Abstract
Purpose of Review
Resistant hypertension is diagnosed if the blood pressure (BP) is not controlled despite optimum doses of 3 first-line classes of antihypertensive drugs including a thiazide diuretic or if adequate BP control needs 4 or more antihypertensive drugs from different classes.
Recent Findings
Pseudohypertension and white coat hypertension must be excluded. Poor patient compliance, inadequate doses of antihypertensive drugs, poor office BP measurement technique, and having to pay for costs of drugs are factors associated with pseudoresistant hypertension. Secondary hypertension must be excluded and treated. Therapy of resistant hypertension includes improving compliance with use of medication, detection, and treatment of secondary hypertension, use of lifestyle measures, and treatment of obesity and other comorbidities. Switching the patient from hydrochlorothiazide to a longer acting thiazide-type diuretic such as chlorthalidone may improve BP control. The beneficial effects of thiazide diuretics are reduced when the glomerular filtration rate is reduced to less than 40 mL/min/1.73 m2. These patients should be treated with a loop diuretic such as furosemide every 12 h. If a fourth antihypertensive drug is needed to control blood pressure in persons treated with adequate doses of antihypertensive drugs from different classes including a thiazide-type diuretic, a mineralocorticoid receptor antagonist should be added to the therapeutic regimen. Further research is needed on investigational drugs and device therapy for treating resistant hypertension.
Summary
Clinical trials are indicated for the treatment of resistant hypertension by sacubitril/valsartan and also by firibastat.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The 2017 American College of Cardiology (ACC)/American Heart Association (AHA) hypertension guidelines reported that stage 1 hypertension is a systolic blood pressure of 130–139 mmHg or a diastolic blood pressure of 80–89 mmHg [1••]. Stage 2 hypertension is a systolic blood pressure of 140 mmHg and higher or a diastolic blood pressure of 90 mmHg and higher [1••]. These hypertension guidelines recommend lifestyle measures plus blood pressure-lowering drugs for secondary prevention of recurrent cardiovascular disease events in persons with clinical cardiovascular disease (coronary heart disease, congestive heart failure, and stroke) and an average systolic blood pressure of 130 mmHg and higher or an average diastolic blood pressure of 80 mmHg and higher [1••, 2, 3]. The prevalence of resistant hypertension has increased with these new guidelines. These guidelines recommend lifestyle measures plus blood pressure-lowering drugs for primary prevention of cardiovascular disease in persons with an estimated 10-year risk of atherosclerotic cardiovascular disease ≥ 10% [4] and an average systolic blood pressure of 130 mmHg and higher or an average diastolic blood pressure of 80 mmHg and higher [1••, 5]. These guidelines recommend lifestyle measures plus blood pressure-lowering drugs for primary prevention of cardiovascular disease in persons with an estimated 10-year risk of atherosclerotic cardiovascular disease of < 10% [4] and an average systolic blood pressure of 140 mmHg and higher or an average diastolic blood pressure of 90 mmHg and higher [1••, 5, 6]. These guidelines recommend treatment with antihypertensive drug therapy with 2 first-line drugs from different classes either as separate agents or in a fixed-dose combination in persons with a blood pressure of 140/90 mmHg and higher or with a blood pressure more than 20/10 mmHg above their blood pressure target [1••, 6]. White coat hypertension must be excluded before using antihypertensive drugs in persons with hypertension at low risk for atherosclerotic cardiovascular disease [1••].
Secondary hypertension should be suspected if there is new onset or uncontrolled hypertension in adults [1••, 7]. Screen for secondary hypertension if there is drug-resistant/induced hypertension, abrupt onset of hypertension, onset of hypertension in a person younger than 30 years or later after 50 years, exacerbation of previously controlled hypertension, disproportionate target organ damage for the degree of hypertension, accelerated/malignant hypertension, onset of diastolic hypertension in older persons, or unprovoked or excessive hypokalemia [1••, 7]. Common causes of secondary hypertension include renal parenchymal disease, renovascular disease, primary aldosteronism, obstructive sleep apnea, and drug- or alcohol-induced hypertension [1••]. Uncommon causes of secondary hypertension include pheochromocytoma/paraganglioma, Cushing’s syndrome, hypothyroidism, hyperthyroidism, aortic coarctation, primary hyperparathyroidism, congenital adrenal hyperplasia, mineralocorticoid excess syndromes, and acromegaly [1••].
The 2017 ACC/AHA hypertension guidelines recommend that the blood pressure should be lowered to less than 130/80 mmHg in persons with ischemic heart disease [1••, 3, 8,9,10,11,12,13], in persons with heart failure with a decreased left ventricular ejection fraction [1••, 14], in persons with heart failure with a preserved left ventricular ejection fraction [1••, 14], in persons with chronic kidney disease [1••, 15], in persons after renal transplantation [1••], in persons with lacunar stroke [1••, 16, 17], in persons with peripheral arterial disease [1••, 2], in persons with diabetes mellitus [1••, 18,19,20,21], in noninstitutionalized ambulatory community-dwelling persons older than 65 years of age [1••, 8, 9], and for secondary stroke prevention [1••, 22].
Lifestyle Measures
Lifestyle modification should be used in the treatment of hypertension [1••, 23••]. Weight reduction, consuming a diet rich in fruits, vegetables, and low-fat dairy products with less saturated fat and total fat, sodium reduction to not exceed 1.5 g daily, smoking cessation, regular aerobic physical activity, avoidance of excessive alcohol intake, avoidance of excessive caffeine, and avoidance of drugs which can increase blood pressure, including nonsteroidal anti-inflammatory drugs, glucocorticoids, and sympathomimetics, are recommended [1••, 6, 23••, 24].
Drug Treatment of Primary Hypertension
The 2017 ACC/AHA hypertension guidelines recommend for white and other non-black persons younger than 60 years of age with primary hypertension, the first antihypertensive drug should be an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, the second drug a thiazide diuretic (preferably chlorthalidone) or a calcium channel blocker, and if a third antihypertensive drug is needed, an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker plus a thiazide diuretic plus a calcium channel blocker should be administered [1••]. For white and other non-black persons aged 60 years of age and older with primary hypertension, the first antihypertensive drug should be a thiazide diuretic (preferably chlorthalidone) or a calcium channel blocker, and if a third antihypertensive drug is required, a thiazide diuretic plus a calcium channel blocker plus an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker should be administered [1••]. For African-Americans with primary hypertension, the first antihypertensive drug should be a thiazide diuretic (preferably chlorthalidone) or a calcium channel blocker, and if a third antihypertensive drug is needed, a thiazide diuretic plus a calcium channel blocker plus an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker should be administered [1••].
Drug Treatment of Hypertension Associated with Comorbidities
Patients with stable ischemic heart disease and hypertension should be treated with a beta blocker plus an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, and if a third antihypertensive drug is needed, a beta blocker plus an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker plus a thiazide diuretic or a calcium channel blocker should be administered [1••, 25••, 26,27,28,29,30,31,32,33]. If a fourth antihypertensive drug is needed to adequately control hypertension, a mineralocorticoid receptor antagonist should be added [1••]. In patients with stable ischemic heart disease who have angina pectoris despite beta blocker therapy and persistent uncontrolled hypertension, a dihydropyridine calcium channel blocker should be added [1••, 25••, 26, 34]. Beta blockers which should be administered in treating ischemic heart disease with hypertension include carvedilol, metoprolol tartrate, metoprolol succinate, bisoprolol, nadolol, propranolol, and timolol [1••]. Atenolol should not be given [1••, 28]. Nondihydropyridine calcium channel blockers such as verapamil and diltiazem are contraindicated if there is left ventricular systolic dysfunction [1••]. If there is left ventricular systolic dysfunction, the beta blockers that should be administered are carvedilol, metoprolol succinate, or bisoprolol [1••, 25••, 26, 35].
If hypertension persists after treatment with a beta blocker plus an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker in patients with an acute coronary syndrome, a long-acting dihydropyridine calcium channel blocker should be added to the therapeutic regimen [26]. Aldosterone antagonists should be administered to patients treated with beta blockers plus angiotensin-converting enzyme inhibitors or angiotensin receptor blockers after myocardial infarction who have left ventricular systolic dysfunction and either heart failure or diabetes mellitus if their serum potassium is less than 5.0 meq/L and if their serum creatinine is ≤ 2.5 mg/dL in men and ≤ 2.0 mg/dL in women [1••, 25••, 26, 36].
Patients with hypertension who have heart failure with a decreased left ventricular ejection fraction should be treated with a beta blocker (carvedilol, metoprolol succinate, or bisoprolol) plus an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker or preferably an angiotensin receptor-neprilysin inhibitor plus a diuretic and if indicated with a mineralocorticoid receptor antagonist [1••, 14, 25••, 26, 28, 36]. Nondihydropyridine calcium channel blockers are contraindicated in patients with heart failure and a decreased left ventricular ejection fraction [1••, 14, 25••, 26, 37, 38].
Patients with hypertension and heart failure with a preserved left ventricular ejection fraction should have their volume overload treated with diuretics, their other comorbidities treated, and their hypertension treated with a beta blocker plus an angiotensin-converting enzyme inhibitor or angiotensin blocker plus a mineralocorticoid receptor antagonist [1••, 14, 39, 40].
Patients with hypertension and chronic kidney disease stage 3 or higher or stage 1 or 2 chronic kidney disease with albuminuria ≥ 300 mg per day should be treated with an angiotensin-converting enzyme inhibitor to slow progression of chronic kidney disease [1••, 41]. If an angiotensin-converting enzyme inhibitor is not tolerated, these patients should be treated with an angiotensin receptor blocker [1••]. Patients with stage 1 or 2 chronic kidney disease who do not have albuminuria may be treated with usual first-line antihypertensive drugs [1••]. If 3 antihypertensive drugs are necessary, these patients should be treated with an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker plus a thiazide diuretic plus a calcium channel blocker. After kidney transplantation, treat hypertension with a calcium channel blocker to improve glomerular filtration rate and kidney survival [1••].
Patients with hypertension and a prior stroke or transient ischemic attack should receive treatment with a thiazide diuretic or angiotensin-converting enzyme or angiotensin receptor blocker [1••, 42]. If a third antihypertensive drug is needed, these patients should be treated with a thiazide diuretic plus an angiotensin-converting enzyme or angiotensin receptor blocker plus a calcium channel blocker.
Patients with hypertension and peripheral arterial disease should be treated with an angiotensin-converting enzyme or angiotensin receptor blocker or a calcium channel blocker or thiazide diuretic or beta blocker [1••, 43]. There is no evidence that any one class of antihypertensive drugs is superior to treat hypertension in patients with peripheral arterial disease [1••, 43].
Thiazide diuretics, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers are effective antihypertensive drugs in patients with hypertension and diabetes mellitus and may be used as initial therapy [1••, 44]. Angiotensin-converting enzymes or angiotensin receptor blockers should be used for treating diabetics with hypertension and persistent albuminuria [1••, 45]. Chlorthalidone was better than lisinopril, amlodipine, and doxazosin in reducing cardiovascular disease and renal outcomes in nondiabetics with hypertension and the metabolic syndrome [1••, 46].
Beta blockers are the preferred antihypertensive drugs in patients with hypertension and thoracic aortic aneurysm [1••, 47]. Beta blockers also improve survival in adults with type A and with type B acute and chronic thoracic aortic dissection [1••]. If thoracic aorta dissection develops, beta blockers are the initial drug of choice for reducing blood pressure, ventricular rate, dP/dt, and stress on the aorta [47, 48]. Systolic blood pressure should be lowered to 100 to 120 mmHg and the ventricular rate decreased to less than 60 beats/min by intravenous propranolol, metoprolol, labetalol, or esmolol [47, 48, 49••].
Pregnant women with hypertension should not receive treatment with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, direct renin inhibitors, or atenolol because these drugs are fetotoxic [1••]. Pregnant women with hypertension should be treated with methyldopa, nifedipine, and/or labetalol [1••].
Treatment-Resistant Hypertension
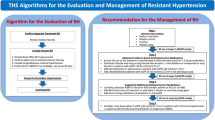
Resistant hypertension is diagnosed if the blood pressure is not controlled despite optimum doses of 3 first-line classes of antihypertensive drugs including a thiazide diuretic or if adequate blood pressure control needs 4 or more antihypertensive drugs from different classes [1••, 49••, 50, 51]. The National Institute for Health ad Clinical Excellence guideline suggests that the 3 drugs should be an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker plus a calcium channel blocker plus a thiazide-type diuretic [51]. Pseudohypertension and white coat hypertension must be excluded.
Pseudohypertension in the elderly is a falsely high systolic blood pressure which results from markedly sclerotic arteries which do not collapse under the blood pressure cuff [1••, 25••]. Pseudohypertension can be confirmed by measuring intra-arterial pressure [1••, 25••]. White coat hypertension is diagnosed in persons with persistently elevated office blood pressure but normal home blood pressure or normal 24-h ambulatory blood pressure [1••, 25••]. Poor patient compliance, inadequate doses of antihypertensive drugs, poor office blood pressure measurement technique, and having to pay for costs of drugs are factors associated with pseudoresistant hypertension [1••, 25••, 52].
Factors contributing to resistant hypertension include obesity, a high-sodium, low-fiber diet, excess alcohol intake, physical inactivity, obstructive sleep apnea, use of cocaine, amphetamines, nonsteroidal anti-inflammatory drugs, oral contraceptive hormones, adrenal steroid hormones, sympathomimetic drugs (nasal decongestants and diet pills), erythropoietin, licorice, herbal supplements such as ephedra, progressive renal insufficiency, and inadequate diuretic therapy [1••, 25••, 51, 53].
Persons with resistant hypertension also need to be screened for secondary causes of hypertension with treatment of these secondary causes [1••, 25••]. Lifestyle measures as previously discussed must be instituted [1••, 6, 23••].
Among 205,750 patients with incident hypertension, 1.9%, mean age 60.6 years, developed resistant hypertension within a median of 1.5 years from initial treatment [54]. Over 3.8 years median follow-up, cardiovascular events were 47% (33 to 62%) higher in those with resistant hypertension [54]. In 53,380 patients with hypertension and atherothrombotic disease in the International Reduction of Atherothrombosis for Continued Health (REACH) registry, the prevalence of resistant hypertension was 12.7% with 4.6% receiving 4 antihypertensive drugs and 1.9% receiving 5 or more antihypertensive drugs [55]. Those with resistant hypertension had at 4 years follow-up a higher incidence of cardiovascular death or myocardial infarction, or stroke and a higher incidence of hospitalization for congestive heart failure [55]. Of 614 patients with hypertension followed in a university cardiology or general medicine clinic, 40 patients (7%) were receiving 4 antihypertensive drugs, and 9 patients (1%) were receiving 5 antihypertensive drugs [52]. Of 14,684 patients with hypertension in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) randomized to chlorthalidone, amlodipine, or lisinopril, 9.6%, 11.4%, and 19.7%, respectively, had treatment-resistant hypertension [56]. The 2018 AHA Scientific Statement on resistant hypertension [57••] stated that the prevalence of treatment-resistant hypertension among 4158 US persons with hypertension taking antihypertensive drugs in the 2009 to 2014 National Health and Nutrition Examination Survey was 17.7% using the criteria for diagnosis stated in their 2008 statement [49••] and 19.7% using the criteria for diagnosis recommended by the 2017 ACC/AHA hypertension guidelines [1••]. Using the 2018 definition [1••, 57••], 3.2% of US adults taking chlorthalidone or indapamide and 9.0% taking spironolactone or eplerenone had resistant hypertension.
Therapy of resistant hypertension includes improving compliance with use of medication, detection, and treatment of secondary hypertension, use of lifestyle measures, and treatment of obesity and other comorbidities [1••, 23••]. If a fourth antihypertensive drug is needed to control blood pressure in persons treated with adequate doses of antihypertensive drugs from different classes including a thiazide-type diuretic, a mineralocorticoid receptor antagonist should be added to the therapeutic regimen [1••, 50].
Patient nonadherence to both lifestyle measures and antihypertensive drug therapy is a major factor for treatment-resistant hypertension [58,59,60,61,62,63]. Methods for assessment of patient nonadherence to antihypertensive drug therapy include clinical impression, questioning of the patient, self-reports, pill counts, refill records, electronic bottle cap monitoring, and measuring concentrations of prescribed antihypertensive drugs in blood and urine [58,59,60,61,62,63]. The prevalence of nonadherence to antihypertensive drug therapy in patients with treatment-resistant hypertension in a pooled analysis of 24 studies was 31.2% [64••].
The prevalence of nonadherence to antihypertensive drug therapy in patients with treatment-resistant hypertension varies from 20.3 to 41.1% depending on the assessment method used [65, 66••]. In a study of 76 patients with treatment-resistant hypertension prescribed at least 4 antihypertensive drugs who had urine screening for nonadherence, 40 patients (53%) were found to be non-adherent to taking their antihypertensive drugs [63]. Of these 40 patients, 30% had complete adherence and 70% had incomplete adherence to their antihypertensive drugs [63]. An analysis of 62 trials showed that interventions that may improve adherence to self-administered antihypertensive drugs include policy interventions to reduce drug copayments or improve prescription drug coverage, system interventions to offer case management, and patient-level educational interventions with behavioral support [60].
Drug Treatment of Resistant Hypertension
Drug treatment of resistant hypertension should maximize diuretic therapy [1••, 25••]. Excess sodium and fluid retention is an important cause of resistant hypertension [49••, 66••, 67]. Switching the patient from hydrochlorothiazide to a longer acting thiazide-type diuretic such as chlorthalidone may improve blood pressure control [1••, 68]. The beneficial effects of thiazide diuretics are reduced when the glomerular filtration rate is reduced to less than 40 cc/min [1••, 25••, 49••, 66••, 69]. These patients should be treated with a loop diuretic such as furosemide every 12 h [1••, 25••, 66••].
Increased activation of the renin-angiotensin-aldosterone system also plays an important role in the development of treatment-resistant hypertension [66••, 67, 70••]. Low-dose eplerenone has also been found to reduce aortic stiffness in patents with resistant hypertension [71]. The available data support the use of mineralocorticoid receptor antagonist such as spironolactone or eplerenone as the fourth antihypertensive drug to prescribe in patients with treatment-resistant hypertension [1••, 25••, 51, 66••, 67, 70••, 71, 72••, 73,74,75,76,77]. In the PATHWAY-2 trial, spironolactone was superior to placebo, bisoprolol, and doxazosin in the treatment of drug-resistant hypertension [74].
The patient should receive appropriate antihypertensive drugs for their comorbidities as discussed earlier in this review. For example, patients with coronary heart disease or heart failure should be treated with beta blockers. If additional antihypertensive drug therapy is indicated, centrally active alpha agonists such as clonidine or methyldopa or direct vasodilators such as hydralazine and minoxidil are further options [1••, 25••, 51, 77].
A pooled analysis of 14,094 patients treated for hypertension in the Systolic Blood Pressure Intervention Trial and the Action to Control Cardiovascular Risk in Diabetes trial showed that 2710 patients (19.2%) had resistant hypertension [78••]. The optimal systolic blood pressure goal for reducing the outcome of myocardial infarction, stroke, cardiovascular death, and heart failure and the same outcomes plus all-cause mortality in patients with and without resistant hypertension was less than 120 mmHg [78••].
Investigational Drugs for Resistant Hypertension
Investigational drugs for treatment of resistant hypertension include aldosterone synthase inhibitors, activators of the angiotensin-converting enzyme 2/angiotensin (1-7)/MAS receptor axis, centrally acting aminopeptidase inhibitors, vasopeptidase inhibitors, dual-acting angiotensin receptor-neprilysin inhibitors, dual-acting endothelin-converting enzyme-neprilysin inhibitors, natriuretic peptide receptor agonists, soluble epoxide hydrolase inhibitors, vasoactive intestinal peptide receptor agonists, intestinal Na+/H+ exchanger 3 inhibitors, and dopamine beta-hydroxylase inhibitors and are discussed elsewhere [70••, 79,80,81]. None of these investigational drugs has been approved in the USA for treatment of resistant hypertension.
Sacubitril/valsartan was demonstrated in a double-blind, randomized controlled trial to be superior to olmesartan in reducing clinic and ambulatory central aortic and brachial pressures in 454 patients, mean age 67.7 years, with systolic hypertension and stiff arteries [82]. A meta-analysis of 11 randomized controlled trials in 6028 participants found that sacubitril/valsartan was more effective than angiotensin receptor antagonists for the management of patients with hypertension [81]. Sacubitril/valsartan merits investigation of treatment of resistant hypertension [82,83,84].
A phase 2, open-label, multicenter, dose-titrating study in 256 overweight or obese hypertensive patients (56% black or Hispanic) showed that firibastat, a first-in-class brain aminopeptidase A inhibitor, was effective in lowering blood pressure [85]. Firibastat should be investigated for the treatment of resistant hypertension.
Device Therapy for Drug-Resistant Hypertension
Device therapy under investigation for drug-resistant hypertension includes radiofrequency sympathetic denervation of the renal arteries, baroreflex activation therapy, carotid body ablation, a central arteriovenous anastomosis, carotid artery ablation, and neurovascular decompression [70••, 79, 86,87,88,89,90,91,92,93]. None of these devices has been approved for treatment of resistant hypertension in the USA. The novel device of greatest interest under investigation is sympathetic denervation of the renal arteries [86,87,88,89,90,91]. A sham-controlled trial of renal artery denervation in 535 patients with resistant hypertension showed no significant reduction in systolic blood pressure 6 months after renal artery denervation compared with the sham procedure [86]. This trial also did not show a benefit of renal artery denervation on reduction in ambulatory blood pressure in either the 24-h or day and night periods 6 months after the procedure compared with the sham procedure [87]. However, an analysis of 6 trials with 977 patients suggested a benefit in reducing blood pressure by this procedure [91]. The 2017 ACC/AHA hypertension guidelines do not recommend any device therapy for treatment of resistant hypertension [1••]. These guidelines state that 2 randomized controlled trials of renal sympathetic nerve ablation have been negative [1••, 86, 87, 94••].
Conclusion
Despite advances in this important area, resistant hypertension still presents significant challenges for appropriate diagnosis and management. White coat hypertension and pseudohypertension must be excluded before diagnosing resistant hypertension. Poor patient compliance, inadequate doses of antihypertensive drugs, poor office blood pressure measurement technique, and having to pay for costs of drugs are factors associated with pseudoresistant hypertension. Secondary hypertension must be excluded and treated. Primary hypertension and hypertension associated with different comorbidities must be treated as recommended by the 2017 ACC/AHA hypertension guidelines. Factors contributing to resistant hypertension include obesity, a high-sodium, low-fiber diet, excess alcohol intake, physical inactivity, obstructive sleep apnea, use of cocaine, amphetamines, nonsteroidal anti-inflammatory drugs, oral contraceptive hormones, adrenal steroid hormones, sympathomimetic drugs (nasal decongestants and diet pills), erythropoietin, licorice, herbal supplements such as ephedra, progressive renal insufficiency, and inadequate diuretic therapy. Patient nonadherence to both lifestyle measures and antihypertensive drug therapy are major factors for treatment-resistant hypertension. Therapy of resistant hypertension includes improving compliance with use of medication, detection, and treatment of secondary hypertension, use of lifestyle measures, and treatment of obesity and other comorbidities. Switching the patient from hydrochlorothiazide to a longer acting thiazide-type diuretic such as chlorthalidone may improve blood pressure control. The beneficial effects of thiazide diuretics are reduced when the glomerular filtration rate is reduced to less than 40 mL/min/1.73 m2. These patients should be treated with a loop diuretic such as furosemide every 12 h. If a fourth antihypertensive drug is needed to control blood pressure in persons treated with adequate doses of antihypertensive drugs from different classes including a thiazide-type diuretic, a mineralocorticoid receptor antagonist should be added to the therapeutic regimen. Further research is needed on investigational drugs and device therapy for treating resistant hypertension. Clinical trials are indicated for the treatment of resistant hypertension by sacubitril/valsartan and also by firibastat.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Coillins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH ASPC/NMA/PCNA guideline for the prevention, detection, evaluation and management of high blood pressure in adults. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–248 These guidelines discuss the management of resistant hypertension.
Thompson AM, Hu T, Eshelbrenner CL, Reynolds K, He J, Bazzano LA. Antihypertensive treatment and secondary prevention of cardiovascular disease events among persons without hypertension: a meta-analysis. JAMA. 2011;305:913–22.
Czernichow S, Zanchetti A, Turnbull F, Barzi F, Ninomiya KAP, et al. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. J Hypertens. 2011;29:4–16.
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB Sr, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–59.
Blood Pressure-Lowering Treatment Trialists’ Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384:591–8.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 Report. JAMA. 2003;289:2560–72.
Chiong JR, Aronow WS, Khan IA, Nair CK, Vijayaraghavan K, Dart RA, et al. Secondary hypertension : current diagnosis and treatment. Int J Cardiol. 2008;124:6–21.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years. A randomized clinical trial. JAMA. 2016;315:2673–82.
Bundy JD, Li C, Stuchlik P, Bu X, Kelly TN, Mills KT, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017;2:775–81.
Oparil S, Lewis CE. Should patients with cardiovascular risk factors receive intensive treatment of hypertension to <120/80 mm target? A protagonist view from the SPRINT trial (Systolic Blood Pressure Intervention trial). Circulation. 2016;134:1308–10.
Aronow WS. Managing hypertension in the elderly: what is different, what is the same? Curr Hypertens Rep. 2017;19:67. https://doi.org/10.1007/s11906-017-0764-8.
Rochlani Y, Khan MH, Aronow WS. Managing hypertension in patients aged 75 years and older. Curr Hypertens Rep. 2017;19:88. https://doi.org/10.1007/s11906-017-0785-3.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure. A report of the American College of Cardiology /American Heart Association Task Force on clinical Practice Guidelines and the Heart Failure Society of America. Developed in collaboration with the American Academy of Family Physicians, the American College of Chest Physicians, and International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2017;70:776–803.
Upadhyay A, Earley A, Haynes SM, Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Ann Intern Med. 2011;154:541–8.
SPS3 Study Group, Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet 2013; 382: 507–515.
Oparil S. SPS3 evidence supports intensive blood pressure control. Circulation. 2016;133:552–4.
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313:603–15.
Margolis KL, O'Connor PJ, Morgan TM, Buse JB, Cohen RM, Cushman WC, et al. Outcomes of combined cardiovascular risk factor management strategies in type 3 diabetes: the ACCORD randomized trial. Diabetes Care. 2014;37:1721–8.
Soliman EZ, Byington RP, Bigger JT, Evans G, Okin PM, Goff DC Jr, et al. Effect of intensive blood pressure lowering on left ventricular hypertrophy in patients with diabetes mellitus: Action to Control Cardiovascular Risk in Diabetes Blood Pressure Trial. Hypertension. 2015;66:1123–9.
Aronow WS. Orthostatic hypotension in diabetics in the ACCORD (Action to Control Cardiovascular Risk in Diabetes) blood pressure trial. Hypertension. 2016;68:851–2.
Wang WT, You LK, Chiang CE, Sung SH, Chuang SY, Cheng HM, et al. Comparative effectiveness of blood pressure-lowering drugs in patients who have already suffered from stroke: traditional and Bayesian network meta-analysis of randomized trials. Medicine. 2016;95:e3302.
•• Aronow WS. Lifestyle measures for treating hypertension. Arch Med Sci. 2017;13:1241–3 This paper discusses lifestyle measures for treating hypertension.
Ojji DB, Mayosi B, Francis V, Badri M, Cornelius V, Smythe W, et al. Comparison of drug therapies for lowering blood pressure in black Africans. N Engl J Med. 2019;380:2429–39.
•• Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57:2037–114 These guidelines discuss management of resistant hypertension.
Rosendorff C, Lackland DT, Allison M, Aronow WS, Black HR, Blumenthal RS, et al. AHA/ACC/ASH scientific statement. Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. J Am Coll Cardiol. 2015;65:1998–2038.
Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. https://doi.org/10.1136/bmj.b1665.
Aronow WS. Current role of beta blockers in the treatment of hypertension. Expert Opin Pharmacother. 2010;11:2599–607.
The CAPRICORN Investigators. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001;357:1385–90.
Freemantle N, Cleland J, Young P, Mason J, Harrison J. Beta blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318:1730–7.
HOPE (Heart Outcomes Prevention Evaluation) Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342:145–53.
The European trial on reduction of cardiac events with perindopril in stable coronary artery disease investigators. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study). Lancet. 2003;362:782–8.
Pfeffer MA, Braunwald E, Moye LA, Basta L, Brown EJ Jr, Cuddy TE, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the Survival and Ventricular Enlargement Trial. N Engl J Med. 1992;327:669–77.
Leon MB, Rosing DR, Bonow RO, Lipson LC, Epstein SE. Clinical efficacy of verapamil alone and combined with propranolol in treating patients with chronic stable angina pectoris. Am J Cardiol. 1981;48:131–9.
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease:2011 update. A guideline from the American Heart Association and American College of Cardiology Foundation. Endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58:2432–46.
Pitt B, White H, Nicolau J, Martinez F, Gheorghiade M, Aschermann M, et al. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol. 2005;46:425–31.
Elkayam U, Amin J, Mehra A, Vasquez J, Weber L, Rahimtoola SH. A prospective, randomized, double-blind, crossover study to compare the efficacy and safety of chronic nifedipine therapy with that of isosorbide dinitrate and their combination in the treatment of chronic congestive heart failure. Circulation. 1990;82:1954–61.
Goldstein RE, Boccuzzi SJ, Cruess D, Nattel S. Diltiazem increases late-onset congestive heart failure in postinfarction patients with early reduction in ejection fraction. Circulation. 1991;83:52–60.
Aronow WS, Ahn C, Kronzon I. Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or = 40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol. 1997;80:207–9.
Pfeffer MA, Claggett B, Assmann SF, Boineau R, Anand IS, Clausell N, et al. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation. 2015;131:34–42.
Appel LJ, Wright JT Jr, Greene T, Agodoa LY, Astor BC, Bakris GL, et al. Intensive blood pressure control in hypertensive chronic kidney disease. N Engl J Med. 2010;363:918–29.
PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–41.
Bavry AA, Anderson RD, Gong Y, Denardo SJ, Cooper-Dehoff RM, Handberg EM, et al. Outcomes among hypertensive patients with concomitant peripheral and coronary artery disease: findings from the INternational VErapamil-SR/Trandolapril STudy. Hypertension. 2010;55:48–53.
Turnbull F, Neal B, Algert C, Chalmers J, Chapman N, Cutler J, et al. Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med. 2005;165:1410–9.
Palmer SC, Mavridis D, Navarese E, Craig JC, Tonelli M, Salanti G, et al. Comparative efficacy and safety of blood pressure-lowering agents in adults with diabetes and kidney disease: a network meta-analysis. Lancet. 2015;385:2047–56.
Black HR, Davis B, Barzilay J, Nwachuku C, Baimbridge C, Marginean H, et al. Metabolic and clinical outcomes in nondiabetic individuals with the metabolic syndrome assigned to chlorthalidone, amlodipine, or lisinopril as initial treatment for hypertension: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Diabetes Care. 2008;32:353–60.
Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, et al. ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. J Am Coll Cardiol. 2010;55:e27–12.
Tsai TT, Nienaber CA, Eagle KA. Acute aortic syndromes. Circulation. 2005;112:3802–13.
•• Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–26 This American Heart Association 2008 scientific statement discusses the diagnosis, evaluation, and treatment of resistant hypertension.
Tataru AP, Barry AR. A systematic review of add-on pharmacologic therapy in the treatment of resistant hypertension. Am J Cardiovasc Drugs. 2017;17:311–8.
Myat A, Redwood SR, Qureshi AC, Spertus JA, Williams B. Resistant hypertension. BMJ. 2012;345:e7473.
Gandelman G, Aronow WS, Varma R. Prevalence of adequate blood pressure control in self pay or Medicare patients versus Medicaid or private insurance patients with systemic hypertension followed in a university cardiology or general medicine clinic. Am J Cardiol. 2004;94:815–6.
Vongpatanasin W. Resistant hypertension. A review of diagnosis and management. JAMA. 2014;311:2216–24.
Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125:1635–42.
Kumbhani DJ, Steg PG, Cannon CP, Eagle KA, Smith SC Jr, Crowley K, et al. Resistant hypertension: a frequent and ominous finding among hypertensive patients with atherothrombosis. Eur Heart J 2013; 34: 1204–1214.
Bangalore S, Davis BR, Cushman WC, Pressel SL, Muntner PM, Calhoun DA, et al. Treatment-resistant hyprtension and outcomes based on randomized treatment groups in ALLHAT. Am J Med. 2017;130:439–48.
•• Carey RM, Sakhuja S, Calhoun DA, Whelton PK, Muntner P. Prevalence of apparent treatment-resistant hypertension in the United States. Comparison of the 2008 and 2018 American Heart Association Scientific Statements on resistant hypertension. Hypertension. 2019;73:424–31 The 2018 American Heart Association scientific statement reports that the prevalence of treatment-resistant hypertension in the United States is 9.7%, that 3.2% of those with resistant hypertension are taking chlorthalidone or indapamide, and that 9.0% of those with resistant hypertension are taking spironolactone or eplerenone.
Petry NM, Rash CJ, Byrne S, Ashraf S, White WB. Financial reinforcers for improving medication adherence: findings from a meta-analysis. Am J Med. 2012;125:888–96.
Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J. Measuring, analyzing, and managing drug adherence in resistant hypertension. Hypertension. 2013;62:218–25.
Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RC, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. 2012;157:785–95.
Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;16:CD000011.
Ceral J, Habrdova V, Vorisek V, Bima M, Pelouch R, Solar M. Difficult-to-control arterial hypertension or uncooperative patients? The assessment of serum antihypertensive drug levels to differentiate non-responsiveness from non-adherence to recommended therapy. Hypertens Res. 2011;34:87–90.
Jung O, Gechter JL, Wunder C, Paulke A, Bartel C, Geiger H, et al. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J Hypertens. 2013;31:766–74.
•• Durand H, Hayes P, Morrissey EC, Newell J, Casey M, Murphy AW, et al. Medication adherence among patients with apparent treatment-resistant hypertension: systematic review and meta-analysis. J Hypertens. 2017;35:2346–57 An analysis of 24 studies showed that the prevalence of nonadherence to drug therapy is 31.2% in patients with resistant hypertension.
Durand H, Hayes P, Hasrhen B, Conneely A, Finn DP, Casey M, et al. Medication adherence for resistant hypertension: assessing theoretical predictors of adherence using direct and indirect adherence measures. Br J Health Psychol. 2018;23:949–66.
•• Adams M, Bellone JM, Wright BM, Rutecki GW. Evaluation and pharmacologic approach to patients with resistant hypertension. Postgrad Med. 2012;124:74–82 This paper discusses the evaluation and drug treatment of resistant hypertension.
Hwang AY, Dietrich E, Pepine CJ, Smith SM. Resistant hypertension: mechanisms and treatment. Curr Hypertens Rep. 2017;56. https://doi.org/10.1007/s11906-017-0754-x.
Ernst ME, Carter BL, Geordt CJ, Steffensmeier JJ, Phillips BB, Zimmerman MB, et al. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertens. 2006;47:352–8.
Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52:1749–57.
•• Oparil S, Schmieder RE. New approaches in the treatment of hypertension. Circ Res. 2015;116:1074–95 This paper discusses new approaches to the treatment of resistant hypertension.
Kalizki T, Schmidt BMW, Raff U, Reinold A, Schwarz TK, Schneider MP, et al. Low dose-eplerenone treatment decreases aortic stiffness in patients with resistant hypertension. J Clin Hypertens. 2017;19:669–76.
•• Chapman N, Dobson J, Wilson S, Dahlof B, Sever PS, Wedel H, et al. Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension. 2007;49:839–45 This study supports the use of spironolactone in patients with resistant hypertension.
Egan BM, Li J. Role of aldosterone blockade in resistant hypertension. Semin Nephrol. 2014;34:273–84.
Williams B, MacDonald TM, Moran S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386:2059–68.
Williams B, MacDonald TM, Moran S, Webb DJ, Sever P, McInnes GT, et al. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies. Lancet Diabetes Endocrinol. 2018;6:464.
Makai P, IntHout J, Deinum J, Jenniskens K, GJV W. A network meta-analysis of clinical management strategies for treatment-resistant hypertension: making optimal use of the evidence. J Gen Intern Med. 2017;32:921–30.
Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone versus clonidine as a fourth-drug therapy for resistant hypertension. The ReHOT randomized study (Resistant Hypertension Optimal Treatment). Hypertens. 2018;71:681–90.
•• Smith SM, Gurka MJ, Calhoun DA, Gong Y, Pepine CJ, RM C-DH. Optimal systolic blood pressure target in resistant and non-resistant hypertension: a pooled analysis of patient-level data from SPRINT and ACCORD. Am J Med. 2018;131:1463–72 This study supports a systolic blood pressure goal of less than 120 mmHg to reduce cardiovascular events and all-cause mortality in patients with resistant hypertension.
Laurent S, Schlaich M, Esler M. New drugs, procedures, and devices for hypertension. Lancet. 2012;380:593–600.
Burnier M. Update on endothelin receptor antagonists in hypertension. Curr Hypertens Rep. 2018;51. https://doi.org/10.1007/s11906-018-0848-0.
Dhaun N, Webb DJ. Endothelins in cardiovascular biology and therapeutics. Nat Rev Cardiol. 2019;16:491–502.
Williams B, Cockcroft JR, Kario K, Zappe DH, Brunel PC, Wang Q, et al. Effects of sacubitril/valsartan versus olmesartan on central hemodynamics in the elderly with systolic hypertension: the PARAMETER study. Hypertens. 2017;69:411–20.
Malik AH, Aronow WS. Efficacy of sacubitril/valsartan in hypertension. Am J Ther. 2019; In press. https://doi.org/10.1097/MJT.0000000000000925.
Kario K. The sacubitril/valsartan, a first-in-class, angiotensin receptor neprilysin inhibitor (ARNI): potential uses in hypertension, heart failure, and beyond. Curr Cardiol Rep. 2018;20:1–8. https://doi.org/10.1007/s11886-018-0944-4.
Ferdinand KC, Balavoine F, Besse B, Black HR, Desbrandes S, Dittrich HC, et al. Efficacy and safety of firibastat, a first-in-class brain aminopeptidae A inhibitor, in hypertensive overweight patients of multiple ethnic origins. A phase2, open-label, multicenter, dose-titrating study. Circulation. 2019;140:138–46.
Bhatt DL, Kandzari DE, O'Neill WW, D’Agostino R, Flack JM, Katzen BT, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393–401.
Bakris GL, Townsend RR, Liu M, Cohen SA, D’Agostino R, Flack JM, et al. Impact of renal denervation on 24-hour ambulatory blood pressure: results from SYMPLICITY HTN-3. J Am Coll Cardiol. 2014;64:1071–8.
Townsend RR, Mahfoud F, Kandzari DE, Kario K, Pocock S, Weber MA, et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomized, sham-controlled, proof-of-concept trial. Lancet. 2017;390:2160–70.
Kandzari DE, Bohm M, Mahfoud F, Townsend RR, Weber MA, Pocock S, et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HT-ON MED proof-of-concept randomized trial. Lancet. 2018;391:2346–55.
Azizi M, Schmieder RE, Mahfoud F, Weber MA, Daemen J, Davies J, et al. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicenter, international, single-blind, randomized, sham-controlled trial. Lancet. 2018;391:2335–45.
Sardar P, Bhatt DL, Kirtane AJ, Kennedy KF, Chatterjee S, Giri J, et al. Sham-controlled randomized trials of catheter-based renal denervation in patients with hypertension. J Am Coll Cardiol. 2019;73:1633–42.
Scheffers IJ, Kroon AA, Schmidli J, Jordan J, Tordoir JJ, Mohaupt MG, et al. Novel baroreflex activation therapy in resistant hypertension: results of a European multi-center feasibility study. J Am Coll Cardiol. 2010;56:1254–8.
Lobo MD, Sobatka PA, Stanton A, Cockcroft JR, Sulke N, Dolan E, et al. Central arteriovenous anastomosis for the treatment of patients with uncontrolled hypertension (the ROX CONTROL HTN study): a randomised controlled trial. Lancet. 2015;385:3634–41.
•• Rosa J, Widimsky P, Waldauf P, Lambert L, Zelinka T, Taborsky M, et al. Role of adding spironolactone and renal denervation in true resistant hypertension: one-year outcomes of randomized PRAGUE-15 study. Hypertens. 2016;67:397–403 This study showed that addition of spironolactone was more effective than renal artery denervation in reducing systolic blood pressure in patients with resistant hypertension.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Aronow has no conflicts of interest to disclose. This author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or drugs or devices discussed in this manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Resistant Hypertension
Rights and permissions
About this article
Cite this article
Aronow, W.S. Approaches for the Management of Resistant Hypertension in 2020. Curr Hypertens Rep 22, 3 (2020). https://doi.org/10.1007/s11906-019-1013-0
Published:
DOI: https://doi.org/10.1007/s11906-019-1013-0