Abstract
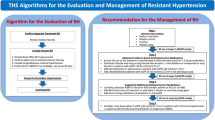
When a truly drug-resistant hypertension (dRHTN) has been identified, physicians have to decide which therapeutic option might offer the best chance to effectively lower the elevated blood pressure (BP) values, hopefully leading the patient’s status to BP control (<140/90 mmHg). Although invasive procedures such as renal denervation and carotid baroreflex stimulation can achieve this goal in a number of patients, there is no question that the first treatment approach to consider is the (1) removal of lifestyle factors that may oppose the BP lowering effect of the administered drugs, such as a high intake of salt, abuse of alcohol, obesity or co-treatments that have direct or indirect pressor effects and (2) modification of the existing treatment regimen by an increase of the dose or the extension of the medicaments already prescribed. This chapter will discuss how to make the best use of the medicament option.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Blood Pressure Control
- Resistant Hypertension
- Renal Denervation
- Blood Pressure Lowering Effect
- Mineralocorticoid Receptor Antagonist
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
When a truly drug-resistant hypertension (dRHTN) has been identified [1], physicians have to decide which therapeutic option might offer the best chance to effectively lower the elevated blood pressure (BP) values, hopefully leading the patient’s status to BP control (<140/90 mmHg) [1, 2]. Although invasive procedures such as renal denervation and carotid baroreflex stimulation can achieve this goal in a number of patients [3, 4], there is no question that the first treatment approach to consider is the (1) removal of lifestyle factors that may oppose the BP lowering effect of the administered drugs, such as a high intake of salt, abuse of alcohol, obesity [5, 6] or co-treatments that have direct or indirect pressor effects [7] and (2) modification of the existing treatment regimen by an increase of the dose or the extension of the medicaments already prescribed. This chapter will discuss how to make the best use of the medicament option.
2 Rationalization of the Three Drug Treatment Regimen
Hypertension guidelines emphasize the need for combination treatment to be based on drugs with different and complementary mechanisms of the BP lowering effect. They recommend a three drug combination to make use of a diuretic, a blocker of the renin-angiotensin system (RAS), be it an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin receptor antagonist and a calcium channel blocker because this fulfils the above requirement and has been shown to markedly reduce BP (up to 30–40 mmHg reduction of systolic values) in hypertensive patients with a variety of clinical characteristics [8–10]. In resistant hypertensive patients under treatment with three drugs, a therapeutic option is thus to ensure that a diuretic/RAS blocker/calcium channel blocker combination is used, provided that (1) no contraindication to one or another of these drugs exists or (2) the clinical condition of the patient requires other drugs to be part of the combination, such as a beta-blocker in patients with a history of coronary disease or heart failure. Of special importance is the inclusion of a diuretic in the three drug treatment regimen because diuretics enhance the antihypertensive effect of most antihypertensive agents, and difficult-to-treat hypertension may not rarely be associated with sodium and fluid retention as well as hypervolemia [11].
3 Increasing the Dose of the Prescribed Three Drugs
Drug underdosing is frequent in treated hypertensive patients; its high prevalence is one of the factors responsible for the low rate of BP control exhibited by the hypertensive population worldwide [12]. Careful checking of the drug doses prescribed (or assumed) is thus mandatory when dealing with a BP that remains uncontrolled under a three drug therapeutic regimen, an adequate dose of each of them being indeed a prerequisite for patient inclusion in the dRHTN category. Once this is established, however, a further increase in the dose of the prescribed drugs does not appear to be particularly helpful because (1) the shape of the dose/effect relationship can make the additional BP lowering effect far from substantial and (2) there may be with a number of drug classes (e.g., calcium channel blockers) a more prominent increase in the drug-related side effects [13]. It should nevertheless be emphasized that this may not be entirely true for diuretics because, as shown in Fig. 8.1, increasing the dose of hydrochlorothiazide beyond the usual 25 mg daily has been associated with a clear-cut further BP reduction; that is also the case for an increase of the thiazide-like diuretic chlorthalidone beyond the usual 12.5 mg, daily [14]. Along this line, several studies have shown an increase in the usual dose of diuretics to be accompanied by an increase in the number of resistant hypertensive patients reaching BP control. For example, in an American study on a cohort of about 150 resistant hypertensive patients, optimization of the existing treatment regimen that included an increase of the dose of diuretic was followed by BP control (<140/90 mmHg) in more than 50 % of the cases [15].
Effect of hydrochlorothiazide (HCTZ) and chlorthalidone (chlor) on systolic blood pressure (SBP) as a function of the daily dose (mg) (From Carter et al. [14], by permission)
4 Addition of a Fourth Drug
The drugs that are available as fourth step treatment of dRHTN have mechanisms of action that are only partly different from those of the drugs included in the background of three drug treatment regimen. Beta-blockers, alpha-I blockers and central agents, for example, share their sympatho-moderating influence with RAS blockers [16]. Beta-blockers and mineralocorticoid receptor antagonists share their opposition to the pressor and sodium retaining the effect of angiotensin II with RAS blockers. Direct vasodilators share their ability to reduce vasomotor tone with calcium channel blockers. Despite this potential mechanistic overlapping, however, addition of any fourth drug to the existing drug regimen stands a chance to lower BP and achieve control in a number of resistant hypertensive patients, which makes this approach the preferable one in this clinical condition.
Which drug to select among the available options is difficult to decide on an evidence basis because very few studies have addressed this issue by a randomized double-blind design, making the present fourth drug choice largely empiric. In this context, however, mineralocorticoid receptor antagonists and alpha-I blockers should probably be regarded as the preferred choice for pathophysiological considerations as well as for the extent of therapeutic data. Pathophysiological evidence leaves no doubt that hypertension is accompanied by (1) a sympathetic activation that is increased with the degree of BP elevation [17] and is particularly pronounced in patients whose BP is resistant to treatment (Fig. 8.2) [18] and (2) a plasma and tissue elevation of aldosterone whose secretion by the adrenal glands escapes, for a variety of reasons, the inhibitory effect of RAS blockers even when combined to oppose the production or influence of angiotensin II more effectively [19] (Fig. 8.3). Therapeutic evidence shows that these two drug classes lower BP in patients in whom multidrug treatment did not achieve control. This is exemplified by the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) in which the addition of the alpha-I blocker doxazosin in a large number of hypertensives uncontrolled by combination of various drugs lowered systolic BP by about 13–14 mm Hg, this being the case in a variety of clinical or demographic conditions (Fig. 8.4) [20]. Interestingly, the BP lowering effect was associated with no major side effect and no increased risk of heart failure, at variance from what has been reported in the doxazosin-treated hypertensive patients of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [21]. It is further exemplified by the BP reduction observed in the same trial when a similarly large number of patients in whom multidrug treatment had failed to achieve BP control were given spironolactone (Fig. 8.5) [22].
Office, ambulatory and beat-to-beat (finger) blood pressure (BP) in normotensives (NT), non-resistant hypertensives (HT) and resistant hypertensives (RHT). Muscle sympathetic nerve traffic (MSNA) measured by microneurography in the three groups is also shown. *P < 0.05; **P < 0.01 (From Grassi et al. [18], by permission)
Escape of aldosterone (serum concentration) in patients under treatment with an angiotensin receptor antagonist or an angiotensin receptor antagonist/ACE inhibitor combination (From McKelvie et al. [19], by permission)
Systolic blood pressure (SBP) reduction induced by doxazosin administration in patients in whom SBP was not controlled by multiple drug treatment. Data from different patient subgroups. Ys years, M males, F females, Ate group initially treated with atenolol, Amlo group initially treated with amlodipine, DM diabetes mellitus, MS metabolic syndrome (From Chapman et al. [20], by permission)
Systolic blood pressure (SBP) and diastolic blood pressure (DBP) before (pre) and after (post) administration of spironolactone in patients in whom BP was not controlled by multiple drug treatment. Treatment-induced changes are shown at the top of the histograms. CI confidence intervals (From Davis et al. [21], by permission)
5 Mineralocorticoid Receptor Antagonists: Further Evidence
Support to use of mineralocorticoid receptor antagonists as the fourth drug to be administered in dRHTN can be found in several other studies that have shown, in some instances via a randomized, placebo-controlled design, the BP lowering ability of this class to include not only spironolactone but also eplerenone at adequate doses [23–30]. The most important documentation of the effectiveness of these drugs, however, comes from the recently published The Prevention and Treatment of Hypertension with Algorithm-based therapy (PATHWAY-2) study in which several hundred patients with a BP uncontrolled by the recommended three drug treatment regimen were randomized to the addition of spironolactone, bisoprolol, doxazosin or placebo. Following a few months of treatment, patients taking spironolactone showed a significantly greater BP reduction than patients taking doxazosin or bisoprolol, whose effect was modestly, albeit significantly, more evident than placebo. This was the case not only for office but also for home BP whose treatment-induced modification was the primary end point of the study (Fig. 8.6) [31]. This will probably lead future guidelines to privilege mineralocorticoid receptor antagonists over other drug options as the preferred fourth choice in dRHTN and perhaps also to define hypertension as resistant to treatment only after administration of a drug of this class has proven ineffective.
Home blood pressure (BP) values at baseline and during treatment with placebo, spironolactone, doxazosin and bisoprolol (From Williams et al. [31], by permission)
6 Unmet Needs
Although more effective than any other added drug currently available, mineralocorticoid receptor antagonists by no means take care of all the problems posed by treatment of dRHTN. First, these drugs are associated with a number of serious side effects such as hyperkalemia and reduction of renal function [22, 32]. Second, both hyperkalemia and reduction of renal function are more frequent and severe in patients with a seriously impaired glomerular filtration, a condition that was excluded in the patients enrolled for the PATHWAY-2 study but that is not at all uncommon in dRHTN [33]. Third, despite the greater BP lowering effect in the PATHWAY-2 study, spironolactone failed to effectively lower BP in about 40 % of the study population, i.e. those with a high renin level, and perhaps a concomitant sympathetic hyperactivity (Fig. 8.7) [31]. Thus, more than a single drug class appears to be needed as fourth choice in order to extend effective treatment to the vast majority of resistant hypertensive individuals.
Relationship between the home systolic blood pressure (SBP) change induced by spironolactone and plasma renin activity in the PATHWAY-2 study (From Williams et al. [31], by permission)
Future studies will have to address this issue by comparing the addition of a fourth drug with the combination of two or more additional agents, hopefully clarifying which combinations have the greatest potential to extend BP control. They may also, however, elect to address alternative possibilities, namely, whether (1) BP can be reduced in a larger number of resistant hypertensive patients by the use of drugs belonging to the same class but having a different site of action [34], an approach that sequential administration of a thiazide diuretic, a loop diuretic and amiloride has proven effective [35], or (2) a more precise assessment of the resistant hypertension phenotype. The latter approach will mean to (1) identify as precisely as possible the nature and extent of the alterations of the structure and function of the organs (the heart, brain, kidney and vessels) targeted by the uncontrolled BP status and (2) determine which among the multiple neural and humoral mechanisms controlling circulation is more severely deranged, in order to try to individualize treatment and increase its success rate.
Finally, drug treatment of dRHTN may in the future count on new effective BP lowering agents. In the past, the use of endothelin antagonists has been disappointing because their BP lowering effect turned out to be questionable and accompanied by an unfavourable side effect profile [36]. Drugs targeting arterial stiffening (a structural alteration majorly responsible for the difficulty of lowering systolic values) have also met with difficulties that have prevented their extensive testing in humans. However, new dual-acting molecules as well as new powerful and better tolerated vasodilators are promising medicaments that may allow to more successfully face therapeutic control of a condition that may have a prevalence greater than 5 % of the overall hypertensive population [1], thereby involving in Europe several hundred thousand individuals.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- BP:
-
Blood pressure
- DBP:
-
Diastolic blood pressure
- dRHTN:
-
Drug-resistant hypertension
- RAS:
-
Renin-angiotensin system
- SBP:
-
Systolic blood pressure
References
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F (2013) The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). 2013 ESH/ESC Guidelines for the management of arterial hypertension. J Hypertens 31:1281–1357
Burnier M, Pechere Bertschi A, Wuezner G (2013) Treatment of resistant hypertension. Which additional antihypertensive drugs. In: Mancia G (Ed). Resistant Hypertension. Springer, Milan. pp 115–126
Schmieder RE, Redon J, Grassi G, Kjeldsen SE, Mancia G, Narkiewicz K, Parati G, Ruilope L, van de Borne P, Tsioufis C (2012) ESH position paper: renal denervation – an interventional therapy of resistant hypertension. J Hypertens 30:837–841
Bakris GL, Nadim MK, Haller H, Lovett EG, Schafer JE, Bisognano JD (2012) Baroreflex activation therapy provides durable benefit in patients with resistant hypertension: results of long-term follow-up in the Rheos Pivotal Trial. J Am Soc Hypertens 6:152–158
Florczak E, Prejbisz A, Szwench-Pietrasz E, Sliwiński P, Bieleń P, Klisiewicz A, Michałowska I, Warchoł E, Januszewicz M, Kała M, Witkowski A, Więcek A, Narkiewicz K, Somers VK, Januszewicz A (2013) Clinical characteristics of patients with resistant hypertension: the RESIST-POL study. J Hum Hypertens 27:678–685
Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell’Italia LJ, Calhoun DA (2009) Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension 54:475–481
Forman JP, Rimm EB, Curhan GC (2007) Frequency of analgesic use and risk of hypertension among men. Arch Intern Med 167:394–399
Tóth K, PIANIST Investigators (2014) Antihypertensive efficacy of triple combination perindopril/indapamide plus amlodipine in high-risk hypertensives: results of the PIANIST study (Perindopril-Indapamide plus AmlodipiNe in high rISk hyperTensive patients). Am J Cardiovasc Drugs 14:137–145
Calhoun DA, Lacourcière Y, Chiang YT, Glazer RD (2009) Triple antihypertensive therapy with amlodipine, valsartan, and hydrochlorothiazide: a randomized clinical trial. Hypertension 54:32–39
Kjeldsen SE, Messerli FH, Chiang CE, Meredith PA, Liu L (2012) Are fixed-dose combination antihypertensives suitable as first-line therapy? Curr Med Res Opin 28:1685–1697
Rossi GP (2013) Resistant hypertension. Neurohumoral aspects. In: Mancia G (ed) Resistant hypertension. Springer, Milan, pp 11–21
Pereira M, Lunet N, Azevedo A, Barros H (2009) Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens 27:963–975
Law MR, Wald NJ, Morris JK, Jordan RE (2003) Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ 326:1427
Carter BL, Ernst ME, Cohen JD (2004) Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension 43:4–9
Garg JP, Elliott WJ, Folker A, Izhar M, Black HR, RUSH University Hypertension Service (2005) Resistant hypertension revisited: a comparison of two university-based cohorts. Am J Hypertens 18:619–626
Saino A, Pomidossi G, Perondi R, Valentini R, Rimini A, Di Francesco L, Mancia G (1997) Intracoronary angiotensin II potentiates coronary sympathetic vasoconstriction in humans. Circulation 96:148–153
Mancia G, Grassi G (2014) The autonomic nervous system and hypertension. Circ Res 114:1804–1814
Grassi G, Seravalle G, Brambilla G, Pini C, Alimento M, Facchetti R, Spaziani D, Cuspidi C, Mancia G (2014) Marked sympathetic activation and baroreflex dysfunction in true resistant hypertension. Int J Cardiol 177:1020–1025
McKelvie RS, Yusuf S, Pericak D, Avezum A, Burns RJ, Probstfield J, Tsuyuki RT, White M, Rouleau J, Latini R, Maggioni A, Young J, Pogue J (1999) Comparison of candesartan, enalapril, and their combination in congestive heart failure: randomized evaluation of strategies for left ventricular dysfunction (RESOLVD) pilot study. The RESOLVD Pilot Study Investigators. Circulation 100:1056–1064
Chapman N, Chang CL, Dahlöf B, Sever PS, Wedel H, Poulter NR, ASCOT Investigators (2008) Effect of doxazosin gastrointestinal therapeutic system as third-line antihypertensive therapy on blood pressure and lipids in the Anglo-Scandinavian Cardiac Outcomes Trial. Circulation 118:42–48
Davis BR, Kostis JB, Simpson LM, Black HR, Cushman WC, Einhorn PT, Farber MA, Ford CE, Levy D, Massie BM, Nawaz S, ALLHAT Collaborative Research Group (2008) Heart failure with preserved and reduced left ventricular ejection fraction in the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Circulation 118:2259–2267
Chapman N, Dobson J, Wilson S, Dahlöf B, Sever PS, Wedel H, Poulter NR, Anglo-Scandinavian Cardiac Outcomes Trial Investigators (2007) Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension 49:839–845
Azizi M, Sapoval M, Gosse P, Monge M, Bobrie G, Delsart P, Midulla M, Mounier-Véhier C, Courand PY, Lantelme P, Denolle T, Dourmap-Collas C, Trillaud H, Pereira H, Plouin PF, Chatellier G, Renal Denervation for Hypertension (DENERHTN) investigators (2015) Optimum and stepped care standardised antihypertensive treatment with or without renal denervation for resistant hypertension (DENERHTN): a multicentre, open-label, randomised controlled trial. Lancet 385:1957–1965
Rosa J, Widimský P, Toušek P, Petrák O, Čurila K, Waldauf P, Bednář F, Zelinka T, Holaj R, Štrauch B, Šomlóová Z, Táborský M, Václavík J, Kociánová E, Branny M, Nykl I, Jiravský O, Widimský J Jr (2015) Randomized comparison of renal denervation versus intensified pharmacotherapy including spironolactone in true-resistant hypertension: six-month results from the Prague-15 study. Hypertension 65:407–413
Václavík J, Sedlák R, Plachy M, Navrátil K, Plásek J, Jarkovsky J, Václavík T, Husár R, Kociánová E, Táborsky M (2011) Addition of spironolactone in patients with resistant arterial hypertension (ASPIRANT): a randomized, double-blind, placebo-controlled trial. Hypertension 57:1069–1075
Nishizaka MK, Zaman MA, Calhoun DA (2003) Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens 16:925–930
Pitt B, Reichek N, Willenbrock R, Zannad F, Phillips RA, Roniker B, Kleiman J, Krause S, Burns D, Williams GH (2003) Effects of eplerenone, enalapril, and eplerenone/enalapril in patients with essential hypertension and left ventricular hypertrophy: the 4E-left ventricular hypertrophy study. Circulation 108:1831–1838
de Souza F, Muxfeldt E, Fiszman R, Salles G (2010) Efficacy of spironolactone therapy in patients with true resistant hypertension. Hypertension 55:147–152
Rodilla E, Costa JA, Pérez-Lahiguera F, Baldó E, González C, Pascual JM (2009) Spironolactone and doxazosin treatment in patients with resistant hypertension. Rev Esp Cardiol 62:158–166
Ramsay LE, Silas JH, Freestone S (1980) Diuretic treatment of resistant hypertension. Br Med J 281:1101–1103
Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, Ford I, Cruickshank JK, Caulfield MJ, Salsbury J, Mackenzie I, Padmanabhan S, Brown MJ, British Hypertension Society’s PATHWAY Studies Group (2015) Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet 386:2059–2068
Bianchi S, Bigazzi R, Campese VM (2006) Long-term effects of spironolactone on proteinuria and kidney function in patients with chronic kidney disease. Kidney Int 70:2116–2123
Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, O’Connor PJ, Selby JV, Ho PM (2012) Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 125:1635–1642
Mancia G (2012) Additional drug treatment in resistant hypertension: need for randomized studies. J Hypertens 30:1514–1515
Bobrie G, Frank M, Azizi M, Peyrard S, Boutouyrie P, Chatellier G, Laurent S, Menard J, Plouin PF (2012) Sequential nephron blockade versus sequential renin-angiotensin system blockade in resistant hypertension: a prospective, randomized, open blinded endpoint study. J Hypertens 30:1656–1664
Weber MA, Black H, Bakris G, Krum H, Linas S, Weiss R, Linseman JV, Wiens BL, Warren MS, Lindholm LH (2009) A selective endothelin-receptor antagonist to reduce blood pressure in patients with treatment-resistant hypertension: a randomised, double-blind, placebo-controlled trial. Lancet 374:1423–1431
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mancia, G. (2016). Optimization of Antihypertensive Drug Treatment in Resistant Hypertension. In: Tsioufis, C., Schmieder, R., Mancia, G. (eds) Interventional Therapies for Secondary and Essential Hypertension. Updates in Hypertension and Cardiovascular Protection. Springer, Cham. https://doi.org/10.1007/978-3-319-34141-5_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-34141-5_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-34140-8
Online ISBN: 978-3-319-34141-5
eBook Packages: MedicineMedicine (R0)