Abstrac
Purpose of Review
Hispanic/Latino Americans are among the fastest growing ethnic populations in the United States (US). Hypertension, in particular uncontrolled hypertension, is a significant source of cardiovascular morbidity and mortality in this population. In this review, we outline the epidemiology of hypertension and certain considerations in the management of hypertension in this heterogeneous population.
Recent Findings
Substantial variation in hypertension prevalence and control exists among different ethnic subgroups of Hispanics. More specifically, and in the community, outcomes for hypertension management are less favorable, suggesting that suboptimal hypertension control may be the result of social factors. In this regard, community-based interventions have shown promise in addressing these shortfalls. Nonetheless, significant barriers to effective hypertension care exist in the Hispanic community, including the increasing prevalence of comorbidities that impact hypertension such as obesity. Pharmacologic therapies for hypertension have been highly effective in Hispanic subjects participating in clinical trials. Notably, studies that disaggregate Hispanics by their ancestral origin may provide greater insight into the sources of ethnic disparities.
Summary
Culturally tailored interventions may improve hypertension management and outcomes in Hispanic populations. Additional population and clinical trials in Hispanic patients of different ancestral heritages are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hispanic/Latino individuals account for 18% (~ 57 million) of the United States (US) population [1]. The Hispanic American population is one of the fastest growing ethnic minority groups in the US, which is expected to double within the next four decades [2•]. Of note, Hispanics are a heterogeneous population comprised of a number of ethnic subgroups with diverse lineages and cultural mores. Like in many aging populations, hypertension has become increasingly common among Hispanics as a whole and contributes to a substantial burden of cardiovascular disease. As a result, a number of considerations are important when determining the management of hypertension in Hispanics, including potential biologic, socioeconomic, and cultural determinants of health. In this review, we explore many of these considerations through an evaluation of the current medical literature on hypertension in Hispanics.
Epidemiology of Hypertension in Hispanics
In 2015–2016, the age-adjusted prevalence of hypertension in Hispanic adults in the US was 27.8% [3], which was similar to that found in non-Hispanic White (27.8%) and Asian adults (25.0%), but lower than that found in non-Hispanic Black or African American adults (40.3%). With the recent lowering of the hypertension threshold from 140/90 to 130/80 mmHg in clinical practice guidelines, the prevalence of hypertension is estimated at 44% for Hispanic men and 42% for Hispanic women [4••].
In the National Health and Nutrition Examination Survey (NHANES), the prevalence of uncontrolled hypertension (defined as a systolic blood pressure of 140 mmHg or higher or a diastolic blood pressure of 90 mmHg or higher in an individual with hypertension) was lower in non-Hispanic White adults (49.2%) than in Hispanic (55.0%), non-Hispanic Black (55.4%), and Asian (62.6%) adults [3]. A similar pattern was observed in Hispanic participants of the Multi-Ethnic Study of Atherosclerosis (MESA), a prospective cohort study of adults across the US. Among hypertensive participants in MESA, the percentage of treated but uncontrolled hypertension was significantly higher among Hispanics (32%) compared to non-Hispanic Whites (24%), and comparable to African Americans (35%), and Chinese (33%) [5].
For adults without hypertension and aged 45 years, the 40-year risk of incident hypertension is 92% for Hispanic adults, which is similar to 86% for white adults, and 93% for African American adults [4••]. In the MESA, the incidence of hypertension was modestly higher for Hispanic (65.7 per 1000 person-years) compared to White (56.8 per 1000 person-years) participants. After adjusting for age and gender, the incidence rate ratio for hypertension among Hispanics was significantly higher compared to White participants (1.29, 95% confidence interval 1.06–1.57). With further adjustment for several comorbidities including body mass index and renal dysfunction, this association was attenuated (incidence rate ratio 0.98, 95% confidence interval 0.78–1.23), suggesting that the higher incidence of hypertension among Hispanics may be mediated by these risk factors [6].
Hypertension by Hispanic Ethnic Subgroup
Although Hispanics are often classified as a single ethnic group, there is considerable heterogeneity in cultural, socioeconomic, and genetic factors that may influence the prevalence and treatment of hypertension. In the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), a population-based cohort study performed in four US communities, the age-standardized prevalence of hypertension was found to be highest among the Hispanic individuals of Dominican (men, 32.6%; women, 26.1%), followed by Cuban (men, 28.9%; women, 26.4%), Puerto Rican (men, 27.4%; women, 29.1%), and Central American (men, 25.0%; women, 25.6%) ancestry [7••]. Notably, the prevalence of hypertension among Hispanics of Mexican (men, 21.4%; women, 19.5%) and South American (men, 19.9%; women, 15.9%) ancestry was lower [8••]. Similarly, and in the MESA, Dominican Americans had a markedly higher prevalence of hypertension (52.9%) compared to Mexican Americans (37.6%), Puerto Rican Americans (43.3%), and Hispanic Americans of other descent (42.1%) [9].
Similar variations in hypertension prevalence have been observed in Hispanics living outside of the US. In the Cardiovascular Risk Factor Multiple Evaluation in Latin America (CARMELA), a cross-sectional population-based study of individuals aged 25–64 years living in seven Latin American cities, the prevalence of hypertension approximated US averages (~ 25–30%). However, in some city centers, the prevalence of hypertension was found to be markedly lower than that encountered in US Hispanics. For instance, in Mexico City, the prevalence of hypertension was 11.7% [10]. In urban centers across Mexico, age-adjusted rates of hypertension have been reported to be considerably higher at 33.5% [11].
In an analysis of 2002 death certificate data, the Centers for Disease Control and Prevention found that the age-standardized hypertension-related mortality rate among Hispanics (127 per 100,000) was similar to that of non-Hispanic Whites (136 per 100,000). However, this mortality rate varied significantly among Hispanic subgroups, with Puerto Rican Americans having the highest mortality rate (154 per 100,000) and Cuban Americans having the lowest (83 per 100,000). The hypertension-related mortality rate for Mexican Americans (135 per 100,000) did not differ from non-Hispanic Whites. However, between 1995 and 2002, rates of hypertension-related mortality appeared to be increasing more rapidly for Hispanic ethnic subgroups, with a 30.7% increase found in Mexican Americans and a 46.1% increase for other Hispanic Americans (exclusive of Puerto Rican and Cuban Americans), both of which were lower than the 26.5% increase found among non-Hispanic Whites [12].
These data suggest that aggregating data for all Hispanic subgroups may not accurately reflect the impact of ethnicity on hypertension rates and cardiovascular disease risk among Hispanics. However, few studies evaluate Hispanic individuals by ancestral origin. A notable exception is the HCHS/SOL, which recruited study subjects from diverse Hispanic ethnic origins, and may provide insight into the heterogeneous composition of the Hispanic ethnicity and subgroup sample sizes needed to perform meaningful analyses.
Pharmacologic Interventions
Few studies have assessed the effects of pharmacologic antihypertensive therapies in Hispanic individuals. However, subgroup analyses of clinical trials that enrolled racial minorities have suggested that the effect of antihypertensive agents may vary by race/ethnicity. For instance, in a pre-specified analysis of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), a randomized trial of antihypertensive drugs in hypertensive adults aged 55 years and older, randomization to chlorthalidone versus lisinopril resulted in a greater reduction in blood pressure (p < 0.001), risk for stroke (p = 0.01), and risk for combined cardiovascular disease outcomes (p = 0.04) among Black study participants in comparison to non-Black participants [13].
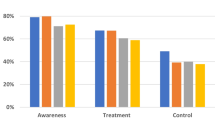
Although starting with lower rates of controlled hypertension at the onset of the trial, Hispanic subjects in ALLHAT had similar or slightly higher rates of control throughout the remaining follow-up compared to non-Hispanic White participants, with 72% of Hispanic participants achieving hypertension control at 48 months of follow-up (Fig. 1) [14••]. Comparisons of cardiovascular disease outcomes between Hispanic and non-Hispanic participants in ALLHAT have not been reported.
Percentage of race/ethnicity subgroups with controlled hypertension over follow-up in ALLHAT. Reprinted with permission from [14]
Similar results were found in the subanalysis of Hispanic patients in the International Verapamil SR/Trandolapril Study (INVEST). INVEST was an international prospective, randomized trial of verapamil versus atenolol in hypertensive patients with coronary artery disease. Hispanic patients in this trial were recruited primarily from the mainland US, Mexico, Puerto Rico, and Cuba. Compared to non-Hispanic subjects, Hispanic subjects achieved a lower average systolic blood pressure and a greater proportion of Hispanic patients had controlled blood pressure (< 140/90 mmHg) by the end of the study (Fig. 2) [15••]. Of those with controlled blood pressure at baseline, 78% of Hispanics and 70% of non-Hispanics had controlled blood pressure at 24 months (p < 0.001). Of those with uncontrolled blood pressure at baseline, 66% of Hispanics and 57% of non-Hispanics had controlled blood pressure at 24 months (p < 0.001). After adjusting for baseline blood pressure levels, Hispanic patients had an average systolic blood pressure reduction of 21.3 mmHg, compared to 17.4 mmHg for non-Hispanic patients (p < 0.001). Hispanic patients also required fewer study drugs to achieve these systolic blood pressure reductions at a mean of 2.4 versus 2.7 in non-Hispanic patients (p < 0.001). These greater improvements in hypertension control appeared to translate into improved outcomes. That is, and with adjustment for baseline characteristics, Hispanic patients had a lower risk of the composite endpoint of all-cause death, nonfatal myocardial infarction, or nonfatal stroke compared to non-Hispanic patients, with a hazard ratio of 0.87 (95% confidence interval 0.78–0.97) [15••]. This improvement in outcomes did not vary by the blood pressure medication regimen employed.
Systolic and diastolic blood pressures over follow-up for Hispanic and non-Hispanic patients in INVEST. Reprinted with permission from [15]
The recently published Systolic Blood Pressure Intervention Trial (SPRINT) was a randomized trial enrolling hypertensive individuals of elevated cardiovascular disease risk from sites across the US and Puerto Rico comparing intensive systolic blood pressure control to a target of less than or equal to 120 mmHg versus standard systolic blood pressure control to a target of less than or equal to 140 mmHg. Of the participants, 11% (n = 984) were Hispanic [16]. At baseline, mean systolic blood pressure was higher, and the average number of prescribed antihypertensive agents was lower, among Hispanics compared to non-Hispanics. In multivariable analysis, neither medication adherence nor medical insurance status was significantly associated with controlled blood pressure at baseline among Hispanics [17]. Notably, approximately 56% of Hispanics in SPRINT were living in Puerto Rico at the time of enrollment. Compared to Hispanics in the mainland US, Hispanics in Puerto Rico had higher blood pressure readings, were less likely to have blood pressure controlled, and had a lower average number of prescribed antihypertensive medications [17].
During the trial, Hispanic participants achieved similar levels of systolic blood pressure in both intervention arms when compared to non-Hispanic White and non-Hispanic Black participants. Outcomes for Hispanics participants in the intensive arm were broadly similar to non-Hispanic participants. The hazard ratios (with 95% confidence intervals) for the primary composite outcome of first acute coronary syndrome, stroke, decompensated heart failure, or cardiovascular death were 0.70 (0.57–0.86), 0.71 (0.51–0.98), and 0.62 (0.33–1.15) for non-Hispanic White, non-Hispanic Black, and Hispanics, respectively, with no significant heterogeneity of treatment effect by race/ethnicity observed. Similarly, renal disease outcomes, as well as risks of serious adverse events, did not differ by race/ethnicity [18•].
Clinical practice guidelines recommend that for non-Hispanic Black individuals, where rates of hypertension and resistant hypertension are high, initial antihypertensive drug treatment should include a thiazide-type diuretic or a calcium-channel blocker [4••]. These recommendations arose from observations of treatment effects by race in the ALLHAT trial [13]. As Hispanics are generally underrepresented in trials of antihypertensive therapies, specific recommendations for drug therapies in Hispanics are not available [19]. However, in the clinical trial setting with access to high-quality, protocol-driven hypertension care, Hispanic patients achieve equal or lower blood pressures and equal or higher rates of controlled blood pressure as non-Hispanic patients. Thus, it is unlikely that underlying biological differences contribute to poor blood pressure control observed among Hispanics. Rather, impediments to delivery of care, such as patient awareness, socioeconomic factors, and language barriers may play a large role in producing ethnic disparities in hypertension control observed in the Hispanic population.
Community-Based Interventions
Culturally tailored lifestyle interventions have been effective in lowering blood pressure in Hispanic populations. In a single-arm community-based intervention study of 5714 primarily Hispanic adults with hypertension in San Antonio, Texas, investigators evaluated the effect of an intervention incorporating home blood pressure monitoring, fitness and nutritional counseling, and regular follow-up provided by non-clinician patient navigators [20•]. These navigators assisted subjects in overcoming barriers and reducing disparities related to language and cultural gaps. Over the course of 90 days, the intervention resulted in a significant reduction in systolic blood pressure, from 139.1 to 131.5 mmHg. In the Hypertension Improvement Project (HIP) Latino pilot study, Hispanic/Latino adults with hypertension or pre-hypertension in Durham, North Carolina, were enrolled in group intervention sessions using motivational interviewing techniques to encourage the study subjects to identify and implement lifestyle changes intended to lower blood pressure [21]. The intervention was culturally adapted by utilizing food recipes and physical activities (e.g., dancing) that are common in Hispanic culture. Over the course of six weekly sessions, systolic blood pressure was markedly reduced by an average of 10.4 ± 10.6 mmHg.
Barriers to Hypertension Management in Hispanics
Health Literacy/Access to Care
The majority of Hispanics with hypertension appear to be aware of their diagnosis. In HCHS/SOL, 74.1% of hypertensive participants were aware, which was comparable to the 77.7% of Hispanics in NHANES, but slightly lower than the 81.4% of non-Hispanic White NHANES participants. While the prevalence and awareness of hypertension among Hispanics were broadly similar to that of non-Hispanic Whites, the rates of medication-treated hypertension and controlled hypertension (defined as having hypertension and a measured blood pressure of < 140/90 mmHg) were 63.4% and 37.5%, respectively, which compare unfavorably to non-Hispanics White in NHANES, where 76.6% were treated and 56.3 were controlled [8••]. Among Hispanic men aged < 40 years with hypertension, only 20% had their blood pressure levels controlled.
In a study of 159,947 adults with hypertension participating in the Behavioral Risk Factor Surveillance System, an ongoing phone survey tracking health conditions and health-related behaviors across the US, Hispanic American ethnicity was associated with indicators of poor access to health care such as no health insurance, no personal health care provider, and an inability to visit a doctor due to cost [22]. In an analysis of the 2001–2006 NHANES survey, Mexican Americans had the highest proportions of individuals who were impoverished, lacked medical insurance, or had less than 12 years of education [23]. In the 2009 Racial and Ethnic Approached to Community Health Across the U.S. (REACH US) survey, 21.8% of men in Hispanic communities identified a time during the prior 12 months where they needed to see a doctor but could not do so because of cost, which was substantially higher than the national median for men (12.2%) [24].
In the HCHS/SOL, the prevalence of hypertension among all participants did not appear to vary significantly by level of education (high school or greater versus less than high school) or annual income level [8••]. Furthermore, there were no differences in awareness, treatment, or control of hypertension by level of education or income. However, and compared to those without health insurance, higher proportions of hypertensive Hispanics with health insurance reported being aware of their diagnosis, receiving treatment, and having their blood pressure levels adequately controlled [25]. Low rates of hypertension treatment and (to a lesser extent) hypertension awareness, combined with high rates of comorbid cardiovascular disease risk factors such as obesity, likely contribute to the age-adjusted hypertension-attributable mortality rate per 1000 persons of 19.1 and 14.6 for Hispanic men and women, respectively [4••].
Acculturation
Cultural influences on Hispanic individuals may also impact hypertension management. Acculturation, or the process by which minority groups adopt behaviors of the majority group, may play a detrimental role among Hispanic Americans. In the 2007 California Health Interview Survey of 51,048 White, Black, Latino, and Asian individuals, greater acculturation (determined using acculturation surrogates of country of birth, parents’ country of birth, language at home, and duration of stay in the US) was associated with a higher prevalence of hypertension independent of several risk factors including education, smoking, physical activity, and body mass index [24].
Similarly, in the MESA, surrogates for acculturation such as place of birth, language spoken at home, and number of years residing in the US were each associated with prevalent hypertension, with languages other than English spoken at home and place of birth other than the US inversely associated with hypertension. Additionally, years living in the US was positively associated with hypertension, with an association that was robust to adjustment for demographic, socioeconomic, and hypertension risk factor variables [26]. Conversely, an analysis of NHANES data showed no significant association between acculturation and prevalent hypertension among Hispanic Americans. In this study, acculturation was measured by a 5-item scale that centers on a respondent’s use of the English language [27].
Language barriers for Hispanic patients being treated for hypertension by English-speaking providers may influence rates of uncontrolled hypertension in this population. A study of 131,277 patients with diabetes treated in the Northern California Kaiser Permanente health system found that among patients whose preferred language was Spanish, having a provider fluent in Spanish was associated with a slightly higher rate of adherence to cardiovascular disease-related medications (50.6% vs. 44.8%), after adjusting for a host of demographic and clinical variables [28].
Cultural and Behavioral Factors
Culture is an important determinant of behavior and influences many of the lifestyle factors that contribute to the development and management of hypertension. While dietary habits contribute significantly toward hypertension, Hispanic Americans have been reported to adhere to dietary patterns that are generally protective for hypertension. For instance, and using NHANES data, Mexican Americans had the lowest proportion of adults ingesting high-sodium, high-alcohol, and high-total calorie diets. Fiber intake, which has been associated with lower blood pressure, was highest among Mexican Americans [23].
Physical activity is protective for hypertension and can help lower blood pressure among individuals with hypertension. Self-reported physical activity data collected for the 1998–2008 National Health Interview Survey showed that only 33.8% of Hispanics performed recommended amounts of aerobic physical activity (> 150 min of moderate or > 75 min of vigorous activity weekly), compared to 47.6% for non-Hispanic Whites [29]. In HCHS/SOL, participants wore accelerometers and objective data regarding physical activity were obtained showing that 40.8% of Hispanic participants were meeting physical activity guideline recommendations [30•]. Daily physical activity varied by Hispanic subgroup: Mexicans had the highest number of moderate or vigorous physical activity per day (32.1 min) and Cubans had the lowest (15.3 min).
Excessive sedentary behavior is also associated with adverse health outcomes, including hypertension. In the 2001–2006 NHANES survey, Mexican Americans reported the highest age-adjusted percentage of no weekly physical activity (32.7%), a percentage twice as high as that reported by non-Hispanic whites) [23]. In HCHS/SOL, accelerometer-based measures of sedentary time found Hispanic adults spending 11.9 h per day, or 74% of their monitored time, in sedentary behaviors on average [31•].
Fatalism, or the belief that one’s health and health outcomes are determined by fate and are outside of one’s control, has been proposed as a potential barrier to hypertension treatment in certain cultural groups, including Hispanic Americans. In this regard, 5313 HCHS/SOL participants underwent in-depth sociocultural self-report assessments including an 8-item fatalism scale with statements about whether the future is outside of one’s control, with a higher score on this scale corresponding to a greater endorsement of fatalism [32]. In this sample, lower income, lower education level, and Spanish language preference were associated with a higher fatalism score. In cross-sectional, multivariable analysis adjusting for demographic, socioeconomic, and acculturation variables, higher fatalism scores were modestly associated with prevalent hypertension (odds ratio 1.14, 95% confidence interval 1.02, 1.28). With additional adjustment for health variables such as diabetes, body mass index, dietary quality, and physical activity, the association was attenuated to non-significance, suggesting that the association of fatalism with hypertension may be confounded, or potentially mediated, by factors heavily determined by behavior.
Comorbidities
Obesity is a major risk factor for hypertension [33]. In the US, Hispanic adults have the highest age-adjusted prevalence of obesity (47.0%) followed by non-Hispanic Blacks (46.8%), non-Hispanic Whites (37.9%), and non-Hispanic Asians (12.7%) [34]. The prevalence of obesity is 43.1% among Hispanic men, and 50.6% among Hispanic women. Hispanic youth are similarly affected by the US obesity epidemic, with obesity in 25.8% of Hispanic youth aged 2–19 years, the highest prevalence of any race/ethnicity. The high percentage of obesity among Hispanic youth is of particular concern given its association with early hypertension in adolescence. For instance, in a cross-sectional study of 21,062 adolescents evaluated via school-based screenings, obesity was associated with a nearly sixfold higher risk of hypertension in Hispanics, compared to a fourfold, threefold, and twofold higher risk for White, Asian, and African American adolescents, respectively [35•].
For a number of Hispanic individuals, hypertension is only one component in a diagnosis of the metabolic syndrome (large waist circumference, elevated triglycerides, low high-density lipoprotein cholesterol level, elevated fasting blood sugar, and hypertension). Among Hispanics, the metabolic syndrome is common. In NHANES, 40.6% of Mexican Americans met criteria for the metabolic syndrome, compared to 38.8% percent of non-Hispanic Blacks and 31.5% of non-Hispanic Whites [37]. In HCHS/SOL, the age-standardized prevalence of metabolic syndrome was 33.7% in Hispanic men and 36.0% in women [38•]. The prevalence was highest in Puerto Ricans (37%) and lowest in South Americans (27%). Of those with the metabolic syndrome, 96% of women and 73% of men had a large waist circumference. In this sample, only 21% of men and 14% of women had none of the cardiometabolic abnormalities that were components of the metabolic syndrome.
While the clustering of these risk factors for cardiovascular disease and diabetes is commonly observed, the underlying pathogenesis uniting these risk factors is unclear. One potential mechanism involves insulin resistance. More specifically, and in a study of moderately obese individuals (BMI, 30–35), those with the most insulin resistance had significantly higher systolic and diastolic blood pressure (139 ± 20 vs. 123 ± 18 mmHg and 83 ± 3 vs. 75 ± 10 mmHg, respectively), in addition to less favorable metabolic profiles [36]. These findings suggest that weight reduction and other measures that improve insulin sensitivity may be of enhanced importance in hypertension management in individuals with the metabolic syndrome.
Obesity is also associated with sleep-disordered breathing. This condition and obstructive sleep apnea, in particular, are associated with hypertension. Treatment of sleep apnea through continuous positive airway pressure devices results in significant reductions in blood pressure among hypertensive patients [39, 40]. In HCHS/SOL, participants used a sleep apnea monitor overnight, and individuals who were overweight or obese had a higher likelihood of sleep-disordered breathing. In addition, while 25.8% of the study population met criteria for sleep-disordered breathing, only 1.3% of participants reported carrying a clinical diagnosis of sleep apnea. In line with studies from other cohorts, Hispanics in HCHS/SOL with sleep apnea had a significantly higher likelihood of hypertension, with an odds ratio of 1.4 (95% confidence interval, 1.2, 1.7) after adjusting for demographic and clinical variables, including body mass index and waist circumference [41•].
Conclusions
The Hispanic American population is projected to be one of the fastest growing ethnic groups over the next several decades. While hypertension is common in both Hispanic and non-Hispanic ethnic groups, rates of uncontrolled hypertension are higher among Hispanics. Moreover, Hispanic ethnicity is comprised of several heterogeneous subgroups, and there is substantial variability in rates of hypertension among them. Clinical trial data suggest that barriers to hypertension management may be the primary drivers of this disparity. Culturally tailored, community-interventions may improve hypertension management and outcomes in the Hispanic population, but barriers to care, including access to high-quality health care and the preponderance of comorbidities such as obesity could impose significant challenges. Additional population studies such as HCHS/SOL and clinical trials in Hispanic patients of different ancestral heritages are needed to address these disparities.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
U.S. Census Bureau PD. Annual estimates of the resident population by sex, age, race, and Hispanic origin for the United States and States: April 1, 2010 to July 1, 2016. June 2017.
• Vespa J, Armstrong D, Medina L. Demographic turning points for the United States: population projections for 2020 to 2060. Current population reports US Census Bureau. 2018. Up-to-date projection of trends in demographics for the US population.
Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015-2016. NCHS Data brief. 2017;289:1–8.
•• Whelton Paul K, Carey Robert M, Aronow Wilbert S, Casey Donald E, Collins Karen J, Dennison Himmelfarb C, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension (Dallas, Tex : 1979). 2017;71(6):e13–e115 2018. Major clinical practice guideline for the evaluation and management of hypertension, including the lowering of the threshold for elevated blood pressure.
Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R, et al. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA). Am J Hypertens. 2004;17(10):963–70.
Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: the multi-ethnic study of atherosclerosis. Hypertension (Dallas, Tex : 1979). 2011;57(6):1101–7.
•• Daviglus ML, Talavera GA, Aviles-Santa ML, Allison M, Cai J, Criqui MH, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. Jama. 2012;308(17):1775–84 Report from HCHS/SOL evaluating the prevalence of cardiovascular risk factors in the US Hispanic/Latino population by ethnic subgroup.
•• Avilés-Santa ML, Sorlie PD, Allison MA, Howard AG, Cai J, LaVange LM, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic community health study/study of Latinos. Am J Hypertens. 2014;27(6):793–800 Report from HCHS/SOL evaluating treatment and control of hypertension in Hispanic/Latino population.
Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167(8):962–9.
Schargrodsky H, Hernández-Hernández R, Champagne BM, Silva H, Vinueza R, Silva Ayçaguer LC, et al. CARMELA: assessment of cardiovascular risk in seven Latin American cities. Am J Med. 2008;121(1):58–65.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23.
Centers for Disease Control and Prevention (CDC). Hypertension-related mortality among Hispanic subpopulations--United States, 1995-2002. MMWR Morb Mortal Wkly Rep. 2006;55(7):177–80.
Wright JT Jr, Dunn JK, Cutler JA, Davis BR, Cushman WC, Ford CE, et al. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. Jama. 2005;293(13):1595–608.
•• Margolis KL, Piller LB, Ford CE, Henriquez MA, Cushman WC, Einhorn PT, et al. Blood pressure control in Hispanics in the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Hypertension (Dallas, Tex : 1979). 2007;50(5):854–61 Results of anti-hypertensive therapies among Hispanics in the ALLHAT trial, showing effective blood pressure lowering.
•• Cooper-DeHoff RM, Aranda JM, Gaxiola E, Cangiano JL, Garcia-Barreto D, Conti CR, et al. Blood pressure control and cardiovascular outcomes in high-risk Hispanic patients—findings from the International Verapamil SR/Trandolapril Study (INVEST). Am Heart J. 2006;151(5):1072–9 Results of anti-hypertensive therapies among Hispanics in the PREVENT trial, showing effective blood pressure lowering.
A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Rodriguez CJ, Still CH, Garcia KR, Wagenknecht L, White S, Bates JT, et al. Baseline blood pressure control in Hispanics: characteristics of Hispanics in the Systolic Blood Pressure Intervention Trial. J Clini Hypertens (Greenwich, Conn). 2017;19(2):116–25.
• Still CH, Rodriguez CJ, Wright JT Jr, Craven TE, Bress AP, Chertow GM, et al. Clinical outcomes by race and ethnicity in the Systolic Blood Pressure Intervention Trial (SPRINT): a randomized clinical trial. Am J Hypertens. 2017;31(1):97–107 Analysis showing that outcomes in the SPRINT trial of aggressive blood pressure lowering did not vary by Hispanic ethnicity.
Park IU, Taylor AL. Race and ethnicity in trials of antihypertensive therapy to prevent cardiovascular outcomes: a systematic review. Ann Fam Med. 2007;5(5):444–52.
• Langabeer James R, Henry Timothy D, Perez Aldana C, DeLuna L, Silva N, Champagne-Langabeer T. Effects of a community population health initiative on blood pressure control in Latinos. J Am Heart Assoc. 2018;7(21):e010282 Study showing community-based interventions addressing cultural barriers can improve hypertension in Latinos.
Rocha-Goldberg Mdel P, Corsino L, Batch B, Voils CI, Thorpe CT, Bosworth HB, et al. Hypertension Improvement Project (HIP) Latino: results of a pilot study of lifestyle intervention for lowering blood pressure in Latino adults. Ethn Health. 2010;15(3):269–82.
Fang J, Yang Q, Ayala C, Loustalot F. Disparities in access to care among US adults with self-reported hypertension. Am J Hypertens. 2014;27(11):1377–86.
Redmond N, Baer HJ, Hicks LS. Health behaviors and racial disparity in blood pressure control in the national health and nutrition examination survey. Hypertension (Dallas, Tex : 1979). 2011;57(3):383–9.
Liao Y, Bang D, Cosgrove S, Dulin R, Harris Z, Taylor A, et al. Surveillance of health status in minority communities - racial and ethnic approaches to community health across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. Morb Mortal Wkly Rep Surveill Summ (Washington, DC : 2002). 2011;60(6):1–44.
Sorlie PD, Allison MA, Aviles-Santa ML, Cai J, Daviglus ML, Howard AG, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27(6):793–800.
Moran A, Diez Roux AV, Jackson SA, Kramer H, Manolio TA, Shrager S, et al. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20(4):354–63.
Eamranond PP, Wee CC, Legedza ATR, Marcantonio ER, Leveille SG. Acculturation and cardiovascular risk factor control among Hispanic adults in the United States. Public Health Reports (Washington, DC : 1974). 2009;124(6):818–24.
Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter. J Gen Intern Med. 2010;25(11):1172–7.
Carlson SA, Fulton JE, Schoenborn CA, Loustalot F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. Am J Prev Med. 2010;39(4):305–13.
• Arredondo EM, Sotres-Alvarez D, Stoutenberg M, Davis SM, Crespo NC, Carnethon MR, et al. Physical activity levels in U.S. Latino/Hispanic adults: results from the Hispanic community health study/study of Latinos. Am J Prev Med. 2016;50(4):500–8 Study from HCHS/SOL reporting objective accelerometer-based measures of physical activity among Hispanics.
• Merchant G, Buelna C, Castañeda SF, Arredondo EM, Marshall SJ, Strizich G. Accelerometer-measured sedentary time among Hispanic adults: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prev Med Rep. 2015;2:845–53 Study from HCHS/SOL reporting objective accelerometer-based measures of sedentary behavior among Hispanics.
Gutierrez AP, McCurley JL, Roesch SC, Gonzalez P, Castañeda SF, Penedo FJ, et al. Fatalism and hypertension prevalence, awareness, treatment and control in US Hispanics/Latinos: results from HCHS/SOL Sociocultural Ancillary Study. J Behav Med. 2017;40(2):271–80.
Hall John E, do Carmo Jussara M, da Silva Alexandre A, Wang Z, Hall Michael E. Obesity-induced hypertension. Circ Res. 2015;116(6):991–1006.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief. 2017;288:1–8.
• Cheung EL, Bell CS, Samuel JP, Poffenbarger T, Redwine KM, Samuels JA. Race and obesity in adolescent hypertension. Pediatrics. 2017;139(5):e20161433 Large study of adolescents reporting on the cross-sectional association of obesity with early hypertension, with the greatest association observed in Hispanic youth.
McLaughlin T, Abbasi F, Lamendola C, Reaven G. Heterogeneity in the prevalence of risk factors for cardiovascular disease and type 2 diabetes mellitus in obese individuals: effect of differences in insulin sensitivity. Arch Intern Med. 2007;167(7):642–8.
Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003-2006. Natl Health Stat Reports. 2009 (13):1–7.
• Heiss G, Snyder ML, Teng Y, Schneiderman N, Llabre MM, Cowie C, et al. Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: the Hispanic Community Health Study/Study of Latinos. Diabetes Care. 2014;37(8):2391–9 Study from HCHS/SOL reporting the prevalence of the metabolic syndrome among different Hispanic ethnic subgroups.
Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–84.
Martinez-Garcia MA, Capote F, Campos-Rodriguez F, Lloberes P, Diaz de Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. Jama. 2013;310(22):2407–15.
• Redline S, Sotres-Alvarez D, Loredo J, Hall M, Patel SR, Ramos A. Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds. The Hispanic Community Health Study/Study of Latinos. Am J Respir Crit Care Med. 2014;189(3):335–44 Study from HCHS/SOL reporting the high rate of sleep-disordered breathing among Hispanic individuals.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Implementation to Increase Blood Pressure Control: What Works?
Rights and permissions
About this article
Cite this article
Thomas, I.C., Allison, M.A. Hypertension in Hispanics/Latinos: Epidemiology and Considerations for Management. Curr Hypertens Rep 21, 43 (2019). https://doi.org/10.1007/s11906-019-0947-6
Published:
DOI: https://doi.org/10.1007/s11906-019-0947-6