between accelerated DNAm age and both cognitive decline and neuropathologic biomarkers in Alzheimer’s disease [49]. Shireby et al. developed a DNAm clock specifically calibrated to human cortical tissue, which outperformed DNAm clocks developed for other tissues [48]. Kular et al. used Shireby’s cortical clock to demonstrate increased epigenetic age acceleration in the glial cells of MS patients compared to controls [50]. Maltby et al. recently demonstrated advanced epigenetic age (“GrimAge”) in B cells of participants with MS [51•]. While both LTL and epigenetic clocks assess biological age, there is only modest correlation between the two methods suggesting a benefit in combining these methods [52, 53].
Another approach to measuring biological age is to use multi-organ system indices. These may be more robust than single biomarker markers to capture an organism’s overall susceptibility to the deleterious effects of aging. Miner et al. reported accelerated biological aging in MS participants compared to controls using the NHANES Biological Age Index [54•]. This index uses readily available clinical values such as blood pressure and creatinine to estimate biologic age. It has been shown to accurately predict mortality and risk of cardiovascular disease [54•].
Senescent cells in multiple sclerosis
Age-related immune dysfunction, referred to as immunesenescence, is characterized by the impaired ability to respond to novel antigens and chronic low-grade inflammation [55]. Age-related changes in adaptive immunity are characterized by decreased peripheral naïve T cells, increased terminally differentiated memory T cells, senescent B cells and the development of the senescence-associated secretory phenotype (SASP) in lymphocytes and myelocytes. As individuals age, repeated antigenic exposures cause peripheral naïve T cell activation, replication, and eventual terminal differentiation into effector memory T cells [55]. This gradually depletes the reserve of peripheral naïve T lymphocytes and reduces an individual’s ability to respond to novel antigens such as new infections or vaccinations [55].
Terminally differentiated effector memory T cells take on a senescent phenotype, losing their costimulatory CD28 molecule, and expressing a variety of soluble and insoluble senescence markers including CD27, CD57, KLRG1, and granzyme K [55, 56]. Senescent T cells are proinflammatory, fill up immunologic space, and are less responsive to regulatory mechanisms [57]. Immunologic senescence has been reported to occur earlier in individuals with MS compared to controls, which may be due to increased antigenic stimulation in the setting of chronic inflammation [58]. Thewissen et al. demonstrated decreased T cell receptor excision circles (TRECs), a measure of thymic function, in MS patients relative to controls, suggesting premature thymic involution [57, 59]. Thewissen et al. also found higher levels of senescent CD4 + CD28(null) T cells in patients with MS compared to controls [57, 59]. Claes et al. found increased senescent B cells, expressing IgD-CD27(null) and CD21(null)CD11c + , in MS patients compared to controls [60]. Senescent B cells contribute to inflammation by activating T cells and producing proinflammatory cytokines [60].
Microglia are the primary innate immune cells of the central nervous system and play an integral role in immune surveillance, coordinating immune responses, and clearing debris [61]. As individuals age, their microglia undergo senescence, wherein they develop dysmorphic features, impaired mobility, impaired phagocytic capacity, and a proinflammatory phenotype [62,63,64]. Matsudaira et al. demonstrated that microglia expressing the senescent marker p16INK4a accumulate in the brains of old mice [65•]. Furthermore, this marker was associated with disease-associated microglia (DAM), a subset of microglia expressing characteristic transcriptional signatures found in the brains of the elderly or individuals with neurodegenerative disease [65•]. As microglia enter senescence, their ability to travel to sites of injury and phagocytose debris becomes impaired, which impedes the repair of damaged tissues in the central nervous system [62, 63]. Additionally, aged microglia develop a proinflammatory phenotype, expressing certain surface molecules (MHC II, CD11b, CD68, and CD86) and increased production of mRNA coding for proinflammatory cytokines (TNFa, IL-1B, and IL-6) [64]. This inflammatory phenotype results in more aggressive, protracted inflammatory responses to antigenic stimulation [64]. Together, these senescent changes contribute to an environment of chronic inflammation and impaired healing.
Age-related failure of remyelination in multiple sclerosis
Demyelinated axons can be repaired through the spontaneous regenerative process of remyelination, which restores function and preserves axonal integrity [66]. Remyelination can be driven by both surviving, mature oligodendrocytes and new oligodendrocytes derived from oligodendrocyte progenitor cells (OPCs) [67]. Remyelination slows as individuals age leaving more axons demyelinated and increasingly vulnerable to degeneration [68, 69]. Animal studies suggest age-related remyelination failure is related to impaired activation, recruitment, and differentiation of OPCs [66, 70]. In animal models, aged OPCs are unresponsive to pro-differentiation signals and fail to differentiate into mature oligodendrocytes preventing remyelination [71]. Differentiation may be impaired by inhibition from soluble factors related to chronic inflammation and/or age-related loss of regenerative potential in OPCs (Fig. 1) [66, 70,71,72]. Willis et al. demonstrated that extracellular vesicles (EVs) from astrocytes helped support oligodendrocyte differentiation and that this benefit was lost as astrocytes aged and developed a pro-inflammatory, senescence-like phenotype (Fig. 1) [73•]. Senescent astrocytes also impact synaptic plasticity, metabolic homeostasis and blood brain barrier permeability, further impacting neuronal recovery and function [74].
Age-related remyelination impairment has been implicated in the transition from relapsing to progressive MS. Remyelination occurs more frequently at younger ages and earlier in the disease course and wanes over time [75]. Hess et al. identified remyelination in 40% of acute MS plaques, while 89% of smoldering plaques had no evidence of remyelination [72]. Hess et al. demonstrated that supernatant from activated microglia prevented terminal differentiation of pluripotent stem cell derived oligodendrocytes, suggesting chronic inflammation driven by microglia may contribute to preventing remyelination [72].
Damage from cellular aging appears to be reversible. OPC differentiation capacity in aged OPCs have been restored with treatment using fasting-mimetic metformin [71], increased expression of transcription factor c-MyC [76], increased expression of retinoid X receptor gamma (RXR-γ) [77], and other biologically and synthetically produced environments [78]. These studies suggest that nutrient regulation, signaling pathways, and biomechanical structure contribute to rejuvenating remyelination processes. As such, cell therapies could pose a promising treatment to MS lesions, as regulation of these rejuvenating factors could restore OPCs, even if transplanted cells are aged. In addition to restoring OPC proliferation and differentiation into remyelinating oligodendrocytes, alternative treatments could reverse age-related effects of microglial-macrophage populations that regulate lesion environments [79,80,81].
Reproductive aging in multiple sclerosis
In addition to somatic aging, reproductive aging may influence MS phenotype. Sex hormones have widespread effects on many biologic systems including the immune and nervous systems. In animal models, sex hormones have both anti-inflammatory and neuroprotective effects [82]. In both males and females, the production of sex hormones declines over time [83]. This change may drive changes in MS disease expression over the lifespan.
MS most commonly occurs in young adulthood where the female to male ratio is 3:1. Before puberty and after menopause the sex ratio is closer to 1:1, suggesting the importance of the two reproductive milestones in defining the lifespan period of sex dimorphism in MS [83]. Animal models suggest the sex differences observed in MS incidence are due to intrinsic sex differences in biology rather than gender based environmental factors [71]. Borziak et al. recently described 20 X-linked single nucleotide polymorphisms (SNP) involved in immunity and myelination function which were more common in individuals with MS [84•]. The decreased MS prevalence in males may be related to protective effects from testosterone, however males tend to have more severe progression at younger ages. Females catch up to males in terms of disability progression after menopause. The mean age of onset of progressive MS is around 45, which aligns with perimenopause in women [83].
Estrogen has a dose dependent effect where it stimulates the immune system at the lower levels seen in menstrual cycling and suppresses the immune system at the higher levels observed in pregnancy [85, 86]. This correlates with the observations that earlier age of menarche is associated with increased risk of MS, while pregnancy has been shown to be associated with a decreased risk of MS in a “dose dependent” fashion [87]. In patients with MS, pregnancy is associated with a reduced risk of relapse, while this risk transiently increases postpartum [83].
Perimenopause is a prolonged and critical biological transition period associated with a decline in female sex steroid hormones. Bove et al. and Baroncini et al. separately demonstrated an accelerated functional decline following the perimenopausal-menopausal transition [88, 89]. Zeydan et al. found that premature/early menopause was associated with earlier onset of progressive MS [90]. Graves et al. demonstrated that AMH levels, as a sensitive marker of ovarian aging, were associated with significant increases in disability and gray matter atrophy, even with adjustment for chronological age, BMI, and disease duration for women with MS [91]. These studies suggest a relationship between sex hormone concentrations and disease phenotype, and a particular link between the decline in female sex hormones and progressive disease.
Age-related comorbidities in patients with multiple sclerosis
Advancing biological age also increases the risk of comorbid illnesses in patients with MS. Vascular comorbidities are associated with faster time to needing to walk with a cane [92]. Obesity and hyperlipidemia are also associated with increased disability and relapse rate in individuals with MS [93, 94]. The risk of MS disability progression is increased greater than 200% in individuals with 2 or more comorbidities [92].
Several studies have found a higher prevalence of hypertension, hyperlipidemia, and cardiovascular disease in individuals with MS compared to the general population [95, 96]. One study found a 1.5-fold increase in cardiovascular mortality in individuals with MS [96]. On autopsy there is increased cerebral small vessel disease in individuals with MS compared to age matched controls [97]. The exact reason for these differences is unclear and is likely multifactorial. Disability frequently limits an individual’s ability to exercise, contributing to weight gain and metabolic dysfunction. Altered immune function and accelerated biologic aging in individuals with MS may also contribute [95]. In conditions like rheumatoid arthritis and psoriasis, the risk of vascular disease is not fully explained by traditional cardiovascular risk factors and is hypothesized to be driven by inflammatory activity [95].
Comorbidities can increase risk of side effects with disease modifying therapies, another complication arising in those aging with MS. Uncontrolled hypertension may preclude the use of teriflunomide or sphingosine-1-phosphate receptor modulators, both of which can cause hypertension [98] Diabetic retinopathy may increase the risk of macular edema in patients using sphingosine-1-phosphate receptor modulators [98]. The risk of malignancy increases with age and may be increased by immunosuppressants. Several DMTs have been associated with malignancy [99]. One study found increased cancer incidence among MS patients in the treatment era compared to the pre-treatment era [100]. Given the potential for increased malignancy risk, it is important that MS patients are regularly screened for cancer. Unfortunately, Groome et al. found that MS patients were less likely to have cancer detected by routine screening due to missed routine screening because of MS related disability [101].
Clinical management of aging individuals with multiple sclerosis
Aging and immunosenescence result in increased infection risk and waning efficacy from currently available disease modifying therapies (DMTs). Most DMT trials specifically exclude individuals over 60 years and use the number of relapses and/or new lesions as primary outcomes. This has resulted in DMTs that are effective in preventing relapses in younger individuals, but which have less robust efficacy in treating older individuals with progressive MS. [18, 21, 102, 103]. The exclusion of older individuals from clinical trials limits our ability to apply these data to this population and highlights the need for further studies addressing treatment in this population.
At the time of writing this article there are over 20 DMTs indicated to treat relapsing forms of MS, including active secondary progressive MS. Most of these medications have been shown to reduce disability progression in the younger, relapsing populations in which they were studied. Currently, only anti-CD20 therapies (e.g., ocrelizumab) are FDA approved to treat primary progressive MS [90]. Despite having a few DMTs demonstrating efficacy in progressive forms of MS, these effects are primarily demonstrated in younger individuals with active progressive disease manifesting with either enhancing MRI lesions or clinical relapses [98, 102, 104]. The ORATORIO and EXPAND studies showed less efficacy on disability progression in patients over 45 years taking ocrelizumab or siponimod, respectively [102, 103]. The OLYMPUS study showed no benefit from rituximab in patients > 51 years without gadolinium enhancing lesions [105]. A Swedish national post-marketing surveillance study of natalizumab showed no significant change in EDSS in individuals > 50 years [106].
Safety is a major concern when using DMTs in older adults with MS. Immunosenescence results in impaired adaptive immunity, increasing susceptibility to infection and reducing the effectiveness of vaccines [55]. Most DMTs suppress the immune system and increase the risk for infection. Most MS clinical trials have not enrolled individuals > 55 years which limits the ability to apply available safety data to this population. One study looking at infection-related healthcare utilization in individuals with MS found increased risk of infection in all age groups compared to the general population. The increased risk of infection was higher in individuals > 60 years (2.7-fold) compared to < 40 years (1.5-fold) [107]. Specific age-related infection concerns include increased John Cunningham virus (human polyomavirus 2) seroconversion and VZV reactivation. In addition to the increased infection risk, older individuals have more medical comorbidities which may put them at greater risk of other medication side effects as detailed above.
Given the increasing risks and waning benefits associated with DMT use in advancing chronologic age, there is a need for evidence based DMT discontinuation guidelines. Several studies have sought to answer this question, but most data are observational. Yano et al. found no significant difference in time to next clinical or radiologic event in patients who discontinued DMT after 2 years of stability compared to patients who remained on DMT [108]. They noted a significant difference in time to disease activity between patients > 45 years compared to patients < 45 years [108]. Hua et al. found that most individuals over 60 years who discontinued DMTs after a period of stability remained off DMTs without relapse [109]. Coever et al. found that older age at time of DMT discontinuation was associated with less clinical or MRI activity, reporting recurrent disease activity in 25.3% of patients > 55 years, compared to 82.4% of patients < 45 years of age [110]. While these studies suggest it may be safe to discontinue DMTs in older patients, they are limited by their observational designs. DISCOMS was a recently published randomized, controlled, non-inferiority trial investigating DMT continuation vs discontinuation in MS patients > 55 years. Relapse or new expanding brain lesion occurred in 4.7% of patients on DMT compared to 12.2% of patients who discontinued DMT. The authors were unable to conclude that discontinuing DMT was non-inferior to continuation [111•]. Importantly, clinical events were low in both groups with no significant difference in relapse or progression. Instead, most primary events were MRI lesions of uncertain clinical relevance [111•]. Together, these studies suggest that DMTs can be safely discontinued in most older individuals, however, there are exceptions and the decision to do so still has to be made on a case-by-case basis. The measurement of biological age may in the future aid in this decision-making. Two other randomized controlled trials are underway in France (NCT03653273) and the Netherlands (NCT04260711), which will hopefully provide additional guidance on discontinuing DMT [111•].
Conclusions
As individuals with MS age, their clinical phenotype and the pathophysiology that underlies it change. Initially the disease is characterized by frequent, highly inflammatory relapses, which gradually become less frequent, and ultimately give way to progressive, relapse-independent disability accumulation. The change in clinical phenotype is driven by fundamental shifts in the underlying pathophysiology. from highly active inflammatory lesions driven by peripheral lymphocytes to chronic slowly expanding lesions driven by activated microglia. This change marks a shift from the adaptive immune system to the innate immune system. Cellular senescence in the immune and central nervous system also contributes to changes in pathophysiology and treatment responses. Current treatment strategies are effective in preventing relapses but are less effective in preventing progressive disease. This likely reflects the fact that current treatments target the adaptive immune response but are less effective in altering innate immunity. In addition, older individuals have different comorbidities and are at higher risk of infection, which needs to be taken into consideration when making treatment diseases. Understanding the clinical and pathologic changes that occur as individuals with MS age is critical to providing care and developing future treatments. Chronologic or biologic age needs to be more specifically considered when designing clinical trials, and older individuals need to be increasingly included in future trials.
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ropper AH, Samuels MA, Klein J. Adams and Victor’s principles of neurology. Eleventh. New York: McGraw-Hill Education; 2019.
Wallin MT, et al. The prevalence of MS in the United States: A population-based estimate using health claims data. Neurol. 2019;92(10):e1029–40. https://doi.org/10.1212/WNL.0000000000007035.
Kuhlmann T, et al. Multiple sclerosis progression: time for a new mechanism-driven framework. Lancet Neurol. 2023;22(1):78–88. https://doi.org/10.1016/S1474-4422(22)00289-7.
Stankoff B, et al. Age at onset determines the occurrence of the progressive phase of multiple sclerosis. Neurol. 2007;68(10):779–81. https://doi.org/10.1212/01.wnl.0000256732.36565.4a.
M. P. Gorman, B. C. Healy, M. Polgar-Turcsanyi, and T. Chitnis, “Increased Relapse Rate in Pediatric-Onset Compared With Adult-Onset Multiple Sclerosis,” Arch. Neurol., vol. 66, no. 1, 2009, https://doi.org/10.1001/archneurol.2008.505.
Scalfari A, Neuhaus A, Daumer M, Ebers GC, Muraro PA. Age and disability accumulation in multiple sclerosis. Neurology. 2011;77(13):1246–52. https://doi.org/10.1212/WNL.0b013e318230a17d.
Harding KE, et al. Long-term outcome of paediatric-onset multiple sclerosis: a population-based study. J Neurol Neurosurg Psychiatry. 2013;84(2):141–7. https://doi.org/10.1136/jnnp-2012-303996.
Tutuncu M, et al. Onset of progressive phase is an age-dependent clinical milestone in multiple sclerosis. Mult Scler J. 2013;19(2):188–98. https://doi.org/10.1177/1352458512451510.
E. Waubant et al., “Difference in Disease Burden and Activity in Pediatric Patients on Brain Magnetic Resonance Imaging at Time of Multiple Sclerosis Onset vs Adults,” Arch Neurol., vol. 66, no. 8, 2009, https://doi.org/10.1001/archneurol.2009.135.
Pfeifenbring S, et al. Extensive acute axonal damage in pediatric multiple sclerosis lesions. Ann Neurol. 2015;77(4):655–67. https://doi.org/10.1002/ana.24364.
Tremlett H, Zhao Y, Joseph J, Devonshire V, the UBCMS Clinic Neurologists. 2“Relapses in multiple sclerosis are age- and time-dependent.” J Neurol Neurosurg Psychiatry. 2008;79(12):1368–74. https://doi.org/10.1136/jnnp.2008.14580.
Lucchinetti C, Bruck W, Parisi J, Scheithauer B, Rodriguez M, Lassmann H. Heterogeneity of multiple sclerosis lesions: Implications for the pathogenesis of demyelination. Ann Neurol. 2000;47(6):707–17. https://doi.org/10.1002/1531-8249(200006)47:6%3c707::AID-ANA3%3e3.0.CO;2-Q.
Frischer JM, et al. Clinical and pathological insights into the dynamic nature of the white matter multiple sclerosis plaque. Ann Neurol. 2015;78(5):710–21. https://doi.org/10.1002/ana.24497.
Jäckle K, et al. Molecular signature of slowly expanding lesions in progressive multiple sclerosis. Brain. 2020;143(7):2073–88. https://doi.org/10.1093/brain/awaa158.
• M. Absinta et al., “A lymphocyte–microglia–astrocyte axis in chronic active multiple sclerosis,” Nature, vol. 597, no. 7878, pp. 709–714, 2021https://doi.org/10.1038/s41586-021-03892-7This study describes a genetic profile of disease associated microglia in MS.
Nicaise AM, et al. Cellular senescence in progenitor cells contributes to diminished remyelination potential in progressive multiple sclerosis. Proc Natl Acad Sci. 2019;116(18):9030–9. https://doi.org/10.1073/pnas.1818348116.
• A. Calvi et al., “Relationship between paramagnetic rim lesions and slowly expanding lesions in multiple sclerosis,” Mult Scler J., vol. 29, no. 3, pp. 352–362, Mar. 2023https://doi.org/10.1177/13524585221141964This study describes paramagnetic rim and slowly expanding lesions in multiple sclerosis and reports association with progression.•
Elliott C, et al. Chronic white matter lesion activity predicts clinical progression in primary progressive multiple sclerosis. Brain. 2019;142(9):2787–99. https://doi.org/10.1093/brain/awz212.
P. Maggi et al., “Chronic White Matter Inflammation and Serum Neurofilament Levels in Multiple Sclerosis,” Neurology, vol. 97, no. 6, 2021, https://doi.org/10.1212/WNL.0000000000012326.
Absinta M, et al. Association of Chronic Active Multiple Sclerosis Lesions With Disability In Vivo. JAMA Neurol. 2019;76(12):1474. https://doi.org/10.1001/jamaneurol.2019.2399.
Absinta M, et al. Persistent 7-tesla phase rim predicts poor outcome in new multiple sclerosis patient lesions. J Clin Invest. 2016;126(7):2597–609. https://doi.org/10.1172/JCI86198.
Vollmer T, et al. The natural history of brain volume loss among patients with multiple sclerosis: A systematic literature review and meta-analysis. J Neurol Sci. 2015;357(1–2):8–18. https://doi.org/10.1016/j.jns.2015.07.014.
Azevedo CJ, Cen SY, Jaberzadeh A, Zheng L, Hauser SL, Pelletier D. Contribution of normal aging to brain atrophy in MS. Neurol Neuroimmunol Neuroinflammation. 2019;6(6): e616. https://doi.org/10.1212/NXI.0000000000000616.
Zhang J, et al. Gray matter atrophy cannot be fully explained by white matter damage in patients with MS. Mult Scler J. 2021;27(1):39–51. https://doi.org/10.1177/1352458519900972.
M. A. Rocca et al., “Association of Gray Matter Atrophy Patterns With Clinical Phenotype and Progression in Multiple Sclerosis,” Neurology, vol. 96, no. 11, 2021, https://doi.org/10.1212/WNL.0000000000011494.
Bø L, Vedeler CA, Nyland HI, Trapp BD, Mørk SJ. Subpial Demyelination in the Cerebral Cortex of Multiple Sclerosis Patients. J Neuropathol Exp Neurol. 2003;62(7):723–32. https://doi.org/10.1093/jnen/62.7.723.
Bell L, Lenhart A, Rosenwald A, Monoranu CM, Berberich-Siebelt F. Lymphoid Aggregates in the CNS of Progressive Multiple Sclerosis Patients Lack Regulatory T Cells. Front Immunol. 2020;10:3090. https://doi.org/10.3389/fimmu.2019.03090.
Van Olst L, et al. Meningeal inflammation in multiple sclerosis induces phenotypic changes in cortical microglia that differentially associate with neurodegeneration. Acta Neuropathol (Berl). 2021;141(6):881–99. https://doi.org/10.1007/s00401-021-02293-4.
Levine ME. Modeling the Rate of Senescence: Can Estimated Biological Age Predict Mortality More Accurately Than Chronological Age? J Gerontol A Biol Sci Med Sci. 2013;68(6):667–74. https://doi.org/10.1093/gerona/gls233.
Blackburn EH, Epel ES, Lin J. Human telomere biology: A contributory and interactive factor in aging, disease risks, and protection. Science. 2015;350(6265):1193–8. https://doi.org/10.1126/science.aab3389.
Krysko KM, et al. Telomere Length Is Associated with Disability Progression in Multiple Sclerosis. Ann Neurol. 2019;86(5):671–82. https://doi.org/10.1002/ana.25592.
Musella A, et al. Interplay Between Age and Neuroinflammation in Multiple Sclerosis: Effects on Motor and Cognitive Functions. Front Aging Neurosci. 2018;10:238. https://doi.org/10.3389/fnagi.2018.00238.
R. G. Morgan, A. J. Donato, and A. E. Walker, “Telomere uncapping and vascular aging,” Am J Physiol-Heart Circ Physiol., vol. 315, no. 1, pp. H1–H5, 2018, https://doi.org/10.1152/ajpheart.00008.2018.
M. A. Giardini, M. Segatto, M. S. Da Silva, V. S. Nunes, and M. I. N. Cano, “Telomere and Telomerase Biology,” in Progress in Molecular Biology and Translational Science, vol. 125, Elsevier, 2014, pp. 1–40. https://doi.org/10.1016/B978-0-12-397898-1.00001-3.
Goglin SE, Farzaneh-Far R, Epel ES, Lin J, Blackburn EH, Whooley MA. Change in Leukocyte Telomere Length Predicts Mortality in Patients with Stable Coronary Heart Disease from the Heart and Soul Study. PLoS ONE. 2016;11(10): e0160748. https://doi.org/10.1371/journal.pone.0160748.
Willeit P, et al. Cellular Aging Reflected by Leukocyte Telomere Length Predicts Advanced Atherosclerosis and Cardiovascular Disease Risk. Arterioscler Thromb Vasc Biol. 2010;30(8):1649–56. https://doi.org/10.1161/ATVBAHA.110.205492.
Topiwala A, et al. Alcohol consumption and telomere length: Mendelian randomization clarifies alcohol’s effects. Mol Psychiatry. 2022;27(10):4001–8. https://doi.org/10.1038/s41380-022-01690-9.
Galiè S, Canudas S, Muralidharan J, García-Gavilán J, Bulló M, Salas-Salvadó J. Impact of Nutrition on Telomere Health: Systematic Review of Observational Cohort Studies and Randomized Clinical Trials. Adv Nutr. 2020;11(3):576–601. https://doi.org/10.1093/advances/nmz107.
Song S, Lee E, Kim H. Does Exercise Affect Telomere Length? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Medicina (Mex). 2022;58(2):242. https://doi.org/10.3390/medicina58020242.
Khosravaniardakani S, et al. Obesity Accelerates Leukocyte Telomere Length Shortening in Apparently Healthy Adults: A Meta-Analysis. Front Nutr. 2022;9: 812846. https://doi.org/10.3389/fnut.2022.812846.
Astuti Y, Wardhana A, Watkins J, Wulaningsih W. Cigarette smoking and telomere length: A systematic review of 84 studies and meta-analysis. Environ Res. 2017;158:480–9. https://doi.org/10.1016/j.envres.2017.06.038.
Gardner M, et al. Gender and telomere length: Systematic review and meta-analysis. Exp Gerontol. 2014;51:15–27. https://doi.org/10.1016/j.exger.2013.12.004.
Needham BL, Salerno S, Roberts E, Boss J, Allgood KL, Mukherjee B. Do black/white differences in telomere length depend on socioeconomic status? Biodemography Soc Biol. 2020;65(4):287–312. https://doi.org/10.1080/19485565.2020.1765734.
Benetos A, Aviv A. Ancestry, Telomere Length, and Atherosclerosis Risk. Circ Cardiovasc Genet. 2017;10(3): e001718. https://doi.org/10.1161/CIRCGENETICS.117.001718.
Habib R, Ocklenburg S, Hoffjan S, Haghikia A, Epplen JT, Arning L. Association between shorter leukocyte telomeres and multiple sclerosis. J Neuroimmunol. 2020;341: 577187. https://doi.org/10.1016/j.jneuroim.2020.577187.
Hecker M, et al. Leukocyte Telomere Length in Patients with Multiple Sclerosis and Its Association with Clinical Phenotypes. Mol Neurobiol. 2021;58(6):2886–96. https://doi.org/10.1007/s12035-021-02315-y.
Redondo J, et al. Reduced cellularity of bone marrow in multiple sclerosis with decreased MSC expansion potential and premature ageing in vitro. Mult Scler J. 2018;24(7):919–31. https://doi.org/10.1177/1352458517711276.
Shireby GL, et al. Recalibrating the epigenetic clock: implications for assessing biological age in the human cortex. Brain. 2020;143(12):3763–75. https://doi.org/10.1093/brain/awaa334.
Levine ME, Lu AT, Bennett DA, Horvath S. Epigenetic age of the pre-frontal cortex is associated with neuritic plaques, amyloid load, and Alzheimer’s disease related cognitive functioning. Aging. 2015;7(12):1198–211. https://doi.org/10.18632/aging.100864.
Kular L, et al. Epigenetic clock indicates accelerated aging in glial cells of progressive multiple sclerosis patients. Front Aging Neurosci. 2022;14: 926468. https://doi.org/10.3389/fnagi.2022.926468.
• V. Maltby et al., “Evaluation of Cell-Specific Epigenetic Age Acceleration in People With Multiple Sclerosis,” Neurology, vol. 101, no. 7, 2023, https://doi.org/10.1212/WNL.0000000000207489. This study describes accelerated epigenetic aging within B cells in MS.
Pearce EE, et al. Telomere length and epigenetic clocks as markers of cellular aging: a comparative study. GeroScience. 2022;44(3):1861–9. https://doi.org/10.1007/s11357-022-00586-4.
Marioni RE, et al. The epigenetic clock and telomere length are independently associated with chronological age and mortality. Int J Epidemiol. 2016;45(2):424–32. https://doi.org/10.1093/ije/dyw041.
• A. E. Miner, J. H. Yang, R. P. Kinkel, and J. S. Graves, “The NHANES Biological Age Index demonstrates accelerated aging in MS patients,” Mult Scler Relat Disord., vol. 77, p. 104859, 2023 https://doi.org/10.1016/j.msard.2023.104859This study uses biologic aging index utilizing common laboratory findings to show accelerated aging in MS patients.•
Aiello A, et al. Immunosenescence and Its Hallmarks: How to Oppose Aging Strategically? A Review of Potential Options for Therapeutic Intervention. Front Immunol. 2019;10:2247. https://doi.org/10.3389/fimmu.2019.02247.
Mogilenko DA, et al. Comprehensive Profiling of an Aging Immune System Reveals Clonal GZMK+ CD8+ T Cells as Conserved Hallmark of Inflammaging. Immunity. 2021;54(1):99-115.e12. https://doi.org/10.1016/j.immuni.2020.11.005.
Thewissen M, et al. Analyses of immunosenescent markers in patients with autoimmune disease. Clin Immunol. 2007;123(2):209–18. https://doi.org/10.1016/j.clim.2007.01.005.
Eschborn M, et al. Evaluation of Age-Dependent Immune Signatures in Patients With Multiple Sclerosis. Neurol Neuroimmunol Neuroinflammation. 2021;8(6): e1094. https://doi.org/10.1212/NXI.0000000000001094.
Thewissen M, Linsen L, Somers V, Geusens P, Raus J, Stinissen P. Premature Immunosenescence in Rheumatoid Arthritis and Multiple Sclerosis Patients. Ann N Y Acad Sci. 2005;1051(1):255–62. https://doi.org/10.1196/annals.1361.066.
Claes N, et al. Age-Associated B Cells with Proinflammatory Characteristics Are Expanded in a Proportion of Multiple Sclerosis Patients. J Immunol. 2016;197(12):4576–83. https://doi.org/10.4049/jimmunol.1502448.
Greenwood EK, Brown DR. Senescent Microglia: The Key to the Ageing Brain? Int J Mol Sci. 2021;22(9):4402. https://doi.org/10.3390/ijms22094402.
Ng PY, McNeely TL, Baker DJ. Untangling senescent and damage-associated microglia in the aging and diseased brain. FEBS J. 2023;290(5):1326–39. https://doi.org/10.1111/febs.16315.
Oost W, Talma N, Meilof JF, Laman JD. Targeting senescence to delay progression of multiple sclerosis. J Mol Med. 2018;96(11):1153–66. https://doi.org/10.1007/s00109-018-1686-x.
Norden DM, Godbout JP. Review: Microglia of the aged brain: primed to be activated and resistant to regulation. Neuropathol Appl Neurobiol. 2013;39(1):19–34. https://doi.org/10.1111/j.1365-2990.2012.01306.x.
• T. Matsudaira et al., “Cellular senescence in white matter microglia is induced during ageing in mice and exacerbates the neuroinflammatory phenotype,” Commun Biol., vol. 6, no. 1, p. 665, 2023https://doi.org/10.1038/s42003-023-05027-2This study demonstrates cellular senescence in aging microglia and describes the association with disease associated microglia.•
Franklin RJM, ffrench-Constant C. Regenerating CNS myelin — from mechanisms to experimental medicines. Nat Rev Neurosci. 2017;18(12):753–69. https://doi.org/10.1038/nrn.2017.136.
Franklin RJM, Frisén J, Lyons DA. Revisiting remyelination: Towards a consensus on the regeneration of CNS myelin. Semin Cell Dev Biol. 2021;116:3–9. https://doi.org/10.1016/j.semcdb.2020.09.009.
Rist JM, Franklin RJM. Taking ageing into account in remyelination-based therapies for multiple sclerosis. J Neurol Sci. 2008;274(1–2):64–7. https://doi.org/10.1016/j.jns.2008.04.027.
Ruckh JM, et al. Rejuvenation of Regeneration in the Aging Central Nervous System. Cell Stem Cell. 2012;10(1):96–103. https://doi.org/10.1016/j.stem.2011.11.019.
Sim FJ, Zhao C, Penderis J, Franklin RJM. The Age-Related Decrease in CNS Remyelination Efficiency Is Attributable to an Impairment of Both Oligodendrocyte Progenitor Recruitment and Differentiation. J Neurosci. 2002;22(7):2451–9. https://doi.org/10.1523/JNEUROSCI.22-07-02451.2002.
Neumann B, et al. Metformin Restores CNS Remyelination Capacity by Rejuvenating Aged Stem Cells. Cell Stem Cell. 2019;25(4):473-485.e8. https://doi.org/10.1016/j.stem.2019.08.015.
Heß K, et al. Lesion stage-dependent causes for impaired remyelination in MS. Acta Neuropathol (Berl). 2020;140(3):359–75. https://doi.org/10.1007/s00401-020-02189-9.
• C. M. Willis et al., “Astrocyte Support for Oligodendrocyte Differentiation can be Conveyed via Extracellular Vesicles but Diminishes with Age,” Sci Rep., vol. 10, no. 1, p. 828, 2020https://doi.org/10.1038/s41598-020-57663-xThis study shows the importance of astrocyte support in oligodendrocyte differentiation and describes how this declines with age.•
J. Correale and M. F. Farez, “The Role of Astrocytes in Multiple Sclerosis Progression,” Front Neurol., vol. 6, 2015, https://doi.org/10.3389/fneur.2015.00180.
Goldschmidt T, Antel J, König FB, Brück W, Kuhlmann T. Remyelination capacity of the MS brain decreases with disease chronicity. Neurology. 2009;72(22):1914–21. https://doi.org/10.1212/WNL.0b013e3181a8260a.
Neumann B, et al. Myc determines the functional age state of oligodendrocyte progenitor cells. Nat Aging. 2021;1(9):826–37. https://doi.org/10.1038/s43587-021-00109-4.
Huang JK, et al. Retinoid X receptor gamma signaling accelerates CNS remyelination. Nat Neurosci. 2011;14(1):45–53. https://doi.org/10.1038/nn.2702.
Segel M, et al. Niche stiffness underlies the ageing of central nervous system progenitor cells. Nature. 2019;573(7772):130–4. https://doi.org/10.1038/s41586-019-1484-9.
Natrajan MS, et al. Retinoid X receptor activation reverses age-related deficiencies in myelin debris phagocytosis and remyelination. Brain. 2015;138(12):3581–97. https://doi.org/10.1093/brain/awv289.
Cantuti-Castelvetri L, et al. Defective cholesterol clearance limits remyelination in the aged central nervous system. Science. 2018;359(6376):684–8. https://doi.org/10.1126/science.aan4183.
Rawji KS, et al. Niacin-mediated rejuvenation of macrophage/microglia enhances remyelination of the aging central nervous system. Acta Neuropathol (Berl). 2020;139(5):893–909. https://doi.org/10.1007/s00401-020-02129-7.
Voskuhl RR, Palaszynski K. Sex Hormones in Experimental Autoimmune Encephalomyelitis: Implications for Multiple Sclerosis. Neuroscientist. 2001;7(3):258–70. https://doi.org/10.1177/107385840100700310.
Krysko KM, et al. Sex effects across the lifespan in women with multiple sclerosis. Ther Adv Neurol Disord. 2020;13:175628642093616. https://doi.org/10.1177/1756286420936166.
• K. Borziak and J. Finkelstein, “X-linked genetic risk factors that promote autoimmunity and dampen remyelination are associated with multiple sclerosis susceptibility,” Mult Scler Relat Disord., vol. 66, p. 104065, 2022https://doi.org/10.1016/j.msard.2022.104065This study describes sex linked immune genes that are associated with MS susceptibility.•
Correale J, Arias M, Gilmore W. Steroid hormone regulation of cytokine secretion by proteolipid protein-specific CD4+ T cell clones isolated from multiple sclerosis patients and normal control subjects. J Immunol Baltim Md 1950. 1998;161(7):3365–74.
Soldan SS, Retuerto AIA, Sicotte NL, Voskuhl RR. Immune Modulation in Multiple Sclerosis Patients Treated with the Pregnancy Hormone Estriol. J Immunol. 2003;171(11):6267–74. https://doi.org/10.4049/jimmunol.171.11.6267.
Magyari M. Role of socio-economic and reproductive factors in the risk of multiple sclerosis. Acta Neurol Scand. 2015;132:20–3. https://doi.org/10.1111/ane.12426.
Bove R, Healy BC, Musallam A, Glanz BI, De Jager PL, Chitnis T. Exploration of changes in disability after menopause in a longitudinal multiple sclerosis cohort. Mult Scler J. 2016;22(7):935–43. https://doi.org/10.1177/1352458515606211.
Baroncini D, et al. Impact of natural menopause on multiple sclerosis: a multicentre study. J Neurol Neurosurg Psychiatry. 2019;90(11):1201–6. https://doi.org/10.1136/jnnp-2019-320587.
Zeydan B, et al. Reproductive history and progressive multiple sclerosis risk in women. Brain Commun. 2020;2(2):fcaa185. https://doi.org/10.1093/braincomms/fcaa185.
J. S. Graves et al., “Ovarian aging is associated with gray matter volume and disability in women with MS,” Neurology, vol. 90, no. 3, 2018, https://doi.org/10.1212/WNL.0000000000004843.
Marrie RA, et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74(13):1041–7. https://doi.org/10.1212/WNL.0b013e3181d6b125.
Tettey P, et al. Frequency of Comorbidities and Their Association with Clinical Disability and Relapse in Multiple Sclerosis. Neuroepidemiology. 2016;46(2):106–13. https://doi.org/10.1159/000442203.
Kowalec K, et al. Comorbidity increases the risk of relapse in multiple sclerosis: A prospective study. Neurology. 2017;89(24):2455–61. https://doi.org/10.1212/WNL.0000000000004716.
Marrie RA, et al. A systematic review of the incidence and prevalence of comorbidity in multiple sclerosis: Overview. Mult Scler J. 2015;21(3):263–81. https://doi.org/10.1177/1352458514564491.
Palladino R, Marrie RA, Majeed A, Chataway J. Evaluating the Risk of Macrovascular Events and Mortality Among People With Multiple Sclerosis in England. JAMA Neurol. 2020;77(7):820. https://doi.org/10.1001/jamaneurol.2020.0664.
Geraldes R, et al. Distinct influence of different vascular risk factors on white matter brain lesions in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2020;91(4):388–91. https://doi.org/10.1136/jnnp-2019-322369.
Cross A, Riley C. Treatment of Multiple Sclerosis. Contin Lifelong Learn Neurol. 2022;28(4):1025–51. https://doi.org/10.1212/CON.0000000000001170.
Horton DB, Reder AT. Medications for Multiple Sclerosis and Risk of Malignancy: What Next? Neurotherapeutics. 2021;18(3):1650–3. https://doi.org/10.1007/s13311-021-01107-5.
Grytten N, et al. Incidence of cancer in multiple sclerosis before and after the treatment era– a registry- based cohort study. Mult Scler Relat Disord. 2021;55: 103209. https://doi.org/10.1016/j.msard.2021.103209.
P. A. Groome et al., “Multiple Sclerosis and the Cancer Diagnosis: Diagnostic Route, Cancer Stage, and the Diagnostic Interval in Breast and Colorectal Cancer,” Neurology, vol. 98, no. 18, 2022, https://doi.org/10.1212/WNL.0000000000200163.
Montalban X, et al. Ocrelizumab versus Placebo in Primary Progressive Multiple Sclerosis. N Engl J Med. 2017;376(3):209–20. https://doi.org/10.1056/NEJMoa1606468.
Kappos L, et al. Siponimod versus placebo in secondary progressive multiple sclerosis (EXPAND): a double-blind, randomised, phase 3 study. The Lancet. 2018;391(10127):1263–73. https://doi.org/10.1016/S0140-6736(18)30475-6.
Lublin FD, et al. Defining the clinical course of multiple sclerosis: The 2013 revisions. Neurology. 2014;83(3):278–86. https://doi.org/10.1212/WNL.0000000000000560.
Hawker K, et al. Rituximab in patients with primary progressive multiple sclerosis: Results of a randomized double-blind placebo-controlled multicenter trial. Ann Neurol. 2009;66(4):460–71. https://doi.org/10.1002/ana.21867.
Holmén C, et al. A Swedish national post-marketing surveillance study of natalizumab treatment in multiple sclerosis. Mult Scler J. 2011;17(6):708–19. https://doi.org/10.1177/1352458510394701.
Wijnands JM, et al. Infection-related health care utilization among people with and without multiple sclerosis. Mult Scler J. 2017;23(11):1506–16. https://doi.org/10.1177/1352458516681198.
Yano H, Gonzalez C, Healy BC, Glanz BI, Weiner HL, Chitnis T. Discontinuation of disease-modifying therapy for patients with relapsing-remitting multiple sclerosis: Effect on clinical and MRI outcomes. Mult Scler Relat Disord. 2019;35:119–27. https://doi.org/10.1016/j.msard.2019.07.021.
Hua LH, Fan TH, Conway D, Thompson N, Kinzy TG. Discontinuation of disease-modifying therapy in patients with multiple sclerosis over age 60. Mult Scler J. 2019;25(5):699–708. https://doi.org/10.1177/1352458518765656.
Coerver EME, et al. Discontinuation of first-line disease-modifying therapy in relapse onset multiple sclerosis. Mult Scler Relat Disord. 2023;74: 104706. https://doi.org/10.1016/j.msard.2023.104706.
• J. R. Corboy et al., “Risk of new disease activity in patients with multiple sclerosis who continue or discontinue disease-modifying therapies (DISCOMS): a multicentre, randomised, single-blind, phase 4, non-inferiority trial,” Lancet Neurol., vol. 22, no. 7, pp. 568–577,2023https://doi.org/10.1016/S1474-4422(23)00154-0This is the first randomized controlled trial assessing DMT discontinuation in MS patients over age 55.•
Funding
No authors received funding for the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
Christopher Goyne designed the review, performed literature searches, drafted the manuscript, critically edited, and approved and submitted the final draft of the manuscript. All other authors performed literature searches, drafted the manuscript, critically edited, and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
No authors had direct conflicts of interest with regard to the content of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Keypoints
• Chronologic age is one of the strongest predictors of MS disease phenotype.
• Older age is associated with less frequent MS relapses but also relapse free progression.
• MS pathophysiology changes over time, shifting from highly active inflammatory lesions driven by peripheral lymphocytes to chronic slowly expanding lesions characterized by activated microglia.
• Age can be measured chronologically or biologically by telomere length, epigenetic age, and with multi-organ system indices. Biologic age may be a more accurate representation of overall aging than chronological age.
• Biologic aging results in immunosenescence, which results in immune cells shifting to a chronic inflammatory phenotype and secreting pro-inflammatory molecules.
• Aging is associated with numerous other age-related conditions that affect disability progression in MS and treatment options.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Goyne, C.E., Fair, A.E., Sumowski, P.E. et al. The Impact of Aging on Multiple Sclerosis. Curr Neurol Neurosci Rep 24, 83–93 (2024). https://doi.org/10.1007/s11910-024-01333-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-024-01333-2