Abstract
Purpose of review
Small intestinal bacterial overgrowth (SIBO) is a chronic gastrointestinal disorder wherein excessive and abnormal growth of bacteria in the small bowel generally causes abdominal pain, bloating, and change in bowel habits. Our understanding of the underlying pathology and microbiome changes in SIBO has advanced greatly in the last 20 years in parallel with advances in treatment methods and diagnostics. Here, we review many of the latest findings that describe the pathophysiology of SIBO as well as its risk factors, clinical behavior, diagnosis, and management.
Recent findings
Studies have begun to employ advanced molecular assays to sequence the small bowel microbiome to reveal the changes evident in SIBO. An increase in the abundance of members of the Enterobacteriaceae is the main alteration to the gut microbiome that correlates with SIBO diagnosis and symptom severity, and enhancement of specific gas-producing pathways has been demonstrated in SIBO. Diagnostic methods continue to evolve with novel methods of small bowel aspiration and changes to interpretation of hydrogen breath tests. Elemental diets are the newest treatment modality that offer an exciting alternative to antibiotic therapy.
Summary
The study of SIBO provides valuable insights into the small bowel microbiome, particularly using molecular testing. Exciting changes to our understanding and treatment of SIBO are already in progress. Future work will be able to better elucidate not only the altered microbiology, but also its gold standard of diagnosis, treatment modalities, and secondary prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distribution and abundance of bacteria is quite variable in the gastrointestinal (GI) tract. There are 106 and 109 colony-forming units per milliliter (CFU/mL) of bacteria existing in the oral cavity and the colon respectively. In contrast, there are normally < 1000 and < 100 CFU/mL of bacteria residing in the small bowel and stomach, respectively [1]. Small intestinal bacterial overgrowth (SIBO) is a GI disorder characterized by excessive and abnormal growth of bacteria in the small bowel. It has generally been defined based on the culture of small bowel aspirates as the “gold standard” with greater than 103 CFU/mL as the most recent diagnostic threshold [2]. Though initially thought to only occur in patients with surgically altered enteric anatomy (e.g. Billroth 2 or Roux-en-Y gastric bypass (RYGB)), SIBO occurs frequently in nonsurgical patients with dysmotility and loss of inherent mechanisms of enteric antisepsis. The prevalence of SIBO is not well understood but it is known to be comorbid with many other diseases. Current tests to diagnose SIBO including breath testing and small bowel aspiration have strengths and limitations that require careful correlation to the pretest probability of the index clinical setting. Similarly, treatment of SIBO has evolved significantly in the last 20 years where induction of remission with antibiotics or elemental diet and maintenance of remission with promotility drugs, addressing the underlying modifying cause, or dietary modifications are the mainstays of management. The aim of this paper is to review the epidemiology, risk factors, pathophysiology, diagnosis, and management of SIBO. Discussion will be limited to SIBO; the related conditions of intestinal methanogen overgrowth and small intestinal fungal overgrowth will not be reviewed here.
Epidemiology
The prevalence of SIBO is not well-defined. This is in part due to variability in presenting symptoms and similarities to other conditions, but also due to variation in prevalence based on study population [3,4,5]. Prevalence estimates in asymptomatic subjects range from 0 to 35% depending on the type of breath test used for diagnosis [6]. Among patients referred for GI symptoms including those with irritable bowel syndrome (IBS), anywhere from 30 to 85% of patients had a positive breath test diagnostic of SIBO [6, 7]. A meta-analysis of patients that underwent RYGB suggested 29% of patients developed SIBO in the first 3 years after surgery, and 53% developed SIBO when tested more than 3 years after surgery [8]. With introduction of dedicated International Statistical Classification of Diseases-10 (ICD-10) codes by the National Center for Health Statistics division of Centers for Disease Control and Prevention (CDC) for SIBO (K82.11) in 2024, future epidemiologic studies will be able to assess the global and national prevalence/incidence of SIBO more accurately.
Risk Factors
For much of its history, altered bowel anatomy was the primary risk factor for the development of SIBO. The blind small bowel loop formed during bypass surgery was postulated to result in increased stasis and promote excessive growth of enteric bacteria. Other consequences of intra-abdominal surgery can also lead to development of SIBO, including postsurgical adhesions, ileocecal resection which results in backflow of colonic microbes into the small bowel, or anastomotic strictures. Dysmotility resulting in slow intestinal transit has more recently become its own independent risk factor for SIBO. Notably, adhesions can occur in the absence of prior surgery, most commonly in the setting of endometriosis, missed appendicitis or ovarian pathology [9]. This includes dysmotility related to autoimmune diseases such as systemic sclerosis and celiac disease, inflammatory conditions such as Crohn’s disease and radiation enteritis, use of opioids and anticholinergics, visceral neuropathies such as gastroparesis, and even autoimmune reactions directed towards the gut i.e. anti-vinculin antibodies seen in postinfectious IBS [10]. A 2015 study by Roland et al. gives credence to the association between dysmotility and SIBO by demonstrating significantly longer intestinal and small bowel transit times in SIBO patients compared to healthy controls undergoing wireless motility capsule testing [11]. Proton pump inhibitor (PPI) therapy has some evidence to support it as a risk factor, but strength of association and evidence is inconsistent due to variations in testing methods [12, 13]. A recent study of sterile-collection duodenal aspirates showed no association between PPI use and SIBO via 16S ribosomal ribonucleic acid (rRNA) sequencing though fecal samples did have an increased relative abundance (RA) of oral organisms [14]. Liver disease, celiac disease, autoimmune gastritis, Parkinson’s disease, and chronic pancreatitis also have known associations with incidence of SIBO [6, 10]. Table 1 summarizes diseases that can lead to SIBO and the fundamentals of their treatment.
Pathophysiology
Patients with culture proven SIBO demonstrate significant alterations in the gut microbiome. Recent works by Leite et al. reveal significant decreases in the overall diversity of the gut microbiome in patients with SIBO when sterile catheter collected duodenal aspirates were examined using 16S rRNA sequencing and metagenomic shotgun sequencing [15]. Patients with culture positive SIBO were found to have decreased alpha-diversity and decreased beta-diversity, the latter of which was more prominent in samples that grew ≥ 105 CFU/mL compared to those growing ≥ 103 to < 105 CFU/mL. Patients with SIBO had a higher abundance of anaerobes, with predominance of the phylum Proteobacteria and a decreased abundance of Firmicutes. This was an inversion of the findings in healthy controls, who had a much higher predominance of Firmicutes to the point that the ratio of Proteobacteria to Firmicutes was diagnostic for SIBO with a cutoff of 0.39. Among class, there is an overrepresentation of Gammaproteobacteria and Deltaproteobacteria with an increase in Enterobacteriaceae being responsible for the increased presence of the former. The greater presence of Gammaproteobacteria was largely responsible for the increased RA of Proteobacteria. At the family level, Enterobacteriaceae, Aeromonadaceae, and Moraxellaceae had increased RA with the first family responsible for the vast majority of Gammaproteobacteria RA. At this level, family RA was able to correlate with symptoms. Increased RA of Enterobacteriaceae had a positive correlation specifically with bloating; increased RA of Aeromonadaceae was positively associated with stool urgency. At the level of genera, SIBO patients have a higher relative abundance of Klebsiella, Escherichia/Shigella, and Acinetobacter species.
Enterobacteriaceae have been of particular interest in SIBO as it possesses many disease-causing pathogens, including Escherichia coli, Enterococcus species, Klebsiella pneumoniae, and Proteus mirabilis, and its relevance is supported both by recent and older sequencing work [6]. Increases in RA of aerobes within the Enterobacteriaceae were negatively correlated with presence of strict anaerobes in duodenal aspirates as well as lower measures of microbial diversity in the same body of work by Leite et al.
Leite et al. also employed different sequencing methods to reveal metabolomic alterations in patients with SIBO consistent with some of its known diagnostic features. Pathways involved in gas production were upregulated in SIBO patients and correlated with more severe symptoms when analyzed via 16S rRNA sequencing and shotgun sequencing. Pyruvate fermentation, sulfate-reduction, and both aerobic and anaerobic respiratory pathways have all been shown to be enriched in the microbiome of SIBO patients. Increased sulfate reduction supports other data that have shown hydrogen sulfide (H2S) gas on lactulose breath testing was higher in individuals with higher RA of Fusobacterium and Desulfovibrio species, which are known to possess pathways specifically for the production of H2S.
Construction of microbial networks indicated that SIBO patients have significant disruption of their normal networks with dysconnectivity occurring in patients growing more than 103 CFU/mL.
Findings that members of the Enterobacteriaceae are vital drivers in the pathogenesis of SIBO are further supported by another study by Barlow and Leite et al., which sought to identify microbes that disrupted the normal bacterial communities and dominated over other taxa when present [16]. These “disruptor taxa” were aerobes from the Enterobacteriaceae, such as Klebsiella, Escherichia, Enterococcus, and Clostridium, and their abundance resulted in a paucity of strict anaerobes that are normally found in high numbers in the duodenal microbiome. The increase in microbes belonging to Enterobacteriaceae, Escherichia, and Clostridium was more strongly associated with SIBO than microbial load, suggesting that overgrowth of these groups may be more responsible for causing disease than increased microbial load of other microbes.
Other studies have used other means to assess the microbiome [17, 18]. Li et al. found decreased microbial diversity in cultured mucosal samples of the duodenum and ileum of SIBO patients via 16S rRNA sequencing, but no changes in diversity were identified in the fecal microbiome. Subjects without SIBO demonstrated enrichments in Lactobacillus, Prevotella, Bifidobacterium, Dialister, Ruminococcaceae, and Clostridium species in duodenal mucosa via differential expression analysis. Subjects with SIBO had enriched Absconditabacteriales in the duodenal mucosa. Ileal mucosa in subjects without SIBO showed enrichment of Lactobacillus, Prevotella, Clostridium, Klebsiella, and 9 other genera compared to enrichment of Ruminococcus, Enterococcus, Sutterella, Holdemanella, and Butyricimonas in SIBO subjects. It is important to note that ileal mucosal samples were obtained via colonoscopic approach; thus there is potential for contamination by large bowel microbes in this study.
Maslennikov et al. relied on 16S rRNA sequencing of stool samples in subjects with cirrhosis stratified based on a positive lactulose breath test. Fecal microbiome analysis presents some methodological problems in assessing SIBO given that fecal samples are populated by far higher concentrations of microbes than samples from the small bowel–a fold difference on the order of 109. In general, the large and small bowel are different microenvironments with different degrees of immune activity/presence, mucosal secretions, and nutrient substrates. Nevertheless, they found a higher abundance of Firmicutes and Fusobacteria plus lower abundance of Bacteroidetes in subjects with SIBO.
Ultimately, the decreases in microbial diversity and increased presence of pathogenic bacteria can contribute to the disease state by destruction of the intestinal barrier, increasing intestinal permeability, increased release of bacterial endotoxins, and translocation of colonic bacteria into the small bowel.
Clinical Presentation
The signs and symptoms of SIBO are very nonspecific. Typical symptoms include post-prandial bloating, excessive belching or flatulence, and change in bowel habits. Symptoms are typically chronic in nature, food related, and indolent in their onset. More severe cases can result in weight loss and steatorrhea as well as manifestations of malabsorption; for example, decreased absorption of vitamin D and B12 can result in fatigue, weakness, numbness, ataxia, and muscle cramps if disease progresses to causing symptomatic hypocalcemia or B12 deficiency. On physical exam, patients may only demonstrate abdominal distension or tympany in mild cases. Cases that develop micronutrient deficiencies due to SIBO can manifest with spastic weakness of the lower extremities, confusion, glossitis, tetany, and papilledema, but the frequency of these deficiencies and exam findings is not well-defined. Ultimately, physical exam findings are rarely present in SIBO and initiation of testing requires a high degree of suspicion. It is worth considering testing for SIBO in patients who express significant bloating or who have otherwise unexplained micronutrient deficiencies especially in the presence of risk factors for dysmotility.
Differential Diagnosis
SIBO has a broad differential diagnosis due to the vague nature of its signs and symptoms (Table 2). It is important to consider other causes of chronic diarrhea in the evaluation of SIBO [19]. Celiac disease can cause many similar symptoms and even result in steatorrhea and villous blunting. Crohn’s disease can similarly cause chronic diarrhea, though there may be exam findings more specific for Crohn’s disease depending on the case, such as perianal disease or cutaneous manifestations like pyoderma gangrenosum. Several infectious gastroenteritides can also cause similar symptoms, including giardiasis, cryptosporidiosis, and Whipple’s disease.
Diagnostic Testing
Testing for SIBO has changed significantly since its earlier descriptions. Currently, the “gold standard” relies on culturing duodenal aspirates on MacConkey agar with growth of more than 103 CFU/mL being the most agreed-upon threshold for diagnosis of SIBO [20]. While duodenal aspirate culture can yield antibiotic susceptibilities, it has several limitations to consider. Sampling protocols have not been fully standardized and validated, and small bowel aspirates are vulnerable to contamination by microbes from the upper airways, affecting as many as 20% of samples [21]. Small bowel aspirates are also costly and time-consuming, require patients to be exposed to the risks associated with esophagogastroduodenoscopy with anesthesia, and cannot sample the mid to distal small bowel in its routine form, thus potentially missing the diagnosis in patients with more distal SIBO. Recent work by Leite et al. has attempted to use a sterile double-lumen catheter for sample collection to reduce the possibility of contamination [15, 22]. Additionally, only a short segment of the small bowel is aspirated which may not necessarily represent the whole length of the small bowel, hence, the possibility of false negative results.
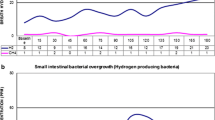
Hydrogen breath testing is the more practical and widely used method to diagnose SIBO, specifically after administration of a pre-defined oral load of glucose (GBT) or lactulose (LBT). In SIBO, administration of these sugars results in fermentation by gut microbes, releasing hydrogen gas that is absorbed into the bloodstream and released in the breath. Lactulose is expected to produce hydrogen in healthy individuals once reaching the cecum but causes an early rise in hydrogen in SIBO due to the more proximal presence of fermenting microbes. Glucose is expected to be completely absorbed before it reaches fermenting microbes with a significant rise at any time thought to be related to proximal migration of fermenting microbes. The LBT and GBT have been subjects of increased study in recent years, with differences in protocols for performing and interpreting the tests affecting accuracy. Depending on the trial, sensitivity and specificity vary as much as 20–93% and 30–86% for the GBT, 17–68% and 44–86% for the LBT [23]. The LBT and GBT are also prone to false positives (such as in patients with a history of foregut surgery, resulting in rapid transit) in as many as 20% of otherwise healthy subjects [24] and false negatives (such as in patients with more severe dysmotility causing delayed peaks in gases) [23, 25, 26]. It should be noted that sensitivity and specificity of breath testing is calculated by comparison to small bowel aspirate culture as the “gold standard”. However as mentioned above the test characteristics of small bowel aspirate culture with regular techniques are not optimal with known false positive and false negative results. Hence, calculation of sensitivity and specificity of breath testing based on cultures may not be appropriate.
The most recent consensus guidelines recommend a rise in hydrogen > 20 parts per million (ppm) above baseline within 90 min during LBT or an increase in hydrogen > 20 ppm above baseline during GBT. A recent study of the GBT comparing the 2017 North American Consensus protocol (cutoff > 20 ppm) to a cutoff > 12 ppm suggested the methodology of the latter may be more sensitive for detecting SIBO [25]. Elevated hydrogen at baseline > 20 ppm and a flatline pattern (non-methane and fixed-hydrogen production) are also considered abnormal and suggestive of SIBO [27].
Management
Optimal SIBO treatment requires treatment of the underlying or predisposing cause, induction of remission, and maintenance of remission. The underlying cause may not be apparent or modifiable (e.g. presence of blind loop), however when applicable, attempts should be made to remove or alleviate the cause of SIBO. Patients with opioid-related dysmotility, for example, should consider decreasing and even discontinuing opioids or starting a peripherally acting mu opioid receptor antagonist.
Induction of remission most often is achieved with antibiotics such as rifaximin. A 14-day course of rifaximin leads to resolution of symptoms in about 50% of patients [28, 29]. Recurrence after treatment with rifaximin is common, and patients are often treated with more than one course before finding durable symptom relief. Second-line antibiotics include trimethoprim-sulfamethoxazole, ciprofloxacin, amoxicillin-clavulanic acid, metronidazole, doxycycline, and tetracycline. There is a paucity of high-quality data evaluating their use compared to rifaximin. Those that do not respond adequately to antibiotics or unwilling to try antibiotics can also attempt treatment with an elemental diet, which has been shown to lead to symptom improvement and normalization of lactulose hydrogen breath tests in SIBO patients after a 2- to 3-week course [10, 30]. A recent clinical trial with a 2-week course of exclusive novel palatable elemental diet (mBiota Elemental) achieved cure rates of 100% among 6 SIBO patients and 75% among 12 combination SIBO and IMO patients, suggesting excellent efficacy. Significant clinical response was sustained 2 weeks after reintroduction of regular diet [31].
Maintaining remission can be challenging; recurrence occurs in up to 44% of patients 9 months after remission is achieved [10]. Patients should be educated by the providers about the high rate of recurrence and possibility of repeated therapy. There is some evidence to support the use of prokinetic agents increasing time to relapse, specifically the 5HT4 receptor agonist cisapride and the combination 5HT4 agonist/5HT-2B antagonist tegaserod, which are thought to increase the frequency of phase III migrating motor complexes (i.e. small bowel housekeeper waves) that clear food particles and secretions from the foregut [32, 33]. Dietary changes to maintain remission in SIBO have not been rigorously studied, but data extrapolated from IBS trials suggests that there may be utility in a low fermentation diet [10, 34]. A low-fermentation diet theoretically could reduce the risk of recurrence as well. Low fermentation eating also incorporates meal spacing (at least 5 hours between each meal) and avoidance of overnight eating which further facilitates the occurrence of phase III migrating motor complexes in the small bowel.
Future Directions and Controversies
There are abundant opportunities to advance the study of SIBO. The process of small bowel aspirate culture has room for improvement and standardization of the protocol to reduce contamination. This ought to facilitate more work to understand the small bowel microbiome in healthy individuals and its alterations in SIBO. The link between SIBO and IBS also deserves further investigation. While there is an overlap between IBS and SIBO, not all IBS patients respond to microbiome-modulating treatments; therefore, developing and optimizing objective biomarkers to amplify response rate is critical for the benefit of patients and health care systems.
Data Availability
No datasets were generated or analysed during the current study.
References
Greiner AK, Papineni RV, Umar S. Chemoprevention in gastrointestinal physiology and disease. Natural products and microbiome. Am J Physiol Gastrointest Liver Physiol. 2014;307(1):G1–15. https://doi.org/10.1152/ajpgi.00044.2014.
Pimentel M, Saad RJ, Long MD, Rao SSC. ACG Clinical Guideline: small intestinal bacterial overgrowth. Official J Am Coll Gastroenterol | ACG. 2020;115(2):165–78. https://doi.org/10.14309/ajg.0000000000000501.
Karakosta A, Bousvaros K, Margaritis A, Moschovi P, Mousafiri O, Fousekis F, et al. High prevalence of small intestinal bacterial overgrowth syndrome in ICU patients: an observational study. J Intensive Care Med. 2024;39(1):69–76. https://doi.org/10.1177/08850666231190284.
Onana Ndong P, Boutallaka H, Marine-Barjoan E, Ouizeman D, Mroue R, Anty R, et al. Prevalence of small intestinal bacterial overgrowth in irritable bowel syndrome (IBS): correlating H(2) or CH(4) production with severity of IBS. JGH Open. 2023;7(4):311–20. https://doi.org/10.1002/jgh3.12899.
Gudan A, Jamiol-Milc D, Hawrylkowicz V, Skonieczna-Zydecka K, Stachowska E. The prevalence of small intestinal bacterial overgrowth in patients with non-alcoholic liver diseases: NAFLD, NASH, Fibrosis, Cirrhosis-A systematic review, Meta-analysis and Meta-regression. Nutrients. 2022;14(24). https://doi.org/10.3390/nu14245261.
Sachdev AH, Pimentel M. Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance. Ther Adv Chronic Dis. 2013;4(5):223–31. https://doi.org/10.1177/2040622313496126.
Liu Chen Kiow J, Bellila R, Therrien A, Sidani S, Bouin M. Predictors of small intestinal bacterial overgrowth in symptomatic patients referred for Breath Testing. J Clin Med Res. 2020;12(10):655–61. https://doi.org/10.14740/jocmr4320.
Kitaghenda FK, Hong J, Shao Y, Yao L, Zhu X. The prevalence of small intestinal bacterial overgrowth after Roux-en-Y gastric bypass (RYGB): a systematic review and Meta-analysis. Obes Surg. 2024;34(1):250–7. https://doi.org/10.1007/s11695-023-06974-9.
Pichetshote N, Rezaie A. Bloating and abdominal distension: exploring hidden depths and insights. Curr Treat Options Gastroenterol. 2020;18(2):337–52. https://doi.org/10.1007/s11938-020-00288-w.
Rezaie A, Pimentel M, Rao SS. How to test and treat small intestinal bacterial overgrowth: an evidence-based Approach. Curr Gastroenterol Rep. 2016;18(2):8. https://doi.org/10.1007/s11894-015-0482-9.
Roland BC, Ciarleglio MM, Clarke JO, Semler JR, Tomakin E, Mullin GE, et al. Small intestinal transit time is delayed in small intestinal bacterial overgrowth. J Clin Gastroenterol. 2015;49(7):571–6. https://doi.org/10.1097/MCG.0000000000000257.
Lo WK, Chan WW. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis. Clin Gastroenterol Hepatol. 2013;11(5):483–90. https://doi.org/10.1016/j.cgh.2012.12.011.
Efremova I, Maslennikov R, Poluektova E, Vasilieva E, Zharikov Y, Suslov A, et al. Epidemiology of small intestinal bacterial overgrowth. World J Gastroenterol. 2023;29(22):3400–21. https://doi.org/10.3748/wjg.v29.i22.3400.
Weitsman S, Celly S, Leite G, Mathur R, Sedighi R, Barlow GM, et al. Effects of Proton Pump inhibitors on the small bowel and stool microbiomes. Dig Dis Sci. 2022;67(1):224–32. https://doi.org/10.1007/s10620-021-06857-y.
Leite G, Rezaie A, Mathur R, Barlow GM, Rashid M, Hosseini A, et al. Defining small intestinal bacterial overgrowth by culture and high throughput sequencing. Clin Gastroenterol Hepatol. 2024;22(2):259–70. https://doi.org/10.1016/j.cgh.2023.06.001.
Barlow JT, Leite G, Romano AE, Sedighi R, Chang C, Celly S, et al. Quantitative sequencing clarifies the role of disruptor taxa, oral microbiota, and strict anaerobes in the human small-intestine microbiome. Microbiome. 2021;9(1):214. https://doi.org/10.1186/s40168-021-01162-2.
Li J, Zhang R, Ma J, Tang S, Li Y, Li Y, et al. Mucosa-Associated Microbial Profile is altered in small intestinal bacterial overgrowth. Front Microbiol. 2021;12:710940. https://doi.org/10.3389/fmicb.2021.710940.
Maslennikov R, Ivashkin V, Efremova I, Poluektova E, Kudryavtseva A, Krasnov G. Gut dysbiosis and small intestinal bacterial overgrowth as independent forms of gut microbiota disorders in cirrhosis. World J Gastroenterol. 2022;28(10):1067–77. https://doi.org/10.3748/wjg.v28.i10.1067.
Lim J, Rezaie A. Irritable bowel syndrome-like symptoms in quiescent inflammatory bowel disease: a practical Approach to diagnosis and treatment of Organic causes. Dig Dis Sci. 2023;68(11):4081–97. https://doi.org/10.1007/s10620-023-08095-w.
Rezaie A, Buresi M, Lembo A, Lin H, McCallum R, Rao S, et al. Hydrogen and methane-based Breath Testing in Gastrointestinal disorders: the North American Consensus. Official J Am Coll Gastroenterol | ACG. 2017;112(5):775–84. https://doi.org/10.1038/ajg.2017.46.
Cangemi DJ, Lacy BE, Wise J. Diagnosing small intestinal bacterial overgrowth: a comparison of Lactulose Breath tests to small Bowel aspirates. Dig Dis Sci. 2021;66(6):2042–50. https://doi.org/10.1007/s10620-020-06484-z.
Leite GGS, Morales W, Weitsman S, Celly S, Parodi G, Mathur R, et al. Optimizing microbiome sequencing for small intestinal aspirates: validation of novel techniques through the REIMAGINE study. BMC Microbiol. 2019;19(1):239. https://doi.org/10.1186/s12866-019-1617-1.
Saad RJ, Chey WD. Breath testing for small intestinal bacterial overgrowth: maximizing test accuracy. Clin Gastroenterol Hepatol. 2014;12(12):1964–72. https://doi.org/10.1016/j.cgh.2013.09.055. quiz e1119-1920.
Khoshini R, Dai SC, Lezcano S, Pimentel M. A systematic review of diagnostic tests for small intestinal bacterial overgrowth. Dig Dis Sci. 2008;53(6):1443–54. https://doi.org/10.1007/s10620-007-0065-1.
Baker JR, Chey WD, Watts L, Armstrong M, Collins K, Lee AA, et al. How the North American Consensus Protocol affects the performance of glucose breath testing for bacterial overgrowth Versus a traditional method. Am J Gastroenterol. 2021;116(4):780–7. https://doi.org/10.14309/ajg.0000000000001110.
Lim J, Rezaie A. Pros and cons of Breath Testing for small intestinal bacterial overgrowth and intestinal methanogen overgrowth. Gastroenterol Hepatol (N Y). 2023;19(3):140–6.
Rezaie A. Shedding light on elevated baseline hydrogen and flat-line patterns during Breath Testing. Am J Gastroenterol. 2020;115(6):956–7. https://doi.org/10.14309/ajg.0000000000000659.
Shah SC, Day LW, Somsouk M, Sewell JL. Meta-analysis: antibiotic therapy for small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2013;38(8):925–34. https://doi.org/10.1111/apt.12479.
Takakura W, Rezaie A, Chey WD, Wang J, Pimentel M. Symptomatic response to antibiotics in patients with small intestinal bacterial overgrowth: a systematic review and Meta-analysis. J Neurogastroenterol Motil. 2024;30(1):7–16. https://doi.org/10.5056/jnm22187.
Pimentel M, Constantino T, Kong Y, Bajwa M, Rezaei A, Park S. A 14-day elemental diet is highly effective in normalizing the lactulose breath test. Dig Dis Sci. 2004;49(1):73–7. https://doi.org/10.1023/b:ddas.0000011605.43979.e1.
Ali Rezaie BC, Houser K, Mathur R, Brimberry D, Rashid M, Hosseini A, Mehravar S, Chan Y, Leite G, Morales W, Sanchez M, Yip C, Fajardo CM, Rivera I, Gillian M, Barlow J, Nasser A, Kamboj J, Lim C, Scarcello M. Pimentel (2024). Compliance, safety, and effect of exclusive palatable elemental diet in microbial overgrowth: A prospective clinical trial Paper presented at the Digestive Diseases Week, Washington, D.C., United States, 2024, May 19–21.
Madrid AM, Hurtado C, Venegas M, Cumsille F, Defilippi C. Long-term treatment with cisapride and antibiotics in liver cirrhosis: effect on small intestinal motility, bacterial overgrowth, and liver function. Am J Gastroenterol. 2001;96(4):1251–5. https://doi.org/10.1111/j.1572-0241.2001.03636.x.
Pimentel M, Morales W, Lezcano S, Sun-Chuan D, Low K, Yang J. Low-dose nocturnal tegaserod or erythromycin delays symptom recurrence after treatment of irritable bowel syndrome based on presumed bacterial overgrowth. Gastroenterol Hepatol (N Y). 2009;5(6):435–42.
Rao SS, Yu S, Fedewa A. Systematic review: dietary fibre and FODMAP-restricted diet in the management of constipation and irritable bowel syndrome. Aliment Pharmacol Ther. 2015;41(12):1256–70. https://doi.org/10.1111/apt.13167.
Min YW, Rezaie A, Pimentel M. Bile acid and gut microbiota in irritable bowel syndrome. J Neurogastroenterol Motil. 2022;28(4):549–61. https://doi.org/10.5056/jnm22129.
Weinstock LB, Pace LA, Rezaie A, Afrin LB, Molderings GJ. Mast cell activation syndrome: a primer for the gastroenterologist. Dig Dis Sci. 2021;66(4):965–82. https://doi.org/10.1007/s10620-020-06264-9.
Acknowledgements
None.
Funding
Funding was provided in part by the John and Geraldine Cusenza Family Foundation.
Open access funding provided by SCELC, Statewide California Electronic Library Consortium
Author information
Authors and Affiliations
Contributions
All authors were involved in preparation of the main manuscript text, tables, and reviewing and editing of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
AR is a consultant/speaker for Bausch Health and has equity in Gemelli Biotech and Good LFE. Cedars-Sinai has licensing agreements with Hobbs Medical and Gemelli Biotech. ES has no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sharabi, E., Rezaie, A. Small Intestinal Bacterial Overgrowth. Curr Infect Dis Rep (2024). https://doi.org/10.1007/s11908-024-00847-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s11908-024-00847-7