Abstract
Purpose of Review
The COVID-19 pandemic has been responsible for more than 6.3 million deaths worldwide. During the pandemic, the indiscriminate use of antibiotics has increased, contributing to the spread of multidrug-resistant bacteria. In this review, we aim to determine the spread and impact of antibiotic treatments in patients with COVID-19, focusing on underdeveloped and developing countries.
Recent Findings
Meta-analysis revealed that bacterial co-infections and secondary infections are relatively rare in COVID-19 patients, corresponding to less than 20% of hospitalized patients. Even so, most of these patients have received antibiotic treatments.
Summary
This review discusses how the COVID-19 pandemic could increase the emergence of multidrug-resistant strains to currently available antibiotics. Initially, we discussed the spread and impact of multidrug resistance of ESKAPE pathogens associated with nosocomial infections and analyzed their risk of secondary infections in patients with COVID-19. Then we highlight three factors related to the spread of resistant bacteria during the current pandemic: overprescription of antibiotics followed by self-medication. Finally, we discussed the lack of availability of diagnostic tests to discriminate the etiologic agent of a disease. All these factors lead to inappropriate use of antibiotics and, therefore, to an increase in the prevalence of resistance, which can have devastating consequences shortly. The data compiled in this study underscore the importance of epidemiological surveillance of hospital isolates to provide new strategies for preventing and controlling infections caused by multidrug-resistant bacteria. In addition, the bibliographic research also highlights the need for an improvement in antibiotic prescribing in the health system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2020, the World Health Organization (WHO) declared that the outbreak of the newly identified severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2), a strain of coronavirus and the etiological agent of the coronavirus disease (COVID-19). The disease constituted an international public health emergency [1]. The new coronavirus quickly spread worldwide, and outbreaks of COVID-19 have been reported by several countries and regions of the world. In mid-March 2020, the WHO declared COVID-19 a pandemic. As of June 14, 2022, more than 532 million confirmed cases and more than 6.3 million deaths had been reported from the COVID-19 pandemic. In late 2020, the efforts of scientists around the world resulted in the development of safe and efficient vaccines against COVID-19. With the availability of these vaccines, the number of cases and deaths began to progressively decrease, indicating that mass vaccination can contain outbreaks of COVID-19 [2, 3], also showing the possibility of the end of the COVID-19 pandemic.
Although we are probably close to the end, it is believed that in the future, we will have to deal with many problems arising from the COVID-19 pandemic. One of the possible problems that we will have to face is the increase in antimicrobial resistance [4•]. Resistance is currently the biggest problem with antimicrobials and one enormous burden on the public health system worldwide. A recent study analyzed the worldwide prevalence of antimicrobial resistance and estimated that 4.95 million deaths were associated with antimicrobial resistance in 2019, among which 1.27 million were directly attributable [5]. Treating patients with antimicrobial resistance is associated with high economic costs due to prolonged hospitalizations, high cost of second-line antibiotics, additional detection testing to identify pathogens, and decreased productivity, representing a tremendous burden on the economy of countries. It is estimated that by 2050 antimicrobial resistance will be responsible for the death of approximately 10 million people worldwide [5, 6] at the cost of between $300 billion to $10 trillion [7]. Some authors estimate that the capital loss will be $100 trillion [6]. Therefore, antimicrobial resistance could increase poverty in countries, especially in underdeveloped or developing countries.
The discovery of antimicrobials in the nineteenth century revolutionized medicine and considerably increased half-life worldwide. Infectious diseases represented one of the leading causes of death in the early nineteenth century. However, this changed with the era of antibiotics [8], starting in 1943 with the approval and commercialization of penicillin. After the commercialization of antibiotics, the half-life increased significantly, and the mortality rate associated with infectious diseases decreased. For example, in 1920, the life expectancy in the USA was 56.4 years, and today it has risen to 80 years [9]. However, a few decades after the discovery of antimicrobials, the first antibiotic resistances began to be described, and even at least 3 years before the commercialization of penicillin, penicillin-resistant strains of Staphylococcus aureus were reported in the literature [10]. In 1950 resistance to beta-lactam penicillin was described. Later in 1962, a methicillin-resistant strain of S. aureus was identified. Later strains resistant to tetracycline, gentamicin, erythromycin, levofloxacin, and vancomycin were also reported [10]. Bacteria have now developed multiple resistances to most available antibiotics.
This antimicrobial resistance occurs due to genetic changes in bacteria. Although antibiotic resistance is a naturally occurring event, it is often potentiated and caused by the overuse of antibiotics, causing them to lose their effectiveness [11]. As a result of this resistance, infections caused by these agents become challenging to treat. This, in turn, increases the risk of the disease spreading, resulting in more severe cases and deaths. In addition, the emergence and spread of resistant pathogens threaten our ability to treat previously common infections [2, 12•, 13•]. Based on this precept, the WHO has released a list of drug-resistant bacteria that pose the greatest threat to human health [2], categorizing them as critical, high, and medium priority organisms in terms of antimicrobial resistance.
Studies show that the indecency of infections caused by multidrug-resistant microorganisms resistant to multiple antibiotics occurs worldwide regardless of income [14•]. However, the regions most affected by this problem are the poorest and most populous on the planet [14•, 15]. According to a study carried out by Wirtz et al. [16], in the 10 years, from 1997 to 2007, there was an increase in resistance to several classes of antimicrobials in Latin America, mainly quinolones, corroborating the data found in the 2020 systematic review [17] that demonstrated the existence of 9 different genes related to the quinolone resistance plasmid in Latin America. In addition, Domínguez et al. [18] showed resistance to beta-lactams in aquatic environments also in Latin America.
In parallel with the emergence of antibiotic resistance, the development and approval of new antimicrobials have declined dramatically over the years [11, 19]. The WHO published in January 2020 a report on studies with new antibiotics at preclinical and clinical levels. The study showed that only 52 new antimicrobial compounds are being tested. Even more alarming data showed that only 32 of these were aimed at treating multidrug-resistant pathogens considered a priority by the organization [20•].
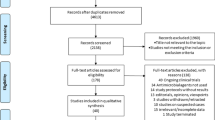
In addition, since the beginning of the COVID-19 pandemic, antibiotic consumption worldwide has increased, and researchers are warning of a possible rise in antibiotic-resistant strains and an increase in multidrug-resistant strains of concern, globally, such as strains of the ESKAPE group (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) [13•, 21]. Therefore, this review aims to describe recent data on the COVID-19 pandemic and its impact on the appearance of multidrug-resistant strains of the ESKAPE group, focusing mainly on underdeveloped and developing countries. This study uses PubMed, Web of Science, Science Direct, LILACS, and SciELO databases. To search for data regarding the impact of the COVID-19 pandemic on antibiotic resistance, “COVID-19” and “antibiotic resistance” were used to search for data. The articles found were analyzed and the data described in this study. This review suggests strict surveillance and implementation of antimicrobial resistance control policies. It indicates the need for research focused on understanding the impact of the COVID-19 pandemic on antimicrobial resistance in the coming years, especially in underdeveloped and developing countries, as well as the implementation of molecular biology tools for diagnosing bacterial infections.
Spread and Impact of Diseases Caused by Multidrug-Resistant Bacteria Around the World
According to Murray et al. [14•], approximately 5 million deaths associated with multidrug-resistant bacteria occurred worldwide in 2019. Also according to Murray et al. [14•], the most affected regions are Africa, where approximately 400 deaths per 100,000 inhabitants are reported, followed by America, Asia, Europe, and Oceania. The regions with the highest deaths are, not coincidentally, the poorest regions on the planet [15]: sub-Saharan Africa, with 375 deaths per 100,000 inhabitants, and South Asia, with 80 deaths per 100,000 inhabitants [14•]. South America is the fourth subregion on the list, with about 75 deaths caused by multidrug-resistant bacteria for every 100,000 inhabitants [14•].
In underdeveloped or developing countries, factors such as (I) inadequate access to effective drugs, (II) unregulated administration and manufacturing of antimicrobials, and (III) truncated antimicrobial therapy due to cost are contributing to the development of multidrug-resistant organisms [15]. Furthermore, the causes of antimicrobial resistance in developing countries are complex and may be related to (I) the practices of health professionals, (II) the behavior of patients concerning the use of antimicrobials, and (III) the antimicrobial supply chain. These factors may include poor prescribing practices, inadequate patient education, limited diagnostic facilities, unauthorized sales of antimicrobials, lack of adequate drug regulatory mechanisms, and non-human use of antimicrobials [22].
ESKAPE Pathogens Cause Most of the Hospital-Acquired Infections in the World
In February 2017, to focus on and guide research and development related to new antibiotics, the WHO published its list of pathogens for which antimicrobial development is urgently needed [2]. This comprehensive list has designated ESKAPE pathogens as “priority status” [23]. The ESKAPE group comprises multidrug-resistant strains that are the main causative agents of nosocomial infections worldwide [24].
ESKAPE pathogens have developed resistance mechanisms against oxazolidinones, lipopeptides, macrolides, fluoroquinolones, tetracyclines, β-lactams, combinations of β-lactam inhibitors, and antibiotics that are the last line of defense, including carbapenems, glycopeptides, and polymyxins [25,26,27]. The acquisition of resistance occurs through random genetic mutations and/or the acquisition of mobile genetic elements such as transposons and plasmids (Table 1) [28, 29].
Before the pandemic, a study by Zhen et al. [64] evaluated the economic impact of antibiotic resistance in organisms of the ESKAPE group. The authors observed that the most studied organism is S. aureus, followed by Enterococcus spp., A. baumannii, K. pneumoniae, and P. aeruginosa. Approximately 85% of the studies eligible for analysis assessed the total hospital cost, 14% the cost of antibiotic treatment, and 5% the cost in intensive care units. Overall, the authors observed that multidrug-resistant organisms are significantly associated with more economic burdens than susceptible organisms or those without infection or colonization. Indeed, Marturano and Lowery (2019) [65] determined that the total cost of care for patients with infections caused by pathogens in the ESKAPE group is higher than for those with non-ESKAPE pathogens by an average of $5500.
ESKAPE group pathogens constitute a significant healthcare burden, and recent studies suggest upward trends in prevalence [66], economic cost [67], and resistance [68] in the coming years.
A bibliometric study by Ayobami et al. [69•] evaluated antibiotic resistance in nosocomial infections caused by bacteria from the ESKAPE group in low- and middle-income countries between 2010 and 2020. The authors observed that the proportion of methicillin resistance pooled in S. aureus was 48.4%. In addition, the pooled proportions of carbapenem resistance were higher in Gram-negative pathogens: K. pneumoniae (34.9%), A. baumannii (72.4%), P. aeruginosa (37.1%), and Enterobacter spp. (51.2%). Furthermore, third-generation cephalosporins were observed with higher proportions of resistance in K. pneumoniae (78.7%) and Enterobacter spp. (83.5%). In summary, the combined resistance ratios for Gram-negative pathogens were higher in low- and middle-income countries than regional and national estimates from high-income countries. This study demonstrated that patients in resource-limited regions are particularly affected by antimicrobial resistance, which has been previously reported [15]. The authors further suggested that to combat high antibiotic resistance in low- and middle-income countries and reduce health disparities, strengthening local surveillance and health systems, in general, is crucial.
Patients with COVID-19 Are at Risk of Secondary Infections by ESKAPE Pathogens
Bacterial infections are commonly identified in patients with viral respiratory infections and are important causes of morbidity and mortality in patients infected with SARS-CoV-2 [70•]. Therefore, it is essential to differentiate between co-infection and secondary infection. Co-infections are present in the patient at admission, while secondary infections are acquired during hospitalization. Patients with COVID-19 are more likely to develop secondary infections during hospitalizations [71]. However, in clinical practice, it is not very common to differentiate whether a patient with COVID-19 has a co-infection or has acquired a secondary infection due to the lack of initial diagnostic tests (this topic will be discussed later). In any cases of bacterial infection in patients with COVID-19 (secondary infection or co-infection), the patients need to be treated with antibiotics (Table 2) [70•].
A study by Langford et al. [72•] evaluated 3338 patients with COVID-19. Among these, 3.5% had acute bacterial co-infections, and 14.3% had secondary bacterial infections. The overall proportion of COVID-19 patients with bacterial infection was 6.9%. The authors also observed that bacterial co-infection was more common in critically ill patients, accounting for 8.1%; however, most COVID-19 patients received antibiotic treatment.
Another study by Lansbury et al. [73], including 3834 patients, observed that 7% of hospitalized patients with COVID-19 had a bacterial co-infection and/or secondary infection. As Langford et al. [72•] and Lansbury et al. [73] observed, a more significant proportion of patients in intensive care units (ICU) had bacterial infections (14%) than patients in mixed ward/ICU settings (4%).
Also, Gaspari et al. [74] evaluated 173 patients in the COVID-19 period and 132 in the pre-COVID-19 period. Co-infections and/or secondary infections with pathogens from the ESKAPE group were documented in 23 (13.3%) and 35 (26.5%) patients in the pandemic and pre-pandemic periods, respectively. Poyil [75•] also assessed the prevalence of bacterial infections with ESKAPE pathogens in patients with COVID-19. Finally, the author observed several studies that reported bacterial infections with COVID-19 at various levels. The causative agents included multidrug-resistant strains from high-priority categories such as vancomycin-resistant Enterococcus, intermediate/vancomycin-resistant Enterococcus faecium, vancomycin- and methicillin-resistant S. aureus, extended-spectrum beta-lactamases-producing K. pneumoniae, A baumannii resistant to carbapenems, and P. aeruginosa producing extended-spectrum beta-lactamases.
Bacterial infections are relatively infrequent in hospitalized patients with COVID-19, less so than in previous flu pandemics. Thus, most of these patients may not require empirical antibacterial treatment, which does not support the routine use of antibiotics in managing confirmed COVID-19 infection. Most bacterial infections, whether or not they belong to the ESKAPE group, are more frequently associated with more severe disease cases (Table 3). Thus, there has been concern about the worsening of antimicrobial resistance in patients with COVID-19, as the choice of antibiotics in patients with the disease is often empirical [76].
Factors Associated with the Appearance and Spread of Antibiotic-Resistant Bacteria During the COVID-19 Pandemic
Excessive and Reckless Medical Prescription in the COVID-19 Pandemic
One of the strategies implemented to combat COVID-19 is using antibiotics in some severe cases, but inappropriately prescribing antibiotics to patients with COVID-19 could generate antibiotic resistance and compromise efforts in the fight against antimicrobial resistance, which could have devastating consequences shortly. For example, patients with respiratory infections other than COVID-19 and who had symptoms similar to COVID-19, as well as efforts to prevent the spread of COVID-19, have led to the empirical use of antibiotics in hospitals [99]. Given the empirical use of antibiotics, the WHO recommends administering antibiotics only for severe cases of COVID-19 or when there are signs and symptoms of bacterial infection. However, many patients with mild COVID-19 without pneumonia or moderate COVID-19 with pneumonia receive antibiotics [21, 72•]. Previous studies have associated higher mortality in patients due to bacterial co-infections in influenza [100]. In addition, death cases of patients with COVID-19 along with bacterial co-infections have also been frequently reported [101]. However, the available evidence suggests that in both influenza and COVID-19 cases, rates of bacterial co-infection are low (less than 20%).
In three studies conducted in Wuhan of hospitalized patients with COVID-19, it was reported that most patients received antibacterial therapy. In the first study of 191 patients, 95% received antibiotics. In the second study, 72% of the patients were treated with antibiotics. Still, only 8% showed bacterial or fungal co-infections. In the third study, all patients in a hospital received antibacterial therapy with an antibiotic or a combination of antibiotics [101,102,103]. Similarly, a study that analyzed 925 patients from four Dutch hospitals found that 556 patients (60.1%) received antibiotic therapy, but only 12 patients (1.2%) had bacterial co-infection [99]. These data suggest that bacterial co-infections in COVID-19 patients are rare, and often these patients undergo antibiotic therapy even in the absence of bacterial infections. Consequently, antibiotics are empirically unnecessary and over-prescribed.
Antibiotics prescribed to COVID-19 patients are often broad-spectrum to ensure sensitivity to a wide range of suspect organisms. Among the most prescribed antibiotics are β-lactamases inhibitors, cephalosporins, fluoroquinolones, and macrolides [21, 104]. Azithromycin macrolide was the second most prescribed treatment for COVID-19 [12•]. Misinformation, in combination with the lack of treatment against COVID-19, has led many doctors to overprescribe antibiotics. In addition, educating physicians who treat COVID-19 patients with principles of antibiotic administration could decrease unnecessary antibiotic use.
The other reason for prescribing antibiotics in COVID-19 patients is the close similarity between COVID-19 pneumonia and bacterial pneumonia [72•]. The symptomatology described in patients with COVID-19 often overlaps with bacterial infections [105]. However, there are many difficulties differentiating pneumonia from bacterial or COVID-19 infection. Common biomarkers such as C-reactive protein or procalcitonin used to distinguish viral from bacterial pneumonia are often ineffective in patients with COVID-19. They require hours or days to obtain a result, making immediate treatment difficult [106]. C-reactive protein quantification is a rapid test to distinguish bacterial from viral pneumonia. C-reactive protein is a biomarker elevated in bacterial infections but not generally in viral infections. Before the COVID-19 pandemic, 90% of C-reactive protein elevations were attributed to infections whose etiologic agents were bacterial pathogens [107]. However, studies have shown that this biomarker can be increased in patients with COVID-19 [108], leading many clinicians to prescribe empiric antibiotics to patients with COVID-19 without a microbiological confirmation of bacterial infection. The research focused on the predictive value of diagnostic tools could considerably help in making clinical decisions when prescribing.
Lack of Availability of Diagnostic Tests
At a general level, the health system is lacking in identifying pathogens [109]. Antibiotics are often prescribed in medical care centers without a positive result of bacterial infection, contributing to the indiscriminate use of antibiotics and, therefore, the appearance of multidrug-resistant bacteria [109]. Antibiotics are also prescribed without knowing the pathogen causing the infection and the resistance profile, leading to the administration of ineffective treatments. Requesting diagnostic tests could resolve these issues. However, the most accepted diagnostic tests for microorganisms are based on microscopy, culture, and sensitivity. They need 24–48 h to show the result, which can discourage healthcare professionals from ordering laboratory tests [110]. Therefore, doctors often do not order antimicrobial tests before prescribing antibiotics, contributing to the indiscriminate use of antibiotics.
One option to combat this problem would be implementing diagnostic approaches based on molecular biology, which detect the pathogen’s DNA. These tests could ensure an early, accurate diagnosis and efficient antibacterial therapy for bacterial infections, thus avoiding fatal consequences such as the ineffectiveness of empirical treatments and increased multidrug-resistant strains [111]. However, implementing tests based on molecular biology still has some limitations, such as the high cost of the equipment used and the lack of availability in health centers in low- and middle-income countries [112]. This leads to the conclusion that we have the biotechnological tools available to make an adequate diagnosis, which helps to avoid the indiscriminate use of antibiotics. However, the economic deficiencies of the health system are still an obstacle. Greater investment is needed in the health system and antibiotic administration programs.
In this context, the implementation of molecular biological-based tests for the detection of bacteria during the COVID-19 pandemic could considerably help the easy and rapid identification of co-infections or secondary infections, leading to the administration of antibiotics only when necessary. The primary test for the diagnosis of COVID-19 is PCR (polymerase chain reaction). PCR is a susceptible and efficient molecular biology-based test that detects SARS-CoV-2 [113] or even Nanopore sequencing [114].
Despite the high costs of this test, during the COVID-19 pandemic, PCR was widely implemented in many countries, which considerably helped to diagnose many patients. However, the same patients were not analyzed for the presence of bacterial infections. Still, these same patients have often been prescribed antibiotics, which clearly shows the indiscriminate use of antibiotics during the COVID-19 pandemic. In addition, the accessibility and availability of these diagnostic tests will lead to a substantial decrease in the empirical administration of antibiotics.
Self-Medication and the COVID-19 Pandemic
Self-medication with antibiotics can lead to several public health problems, for example, the significant increase in antibiotic resistance. Self-medication is characterized by the inappropriate use of antibiotics by people who treat their illnesses without a prescription or medical supervision [115].
Since the beginning of the COVID-19 pandemic, preliminary studies in cell culture have suggested several drugs as promising candidates against SAR-CoV-2 [116]. For example, hydroxychloroquine, combined with azithromycin, has shown favorable results in cell culture trials and small, uncontrolled studies [117]. Many countries quickly spread news encouraging the use of hydroxychloroquine and azithromycin as a prophylactic or curative treatment against the new coronavirus [118], leading many people to self-medicate with various drugs, mainly antibiotics (azithromycin, ceftriaxone, and penicillins), and antiparasitics (chloroquine, hydroxychloroquine, nitazoxanide, ivermectin) during the COVID-19 pandemic [119]. However, evidence in hospitalized patients has shown that these drugs, as prophylactics or curatives, are ineffective against COVID-19 and can even be harmful [120, 121]. During the pandemic, the lack of knowledge and the massive spread of false news on social networks led many people to self-medicate with different medications, including antibiotics [121].
Self-medication with antibiotics is more frequent in low- and middle-income countries, where many antibiotics are freely sold, and counterfeiting antibiotics are more frequent [9, 12•]. Recently, a study reported that self-medication with antibiotics is more frequent in young people from low- and middle-income countries [9]. In another review study including 7676 participants, it was reported that all participants self-medicated with antibiotics in the last 3 months to 1 year before the study [122]. According to Ferdiana et al. [123], in Indonesia, participants reported using antibiotics without a doctor’s prescription because it was more convenient and cost-effective than looking for public healthcare or pay for a private consultation, mostly to treat common symptoms, as muscle relaxant and energy booster. There were reports of antibiotics that had already been prescribed by doctors, or by suggestions, even pharmacists. In India, the indiscriminate use of antibiotics is reported by the administration of different doses in public and private sectors [124]. In Sri Lanka, 77% of participants who reported self-medication with antibiotics had respiratory symptoms as a complaint [125].
Antibiotic access in developed countries is well regulated, and a prescription is required to dispense antibiotics [109]. However, in developing countries, the reality is different. In these countries, the policies to control and regulate antibiotic access are deficient [126, 127]. Antibiotics can be purchased over-the-counter, without a prescription at any pharmacy, or even when needed, they are sold freely due to lack of supervision [10, 123, 126, 128]. In the review carried out by Ocan et al. [129], most self-medication drugs are antibiotics and antimalarials, including chloroquine. In addition to using these drugs without a prescription, there are reports of shorter treatment times, wrong dosages, and misuse. The prevalence of self-medication found by Ocan et al. [129] was 38.8% in low- and middle-income countries, which corroborates the data found by Do et al. [126], where self-medication in these countries is 35%.
In 2020 in Peru, a study showed that 33.9% of hospitalized patients with COVID-19 self-medicated before entering the hospital, with the most frequent drugs being antibiotics (mainly azithromycin and ceftriaxone) and ivermectin [130]. On the other hand, a study conducted in Australia with 2217 participants revealed that during the first wave of the COVID-19 pandemic, approximately 20% of study participants self-medicated with antibiotics to protect themselves against COVID-19 [131]. In addition, a systematic review of eight cross-sectional studies found that the prevalence of self-medication with antibiotics ranged from 4 to 88.3% [121]. Therefore, implementing policies to educate the public about the problems associated with the indiscriminate use of antibiotics could help reduce self-medication. Consequently, it is crucial to use antibiotics appropriately, even during the pandemic, to avoid the appearance of multidrug-resistant strains.
A recent study in Mexico that evaluated changes in the resistance profile of critical and high-priority microorganisms collected before and during the COVID-19 pandemic showed an increase in antimicrobial resistance. This same study found a rise in oxacillin resistance by S. aureus and carbapenems by K. pneumoniae, as well as an increase in erythromycin macrolide resistance in S. aureus. The latter may be associated with excessive use of azithromycin [4•]. These results indicate that the COVID-19 pandemic strongly influenced the emergence of multidrug-resistant strains. However, we still do not have enough data to know the real impact of the COVID-19 pandemic on antimicrobial resistance. Therefore, more studies are needed to discover the real impact of the pandemic on antimicrobial resistance.
Conclusion
As analyzed in this review, bacterial pathogens from the ESKAPE group play a crucial role in turning bacterial infection into a fatal disease and being a deadly factor for COVID-19 patients. Even in the current pandemic scenario, bacterial co-infections with Gram-negative bacteria from the ESKAPE group are more common in patients with severe cases of COVID-19 than in patients with milder symptoms of the disease. Species in this group are commonly associated with highly virulent and antibiotic-resistant strains. As mentioned earlier, treating nosocomial infections caused by bacteria is still empirical, which may even contribute to the emergence of multidrug-resistant bacteria. In addition, the empirical prescription of antibiotics, self-medication, and the lack of availability of rapid diagnostic tests evidence the lack of control, government surveillance, and investment in the public health system, leading to the emergence of multidrug-resistant and the worsening of resistance of strains already known. More studies are still needed to know the actual damage of the COVID-19 pandemic. However, the data compiled in this study underscore the importance of epidemiological surveillance and analysis of the genetic evolution of hospital isolates to provide new strategies for preventing and controlling infections caused by multidrug-resistant bacteria. Furthermore, the bibliographic study also suggests that it is possible to mitigate this problem with coordinated efforts to implement new health policies based on the appropriate use of antibiotics, as well as the surveillance of the proper use of antibiotics, the training of medical personnel, and more significant investment in the health system and in research, which is undoubtedly a critical factor in the fight against antibiotic resistance and the development of new antibacterial agents.
Change history
07 November 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11908-022-00791-4
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Khan S, Siddique R, Bai Q, Shabana null, Liu Y, Xue M, et al. Coronaviruses disease 2019 (COVID-19): causative agent, mental health concerns, and potential management options. J Infect Public Health. 2020;13:1840–4
Mogasale VV, Saldanha P, Pai V, Rekha PD, Mogasale V. A descriptive analysis of antimicrobial resistance patterns of WHO priority pathogens isolated in children from a tertiary care hospital in India. Sci Rep. Nature Publishing Group; 2021;11:5116.
Tenforde MW, Self WH, Adams K, Gaglani M, Ginde AA, McNeal T, et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA. 2021;326:2043–54.
• López-Jácome LE, Fernández-Rodríguez D, Franco-Cendejas R, Camacho-Ortiz A, Morfin-Otero MDR, Rodríguez-Noriega E, et al. Increment antimicrobial resistance during the COVID-19 pandemic: results from the Invifar Network. Microb Drug Resist. 2022;28:338–45. A contemporary compilation study highlighting the emergence of antimicrobial resistant bacteria as a consequence of the COVID-19 pandemic
de Kraker MEA, Stewardson AJ, Harbarth S. Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med. 2016;13: e1002184.
Cooke J. Antimicrobial resistance: a major priority for global focus. Eur J Hosp Pharm. British Medical Journal Publishing Group; 2022;29:63–4.
Burki TK. Superbugs: an arms race against bacteria. Lancet Respir Med. Elsevier; 2018;6:668.
Katz L, Baltz RH. Natural product discovery: past, present, and future. J Ind Microbiol Biotechnol. 2016;43:155–76.
Aslam B, Wang W, Arshad MI, Khurshid M, Muzammil S, Rasool MH, et al. Antibiotic resistance: a rundown of a global crisis. Infect Drug Resist. 2018;11:1645–58.
Ventola CL. The antibiotic resistance crisis. P T. 2015;40:277–83.
Larsen J, Raisen CL, Ba X, Sadgrove NJ, Padilla-González GF, Simmonds MSJ, et al. Emergence of methicillin resistance predates the clinical use of antibiotics. Nature Nature Publishing Group. 2022;602:135–41.
• Ghosh S, Bornman C, Zafer MM. Antimicrobial resistance threats in the emerging COVID-19 pandemic: where do we stand? J Infect Public Health. 2021;14:555–60. A comprehensive review of antimicrobial resistance in the pandemic context
• Cantón R, Gijón D, Ruiz-Garbajosa P. Antimicrobial resistance in ICUs: an update in the light of the COVID-19 pandemic. Curr Opin Crit Care. 2020;26:433–41. An authoritative review of antimicrobial resistance in hospitalized COVID-19 patients
• Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. Elsevier; 2022;399:629–55. The biggest reference of data compilation on antimicrobial resistance before the pandemic
Planta MB. The role of poverty in antimicrobial resistance. J Am Board Fam Med. 2007;20:533–9.
Wirtz VJ, Dreser A, Gonzales R. Trends in antibiotic utilization in eight Latin American countries, 1997–2007. Rev Panam Salud Publica. 2010;27:219–25.
Vieira DC, Lima WG, de Paiva MC. Plasmid-mediated quinolone resistance (PMQR) among Enterobacteriales in Latin America: a systematic review. Mol Biol Rep. 2020;47:1471–83.
Domínguez DC, Chacón LM, Wallace D. Anthropogenic activities and the problem of antibiotic resistance in Latin America: a water issue. Water. Multidisciplinary Digital Publishing Institute; 2021;13:2693.
Browne AJ, Chipeta MG, Haines-Woodhouse G, Kumaran EPA, Hamadani BHK, Zaraa S, et al. Global antibiotic consumption and usage in humans, 2000–18: a spatial modelling study. Lancet Planet Health; Elsevier. 2021;5:e893-904.
• Lancet T. The antimicrobial crisis: enough advocacy, more action. The Lancet. Elsevier; 2020;395:247. An insightful paper addressing the issues of antimicrobial drugs development.
Rawson TM, Moore LSP, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, et al. Bacterial and fungal co-infection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71:2459–68.
Ayukekbong JA, Ntemgwa M, Atabe AN. The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrob Resist Infect Control. 2017;6:47.
Rice LB. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis. 2008;197:1079–81.
Santajit S, Indrawattana N. Mechanisms of antimicrobial resistance in ESKAPE pathogens. Biomed Res Int. 2016;2016:2475067.
Iguchi S, Mizutani T, Hiramatsu K, Kikuchi K. Rapid acquisition of linezolid resistance in methicillin-resistant Staphylococcus aureus: role of hypermutation and homologous recombination. PLoS ONE. 2016;11: e0155512.
Naylor NR, Atun R, Zhu N, Kulasabanathan K, Silva S, Chatterjee A, et al. Estimating the burden of antimicrobial resistance: a systematic literature review. Antimicrob Resist Infect Control. 2018;7:58.
Zaman SB, Hussain MA, Nye R, Mehta V, Mamun KT, Hossain N. A review on antibiotic resistance: alarm bells are ringing. Cureus. 2017;9: e1403.
Partridge SR, Kwong SM, Firth N, Jensen SO. Mobile genetic elements associated with antimicrobial resistance. Clin Microbiol Rev. 2018;31:e00088-e117.
Woodford N, Ellington MJ. The emergence of antibiotic resistance by mutation. Clin Microbiol Infect. 2007;13:5–18.
Gao W, Howden BP, Stinear TP. Evolution of virulence in Enterococcus faecium, a hospital-adapted opportunistic pathogen. Curr Opin Microbiol. 2018;41:76–82.
Trościańczyk A, Nowakiewicz A, Osińska M, Łagowski D, Gnat S, Chudzik-Rząd B. Comparative characteristics of sequence types, genotypes and virulence of multidrug-resistant Enterococcus faecium isolated from various hosts in eastern Poland. Spread of clonal complex 17 in humans and animals. Res Microbiol. 2022;173:103925.
Ahmad-Mansour N, Loubet P, Pouget C, Dunyach-Remy C, Sotto A, Lavigne J-P, et al. Staphylococcus aureus toxins: an update on their pathogenic properties and potential treatments. Toxins (Basel). 2021;13:677.
Cheung GYC, Bae JS, Otto M. Pathogenicity and virulence of Staphylococcus aureus. Virulence. 2021;12:547–69.
Cruz AR, van Strijp JAG, Bagnoli F, Manetti AGO. Virulence gene expression of Staphylococcus aureus in human skin. Front Microbiol. 2021;12: 692023.
Pantosti A, Sanchini A, Monaco M. Mechanisms of antibiotic resistance in Staphylococcus aureus. Future Microbiol. 2007;2:323–34.
Annavajhala MK, Gomez-Simmonds A, Uhlemann A-C. Multidrug-resistant Enterobacter cloacae complex emerging as a global, diversifying threat. Front Microbiol. 2019;10:44.
Bengoechea JA, Sa PJ. Klebsiella pneumoniae infection biology: living to counteract host defences. FEMS Microbiol Rev. 2019;43:123–44.
Chan XHS, O’Connor CJ, Martyn E, Clegg AJ, Choy BJK, Soares AL, et al. Reducing broad-spectrum antibiotic use in intensive care unit between first and second waves of COVID-19 did not adversely affect mortality. J Hosp Infect. 2022;124:37–46.
De Champs C, Sauvant MP, Chanal C, Sirot D, Gazuy N, Malhuret R, et al. Prospective survey of colonization and infection caused by expanded-spectrum-beta-lactamase-producing members of the family Enterobacteriaceae in an intensive care unit. J Clin Microbiol. 1989;27:2887–90.
Li B, Zhao Y, Liu C, Chen Z, Zhou D. Molecular pathogenesis of Klebsiella pneumoniae. Future Microbiol. 2014;9:1071–81.
Munita JM, Arias CA. Mechanisms of antibiotic resistance. Microbiol Spectr. 2016;4.
Murphy CN, Clegg S. Klebsiella pneumoniae and type 3 fimbriae: nosocomial infection, regulation and biofilm formation. Future Microbiol. 2012;7:991–1002.
Peirano G, Matsumura Y, Adams MD, Bradford P, Motyl M, Chen L, et al. Genomic epidemiology of global carbapenemase-producing Enterobacter spp., 2008–2014. Emerg Infect Dis. 2018;24:1010–9.
Périchon B, Courvalin P, Galimand M. Transferable resistance to aminoglycosides by methylation of G1405 in 16S rRNA and to hydrophilic fluoroquinolones by QepA-mediated efflux in Escherichia coli. Antimicrob Agents Chemother. 2007;51:2464–9.
Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998;11:589–603.
Vuotto C, Longo F, Balice MP, Donelli G, Varaldo PE. Antibiotic resistance related to biofilm formation in Klebsiella pneumoniae. Pathogens. 2014;3:743–58.
Adams-Haduch JM, Paterson DL, Sidjabat HE, Pasculle AW, Potoski BA, Muto CA, et al. Genetic basis of multidrug resistance in Acinetobacter baumannii clinical isolates at a tertiary medical center in Pennsylvania. Antimicrob Agents Chemother. 2008;52:3837–43.
Beceiro A, Llobet E, Aranda J, Bengoechea JA, Doumith M, Hornsey M, et al. Phosphoethanolamine modification of lipid A in colistin-resistant variants of Acinetobacter baumannii mediated by the pmrAB two-component regulatory system. Antimicrob Agents Chemother. 2011;55:3370–9.
Coyne S, Rosenfeld N, Lambert T, Courvalin P, Périchon B. Overexpression of resistance-nodulation-cell division pump AdeFGH confers multidrug resistance in Acinetobacter baumannii. Antimicrob Agents Chemother. 2010;54:4389–93.
Gao S, Jung J-H, Lin S-M, Jang A-Y, Zhi Y, Bum Ahn K, et al. Development of oxytolerant salmonella typhimurium using radiation mutation technology (RMT) for cancer therapy. Sci Rep. 2020;10:3764.
Houang ETS, Chu Y-W, Lo W-S, Chu K-Y, Cheng AFB. Epidemiology of rifampin ADP-ribosyltransferase (arr-2) and metallo-beta-lactamase (blaIMP-4) gene cassettes in class 1 integrons in Acinetobacter strains isolated from blood cultures in 1997 to 2000. Antimicrob Agents Chemother. 2003;47:1382–90.
Jacobs AC, Hood I, Boyd KL, Olson PD, Morrison JM, Carson S, et al. Inactivation of phospholipase D diminishes Acinetobacter baumannii pathogenesis. Infect Immun. 2010;78:1952–62.
Lee H-W, Koh YM, Kim J, Lee J-C, Lee Y-C, Seol S-Y, et al. Capacity of multidrug-resistant clinical isolates of Acinetobacter baumannii to form biofilm and adhere to epithelial cell surfaces. Clin Microbiol Infect. 2008;14:49–54.
Luke NR, Sauberan SL, Russo TA, Beanan JM, Olson R, Loehfelm TW, et al. Identification and characterization of a glycosyltransferase involved in Acinetobacter baumannii lipopolysaccharide core biosynthesis. Infect Immun. 2010;78:2017–23.
Moffatt JH, Harper M, Harrison P, Hale JDF, Vinogradov E, Seemann T, et al. Colistin resistance in Acinetobacter baumannii is mediated by complete loss of lipopolysaccharide production. Antimicrob Agents Chemother. 2010;54:4971–7.
Russo TA, Luke NR, Beanan JM, Olson R, Sauberan SL, MacDonald U, et al. The K1 capsular polysaccharide of Acinetobacter baumannii strain 307–0294 is a major virulence factor. Infect Immun. 2010;78:3993–4000.
Vallenet D, Nordmann P, Barbe V, Poirel L, Mangenot S, Bataille E, et al. Comparative analysis of Acinetobacters: three genomes for three lifestyles. PLoS ONE. 2008;3: e1805.
Yu Y, Zhou H, Yang Q, Chen Y, Li L. Widespread occurrence of aminoglycoside resistance due to ArmA methylase in imipenem-resistant Acinetobacter baumannii isolates in China. J Antimicrob Chemother. 2007;60:454–5.
Alonso B, Fernández-Barat L, Di Domenico EG, Marín M, Cercenado E, Merino I, et al. Characterization of the virulence of Pseudomonas aeruginosa strains causing ventilator-associated pneumonia. BMC Infect Dis. 2020;20:909.
Breidenstein EBM, de la Fuente-Núñez C, Hancock REW. Pseudomonas aeruginosa: all roads lead to resistance. Trends Microbiol. 2011;19:419–26.
Cavalcanti FL de S, Mirones CR, Paucar ER, Montes LÁ, Leal-Balbino TC, Morais MMC de, et al. Mutational and acquired carbapenem resistance mechanisms in multidrug resistant Pseudomonas aeruginosa clinical isolates from Recife, Brazil. Mem Inst Oswaldo Cruz. 2015;110:1003–9.
Azevedo PAA, Furlan JPR, Oliveira-Silva M, Nakamura-Silva R, Gomes CN, Costa KRC, et al. Detection of virulence and β-lactamase encoding genes in Enterobacter aerogenes and Enterobacter cloacae clinical isolates from Brazil. Braz J Microbiol. 2018;49(Suppl 1):224–8.
Eisenstein BI, Jones GW. The spectrum of infections and pathogenic mechanisms of Escherichia coli. Adv Intern Med. 1988;33:231–52.
Zhen X, Lundborg CS, Sun X, Hu X, Dong H. Economic burden of antibiotic resistance in ESKAPE organisms: a systematic review. Antimicrob Resist Infect Control. 2019;8:137.
Marturano JE, Lowery TJ. ESKAPE pathogens in bloodstream infections are associated with higher cost and mortality but can be predicted using diagnoses upon admission. Open Forum Infect Dis. 2019;6:ofz503.
De Angelis G, Fiori B, Menchinelli G, D’Inzeo T, Liotti FM, Morandotti GA, et al. Incidence and antimicrobial resistance trends in bloodstream infections caused by ESKAPE and Escherichia coli at a large teaching hospital in Rome, a 9-year analysis (2007–2015). Eur J Clin Microbiol Infect Dis. 2018;37:1627–36.
Founou RC, Founou LL, Essack SY. Clinical and economic impact of antibiotic resistance in developing countries: a systematic review and meta-analysis. PLoS ONE. 2017;12: e0189621.
De Socio GV, Rubbioni P, Botta D, Cenci E, Belati A, Paggi R, et al. Measurement and prediction of antimicrobial resistance in bloodstream infections by ESKAPE pathogens and Escherichia coli. J Glob Antimicrob Resist. 2019;19:154–60.
• Ayobami O, Brinkwirth S, Eckmanns T, Markwart R. Antibiotic resistance in hospital-acquired ESKAPE-E infections in low- and lower-middle-income countries: a systematic review and meta-analysis. Emerg Microbes Infect. 2022;11:443–51. A compilation study addressing bacterial co-infections and secondary infections in COVID-19 patients.
• Garcia-Vidal C, Sanjuan G, Moreno-García E, Puerta-Alcalde P, Garcia-Pouton N, Chumbita M, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021;27:83–8. Another compilation study addressing bacterial co-infections and secondary infections in COVID-19 patients.
Ruiz-Garbajosa P, Cantón R. COVID-19: impact on prescribing and antimicrobial resistance. Rev Esp Quimioter. 2021;34(Suppl 1):63–8.
• Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26:1622–9. A meta-analysis containing a data compilation of bacterial infections in COVID-19 patients.
Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81:266–75.
Gaspari R, Spinazzola G, Teofili L, Avolio AW, Fiori B, Maresca GM, et al. Protective effect of SARS-CoV-2 preventive measures against ESKAPE and Escherichia coli infections. Eur J Clin Invest. 2021;51: e13687.
• Poyil MM. Prevalence of co-infections with ESKAPE pathogens in COVID-19 patients: a review. Ann Phytomedicine-an Int J. 2021;S188–94. Another study on bacterial infections on COVID-19 patients, this time addressing the prevalence of ESKAPE pathogens.
Lucien MAB, Canarie MF, Kilgore PE, Jean-Denis G, Fénélon N, Pierre M, et al. Antibiotics and antimicrobial resistance in the COVID-19 era: perspective from resource-limited settings. Int J Infect Dis. 2021;104:250–4.
Timbrook TT, Hueth KD, Ginocchio CC. Identification of bacterial co-detections in COVID-19 critically Ill patients by BioFire® FilmArray® pneumonia panel: a systematic review and meta-analysis. Diagn Microbiol Infect Dis. 2021;101: 115476.
Adeiza SS, Shuaibu AB, Shuaibu GM. Random effects meta-analysis of COVID-19/S. aureus partnership in co-infection. GMS Hyg Infect Control. 2020;15:Doc29.
Musuuza JS, Watson L, Parmasad V, Putman-Buehler N, Christensen L, Safdar N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: a systematic review and meta-analysis. PLoS ONE. 2021;16: e0251170.
Liu L, Nimkar A, Nava C, Hambardzumyan A, Romano C, Mandel M, et al. Massive spontaneous pleural effusion in end-stage renal disease patient with vancomycin resistant enterococcus empyema and covid-19 infection. Chest. 2021;160:A1362–3.
Fidelis L da S, Leme EFP. Perfil das infecções de corrente sanguínea em pacientes hospitalizados por covid-19. Braz J Infect Dis. 2022;26:101811.
Toc DA, Butiuc-Keul AL, Iordache D, Botan A, Mihaila RM, Costache CA, et al. Descriptive analysis of circulating antimicrobial resistance genes in vancomycin-resistant Enterococcus (VRE) during the COVID-19 pandemic. Biomedicines. Multidisciplinary Digital Publishing Institute. 2022;10:1122.
Pinheiro K de S, Pereira MLS, Gonçalves SS, Santana B, Valéria dos Santos K. Evolução da concentração inibitória mínima de vancomicina em staphylococcus aureus isolados de hemocultura em um hospital público referência para covid-19 no espírito santo. Braz J Infect Dis. 2022;26:101750.
Gaspar GG, Bollela VR, Martinez R. Incidência de infecções relacionadas à saúde e perfil de sensibilidade de staphylococcus aureus, klebsiella pneumoniae e acinetobacter baumannii no período pré e durante a pandemia de covid-19 em unidade de terapia intensiva adulto. Braz J Infect Dis. 2021;25: 101062.
Yildirim Arslan S, Sahbudak Bal Z, Guner Ozenen G, Bilen NM, Kurugol Z, Ozkinay F. Cervical abscess caused by methicillin-susceptible Staphylococcus aureus in an infant infected with SARS-CoV-2: Diagnostic dilemma. J Infect Chemother. 2021;27:1092–6.
Loftus MJ, Young-Sharma TEMW, Wati S, Badoordeen GZ, Blakeway LV, Byers SMH, et al. Epidemiology, antimicrobial resistance and outcomes of Staphylococcus aureus bacteraemia in a tertiary hospital in Fiji: a prospective cohort study. The Lancet Regional Health - Western Pacific. 2022;22: 100438.
Wu M, Zou Z-Y, Chen Y-H, Wang C-L, Feng Y-W, Liu Z-F. Severe COVID-19-associated sepsis is different from classical sepsis induced by pulmonary infection with carbapenem-resistant klebsiella pneumonia (CrKP). Chin J Traumatol. 2022;25:17–24.
Ahmed OB, Asghar AH, Bahwerth FS. Increasing frequency of aminoglycoside-resistant Klebsiella pneumoniae during the era of pandemic COVID-19. Materials Today: Proceedings [Internet]. 2021 [cited 2022 May 27]; Available from: https://www.sciencedirect.com/science/article/pii/S2214785321039432
Cunha AKB, Gomes RS, Vasconcellos LAR, Viana MN, de Figueiredo VSR, de Souza LS, et al. Surto de klebsiella pneumoniae resistente aos carbapenêmicos em unidade de terapia intensiva (uti) adulto destinada a internação de pacientes com covid-19 em hospital privado em salvador (ba). Braz J Infect Dis. 2022;26: 101955.
Birssi EC, de Mattos Andriato P, Shinohara DR, Altafini DD, Albiero J, Mitsugui CS, et al. Avaliação do uso de antibacterianos no tratamento de infecção por klebsiella pneumoniae produtora de carbapenemase (cb-kp) em pacientes com covid-19 atendidos em uma unidade de terapia intensiva (uti-covid). Braz J Infect Dis. 2022;26:101741.
Gottesman T, Fedorowsky R, Yerushalmi R, Lellouche J, Nutman A. An outbreak of carbapenem-resistant Acinetobacter baumannii in a COVID-19 dedicated hospital. Infect Prevent Pract. 2021;3:100113.
de Souza ÂC, Giordani L, Rodrigues GM, Barth PO, Cavatão FG, Azevedo A dos S, et al. Impacto da pandemia de covid-19 na concentração inibitória mínima para polimixina b em isolados de acinetobacter baumannii resistentes aos carbapenêmicos: experiência de um hospital terciário. Braz J Infect Dis. 2022;26:102244.
Kalenchic TI, Kabak SL, Primak SergeyV, Melnichenko YM, Kudelich OA. Bilateral parapneumonic pleural effusion with pneumothorax in a patient with covid 19 pneumonia: case report. Radiol Case Rep. 2022;17:869–74.
Reyes LF, Rodriguez A, Bastidas A, Parra-Tanoux D, Fuentes YV, García-Gallo E, et al. Dexamethasone as risk-factor for ICU-acquired respiratory tract infections in severe COVID-19. J Crit Care. 2022;69: 154014.
Vieira CCAR, de Mendonça HSL, Reis AT, de Oliveira LPA, Paiva PB, Costa NDVL, et al. Perfil de resistência de pseudomonas aeruginosa em uma unidade pública materno-infantil na pandemia da covid-19. Braz J Infect Dis. 2022;26: 101761.
Danda GJ da N. Espondilodiscite por pseudomonas aeruginosa multirresistente pós-covid-19 tratado com ceftazidima-avibactam. Braz J Infect Dis. 2022;26:101749.
Silva LM, Calich L, Cunha EQ, Cunha MA. Surto de colonização/infecção por pseudomonas aeruginosa em uti de pacientes com covid-19: descrição de casos e medidas adotadas. Braz J Infect Dis. 2021;25: 101369.
de Macedo V, Santos GS, Silva RN, Couto CNM, Bastos C, Viecelli E, et al. Healthcare-associated infections: a threat to the survival of patients with COVID-19 in intensive care units. J Hospital Infect [Internet]. 2022 [cited 2022 May 27]; Available from: https://www.sciencedirect.com/science/article/pii/S0195670122001645
Karami Z, Knoop BT, Dofferhoff ASM, Blaauw MJT, Janssen NA, van Apeldoorn M, et al. Few bacterial co-infections but frequent empiric antibiotic use in the early phase of hospitalized patients with COVID-19: results from a multicentre retrospective cohort study in The Netherlands. Infect Dis (Lond). 2021;53:102–10.
Klein EY, Monteforte B, Gupta A, Jiang W, May L, Hsieh Y-H, et al. The frequency of influenza and bacterial co-infection: a systematic review and meta-analysis. Influenza Other Respir Viruses. 2016;10:394–403.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62.
Firth A, Prathapan P. Azithromycin: the first broad-spectrum therapeutic. Eur J Med Chem. 2020;207: 112739.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China The Lancet Elsevier. 2020;395:497–506.
Beović B, Doušak M, Ferreira-Coimbra J, Nadrah K, Rubulotta F, Belliato M, et al. Antibiotic use in patients with COVID-19: a “snapshot” Infectious Diseases International Research Initiative (ID-IRI) survey. J Antimicrob Chemother. 2020;75:3386–90.
Cherry G, Rocke J, Chu M, Liu J, Lechner M, Lund VJ, et al. Loss of smell and taste: a new marker of COVID-19? Tracking reduced sense of smell during the coronavirus pandemic using search trends. Expert Rev Anti Infect Ther. 2020;18:1165–70.
Pink I, Raupach D, Fuge J, Vonberg R-P, Hoeper MM, Welte T, et al. C-reactive protein and procalcitonin for antimicrobial stewardship in COVID-19. Infection. 2021;49:935–43.
Landry A, Docherty P, Ouellette S, Cartier LJ. Causes and outcomes of markedly elevated C-reactive protein levels. Can Fam Physician. 2017;63:e316–23.
Knight GM, Glover RE, McQuaid CF, Olaru ID, Gallandat K, Leclerc QJ, et al. Antimicrobial resistance and COVID-19: intersections and implications. Elife. 2021;10: e64139.
Ukuhor HO. The interrelationships between antimicrobial resistance, COVID-19, past, and future pandemics. J Infect Public Health. 2021;14:53–60.
Maurer FP, Christner M, Hentschke M, Rohde H. Advances in rapid identification and susceptibility testing of bacteria in the clinical microbiology laboratory: implications for patient care and antimicrobial stewardship programs. Infect Dis Rep. 2017;9:6839.
Dryden M, Johnson AP, Ashiru-Oredope D, Sharland M. Using antibiotics responsibly: right drug, right time, right dose, right duration. J Antimicrob Chemother. 2011;66:2441–3.
Finch R. Innovation - drugs and diagnostics. J Antimicrob Chemother. 2007;60(Suppl 1):i79-82.
Vogels CBF, Brito AF, Wyllie AL, Fauver JR, Ott IM, Kalinich CC, et al. Analytical sensitivity and efficiency comparisons of SARS-CoV-2 RT–qPCR primer–probe sets. Nat Microbiol Nature Publishing Group. 2020;5:1299–305.
Prasetyoputri A. Detection of bacterial co-infection in COVID-19 patients is a missing piece of the puzzle in the COVID-19 management in Indonesia. ACS Infect Dis Am Chem Soc. 2021;7:203–5.
Bogdan I, Citu C, Bratosin F, Malita D, Romosan I, Gurban CV, et al. The impact of multiplex PCR in diagnosing and managing bacterial infections in COVID-19 patients self-medicated with antibiotics. Antibiotics. Multidisciplinary Digital Publishing Institute. 2022;11:437.
Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323:1824–36.
Ng TSB, Leblanc K, Yeung DF, Tsang TSM. Medication use during COVID-19: review of recent evidence. Can Fam Physician. 2021;67:171–9.
Chauhan V, Galwankar S, Raina S, Krishnan V. Proctoring hydroxychloroquine consumption for health-care workers in India as per the revised national guidelines. J Emerg Trauma Shock. 2020;13:172–3.
Erku DA, Belachew SA, Abrha S, Sinnollareddy M, Thomas J, Steadman KJ, et al. When fear and misinformation go viral: pharmacists’ role in deterring medication misinformation during the “infodemic” surrounding COVID-19. Res Social Adm Pharm. 2021;17:1954–63.
Kim MS, An MH, Kim WJ, Hwang T-H. Comparative efficacy and safety of pharmacological interventions for the treatment of COVID-19: a systematic review and network meta-analysis. PLoS Med. 2020;17: e1003501.
Quincho-Lopez A, Benites-Ibarra CA, Hilario-Gomez MM, Quijano-Escate R, Taype-Rondan A. Self-medication practices to prevent or manage COVID-19: a systematic review. PLoS ONE. 2021;16: e0259317.
Torres NF, Chibi B, Middleton LE, Solomon VP, Mashamba-Thompson TP. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: a systematic scoping review. Public Health. 2019;168:92–101.
Ferdiana A, Liverani M, Khan M, Wulandari LPL, Mashuri YA, Batura N, et al. Community pharmacies, drug stores, and antibiotic dispensing in Indonesia: a qualitative study. BMC Public Health. 2021;21:1800.
Kotwani A, Holloway K. Trends in antibiotic use among outpatients in New Delhi. India BMC Infect Dis. 2011;11:99.
Zawahir S, Lekamwasam S, Halvorsen KH, Rose G, Aslani P. Self-medication Behavior with antibiotics: a national cross-sectional survey in Sri Lanka. Expert Review of Anti-infective Therapy. Taylor & Francis; 2021;19:1341–52.
Do NTT, Vu HTL, Nguyen CTK, Punpuing S, Khan WA, Gyapong M, et al. Community-based antibiotic access and use in six low-income and middle-income countries: a mixed-method approach. Lancet Glob Health Elsevier. 2021;9:e610–9.
Malik M, Tahir MJ, Jabbar R, Ahmed A, Hussain R. Self-medication during Covid-19 pandemic: challenges and opportunities. Drugs Ther Perspect. 2020;36:565–7.
Nothias L-F, Knight R, Dorrestein PC. Antibiotic discovery is a walk in the park. Proc Natl Acad Sci U S A. 2016;113:14477–9.
Ocan M, Obuku EA, Bwanga F, Akena D, Richard S, Ogwal-Okeng J, et al. Household antimicrobial self-medication: a systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health. 2015;15:742.
Zavala-Flores E, Salcedo-Matienzo J, Zavala-Flores E, Salcedo-Matienzo J. Medicación prehospitalaria en pacientes hospitalizados por COVID-19 en un hospital público de Lima-Perú. Acta Médica Peruana. Colegio Médico del Perú. 2020;37:393–5.
Zhang A, Hobman EV, De Barro P, Young A, Carter DJ, Byrne M. Self-medication with antibiotics for protection against COVID-19: the role of psychological distress, knowledge of, and experiences with antibiotics. Antibiotics (Basel). 2021;10:232.
Acknowledgements
G.P.J. is supported by Departamento Administrativo de Ciencia, Tecnologia e Innovacion, grant number 2016/772. I.C.R.S.G. is supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, grant number 88887.516158/2020-00. M.T.P.G. is supported by Fulbright-CAPES, grant number 88881.625374/2021-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any conflict of interest to disclose.
Human and Animal Rights and Informed Consent
This study does not contain studies with human or animal subjects performed by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Healthcare Associated Infections
The original online version of this article was updated to display correctly the name of the first author, 'Genesy Pérez Jorge'.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pérez Jorge, G., Rodrigues dos Santos Goes, I. & Gontijo, M.T.P. Les misérables: a Parallel Between Antimicrobial Resistance and COVID-19 in Underdeveloped and Developing Countries. Curr Infect Dis Rep 24, 175–186 (2022). https://doi.org/10.1007/s11908-022-00788-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-022-00788-z